Cholangiocarcinoma is an aggressive tumor of the biliary epithelium that commonly presents at an advanced inoperable stage. Early identification and intervention could improve the poor prognosis. Intraductal papillary neoplasm of the bile duct (IPNB) is a premalignant precursor of cholangiocarcinoma and constitutes 10% to 15% of all bile-duct tumors.1 IPNB is classified by its pathologic features into 4 subtypes: pancreatobiliary, intestinal, gastric, and oncocytic.2 The grade of intraepithelial neoplasia is defined as low-to-intermediate, high, or invasive carcinoma.
A 71-year-old woman had abnormal liver function test results detected by routine screening. She had never had jaundice or symptoms of biliary obstruction. Her medical history included hypertension, GERD, thyroid disease that required radioiodine treatment, total abdominal hysterectomy, and bladder lesions that required regular transurethral removal of bladder tumor. Physical examination revealed a lower-midline laparotomy scar from a previous hysterectomy, but was otherwise unremarkable.
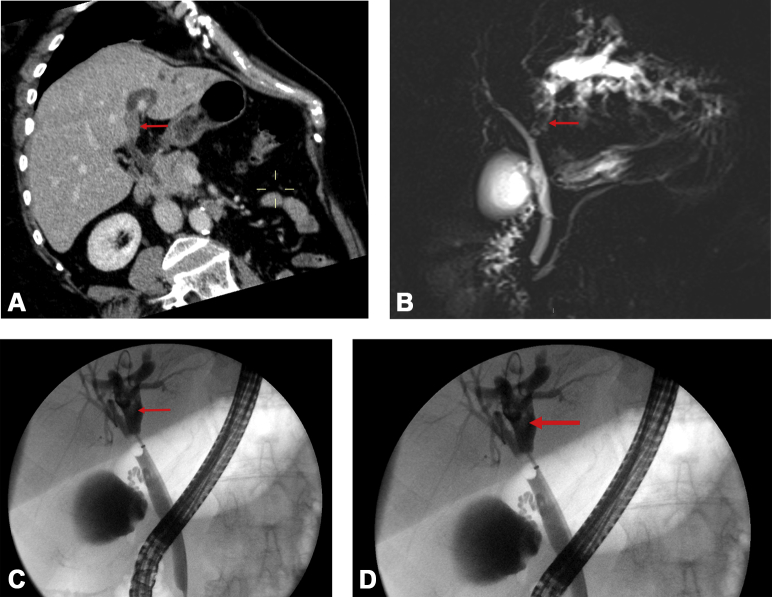
Abdominal US, CT of the abdomen (Fig. 1A), and MRCP (Fig. 1B) all showed dilatation of the left intrahepatic biliary system with a lesion in the left hepatic duct impinging on the hilar confluence, suggestive of a small cholangiocarcinoma. After discussion, the multidisciplinary team recommended an extended left hepatectomy to include the caudate lobe and radical bile duct excision until the exact location and pathologic features were determined.
Figure 1.
A, CT view showing hyperdense lesion (red arrow) in the left main hepatic duct and left intrahepatic biliary dilatation. B, MRCP view showing a filling defect (red arrow) in the left main hepatic duct close to the hilar bifurcation and left intrahepatic biliary dilatation. C, D, ERCP views showing a filling defect (red arrows) in the left hepatic duct with left intrahepatic biliary dilatation.
Before surgery, a triple-phase CT of the liver showed a stable appearance of the left hepatic duct lesion and no other hepatic abnormalities. In addition, ERCP and SpyGlass cholangioscopy (Boston Scientific, Marlborough, Mass) were performed to determine the exact nature of the lesion. Cholangiography showed a normal right ductal system but a clear filling defect in the left hepatic duct (Figs. 1C and D). SpyGlass cholangioscopy showed a villous tumor in the left hepatic duct, which was clear of the bifurcation and approximately 1 cm above it (Fig. 2). The cholangioscope passed the tumor easily after 2 to 3 cm into normal-looking ducts in segments II to IV (Video 1, available online at www.VideoGIE.org). Spybite biopsy specimens were taken, and a long straight plastic stent was placed to decompress the left ductal system.
Figure 2.

SpyGlass cholangioscopic view revealing a large villous tumor in the left hepatic duct, which was clear of the bifurcation and approximately 1 cm above it.
Examination of biopsy specimens from the lesion showed papillary low-grade dysplasia with no evidence of malignancy. Given the potential for malignant transformation and the suspicion of cholangiocarcinoma, the decision was made to proceed to a standard left hepatectomy and cholecystectomy. Pathologic examination of the resected left hepatectomy specimen showed IPNB, gastric type, that had been completely excised. There was low-to-intermediate grade dysplasia within the lesion but no definite evidence of invasion (Figure 3, Figure 4C). The patient made a good recovery and did not require any adjuvant therapy or further investigation.
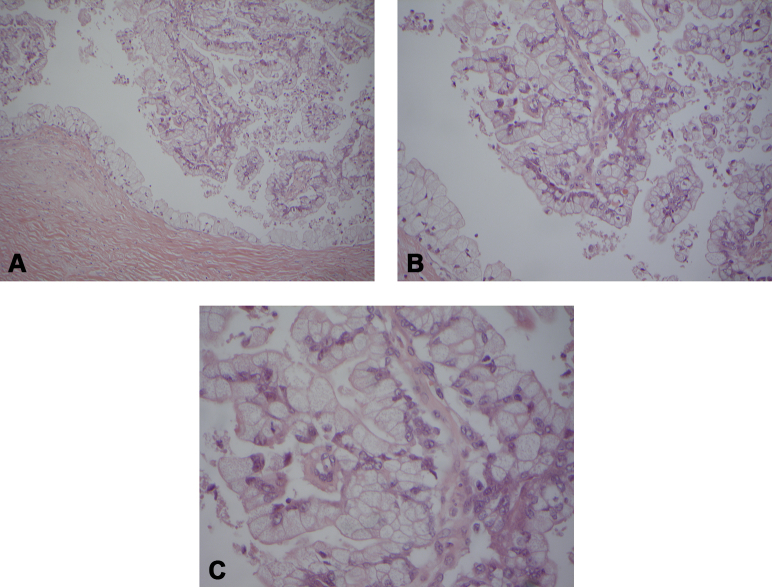
Figure 3.

Macroscopic appearance of the resected specimen showing the intraductal tumor (white arrow) within the left main hepatic duct.
Figure 4.
Histopathologic slides showing intraductal papillary neoplasm of the bile duct, gastric type, with low-to-intermediate dysplasia, but no invasion (A, H&E, orig. mag. x10, B, H&E, orig. mag. x20, C, H&E, orig. mag. x40.).
This case report illustrates the invaluable role of direct cholangioscopy in the workup of IPNB. Although cross-sectional imaging demonstrated intrahepatic biliary dilatation secondary to an intraductal lesion, the precise location and exact nature of the lesion were not definite. SpyGlass cholangioscopy allowed not only direct visualization of the lesion to pinpoint its location but also tissue sampling of the lesion to facilitate pathologic diagnosis. Exclusion of disease involvement at the hilar confluence during cholangioscopy helped inform the surgical approach and the extent of resection required. In this case, a standard left hepatectomy was sufficient to achieve oncologic clearance, avoiding a more extensive extended left hepatectomy, including caudate lobe resection and radical bile duct excision with Roux-en-Y reconstruction.
Because of its rarity in the Western world and its propensity to masquerade as biliary stone disease, IPNB remains a diagnostic challenge. Successful management of IPNB therefore relies on a multimodal imaging approach, including the use of SpyGlass cholangioscopy and input from all members of the hepatobiliary multidisciplinary team.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Video showing the utility of SpyGlass cholangioscopy in determining the location of the intraductal tumor and in facilitating tissue diagnosis.
References
- 1.Egri C., Yap W.W., Scudamore C.H. Intraductal papillary neoplasm of the bile duct: multimodality imaging appearances and pathological correlation. Can Assoc Radiol J. 2017;68:77–83. doi: 10.1016/j.carj.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Nakanuma Y., Curado M., Fransceschi S. Intrahepatic cholangiocarcinoma. In: Bosman F.T., Carneiro F., Hruban R.H., editors. IARC WHO classification of tumours of the digestive system. 4th ed. France; Lyon: 2010. pp. 217–227. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video showing the utility of SpyGlass cholangioscopy in determining the location of the intraductal tumor and in facilitating tissue diagnosis.