Abstract
Primary cutaneous extraskeletal osteosarcoma (PCEO) is a rare malignant neoplasm with less than 20 cases reported in the literature to date. Presenting as a nodule or mass on the skin, commonly at sites of previous trauma or radiation, these lesions are differentiated from other neoplasms through their characteristic microscopic appearance. This report highlights a case of PCEO in a 75-year-old man with a history of squamous cell carcinoma (SCC) of the scalp. Histological examination of a scalp nodule in the region of a previously excised SCC revealed proliferation of osteoid surrounded by malignant osteocytes. An overview of this condition and differential diagnoses are presented in this report.
Keywords: pathology, dermatology, plastic and reconstructive surgery, head and neck surgery, skin cancer
Background
Extraskeletal osteosarcomas (ESOS) are rare, with only 2%–4% of osteosarcomas identified outside the skeletal system.1 Cutaneous ESOS are even rarer. The majority of these are metastatic in nature, but primary cutaneous ESOS (PCEO) have also been described in literature.2 However, due to their relative scarcity, very little is known about its presentation and behaviour.
Case presentation
A 75-year-old man with a medical history of ischaemic heart disease, previous coronary artery bypass grafts and an internal cardiac defibrillator in situ, presented with multiple ulcerating plaques on the scalp. Two years prior to his current presentation, he underwent excision of a scalp squamous cell carcinoma (SCC). The SCC was excised under local anaesthesia and subsequently, the patient underwent brachytherapy for the residual tumour. Part of the frontoparietal bone was exposed a year after the brachytherapy, which showed no evidence of tumour recurrence. The current ulcers were present in the vicinity of the previous excision and in view of the history of high risk SCC, they were considered to be highly suspicious of recurrence.
Investigations
An initial biopsy confirmed recurrence of SCC. A separate nodule adjacent to the ulcer was also biopsied. This showed a cellular dermal tumour composed of pleomorphic mitotically active spindle cells, positive for CD10, smooth muscle actin (SMA) with weak patchy p63 positivity. Immunostains for cytokeratins, S100, CD34, desmin and CD99 were negative. The differential diagnosis of this nodule included a spindle cell SCC and atypical fibroxanthoma. Following the biopsy, the entire lesion was excised. The excision specimen contained predominantly a poorly differentiated SCC. But the nodule revealed, apart from the proliferation of atypical spindle-shaped cells identified during the initial biopsy, central malignant osteoid formation rimmed by atypical osteocytes (figures 1-4). Immunohistochemistry showed focal positivity for SMA, while S100 protein showed a subpopulation of presumed dendritic cells. Results for cytokeratins AE1/AE3 and CK5/6, CD34, desmin, h-caldesmon, Melan A and HMB45 were all negative. CD10 was diffusely positive in the spindle cell component but weak and patchy in the region of the malignant osteoid. Morphologically, the appearances were those of an osteosarcoma, and in view of its location, and the absence of a primary bone osteosarcoma on a full body CT scan, this was considered to be a PCEO. Unfortunately, clinical photographs are not available as the possibility of this diagnosis was not considered preoperatively.
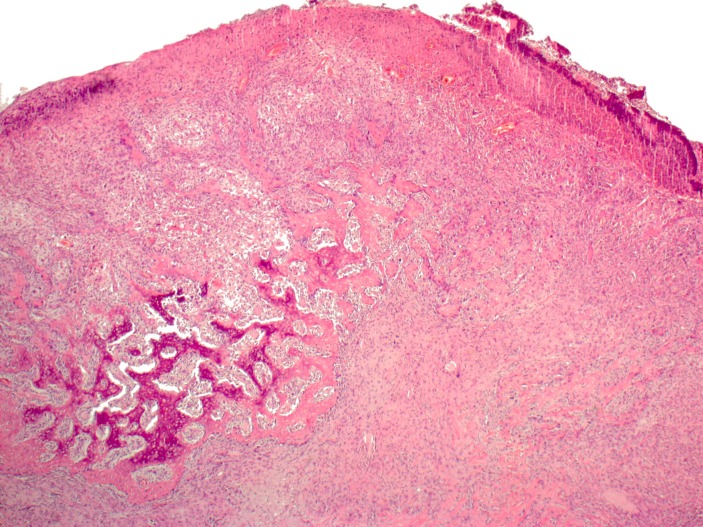
Figure 1.
Ulcerated nodule showing central ossification surrounded by atypical pleomorphic spindle cell population (H&E, ×2.5).
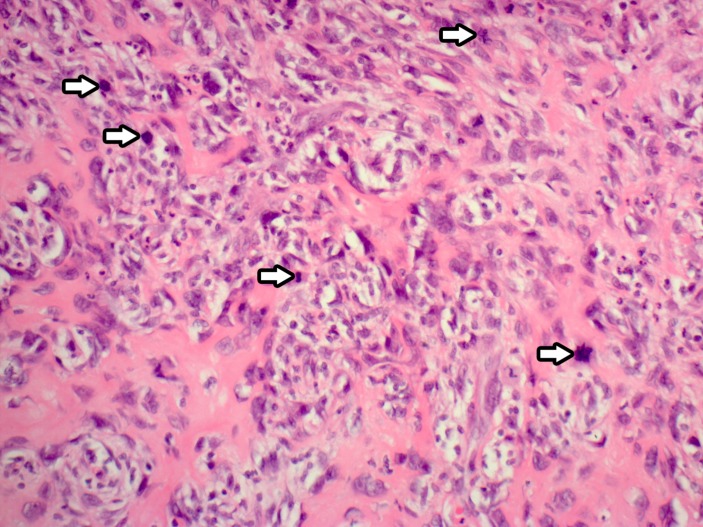
Figure 2.
High-power view of the malignant cells with areas of ossification. Mitosis is prominently seen (arrows) (H&E, ×10).
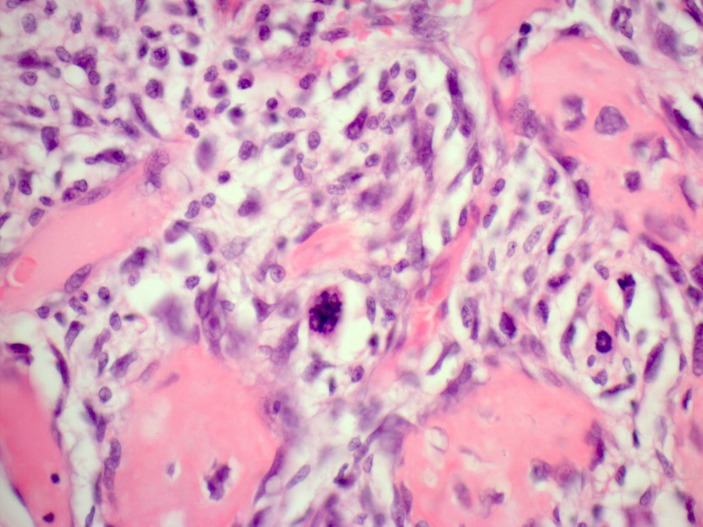
Figure 3.
High-power view (H&E, ×20) showing osteoid rimmed by large atypical cells.
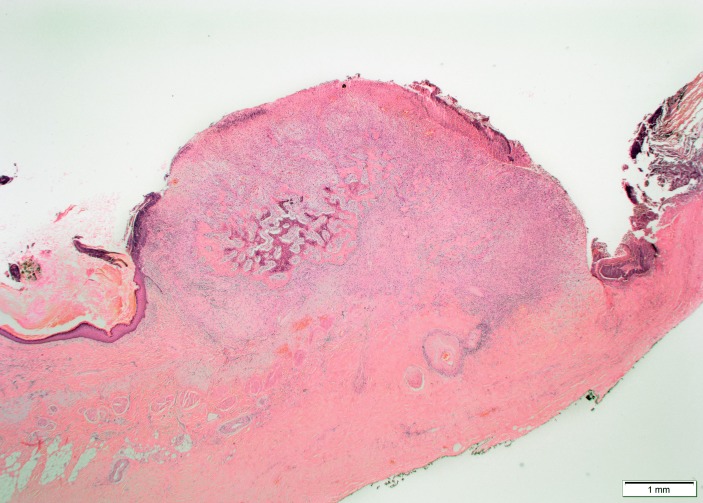
Figure 4.
Panoramic view of the lesion (H&E).
Differential diagnosis
For PCEO, the differential diagnoses include primary ossification of the skin (osteoma cutis) or metaplastic ossification following on from trauma, radiation or inflammation. Ossification may also be seen in a variety of neoplasms including melanoma, pleomorphic sarcoma, basal cell carcinoma, intradermal nevus, pilomatricoma, chondroid syringoma or metastasis.1 3 4 The proliferation of atypical cells with conspicuous mitosis in this case is in keeping with a malignant neoplasm rather than osteoma cutis. While we considered this case could represent a heterologous differentiation in sarcomatoid SCC; this diagnosis is unlikely due to the negative cytokeratin immunohistochemistry,5 though a heterologous dedifferentiation cannot be excluded completely. The fact that SSC was present nearby to the lesion raises the possibility of divergent differentiation or tumour collision. Though divergent differentiation cannot be entirely excluded, this is unlikely as the SSC was present separate to this nodule with no evidence of tumour collision (figure 4).
Furthermore, a diagnosis of postradiation sarcoma was also considered; however, the time interval between radiation and presentation was rather short (2 years). The average latency period of sarcoma following radiation therapy is reported to be around 12 years.6 7 This case therefore, represents an example of PCEO.
Outcome and follow-up
In the months following the surgical excision of the nodule, the patient had recurrence of SCC in the scalp and pinna with the lesions undergoing successful excision. The patient declined surgical intervention of further lesions. The patient’s exposed calvarium started to appear non-viable (osteonecrosis). After extensive assessment and discussion with the patient, it was agreed to continue with conservative management. A CT scan 38 months after the surgery revealed widespread SCC metastasis.
Discussion
PCEO is an uncommon neoplasm which, although arising separately from bone, exhibits osteoid or chondroid-producing cells.8 As far as we are aware, less than 20 cases of PCEO have been reported in literature.9 The presentation is usually as a cutaneous nodule or mass in elderly patients, increasing in size and at times associated with pain.10 The mean age of development is 70 years. Some of these lesions occurred on the cephalic area at sites of previous radiation, trauma or scars.2 9 Histologically, six distinct subtypes of ESOS have been described: osteoblastic, chondroblastic, fibroblastic, small cell, telangiectatic and well differentiated.10 A recent report in 2016 presented two cases of PCEO, one with an ulcerated tumour in the left hand of a patient with a background of colonic carcinoma and another patient with an ulcerated nodule on the ear pavilion.11 The positivity of the immunohistochemistry marker SATB2 in PCEO is described, similar to that observed in primary osteosarcoma of the bone.11 As it becomes more widely available, SATB2 is likely to assist in the differentiation of osteosarcoma from its histological mimics.
The aggressive nature of the tumour and tendency to metastasise, most readily to the lungs, means 5-year survival is below 40%.9 Though treatment for PCEO is not standardised due to its rarity, it is treated with surgical excision and can be combined with chemotherapy or radiotherapy.12 A recent case report of PCEO on the temple being successfully treated with Mohs micrographic surgery has been described13 giving a greater insight into the treatment options for PCEO.
Learning points.
Extraskeletal osteosarcomas (ESOS) can rarely arise from the skin with less than 20 cases of primary cutaneous ESOS (PCEO) reported in the literature.
These lesions present as a cutaneous nodule or mass and have been reported to occur on sites of previous trauma or radiation.
Differential diagnoses of PCEO are numerous and histological subtypes of ESOS are defined by the predominant characteristic of the matrix of the cells.
Footnotes
Contributors: YAl-J’s role was in the writing of the article, gaining information from patient case notes, reviewing the research. KAl-J’s role was in diagnosis of the case, contribution to case report writing and planning. KT’s role was in patient management, contribution to case writing and planning. MP’s role was his contribution to case writing and planning, obtaining and annotating histology slides.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Riddle ND, Bowers JW, Bui MM, et al. . Primary cutaneous osteoblastic osteosarcoma: a case report and review of the current literature. Clin Exp Dermatol 2009;34:e879–e880. 10.1111/j.1365-2230.2009.03637.x [DOI] [PubMed] [Google Scholar]
- 2.Park SG, Song JY, Song IG, et al. . Cutaneous extraskeletal osteosarcoma on the scar of a previous bone graft. Ann Dermatol 2011;23:S160 10.5021/ad.2011.23.S2.S160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Massi D, Franchi A, Leoncini G, et al. . Primary cutaneous osteosarcoma of the scalp: a case report and review of the literature. J Cutan Pathol 2007;34:61–4. 10.1111/j.1600-0560.2006.00562.x [DOI] [PubMed] [Google Scholar]
- 4.Buehler D, Billings S. Soft tissue tumors and tumor-like reactions Busam K, Dermatopathology. 2nd ed Philadelphia: PA: Elsevier, 2016. [Google Scholar]
- 5.Hall JM, Saenger JS, Fadare O. Diagnostic utility of P63 and CD10 in distinguishing cutaneous spindle cell/sarcomatoid squamous cell carcinomas and atypical fibroxanthomas. Int J Clin Exp Pathol 2008;1:524–30. [PMC free article] [PubMed] [Google Scholar]
- 6.Lagrange J-L, Ramaioli A, Chateau M-C, et al. . Sarcoma after radiation therapy: retrospective multiinstitutional study of 80 histologically confirmed cases. Radiology 2000;216:197–205. 10.1148/radiology.216.1.r00jl02197 [DOI] [PubMed] [Google Scholar]
- 7.Makimoto Y, Yamamoto S, Takano H, et al. . Imaging findings of radiation-induced sarcoma of the head and neck. Br J Radiol 2007;80:790–7. 10.1259/bjr/20938070 [DOI] [PubMed] [Google Scholar]
- 8.Llamas-Velasco M, Rütten A, Requena L, et al. . Primary cutaneous osteosarcoma of the skin. Am J Dermatopathol 2013;35:e106–e113. 10.1097/DAD.0b013e31827f0a6f [DOI] [PubMed] [Google Scholar]
- 9.Lee MA, Yi J, Chae JM. Cutaneous osteosarcoma arising from a burn scar. Skeletal Radiol 2017;46:547–51. 10.1007/s00256-016-2565-6 [DOI] [PubMed] [Google Scholar]
- 10.Salamanca J, Dhimes P, Pinedo F, et al. . Extraskeletal cutaneous chondroblastic osteosarcoma: a case report. J Cutan Pathol 2008;35:231–5. 10.1111/j.1600-0560.2007.00785.x [DOI] [PubMed] [Google Scholar]
- 11.Falconieri G, Cataldi P, Kavalar R, et al. . Cutaneous osteoblastic osteosarcoma: report of 2 new cases integrated with SATB2 immunohistochemistry and review of the literature. Am J Dermatopathol 2016;38:824–31. 10.1097/DAD.0000000000000555 [DOI] [PubMed] [Google Scholar]
- 12.Gardner J, Smoller B. Primary cutaneous extraskeletal osteosarcoma In: Rongioletti F, Margaritescu I, Smoller B, eds Rare Malignant Skin Tumors. New York: Springer, 2015:201. [Google Scholar]
- 13.Barnes L, Carroll B. Primary cutaneous osteosarcoma of the temple treated with Mohs micrographic surgery. J Am Acad Dermatol 2017;6(Suppl. 1):AB204. [DOI] [PubMed] [Google Scholar]