Abstract
A 10-year-old girl presented with episodes of migraine. A nasal mass was found randomly during work-up. Interpreted as an osteoma, the mass was removed during endoscopic surgery. However, the histopathological examination turned out to be a pyomucocele in the right middle turbinate, which is an extremely rare yet benign condition in children.
Keywords: otolaryngology / ent, paediatric surgery, radiology
Background
A concha bullosa is an aeration of a turbinate and is considered a quite normal finding in both adults1 and children.2 It is one of the most frequent anatomical variants of the middle turbinate in adults and can compromise the natural drainage of the surrounding sinuses or cause stenosis of the nasal cavity.3 4 A mucocele inside a turbinate is a mucus-filled sack with epithelial lining in contrast to other types of mucoceles where the epithelial lining is absent. Bacterial contamination may eventually lead to a localised infection, a pyomucocele. Such turbinate pyomucoceles are rare conditions with only three paediatric cases previously described.5 6
Case presentation
A 10-year-old girl was referred to our tertiary university centre because of a right-sided nasal mass radiologically described as a random finding during work-up because of suspected migraine.
During the preceding months, the girls’ mother had found her daughter’s voice to be more nasal than usual and the girl had developed snoring, right-sided nasal stenosis and a constant ipsilateral, serous nasal discharge. She furthermore complained of effusion from her left ear during the previous 2–3 weeks.
A removal of both the middle turbinate and the tumour in general anaesthesia was scheduled.
Investigations
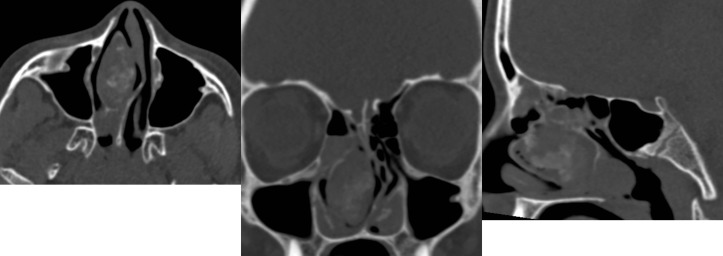
Neuroradiologists re-evaluated the CT and MRI scans obtained during the neurological work-up. An inhomogeneous tumour measuring 17.8×36×29 mm was described in the right nasal cavity. It was found to be confined within the right middle turbinate, the growth pattern was non-invasive and the mass was well defined with regards to the surrounding anatomical structures, though it displaced the nasal septum medially (figure 1).
Figure 1.
Non-enhanced CT scan of the sinonasal cavity, axial, coronal and sagittal view, showing a mucopyocele involving the right concha bullosa.
Differential diagnosis
Nasal polyposis.
Benign or malignant neoplasm of any origin (eg, carcinoma, osteoma, sarcoma, lymphoma).
Meningocele or encephalocele.
Treatment
During an endoscopic end nasal approach and by the use of perioperative navigation via prior CT scans and computer-assisted surgery, the tumour was removed in toto.
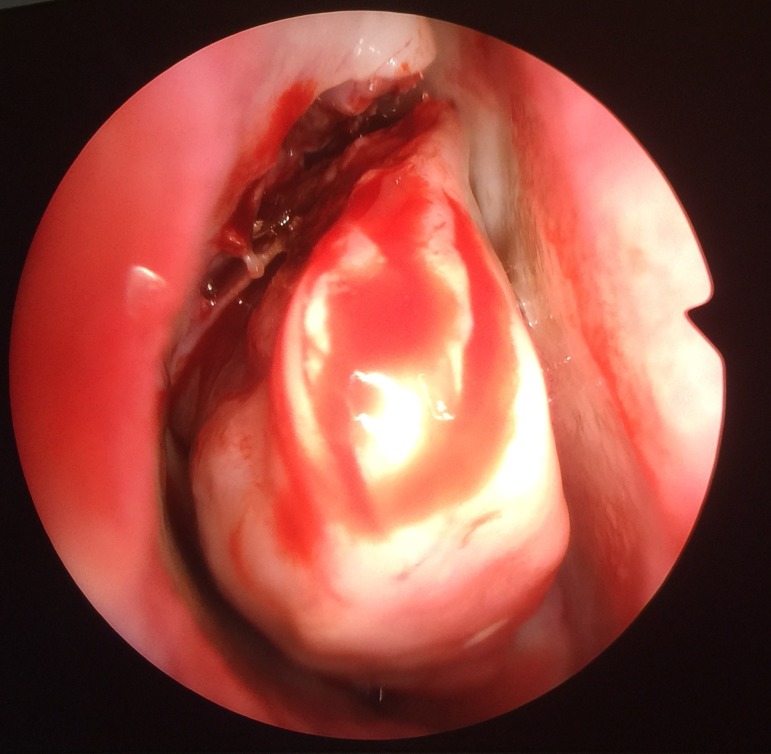
The endoscopic examination confirmed the radiological findings of an expanding non-infiltrative mass (figure 2). Thus, removal was possible by right middle turbinectomy, during which a thick pus-like substance was seen leaking from the turbinate. This led us to suspect the diagnosis, which was later confirmed by the pathologists.
Figure 2.
Perioperative view of the middle right turbinate.
Outcome and follow-up
At follow-up 1 month after the procedure, the girl had experienced no complications and reported no nasal symptoms. She still complained of intermittent effusions from her left ear. At 6-month follow-up, her mucosa was normalised and she had no symptoms.
Histology showed pseudostratified columnar epithelium with groups of plasma cells and lymphocytes as well as trabecular bone. All consistent with the diagnosis of a pyomucocele originating from the right middle turbinate.
Discussion
Concha bullosas are common in children. They are often asymptomatic and correlate poorly with sinus disease, as does any other intranasal anatomical variations.2 3 In this case, however, it seems logical that the bacterial contamination of the mucocele caused continuous expansion of the turbinate, which eventually led to nasal obstruction. In previously described cases, headache and nasal obstruction are also predominant symptoms.6 Surgical removal of the turbinate and thus the mucocele/pyomucocele is the standard procedure and usually relieves the patient from all symptoms. Interestingly, concha bullosas have been reported to cause migraine.7 In our case, the pyomucocele might explain the headaches, and certainly the nasal obstruction, but we cannot explain the neurological symptoms interpreted as aura by the paediatricians. Most likely the timely debut of migraine was a coincidence.
A pyomucocele cannot be differentiated from a mucocele on a CT scan.6 This is important, as the infection of a pyomucocele might spread to important surrounding anatomical structures like the orbit and the brain.8 Furthermore, mucoceles might be mistaken for a neoplasm and vice versa. In this light, mucoceles and pyomucoceles of the turbinates should always be surgically removed, even if they cause no symptoms.
While sinonasal pathology is rare in children, malignancy in this area is easily overlooked, nasal tumours being rare and difficult to ascertain9 while providing sparse and non-specific symptoms.
Ongoing nasal symptoms, that is, congestion, drip, nosebleeds or pain, should always and with no regards to the age of the patient prompt further investigation, especially if the symptom is unilateral. An endoscopic rhinopharyngolaryngoscopy is in such cases mandatory.
This case highlights a very rare finding with symptoms mimicking sinusitis or the presence of adenoid tissue. It is a reminder of the importance of a thorough examination despite harmless symptomatology.
Learning points.
Unilateral nasal symptoms should in all cases prompt further investigations including nasoendoscopy and CT scans.
A pyomucocele/mucocele should be considered a potential differential diagnosis in case of patients presenting a nasal mass in close proximity to one of the nasal turbinates.
Endoscopic removal of the affected concha is recommended, yet a final histopathological diagnosis is always important to obtain.
Footnotes
Contributors: All authors have made substantial contributions to the conception or design of the work and acquisition, analysis and interpretation of data for the work, drafting the work or revising it critically for important intellectual content. All authors gave final approval of the version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Zinreich SJ, Mattox DE, Kennedy DW, et al. Concha bullosa: CT evaluation. J Comput Assist Tomogr 1988;12:778–84. [DOI] [PubMed] [Google Scholar]
- 2.Eryilmaz A, Göçer C, Dursun E, et al. The incidence of anatomic variations and sinus opacities in pediatric patients with chronic sinonasal symptoms. Kulak Burun Bogaz Ihtis Derg 2004;13:116–21. [PubMed] [Google Scholar]
- 3.Kim HJ, Jung Cho M, Lee JW, et al. The relationship between anatomic variations of paranasal sinuses and chronic sinusitis in children. Acta Otolaryngol 2006;126:1067–72. 10.1080/00016480600606681 [DOI] [PubMed] [Google Scholar]
- 4.Stallman JS, Lobo JN, Som PM. The incidence of concha bullosa and its relationship to nasal septal deviation and paranasal sinus disease. AJNR Am J Neuroradiol 2004;25:1613–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen SD, Matthews BL. Large concha bullosa mucopyocele replacing the anterior ethmoid sinuses and contiguous with the frontal sinus. Ann Otol Rhinol Laryngol 2008;117:15–17. 10.1177/000348940811700104 [DOI] [PubMed] [Google Scholar]
- 6.Khalife S, Marchica C, Zawawi F, et al. Concha bullosa mucocele: a case series and review of the literature. Allergy Rhinol 2016;7:233–43. 10.2500/ar.2016.7.0179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shihada R, Luntz M. A concha bullosa mucopyocele manifesting as migraine headaches: a case report and literature review. Ear Nose Throat J 2012;91:E16–18. [DOI] [PubMed] [Google Scholar]
- 8.Marianowski R, Farragi M, Zerah M, et al. Subdural empyema complicating a concha bullosa pyocele. Int J Pediatr Otorhinolaryngol 2002;65:249–52. 10.1016/S0165-5876(02)00174-X [DOI] [PubMed] [Google Scholar]
- 9.Holsinger FC, Hafemeister AC, Hicks MJ, et al. Differential diagnosis of pediatric tumors of the nasal cavity and paranasal sinuses: a 45-year multi-institutional review. Ear Nose Throat J 2010;89:534–40. [PubMed] [Google Scholar]