Geospatial epidemiology has a long history. From Snow's [1] famous investigation of the 1854 cholera outbreak in London to today, observing diseases in relation to people, place, and time has been essential for understanding and responding to epidemics. In 2016, the response to HIV/AIDS sustained more than 17 million people worldwide on lifesaving antiretroviral treatment [2]. Yet in the current era of falling donor support [3] and with governments of low-income countries needing to balance many spending priorities, it is vital to maximize the impact and efficiency of the AIDS response. National and international stakeholders have increasingly supported geospatial targeting of resources as a means to accomplish this [4–6], and the challenge for program designers has become how best to link the ‘who’ and ‘where’ with the ‘what’ and ‘when’. However, a key question is whether geospatial efforts ultimately translate into more effective interventions to reduce HIV incidence. We contend here that geospatial analysis has indeed delivered some successes thus far, but that the gap between academic studies and the needs of policy-setters must be narrowed if its full potential is to be realized.
Until recently, data limitations meant that intervention policies were designed under an assumption of homogeneous HIV epidemics. But with improvements in data availability and sophistication, it is now well established that the HIV epidemic and its drivers are highly heterogeneous, with studies confirming spatial variation between provinces [7], districts [8,9], and at finer scales [10–14] in sub-Saharan Africa. Even in generalized HIV epidemics, incidence may be concentrated in certain regions or population groups, such as slums in Kenya, periurban regions of South Africa, and fishing communities in Uganda [15]. Policies that fail to account for such heterogeneity are inherently biased and will leave some places and populations underserved, limiting overall effectiveness and equity.
Geospatial analysis exploits spatiotemporal information by integrating it into traditional classification and regression techniques to predict surfaces at a variety of spatial resolutions. This requires describing the factors underpinning patterns observed in sparse data, with geographic information leveraged from multiple sources (ranging from satellite imagery to expert opinion) alongside structured spatiotemporal correlations. Gaussian processes and other shrinkage estimators enable geospatial methods to both uncover the drivers of transmission and generalize accurately to new unseen data, and embedding these methods in a Bayesian statistical framework allows for rigorous treatment of uncertainty. Moreover, the methods can be synthesized with mechanistic representations of epidemic dynamics – including transmission – to place epidemiological constraints on the underlying functional process. Table 1 gives a brief overview of important methods for geospatial analysis, with examples of applications and findings in the setting of sub-Saharan Africa.
Table 1.
Methods for geospatial analysis with (nonexhaustive) examples of applications and findings.
| Method | Reference | Geographical unit and location | Key findings |
| Spatial interpolation methods | Zulu et al. [16] | Subnational (district) level in Malawi | An application of inverse distance weighting suggested that intervention strategies should emphasize improved access to health/HIV services, basic education, and syphilis management, particularly in rural hotspot districts |
| Messina et al. [17] | Subnational (second administrative) level in the Democratic Republic of Congo | Inverse distance weighting highlighted the importance of improved surveillance systems in Democratic Republic of Congo and the use of spatial analytical methods for understanding the determinants of HIV infection and geographic patterns of prevalence | |
| Larmarange and Bendaud [18] | Subnational level in six countries in sub-Saharan Africa | Kernel density estimates were developed with the aim to help countries better understand their HIV epidemics and inform programing at lower geographical levels | |
| Cuadros et al. [19] | National level in four countries in sub-Saharan Africa | A method was presented for generating high-resolution maps of international HIV prevalence based on Kriging interpolation of spatial variables | |
| Spatial statistics | Wabiri et al. [20] | District level in South Africa | High HIV prevalence districts have very homogeneous population defined by unfavorable sex ratio (high proportion of females), low socioeconomic status, being single, having multiple sexual partners, and intergenerational sex |
| Coburn et al. [21] | Local level in Lesotho | United Nations Programme on HIV/AIDS targets for treatment coverage may be infeasible for highly spatially dispersed rural populations | |
| Tanser et al. [22] | Micro-geographical level in South Africa | Despite clear evidence of spatial clustering of high viral loads in some communities, commonly-used population viral load (PVL) metrics did not predict prospective HIV incidence. Only combining viral load information with the underlying spatial variation in the proportion of the population infected was found to have a consistently strong relationship with HIV incidence | |
| Cuadros and Abu-Raddad [23] | National level in several countries in sub-Saharan Africa | Spatial clusters of HIV sero-discordancy overlap with those for HIV prevalence and are not distinct in sub-Saharan Africa | |
| Tanser et al. [24] | Microgeographical level in South Africa | Clear ‘corridors of transmission’ were identified where new HIV infections were clustered. Though these clusters comprise just 6.8% of the study area, they account for one out of every four sero-conversions observed over the study period | |
| Bayesian geoadditive models | Ngesa et al. [25] | Subnational (district) level in Kenya | Local HIV prevalence maps established significant spatial variation of HIV infection among men in Kenya |
| Kandala et al. [26] | Subnational (district) level in Botswana | Botswana was found to exhibit clear geographic variation in its HIV epidemic, with the highest prevalence occurring in the east-central districts of the country. This study provided maps that could be used for the targeting of HIV programs and efficient allocation of resources to higher risk groups | |
| Wand et al. [10] | Local level in South Africa | Significant spatial patterns were found that could not be explained by demographic or sexual risk behaviors | |
| Niragire et al. [27] | Subnational (district) level in Rwanda | Areas of Rwanda where women are at a higher risk of infection were identified. Distinctive geographic patterns of the risk of HIV infection suggested the potential effectiveness of district-specific interventions | |
| HIV transmission models calibrated to spatially averaged local data | Anderson et al. [28] | Subnational (county) level in Kenya | Targeting prevention interventions by population and place was found to be more impactful than a nontargeted approach under a limited budget in Kenya |
| McGillen et al. [29] | Subnational (provincial) level in 18 countries in sub-Saharan Africa | On a large scale, key populations may be more important than locations for efficient spending, but prioritizing both was the most impactful strategy over a range of continental budgets |
Geospatial analysis holds great potential for improving the efficiency of both a single program at a given level of spending (economic efficiency) and the allocation of limited funds across several programs (allocative efficiency). The specific aim of a geospatial analysis could be, for example, to help target HIV testing to the subnational units (e.g. districts) with the highest HIV burden or prevalence in a country, or to explore how prevention interventions can be combined in different locations and populations for maximum cost-effectiveness under national [28] or continental [29] spending limitations. A recent spatial regression of HIV in South Africa [20] showed that high-prevalence districts had several factors in common (including an unfavorable sex ratio, low socioeconomic status, and intergenerational sex), illustrating the importance of such factors for guiding programs and calling attention to the need for more local-level data collection and analysis. A study of layered maps of HIV prevalence and demographic factors at fine resolution in Lesotho [21] revealed that United Nations Programme on HIV/AIDS targets for treatment coverage may be hindered or even rendered infeasible by high spatial population dispersion in rural areas. New mapping efforts aiming to characterize HIV prevalence at very high resolution in multiple countries in sub-Saharan Africa [19] could provide essential information for strategic resource targeting. However, these high-resolution maps are constrained by data scarcity, with community surveillance data not always available. Additional data sources for mapping the risk of HIV infection, such as population prevalence of detectible viremia [22], routinely collected clinic-based antenatal HIV prevalence data (DF Cuadros, personal communication), and HIV sero-discordant couples [23], are thus being evaluated. All available data, including from new sources where possible, should be incorporated in geospatial analysis.
Much existing literature has been dedicated to improving the accuracy of geospatial modeling, often by prioritizing model complexity over ease or speed of analysis. However, this has left a gap between the modeling and its relevance to real-world policy change. A major challenge for geospatial analysis is now: What is the appropriate spatial resolution? This question must be answered at three stages during any analysis if the gap between theory and application is to be bridged.
First, geospatial modeling requires the integration of a variety of data sources at different levels of resolution and spatial locations. For example, data on HIV prevalence and risk behaviors may be available from national surveys, such as the Demographic and Health Surveys (DHS) (Fig. 1), whereas program data on the provision of antiretroviral therapy may be available only from selected clinics with access to an electronic monitoring system. Moreover, high-risk subpopulations – particularly mobile individuals and migration patterns – could be underrepresented by population-based samples such as DHS, and the contribution of these core groups to the spatial structure of HIV may be missed, although the impact of such undersampling on maps of generalized epidemics is not yet clear. The granularity of input data may have an effect on model predictions that dominates any other factors. In a recent comparison of six geospatial methods for modeling HIV, the Subnational Working Group of the HIV Modelling Consortium [30] found that the accuracy of model predictions and the magnitude of model error depended more on country-specific HIV prevalence estimates and the type of survey sample from which data were drawn, and less on the analytical method used. With the continual generation of new data, it is becoming essential to have a geospatial framework that can integrate multiple data sources, making sure that no single data source overwhelms the others or biases the signal.
Fig. 1.
Demographic and Health Survey sample locations (blue dots).
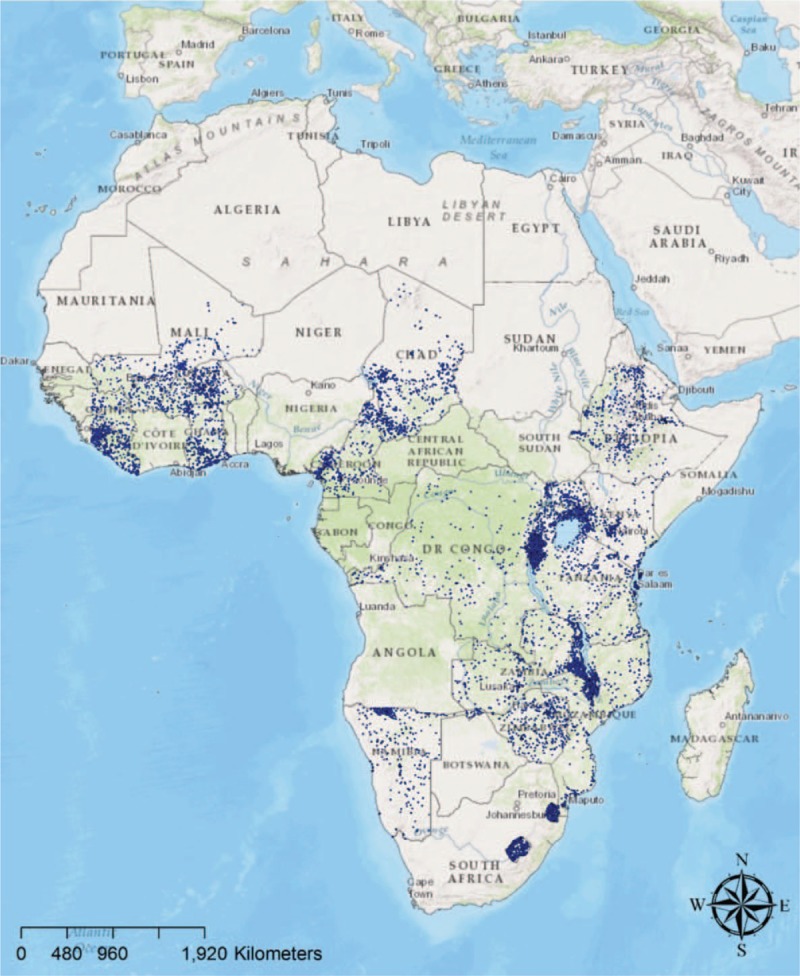
The Demographic and Health Survey has conducted samples including geographical information in more than 20 countries in sub-Saharan Africa, for a total of 8510 datapoints sampled. Maps were created using ArcGIS software by Esri, version 10.3 [31].
Second, the granularity of model results must be appropriate for the administrative and decision structures of the country or countries of interest, as well as their monitoring and evaluation capacity (e.g. refer to Fig. 2). Otherwise, results may be produced, for example, at the provincial level for reasons of data availability when budgetary responsibility for HIV programs lies at the district or facility level. However, the precision and accuracy of estimates becomes limited at smaller scales, and whereas model results can easily be aggregated to higher administrative levels, it is much more difficult to disaggregate results to lower levels without recourse to additional data manipulation, which is often based on weaker evidence than what was included in the model. A balance must therefore be struck between politics, data availability, and the reliability of the analytical method. A further mismatch may occur between modeling results and coverage targets for interventions set by program planners or international funding bodies. Extrapolation of, for example, clinic-level survey data for target-setting across small geographical units may not make sense if some of those units do not contain a clinic that requires targets. In our view, there is an optimally useful geographical level for model outputs, and this does not always need to be the lowest possible level. Models must also retain the flexibility to adjust to changing political boundaries. Interventions based on model-derived targets should be amenable to monitoring, and, optimally, there should be structures in place at this level which have a mandate to monitor. If monitoring by civil society bodies is not currently done, tools similar to AIDSvu [32–34] – maps of data on HIV epidemics in the United States which are interactive and publicly available online – could be beneficial. In general, the research question at hand will determine the exact point of intersection between the geographic scale of decision-making and the scale at which modeling techniques are adding value.
Fig. 2.
Using data from Demographic and Health Surveys conducted in 10 countries in eastern sub-Saharan Africa, HIV prevalence was mapped at three different scales of aggregation: (a) national level, (b) district level, and (c) high resolution mapping of 1 km2 pixel resolution using a Kriging interpolation technique.
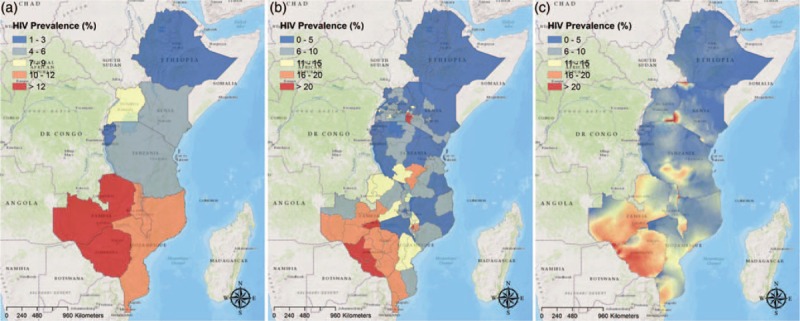
Maps were created using ArcGIS software by Esri, version 10.3 [31].
Third, recommendations that come out of geospatial analyses should be translated into policy with caution. Oversimplification of geospatial conclusions may result in lower impact than the theoretical maximum [35,36] due to funds being trapped in allocations which are locally inefficient. Models may also be naive to the additional costs of changing intervention programs or implementing them only in certain regions or populations in a country. In addition, local socioeconomic or cultural determinants of demand for interventions may affect the success of policies derived from models which did not take those factors into account. There is a further danger that the geo-location of small areas and populations at high risk of HIV transmission or acquisition may lead to stigma and discrimination against those groups, who are often already vulnerable or marginalized. The enormous benefits of geospatial analysis in terms of understanding epidemic dynamics and allocating resources efficiently may thus be offset by detrimental social consequences for the very people it aims to help. To avoid this, substantial efforts are undertaken to preserve the confidentiality of survey participants, such as the global positioning system displacement process for DHS sampling data points [37]. Similarly, when using geospatial analyses to rank administrative units by progress toward an HIV indicator – such as HIV prevalence, number of people living with HIV, or coverage of an intervention – it must be remembered that the objective function measuring this progress is highly context-specific.
Although geospatial analysis has not yet led to direct policy change, the semispatial study by Anderson et al.[28] provides an early step in this direction and will be used here as an example of how our recommendations could be applied. Using Kenya as a case study, Anderson et al. developed a mathematical model of HIV transmission and explored the potential impact of resource allocation strategies designed at different geographical scales. To calibrate the model, the authors integrated data from several sources, disaggregated to the local level. Counties (similar to districts elsewhere) and major cities were selected as the local unit of analysis as they corresponded to the finest resolution of both budget decisions and available input data in Kenya. The authors extracted information from official reports on historical scale-up of treatment and prevention, and data on sexual behaviors in the population from national surveys, with a literature review and mapping of key populations providing data on MSM in Kenya's urban settings. For information on HIV prevalence, geostatistical techniques were used to interpolate between sample cluster locations in antenatal clinic and household survey data, generating county-level averages. A maximum-likelihood fit between model parameters and these data was found for each local unit in Kenya. Using this calibrated HIV model, Anderson et al. characterized the potential impact, in terms of aggregate infections averted, of making decisions at the national level (i.e. rolling out prevention interventions uniformly across the country) versus the subnational level (tailoring interventions to specific populations and counties). The authors found the locally focused approach could reduce HIV infections by 33% per year than the national-level approach for the same total cost. This study lent support to the Kenya Strategic Framework for 2014/15–2018/19, developed by the National AIDS Control Council of Kenya to guide the devolution of programmatic decision-making for the country's HIV response to the county level. However, political and practical issues associated with focusing resources on certain areas of a socioculturally complex country continue to pose challenges.
In general, although geospatial analysis can uncover the locations of vulnerable populations suffering a high transmission burden, it cannot yet reveal the behavioral and biological drivers of the uneven geographical distribution of the epidemic, quantify the role of ‘hotspots’ in the transmission dynamics of the entire community, or convey a comprehensive picture of the changing epidemic over time. The field is now moving toward the integration of geospatial dynamics with transmission models that would be able to elucidate this information. If geographical ’hotspots’ play a role similar to behavioral core groups in the transmission networks of concentrated epidemics, then it is possible that targeting these places would not only impact HIV incidence within the ‘hotspot’ but also disrupt the much wider transmission network surrounding it. Phylogenetic analysis, phylogeography, and network diffusion analysis techniques could be combined to depict geographical transmission networks of large-scale communities and thereby advance our understanding of this critical issue.
In summary, geospatial analysis needs to be able to integrate data generated at different locations and levels of resolution. Its results need to be disaggregated or aggregated to the level that is most relevant for decision-making, budgeting, and monitoring (including the district or facility levels). Recommendations based on it need to safeguard against oversimplification and against stigmatizing communities, and should bear in mind that progress toward targets is context-specific and might involve behavioral or biological factors not included in the analysis.
In the HIV response, a model contributes just one piece of information to a complex decision process that may also include political concerns, budgetary constraints, and priorities that reach beyond direct health impact, such as national economic development. Nevertheless, geospatial analysis can be a valuable component of this decision-making landscape. In our view, the way forward is a flexible, pragmatic approach that seeks to establish the decision and monitoring structures in a country or countries via continual engagement with decision-makers and provision of model results at the most appropriate level for each step of the engagement.
Acknowledgements
Research toward this article was made possible by the generous support of the American people through the US Agency for International Development (USAID) under award number AID 674-A-12-00029 (G.M.R.'s time). J.B.M. and T.B.H. thank the Bill & Melinda Gates Foundation for funding through a grant to the HIV Modelling Consortium at Imperial College London. The authors wish to thank the Measure Demographic and Health Surveys (Measure DHS) for publishing national surveys in service of science and USAID and other donors for supporting those initiatives.
Support/disclosures: G.M.R. reports funding through USAID under award number AID 674-A-12-00029. J.B.M. and T.B.H. report funding from the Bill & Melinda Gates Foundation in the form of a grant to the HIV Modelling Consortium at Imperial College London.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Snow J. Mode of communication of cholera. 2nd ed.London: John Churchill; 1855. [Google Scholar]
- 2.Joint United Nations Programme on HIV/AIDS (UNAIDS). AIDS Info dashboard. Geneva, Switzerland. URL: http://aidsinfo.unaids.org/ [Accessed 31 July 2017]. [Google Scholar]
- 3.Kaiser Family Foundation and UNAIDS. Report: donor government funding for HIV in low- and middle-income countries in 2016. July 2017. URL: http://files.kff.org/attachment/Report-Donor-Government-Funding-for-HIV-in-Low-and-Middle-Income-Countries-in-2016 [Accessed 31 July 2016]. [Google Scholar]
- 4.Joint United Nations Programme on HIV/AIDS (UNAIDS). Location, location: connecting people faster to HIV services. Geneva, Switzerland; 2013. [Google Scholar]
- 5.PEPFAR. PEPFAR 3.0 – controlling the epidemic: delivering on the promise of an AIDS-free generation. Washington, DC, USA; 2017. Available at: https://www.pepfar.gov/documents/organization/234744.pdf [Accessed 31 July 2017]. [Google Scholar]
- 6.The Global Fund. The Global Fund strategy 2017–2022: investing to end epidemics. Geneva, Switzerland; 2017. Available at: https://www.theglobalfund.org/media/2531/core_globalfundstrategy2017-2022_strategy_en.pdf [Accessed 31 July 2017]. [Google Scholar]
- 7.Shaikh N, Abdullah F, Lombard CJ, Smit L, Bradshaw D, Makubalo L. Masking through averages – intraprovincial heterogeneity in HIV prevalence within the Western Cape. 2006; 96:538–543. [PubMed] [Google Scholar]
- 8.Kleinschmidt I, Pettifor A, Morris N, MacPhail C, Rees H. Geographic distribution of human immunodeficiency virus in South Africa. 2007; 77:1163–1169. [PMC free article] [PubMed] [Google Scholar]
- 9.Coburn BJ, Okano JT, Blower S. Current drivers and geographic patterns of HIV in Lesotho: implications for treatment and prevention in sub-Saharan Africa. 2013; 11:224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wand H, Whitaker C, Ramjee G. Geoadditive models to assess spatial variation of HIV infections among women in Local communities of Durban, South Africa. 2011; 10:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wand H, Ramjee G. Targeting the hotspots: investigating spatial and demographic variations in HIV infection in small communities in South Africa. 2010; 13:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tanser F, Bärnighausen T, Newell M. Identification of localized clusters of high HIV incidence in a widely disseminated rural South African epidemic: a case for targeted intervention strategies. , Boston, MA, USA, 2011. [Google Scholar]
- 13.Cuadros DF, Awad SF, Abu-Raddad LJ. Mapping HIV clustering: a strategy for identifying populations at high risk of HIV infection in sub-Saharan Africa. 2013; 12:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aral SO, Torrone E, Bernstein K. Geographical targeting to improve progression through the sexually transmitted infection/HIV treatment continua in different populations. 2015; 10:477–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tanser F, de Oliveira T, Maheu-Giroux M, Bärnighausen T. Concentrated HIV sub-epidemics in generalized epidemic settings. 2014; 9:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zulu LC, Kalipeni E, Johannes E. Analyzing spatial clustering and the spatiotemporal nature and trends of HIV/AIDS prevalence using GIS: the case of Malawi. 2014; 14:285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Messina JP, Emch M, Muwonga J, Mwandagalirwa K, Edidi SB, Mama N, et al. Spatial and socio-behavioral patterns of HIV prevalence in the Democratic Republic of Congo. 2010; 71:1428–1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larmarange J, Bendaud V. HIV estimates at second subnational level from national population-based surveys. 2014; 28:S469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cuadros DF, Li J, Branscum AJ, Akullian A, Jia P, Mziray EN, Tanser T. Mapping the spatial variability of HIV infection in sub-Saharan Africa: effective information for localized HIV prevention and control. 2017; 7:9093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wabiri N, Shisana O, Zuma K, Freeman J. Assessing the spatial nonstationarity in relationship between local patterns of HIV infections and the covariates in South Africa: a geographically weighted regression analysis. 2017; 16:88–99. [DOI] [PubMed] [Google Scholar]
- 21.Coburn BJ, Okano JT, Blower S. Using geospatial mapping to design HIV elimination strategies for sub-Saharan Africa. 2017; 9:eaag0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tanser F, Vandormael A, Cuadros D, Phillips AN, de Oliveira T, Tomita A, Bärnighausen T, Pillay D. Effect of population viral load on prospective HIV incidence in a hyper-endemic rural African community. 2017; 9:eaam8012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cuadros DF, Abu-Raddad LJ. Geographical patterns of HIV sero-discordancy in high HIV prevalence countries in Sub-Saharan Africa. 2016; 13:865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tanser F, Bärnighausen T, Sartorius B. Identifying ‘corridors of HIV transmission’ in a severely affected rural South African population: a case for a shift toward targeted prevention strategies. 2017. dyx257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ngesa O, Mwambi H, Achia T. Bayesian spatial semi-parametric modeling of HIV variation in Kenya. 2014; 9:e103299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kandala NB, Campbell EK, Rakgoasi SD, Madi-Segwagwe BC, Fako TT. The geography of HIV/AIDS prevalence rates in Botswana. 2012; 4:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niragire F, Achia TN, Lyambabaje A, Ntaganira J. Bayesian mapping of HIV infection among women of reproductive age in Rwanda. 2015; 10:e0119944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson SJ, Cherutich P, Kilonzo N, Cremin I, Fecht D, Kimanga D, et al. Maximising the effect of combination HIV prevention through prioritisation of the people and places in greatest need: a modelling study. 2014; 384:249–256. [DOI] [PubMed] [Google Scholar]
- 29.McGillen JB, Anderson S-J, Dybul MR, Hallett TB. Optimum resource allocation to reduce HIV incidence across sub-Saharan Africa: a mathematical modelling study. 2016; 3:e441–e448. [DOI] [PubMed] [Google Scholar]
- 30.The Subnational Estimates Working Group of the HIV Modelling Consortium. Evaluation of geospatial methods to generate subnational HIV prevalence estimates for local level planning. 2016; 30:1467–1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.ESRI. ArcGIS 10.x. 2004; Redlands, CA, USA:Available at: http://www.esri.com/. [Accessed 31 July 2017]. [Google Scholar]
- 32.Nunn A, Yolken A, Cutler B, Trooskin S, Wilson P, Little S, Mayer K. Geography should not be destiny: focusing HIV/AIDS implementation research and programs on microepidemics in US neighborhoods. 2014; 104:775–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goswami ND, Schmitz MM, Sanchez TH, Dasgupta S, Sullivan P, Cooper H, Waller LA. Understanding local spatial variation along the care continuum: the potential impact of transportation vulnerability on HIV linkage to care and viral suppression in high-poverty areas. 2016; 72:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dasgupta S, Kramer MR, Rosenberg ES, Sanchez TH, Sullivan PS. Development of a comprehensive measure of spatial access to HIV provider services, with application to Atlanta, Georgia. 2016; 5:984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McGillen JB, Anderson S-J, Hallett TB. PrEP as a feature in the optimal landscape of combination HIV prevention in sub-Saharan Africa. 2016; 19 suppl 6:21104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Anderson SI, Ghys PD, Ombam R, Hallett TB. HIV prevention where it is needed most: comparison of strategies for the geographical allocation of interventions. 2017; 20:e25020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burget CR, Colston J, Roy T, Zachary B. Geographic displacement procedure and georeferenced data release policy for the Demographic and Health Surveys. . Calverton, Maryland, USA: ICF International; 2013. [Google Scholar]


