Supplemental digital content is available in the text.
Key Words: patient safety, cost, harm reduction, DRG, contribution margin, readmissions, mortality, length of stay, Global Trigger Tool
Abstract
Objective
The aim of this study was to determine the impact of all-cause inpatient harms on hospital finances and patient clinical outcomes.
Research Design
A retrospective analysis of inpatient harm from 24 hospitals in a large multistate health system was conducted during 2009 to 2012 using the Institute of Healthcare Improvement Global Trigger Tool for Measuring Adverse Events. Inpatient harms were detected and categorized into harm (F–I), temporary harm (E), and no harm.
Results
Of the 21,007 inpatients in this study, 15,610 (74.3%) experienced no harm, 2818 (13.4%) experienced temporary harm, and 2579 (12.3%) experienced harm. A patient with harm was estimated to have higher total cost ($4617 [95% confidence interval (CI), $4364 to 4871]), higher variable cost ($1774 [95% CI, $1648 to $1900]), lower contribution margin (−$1112 [95% CI, −$1378 to −$847]), longer length of stay (2.6 d [95% CI, 2.5 to 2.8]), higher mortality probability (59%; odds ratio, 1.4 [95% CI, 1.0 to 2.0]), and higher 30-day readmission probability (74.4%; odds ratio, 2.9 [95% CI, 2.6 to 3.2]). A patient with temporary harm was estimated to have higher total cost ($2187 [95% CI, $2008 to $2366]), higher variable cost ($800 [95% CI, $709 to $892]), lower contribution margin (−$669 [95% CI, −$891 to −$446]), longer length of stay (1.3 d [95% CI, 1.2 to 1.4]), mortality probability not statistically different, and higher 30-day readmission probability (54.6%; odds ratio, 1.2 [95% CI, 1.1 to 1.4]). Total health system reduction of harm was associated with a decrease of $108 million in total cost, $48 million in variable cost, an increase of contribution margin by $18 million, and savings of 60,000 inpatient care days.
Conclusions
This all-cause harm safety study indicates that inpatient harm has negative financial outcomes for hospitals and negative clinical outcomes for patients.
Fifteen years after the report To Err Is Human: Building a Better Health System by the Institute of Medicine (IOM) and more than 3 years after the implementation of the Affordable Care Act, patient safety remains a major challenge for the U.S. health care system today. A recent IOM report suggests that, in the United States, one-third of all hospital patients experience harm during their stay and, each year, more than 400,000 preventable hospital deaths occur.1,2 Despite significant developments in patient safety interventions, reduction in patient harm has been elusive, exemplified by a 5-year study of North Carolina hospitals that failed to show improvement in patient safety.3 Similarly, the 2010 Office of Inspector General study demonstrated that 27% of Medicare patients experience harm during their hospitalization.4 These findings have led government calls to action through programs to improve patient safety. The Centers for Medicare and Medicaid Services program Partnership for Patients has strategic goals to make care safer through 40% reduction in preventable harms and 20% reduction in readmissions.5 Although the Partnership for Patients program has focused narrowly on patient safety problems using the Medicare Patient Safety Monitoring System to assess individual harms, such as central line–associated bloodstream infections and pressure ulcers, these efforts have failed to address broader all-cause harm issues.6
Identifying all-cause patient harm is challenging. Estimates of inpatient harms are often underreported and rely on self-reported events, the use of administrative data, or internal hospital incident reporting systems.7–11 Recently, hospitals and health systems have used the Institute for Healthcare Improvement (IHI) Global Trigger Tool (GTT) for Measuring Adverse Events. The GTT is a standardized, 2-stage review process refined from the Harvard Medical Practice Study's methodology to identify and measure the rate of all-cause harm over time in a variety of settings. It consists of a centralized team of registered nurse reviewers (primary reviewers) and physician authenticators (secondary reviewers).12 Institutions using the GTT have shown that as many as one-third of inpatients experience 1 or more harms during their stay.7,13,14 The economic costs of these patient safety problems are significant and variable depending on payor, provider, and setting of care. Although calculations of cost of harms are often focused on specific complications, our study objective was to measure all-cause inpatient harm impact on hospital financial measures such as total cost, variable cost, and contribution margin as well as clinical outcome measures such as length of stay (LOS), mortality, and readmissions.15–18
METHODS
Study Population and Data Collection
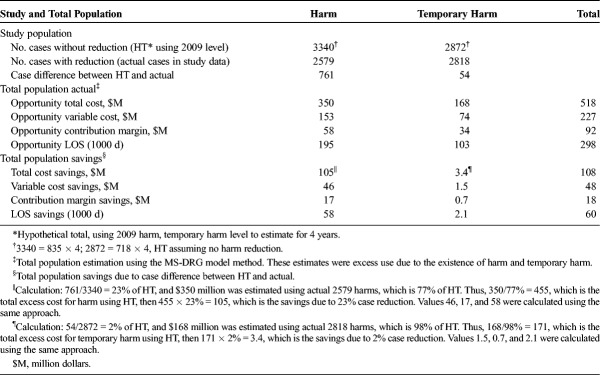
This study was conducted by a large multistate health system with a total of 716,172 hospital inpatient discharges across 24 hospitals in the Southern and Central U.S. regions from 2009 to 2012. Exclusions from this study population consisted of patients admitted for hospice, rehabilitation, and primary behavioral health; those younger than 18 years; or patients with an LOS of less than 1 day. Of the 566,325 discharges remaining, we used the IHI GTT to randomly review 20 patient charts per month for each of the 24 hospitals to detect patient harm, which generated our study population of 21,007 inpatients. A sample size of 23,040 was expected, but actual numbers were lower because of 171 cases in 2 small-bed hospitals and 1862 present-on-admission cases excluded (Fig. 1). Data points on each study patient included harm level, age, sex, race, admission status, LOS, discharge status, insurance payor, hospital name, principal International Classification of Diseases, Ninth Revision procedure and diagnosis codes, as well as present-on-admission indicator. In addition, we matched total cost, variable cost, contribution margin, Medicare Severity-Diagnosis Related Groups (MS-DRGs), DRG weight, inpatient mortality, readmissions (30/60/90/180/365-day), risk for mortality, and severity of illness.
FIGURE 1.
Flow Diagram for Study Population Selection.
Harm Identification
This study used a standardized centralized systematic review process to detect inpatient harm. This GTT methodology, which is refined from the Harvard Medical Practice Study's methodology, is a 2-stage review process.11 It had a centralized team of registered nurse reviewers (primary reviewers) and physician authenticators (secondary reviewers) for all records sampled from the 24 hospitals for 4 years and has achieved a high degree of interrater reliability (Supplemental Digital Content, http://links.lww.com/JPS/A14, Appendix Exhibit A1 and A2). This method was described in a prior report.19 In this study, we used the following definition for harm: “unintended physical injury resulting from or contributed to by medical care that requires additional monitoring, treatment, or hospitalization, or that results in death.”20 All events found were classified using an adaptation of the National Coordinating Council for Medication Error Reporting and Prevention's Index for Categorizing Errors: E, temporary harm requiring intervention; F, temporary harm requiring initial or prolonged hospitalization; G, permanent harm; H, intervention required to sustain life; and I, death.20 The inpatients in this study were classified as no harm, temporary harm (patients with ≥1 E events), or harm (patients with ≥1 F–I events).
Costs and Contribution Margin
This health system used a commercially available financial software to categorize actual general ledger expenses as either variable or fixed costs. Total cost included fixed and variable costs and is defined as all variable and fixed hospital expenditures required to provide direct patient care and to manage and operate the facility. Fixed costs are all expenditures that do not change with business volumes. Examples include management salaries and benefits as well as depreciation of equipment and buildings. Variable costs were defined as all expenditures that vary on the basis of changes in business volumes. Examples include nursing and other direct patient care salaries, benefits, supplies, and drugs. Each patient discharge was allocated a pro rata portion of the variable costs according to specific charges incurred. Contribution margin, an indicator of a hospital’s profitability, was defined as total actual payments minus variable costs.
Analysis
Aggregate
We analyzed the study population (21,007) with the use of descriptive statistics using a traditional hospital financial analysis approach to show means or percentages for age, sex, race, insurance payor, total cost, variable cost, contribution margin, DRG weight, mortality rate, and readmission rate by harm category. We also provided the total population (566,325) for comparison (Table 1). We calculated the difference of the means for harm versus no harm and temporary harm versus no harm in total cost, variable cost, contribution margin, and LOS. On the basis of the total number of harms reduced, we estimated the cost savings to the study population. We then used a multiplier, a ratio of the total population over the study population, to extrapolate the cost savings to the total population.
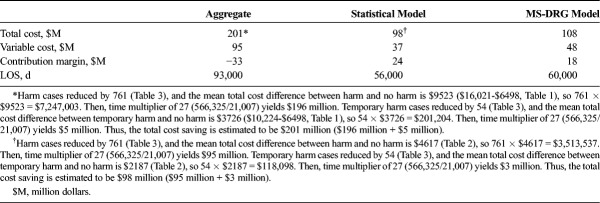
TABLE 1.
Summary Statistics of Patient Count, Demographics, and Financial and Clinical Outcomes by Inpatient Harm Category 2009 to 2012
Statistical Modeling
We applied a traditional health services research approach to the same data set using multivariate regression models and validated them against other models.21–26 We analyzed relationships between patient harms and financial and clinical outcomes using multivariate linear regression to estimate continuous outcome measures including costs, contribution margin, and LOS. Multivariate logistic models were used to estimate binary outcome measures including mortality and readmission.15,27 Both harm and temporary harm patients were modeled separately against no harm patients. To adjust for potential confounding factors, we included the following covariates in the models: DRG relative weight, age, sex, insurance payor, admission source, hospital, admission year, and MS-DRG. Discrete variables including race, insurance payor, admission source, hospital, admission year, and MS-DRG were coded as categorical variables; sex was coded as a binary variable. For each coded variable, we used the value with the largest percentage as default so it would not be included in the variable selection (defaults: female, white, Medicare, non–health care facility admission source, hospitals 23 and 24, admission year 2009, and MS-DRGs with fewer than 25 patients grouped as one). Model evaluation and refinements were also conducted (Supplemental Digital Content, http://links.lww.com/JPS/A14, Statistical Models Evaluation and Refinements Details Text). We used backward elimination methods to select significant independent variables in the model, with a P value of 0.05 or less as criterion. All tests and 95% confidence intervals (CIs) were 2 sided. P values less than 0.05 were considered statistically significant. For regression analysis, we reported our results in terms of estimated parameters, associated P values, and adjusted R2 values from each model. For the logistic model, we reported our results in terms of estimated odds ratios, associated P values, and c-statistics from each model.
To test the robustness of the model results and address potential hospital cluster effects, we used a hierarchical linear model for total cost, variable cost, contribution margin, and LOS as well as a hierarchical generalized linear model for 30-day readmission and mortality. The results of the hierarchical linear model and the hierarchical generalized linear model were very similar to linear regression and logistic model results, and significant hospital cluster effects were not found. We also tested a variety of severity adjustment approaches and found no significant change in the model outcomes with different severity adjusters. All statistical analyses were performed using SAS 9.3 software (SAS Institute Inc., Cary, NC). We used the parametric means of total cost, variable cost, contribution margin, and LOS for harm and temporary harm modeled against no harm and the case reduction to project cost savings to the study population. We projected the cost savings to the total population using the same multiplier described in the aggregate method above.
MS-DRG Model
Because the traditional hospital financial analytic approach and the health services research analytic approach had different results, we performed a hybrid analysis using aspects of both approaches to look at the same data set with a new model approach. This new approach used an MS-DRG model that is broadly applicable to hospital departments such as finance and revenue management to improve financial estimations. Because each patient falls into an MS-DRG and “DRGs are a meaningful way to group patients and procedures that fall together naturally,” our sensitivity-adjusted MS-DRG model calculates means at the DRG level.28 Of the 641 MS-DRGs in the study population, 383 had at least 1 harm. For MS-DRGs with large numbers of harm, we used the difference of means between harm and no harm, multiplied the difference by the number of harm cases in that MS-DRG, and extrapolated to the total population using its specific MS-DRG multiplier. The MS-DRG multiplier is the ratio of patients of an MS-DRG in the total population to the patients of the same MS-DRG in the study population. To account for MS-DRGs with small numbers of harm, we grouped them into 1 category. To obtain the optimal threshold, the minimum number of harms in each MS-DRG, we performed a sensitivity analysis by testing harms ranging from 1 to 50 (Supplemental Digital Content, http://links.lww.com/JPS/A14, Appendix Exhibit A3. MS-DRG Level Sensitivity Analysis Graphs). The final total population projection included all 383 MS-DRGs with harms (Supplemental Digital Content, http://links.lww.com/JPS/A14, Detailed MS-DRG Level Analysis Description Text).
RESULTS
Aggregate Financial Model Results
The descriptive statistics in Table 1 show that, of the 21,007 inpatients, 15,610 (74.3%) had no harm detected, 2818 (13.4%) experienced temporary harm, and 2579 (12.3%) had harm. We found that the mean total cost of hospitalization was $6498 for patients with no harm, $10,224 for patients with temporary harm, and $16,021 for patients with harm. The annual percentage of patients with harm declined during the study period. When projected to the total population, the total cost savings was $201 million, the variable cost savings was $95 million, and the contribution margin loss was $33 million. In addition, we found that LOS savings was 93,000 inpatient days.
Health Services Research Statistical Model Approach
The statistical models’ parametric mean estimation is shown in Table 2. In the regression analysis, both harm and temporary harm were positively correlated with total cost, variable cost, and LOS. The P values of harm and temporary harm were all significant at less than 0.0001. After controlling the covariates, on average, the patients with harm had $4617 more in total cost and $1774 more in variable cost than no harm, the patients with temporary harm had $2187 more in total cost and $800 more in variable cost than no harm, and the patients with harm stayed in the hospital 2.6 days longer and the patients with temporary harm stayed in the hospital 1.3 days longer than no harm. Harm and temporary harm reduced the contribution margin by $1112 and $669 per patient, respectively, compared with no harm. Multivariate logistic models showed that harm was associated with increased risk for mortality (odds ratio, 1.42; P = 0.0376) and risk for 30-day readmission (odds ratio, 2.88; P < 0.0001). Temporary harm was associated with increased risk for 30-day readmission (odds ratio, 1.20; P = 0.0062) but was not significantly correlated with mortality (Supplemental Digital Content, http://links.lww.com/JPS/A14, Detailed Model Results Text and Appendix Exhibit A4 and A5). When projected to the total population, savings for total cost was $98 million, variable cost was $37 million, contribution margin was $24 million, and LOS was 56,000 inpatient days.
TABLE 2.
Summary of Adjusted Model Parameter Estimate Results With 95% CI 2009 to 2012

MS-DRG Model Approach
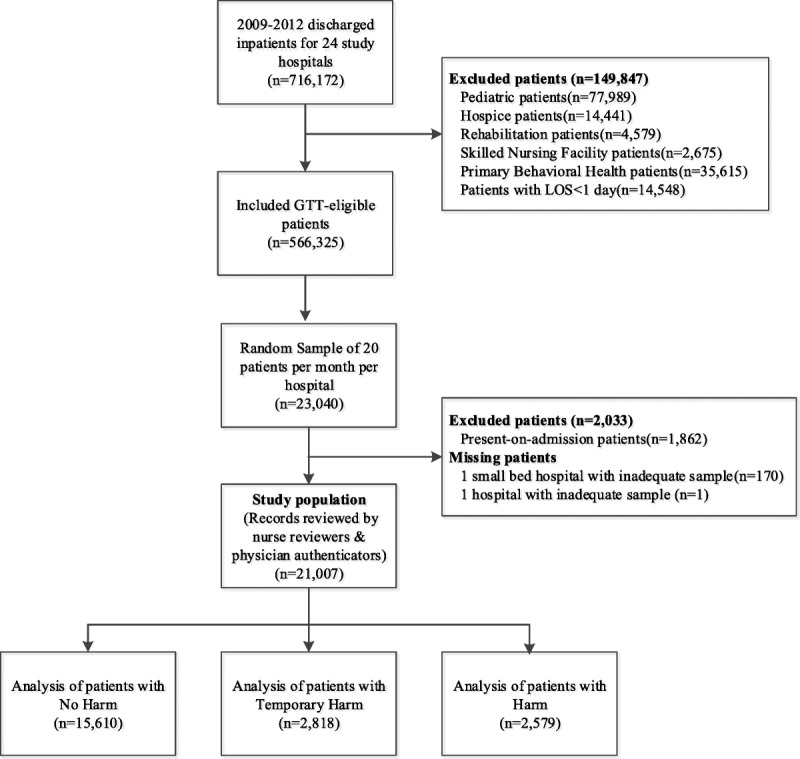
The MS-DRG model results are shown in Table 3. We observed a decrease in harm and a slight decrease in temporary harm during the study period. If we assume no decrease in harm, the total number of harms would be 3340 (hypothetical total [HT]) based on the 2009 harm level. However, the actual number of harm cases was 2579 (77% of HT), and harm decreased by 761 (23% of HT) cases. On the basis of the MS-DRG model estimation described above, we used the actual 2579 harms to calculate the “actual” excess use due to harm and calculated the “savings” based on harm reduction. The impact of temporary harm reduction was derived in the same manner. When projected to the total population, this health system saved $108 million in total cost, $48 million in variable cost, $18 million in contribution margin, and 60,000 inpatient days. However, most of the harms (77% harm and 98% temporary harm) still had a large negative financial impact on hospitals.
TABLE 3.
Harm Reduction and Financial Impact 2009 to 2012
Comparison of All 3 Models
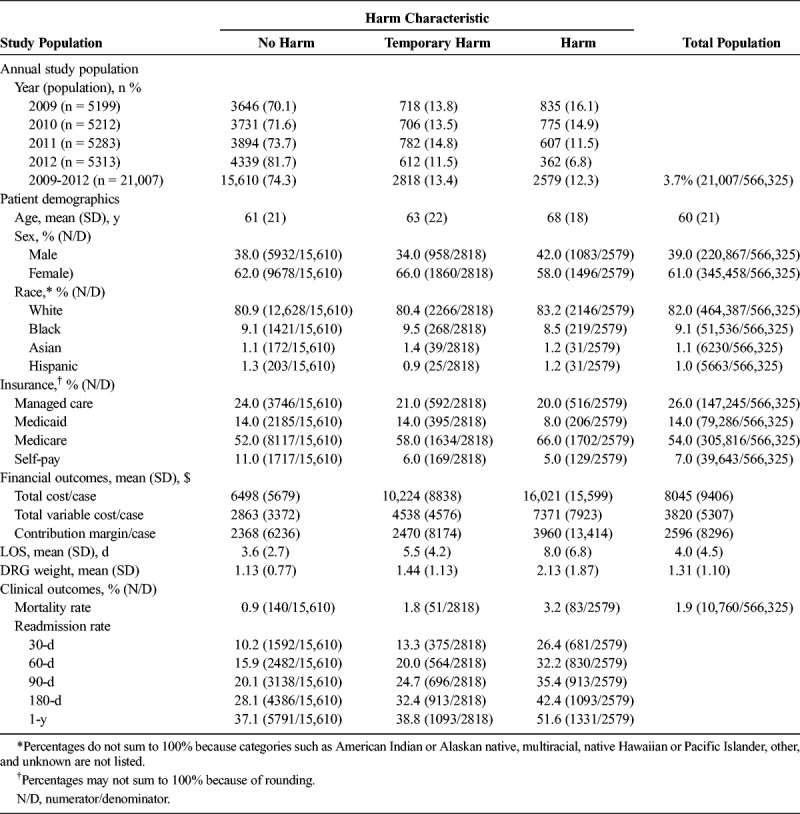
The comparison of total population costs, contribution margin, and LOS savings is shown in Table 4. Estimations from statistical and MS-DRG models are in agreement and different from the results of the aggregate approach.
TABLE 4.
Total Financial Impact of Harms Reduction by Different Methods 2009 to 2012
DISCUSSION
Among the 3 cost estimation models, the aggregate approach is typically used in cost analysis, which takes the grand mean of each harm category without weighing the cost differences among different MS-DRGs. It is an intuitive approach and easy to use; however, its results in this study are misleading and provide a mean in a nonnormal distribution, potentially overestimating the costs. Statistical models use parametric mean estimation and a single multiplier to estimate total population impact in this study. They are popular among researchers to severity adjust populations and are the primary approaches in the literature. The novel sensitivity-adjusted MS-DRG model presented in this study takes differences among various MS-DRGs into consideration and calculates costs within each specific MS-DRG. It uses a specific MS-DRG multiplier for each MS-DRG to estimate total population impact. Although sensitivity adjustments are not typically used by hospital financial departments, we used this approach for MS-DRGs with low volumes of harm cases to reach optimal estimations. Whereas statistical models can provide predictive power in a population study, the MS-DRG method can be more applicable for hospital finance, revenue management, and quality department to analyze costs and achieve results comparable with those of the statistical models. Both methods generate similar total population estimation results, which we believe are more accurate than the aggregate estimates.
The IOM Report Best Care at Lower Cost: The Path to Continuously Learning Health Care in America suggests that improving patient safety may be 1 of the best health care cost reduction opportunities for hospitals.29 One of the challenges with the current state of patient safety is the narrow focus of harm measurement, which may be misleading as to the magnitude of patient harm and financial burden. Recent reports have suggested that hospitals fiscally benefit with an improved financial contribution margin from the occurrence of serious selected inpatient complications.30–33 In contrast, our study reveals that the financial contribution margin is negative for hospitals when the analysis includes all-cause harm compared with no harm, suggesting that, collectively, hospitals have both quality and financial incentives to drive down the incidences of harm.
In our model, we found adverse clinical and financial outcomes for inpatients who experience harm. We also found that these adverse effects extended beyond the hospitalization to the 30-day postdischarge period with an almost 3-fold increased risk for readmission after adjusting for severity of illness and other important confounders. This is a critical finding because none of the currently available models for predicting readmission include the occurrence of an adverse event during the hospitalization. This now seems to be an important factor in 30-day readmission and needs to be included in further efforts to identify readmission risk. Although the current focus of national readmission reduction efforts is at 30 days, we also measured harm impact on a patient's risk for readmission at 60, 90, 180, and 365 days after discharge and found significant increased risks for readmission at all these time intervals (Supplemental Digital Content, http://links.lww.com/JPS/A14, Appendix Exhibit A5). This may be related in part to the “post–hospital discharge syndrome” proposed by Krumholz,34,35 which suggests that inpatient harm increases readmission risk beyond the traditional 30 days and has the potential to increase other health services consumption after discharge. This suggests that our cost estimates of harm are underestimates of the true cost, which should include readmissions and the use of other postdischarge health services for this vulnerable population. Indeed, this may be another high-risk population in addition to patients with chronic disease and needs to be identified and managed to reduce health care costs. As hospitals move into an accountable care role, inpatient harms will not only negatively impact hospital margins but also increase the financial burden and risk associated with providing patient care across the continuum for both accountable care and bundled payment models.
If U.S. hospitals achieve similar harm reductions as this health system, the annualized36 national total cost savings would range between $6 billion and $13 billion and the opportunity cost of remaining harms would range between $33 billion and $63 billion. These estimates are only direct costs to hospitals and do not include ambulatory services and readmission costs, which would likely be substantial.
This study to determine the impact of all-cause harms on hospital finances and clinical outcomes raises the question, how did this health system achieve such significant reduction in harm? This study was not designed to evaluate the impact of specific interventions to reduce harm. However, this organization's approach to improving patient safety was complex and unfolded over time, requiring leadership and health care worker engagement, technological advancements, and focused quality improvement programs. The organization began by educating the Board of Trustees and financially incentivizing senior leadership and medical executives to improve quality and safety. By using a data-driven model, process measurements, detected inpatient harms, and clinical outcomes were compiled and analyzed for review by senior executives and hospital leaders on a monthly basis. As part of this data-driven model, an annual, validated safety culture survey was also administered to assess and improve the patient safety environment at the patient unit level—the critical intervention point for the improvement model described. Integrated electronic health records were introduced including computer provider order entry, evidence-based interdisciplinary plans of care, and a medication bar-coding system. From the data collected in this study, patient safety opportunities were identified including medication events (e.g., bleeding, allergies, mental status changes, and acute kidney injury), patient care (e.g., pressure ulcers, falls with injury, infections), and surgical/procedural events across the system. These issues were addressed using focused system-wide quality and safety performance improvement collaboratives. We believe that this data-driven approach combined with the initiatives above contributed to the reduction in the patient harm observed. To further improve safety, this system plans to implement automated real-time safety monitoring at the bedside.
This study has limitations. The study hospitals may not be nationally representative because of focused U.S. geographic regions of patients in the Southeast and Midwest. Random sampling without factoring hospital bed size may not optimally represent the patient population in certain large-sized hospitals. The IHI methodology measurement tracks incidents of harm over time, and with the use of a centralized review process, a high interrater reliability is possible within an organization12; however, between hospitals, variations may exist.3 In addition, we tracked readmission only to this hospital system but not to other hospital systems; therefore, the readmission estimates may be lower than the actual. Furthermore, other ambulatory events such as emergency department readmissions, ambulatory patient visits, or urgent care visits were not tracked, limiting our visibility to postdischarge safety issues and underestimating the financial and clinical impact. Lastly, we were unable to adjust for local variation in reimbursement rates from Medicare or other payors.
CONCLUSIONS
This study demonstrates that inpatient harm reduction is associated with reduced inpatient LOS, mortality, and readmission rates, which will benefit patients. Harm reduction is also associated with lower costs and higher contribution margin for hospitals. Therefore, reducing harm not only is the right thing to do for patients but also is financially and clinically prudent. The DRG approach proposed in this study provides a novel and practical approach for hospitals or health systems to evaluate the financial impact of harm.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Paul R. Garrett, Jr, MD, for providing invaluable leadership of the GTT project and Donald Kennerly, MD, for conceptualizing cost analysis with all patient harm.
Footnotes
The authors disclose no conflict of interest.
Supplemental digital contents are available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.journalpatientsafety.com).
REFERENCES
- 1.Institute of Medicine. Health IT and patient safety: building safer systems for better care. 2011. Available at: http://www.iom.edu/Reports/2011/Health-IT-and-Patient-Safety-Building-Safer-Systems-for-Better-Care.aspx. Accessed November 23, 2013. [PubMed]
- 2.James JT. A new evidence-based estimate of patient harms associated with hospital care. . 2013;9:122–128. [DOI] [PubMed] [Google Scholar]
- 3.Landrigan CP, Parry GJ, Bones CB, et al. Temporal trends in rates of patient harm resulting from medical care. . 2010;363:2124–2134. [DOI] [PubMed] [Google Scholar]
- 4.Department of Health and Human Services, Office of Inspector General. . Washington, DC: HHS; 2010; OEI-06-09-00090. Available at: http://oig.hhs.gov/oei/reports/oei-06-09-00090.pdf. Accessed October 10, 2014. [Google Scholar]
- 5.Partnership for patients: “It's about time”, say quality expert. . 2011;18:73–75. [PubMed] [Google Scholar]
- 6.Wang Y, Eldridge N, Metersky ML, et al. National trends in patient safety for four common conditions, 2005-2011. . 2014;370:341–351 doi:10.1056/NEJMsa1300991. PubMed PMID: 24450892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Classen DC, Resar R, Griffin F, et al. ‘Global trigger tool’ shows that adverse events in hospitals may be ten times greater than previously measured. . 2011;30:581–589. [DOI] [PubMed] [Google Scholar]
- 8.Cullen DJ, Bates DW, Small SD, et al. The incident reporting system does not detect adverse drug events: a problem for quality improvement. . 1995;21:541–548. [DOI] [PubMed] [Google Scholar]
- 9.Masheter CJ, Hougland P, Xu W. Detection of inpatient health care associated injuries: comparing two ICD-9-CM code classifications. In: Hendriksen K, Battles JB, Marks ES, et al., eds. , vol. 1 Rockville, MD: Agency for Healthcare Research & Quality; 2005. [PubMed] [Google Scholar]
- 10.Department of Health and Human Services, Office of Inspector General. . Washington, DC: HHS; 2010. [Google Scholar]
- 11.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. . 1991;324:370–376. [DOI] [PubMed] [Google Scholar]
- 12.Classen DC, Lloyd RC, Provost L, et al. Development and evaluation of the Institute for Healthcare Improvement Global Trigger Tool. . 2008;4:169–177. [Google Scholar]
- 13.Adler L, Denham CR, McKeever M, et al. Global Trigger Tool: implementation basics. . 2008;4:245–249. [Google Scholar]
- 14.Good VS, Saldaña M, Gilder R, et al. Large-scale deployment of the Global Trigger Tool across a large hospital system: refinements for the characterisation of adverse events to support patient safety learning opportunities. . 2011;20:25–30. [DOI] [PubMed] [Google Scholar]
- 15.Classen DC, Pestotnik SL, Evans RS, et al. Adverse drug events in hospitalized patients. Excess length of stay, extra costs, and attributable mortality. . 1997;277:301–306. [PubMed] [Google Scholar]
- 16.Bates DW, Spell N, Cullen DJ, et al. The costs of adverse drug events in hospitalized patients. Adverse Drug Events Prevention Study Group. . 1997;277:307–311. [PubMed] [Google Scholar]
- 17.Hellsten EK, Hanbidge MA, Manos AN, et al. An economic evaluation of perioperative adverse events associated with spinal surgery. . 2013;13:44–53. [DOI] [PubMed] [Google Scholar]
- 18.Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. . 2009;361:2637–2645. [DOI] [PubMed] [Google Scholar]
- 19.Garrett PR, Jr, Sammer C, Nelson A, et al. Developing and implementing a standardized process for global trigger tool application across a large health system. . 2013;39:292–297. [DOI] [PubMed] [Google Scholar]
- 20.Griffin FA, Resar RK , Cambridge, MA: Institute for Healthcare Improvement, 2009. [Google Scholar]
- 21.Basu A, Manning WG. Issues for the next generation of health care cost analyses. . 2009;47:S109–S114. [DOI] [PubMed] [Google Scholar]
- 22.Jones AM. Models for health care. In: Clements MP Hendry DF, eds. . New York: Oxford University Press; 2011. [Google Scholar]
- 23.Mihaylova B, Briggs A, O'Hagan A, et al. Review of statistical methods for analyzing healthcare resources and costs. . 2011;20:897–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deb P, Burgess JA , New York, NY: Department of Economics Working Papers, Hunter College, 2003. [Google Scholar]
- 25.Hill SC, Miller GE. Health expenditure estimation and functional form: applications of the generalized gamma and extended estimating equations models. . 2010;19:608–627. [DOI] [PubMed] [Google Scholar]
- 26.Jones AM, Lomas J, Moore P, et al. . Heslington, England: University of York; 2013. [Google Scholar]
- 27.Klein-Geltink JE, Rochon PA, Dyer S, et al. Readers should systematically assess methods used to identify, measure and analyze confounding in observational cohort studies. . 2007;60:766–772. [DOI] [PubMed] [Google Scholar]
- 28.Horn SD, Sharkey PD, Chambers AF, et al. Severity of illness within DRGs: impact on prospective payment. . 1985;75:1195–1199 PubMed PMID: 3929632; PubMed Central PMCID: PMC1646367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Research Council. . Washington, DC: The National Academies Press; 2013. [Google Scholar]
- 30.Eappen S, Lane BH, Rosenberg B, et al. Relationship between occurrence of surgical complications and hospital finances. . 2013;309:1599–1606. [DOI] [PubMed] [Google Scholar]
- 31.Griffin FA, Classen DC. Detection of adverse events in surgical patients using the Trigger Tool approach. . 2008;17:253–258. [DOI] [PubMed] [Google Scholar]
- 32.Carey K, Stefos T, Zhao S, et al. Excess costs attributable to postoperative complications. . 2011;68:490–503. [DOI] [PubMed] [Google Scholar]
- 33.Kurichi JE, Vogel WB, Kwong PL, et al. Factors associated with total inpatient costs and length of stay during surgical hospitalization among veterans who underwent lower extremity amputation. . 2013;92:203–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krumholz HM. Post-hospital syndrome—an acquired, transient condition of generalized risk. . 2013;368:100–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krumholz HM, Lin Z, Keenan PS, et al. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. . 2013;309:587–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Health Forum. AHA Hospital Statistics 2014: The Comprehensive Reference Source for Analysis and Comparison of Hospital Trends. 2014 ed Chicago, IL: American Hospital Association; 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.