Abstract
The aim of this study was to systematically review the literature about the capability of CBCT images to identify individuals with low bone mineral density (BMD). As the literature is scarce regarding this topic, the purpose of this systematic review is also to guide future research in this area. A detailed search was performed in five databases without restrictions of time or languages. Additionally, a grey literature search was conducted. The Quality Assessment Tool for Diagnostic Accuracy Studies-2 was applied to evaluate the methodological design of selected studies. With the inclusion of only six studies, the evidence is limited to endorse the use of CBCT assertively as a diagnostic tool for low BMD. All of the three studies that analyzed radiomorphometric indices found that the linear measurements of the mandibular inferior cortex were lower in osteoporotic individuals. CBCT-derived radiographic density vertebral and mandibular measurements were also capable for differentiating individuals with osteoporosis from individuals with normal BMD. The analysis of the cervical vertebrae showed high accuracy measurements. This systematic review indicates a scarcity of studies regarding the potential of CBCT for screening individuals with low BMD. However, the studies indicate that radiomorphometric indices and CBCT-derived radiographic density should be promising tools for differentiating individuals with osteoporosis from individuals with normal BMD.
Keywords: cone-beam computed tomography, bone density, osteoporosis, review
Introduction
Osteoporosis is a common skeletal disease characterized by a decreased bone strength predisposing to an increased risk of fractures. Bone strength reflects the integration of two main features: bone mineral density (BMD) and bone quality.1 Osteoporosis is considered a silent disease that entails significant social and economic burdens.2 Measurements of BMD at the proximal femur and lumbar spine by dual-energy X-ray absorptiometry (DXA) have been considered the reference standard for the diagnosis of low BMD.3 According to the World Health Organization criteria, BMD values are divided into the following diagnostic guidelines: normal (T-score ≥ −1.0), osteopenia (T-score between −1.0 and −2.5) and osteoporosis (T-score ≤ −2.5).4 Although DXA is the reference standard for BMD assessment, the availability is limited for routine use for population screening.5,6 Therefore, some alternative methods to screening the condition could provide an appropriate and more cost-effective use of DXA in post-menopausal females. One of these investigated methods is based on the evaluation of mandibular changes on dental imaging modalities.
Several previous studies have verified correlations between cortical and trabecular mandibular changes on two-dimensional imaging modalities and DXA measurements at the lumbar spine and proximal femur.7–13 However, only few studies have proposed the use of different CBCT measurements to discriminate individuals with normal skeletal BMD from individuals with osteoporosis.14–19 In the aforementioned studies, CBCT images were evaluated using mandibular cortical width measurements,14,18,19 mandibular cortical integrity,14,19 CBCT-derived radiographic density,15,17,18 histogram analysis18 and trabecular bone structure analysis.16,18,19
CBCT is a widely applied imaging method in dentistry which provides a three-dimensional representation of the maxillofacial skeleton with minimal distortion and improved image sharpness.20 Furthermore, the examination has a relatively low cost and low dose compared with other CT techniques.21
Larger numbers of osteoporotic patients are attending dental clinics as a result of higher life expectancies. Many of these patients are partially or totally edentulous and usually perform CBCT scans for implant planning purpose.22–25 Bone characteristics may influence the stability of the implant and have an important role in its success rate.26–29 However, BMD reliability based on CBCT scans has been little studied.29–31 Considering the increasing availability of CBCT scans before implant planning therapy, it would be of a great clinical value if the dental practitioner could use this imaging modality to identify patients with low BMD and refer them for further medical investigation. Few studies have investigated the applicability of different indices on CT images.14–19,23,31,32 Therefore, the main aim of this systematic review was to answer a focused question: “Does CBCT have the capability to identify patients with low BMD?” As the literature is scarce regarding this topic, the purpose of this systematic review was also to guide future research in this area.
Methods and materials
This systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement.33 The review protocol was registered at the International Prospective Register of Systematic Reviews (PROSPERO) under number CRD42015029474.
Study design
A systematic review of human studies was undertaken to evaluate the diagnostic capability of CBCT imaging for detecting low BMD. The CBCT measurements from osteoporotic individuals were compared from individuals with normal BMD according to DXA of the lumbar spine or the femoral neck.
Inclusion criteria
Diagnostic studies in which the primary objective was to evaluate the diagnostic capability of CBCT imaging in assessing adults with low BMD were included. The reference standard imaging was DXA of the proximal femur or DXA of the lumbar spine. No language or time restrictions were applied.
Exclusion criteria
The following exclusion criteria were applied: (1) reviews, letters, personal opinions, book chapters and conference abstracts; (2) studies that evaluated other diagnostic methods such as quantitative CT and micro-CT; (3) studies without the reference standard comparison (DXA); (4) studies with children mixed in the sample; (5) experimental studies in vitro or in vivo animal models; and (6) a different target condition such as evaluation of the relationship between BMD and dimensions of the mandibular residual ridge in edentulous individuals.
Information sources and search strategy
Detailed individual search strategies for each of the following electronic database were performed: LILACS, PubMed, Science Direct, Scopus and Web of Science (Appendix A, Table A1). A partial grey literature was performed using Open Grey, Google Scholar and ProQuest Dissertations & Theses Global. All searches were conducted on 5 October 2016. Duplicate references were removed by reference manager software (EndNote® X7; Thomson Reuters, Philadelphia, PA). In addition to the electronic search, a hand search and consultations with experts were implemented and the reference lists of the selected articles were screened.
Study selection
A two-phase selection of articles was conducted. In Phase 1, two authors (FVB and FTA) reviewed the titles and abstracts of all the references independently. These authors selected articles that appeared to meet the inclusion criteria based on their titles and abstracts. In Phase 2, the same authors (FVB and FTA) assessed the full text of all selected articles and excluded studies that did not meet the inclusion criteria. The disagreements between these two authors were initially resolved by consensus. When they did not reach a consensus, a third author (CP-P) was involved in making a final decision. The final selections were always based on the full text of the publication.
Data items and collection process
One author (FVB) collected the key features of each included article and a second author (FTA) cross-checked all the collected data. Once again, disagreements among them were solved by consensus and the third author (ENSG) was involved, when required, to make a final decision.
For all included studies, the following descriptive characteristics were recorded: study characteristics (authors, year and country), sample characteristics (case group, control group and mean age), intervention characteristics (index test, reference standard and methods) and outcome (main conclusions). If the required data were not complete, attempts were made to contact the authors to retrieve the missing information.
Risk of bias in individual studies
The methodology quality of the selected studies was evaluated using the Quality Assessment Tool for Diagnostic Accuracy Studies-2 (QUADAS-2).34 Two authors (FVB and FTA) independently evaluated the quality of each included study and scored each item as “yes,” “no” or “unclear”. The disagreements were resolved by a third reviewer (ENSG).
Summary measures
The capability of dental CBCT scans to identify low-BMD patients based on cortical and trabecular bone measurements was considered as the primary outcome. Any type of outcome measurement was considered in this review (categorical and continuous variables).
Synthesis of results
If the included studies in the review had enough data and the data were considered homogeneous, a meta-analysis would be performed.
Risk of bias across studies
Individuals with normal BMD were compared with individuals with low BMD or osteoporosis. Clinical heterogeneity (by comparing variability among the participant's characteristics and outcomes studied) and methodological heterogeneity [by comparing the variability in study design and risk of bias (RoB)] were considered.
Results
Study selection
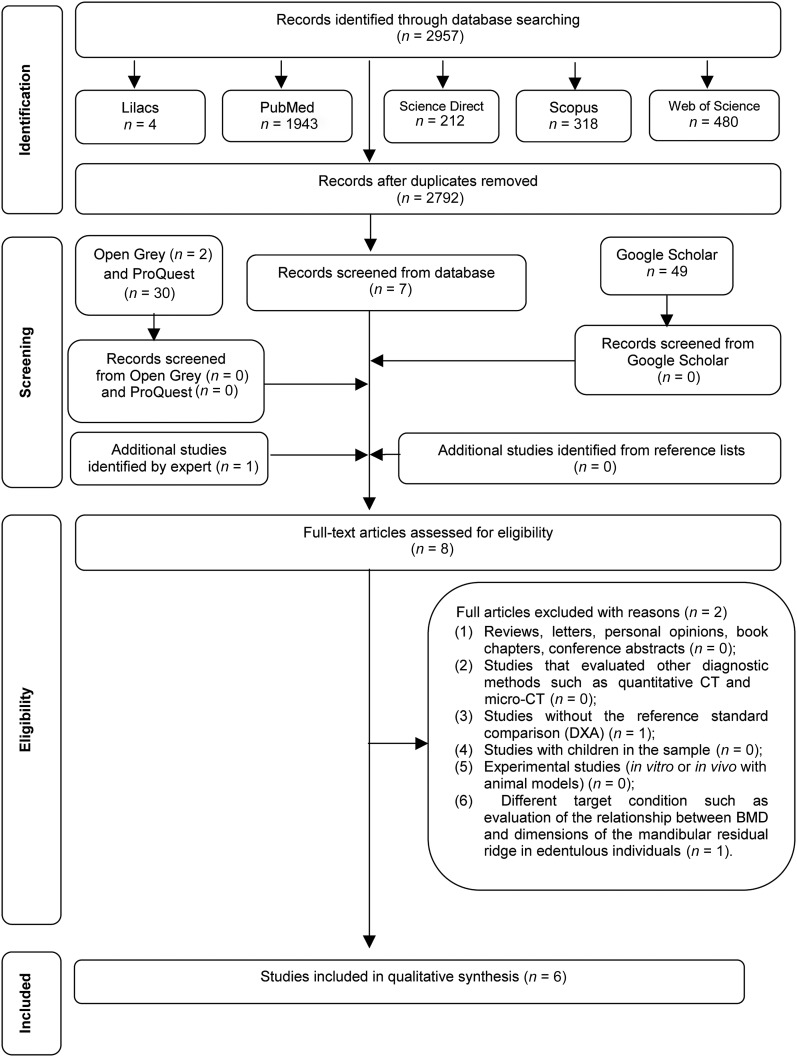
A flow diagram detailing the process of identification, inclusion and exclusion of the studies is shown in Figure 1. A full-text review was conducted on the eight articles retrieved from Phase 1 of the selection. This process led to the exclusion of two studies presented in Appendix B (Table A2). At the end, six articles were retained for qualitative synthesis.14–19
Figure 1.
Flow diagram of literature search and selection criteria adapted from Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA)33. BMD, bone mineral density; DXA, dual-energy X-ray absorptiometry.
Study characteristics
The six included studies were conducted in four different countries: one in Republic of Korea14 three in Syrian Arab Republic,15–17 one in Turkey,18 and one in Egypt.19 All studies were published within a 5-year period (2011–16). All the studies were written in English.
Three studies have used the same sample composed by 38 post-menopausal females who performed CBCT examinations.15–17 The aforementioned studies analyzed separately the densitometric diagnosis of osteoporosis from the lumbar spine and the femoral neck. A summary of the descriptive characteristics of the included articles is provided in Table 1.
Table 1.
Summary of descriptive characteristics of studies in included articles (n = 6)
| Study characteristics | Sample characteristics |
Intervention characteristics |
Outcomes | ||||
|---|---|---|---|---|---|---|---|
| Author, year, country | Case group | Control group | Mean age (SD) | Index test | Reference standard | Methods | Main conclusions |
| Koh and Kim14 2011, Republic of Korea | Postmenopausal osteoporotic females (n = 21) | Postmenopausal normal BMD females (n = 21) | 66.0(6.4)—K 60.0(5.7)—C |
CBCT (voxel size: 0.15 mm)—device PSR-9000N™ Dental CT system (Asahi Roentgen Ind. Co. Ltd, Kyoto, Japan) | DXA (LS and FN) | The relationship between CBCT measurements [CTI(S), CTI(I), CTCI and CTMI] and BMDs were assessed. The intraobserver agreement was determined | CTMI measurements showed no significant difference between the groups (p > 0.05); CTI(S), CTI(I) and CTCI on CBCT images can be used to assess osteoporosis |
| Barngkgei et al15 2014, Syrian Arab Republic | Post-menopausal osteoporotic females regarding LV T-score (n = 13) and FN T-score (n = 10) | Post-menopausal normal BMD females + osteopenic females regarding LV T-score (n = 25) and FN T-score (n = 28) | Groups according to LV T-score: normal BMD 52.3 (3.5); osteopenia 59.1 (7.2); osteoporosis 60.9 (7.1); Groups according to FN T-score: normal BMD 55.1 (4.6); osteopenia 58.1 (8.8); osteoporosis 62.6 (6.9) |
CBCT (FOV: 13 × 15 cm; voxel size: 0.25 mm)—device Whitefox Imaging v. 3 (Acteon Group) | DXA (LS and FN) |
Three groups for FN and LV were assessed; RD from the body and ramus of the mandible was evaluated |
Osteoporosis can be predicted with high accuracy (78.4% for the FN and 75% for the LV) from the RD by using CBCT |
| Barngkgei et al16 2016, Syrian Arab Republic | Post-menopausal osteoporotic females regarding LV T-score (n = 13) and FN T-score (n = 10) | Post-menopausal normal BMD females + osteopenic females regarding LV T-score (n = 25) and FN T-score (n = 28) | 57.9 (7.2)—mean age of total sample | CBCT (FOV: 13 × 15 cm; voxel size: 0.25 mm)—device Whitefox Imaging v. 3 (Acteon Group) | DXA (LS and FN) | Three groups for FN and LV were assessed; Cuboids from jawbones were extracted from CBCT scans; HA using ImageJ; Tb.Th, Tb.Ts, BV/TV, BS/TV and connectivity density calculated by BoneJ |
Jawbone-derived measurements did not differ significantly between osteoporotic and non-osteoporotic females (p > 0.05); Dens-derived measures showed high accuracy of osteoporosis prediction (84.2% for FN and 78.9% for LV) |
| Barngkgei et al17 2015, Syrian Arab Republic | Post-menopausal osteoporotic females regarding LV T-score (n = 13) and FN T-score (n = 10) and osteoporotic + osteopenic females regarding LV T-score (n = 28) and FN T-score (n = 21) | Post-menopausal normal BMD females + osteopenic females regarding LV T-score (n = 25) and FN T-score (n = 28) and normal BMD females regarding LV T-score (n = 10) and FN T-score (n = 17) | Groups according to LV T-score: normal BMD 52.3 (3.5); osteopenia 59.1 (7.2); osteoporosis 60.9 (7.1); Groups according to FN T-score normal BMD 55.1 (4.6); osteopenia 58.1 (8.8); osteoporosis 62.6 (6.9) |
CBCT (FOV: 13 × 15 cm; voxel size: 0.25 mm)—device Whitefox Imaging v. 3 (Acteon Group) | DXA (LS and FN) | RD values from the first and second vertebrae and the dens | CBCT-derived RD of cervical vertebrae showed highest sensitivity (76.9%, 70%), specificity (92%, 92.9%) and accuracy (90.8%, 86.4%) in predicting osteoporosis in the LV and FN, respectively |
| Güngör et al18 2016, Turkey | Osteoporotic patients (n = 26) Osteopenic patients (n = 33) |
Normal BMD patients (n = 31) | Osteoporotic group 58.5 (5.9); Osteopenic group 52.6 (8.6); Normal BMD group 49.8 (10.4) |
CBCT (FOV: 13 × 10 cm; voxel size: 0.3 mm)—device i-CAT (vision; Imaging Sciences International Inc., Hatfield, PA) |
DXA (LS or hip) | Radiomorphometric index measurements [CTI(S), CTI(I), CTMI]; CT values for bone density; HA and FD analysis using ImageJ | Changes in the jaw bone associated with osteoporosis can be defined by radiomorphometric index measurements, CT values, HA and FD analysis on CBCT images |
| Mostafa et al19 2016, Egypt | Osteoporotic females (n = 25) | Normal BMD females (n = 25) | Age of total sample ranging from 55 to 70 years old | CBCT (FOV: 8 × 8 cm; voxel size: 0.2 mm) device Planmeca ProMax® 3D Classic, Helsinki, Finland |
DXA (LS) | Radiomorphometric index measurements (CTCI, CTMI, CTI) and FD analysis using ImageJ | Radiomorphometric index measurements by CBCT can be used as an adjuvant tool to refer patients at risk of osteoporosis. No significant differences were found between the two groups for FD values (p = 0.52) |
BMD, bone mineral density; BS/TV, specific bone surface; BV/TV, bone volume fraction; C, control; CTCI, CT cortical index; CTI, CT mandibular index; CTI(I), CT mandibular index (inferior); CTI(S), CT mandibular index (superior); CTMI, CT mental index; dens, odontoid process; DXA, dual-energy X-ray absorptiometry; FD, fractal dimension; FN, femoral neck; FOV, field of view; HA, histomorphometric analysis; K, case; LS, lumbar spine; LV, lumbar vertebrae; RD, radiographic density; Tb.Th, trabecular thickness; Tb.Ts, trabecular separation.
T-score measures the difference between the patient's BMD and the mean BMD of the young normal population; group according T-score is normal BMD (T-score ≥ −1), osteopenia (−2.5 < T-score < −1) and osteoporosis (T-score ≤ −2.5).
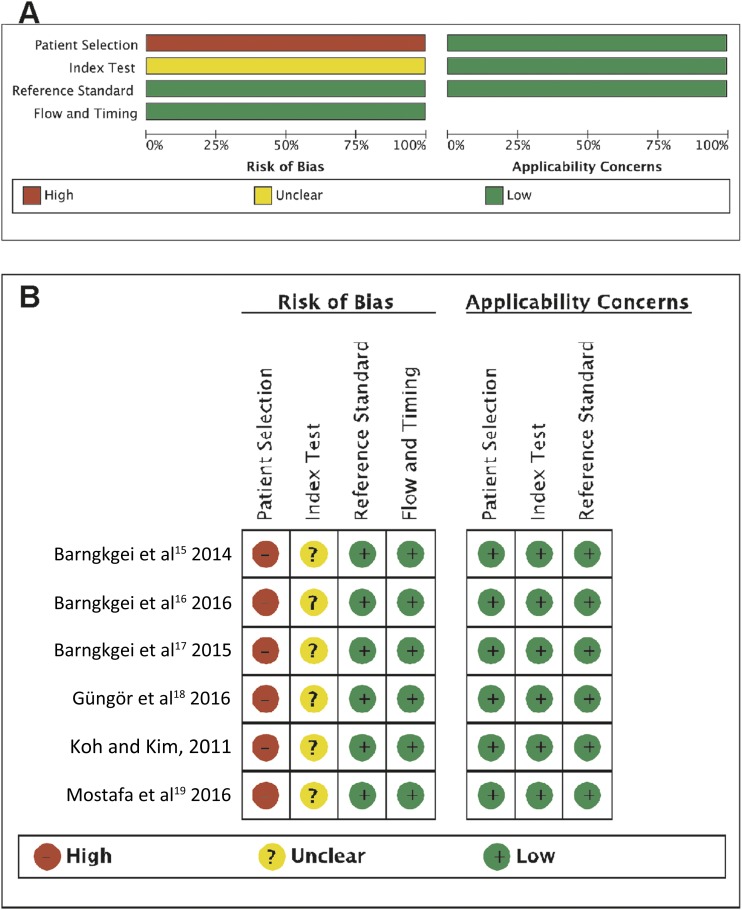
Risk of bias within studies
None of the studies fulfilled all of the methodological quality criteria (Figure 2a,b). For every study, Item 1 of the QUADAS-2 criteria was scored as “no” (Domain 1, “Was a case–control design avoided?”) because each study recruited a group of post-menopausal healthy BMD females and a group known to have post-menopausal low-BMD females. Additionally, the RoB of “index test” (Domain 2, “Could the conduct or interpretation of the index test have introduced bias?”) were scored “unclear” for all studies due to the lack of information about blinding. On average, the selected studies were considered as low RoB according to the QUADAS-2 criteria (Appendix C, Table A3).
Figure 2.
(a) Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies. (b) Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study.
Results of individual studies
In three of the selected studies, radiomorphometric indices were measured on the CBCT scans, which included qualitative indices and linear measurements.14,18,19
Koh and Kim14 evaluated four different CT indices on CBCT images. Three of these indices were quantitative measurements: CT mandibular index superior—CTI(S), CT mandibular index inferior—CTI(I) and CT mental index—CTMI. The other index was a qualitative analysis: CT cortical index. The reference BMD of the lumbar spine and femoral neck by DXA was calculated. Although the osteoporotic group showed lower mean values for all linear measurements, the differences were statistically significant only for CTI(I) and CTI(S). Furthermore, significant differences were found between osteoporotic and normal BMD females concerning the qualitative index CT cortical index (CTCI), as classification C3 was more frequent in the osteoporotic group and classification C1 was more frequent in the normal BMD group.
Mostafa et al19 evaluated one quantitative index (CTMI) and one qualitative index (CTCI) in post-menopausal females. The mandibular cortical width evaluated by the CTMI was significantly lower in the osteoporotic group than in the normal BMD group.
Güngor et al18 selected subjects aged over 30 years who had undergone CBCT for several oral conditions and then referred for DXA of the lumbar spine and proximal femur. All CBCT linear measurements were significantly lower in osteoporotic patients than in patients with normal BMD and in patients with osteopenia.
Fractal dimension (FD) analysis to assess the structural pattern of bone was verified in two studies.18,19 In the former study,18 the mean FD values obtained from the maxilla of osteoporotic patients were significantly lower than those in the osteopenia and control groups. The other study did not find significant differences between case and control groups for FD values; however, the control group showed lower values than the osteoporotic group.19
Two studies investigated the use of CBCT-derived radiographic density (RD) for predicting osteoporosis in post-menopausal females by using the reference standard of DXA at the lumbar spine and femoral neck.15,17 They assessed CBCT-derived RD from the mandible (body and ramus)15 and from the cervical vertebra.17 The accuracy of the mandible evaluation was 75% and 78.4% and that of the cervical vertebra was 90.8% and 86.4% for the lumbar spine and femoral neck, respectively. Both studies concluded that CBCT-derived RD measurements of the mandible and cervical vertebrae could predict osteoporosis.
Other authors evaluated CBCT-derived RD (named in the study as CT values) and HA of the mandible and maxilla to observe differences in jaw bone tissues. The CT and HA values of the maxilla and mandible from osteoporosis patients were significantly lower than measurements obtained from osteopenia and control patients.18 Owing to these results, the authors concluded that radiomorphometric indices, FD, CT and HA values could be used to evaluate and compare osteoporosis, osteopenia and normal BMD patients.
The trabecular bone structure of jawbones and the odontoid process in osteoporotic and normal females using CBCT were evaluated in another study.16 They concluded that the trabecular bone structure of jaws is not affected in osteoporosis and the opposite was observed for the odontoid process.
Synthesis of results
In total, 220 individuals were analyzed on CBCT examinations. Of these examinations, 85 (38.6%) were of osteoporotic individuals and 87 (39.6%) were of individuals with normal BMD. 48 osteopenic individuals (21.8%) were analyzed only in 4 studies.15–18 All studies, except 1 which did not state the gender of the 90 analyzed individuals,18 evaluated only post-menopausal females.
Three studies verified that the mandibular cortical measurements were lower in individuals with osteoporosis.14,18,19 Some CBCT-derived variables such as RD measured by gray values (GV) and bone structural analysis were assessed in four selected studies15–18 with promising capability for differentiating osteoporotic individuals from individuals with normal BMD. Only one study reported excellent sensitivity and specificity values for clinical use of such variables.17 This aforementioned study evaluated RD as GV from the first (C1) and second vertebrae (C2) and the odontoid process (dens). C1 and C2 analysis showed excellent diagnostic test accuracy that was able to distinguish low BMD individuals accurately from healthy individuals concerning the lumbar vertebrae T-score.
Risk of bias across studies
The six selected studies were very heterogeneous which precluded a meta-analysis. Some limitations of these studies should be mentioned. The limited sample size and the selection of the patients could lead to a publication bias. The reproducibility of the bone measurements was not assessed in all the selected studies. Furthermore, the division of the groups according to the DXA diagnosis was different between the selected studies compromising homogeneity of results. In two studies, patients with osteopenia and with normal BMD were included in the control group (named as “not osteoporotic group”) and compared with patients with osteoporosis.15,16 In another study, patients with osteoporosis and osteopenia were grouped and compared with patients with normal BMD.17 All of the three aforementioned studies from the same author analyzed separately the CBCT measurements according to DXA at the lumbar spine and DXA at the femoral neck. In one study, the osteoporosis diagnosis was based on the T-score value ≤−2.5 at both the lumbar spine and the femoral neck.14 On the other hand, in a recent study, the osteoporosis diagnosis was based on the T-score value ≤−2.5 at the lumbar spine or at the femoral neck.18 From the selected studies, this study was the only one which did not characterize the sample according to gender. All of the other selected studies were performed in post-menopausal females.14–17,19 Mostafa et al19 used only the DXA at the lumbar spine as the reference standard for the diagnosis of osteoporosis. Therefore, some biases may be related to these limiting factors.
Discussion
This systematic review investigated the limited available evidence regarding the diagnostic accuracy of CBCT for osteoporosis screening, by discriminating individuals with low BMD from those individuals with normal BMD. Although six studies were found in our review, some cortical and trabecular bone measurements were able to differentiate individuals with osteoporosis from individuals with normal BMD according to skeletal DXA. Dentists increasingly use CBCT scans in dental practice, especially for implant planning in edentulous patients, a potential population for osteoporosis.35,36 Therefore, it would be clinically relevant to further investigate whether CBCT could serve as an adjuvant tool for identifying low-BMD individuals. In addition, as a silent disease, dentists could refer individuals potentially affected by the disease early for further medical investigation. Early diagnosis of the osteoporosis is necessary to allow proper management of the disease, to reduce the risk of fracture and to maximize bone mass retention.37
To the best of the authors' knowledge, this is the first systematic review concerning the capability of CBCT to identify low-BMD patients. A previous systematic review has summarized the use of dental panoramic radiographs for the same purpose. However, the authors have recognized the limitations of this two-dimensional image, especially regarding the geometric distortions and the magnification.13
Different linear and qualitative radiomorphometric indices have been proposed as auxiliary diagnostic tools for low BMD on dental imaging modalities.13,14,18,19 These measurements were analyzed on CBCT scans in few studies.14,18,19,23,29,31,38,39 However, in only three studies these measurements were used to differentiate individuals with osteoporosis from individuals with normal BMD according to DXA.14,18,19 All of these three aforementioned studies have verified that the linear measurements of the mandibular inferior cortex were lower in osteoporotic individuals than in individuals with normal BMD. Two of these studies18,19 have also evaluated the qualitative index CTCI. Both studies verified that classification C3, in which the cortex is obviously porous with dense endosteal residues, was more frequent in osteoporotic individuals. Based on the results of the three aforementioned studies, the radiomorphometric studies should be further investigated on CBCT scans. They should be considered as promising tools for identifying individuals with low BMD.
Four of the selected studies have analyzed radiographic density vertebral and mandibular measurements by using the software supplied by the CBCT device manufacturer.15–18 These structural bone measurements are probably more related to the bone quality. Bone quality in CBCT has been described in the literature related to the evaluation of the pre-implant sites in the jaws.24,26–29,40 These studies stated that the calculation of the radiographic density as gray values may be an inaccurate process, significantly depending on the voxel size. Additionally, there are differences in gray values between CBCT devices and trabecular bone measurements. It should be emphasized that the selected studies have used different CBCT devices and voxel sizes, except the three studies performed by the same group of authors.15–17
In our review, CBCT-derived RD values of the dens and the left part of the first cervical vertebra showed the highest accuracy.16 These data suggest that vertebral analysis could be an effective diagnostic test accurate for screening low BMD. However, the evidence to assert this possibility is weak since the three diagnostic test studies found in our systematic review which presented accuracy measurements were performed in the same small sample of post-menopausal females.15–17
Therefore, the few selected studies of our systematic review revealed that the radiomorphometric analysis of the mandibular inferior cortex on CBCT examinations and the CBCT-derived radiographic density of the first cervical vertebrae could differentiate individuals with osteoporosis from normal BMD individuals. Some authors have stated that cervical vertebrae frequently appear in dental radiographs and could be used for osteoporosis screening.16 However, it should be noted that the C1 and C2 vertebrae only appear on mandibular or full head CBCT scans. In CBCT devices with limited field of view (FOV), the vertebral analysis might not be performed, even in CBCT scans of post-menopausal females, depending on the scanned area. Nonetheless, during implant therapy, the dentists should be aware that when using CBCT, as with other diagnostic tools, their responsibility is not limited to the area of interest being diagnosed or treated. Therefore, when analyzing the CBCT examination, the vertebral area and the mandibular inferior cortex should be evaluated, no matter the initial purpose of the scanning.
The conclusions of the studies included in this review are restricted. In three studies, the same authors have analyzed a small sample size composed by 38 post-menopausal females. Also, the same CBCT device was used in these three studies (WhiteFox®; Acteon Group Ltd., Milan, Italy), with identical FOV and voxel sizes.15–17 The analyses were performed by using the software supplied by the CBCT device manufacturer (WhiteFox Imaging V3). Some authors have verified that the trabecular bone measurements and, consequently, the image quality are significantly affected by technical parameters, such as the voxel size, the unit itself, tube voltage and amperage, and FOV selection.41,42 Generally, the smaller the voxels, the higher the spatial resolution and therefore the sharper the images appear to be.27 Further studies are necessary to verify whether the results would be different by varying the FOV and voxel size. In addition, the bone variables were based on trabecular measurements. The measurements were performed on CBCT scans from the same device, by using similar FOV and voxel sizes.
This systematic review pointed out the need of further standardized studies with larger sample sizes, concerning the bone variable and the measured area, and also focused on the cortical bone. Some trabecular bone structural measurements that may be more related to the bone quality should be further correlated with other skeletal measurements, such as lumbar spine and hip quantitative CT.
Limitations
Some restrictions of this systematic review should be considered. First, all of the studies presented a small sample size and a large heterogeneity was observed in the standard classification of the case and control groups of the included studies (e.g. osteopenic females were classified in the control group, and sometimes in the case group together with females with osteoporosis). Moreover, different mandibular and vertebral areas/variables were tested for differentiate postmenopausal females. Some bone areas may be influenced by local factors, as occlusal forces and masseter muscle tensions that influence the correlation with DXA.16,43,44
Finally, studies did not report the calibrating process of the examiners to ensure accuracy and reproducibility. Such inconsistencies collectively result in large variations in the diagnostic accuracy of CBCT for the screening of patients with low BMD. It has serious implications for diagnostic test accuracy studies because the reference standard directly impacts the test performance estimation.
Conclusions
Although this systematic review indicates a scarcity of studies regarding the accuracy of CBCT as a screening tool for low BMD, it suggests the potential of this imaging modality for this purpose. Linear measurements of the inferior mandibular cortex were lower in osteoporotic individuals, indicating that radiomorphometric indices on CBCT should be a promising tool for identifying individuals with low BMD. CBCT-derived radiographic density using the CBCT-viewer software should also be promising for screening BMD in future studies. In cases where CBCT is prescribed, dentists could have an important role in identifying patients with low BMD. However to date, the evidence is restricted to assertively endorse the use of CBCT as diagnostic tools for low BMD.
Appendix A
Table A1.
Search strategies with appropriated key words and MeSH termsa
| Database | Search strategya |
|---|---|
| LILACS | CBCT or cone beam computed tomography or tomografia computadorizada por feixe cônico or tomografia computadorizada odontológica [Palavras] and osteoporose or densidade óssea or baixa densidade óssea or bisfosfonatos or densidade mandibular or bone density or low bone density [Palavras] |
| PubMed | #1 (((adult) OR adults) OR male) OR female #2 ((((((((((((((((((((((((((“Bone density”) OR “Bone mineral density”) OR “Bone mineral densities”) OR “Bone mineral mass”) OR “Bone mineral quality”) OR “Bone quality assessment”) OR “Alveolar bone mass”) OR “Alveolar bone loss”) OR “Mandibular cortical bone”) OR “Mandibular bone quality”) OR “Mandibular bone mineral density”) OR “Jaws bone density”) OR “Cortical bone mass”) OR “Trabecular bone mass”) OR “Trabecular mandibular bone”) OR “Low bone mass”) OR “Low bone mineral mass”) OR “Low bone mineral densities”) OR “Loss of bone mass”) OR “Loss of bone mineral density”) OR “Mandibular osteopenia”) OR “Metabolic bone loss”) OR “Osteoporosis”) OR “Oral bisphosphonates”) OR “Mandibular cortical indices”) OR “Mandibular radiomorphometric indices”) OR “Bisphosphonates” #3 (((((“CBCT”) OR “cone beam”) OR computed tomography) OR cone beam[MeSH Terms]) OR computer assisted tomography) OR cone beam[MeSH Terms] #4 (((((((((((Densitometry) OR densitometric*) OR “DXA”) OR “DEXA”) OR “dual energy X-ray”) OR “dual energy Xray”) OR “dual energy X-ray”) OR “dual-energy X-ray”) OR “dual-energy Xray”) OR “dual-energy X-ray”) OR dxa scan[MeSH Terms]) OR dxa scans[MeSH Terms] #5 (((#1) AND#2) AND#3) AND#4 |
| Science Direct | (Cone beam computed tomography OR Cone beam CT OR CBCT OR CBCT scans OR Cone beam technique or dental computed tomography) and (Bone density OR Bone mineral density OR Bone mineral mass OR Mandibular cortical bone OR Low bone mass OR Low bone mineral densities OR Loss of bone mass OR Osteoporosis OR Bisphosphonates) AND LIMIT-TO(contenttype, “JL,BS”,“Journal”). |
| Scopus | ALL ((cone beam computed tomography OR cbct OR cone beam ct OR computed tomography AND bone density OR low bone density OR osteoporosis OR radiomorphometric indices OR mandibular indices OR mandibular osteopenia OR mandibular cortical bone)) |
| Web of Science | TS=((Bone density OR Bone mineral density OR Bone mineral densities OR Bone mineral mass OR Bone mineral quality OR Bone quality assessment OR Alveolar bone mass OR Alvelar bone loss OR Mandibular cortical bone OR Mandibular bone quality OR Mandibular bone mineral density OR Jaws bone density OR Cortical bone mass OR Trabecular bone mass OR Trabecular mandibular bone OR Low bone mass OR Low bone mineral mass OR Low bone mineral densities OR Loss of bone mass OR Loss of bone mineral density OR Mandibular osteopenia OR Metabolic bone loss OR Osteoporosis OR Oral bisphosphonates OR Postmenopausal women OR Postmenopausal or mandibular cortical indices or radiomorphometric indices or bisphosphonates) AND (Cone beam computed tomography OR Cone-beam computed tomography OR Cone beam CT OR Cone-beam CT OR CBCT OR CBCT scans OR Cone-beam technique OR Cone beam technique OR Cone beam computed tomography scanners OR Cone-beam computerized tomographic scanning OR Computerized tomography for dental OR Dental cone-beam CT OR Dental cone beam CT or cone beam computer tomography)) |
| Google Scholar | Cone beam AND computed tomography AND CT AND CBCT AND scans AND Cone beam AND technique AND Bone AND density AND Bone mineral AND density AND Bone mineral AND mass AND Mandibular cortical AND bone AND Low AND bone mass AND Low bone AND mineral densities |
| Open Grey | Cone beam AND Bone density |
| ProQuest | su(Cone beam ct) AND su(Bone density) |
Up to 5 October 2016.
Appendix B
Table A2.
Excluded articles and reasons for exclusion
Reasons for exclusion:
(1) reviews, letters, personal opinions, book chapters and conference abstracts (n = 0)
(2) studies that evaluated other diagnostic methods such as quantitative CT and micro-CT (n = 0)
(3) studies without the reference standard comparison (DXA) (n = 1)
(4) studies with children in the sample (n = 0)
(5) experimental studies (in vitro or in vivo with animal models) (n = 0)
(6) a different target condition such as evaluation of the relationship between BMD and dimensions of the mandibular residual ridge in edentulous individuals (n = 1).
References
- A1. Springe B, Slaidina A, Soboleva U, Lejnieks A. Bone mineral density and mandibular residual ridge resorption. Int J Prosthodont 2014; 27: 270–76. [DOI] [PubMed]
- A2. Geibel MA, Löffler F, Kildal D. Osteoporosis detection using cone-beam computed tomography. Orthopade. 2016 Sep 28. Epub ahead of print. [DOI] [PubMed]
Appendix C
Table A3.
Risk of bias in individual studies. Quality Assessment Tool for Diagnostic Accuracy Studies-2 criteria fulfilled.
| Item | Koh and Kim14 2011 | Barngkgei et al15 2014 | Barngkgei et al16 2016 | Barngkgei et al17 2015 | Güngör et al18 2016 | Mostafa et al19 2016 | |
|---|---|---|---|---|---|---|---|
| Domain 1: patient selection | Was a consecutive or random sample of patients enrolled? | Y | Y | Y | Y | Y | Y |
| Was a case–control design avoided? | N | N | N | N | N | N | |
| Did the study avoid inappropriate exclusions? | Y | Y | Y | Y | Y | Y | |
| Could the selection of patients have introduced bias? | H | H | H | H | H | H | |
| Concerns regarding applicability: Is there concern that the included patients do not match the review question? | L | L | L | L | L | L | |
| Domain 2: index test | Were the index test results interpreted without knowledge of the results of the reference standard? | U | U | U | U | U | U |
| If a threshold was used, was it pre-specified? | U | U | U | U | U | U | |
| Could the conduct or interpretation of the index test have introduced bias? | U | U | U | U | U | U | |
| Concerns regarding applicability: Is there concern that the index test, its conduct or interpretation differ from the review question? | L | L | L | L | L | L | |
| Domain 3: reference standard | Is the reference standard likely to correctly classify the target condition? | Y | Y | Y | Y | Y | Y |
| Were the reference standard results interpreted without knowledge of the results of the index test? | Y | Y | Y | Y | Y | Y | |
| Could the reference standard, its conduct or its interpretation have introduced bias? | L | L | L | L | L | L | |
| Concerns regarding applicability: Is there concern that the target condition as defined by the reference standard does not match the review question? | L | L | L | L | L | L | |
| Domain 4: flow and timing | Was there an appropriate interval between index test(s) and reference standard? | Y | Y | Y | Y | Y | Y |
| Did all patients receive a reference standard? | Y | Y | Y | Y | Y | Y | |
| Did patients receive the same reference standard? | Y | Y | Y | Y | Y | Y | |
| Were all patients included in the analysis? | Y | Y | Y | Y | Y | Y | |
| Could the patient flow have introduced bias? | L | L | L | L | L | L |
H, high risk; L, low risk; N, no; U, unclear; Y, yes.
Contributor Information
Eliete N S Guerra, Email: elieteneves@unb.br.
Fabiana T Almeida, Email: fabianatolentino@hotmail.com.
Fernanda V Bezerra, Email: fernandabezerra11@gmail.com.
Paulo T D S Figueiredo, Email: paulofigueiredo@unb.br.
Maria A G Silva, Email: mariaagsilva@gmail.com.
Graziela De Luca Canto, Email: delucacanto@gmail.com.
Camila Pachêco-Pereira, Email: cppereir@ualberta.ca.
André F Leite, Email: andreleite@unb.br.
References
- 1.National Institutes of Health, NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA 2001; 285: 785–95. doi:https://doi.org/10.1001/jama.285.6.785 [DOI] [PubMed] [Google Scholar]
- 2.Atik OS, Gunal I, Korkusuz F. Burden of osteoporosis. Clin Orthop Relat Res 2006; 443: 19–24. doi: https://doi.org/10.1097/01.blo.0000200248.34876.fe. [DOI] [PubMed] [Google Scholar]
- 3.Ebeling PR. Clinical practice. Osteoporosis in men. N Engl J Med 2008; 358: 1474–82. doi: https://doi.org/10.1056/NEJMcp0707217. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO). Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser 1994; 843: 1–129. [PubMed] [Google Scholar]
- 5.Nakamoto T, Taguchi A, Ohtsuka M, Suei Y, Fujita M, Tanimoto K, et al. Dental panoramic radiograph as a tool to detect postmenopausal women with low bone mineral density: untrained general dental practitioners' diagnostic performance. Osteoporos Int 2003; 14: 659–64. doi: https://doi.org/10.1007/s00198-003-1419-y [DOI] [PubMed] [Google Scholar]
- 6.Lane NE. Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstet Gynecol 2006; 194(Suppl. 2): S3–11. doi: https://doi.org/10.1016/j.ajog.2005.08.047. [DOI] [PubMed] [Google Scholar]
- 7.Taguchi A, Suei Y, Sanada M, Ohtsuka M, Nakamoto T, Sumida H, et al. Validation of dental panoramic radiography measures for identifying postmenopausal women with spinal osteoporosis. AJR Am J Roentgenol 2004; 183: 1755–60. doi: https://doi.org/10.2214/ajr.183.6.01831755 [DOI] [PubMed] [Google Scholar]
- 8.Nackaerts O, Jacobs R, Devlin H, Pavitt S, Bleyen E, Yan B, et al. Osteoporosis detection using intraoral densitometry. Dentomaxillofac Radiol 2008; 37: 282–7. doi: https://doi.org/10.1259/dmfr/30424604. [DOI] [PubMed] [Google Scholar]
- 9.Horner K, Allen P, Graham J, Jacobs R, Boonen S, Pavitt S, et al. The relationship between the OSTEODENT index and hip fracture risk assessment using FRAX. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 110: 243–9. doi: https://doi.org/10.1016/j.tripleo.2010.03.035 [DOI] [PubMed] [Google Scholar]
- 10.Leite AF, Figueiredo PT, Guia CM, Melo NS, de Paula AP. Correlations between seven panoramic radiomorphometric indices and bone mineral density in postmenopausal women. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: 449–56. doi: https://doi.org/10.1016/j.tripleo.2009.02.028 [DOI] [PubMed] [Google Scholar]
- 11.Alman AC, Johnson LR, Calverley DC, Grunwald GK, Lezotte DC, Hokanson JE. Diagnostic capabilities of fractal dimension and mandibular cortical width to identify men and women with decreased bone mineral density. Osteoporos Int 2012; 23: 1631–6. doi: https://doi.org/10.1007/s00198-011-1678-y [DOI] [PubMed] [Google Scholar]
- 12.Sindeaux R, Figueiredo PT, de Melo NS, Guimarães AT, Lazarte L, Pereira FB, et al. Fractal dimension and mandibular cortical width in normal and osteoporotic men and women. Maturitas 2014; 77: 142–8. doi: https://doi.org/10.1016/j.maturitas.2013.10.011 [DOI] [PubMed] [Google Scholar]
- 13.Calciolari E, Donos N, Park JC, Petrie A, Mardas N. Panoramic measures for oral bone mass in detecting osteoporosis: a systematic review and meta-analysis. J Dent Res 2015; 94(Suppl. 3): 17S–27S. doi: https://doi.org/10.1177/0022034514554949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koh KJ, Kim KA. Utility of the computed tomography indices on cone beam computed tomography images in the diagnosis of osteoporosis in women. Imaging Sci Dent 2011; 41: 101–6. doi: https://doi.org/10.5624/isd.2011.41.3.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barngkgei I, Al Haffar I, Khattab R. Osteoporosis prediction from the mandible using cone-beam computed tomography. Imaging Sci Dent 2014; 44: 263–71. doi: https://doi.org/10.5624/isd.2014.44.4.263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barngkgei I, Al Haffar I, Shaarani E, Khattab R, Mashlah A. Assessment of jawbone trabecular bone structure amongst osteoporotic women by cone-beam computed tomography: the OSTEOSYR project. J Investig Clin Dent 2016; 7: 332–340. doi: https://doi.org/10.1111/jicd.12170 [DOI] [PubMed] [Google Scholar]
- 17.Barngkgei I, Joury E, Jawad A. An innovative approach in osteoporosis opportunistic screening by the dental practitioner: the use of cervical vertebrae and cone beam computed tomography with its viewer program. Oral Surg Oral Med Oral Pathol Oral Radiol 2015; 120: 651–9. doi: https://doi.org/10.1016/j.oooo.2015.08.008 [DOI] [PubMed] [Google Scholar]
- 18.Güngör E, Yldirim D, Cevik R. Evaluation of osteoporosis in jaw bones using cone beam CT and dual-energy X-ray absorptiometry. J Oral Sci 2016; 58: 185–94. doi: https://doi.org/10.2334/josnusd.15-0609 [DOI] [PubMed] [Google Scholar]
- 19.Mostafa RA, Arnout EA, Abo El-Fotouh M. Feasibility of cone beam computed tomography radiomorphometric analysis and fractal dimension in assessment of postmenopausal osteoporosis in correlation with dual X-ray absorptiometry. Dentomaxillofac Radiol 2016; 45: 20160212. doi: https://doi.org/10.1259/dmfr.20160212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol 1999; 28: 245–8. doi: https://doi.org/10.1038/sj/dmfr/4600448 [DOI] [PubMed] [Google Scholar]
- 21.Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: 106–14. doi: https://doi.org/10.1016/j.tripleo.2008.03.018 [DOI] [PubMed] [Google Scholar]
- 22.Verheij JG, Geraets WG, van der Stelt PF, Horner K, Lindh C, Nicopoulou-Karayianni K, et al. Prediction of osteoporosis with dental radiographs and age. Dentomaxillofac Radiol 2009; 38: 431–7. doi: https://doi.org/10.1259/dmfr/55502190 [DOI] [PubMed] [Google Scholar]
- 23.Gomes CC, de Rezende Barbosa GL, Bello RP, Bóscolo FN, de Almeida SM. A comparison of the mandibular index on panoramic and cross-sectional images from CBCT exams from osteoporosis risk group. Osteoporos Int 2014; 25: 1885–90. doi: https://doi.org/10.1007/s00198-014-2696-3 [DOI] [PubMed] [Google Scholar]
- 24.Pauwels R, Jacobs R, Singer SR, Mupparapu M. CBCT-based bone quality assessment: are Hounsfield units applicable? Dentomaxillofac Radiol 2015; 44: 20140238. doi: https://doi.org/10.1259/dmfr.20140238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Müller R. Bone microarchitecture assessment: current and future trends. Osteoporos Int 2003; 14(Suppl. 5): S89–95. [DOI] [PubMed] [Google Scholar]
- 26.Ibrahim N, Parsa A, Hassan B, van der Stelt P, Wismeijer D. Diagnostic imaging of trabecular bone microstructure for oral implants: a literature review. Dentomaxillofac Radiol 2013; 42: 20120075. doi: https://doi.org/10.1259/dmfr.20120075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ibrahim N, Parsa A, Hassan B, van der Stelt P, Aartman IH, Wismeijer D. The effect of scan parameters on cone beam CT trabecular bone microstructural measurements of human mandible. Dentomaxillofac Radiol 2013; 42: 20130206. doi: https://doi.org/10.1259/dmfr.20130206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parsa A, Ibrahim N, Hassan B, van der Stelt P, Wismeijer D. Bone quality evaluation at dental implant site using multislice CT, micro-CT, and cone beam CT. Clin Oral Implants Res 2015; 26: e1–7. doi: https://doi.org/10.1111/clr.12315 [DOI] [PubMed] [Google Scholar]
- 29.Hua Y, Nackaerts O, Duyck J, Maes F, Jacobs R. Bone quality assessment based on cone beam computed tomography imaging. Clin Oral Implants Res 2009; 20: 767–71. doi: https://doi.org/10.1111/j.1600-0501.2008.01677.x [DOI] [PubMed] [Google Scholar]
- 30.Schulze R, Heil U, Gross D, Bruellmann DD, Dranischnikow E, Schwanecke U, et al. Artefacts in CBCT: a review. Dentomaxillofac Radiol 2011; 40: 265–73. doi: https://doi.org/10.1259/dmfr/30642039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Diniz-Freitas M, Fernández-Montenegro P, Fernández-Feijoo J, Limeres-Posse J, González-Mosquera A, Vázquez-García E, et al. Mandibular cortical indices on cone-beam computed tomography images in osteoporotic women on treatment with oral bisphosphonates. Gerodontology 2016; 33: 155–60. doi: https://doi.org/10.1111/ger.12121 [DOI] [PubMed] [Google Scholar]
- 32.Geibel MA, Löffler F, Kildal D. Osteoporosis detection using cone-beam computed tomography. [In German.] Orthopade 2016; 45: 1066–71. doi: https://doi.org/10.1007/s00132-016-3340-z [DOI] [PubMed] [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010; 8: 336–41. doi: https://doi.org/10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- 34.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. ; QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011; 155: 529–36. doi: https://doi.org/10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 35.Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc 2006; 72: 75–80. [PubMed] [Google Scholar]
- 36.Guerrero ME, Noriega J, Castro C, Jacobs R. Does cone-beam CT alter treatment plans? Comparison of preoperative implant planning using panoramic versus cone-beam CT images. Imaging Sci Dent 2014; 44: 121–8. doi: https://doi.org/10.5624/isd.2014.44.2.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sandhu SK, Hampson G. The pathogenesis, diagnosis, investigation and management of osteoporosis. J Clin Pathol 2011; 64: 1042–50. doi: https://doi.org/10.1136/jcp.2010.077842 [DOI] [PubMed] [Google Scholar]
- 38.Torres SR, Chen CS, Leroux BG, Lee PP, Hollender LG, Schubert MM. Fractal dimension evaluation of cone beam computed tomography in patients with bisphosphonate-associated osteonecrosis. Dentomaxillofac Radiol 2011; 40: 501–5. doi: https://doi.org/10.1259/dmfr/14636637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Torres SR, Chen CS, Leroux BG, Lee PP, Hollender LG, Santos EC, et al. Mandibular cortical bone evaluation on cone beam computed tomography images of patients with bisphosphonate-related osteonecrosis of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: 695–703. doi: https://doi.org/10.1016/j.oooo.2011.11.011 [DOI] [PubMed] [Google Scholar]
- 40.Ibrahim N, Parsa A, Hassan B, van der Stelt P, Aartman IH, Wismeijer D. Accuracy of trabecular bone microstructural measurement at planned dental implant sites using cone-beam CT datasets. Clin Oral Implants Res 2014; 25: 941–5. doi: https://doi.org/10.1111/clr.12163 [DOI] [PubMed] [Google Scholar]
- 41.Kamburoglu K, Murat S, Kolsuz E, Kurt H, Yüksel S, Paksoy C. Comparative assessment of subjective image quality of cross-sectional cone-beam computed tomography scans. J Oral Sci 2011; 53: 501–8. doi: https://doi.org/10.2334/josnusd.53.501 [DOI] [PubMed] [Google Scholar]
- 42.Ibrahim N, Parsa A, Hassan B, van der Stelt P, Aartman IH, Nambiar P. Influence of object location in different FOVs on trabecular bone microstructure measurements of human mandible: a cone beam CT study. Dentomaxillofac Radiol 2014; 43: 20130329. doi: https://doi.org/10.1259/dmfr.20130329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eckstein F, Lochmuller EM, Lill CA. Bone strength at clinically relevant sites displays substantial heterogeneity and is best predicted from site-specific bone densitometry. J Bone Miner Res 2002; 17: 162–71. doi: https://doi.org/10.1359/jbmr.2002.17.1.162 [DOI] [PubMed] [Google Scholar]
- 44.Naitoh M, Kurosu Y, Inagaki K, Katsumata A, Noguchi T, Ariji E. Assessment of mandibular buccal and lingual cortical bones in postmenopausal women. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 104: 545–50. doi: https://doi.org/10.1016/j.tripleo.2007.04.034 [DOI] [PubMed] [Google Scholar]