Abstract
As the volume and complexity of imaging in the UK continues to rise, there is pressure on radiologists to spend increasing lengths of time reporting to cope with the growing workload. However, there is limited guidance for radiologists about structuring the working day to strike the necessary balance between achieving satisfactory reporting volume and maintaining quality and safety. We surveyed 86 neuroradiologists (receiving 59 responses), regarding time spent reporting, frequency and duration of work breaks, and break activities. Our results demonstrate that some neuroradiologists report for up to 12 h a day and for 4 h before taking a break. Mean duration of breaks is less than 15 min and these often consist of computer screen-based or cognitively demanding tasks. Many areas of medicine have looked to the aviation industry to develop improvements in safety through regulated, standardised practices. There are parallels between the work of air traffic controllers (ATCs) and radiologists. We review the legislation that controls the working hours of UK ATCs to minimise fatigue-related errors, and its scientific basis. We also consider the vigilance decrement, a concept in cognitive science which describes the reduction in performance with increasing time-on-task. We conclude that, in comparison with ATCs, work patterns among radiologists are poorly standardised and potentially dangerous. Evidence suggests that placing limits on reporting time and minimum break duration, as well as ensuring appropriate break activities, can benefit reporting quality. It is imperative that radiologists and managers heed these lessons, to improve standards and protect patients from error.
INTRODUCTION
Recent trends in medical practice have led to a significant increase in the reporting workload for radiologists in the UK. In England, average annual growth in the total number of cross-sectional imaging studies (CT and MRI) has been over 10%,1 but the workforce of consultant radiologists is only growing by 3% annually.2 With this mismatch comes mounting pressure on radiologists to report a greater volume of scans.
It is known that radiologists’ behaviours, e.g. time spent reviewing each examination, change over the course of a reporting session3 and that at the end of the working day, radiologists’ visual performance and ability to detect pathology is lower than at the start of the day.4,5 It follows that longer reporting sessions may lead to higher error rates. It has also been established that eye strain is a significant issue for radiologists who report for long periods, contributing to reporting errors and burn out.6,7
Yet, there is no established consensus on the optimum duration and structure of reporting sessions. It also seems likely that there is considerable variability in the preferences of individual radiologists in this regard. The UK’s Royal College of Radiologists, in its guide to job-planning for radiologists, states that “adequate time (should) be provided in job plans to deliver the workload expected safely and without compromise on quality”8 but contains no specific recommendations about length of reporting sessions or work breaks.
It has been suggested that, in the future, intelligent PACS workstations will be developed with integrated fatigue measurement systems, providing direct feedback to users.7 These would not only help individual radiologists to plan workdays around their own individual attributes, but also aid development of generic guidelines for radiologists. However, any such system is a long way off entering routine practice in the UK.
Questionnaire study
To establish current practices, we surveyed neuroradiologists from the UK (including Scotland, Northern Ireland, Wales and England). We restricted our survey to neuroradiologists, as we wanted a group of respondents with a relatively homogeneous type of work. In December 2016, we sent via email the following short questionnaire, allowing free-text responses, to 86 consultant neuroradiologists (a mixture of interventional and diagnostic specialists):
In your current work pattern, what is the longest period in any 1 day in which your primary function is to report?
Generally speaking, after what period of reporting do you actively take a break?
Typically, how long is the work break that you take?
Typically, what does a work break consist of?
We received 59 responses (69% response rate). Where respondents gave a range of times in answer to questions 1–3, we took a midpoint of the range for the purposes of data analysis (i.e. for a response “10–20 min”, we used 15 in our analysis). We excluded from analysis any responses to questions 1–3 which contained non-numerical data (e.g. where a respondent answered “variable” to Question 3).
RESULTS
Question 1: One respondent did not answer this question.
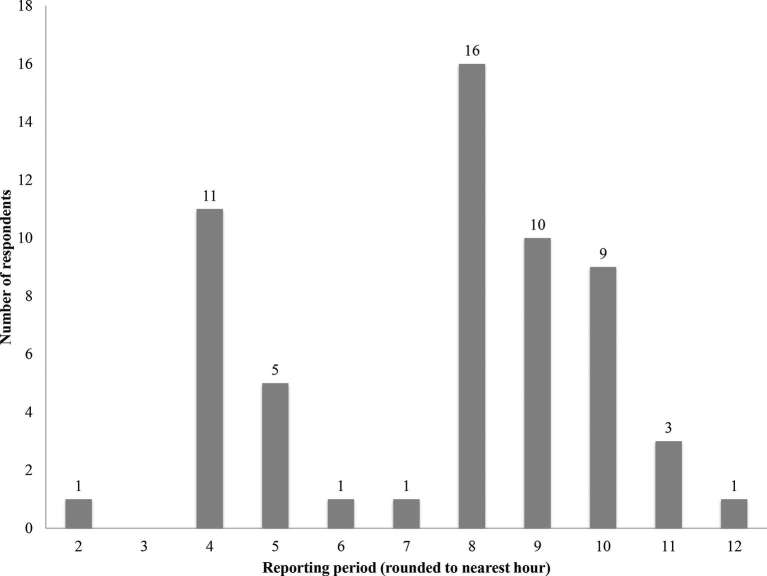
Maximum daily reporting time varied widely (2–12 h). The mean was 7.5 h and the median 8 h. 23 out of 59 respondents (39.0%) report for more than 8 h (Figure 1).
Figure 1.
Responses to Question 1—In your current work pattern, what is the longest period in any one day in which your primary function is to report?
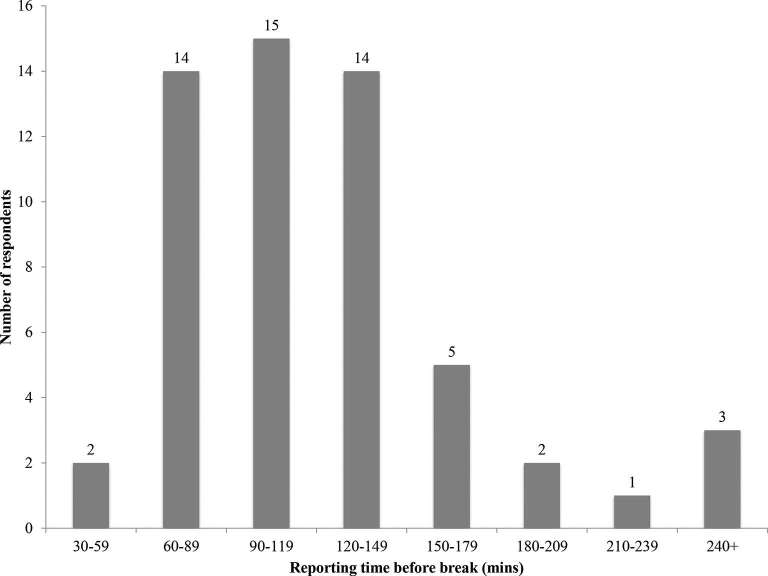
Question 2: Three respondents did not provide numerical answers to this question—their answers have not been included in Figure 2.
Figure 2.
Responses to Question 2—Generally speaking, after what period of reporting do you actively take a break?
Reporting time before taking a break ranged from 45 to 240 min, with a mean of 111 min and a median of 105 min. 41 of 59 of respondents (69.5%) take a break after 1–2 h, with 11 (18.6%) reporting for 2.5 h or more before breaking.
Question 3: One respondent did not answer this question. Two respondents did not provide numerical answers to this question—their answers have not been included in Figure 3.
Figure 3.
Responses to Question 3—Typically, how long is the work break that you take?
Mean break duration was 14.5 min, with a median of 12.5 min. Only 8 out of 59 respondents (13.6%) take breaks of 30 min or more.
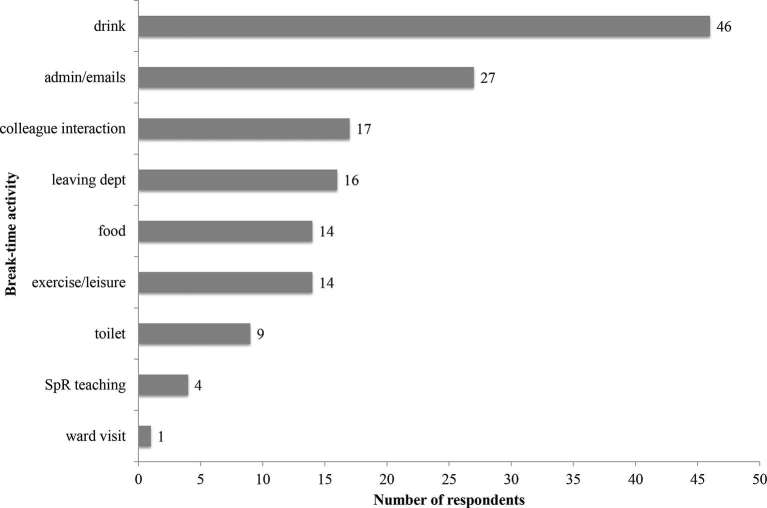
Question 4: One respondent did not answer this question. 41 respondents provided more than one activity in response to this question.
46 of 59 (78%) respondents’ breaks typically include taking a drink of some kind. Emails, letters and other generic administrative tasks featured for 27 out of 59 (46%). Some kind of colleague interaction, leaving the radiology department and exercise were the other common activities (Figure 4). Four responses included supervision or teaching of radiology registrars, four included work-related phone calls or consultations with clinical colleagues and one included visiting the ward to review patients.
Figure 4.
Most frequent responses to Question 4—Typically, what does a work break consist of?
DISCUSSION
Having collected these results, we wanted to compare the working patterns of neuroradiologists with those of professionals working in an industry with more standardised and tightly regulated practices. For many years, medicine has been learning from the aviation industry, not least in the development and implementation of the WHO surgical safety checklist.9 We feel there are clear parallels between the work of radiologists and air traffic controllers (ATCs); in common with radiologists, ATCs’ work involves periods of intense concentration and the analysis of visual information from computer monitors. Both ATCs and radiologists must provide clear and timely information to enable their colleagues (be they pilots or clinicians) to operate safely. Any factors which may impair perception or ability to concentrate can have a significant effect on the performance of both groups, with potentially serious consequences for patients or passengers.
ATCs’ hours are standardised across the UK according to the Civil Aviation Authority’s Scheme for Regulation of Air Traffic Controllers’ Hours (SRATCOH), “to ensure, so far as is reasonably possible, that controller fatigue does not endanger aircraft and thereby to assist controllers to provide a safe and effective service”.10 Key components of SRATCOH are that:
“No operational duty shall exceed a period of 2 h without there being taken during, or at the end of, that period a break or breaks totalling not less than 30 min”10 and “Breaks shall include all measures necessary to ensure that controllers will not be suffering…as a consequence of their duties, mental or physical fatigue… Such measures are expected to include a certain detachment from the operation, e.g. rest areas, which shall afford the individual “quiet space” and facilities for adequate refreshment”.10
We interviewed members of a regional International Airport’s Air Traffic Control team, with a specific focus on working patterns, shift length and break activities. At this Airport, the longest daytime shifts, including breaks and handover periods, are less than 8 h in duration, with working weeks limited to 37 h. For comparison, 39% of our survey respondents report for more than 8 h in a day. ATCs’ night-time shifts are longer (9.5 h) than day shifts, but only because the volume of air traffic during night hours is significantly reduced. In a busier airport, such as Heathrow, where the work is routinely of higher intensity, controllers are generally on duty for only an hour at a time before having a rostered break. Controllers we interviewed, all stated that they strive to avoid cognitively demanding tasks during their 30 min breaks, with favoured activities including food, drink, relaxing in the communal staff room, watching television and walking outside. Contrast this with our survey responses, with a mean break duration of 15 min, only 13.6% taking breaks of 30 min or more, and many breaks including cognitively demanding activities.
The regulations contained in SRATCOH are similar to those in place in other nations across the European Union, being largely based on recommendations from The European Organisation for the Safety of Air Navigation. These recommendations are in turn based on a thorough review11 of the existing literature in the field of ergonomics, the study of human factors and working conditions. We consider below some of the most relevant studies in view of our survey findings.
The work of Rosa has repeatedly shown decreased cognitive performance (measured by reaction time, mental arithmetic and grammatical reasoning tests) and alertness in those working 12 hour days compared to 8 hour days12, 13, although other studies have failed to demonstrate significant performance differences between ATCs working 8 vs 10 h days.14 Among professional drivers, the risk of accidents has been shown to increase with time on shift, with the steepest increase occurring after 10 h on duty.15 On the other hand, there may be psychosocial benefits to working longer hours for fewer days per week, allowing more time for leisure and family activities.16 It should be stressed that many of these studies focus on professions, such as drivers and factory workers, with more physical (and perhaps fewer) cognitive demands than neuroradiology or ATC. Furthermore, much of the ergonomics literature concentrates on working environments which require 24 h staffing, which may be less applicable to neuroradiology, in which the majority of the workload can be dealt with during “normal” working hours.
Multiple breaks during the working day significantly reduce accident risk,17 and taking short breaks every hour (on top of a standard 30 min lunch break) does not decrease productivity among factory workers.18 Studies also show that the design of breaks can result in faster recovery and slow the reduction in performance through the working day; specifically, exercise or “active relaxation” has been shown to accelerate recovery.11
When considering the optimum structure for radiologists’ reporting sessions, we can also look to cognitive psychology for help with certain fundamental questions—how does performance vary with time spent on a cognitively demanding task? How long can we sustain attention during such tasks? And what is the effect of taking breaks on cognitive performance?
A critical concept when attempting to answer these questions is vigilance. For cognitive scientists, vigilance refers to the ability to sustain attention.19 It encompasses both “the degree of arousal… and the level of cognitive performance”20 in experimental subjects. Vigilance was first studied systematically in the mid-20th Century by Mackworth, who proposed the term vigilance decrement to describe the fall in subjects’ performance over time in a number of cognitive tasks.21
It has long been established that vigilance decreases after 30 min on relatively straightforward tasks, such as the Mackworth Clock test, where participants must recognise when a clock jumps forward 2 s rather than 1 s, which it is programmed to do at infrequent, irregular intervals.22 There is some controversy over the degree to which the observed decrement in these original studies is related to boredom (i.e. progressively reduced arousal during a monotonous task) or cognitive fatigue (i.e. increasing difficulty in sustaining mental effort).23 It is questionable whether the relatively simple tasks from the original vigilance experiments are comparable with the more complex process of reporting a radiological investigation; however, later work suggests the vigilance decrement may be more pronounced for more demanding tasks.24 A recent study demonstrates a fall in performance after as little as 20 min for a taxing task, during which participants report a high degree of cognitive arousal,25 which may be a closer analogue of real-life radiology reporting, and may explain the observed change in radiologists’ performance over a session or day of reporting.3–5
The role of breaks in maintaining vigilance has also been widely studied. The original vigilance experiments showed that a 30 min break after 30 min of the vigilance task prevented any decline in performance.19 They also found that a brief distraction in the middle of a 2 h task (e.g. a short telephone message) produced a temporary improvement in performance.19 More recent work shows that regularly interspersing a second cognitive task during a 40 min vigilance test prevents a performance decrement in the primary task.26 The implication for radiologists is that regular breaks and also switching between different activities during reporting sessions are potentially critical to sustaining performance through the working day.
The survey results should be interpreted with a degree of caution—there are reasons why radiologists may over- or underestimate their hours worked in responding to a questionnaire. However, the overall impression from the survey is of a wide variety in reporting practices among UK neuroradiologists, with some reporting for up to 12 h a day and most reporting for 8 h or more. Although most take breaks after 1–2 h of reporting, a significant proportion (18.6%) work for 2.5 h or more before breaking. In contrast, ATCs have working days limited to 8 h, with enforced breaks after every 2 h of work, in line with recommendations from the relevant literature in ergonomics.11
Experimental psychology has established that cognitive performance decreases after as little as 20–30 min on a particular task,21,22,25 with boredom and fatigue contributing to varying degrees. As radiological investigations become increasingly complex, there is an additional risk of cognitive overload, whereby the radiologist’s ability to process the necessary volume of information becomes overwhelmed.27 As radiologists are working increasingly close to their maximum cognitive capacity, the avoidance of fatigue-related performance decrements is all the more important.
Taking regular breaks and switching between different tasks has been shown to protect against such performance decrements.19 Yet, our survey suggests neuroradiologists’ work breaks are generally short, with the majority less than 15 min. A significant proportion (15.3%) stated that their breaks typically consist of cognitively demanding work such as registrar teaching or clinical consultations. Nearly half use breaks to respond to emails and complete other computer screen-based administrative tasks, putting themselves at greater risk of eye strain or visual fatigue. ATCs, on the other hand, take 30-min breaks, with specific guidance that the purpose of breaks is to minimise physical and mental fatigue and should include “detachment” from work-related activities.
Conclusion
In summary, we have established that current working practices among neuroradiologists, in contrast with ATCs, are highly variable and in many cases potentially unsafe. Although we surveyed neuroradiologists, it seems likely that the situation for the general radiology workforce is similar. Our findings are unsurprising given the absence of clear guidance for radiologists, in the face of everincreasing workload. It is, therefore, essential that UK radiologists consider the importance of limiting the duration of reporting sessions and taking regular, adequate breaks. In addition, employers and managers must adjust their expectations of reporting output accordingly. Otherwise, radiologists will be unable to minimise reporting errors and keep patients safe.
Footnotes
ACKNOWLEDGMENTS: Thank you to Dr Steven McKinstry who suggested to us the parallels between radiology reporting and air traffic control.
Contributor Information
John Reicher, Email: Reicher13@gmail.com.
Stuart Currie, Email: stuartcurrie@nhs.net.
Daniel Birchall, Email: daniel.birchall@nuth.nhs.uk.
REFERENCES
- 1.NHS England Analytical Services. NHS imaging and radiodiagnostic activity. 2014. Available from: www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2013/04/KH12-release-2013-14.pdf [August 2014]
- 2.Royal College of Radiologists. Clinical radiology UK workforce census 2015 report. 2016. Available from: www.rcr.ac.uk/system/files/publication/field_publication_files/bfcr166_cr_census.pdf [September 2016]
- 3.Taylor-Phillips S, Elze MC, Krupinski EA, Dennick K, Gale AG, Clarke A, et al. Retrospective review of the drop in observer detection performance over time in lesion-enriched experimental studies. J Digit Imaging 2015; 28: 32–40. doi: 10.1007/s10278-014-9717-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krupinski EA, Berbaum KS, Caldwell RT, Schartz KM, Kim J. Long radiology workdays reduce detection and accommodation accuracy. J Am Coll Radiol 2010; 7: 698–704. doi: 10.1016/j.jacr.2010.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krupinski EA, Berbaum KS, Caldwell RT, Schartz KM, Madsen MT, Kramer DJ. Do long radiology workdays affect nodule detection in dynamic CT interpretation? J Am Coll Radiol 2012; 9: 191–8. doi: 10.1016/j.jacr.2011.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vertinsky T, Forster B. Prevalence of eye strain among radiologists: influence of viewing variables on symptoms. AJR Am J Roentgenol 2005; 184: 681–6. doi: 10.2214/ajr.184.2.01840681 [DOI] [PubMed] [Google Scholar]
- 7.Reiner BI, Krupinski E. The insidious problem of fatigue in medical imaging practice. J Digit Imaging 2012; 25: 3–6. doi: 10.1007/s10278-011-9436-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Royal College of Radiologists. A guide to job planning in clinical radiology. 2013. Available from: https://www.rcr.ac.uk/sites/default/files/BFCR(13)9_job_plans.pdf [December 2013]
- 9.Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009; 360: 491–9. doi: 10.1056/NEJMsa0810119 [DOI] [PubMed] [Google Scholar]
- 10.Safety and Airspace Regulation Group Civil Aviation Authority. CAP 670, Air traffic services safety requireTraffic Services Safety Requirements, Part D Section 2. 2014. Available from: http://publicapps.caa.co.uk/modalapplication.aspx?appid=11&mode=detail&id=200 [May 2014]
- 11.European Organisation for the Safety of Air Navigation. Managing shiftwork in European ATM: literature review. 2006. Available from: https://www.eurocontrol.int/sites/default/files/field_tabs/content/documents/nm/safety/managing-shiftwork-in-european-atm-literature-review.pdf [April 2006]
- 12.Rosa RR, Colligan MJ, Lewis P. Extended workdays: effects of 8-hour and 12-hour rotating shift schedules on performance, subjective alertness, sleep patterns, and psychosocial variables. Work Stress 1989; 3: 21–32. doi: 10.1080/02678378908256877 [DOI] [Google Scholar]
- 13.Rosa RR, Bonnet MH. Performance and alertness on 8 h and 12 h rotating shifts at a natural gas utility. Ergonomics 1993; 36: 1177–93. doi: 10.1080/00140139308967987 [DOI] [PubMed] [Google Scholar]
- 14.Schroeder DJ, Rosa RR, Witt LA. Some effects of 8- vs. 10-hour work schedules on the test performance/alertness of air traffic control specialists. Int J Ind Ergon 1998; 21(3-4): 307–21. doi: 10.1016/S0169-8141(97)00044-9 [DOI] [Google Scholar]
- 15.Folkard S. Black times: temporal determinants of transport safety. Accid Anal Prev 1997; 29: 417–30. doi: 10.1016/S0001-4575(97)00021-3 [DOI] [PubMed] [Google Scholar]
- 16.Williamson AM, Gower CG, Clarke BC. Changing the hours of shiftwork: a comparison of 8- and 12-hour shift rosters in a group of computer operators. Ergonomics 1994; 37: 287–98. doi: 10.1080/00140139408963646 [DOI] [PubMed] [Google Scholar]
- 17.Chen C, Xie Y. The impacts of multiple rest-break periods on commercial truck driver’s crash risk. J Safety Res 2014; 48: 87–93. doi: 10.1016/j.jsr.2013.12.003 [DOI] [PubMed] [Google Scholar]
- 18.Dababneh AJ, Swanson N, Shell RL. Impact of added rest breaks on the productivity and well being of workers. Ergonomics 2001; 44: 164–74. doi: 10.1080/00140130121538 [DOI] [PubMed] [Google Scholar]
- 19.Stroh S. Vigilance: the problem of sustained attention : Eysenck H, International series of monographs in experimental psychology. Vol 13 Oxford, UK: The British Institute of Radiology.; 1971. 1–4. [Google Scholar]
- 20.Oken BS, Salinsky MC, Elsas SM. Vigilance, alertness, or sustained attention: physiological basis and measurement. Clin Neurophysiol 2006; 117: 1885–901. doi: 10.1016/j.clinph.2006.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mackworth JF. Performance decrement in vigilance, threshold, and high-speed perceptual motor tasks. Can J Psychol 1964; 18: 209–23. doi: 10.1037/h0083302 [DOI] [PubMed] [Google Scholar]
- 22.Mackworth NH. The breakdown of vduring prolonged visual search. Q J Exp Psychol 1948; 1: 6–21. doi: 10.1080/17470214808416738 [DOI] [Google Scholar]
- 23.Pattyn N, Neyt X, Henderickx D, Soetens E. Psychophysiological investigation of vigilance decrement: boredom or cognitive fatigue? Physiol Behav 2008; 93: 369–78. doi: 10.1016/j.physbeh.2007.09.016 [DOI] [PubMed] [Google Scholar]
- 24.See JE, Howe SR, Warm JS, Dember WN. Meta-analysis of the sensitivity decrement in vigilance. Psychol Bull 1995; 117: 230–49. doi: 10.1037/0033-2909.117.2.230 [DOI] [Google Scholar]
- 25.Grier RA, Warm JS, Dember WN, Matthews G, Galinsky TL, Parasuraman R. The vigilance decrement reflects limitations in effortful attention, not mindlessness. Hum Factors 2003; 45: 349–59. doi: 10.1518/hfes.45.3.349.27253 [DOI] [PubMed] [Google Scholar]
- 26.Ariga A, Lleras A. Brief and rare mental “breaks” keep you focused: deactivation and reactivation of task goals preempt vigilance decrements. Cognition 2011; 118: 439–43. doi: 10.1016/j.cognition.2010.12.007 [DOI] [PubMed] [Google Scholar]
- 27.Krupinski EA, Berbaum KS. The medical image perception society update on key issues for image perception research. Radiology 2009; 253: 230–3. doi: 10.1148/radiol.2531090237 [DOI] [PMC free article] [PubMed] [Google Scholar]