Abstract
Youth involved in the juvenile justice system are at risk for emotional and behavioral problems. However, research with court-involved adolescents has neglected to examine the mental health of their parents, who may also have significant personal and parenting stress. This sample consisted of 144 parent-adolescent dyads. Adolescents (aged 11 to 17 years) identified by court officials were referred to the study to receive mental health treatment. Parents and adolescents completed surveys about their mental health diagnoses, treatment, and family relationships. Using the clinical cut-off for the global severity index of the Symptom Checklist-90-Revised, bivariate and multiple logistic regression analyses were performed to examine group differences between parents with and without significant mental health symptoms. Results indicated that 35% of parents endorsed clinically significant mental health symptoms. Parents with clinically significant symptoms, compared to those without, reported significantly greater parenting stress (p < .05), and were more likely to have received prior mental health treatment (54% vs. 25%; p < .05) and a psychiatric diagnosis (52% vs. 19%; p < .05). Our findings revealed that more than one in three parents of court-involved adolescents are currently experiencing significant mental health symptoms. Improved mental health screening and intervention that incorporates the unique needs of families is recommended, including the possible use of family-based approaches as well as individualized treatment for the parents of court-involved youth.
Keywords: adolescents, juvenile justice, parents, mental health, parenting stress
The National Center for Juvenile Justice estimates that 1 million adolescents in the United States are charged by the courts each calendar year (Hockenberry & Puzzanchera, 2015). Due to a teenager's status as a minor, parents also interact with court personnel (e.g., judge, probation officer) throughout the course of their child's legal involvement. This process may place a significant burden on parents who might not be adequately supported to manage the additional strain on their family. Engaging with the services needed to comply with court orders and to reduce the likelihood of recidivism (e.g., mental health treatment, psychiatric medication, case management) requires substantial time and resources on the part of the family.
Difficulty engaging in mental health services is particularly problematic given that mental health and substance abuse problems are common among court-involved youth. For example, one study found that 70% were diagnosed with a psychiatric disorder (Skowyra & Cocozza, 2007). Compared to their peers, court-involved youth have high rates of anxiety, depression, and conduct disorders (Carswell, Maughan, Davis, Davenport, & Goddard, 2004; Cocozza & Skowyra, 2000). Studies among juvenile offenders have also found high rates of alcohol and cannabis use in the past year, ranging from 40% to 80% (Mulvey, 2011; Young, Dembo, & Henderson, 2007). Court officials may refer these youth for counseling services, but all too often mental health care is not received (Maschi, Hatcher, Schwalbe, & Rosato, 2008). For example, Burke, Mulvey, and Schulbert (2015) found that 74% of youth who made their first contact with the court system had a psychiatric disorder, yet only 20% reported receipt of mental health services at follow-up assessments. In a study that examined lifetime rates of mental health service use among adolescents who received services in at least one public sector of care (i.e., alcohol and drug services, child welfare, juvenile justice, mental health, and special education services for serious emotional disturbance), court-involved youth had the lowest rates of mental health care utilization (Hazen, Hough, Landsverk, & Wood, 2004). Oftentimes, the referral from a court official is the only mental health recommendation that the family receives. Parents themselves are seldom referred for their own treatment when indicated (Burns et al., 1995; Rosenblatt, Rosenblatt, & Biggs, 2000).
Notably, the degree of monitoring of youth behavior as well as mental health needs varies within the court. The Juvenile Court System is separated into different divisions to address specific issues such as minor offenses, substance use, and truancy. Each of these divisions varies in the frequency and degree to which court officials monitor an adolescent's needs and progress (Hiller & Saum, 2014). For example, juveniles who appear formally in court would be considered to have a “high degree of monitoring” due to regular court hearings and mandated court contacts. Due to nationwide policy changes aimed toward increasing rates of juveniles diverted from contact with formal court processes or detention, many first-time offending youth (with a less severe first time charge) are typically monitored by an intake or diversion program outside of the formal court process (Schwalbe, Gearing, MacKenzie, Brewer, & Ibrahim, 2012). The goal of such diversion programs is to provide the youth and family with services, including referrals, as relevant, to mental health and/or substance use treatment that will reduce risk for recidivism (Cocozza et. al., 2005; Whitehead & Lab, 2001).
The mental health and substance use needs of court-involved youth and their parents is relevant to the juvenile diversion process and reducing rates of juvenile recidivism (Vermeiren, Jespers, & Moffitt, 2006). The few studies that have collected data on the parents of court-involved youth have reported high rates of alcohol abuse (29-52.7%; Barylnik, 2003; Dembo et al., 2000; Lederman, Dakof, Larrea, & Li, 2004), other substance use problems (25-29%; Dembo et al., 2000; Lederman et al., 2004), and mental health problems (18.6-23%; Barylnik, 2003; Dembo et al., 2000; Lederman et al., 2004) among parents. In addition, Dembo et al. (2000) found that 70% of court-involved youth had a family member who had been arrested and 50% had a family member who had been convicted of a crime. Lederman et al. (2004) reported that 61% of detained females indicated that a parent or other close family member had criminal justice involvement.
Notably, the relation between parent and youth mental health/substance use problems is likely transactional and bidirectional (Wills & Dishion, 2004). Indeed, the interactional nature of parent-child relationships (e.g. parent inflicts a stress on the child that the child must react/adapt to and vice versa) and their intersection with mental health problems of both parents and child has been well documented in community samples (Berg-Nielsen, Vikan, & Dahl, 2002). Children who have parents with mental health problems report elevated rates of psychiatric disorders and problem behavior (Angold et al., 1998; Roustit, Campoy, Chaix, & Chauvin, 2010). High levels of parenting stress, often associated with mental health symptoms, have been associated with greater, internalizing and externalizing behaviors in children and adolescents (Anderson, 2008; Duchovic, Gerkensmeyer, & Wu, 2009; Kim, Viner-Brown, & Garcia, 2007). Parents of children with mental health problems, in turn, also report elevated rates of stress and psychiatric disorders. For example, one study found that mothers of children with attention-deficit/ hyperactivity disorder and/or conduct disorder were more likely to have depressive disorders, anti-personality disorders, and histories of court involvement than mothers of children without disorders (Lahey et al., 1988). Other studies have found elevated levels of depression, antisocial behavior, anxiety, and substance use among parents of depressed children (Kaslow, Deering, & Racusin, 1994; Kutcher & Marton, 1991; Livingston, Nugent, Rader, & Smith, 1985; Mitchell, McCauley, Burke, Calderon, & Schloredt, 1989; Puig-Antich et al., 1989).
In addition to affecting youth mental health, parent psychological distress also impacts key processes central to effective parenting such as self-efficacy and parenting competence (Preyde et al., 2014). Yet, strong parenting skills are needed to address behavioral and substance use problems among youth. Incorporating parents in treatment for troubled youth results in improvement in family functioning and contributes to reductions in delinquent behavior (Huey, Henggeler, Brondino, & Pickrel, 2000). However, referrals to address parent-related symptoms in the context of treatment for court-involved youth are typically not pursued. As suggested above, poor parental mental health may interfere with a family's ability to comply with court demands and access needed help, thereby limiting the potential efficacy of interventions for court-involved youth.
Our study therefore sought to contribute to this nascent area of research by examining: (a) the prevalence of mental health symptoms in parents of court-involved adolescents; and (b) the degree to which socio-demographic, legal, and mental health related variables (e.g., income level, court involvement, co-caregiver, parenting stress, adolescent mental health) are associated with parental symptomatology. We hypothesized that parents of court-involved youth would report high rates of mental health symptoms. Further, parents with clinically significant mental health symptoms would be more likely than those without to: (a) have history of psychiatric diagnosis and mental health treatment; (b) be the sole caregiver; (c) have less financial stability; (d) report more stress in their roles as parents; (e) have court-involved youth with greater mental health difficulties; and (f) have court-involved youth with a higher degree of court monitoring because of the adolescent's repeated or more severe charges.
Method
Procedure
All study protocols were approved by the Institutional Review Boards (IRBs) of the two sites conducting research for this study. Participants were recruited to participate in a longitudinal randomized control trial examining the impact of mental health treatment. This report utilizes data collected at baseline. Adolescent participants were between the ages of 11 and 17, so both adolescent assent and parental consent were obtained. Participants completed assessment measures on laptop computers using an audio computer-assisted self-interview (ACASI) program and completed paper copies of the Youth Self Report (YSR) and the Child Behavior Checklist (CBCL).
Participants
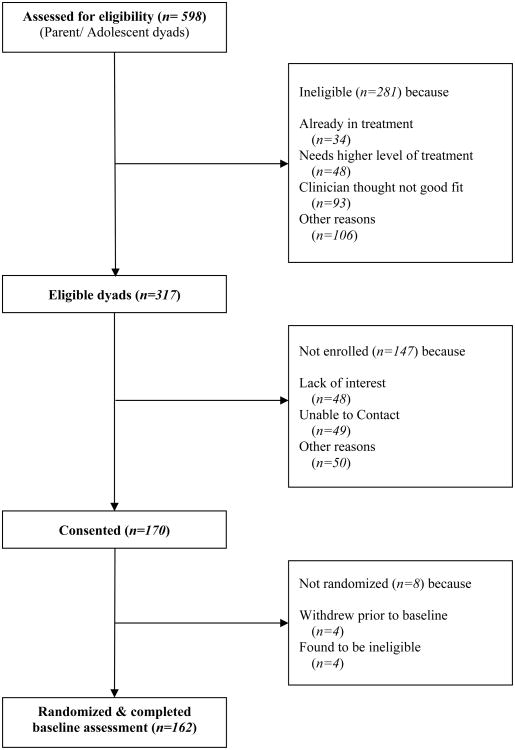
Participants were parent and adolescent dyads recruited in two eastern U.S. cities. Although parents were actively involved with the study, eligibility to participate was based upon the adolescent being referred by the court for mental health treatment. Inclusion criteria for adolescents included: 1) being between the ages of 11 and 17 at the time of the consent; 2) ability to speak and read English (Spanish-speaking parents were eligible to participate); 3) currently residing with a legal guardian able to attend weekly therapy sessions; and 4) having an open petition with the Juvenile Court System at the time of referral for treatment. Adolescents were excluded if they: 1) were already engaged in outpatient mental health treatment; 2) had a history of psychotic symptoms or other symptoms that would require specialized or intensive treatment; or 3) were charged with a sexual offense. Court officials (i.e., intake worker, probation officer, magistrate, judge) referred adolescents to the study when mental health services were thought to be appropriate for the case. Research assistants then screened participants for study eligibility. Court officials referred a total of 598 families to the study. Of the 598 referrals received 53% (n=317) were eligible to participate based upon the screening, and of those eligible 54% (n=170) consented to participate in the study and 162 completed the baseline assessment (Figure 1). The sample for this report includes 144 parents and teens with data on the main outcome variable – parental mental health symptoms.
Figure 1. Consort Sheet.
Measures
Sociodemographics
Parental age (in years), gender (male/ female), race (White/ other/ Native Hawaiian or Pacific Islander/ African American or Black / Asian/ Alaskan Native or American Indian/ multiple racial backgrounds) ethnicity (Hispanic/ Latino: yes/ no), number of children (under the age of 18 living in the home), income (> or ≤ $30,000 annually), employment (currently employed: yes/ no), educational background (highest level of education: elementary school/ middle school/ some high school/ high school graduate or GED/ college degree/ advanced degree/ other), history of psychiatric diagnosis (yes/ no), history of substance use and mental health treatment (yes/ no), arrest history (yes/ no), and presence of a co-parent (e.g., spouse, partner, grandparent) (yes/ no). Adolescents' age (in years), gender (male/ female), race (White/ other/ Native Hawaiian or Pacific Islander/ African American or Black / Asian/ Alaskan Native or American Indian/ multiple racial backgrounds), ethnicity (Hispanic/ Latino: yes/ no), and referral source (truancy or formal/ other) were also assessed.
For the current analysis, adolescents were categorized into two groups to describe their court involvement: those with an open Juvenile Court petition related to truancy and/or delinquency appearing before a judge/magistrate on a weekly, biweekly, or monthly schedule (n=78) are characterized as having a “high degree of court monitoring,” and those monitored informally by intake workers through a diversion or intake program (n=66) are characterized as having a “low degree of court monitoring.” These two groups differ in their level and frequency of court monitoring.
Symptom Checklist-90-Revised (SCL-90-R)
Parents completed the SCL-90-R (Derogatis, 1975), which is a 90 item measure assesses mental health symptom severity over the past week (e.g., “How much were you distressed by nervousness and shakiness inside?”). The Global Severity Index (GSI) was used to measure general parental mental health symptomatology. The GSI incorporates the number of symptoms and intensity of distress endorsed across numerous types of mental health areas (e.g., depression, anxiety, etc.), and thus is often used as a measure of general psychological symptomology (Derogatis & Melisaratos, 1983; Lam, Naar-King, & Wright, 2007). Responses for the measure range from 0 (not at all) to 4 (extremely) on a 5-point Likert-scale. Higher scores reflect more mental health symptoms. The GSI has different norms for females and males. For our analysis, those parents with scores above the threshold are categorized as having “clinically significant” mental health symptoms. Notably, establishing a diagnosis is beyond the scope of any screening instrument (Brown et al., 2015). The reliability and construct validity of this measure have been repeatedly demonstrated since the development of the scale (Derogatis & Unger, 2010). Good internal consistency was demonstrated with a Cronbach's alpha coefficient of .98 in the present sample.
Stress Index for Parents of Adolescents (SIPA)
The SIPA (Sheras & Abidin, 1998) is a screening instrument that identifies stressful aspects of parent-adolescent interactions. Specifically, this measure assesses the degree to which adolescent-parent interactions result in stress for parents, the quality of these interactions, and general stressful life circumstances. This study used the 34 items in the Parent Domain Subscale to assess parenting stress (e.g., “When I think about myself as a parent of a teenager, I believe I can handle anything that happens.”). Responses range from 1 (strongly disagree) to 5 (strongly agree) on a 5-point Likert-scale. Higher scores represent higher levels of parenting stress. The subscale's score is calculated by using the mean item level response for each participant. The SIPA has demonstrated good reliability and validity (Sheras & Abidin, 1998). In the present sample, strong internal consistency was demonstrated with a Cronbach's alpha coefficient of .93 for the Parent Domain Subscale.
Childhood Behavior Checklist (CBCL) and Youth Self-Report (YSR)
The CBCL (parent rated) and YSR (youth rated) are symptom inventories which each include 113 items tapping emotional and problem behaviors in youth, ages 6 to 18 years, evidenced in community and home settings over the past 6 months (Achenbach, 1995; Achenbach, 2001). Composite scores are obtained for internalizing, externalizing, and total problems, as well as for eight behavioral syndromes and six DSM-oriented scales (e.g., CBCL: There is very little that my teen enjoys.”; YSR:. “There is very little that I enjoy.”). Responses range from 0 (not true) to 2 (very true or often true) on a 3-point Likert-scale. Higher scores on both the CBCL and YSR indicate higher levels of emotional and behavioral problems in the youth with a cut-off of T ≥ 70 to denoting clinically significant symptoms. Many studies have confirmed the internal consistency and validity of both the CBCL and YSR with diverse populations (Achenbach, Dumenci, & Rescorla, 2002; Dutra, Campbell, & Westen, 2004; Ivanova et al., 2007).
Data Analyses
A two stage approach guided the analyses. First, to examine differences in the characteristics of parents who did versus did not meet the cut-off for clinically significant mental health symptoms, we conducted a series of bivariate comparisons of demographic and family variables, parent mental health and legal involvement indicators, and adolescent mental health indicators. Bivariate associations were tested for significance (p < .05) using chi-square tests for proportions and t-tests for mean differences. Next, in order to determine the most salient predictors of parents' clinically significant mental health symptoms (i.e., above and beyond the effects of other predictors), characteristics that significantly differentiated between parents with and without significant mental health symptoms at the bivariate level were added simultaneously to a single multiple logistic regression predicting the group with significant symptoms. Adjusted odds ratios (ORs) were examined for significance and effect size.
Of the 162 participants who were assessed, due to human error, the first 15 parent participants did not complete the portion of the survey dealing with prior mental health treatment, psychiatric diagnosis, and legal involvement so they were excluded from our final dataset. Four of the remaining participants did not complete the SCL-90-R used to compute our main outcome so they were also excluded. Analyses were conducted to determine whether participants included in our final dataset (N = 144) differed on key demographic variables (age, race, and gender) from those excluded (n = 19). We found that families with female youth (compared to families with male youth) and parents who identified as non-White (compared to White) were more likely to be excluded. Next, of the remaining 144 participants, 6% were removed from the final model due to missing data. We examined the likelihood of participants being removed from the final model based on all participant characteristics. Parents who identified as non-White were more likely to be excluded than White parents, as were parents with a history of mental health treatment. No other variables were significantly associated with exclusion.
Results
A third of parents (35%) met criteria for clinically significant mental health symptoms (GSI of SCL-90 R greater than threshold). The 144 parents were mostly female (78%), predominately birth parents (87%), middle-aged (44 years), and non-Hispanic (84%). They identified their race as White (72%), African American or Black (9%), Asian (5%), Alaskan Native or American Indian (4%), “other” (10%), and 4% not selecting any category [total greater than 100% because 4% of sample selected multiple categories]. Almost half reported a yearly household income of $30,000 or less and one third indicated no advanced education beyond high school. Youth were majority male (61%) with a mean age of 15 years. They identified their race as White (71%), African American or Black (13%), Alaskan Native or American Indian (7%), Asian (5%), Native Hawaiian or Pacific Islander (1%), and “other” (17%) with 2% not selecting any category [total greater than 100% because 17% of adolescents selected multiple categories]. Adolescents were predominately non-Hispanic (74%).
Table 1 presents comparisons between socio-demographic variables and degree of court monitoring by parents' mental health symptoms (clinically versus non-clinically significant). As shown, parents with (versus without) clinically significant mental health symptoms tended to have lower income, lower educational attainment, and were less likely to have a co-caregiver present in the home. Parents with (versus without) clinically significant mental health symptoms were also more likely to have adolescents who were referred to the study from the “high monitoring” group (truancy or delinquency) than adolescents referred through other sources (e.g., intake or diversion). No significant differences by gender (parent or adolescent), age (parent or adolescent), ethnicity or race (parent), or number of children in the home were found between parents based on their mental health symptoms.
Table 1. Demographics by Parent Mental Health Status (N = 144a).
| Total % yes or M (SD) | Significant Mental Health Symptoms by GSIb | Test (χ2 or t) | ||
|---|---|---|---|---|
|
| ||||
| Yes (n = 50) (% agree or M[SD]) | No (n = 94) (% agree or M[SD]) | |||
| Parents | ||||
| Age | 43.58 (8.25) | 42.58 (8.92) | 44.13 (7.86) | .22 |
| Female | 77% | 80% | 77% | 1.52 |
| White (vs. other) | 69% | 68% | 71% | .11 |
| Hispanic | 16% | 22% | 13% | 1.91 |
| No education beyond high school | 37% | 46% | 33% | 2.48 |
| Low income | 43% | 62% | 34% | 10.55* |
| Absence of co-caregiver | 49% | 68% | 40% | 10.00* |
| Number of children in home | 2.15 (1.10) | 2.22 (1.22) | 2.11 (1.04) | -.57 |
| Adolescents | ||||
| Age | 15.15 (1.39) | 15.10 (1.45) | 15.18 (1.37) | .32 |
| Female | 38% | 47% | 33% | 2.36 |
| Other Factors | ||||
| High degree of court monitoring | 54% | 70% | 46% | 7.74* |
p < .05
N ranges from 142 to 144 due to missing data.
GSI = Global Severity Index from the Symptom Checklist-90-Revised.
Table 2 presents comparisons between mental health and legal involvement indicators by parents' presence of significant mental health symptoms. Parents with clinically significant mental health symptoms, compared to those without, were more likely to have a history of a psychiatric diagnosis and mental health treatment, though differences were not found for substance use treatment. Parents with clinically significant mental health symptoms also reported higher levels of parenting stress and were more likely to have an arrest history, but not a history of incarceration, relative to those without. Parents with significant mental health symptoms also more frequently had adolescents with significant internalizing problems (as reported by parents and adolescents) and total problems (parent report only). Adolescent externalizing problems were not associated with parent mental health status.
Table 2. Mental Health and Legal Involvement by Parent Mental Health Status (N = 143a).
| Total % yes or M (SD) | Significant Mental Health Symptoms by GSIb | Test (χ2 or t) | ||
|---|---|---|---|---|
|
| ||||
| Yes (n = 49) (% agree or M[SD]) | No (n = 94) (% agree or M[SD]) | |||
| Parent Mental Health | ||||
| Psychiatric diagnosis | 29% | 52% | 19% | 16.26* |
| Mental health treatment | 35% | 54% | 25% | 11.94* |
| Substance use treatment | 10% | 12% | 8% | .54 |
| Parenting stress | 2.45 (.67) | 2.84 (.61) | 2.22 (.58) | -6.54* |
| Parent Legal Involvement | ||||
| Ever been arrested | 21% | 32% | 15% | 5.48* |
| Ever been incarcerated | 4% | 6% | 3% | .60 |
| Adolescent Mental Health (Parent Report) | ||||
| Internalizing problems | 27% | 47% | 23% | 9.56* |
| Externalizing problems | 33% | 39% | 34% | .38 |
| Total problems | 29% | 49% | 26% | 9.01* |
| Adolescent Mental Health (Adolescent Report) | ||||
| Internalizing problems | 10% | 23% | 9% | 6.06* |
| Externalizing problems | 17% | 19% | 19% | .00 |
| Total problems | 13% | 21% | 14% | 1.34 |
p < .05
N ranges from 134 to 143 due to missing data.
GSI = Global Severity Index from the Symptom Checklist-90-Revised.
Correlations among factors with significant bivariate associations with parental mental health symptom status were examined prior to conducting the logistic regression (see Table 3). To decrease the potential of multicollinearity and to increase the explanatory power of the predictive domains, if multiple variables in a domain (e.g. parent or adolescent mental health) had moderate to high correlations then the variable with strongest correlation was included in the final model. As prior mental health treatment was significantly correlated with psychiatric diagnosis and with prior arrest, it was included in the logistic regression. Adolescent total problems (by parent report) was the variable most strongly correlated with internalizing problems (by parent and adolescent report), so was included in the regression. Absence of a co-caregiver had a significant association with low income (r = .37). Thus, only income was selected for inclusion. We also included parenting stress and degree of court monitoring in the model as both variables were pertinent to study hypotheses and associated with parental mental health status.
Table 3. Correlations Among Factors Associated with Significant Mental Health Symptoms of Parents (N = 142a).
| Parent Factors | 1 | 2 | 3 |
|---|---|---|---|
| 1. Psychiatric diagnosis | |||
| 2. Mental health treatment | .59* | ||
| 3. Ever been arrested | .10 | .12 | |
|
| |||
| Adolescent Mental Healthb | 1 | 2 | |
|
| |||
| 1. Internalizing problems (P) | |||
| 2. Internalizing problems (A) | .45* | ||
| 3. Total problems (P) | .53* | .17* | |
p < .05
N ranges from 134 to 142 due to missing data.
Based on parent (P) or adolescent (A) report
Results of the multiple logistic regression are presented in Table 4. Overall, the model including all predictors and significant parent mental health symptoms as the outcome was significant (χ2 = 66.11, df = 6, p < .01). Two variables, low income and greater parenting stress, remained significantly associated with parental mental health symptoms. Adolescent mental health (total problems), degree of court monitoring (high vs. low), parent mental health treatment, and parental arrest history were not significantly associated with mental health status in the regression.
Table 4. Multiple Logistic Regression of Associations with Significant Mental Health Symptoms of Parents (N = 135).
| Adjusted ORs | 95% CIs | Wald | |
|---|---|---|---|
| Demographic Factors | |||
| Low income | 7.01 | 2.19 – 22.41 | 10.79 |
| Parent Mental Health | |||
| Mental health treatment | 2.05 | .78 – 5.36 | 2.14 |
| Parenting stress | 14.39 | 4.79 – 43.62 | 22.22 |
| Parent Legal Involvement | |||
| Ever been arrested | 2.00 | .63 – 6.33 | 1.41 |
| Adolescent Mental Health | |||
| Total problems (parent report) | 1.34 | .47 - 3.80 | .10 |
| Other Factors | |||
| High degree of court monitoring | 2.46 | .88 – 6.84 | 2.95 |
Note: Confidence intervals that do not contain zero are significant (p < .05).
Discussion
This study of adolescents referred from Juvenile Courts for mental health treatment found that a third of the parents had mental health symptoms of potential clinical significance. This rate is similar to that found among parents of youth in psychiatric care (Hadley, et al., 2015). Though a few studies have documented rates of mental health problems among parents of court-involved youth as a whole (Barylnik, 2003; Dembo et al., 2000; Lederman et al., 2004), this study examined this issue in a sample of court-involved youth referred for mental health treatment. These findings suggest that when the courts identify youth with significant emotional and behavioral problems, they may also be capturing a significant subset of parents with their own mental health difficulties and heightened parenting stress. Unfortunately, referral of an adolescent for mental health treatment may not result in parents receiving their own mental health treatment when indicated, or the needed parenting support to achieve optimal outcomes for their child. Family therapy may be useful in improving family communication and parental monitoring, but is not likely to address the specific psychiatric needs of the parent. Without a reduction in their distress and symptoms, parents are less likely to be able to assist in promoting their adolescent's healthier behavior. Without their own support and treatment, parents may also be unable to fully comply with all court orders, further increasing the risk for their child's recidivism and mental health deterioration.
Bivariate analyses reveal the complex associations between parents' current significant mental health symptoms, their prior mental health concerns, the mental health concerns of their adolescents (particularly internalizing problems), and legal involvement of both parents and youth (e.g. arrest history, court monitoring). Parents certainly may experience stress due to their child's legal and emotional needs. However, because parents with significant mental symptoms report prior mental health treatment and diagnoses, their current symptoms are perhaps not simply reactions to their adolescent's difficulties. Parents may require support and treatment independent from that of their youth. The association between parental symptoms and greater legal involvement of parent and child is a cogent reminder of the intergenerational pattern of behavioral problems. Such patterns are thought to be multifactorial and due to family genetics, modeling of behavior, trauma, and environmental factors (Barylnik, 2003; Dembo, Wothke, Schmeidler, & Brown, 1992). Whatever the causes of this intergenerational behavioral pattern, a parent's history of legal difficulties is a likely to color their reaction to the adolescent's behavior and monitoring by the Court. Thus, careful assessment of the parent's previous mental health and legal history may be warranted to fully inform the most appropriate course and approach to an adolescent's mental health treatment.
Notably, after accounting for parents' prior mental health and arrest history, adolescents' mental health symptoms, and degree of court monitoring, in a multivariate logistic regression predicting current mental health of parents, only lower income and parenting stress remained significant. It is possible that parents who are vulnerable due to prior mental health and legal challenges and currently have fewer resources (e.g. less income, no co-parent), may be less capable of meeting the demands associated with having a child involved in the court. These factors could result in greater parenting stress, which in turn could increase their own psychological distress and associated mental health symptoms. These data suggest that court-involved families with parent and child mental health needs may benefit from holistic care that considers economic and practical support for families, in addition to mental health treatment for the adolescent and parent. Policies that promote affordable health care will be a significant benefit for those distressed, underserved, and under resourced families.
Interestingly, although parents with significant mental health symptoms were likely to have adolescents with internalizing symptoms, their adolescents were not more likely to have externalizing symptoms. Because of the frequent co-occurrence of internalizing and externalizing symptoms and the intergenerational pattern in families, we anticipated that youth would have more symptoms of both types. The study's finding could be explained by the youth's involvement with the court. Adolescents with behavioral (i.e. externalizing) problems are more likely to have legal involvement than those with emotional (i.e. internalizing) symptoms, potentially resulting in relatively less variability in externalizing symptoms among court-involved youth. The finding that adolescents of parents with (versus without) significant mental health symptoms had higher rates of internalizing symptoms is significant and consistent with another study that found that a high proportion of court-involved youth with internalizing symptoms (Tolou-Shams et al., 2014). Emotional difficulties are likely to be less apparent than disruptive behavior and could be overlooked in a setting, such as the court, that is focused on outward behavior. Thus it is important to closely assess for and refer court-involved youth internalizing symptoms for mental health treatment, given the negative impact on both adolescent and parental health.
Limitations
The interpretation of the study findings must be considered in light of the project's limitations. The study is limited to youth referred from the Juvenile Courts in two states (and sample size prohibited analyses of potential differences between states) and so the results may not be generalizable to other regions of the U.S. Also, adolescents were referred for mental health treatment, so the patterns observed here might not be similar to patterns in all court-involved youth and their families. In addition, the data was self-report and susceptible to bias, although standard, reliable scales were self-administered by computer with audio to reduce desirability bias and problems with literacy. Lastly, these data are cross-sectional, so no inferences can be drawn as to causality. The associations suggested by this study will need to be confirmed with longitudinal data.
Conclusions
This study indicates that among youth identified by the court as in need of mental health treatment, parents also will frequently have significant mental health symptoms and parenting stress. These symptoms may not be observed in the Court. Thus, parents may not receive the individual treatment and support needed to improve their functioning. Without such improvement, parents may not be able to assist in their child's treatment needs and help prevent recidivism. The strong association found between parent's mental health, parenting stress, their youth's mental health, and resource limitations (low income, lack of co-parents) emphasizes the importance of a holistic approach to providing treatment and practical support for all members of these most at-risk families.
Acknowledgments
Funding: The study was funded by the National Institutes of Health (grant R01 MH087520); The National Institute of Mental Health (grant T32 MH078788); The Lifespan Tufts Brown Center for AIDS Research (P30 AI 042853)
Funding: Research supported by National Institutes of Health grant R01 MH087520 (PI: Brown); National Institute of Mental Health grant T32 MH078788 (PI: Brown); Lifespan Tufts Brown Center for AIDS Research P30 AI 042853 (PI: Cu-Uvin)
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Compliance with Ethical Standards: Ethical approval: “All procedures performed in studies involving human participants were in accordance with the ethical standards of Rhode Island Hospital and George Mason University IRBs, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Author Contributions: LKB: designed and executed the study, assisted with data analyses, and wrote the paper. NT: analyzed the data and wrote the results. MTS and CES: collaborated with the study design and implementation, and contributed to writing and editing the study. MGH: wrote the methods, wrote part of the introduction, and collaborated in the writing and editing of the final manuscript. LC: wrote part of the introduction, collaborated in the writing and editing of the final manuscript.
Contributor Information
Nicholas Tarantino, Department of Psychiatry, Rhode Island Hospital, Providence, RI.
Marina Tolou-Shams, University of California San Francisco, San Francisco, CA.
Christianne Esposito-Smythers, George Mason University, Fairfax, VA.
Meredith G. Healy, Department of Psychiatry, Rhode Island Hospital, Providence, RI
Lacey Craker, Department of Psychiatry, Rhode Island Hospital, Providence, RI.
References
- Achenbach TM. Youth self-report. Burlington: University of Vermont, Research Center for Children, Youth, and Families; 1995. [Google Scholar]
- Achenbach TM. Child behavior checklist for ages 6 to 18. Burlington: University of Vermont Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Achenbach TM, Dumenci L, Rescorla LA. Ten-year comparisons of problems and competencies for national samples of youth: self, parent, and teacher reports. Journal of Emotional and Behavioral Disorders. 2002;10:194–203. [Google Scholar]
- Anderson LS. Predictors of parenting stress in a diverse sample of parents and early adolescents in high-risk communities. Nursing Research. 2008;57:340–350. doi: 10.1097/01.NNR.0000313502.92227.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Messer SC, Stangl D, Farmer EMZ, Costello EJ, Burns BJ. Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health. 1998;88:75–80. doi: 10.2105/ajph.88.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barylnik J. Psychopathology, psychosocial characteristics and family environment in juvenile delinquents. German Journal of Psychiatry. 2003;6:30–32. [Google Scholar]
- Brown LK, Whiteley L, Harper GW, Nichols S, Nieves A The ATN 086 Protocol Team for the Adolescent Medicine Trials Network for HIV/AIDS Interventions. Psychological symptoms among 2032 youth living with HIV: a multisite study. AIDS Patient Care and STDs. 2015;29:212–219. doi: 10.1089/apc.2014.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Mulvey EP, Schubert CA. Prevalence of mental health problems and service use among first-time juvenile offenders. Journal of Child and Family Studies. 2015;24:3774–3781. doi: 10.1007/s10826-015-0185-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns BJ, Costello EJ, Angold A, Tweed D, Stangl D, Farmer EM, Erkanli A. Children's mental health service use across service sectors. Health Affairs. 1995;14:147–159. doi: 10.1377/hlthaff.14.3.147. [DOI] [PubMed] [Google Scholar]
- Carswell K, Maughan B, Davis H, Davenport F, Goddard N. The psychosocial needs of young offenders and adolescents from an inner city area. Journal of Adolescence. 2004;27:415–428. doi: 10.1016/j.adolescence.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Cocozza JJ, Skowyra KR. Youth with mental health disorders: issues and emerging responses. Juvenile Justice. 2000;7:3–13. [Google Scholar]
- Cocozza JJ, Veysey BM, Chapin DA, Dembo R, Walters W, Farina S. Diversion from the juvenile justice system: the Miami-Dade juvenile assessment center post-arrest diversion program. Substance Use & Misuse. 2005;40:935–951. doi: 10.1081/ja-200058853. [DOI] [PubMed] [Google Scholar]
- Dembo R, Seeberger W, Shemwell M, Klein L, Rollie M, Pacheco K, et al. Wothke W. Psychosocial functioning among juvenile offenders 12 months after family empowerment intervention. Journal of Offender Rehabilitation. 2000;32:1–56. [Google Scholar]
- Dembo R, Wothke W, Schmeidler J, Brown CH. The role of family factors, physical abuse and sexual victimization experiences in high-risk youths' alcohol and other drug use and delinquency: a longitudinal model. Violence and Victims. 1992;7:245–266. [PubMed] [Google Scholar]
- Derogatis L. Symptom Checklist-90-Revised (SCL-90-R) Pearson; 1975. [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An Introductory Report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Derogatis LR, Unger R. Symptom Checklist-90-Revised. Corsini Encyclopedia of Psychology. 2010:1–2. [Google Scholar]
- Duchovic CA, Gerkensmeyer JE, Wu J. Factors associated with parental distress. Journal of Child and Adolescent Psychiatric Nursing. 2009;22:40–48. doi: 10.1111/j.1744-6171.2008.00168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra L, Campbell L, Westen D. Quantifying clinical judgment in the assessment of adolescent psychopathology: reliability, validity, and factor structure of the child behavior checklist for clinician report. Journal of Clinical Psychology. 2004;60:65–85. doi: 10.1002/jclp.10234. [DOI] [PubMed] [Google Scholar]
- Hadley W, Barker DH, Brown LK, Almy B, Donenberg G, DiClemente RJ Project STYLE Study Group. The moderating role of parental psychopathology on response to a family-based HIV prevention intervention among youth in psychiatric treatment. Journal of Family Studies. 2015;21:178–194. [Google Scholar]
- Hazen AL, Hough RL, Landsverk JA, Wood PA. Use of mental health services by youths in public sectors of care. Mental Health Services Research. 2004;6:213–226. doi: 10.1023/b:mhsr.0000044747.54525.36. [DOI] [PubMed] [Google Scholar]
- Hiller ML, Saum CA. Juvenile drug courts, juvenile mental health courts, and teen courts. In: Roberts AR, Church WT, Springer DW, editors. Juvenile justice source book: Past, present and future. 2nd. New York, NY: Oxford University Press; 2014. [Google Scholar]
- Hockenberry S, Puzzanchera C. Juvenile Court Statistics 2013. Pittsburgh, PA: National Center for Juvenile Justice; 2015. [Google Scholar]
- Huey SJ, Jr, Henggeler SW, Brondino MJ, Pickrel SG. Mechanisms of change in multisystemic therapy: reducing delinquent behavior through therapist adherence and improved family and peer functioning. Journal of Counseling and Clinical Psychology. 2000;68:451–467. [PubMed] [Google Scholar]
- Ivanova MY, Achenbach TM, Dumenci L, Bilenberg N, Broberg AG, Döpfner M, et al. Verhulst FC. The generalizability of the youth self-report syndrome structure in 23 societies. Journal of Counseling and Clinical Psychology. 2007;75:729–738. doi: 10.1037/0022-006X.75.5.729. [DOI] [PubMed] [Google Scholar]
- Kaslow NJ, Deering CG, Racusin GR. Depressed children and their families. Clinical Psychology Review. 1994;14:39–59. [Google Scholar]
- Kim HK, Viner-Brown SL, Garcia J. Children's mental health and family functioning in Rhode Island. Pediatrics. 2007;119:S22–S28. doi: 10.1542/peds.2006-2089E. [DOI] [PubMed] [Google Scholar]
- Kutcher S, Marton P. Affective disorders in first-degree relatives of adolescent onset bipolars, unipolars, and normal controls. Journal of the American Academy of Child & Adolescent Psychiatry. 1991;30:75–78. doi: 10.1097/00004583-199101000-00011. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Piacentini JC, McBurnett K, Stone P, Hartdaghn S, Hynd G. Psychopathology in the parents of children with conduct disorder and hyperactivity. Journal of the American Academy of Child & Adolescent Psychiatry. 1988;27:163–170. doi: 10.1097/00004583-198803000-00005. [DOI] [PubMed] [Google Scholar]
- Lam PK, Naar-King S, Wright K. Social support and disclosure as predictors of mental health in HIV –positive youth. AIDS Patient Care. 2007;21:20–29. doi: 10.1089/apc.2006.005. [DOI] [PubMed] [Google Scholar]
- Lederman CS, Dakof GA, Larrea MA, Li H. Characteristics of adolescent females in juvenile detention. International Journal of Law and Psychiatry. 2004;27:321–337. doi: 10.1016/j.ijlp.2004.03.009. [DOI] [PubMed] [Google Scholar]
- Livingston R, Nugent H, Rader L, Smith GR. Family histories of depressed and severely anxious children. The American journal of psychiatry. 1985;142:1497–1499. doi: 10.1176/ajp.142.12.1497. [DOI] [PubMed] [Google Scholar]
- Maschi T, Hatcher SS, Scwalbe CS, Rosato NS. Mapping the social service pathways of youth to and through the juvenile justice system: A comprehensive review. Children and Youth Services Review. 2008;30:1376–1385. [Google Scholar]
- Mitchell J, McCauley E, Burke P, Calderon R, Schloredt K. Psychopathology in parents of depressed children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1989;28:352–357. doi: 10.1097/00004583-198905000-00008. [DOI] [PubMed] [Google Scholar]
- Mulvey EP. Highlights from pathways to desistance: a longitudinal study of serious adolescent offenders. Washington, DC: US Department of Justice, Office of Justice Programs, Office of Juvenile Justice and Delinquency Prevention; 2011. [Google Scholar]
- Preyde M, VanDonge C, Carter J, Lazure-Valconi K, White S, Ashbourne G. Parents of youth in intensive mental health treatment: associations between emotional and behavioral disorders and parental sense of competence. Child and Adolescent Social Work Journal. 2015;32:317–327. [Google Scholar]
- Puig-Antich J, Goetz D, Davies M, Kaplan T, Davies S, Ostrow L, et al. Ryan ND. A controlled family history study of prepubertal major depressive disorder. Archives of General Psychiatry. 1989;46:406–418. doi: 10.1001/archpsyc.1989.01810050020005. [DOI] [PubMed] [Google Scholar]
- Rosenblatt JA, Rosenblatt A, Biggs EE. Criminal behavior and emotional disorder: comparing youth served by the mental health and juvenile justice systems. The Journal of Behavioral Health Services & Research. 2000;27:227–237. doi: 10.1007/BF02287315. [DOI] [PubMed] [Google Scholar]
- Roustit C, Campoy E, Chaix B, Chauvin P. Exploring mediating factors in the association between parental psychological distress and psychosocial maladjustment in adolescence. European Child and Adolescent Psychiatry. 2010;19:597–604. doi: 10.1007/s00787-010-0094-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwalbe CS, Gearing RE, MacKenzie MJ, Brewer KB, Ibrahim R. A meta-analysis of experimental studies of diversion programs for juvenile offenders. Clinical Psychology Review. 2012;32:26–33. doi: 10.1016/j.cpr.2011.10.002. [DOI] [PubMed] [Google Scholar]
- Sheras P, Abidin R. Psychological Assessment Resources. 1998. Stress Index for Parents of Adolescents (SIPA) [Google Scholar]
- Skowyra KR, Cocozza JJ. Blueprint for change: A comprehensive model for the identification and treatment of youth with mental health needs in contact with the juvenile justice system. Delmar, NY: National Center for Mental Health and Juvenile Justice and Policy Research Associates; 2007. [Google Scholar]
- Tolou-Shams M, Rizzo CJ, Conrad SM, Johnson S, Oliveira C, Brown LK. Predictors of detention among juveniles referred for a court clinic forensic evaluation. Journal of the American Academy of Psychiatry and the Law Online. 2014;42:56–65. [PMC free article] [PubMed] [Google Scholar]
- Vermeiren R, Jespers I, Moffitt T. Mental health problems in juvenile justice populations. Child and Adolescent Psychiatric Clinics of North America. 2006;15:333–351. doi: 10.1016/j.chc.2005.11.008. [DOI] [PubMed] [Google Scholar]
- Whitehead JT, Lab SP. Juvenile justice: An introduction. Cincinnati, OH: Anderson; Publication Co: 2001. [Google Scholar]
- Wills TA, Dishion TJ. Temperament and adolescent substance use: A transactional analysis of emerging self-control. Journal of Clinical Child and Adolescent Psychology. 2004;33:69–81. doi: 10.1207/S15374424JCCP3301_7. [DOI] [PubMed] [Google Scholar]
- Young DW, Dembo MS, Henderson CE. A national survey of substance abuse treatment for juvenile offenders. Journal of Substance Abuse Treatment. 2007;32:255–266. doi: 10.1016/j.jsat.2006.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]