Abstract
We aimed to determine the prevalence of drug and polydrug use in people living with HIV in Austria for the first time for which a two center cross-sectional study was performed. Participants were recruited from consecutive patients during their regularly scheduled visits. In total 438 participants were included in the analysis. For this study we used paper-pencil and online-based questionnaires. The prevalence of illicit drug use was 60.5%; with cannabis use at 31.5%, nitrates at 31.5%, sildenafil/tadalafil at 24% and cocaine at 14%, being the most used substances. Use of more than one substance (polydrug) in drug users was 69.4% or 42.0% in the total study population. Younger age, male gender, and living in an urban area were associated with drug use. Moreover, drug use during clubbing and sex, HIV therapy non-adherence and younger age were associated with polydrug use. Drug users reported condomless sex in 42.4% and performing sexual acts they would not do sober in 44.1%. Results indicate a high prevalence of illicit drug use in PLWHIV in Austria. New research focusing on illicit drug use in PLWHIV should focus on the use of substances during sex and surrounding practices.
Introduction
With the development of antiretroviral therapy (ART) the mortality and morbidity associated with HIV/AIDS has decreased, even as HIV still poses a major global public health concern with 1.8 million newly diagnosed cases in 20161. This reduction in mortality was brought about by newer antiretroviral therapy with improved tolerability and led to HIV being considered a chronic illness2. This paradigm shift calls for a more tailored approach to people living with HIV (PLWHIV) as emerging issues such as healthy aging and non-AIDS conditions are gathering more importance2,3. Moreover, issues of addiction seem to be especially problematic within PLWHIV as multiple studies show a two to three fold higher prevalence of tobacco smoking in comparison to the general population, which is often connected to use of alcohol and illegal drugs4–7.
Additional to tobacco and alcohol use, illegal drug use is a cause of major harm for societies and individuals8. According to the European Drug Report 2017, 26.3% of the European population tried cannabis at least once, with additional estimates of 5.2% for cocaine, 4.2% for 3,4-Methylenedioxymethamphetamine (MDMA) and 3.8% for amphetamines, with injecting drug use showing a decline9. The importance of drug use and its connection to HIV is therefore shifting from the “traditional” issues of intravenous drug users and the associated HIV transmission towards illicit drug use that, although underinvestigated, seem to be of high prevalence in certain “key populations” such as men who have sex with men (MSM). The EMIS-Study in Europe showed high prevalence of drugs associated with “chemsex” (a term describing sexual relations under the influence of various, mostly psychoactive substances) including amyl nitrates (“poppers”) and cannabis10,11. In terms of HIV and sexually transmitted infections (STIs), illicit drug use and chemsex may be linked to an increase in incidence as studies show that drug use is associated with an increase in condomless sex, including among HIV-serodiscordant partners10,12–14. More importantly, studies suggest that MSM who are living with HIV are more likely to use almost all types of illicit drugs in comparison to HIV negative MSM15,16. An even more considerable problem among MSM living with HIV is the high prevalence of polydrug use (use of more than one substance within a time period), which was also associated with condomless sex with multiple new partners11,17,18. Furthermore, results from the ASTRA study showed an association with increasing polydrug use and increasing frequency of condomless sex19. Additionally, methamphetamine use and to a lesser extent use of sildenafil have been shown to be associated with increased high-risk sexual behavior in both MSM and heterosexual samples17.
However, problems of illicit drug use go beyond the increased risk for condomless sex and may have relevant clinical consequences for PLWHIV who are on ART due to adherence problems. A particularly high adherence level is necessary to avoid resistance against antiretrovirals and keep the effectiveness of ART in desired levels20. Furthermore, illicit drug use has been found to be a factor of non-adherence by causing temporary cognitive impairment or by drug-drug interaction causing potentially toxic side effects, on the other hand also limiting the effectiveness due to shared metabolic pathways21,22. Illicit drug use, especially cocaine, amphetamines, methamphetamines, heroin and morphine have been also known to increase the HIV replication and cause epigenetic changes in brain tissue, which can further have a synergistic effect and accelerates neural injury and cognitive impairment23–25.
Most studies dealing with the issues of illicit drug use in PLWHIV are solely focused on the MSM population. A recent review on the recreational drug use in PLWHIV in Europe included 13 studies, however only two studies investigated PLWHIV in general (without any additional factors such as specific comorbidities or use of the same medication)26. The same review noted high use of recreational drugs in Europe with even higher prevalence in PLWHIV as well as more use of new drugs (such as ketamine, mephedrone, gamma-hydroxybutyrate (GHB), etc.) and those associated with sexual practices.
In terms of prevalence of drug use in the general adult population, Austria is in the mid to lower part of the EU range, with use in 2015 being reported for cannabis at 6.4%, 0.4% for cocaine, MDMA and amphetamines respectively9. Long term analysis shows a slight increase in cannabis use, however in general the use of illegal drugs in Austria is concentrated among young adults (aged 15–34) with males reporting higher prevalence9. Prevalence of illicit drug use among PLWHIV in Austria has not been investigated so far. The primary aim of this study was to describe the prevalence of illicit drug and polydrug use in a sample of adult PLWHIV and their associations with socio-demographic, HIV related and lifestyle factors.
Results
A total of 683 patients matched inclusion criteria and 452 (66.1%) agreed to participate. Response rate varied between the centers with center “A” reaching 72.6% (318 approached and 231 agreed) and “B” reaching 60.5% (365 envelopes given and 221 filled out). Further 14 questionnaires needed to be eliminated from analysis as nine filled out less than 50% of the needed questions, four indicated they were not HIV positive and one indicated being 17 years old, leaving 438 participants available for analysis. Significant differences were found between study centers, where center “A” had older participants (45.80 (12.03) v 41.24 (9.66); p < 0.001) with more years passed since HIV diagnosis (13.81 (8.35) v 9.89 (7.40); p < 0.001). In center “B” there were significantly more participants who used drugs (71.1% v 50.0%; p < 0.001) as well as polydrug users (74.2% v 62.7%; p = 0.046).
Our sample consisted of predominantly male, self-identifying homosexual men of high educational level living in urban areas. The sample was stratified by drug use over the past 6 months, where 39.5% (173) participants were classified as non-drug users and 60.5% (265) as drug users. There were significant differences between non-drug and drug users observed in age, sex, sexual orientation, place of residence, mean duration of HIV status and mean duration of ART. Participants classified as drug users were further categorized as monodrug (30.6%; 81) or polydrug (69.4%; 184) users based on the number of drugs they indicated taking within the last 6 months. Significant differences were observed only in age and duration of HIV status (Table 1).
Table 1.
Sociodemographic and HIV related characteristics of the study population stratified by drug and polydruga use.
| Variable | Total (N = 438) | Non drug users (n = 173) | Drug users (n = 265) | p | Monodrug users (n = 81) | Polydrug users (n = 184) | p |
|---|---|---|---|---|---|---|---|
| Mean age in years (SD) | 43.53 (11.14) | 46.87 (11.70) | 41.35 (10.21) | <0.001 | 45.05 (11.40) | 39.72 (9.20) | <0.001 |
| Gender | <0.001 | 0.122 | |||||
| Male % (n) | 86.8 (380) | 79.8 (138) | 91.3 (242) | 87.7 (71) | 92.9 (171) | ||
| Female % (n) | 12.3 (54) | 20.2 (35) | 7.2 (19) | 11.1 (9) | 5.4 (10) | ||
| Sexual Orientation | 0.001 | 0.785 | |||||
| Heterosexual % (n) | 27.4 (120) | 37.0 (64) | 21.1 (56) | 23.5 (19) | 20.1 (37) | ||
| Bisexual % (n) | 10.3 (45) | 8.7 (15) | 11.3 (30) | 9.9 (8) | 12.0 (22) | ||
| Homosexual % (n) | 62.3 (273) | 54.3 (94) | 67.5 (179) | 66.7 (54) | 67.9 (125) | ||
| Current relationship | 0.143 | 0.064 | |||||
| Yes % (n) | 53.4 (234) | 57.8 (100) | 50.6 (134) | 40.7 (33) | 53.3 (98) | ||
| No % (n) | 46.6 (204) | 42.2 (73) | 49.4 (131) | 59.3 (48) | 46.7 (86) | ||
| Country of birth | 0.662 | 0.133 | |||||
| Austria % (n) | 83.1 (364) | 83.8 (145) | 82.6 (219) | 86.4 (70) | 81.0 (149) | ||
| EU member state % (n) | 8.0 (35) | 7.5 (13) | 8.3 (22) | 2.5 (2) | 10.9 (20) | ||
| Non EU state % (n) | 5.3 (23) | 4.0 (7) | 6.0 (16) | 7.4 (6) | 5.4 (10) | ||
| Outside of Europe % (n) | 3.7 (16) | 4.6 (8) | 3.0 (8) | 3.7 (3) | 2.7 (5) | ||
| Residence | 0.032 | 0.427 | |||||
| Community up to 5000 residents % (n) | 9.1 (40) | 13.3 (23) | 6.4 (17) | 9.9 (8) | 4.9 (9) | ||
| Town up to 100000 residents % (n) | 6.6 (29) | 8.7 (15) | 5.3 (14) | 4.9 (4) | 5.4 (10) | ||
| Large town up to million residents % (n) | 6.8 (30) | 6.9 (12) | 6.8 (18) | 4.9 (4) | 7.6 (14) | ||
| City with more than a million residents % (n) | 77.4 (339) | 71.1 (123) | 81.5 (216) | 80.2 (65) | 82.1 (151) | ||
| Highest level of education | 0.961 | 0.061 | |||||
| Primary education % (n) | 8.2 (36) | 7.5 (13) | 8.7 (23) | 9.9 (8) | 8.2 (15) | ||
| Vocational education % (n) | 35.6 (156) | 37.6 (65) | 34.3 (91) | 44.4 (36) | 29.9 (55) | ||
| Secondary education % (n) | 22.4 (98) | 22.0 (38) | 22.6 (60) | 22.2 (18) | 22.8 (42) | ||
| Tertiary education % (n) | 31.7 (139) | 31.2 (54) | 32.1 (85) | 23.5 (19) | 35.9 (66) | ||
| No formal education % (n) | 2.1 (9) | 1.7 (3) | 2.3 (6) | 0 | 3.3 (6) | ||
| Employment status | 0.307 | 0.711 | |||||
| Full time % (n) | 56.4 (247) | 58.4 (101) | 55.1 (146) | 55.6 (45) | 54.9 (101) | ||
| Part time % (n) | 16.7 (73) | 13.3 (23) | 18.9 (50) | 16.0 (13) | 20.1 (37) | ||
| Unemployed % (n) | 26.9 (118) | 28.3 (49) | 26.0 (69) | 28.4 (23) | 25.0 (46) | ||
| HIV related variables | |||||||
| Mode of HIV transmission | 0.086 | 0.822 | |||||
| Sexual contact % (n) | 78.8 (345) | 74.6 (129) | 81.5 (216) | 80.2 (65) | 82.1 (151) | ||
| Intravenous drug use % (n) | 5.7 (25) | 4.6 (8) | 6.4 (17) | 8.6 (7) | 5.4 (10) | ||
| Blood transfusion % (n) | 1.8 (8) | 2.3 (4) | 1.5 (4) | 1.2 (1) | 1.6 (3) | ||
| Not clear % (n) | 13.5 (59) | 18.5 (32) | 10.2 (27) | 9.9 (8) | 10.3 (19) | ||
| Time passed since HIV diagnosis in years (SD) | 11.85 (8.13) | 13.67 (8.44) | 10.66 (7.70) | <0.001 | 12.26 (8.41) | 9.97 (7.29) | 0.038 |
| Current CD4+ count known | 0.333 | 0.076 | |||||
| Yes % (n) | 79.7 (349) | 82.1 (142) | 78.1 (207) | 85.2 (69) | 75.0 (138) | ||
| No % (n) | 20.3 (89) | 17.9 (31) | 21.9 (58) | 14.8 (12) | 25.0 (46) | ||
| Currently on ART | 0.253 | 0.670 | |||||
| Yes % (n) | 431 (98.4) | 99.4 (172) | 97.7 (259) | 98.8 (80) | 97.3 (179) | ||
| No % (n) | 7 (1.6) | 0.6 (1) | 2.3 (6) | 1.2 (1) | 2.7 (5) | ||
| Mean duration of therapy in years (SD) | 9.84 (6.98) | 11.15 (7.23) | 8.96 (6.67) | 0.002 | 9.77 (7.25) | 8.59 (6.38) | 0.194 |
| Number of different ART | 0.701 | 0.607 | |||||
| One % (n) | 57.1 (250) | 59.3 (102) | 57.1 (148) | 57.5 (46) | 57.0 (102) | ||
| Two % (n) | 31.3 (137) | 32.0 (55) | 31.7 (82) | 28.8 (23) | 33.0 (59) | ||
| More than 3% (n) | 10.0 (44) | 8.7 (15) | 11.2 (29) | 13.8 (11) | 10.1 (18) | ||
| Antiretroviral class | |||||||
| Fusion inhibitors % (n) | 0.7 (3) | 0.6 (1) | 0.8 (2) | 1.000 | 0 | 1.1 (2) | 0.571 |
| Protease inhibitors % (n) | 13.0 (56) | 11.6 (20) | 13.9 (36) | 0.560 | 16.3 (13) | 12.8 (23) | 0.560 |
| Integrase inhibitors % (n) | 20.8 (91) | 21.5 (37) | 20.8 (54) | 0.904 | 20.0 (16) | 21.2 (38) | 0.870 |
| Reverse transcriptase inhibitors % (n) | 62.3 (273) | 62.8 (108) | 63.7 (165) | 0.919 | 60.0 (48) | 65.4 (117) | 0.485 |
| Fixed combinations (integrase and reverse transcriptase inhibitors) % (n) | 33.1 (145) | 33.1 (57) | 34.0 (88) | 0.917 | 37.5 (30) | 32.4 (58) | 0.478 |
Drug use
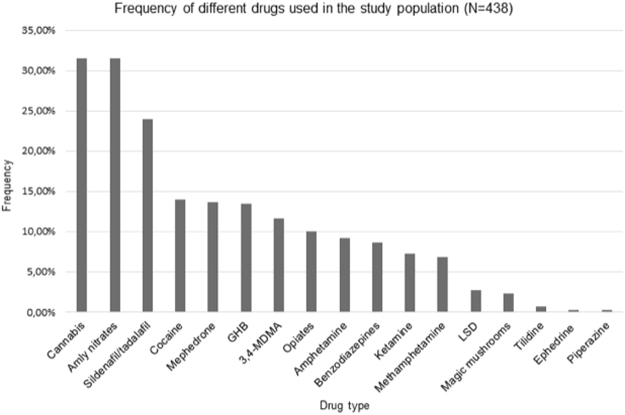
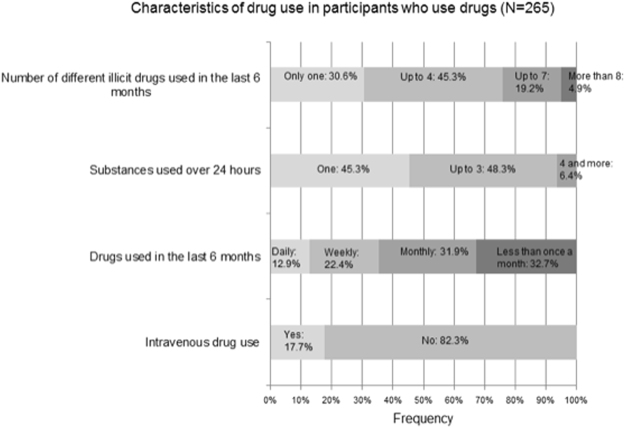
Participants classified as drug users mostly used up to 4 different substances in the past 6 months. Illicit drugs were used less frequently with most of the sample indicating use on a less than monthly and monthly basis. Most used drugs were cannabis and amyl nitrates (“poppers”) followed by sildenafil/tadalafil and cocaine, with the most frequent reason being “for more sexual stimulation”. Accordingly, most drugs were used at home or during sex. Information on drug use can be found in Table 2 and Figs 1 and 2.
Table 2.
Illicit drug use characteristic among participants that reported using drugs (N = 265).
| Variable | Result |
|---|---|
| Reasons for taking drugsa | |
| To feel happy and energetic % (n) | 36.2 (96) |
| To feel calm % (n) | 50.9 (135) |
| To have more fun % (n) | 45.7 (121) |
| For more sexual stimulation % (n) | 72.8 (193) |
| To forget about worries % (n) | 24.5 (65) |
| To feel more selfworth % (n) | 13.6 (36) |
| To feel more close to my friends % (n) | 19.6 (52) |
| Place of drug usea | |
| At home % (n) | 57.4 (151) |
| At private parties % (n) | 35.4 (93) |
| Clubbing % (n) | 15.8 (42) |
| During sex % (n) | 56.7 (149) |
| At work % (n) | 2.3 (6) |
| Other % (n) | 6.8 (18) |
| ART non-adherent % (n) | 21.2 (56) |
| Condomless sex % (n) | 42.4 (112) |
| Preforming sexual acts not doing sober % (n) | 44.1 (116) |
| Able to enjoy sex without drugs % (n) | 82.9 (218) |
| Informed physician about drug use % (n) | 44.9 (118) |
| Feel knowledgeable enough about drug use % (n) | 73.9 (195) |
aMultiple-choice question; ART = antiretroviral therapy.
Figure 1.
Frequency of different drugs used in the study population (N = 438). A multiple-choice question. Sildenafil/tadalafil and opiod use are based on reported use without a prescription. 3,4-MDMA = 3,4-Methylenedioxymethamphetamine; LSD = Lysergic acid diethylamide; GHB = gamma-Hydroxybutyric acid.
Figure 2.
Characteristics of illicit drug use among participants who use drugs (N = 265).
Three percent (9) of participants indicated experiencing side-effects of ART (mostly reported as nausea, vertigo and profuse sweating) consuming ART and drugs and 21.1% (32) said they adjust the dose of ART in preparation for taking drugs, with 49.8% (131) being aware of potential interactions between ART and drugs. Overall 66.7% (176) reported enjoying taking drugs and 73.9% (195) felt their knowledge on drugs was sufficient. Twenty three percent (62) of participants felt that drugs have a negative influence on their life. Not surprising, a significant difference was seen in the univariate analysis whereby polydrug users more frequently reported enjoying taking drugs (77.2% vs 42.5%; p < 0.001) but also more frequently indicated that drugs have a negative influence on their lives (27.7% vs 13.8%; p = 0.024). Polydrug users were also more often non-adherent to their prescribed ART regimens (28.8% vs 3.8%; p < 0.001). In terms of sexual behavior under the influence of drugs, polydrug users reported more condomless sex (51.6% vs 21.3%; p < 0.001) and doing sexual practices they would not do sober (51.4% vs 27.5%; p < 0.001).
Variables associated with illicit drug and polydrug use
According to the multivariate logistic regression analysis older age, female gender, uncertainty about HIV transmission mode, and residing in a smaller community up to 5000 residents were less associated with drug use (Table 3).
Table 3.
Characteristics associated with illicit drug use in the study population (N = 438).
| Variablea | OR | 95% CI | p |
|---|---|---|---|
| Age in years | 0.96 | 0.94–0.98 | <0.001 |
| Gender (Ref: male) | |||
| Female | 0.27 | 0.14–0.53 | <0.001 |
| HIV transmission (Ref: sexual contact) | |||
| IV drug use | 1.72 | 0.65–4.55 | 0.271 |
| Blood transfusion | 0.58 | 0.09–3.50 | 0.548 |
| Not clear | 0.45 | 0.24–0.84 | 0.013 |
| Place of residence (Ref: city with more than a million residents) | |||
| Community up to 5000 residents | 0.42 | 0.20–0.87 | 0.020 |
| Town up to a 100000 residents | 0.48 | 0.21–1.09 | 0.081 |
| Large town up to a million residents | 0.96 | 0.41–2.24 | 0.929 |
aVariables with the cut-off point of p < 0.2 in the univariate analysis were included in the model. During stepwise backwards elimination only those with the significance level of p < 0.05 were retained in the final model. Variables included in the first step were: age, sex, sexual orientation, relationship status, place of residence, mode of HIV transmission, time passed since HIV diagnosis, duration of HAART.
Older age was also significantly negatively associated with polydrug use, while drug use during clubbing, during sex and ART non-adherence were positively associated with polydrug use (Table 4).
Table 4.
Characteristics associated with polydrug use in study participants who use drugs (N = 265).
| Variablea | OR | 95% CI | p |
|---|---|---|---|
| Age in years | 0.97 | 0.94–0.99 | 0.030 |
| Highest finished education level | 1.36 | 0.99–1.89 | 0.062 |
| Country of birth (Ref: Austria) | |||
| EU member state | 2.87 | 0.59–13.78 | 0.189 |
| Non-Eu member state | 0.28 | 0.06–1.28 | 0.101 |
| Non European | 0.16 | 0.11–2.37 | 0.181 |
| Drug use at private parties (Ref: No) | |||
| Yes | 1.96 | 0.89–1.89 | 0.093 |
| Drug use during clubbing (Ref: No) | |||
| Yes | 6.24 | 1.32–29.52 | 0.021 |
| Drug use during sex (Ref: No) | |||
| Yes | 2.11 | 1.09–4.05 | 0.026 |
| ART Adherence (Ref: Adherent) | |||
| Non adherent | 8.09 | 2.19–29.87 | 0.002 |
aVariables with the cut-off point of p < 0.2 in the univariate analysis were included in the model. During stepwise backwards elimination only those with the significance level of p < 0.05 were retained in the final model. Variables included in the first step were: age, sex, current relationship, time passed since HIV diagnosis, duration of HAART, country of birth, highest finished education level, current CD4+ count known, drug use at home, drug use at private parties, drug use while clubbing, drug use during sex, condomless sex, preforming sexual acts not doing sober, awareness of potential interactions between drugs and HAART, drug non-adherence.
Discussion
Our study showed the prevalence of illicit drug use among PLWHIV who visit outpatient HIV treatment clinics in Austria to be at 60.5%. This result is threefold higher than the lifetime drug use prevalence in adults in Austria, which is reported at 20.2%, and almost ten times higher than the point prevalence (which was reported at 6.4%) in the general adult population in 20159. Due to differences in sample characteristics as well as investigated periods there is a great variability in reported prevalence between various studies investigating drug use in PLWHIV26. For instance Peretti-Watel et al. on a large sample of PLWHIV in France report prevalence of 28.6% over the last 12 months, while a recently published study on a Spanish PLWHIV population reports a prevalence level of 44.2% over the last 12 months27,28. High prevalence was also reported among AIDS patients29.
Illicit drug users in our study population were significantly younger and more often male. Older age and female gender were also found to be associated with less risk of drug use, whereby female participants were four times less likely to report illicit drug use, which was confirmed in similar studies19,27 (Table 3). One reason might be the overall lower prevalence of substance use in women, which may be linked to various cultural circumstances9,30–32. Furthermore, drug users lived more often in urban areas and in the multivariate model residence in a smaller community was associated with two times less drug use (Table 3). Reasons for this might be easier availability of illicit drugs in larger communities; however, data on this is inconsistent9,32–34. Additionally, participants who reported drug use had significantly shorter periods of using ART and living with a seropositive status, which might be explained by their younger age. We also observed an effect of not knowing the exact mode of HIV transmission. Differences in HIV transmission mode concerning illicit drug use have been seen in other studies27; however, there is no clear reasoning of this result in literature. One reason might be giving more socially desirable answers or lower educational level found in this group, which was reported to be associated with overall lower drug use35,36.
A potential reason for such an overall high prevalence might be due to our study sample, where more than 80% of male participants self-identified as bisexual or homosexual (Table 1). When looking into studies that measured prevalence only in HIV positive MSM, our results are still high but more similar to those findings11,18,19,35–37. The ASTRA study, one of the largest studies done on recreational drug use in this population reported a 51% prevalence of recreational drug use in the last 3 months, while Hammoud et al. reported illicit drug use in more than half of their participants in the last 6 months11,19. Similarly to our result, a US based study reported overall prevalence of 60% in the past 3 months36. However, even in MSM focused studies prevalence varies considerably with some studies reporting prevalence at around 20%35,38, while a study by Drumright et al. reported prevalence at 71.7%39.
In terms of most frequently used drugs; cannabis and nitrates (“poppers”) were reported as two most commonly used substances, followed by sildenafil/tadalafil and cocaine (Fig. 1). The most frequently used drug in the general adult population in Austria in 2015 was cannabis, however the reported prevalence is almost 6 times lower in comparison to our study population. Considerable differences were also found in other drugs where 2015 adult prevalence for cocaine, amphetamines and MDMA consumption was 0.4%, which is 29 times lower than in our findings9. In a recent Spanish study, Garin et al. similarly report cannabis use at 68.5%, sildenafil 28.3%, nitrates 31.5% and cocaine 45.5% among PLWHIV respectively27. Additionally, reported use of MDMA in drug users was the same in both our studies. Use of sildenafil and nitrates is contraindicated due to increasing cardiovascular effects40, however high prevalence of these substances is reported across studies, with some studies like ours reporting very high prevalence16,27,39,41. Drugs associated with “chemsex” and “slamming” (injecting drugs during or before sex); mephedrone, GHB, MDMA and ketamine were also considerably more prevalent in our study in comparison to others11,27 (Fig. 1). The prevalence of intravenous use at around 18% is also significantly more than in other studies (Fig. 2)19,27. This finding may also be due to a high number of MSM subpopulation in our study sample and as almost 3/4 of our participants indicated using illicit drugs for more sexual stimulation. Both “chemsex” and “slamming” have been identified as practices related to higher risk of condomless sex and HIV transmission in MSM10,19. In our study, participants who use illicit drugs noted engaging in condomless sex and in sexual acts they would not do sober in more than 40% (Table 2). Studies indicate that with having good adherence levels almost completely diminishes the possibility of HIV transmission, however there is still considerable risk of HIV transmission among people who are unaware that they are HIV positive or haven’t received therapy long enough to reach HIV suppression. These are the settings where practicing safe sex is still incredibly important42.
Using two or more substances during the last 6 months was classified as polydrug use and was found in our study at 42% in the total study population and 69.4% among drug using participants, which is considerably more than other studies19,27,36,39. Even though polydrug use is often noted as problematic in PLWHIV, the newest report from the European Monitoring Centre for Drugs and Drug Addiction states polydrug use as problematic in the general young adult population9. Differences between mono- and polydrug users were only found in terms of age, where polydrug users were significantly younger than monodrug users and had a shorter time span living with a seropositive status (Table 1). Condomless sex and preforming sexual acts one would not do sober were also significantly associated with polydrug consumption (Table 2). In contrast to other studies that reported an association between increased polydrug use with increased prevalence of condomless sex, or generally showed an association between high risk sexual behavior and illicit drug use16,19,27,38, we did not find such an association in our multivariate model. However, polydrug use was significantly negatively associated with older age, and positively associated with drug use during clubbing and during sex (Table 4).
Twenty one percent of our participants reported not being adherent to their prescribed ART regime when using or planning to use drugs (Table 2). Literature shows that adherence is not a stagnant mono-dimensional issue but a dynamic process influenced by many variables. This means that individuals show both times of high and also very low adherence depending on favorability of life circumstances43. A meta-analysis of studies on adherence in PLWHIV who use drugs showed an overall optimal adherence in 60% of participants (similar to PLWHIV who do not use drugs) but indicated that studies with a larger investigated time frame showed more variability in adherence than studies with a shorter time frame44. Active drug use was found to be associated with adherence problems in other studies as well where non-adherence was also found to be more prevalent in polydrug users, which in our study carried an 8 times higher risk for polydrug use in the multivariant model19,27,45–47. Reasons for this may be due to the disruptive influence of illicit drugs on the daily rhythm or due to neural damage that leads into cognitive problems as some illicit drugs cause neural damage and contribute to higher viral replication that causes additional tissue damage23–25,46. In terms of ART a particularly high adherence level of over 85% is necessary to achieve viral RNA suppression in patients receiving ART20. However, some studies indicated that even though illicit drug use is associated with adherence problems it does not necessarily bring clinical complications19,27. In terms of non-adherence and drug use in PLWHIV, most studies focus on unintentional non-adherence because of intoxication29. Interestingly, other studies showed purposeful discontinuation with prescribed therapy when planning to use illicit drugs out of fear of potential toxic side effects48. However, while potential side effects may possibly frequently occur, more evidence is still needed21. In contrast, our participants felt they were knowledgeable on issues concerning drug use and were aware of potential side effects. Nonetheless, one fifth were found to be non-adherent (Table 2), however, this might not lead to clinical manifestations as most of our participants who use drugs reported drug use on a monthly level, which might indicate relatively short bouts of non-adherence (Fig. 2). From a perspective of public health this might indicate that disease based campaigns aimed at increasing individual’s ability to protect themselves may not be effective. Rather campaigns ought to take into consideration the broader social context and help in strengthening and mobilizing community resources. Such approaches have been cited as having a positive role in changing harmful social and cultural norms49. This is of particular importance as hard drug users have higher odds of developing AIDS related conditions or dying even after controlling for adherence issues29,50.
Finally, study limitation should be addressed. Overrepresentation of male and MSM participants may prevent generalizability of our results, however our study populations is representative of the PLWHIV population in an extramural setting in Austria. Although the response rate was quite good, a selection bias might have occurred, with people taking illicit drugs being more likely to participate in the study compared to non-responders. Using self-reporting questionnaires may lead to reporting bias in terms of wanting to give more socially desirable answers, which even in light of this very high prevalence might still be underreported. Due to logistical issues we did not gather clinical information (CD4 cell counts, viral load etc.) which prohibits their correlation with drug and polydrug use. Additionally, having problems with remembering over the past 6 months may lead to some data distortion. Lastly, cross sectional study design does not allow causal relations.
In conclusion, prevalence of illicit drug use among PLWHIV in outpatient care in Austria is high, with polydrug use being especially commonplace which suggests a large, and until now, an unknown problem in Austria. The results of our study contribute to the growing literature that point to the emerging issues of substance abuse among the PLWHIV. Our results indicate that PLWHIV who use illicit drugs feel knowledgeable about HIV and drug use, which might indicate that public awareness campaigns aimed at increasing knowledge, might not be effective. In light of emerging sexual behaviors such as chemsex and slamming, public health effort should focus on community empowerment and mobilization interventions aimed at younger, urban and male HIV positive people. Further research should focus on identifying fundamental forces that are associated with polydrug use, as well as longitudinal studies that would allow for temporal and causal information.
Methods
Participants
Our study participants consisted of patients who visited their chosen HIV outpatient treatment clinic in Vienna, Austria between the 1st of December 2016 and 1st of June 2017. Patient recruitment was done in two centers; one being a hospital-based outpatient clinic and the other an outpatient group practice. In order to minimize potential selection bias, participants were chosen from consecutive patients that came for their regular visits to the outpatient clinic and were asked to participate if they matched the inclusion criteria (over 18 years old, serologically confirmed HIV infection) and were included once informed consent was given.
Methods
The study was designed as a multicenter cross-sectional study. Due to structural differences between centers, we employed two different ways of gathering data; a standard paper-pencil (in center “A”) and an online based platform (in center “B”). In center “A”, after the consultations with the physician the patients that matched the inclusion criteria were asked to participate in the study. They were explained the study aims and if agreed they were given the study questionnaire to fill out. For the purposes of the study, a room where patients could fill out the survey in privacy was allocated. The patients sealed the questionnaire in an envelope, which was deposited in a locked cabinet by the study team. A member of the study team was present and was able to help with any issues that might have risen during the filling out of the questionnaire. In center “B”, patients, following a consultation, were asked to participate and if agreed they were asked to choose a plain white envelope from a box. Inside the envelope was a letter from the study team with the link to the questionnaire together with a unique code that allowed access. For additional convenience, the questionnaire could have been accessed via smartphone or tablet for which we supplied a QR-code. After the code was used and the participant accessed the questionnaire, the code became invalid, which allowed response rate calculations and prevented multiple entries. The codes were computer generated and there was no way for the study team or the clinic staff to link the individual patients and their code. Also, only the questionnaire answers were saved on a secure server without any personal information. Throughout the online questionnaire, a hyperlink with an email address to the study team as well as a telephone number were available in order to answer any potential questions. After June 1st 2017, the online questionnaire was no longer active and the data containing only answers to the questionnaire were downloaded by the research team. The paper-pencil data were delivered in sealed envelopes and opened by the research team, who had no contact with patients at the study centers and could not link the individual patients to their respective questionnaires.
Questionnaire
A special questionnaire composed of 31 items divided in 3 parts was created for the purposes of the study. The questionnaire was a combination of single and multiple choice questions as well as open-end questions.
HIV-related questions: questions regarding HIV mode of transmission, CD4+ cell count, duration of HIV status as well as type of ART and years spent on therapy used were asked.
Questions on drug use: questions concerning types of drugs used, frequency of use, reasons of use, sexual behavior during drug use, personal feelings on drug use, problems when taking ART and drugs, adherence to ART medication, disclosure of drug use to their HIV physician etc. were asked. Participants were asked if they used drugs over the past 6 months and if yes which ones, following by a list of 17 substances that were also written under various slang names in order to improve understanding. Illicit drugs included in the study were: mephedrone, cannabis, methamphetamine, 3,4-Methylenedioxymethamphetamine (MDMA), ephedrine, heroin and other opiates, ketamine, cocaine, lysergic acid diethylamide (LSD), piperazine, amphetamine, benzodiazepines, magic mushrooms, amyl nitrates, tilidine, sildenafil/tadalafil and gamma-hydroxybutyrate (GHB). Self-reported non-adherence to HAART was assessed with the question: “When you use drugs do you skip your HIV medication?”, with participants who answered “yes” and “sometimes” being classified as non-adherent.
Socio-demographic questions: questions on socio-demographic characteristics (age, gender, residence, place of birth, level of education, relationship status) of the study populations were asked.
Due to “skip-logic pattern” in both the paper-pencil and online questionnaires the time needed to complete the questionnaire was between 3 and 12 minutes with mean duration being around 7 minutes.
Participants who answered that they used drugs within the last 6 months were classified as drug users; additionally those that indicated using more than one drug within the same period were classified as polydrug users. Furthermore, eleven participants indicated that they used only sildenafil/tadalafil in the past 6 months, which were prescribed by their chosen physician; therefore, these participants were not classified as drug users.
Statistical analysis
Descriptive statistics were performed for each variable. In case of normal distribution, quantitative variables are shown as mean values and standard deviation and qualitative variables as frequency and percentage. Differences in frequencies of categorical variables were calculated using the Chi-square test and t-test for unpaired samples was used to determine differences between mean values.
In order to determine which variables were associated with drug and polydrug use we performed a multivariate logistic regression model. Based on the results of the Chi-square test and t-test all variables with a cut off value of p < 0.2 were included in the multivariate model. For the model on drug use (Table 3) variables are shown in Table 1, while for the polydrug use model (Table 4) variables are presented in Table 1 and in the text of the results section. We used a stepwise backwards elimination model where the results of the Wald test for individual parameters were examined for each variable. With each regression step, the least significant variable was removed from the model with only those variables associated with drug and polydrug use with a p value under 0.05 being kept in the final model. All p-values below 0.05 were considered statistically significant. The analysis was performed using the SPSS 24.0 statistical software.
Ethical consideration
The study was approved by the Ethical Committee (EK 16-088-VK) of the City of Vienna on 22nd of June 2016. The study was performed in accordance to the Helsinki Declaration and the principles of Good Clinical Practice. Informed consent was obtained from all participants prior to their inclusion in the study.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
The authors wish to thank Dr. Karl Heinz Pichler, Mag. Leonie Meemken, Sonja Wolf-Nussmüller and Werner Derler for their help with data preparation and patient recruitment.
Author Contributions
I.G., M.M., H.S., B.L. and T.D. developed the research protocol. M.M., H.S. and B.L. recruited the patients and I.G. and T.D. performed the data analysis. All authors contributed to the data interpretation and writing of the final manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Joint United Nations Programme on HIV/AIDS (UNAIDS). UNAIDS Data 2017. (Geneva, 2017). [PubMed]
- 2.Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. Lancet. 2013;382:1525–1533. doi: 10.1016/S0140-6736(13)61809-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mocroft A, et al. Serious fatal and nonfatal non-AIDS-defining illnesses in Europe. J Acquir Immune Defic Syndr. 2010;55:262–270. doi: 10.1097/QAI.0b013e3181e9be6b. [DOI] [PubMed] [Google Scholar]
- 4.Brath H, Grabovac I, Schalk H, Degen O, Dorner TE. Prevalence and Correlates of Smoking and Readiness to Quit Smoking in People Living with HIV in Austria and Germany. PLoS One. 2016;11:e0150553. doi: 10.1371/journal.pone.0150553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shiau S, Arpadi SM, Yin MT, Martins SS. Patterns of drug use and HIV infection among adults in a nationally representative sample. Addictive Behaviors. 2017;68:39–44. doi: 10.1016/j.addbeh.2017.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tron L, Lert F, Spire B, Dray-Spira R, group, A. N.-V. s. Tobacco smoking in HIV-infected versus general population in france: heterogeneity across the various groups of people living with HIV. PLoS One. 2014;9:e107451. doi: 10.1371/journal.pone.0107451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vijayaraghavan M, et al. Smoking Behaviors in a Community-Based Cohort of HIV-Infected Indigent Adults. Aids and Behavior. 2014;18:535–543. doi: 10.1007/s10461-013-0576-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nutt DJ, King LA, Phillips LD, Independent Scientific Committee on, D Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376:1558–1565. doi: 10.1016/S0140-6736(10)61462-6. [DOI] [PubMed] [Google Scholar]
- 9.European Monitoring Centre for Drugs and Drug Addiction. European Drug Report2017. (Luxembourg, 2017).
- 10.The EMIS Network. EMIS 2010: The European Men-Who-Have-Sex-With-Men Internet Survey. Findings from 38 Countries. (European Center for Disease Prevention and Control, Stockholm, 2013).
- 11.Hammoud MA, et al. Following Lives Undergoing Change (Flux) study: Implementation and baseline prevalence of drug use in an online cohort study of gay and bisexual men in Australia. Int J Drug Policy. 2017;41:41–50. doi: 10.1016/j.drugpo.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 12.Avila MM, et al. High Frequency of Illegal Drug Use Influences Condom Use Among Female Transgender Sex Workers in Argentina: Impact on HIV and Syphilis Infections. Aids and Behavior. 2017;21:2059–2068. doi: 10.1007/s10461-017-1766-x. [DOI] [PubMed] [Google Scholar]
- 13.Clatts MC, Goldsamt LA, Giang LM, Yu G. Sexual practices, partner concurrency and high rates of sexually transmissible infections among male sex workers in three cities in Vietnam. Sexual Health. 2015;12:39–47. doi: 10.1071/SH14101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heiligenberg M, et al. Recreational drug use during sex and sexually transmitted infections among clients of a city sexually transmitted infections clinic in Amsterdam, the Netherlands. Sex Transm Dis. 2012;39:518–527. doi: 10.1097/OLQ.0b013e3182515601. [DOI] [PubMed] [Google Scholar]
- 15.De Ryck I, Van Laeken D, Noestlinger C, Platteau T, Colebunders R. The use of erection enhancing medication and party drugs among men living with HIV in Europe. AIDS Care. 2013;25:1062–1066. doi: 10.1080/09540121.2012.748877. [DOI] [PubMed] [Google Scholar]
- 16.Li J, McDaid LM. Alcohol and drug use during unprotected anal intercourse among gay and bisexual men in Scotland: what are the implications for HIV prevention? Sex Transm Infect. 2014;90:125–132. doi: 10.1136/sextrans-2013-051195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fisher DG, Reynolds GL, Napper LE. Use of crystal methamphetamine, Viagra, and sexual behavior. Curr Opin Infect Dis. 2010;23:53–56. doi: 10.1097/QCO.0b013e328334de0b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fisher MP, Ramchand R, Bana S, Iguchi MY. Risk Behaviors Among HIV-Positive Gay and Bisexual Men at Party-Oriented Vacations. J Stud Alcohol Drugs. 2013;74:158–167. doi: 10.15288/jsad.2013.74.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daskalopoulou M, et al. Recreational drug use, polydrug use, and sexual behaviour in HIV-diagnosed men who have sex with men in the UK: results from the cross-sectional ASTRA study. Lancet HIV. 2014;1:e22–31. doi: 10.1016/S2352-3018(14)70001-3. [DOI] [PubMed] [Google Scholar]
- 20.Viswanathan S, et al. Level of adherence and HIV RNA suppression in the current era of highly active antiretroviral therapy (HAART) AIDS Behav. 2015;19:601–611. doi: 10.1007/s10461-014-0927-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Colfax G, Guzman R. Club drugs and HIV infection: a review. Clin Infect Dis. 2006;42:1463–1469. doi: 10.1086/503259. [DOI] [PubMed] [Google Scholar]
- 22.Marquez C, Mitchell SJ, Hare CB, John M, Klausner JD. Methamphetamine use, sexual activity, patient-provider communication, and medication adherence among HIV-infected patients in care, San Francisco 2004-2006. AIDS Care. 2009;21:575–582. doi: 10.1080/09540120802385579. [DOI] [PubMed] [Google Scholar]
- 23.Shirazi J, et al. Epigenetics, drugs of abuse, and the retroviral promoter. J Neuroimmune Pharmacol. 2013;8:1181–1196. doi: 10.1007/s11481-013-9508-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tyagi M, Bukrinsky M, Simon GL. Mechanisms of HIV Transcriptional Regulation by Drugs of Abuse. Curr HIV Res. 2016;14:442–454. doi: 10.2174/1570162X14666160324124736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tyagi M, Weber J, Bukrinsky M, Simon GL. The effects of cocaine on HIV transcription. J Neurovirol. 2016;22:261–274. doi: 10.1007/s13365-015-0398-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garin N, et al. Recreational drug use among individuals living with HIV in Europe: review of the prevalence, comparison with the general population and HIV guidelines recommendations. Front Microbiol. 2015;6:690. doi: 10.3389/fmicb.2015.00690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garin N, et al. Prevalence and clinical impact of recreational drug consumption in people living with HIV on treatment: a cross-sectional study. BMJ Open. 2017;7:e014105. doi: 10.1136/bmjopen-2016-014105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peretti-Watel P, Spire B, Lert F, Obadia Y, Group V. Drug use patterns and adherence to treatment among HIV-positive patients: evidence from a large sample of French outpatients (ANRS-EN12-VESPA 2003) Drug Alcohol Depend. 2006;82(Suppl 1):S71–79. doi: 10.1016/S0376-8716(06)80012-8. [DOI] [PubMed] [Google Scholar]
- 29.Cohn SE, et al. Association of ongoing drug and alcohol use with non-adherence to antiretroviral therapy and higher risk of AIDS and death: results from ACTG 362. AIDS Care. 2011;23:775–785. doi: 10.1080/09540121.2010.525617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Merline AC, O’Malley PM, Schulenberg JE, Bachman JG, Johnston LD. Substance use among adults 35 years of age: prevalence, adulthood predictors, and impact of adolescent substance use. Am J Public Health. 2004;94:96–102. doi: 10.2105/AJPH.94.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rote SM, Brown RL. Gender differences in alcohol and drug use among Hispanic adults: the influence of family processes and acculturation. J Addict Dis. 2013;32:354–364. doi: 10.1080/10550887.2013.859452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.U.S. Department of Health and Human Services. Results of the 2013 National Survey on Drug Use and Health: Summary of National Findings, https://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.pdf (2014).
- 33.Keyes KM, Cerda M, Brady JE, Havens JR, Galea S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014;104:e52–59. doi: 10.2105/AJPH.2013.301709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rhew IC, David Hawkins J, Oesterle S. Drug use and risk among youth in different rural contexts. Health Place. 2011;17:775–783. doi: 10.1016/j.healthplace.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Folch C, Esteve A, Zaragoza K, Munoz R, Casabona J. Correlates of intensive alcohol and drug use in men who have sex with men in Catalonia, Spain. Eur J Public Health. 2010;20:139–145. doi: 10.1093/eurpub/ckp091. [DOI] [PubMed] [Google Scholar]
- 36.Purcell DW, Moss S, Remien RH, Woods WJ, Parsons JT. Illicit substance use, sexual risk, and HIV-positive gay and bisexual men: differences by serostatus of casual partners. AIDS. 2005;19(Suppl 1):S37–47. doi: 10.1097/01.aids.0000167350.00503.db. [DOI] [PubMed] [Google Scholar]
- 37.Hammoud MA, et al. Off-Label Use of Phosphodiesterase Type 5 Inhibitor Erectile Dysfunction Medication to Enhance Sex Among Gay and Bisexual Men in Australia: Results From the FLUX Study. J Sex Med. 2017;14:774–784. doi: 10.1016/j.jsxm.2017.04.670. [DOI] [PubMed] [Google Scholar]
- 38.Dirks H, et al. Substance use and sexual risk behaviour among HIV-positive men who have sex with men in specialized out-patient clinics. HIV Med. 2012;13:533–540. doi: 10.1111/j.1468-1293.2012.01005.x. [DOI] [PubMed] [Google Scholar]
- 39.Drumright LN, Gorbach PM, Little SJ, Strathdee SA. Associations between substance use, erectile dysfunction medication and recent HIV infection among men who have sex with men. AIDS Behav. 2009;13:328–336. doi: 10.1007/s10461-007-9330-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jackson G, Montorsi P, Cheitlin MD. Cardiovascular safety of sildenafil citrate (Viagra): an updated perspective. Urology. 2006;68:47–60. doi: 10.1016/j.urology.2006.05.047. [DOI] [PubMed] [Google Scholar]
- 41.Schmidt AJ, et al. Trouble with bleeding: risk factors for acute hepatitis C among HIV-positive gay men from Germany–a case-control study. PLoS One. 2011;6:e17781. doi: 10.1371/journal.pone.0017781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Joint United Nations Programme on HIV/AIDS. Public Health and HIV viral load supression. (World Health Organization, Geneva, 2017).
- 43.Hosseini Z, et al. Adherence to HIV/AIDS antiretroviral therapy among drug users: A qualitative study in Iran. Iran J Nurs Midwifery Res. 2016;21:29–37. doi: 10.4103/1735-9066.174757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Malta M, Magnanini MM, Strathdee SA, Bastos FI. Adherence to antiretroviral therapy among HIV-infected drug users: a meta-analysis. AIDS Behav. 2010;14:731–747. doi: 10.1007/s10461-008-9489-7. [DOI] [PubMed] [Google Scholar]
- 45.De Boni RB, et al. Substance Use and Adherence Among People Living with HIV/AIDS Receiving cART in Latin America. AIDS Behav. 2016;20:2692–2699. doi: 10.1007/s10461-016-1398-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Halkitis P, Palamar J, Mukherjee P. Analysis of HIV medication adherence in relation to person and treatment characteristics using hierarchical linear modeling. AIDS Patient Care STDS. 2008;22:323–335. doi: 10.1089/apc.2007.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li L, et al. Antiretroviral therapy adherence and self-efficacy among people living with HIV and a history of drug use in Vietnam. Int J STD AIDS. 2017;28:1247–1254. doi: 10.1177/0956462417696431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kalichman SC, et al. Intentional Medication Nonadherence Because of Interactive Toxicity Beliefs Among HIV-Positive Active Drug Users. J Acquir Immune Defic Syndr. 2015;70:503–509. doi: 10.1097/QAI.0000000000000776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Adimora AA, Auerbach JD. Structural interventions for HIV prevention in the United States. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S132–135. doi: 10.1097/QAI.0b013e3181fbcb38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lucas GM, et al. Illicit drug use and HIV-1 disease progression: a longitudinal study in the era of highly active antiretroviral therapy. Am J Epidemiol. 2006;163:412–420. doi: 10.1093/aje/kwj059. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.