Abstract
As the global burden of cardiovascular disease (CVD) rises, public health-related interventions aimed at prevention of heart disease have gained medical attention. Clinical research reports that exercise is a protective risk factor associated with CVD and that clinicians need to provide exercise recommendations to patients. Nevertheless, physical inactivity remains a public health problem. In certain populations, like firefighters (FF), increased risk of CVD is especially concerning. The workload FF face is extreme, 50% of line-of-duty deaths (LODD) in FF are cardiac-related, and research on the volunteer FF population is scarce. Government regulations do not require volunteer FF companies to have fitness testing or programming, so exercise intervention studies are necessary to improve the burden of CVD risk in this population. Therefore, this study examined the effects of a 4-week exercise circuit training (CT) intervention on vascular health and fitness in volunteer FF (N = 27) from the Philadelphia PA area compared to a control group of Non-FF (N = 25). Carotid artery intima-media thickness (IMT), brachial artery flow-mediated dilation (FMD), augmentation index, and pulse pressure (PP), brachial and central blood pressure (BP) and fitness were measured pre- and post- intervention. Overall, volunteer FF had more significant improvements (p < 0.05) in vascular health measures (FMD, IMT, and PP). In both groups, we also found that brachial and central BP decreased with exercise. We show that a 4 week CT program can improve vascular structure and function in the volunteer FF population, suggesting that clinicians may be able to reduce or prevent cardiac LODD by exercise.
Keywords: Vascular health, Flow-mediated dilation, Blood pressure, Exercise, Carotid artery intima media thickness, Volunteer firefighters
Highlights
-
•
Short term circuit training improves vascular health in volunteer firefighters.
-
•
Core blood pressure and clinic blood pressure are reduced with 4 weeks of training.
-
•
Implementing functional exercise programs in firehouses would improve overall health.
1. Introduction
As the global burden of cardiovascular disease (CVD) rises, public health-related interventions aimed at prevention of heart disease have gained medical attention. Over the years, clinical research has shown that exercise is an independent and protective risk factor associated with CVD, blood pressure (BP), and blood vessel function (Chobanian et al., 2013; Ashor et al., 2014). In fact, population-based studies and meta-analyses have reported that any amount of exercise or a healthy lifestyle can be beneficial and reduce CVD, even reducing risk of all-cause mortality up to 40% (Kodama et al., 2009; Maessen et al., 2016). Despite this, physical inactivity remains a global public health problem and accounts for millions of deaths annually, thus the potential benefit of increased activity could be substantial.
In certain populations, increased risk of CVD is especially concerning. Many physicians and public health officials are unaware that heart disease or cardiac incidents are related to almost 50% of line-of-duty deaths in firefighters (FF) (Geibe et al., 2008). Firefighting is a dangerous occupation because of its many physical and physiological demands. In the U.S, firefighters can be either paid full-time “career FF” or they can be “regular” people who volunteer to be FF, “volunteer FF”.
Many career FF have hypertension, are obese, and have more CVD risk factors than Non-FF (Yoo and Franke, 2009). As outlined by the AHA in Non-FF, CVD risk factors include hypertension, obesity, smoking, inactivity, and abnormal glucose and cholesterol levels. Evidence suggests that career FF have increased possibility of cardiac events due to similar relative risk factors. Volunteer FF make up 70% of the total FF population, and are an understudied population. Considering the well-established fact that exercise can reduce CVD risk, it is interesting that volunteer FF companies are not required by the National Fire Protection Association (NFPA) to have fitness testing or a fitness program for the crew. The NFPA makes suggestions for fitness and has established that demands of FF activities on the cardiovascular system require a fitness level of a VO2max of 42 ml/kg/min (NFPA 1582, 2007); however, it is estimated that only around 20% of volunteer FF meet this fitness threshold (Poston et al., 2011).
There remains a gap in the exercise literature, for the volunteer FF population that examines vascular health changes with exercise. In 2009, Williams-Bell et al. estimated that during firefighting activities, FF may work at 75–80% of their VO2max level (Williams-Bell et al., 2009). Recently, we reported that BP responses to exercise were exaggerated in volunteer FF while wearing full firefighting personal protective equipment (PPE) (Feairheller, 2015) A separate study found that oxidative stress increased and DNA damage occurred in FF wearing PPE while exercising (Park et al., 2016). These studies suggest that the workload FF face is extreme, so exercise intervention studies in FF are necessary.
Exercise-induced vascular health improvements can be evaluated by a number of clinical modalities, including: flow-mediated dilation (FMD, an index of nitric oxide-mediated endothelial-dependent function), carotid artery intima-media thickness (IMT, an index of common carotid artery plaque and atherosclerotic potential), and arterial stiffness measured by pulse pressure (PP) and augmentation index (AIx, an index of arterial stiffness that quantifies the reflected wave at the aorta) (Polak and OLeary, 2016; Harris et al., 2010; Perk et al., 2012). There is not yet a clear consensus on which type of exercise (aerobic, resistance, or combination) has a better effect on CV health overall, but recently it has been suggested that combination training has a greater effect on vascular health, arterial stiffness, BP and VO2max when compared to aerobic or resistance training (Ho et al., 2012). Circuit training (CT), one form of combination training incorporates aerobic movement and resistance type exercises. Clinical research that examines improvements in CVD risk factors with CT exercise are scarce, and few studies are published with only 4 weeks of exercise. In some research, adults who underwent 10–12 weeks of aerobic exercise, but not resistance training, had improvements in FMD and IMT (Beck et al., 2013; Casey et al., 2007). Recently we reported that adults who completed 6 months of aerobic exercise training had improvements in IMT and FMD (Feairheller et al., 2014). Shorter exercise training studies are needed.
Actual clinical exercise intervention studies in the volunteer FF population do not exist. In career FF, it has been reported that 12 or 16 week CT programs which simulate fire-ground activities have beneficial effects on fitness and body composition (Roberts et al., 2002; Pawlak et al., 2015). Also, FF fire suppression training drills are similar to CT and focus on cardiovascular endurance and muscular strength (Rhea et al., 2004). Nevertheless, exercise-induced improvements in vascular health in FF have yet to be measured. Therefore, the purpose of this study was to compare the effects of a 4 week CT program on CV risk factors between a group of volunteer FF and a group of Non-FF. Taking into consideration that guidelines require career fire departments mandate health, wellness, and fitness programs, career FF inherently may be more fit or healthy, so we chose a comparison group of Non-FF instead of career FF. Volunteer FF are “everyday” people who sign up to get fire and rescue training, respond to any number of calls, and are allowed to volunteer as much as they can or have time to, thus a better comparison group to this would be Non-FF. Volunteer FF make up over 70% of the entire FF population, they respond to many fire/rescue calls every year and it needs to be examined how their health compares to the general population. A comparison of career FF to volunteer FF would not be beneficial. Due to the lack of wellness and fitness regulations in volunteer fire stations, the volunteer FF population has worse health than career FF. The question that needs to be addressed is how volunteer FF health compares to “everyday” people.
2. Methods
This was a quasi-experimental pre-post intervention with a comparison group of Non-FF matched by age. Criteria for inclusion were: no more than one BP medication, no cholesterol medications, other medications were allowed, no prior cardiovascular incidents, no diagnosed heart disease or diabetes, non-smoker, no physical limitation that would preclude an exercise program, and >70% adherence to the CT intervention. Each participant gave informed consent and completed a general health history form. The protocol was approved by the Ursinus College Institutional Review Board, and all procedures were in accordance with the ethical standards of the Helsinki Declaration.
All enrolled participants completed pre-testing, underwent a 4 week CT intervention, and then completed post-testing which was a repeat of all baseline tests. The pre- and post- data collection included two visits each, a fasted visit and a fitness test. For the fasted visit, all participants would report to the laboratory following an overnight fast. The visit took place in a quiet, temperature controlled room. Participants were asked to refrain from exercise for 24 h prior and from any food, drink, medication, and caffeine for at least 10 h prior to the test. Participants were also asked to remove any jewelry and other accessories prior to the measurements.
2.1. Circuit training program
The 4 week CT program was completed 3 times per week. Each CT workout involved 6 stations which were completed 3 times per workout. Before the training period, all participants underwent an exercise familiarization session to ensure proper execution of technique. The 6 stations included a 40 lb. carry for 100 ft., 3-min stair climb, 45 s plank pose, 20 lb. carry with a fast walk for 100 ft., right and left single leg stands for as long as balance was maintained, and a 15 lb. carry up and down 30 stairs.
2.2. Blood pressure measurements
Brachial BP measurements were obtained in accordance with JNC-7 guidelines by laboratory personnel on multiple visits using an aneroid sphygmomanometer (Medline Industries, Mundelein, IL) (Chobanian et al., 2013). BP measurements were performed in triplicate with the average of the three values used as the representative BP for that visit. The mean systolic and diastolic BP across the clinical visits is reported as the brachial BP.
2.3. Radial pulse wave analysis (PWA) measurements
Radial artery PWA measurements were collected after the participant had rested supine for 15 min. BP was measured immediately before measurement, and peripheral pulse waveforms were captured using a hand-held tonometer probe (Millar/AtCor Medical pressure tonometer, Houston, TX). The tonometer was applanated (applied to flatten the artery but not occlude it) at the radial artery with the wrist supported and in an extended position. The shape of the peripheral pulse wave was collected electronically with a laptop which was linked to the SphygmoCor PW system (SphygmoCor CPV, software version 8.2, AtCor Medical, Sydney, Australia). Data from quality pulse waveforms were considered acceptable, and this was assessed by the software's internal quality control index (operator index > 80%). The average of 3 measures is reported. PWA is reliable and provides measurement of several main indices: central aortic systolic and diastolic BP, AIx adjusted to heart rate (HR) of 75 beats per minute, PP and subendocardial viability ratio (SEVR) (Crilly et al., 2007). In our laboratory, we have calculated the intraclass correlation coefficient (ICC) for PWA measurements at >0.97.
2.4. Vascular ultrasound measurements
The same operator completed all ultrasounds. Fasted brachial artery diameter measurements using FMD were collected while participant was supine, after 15 min of acclimation to obtain a hemodynamic steady state. HR was continuously monitored using a 3‑lead ECG, and BP measurements were taken in the left arm to confirm a steady state. A 5 × 84-cm automatic cuff (E-20 rapid cuff inflator; D.E. Hokanson Bellevue, WA) was placed around the right forearm distal to the olecranon process following established FMD guidelines (Corretti et al., 2002). Image collection, transducer placement, and detailed methods were completed as previously described (Feairheller et al., 2014). FMD videos were recorded using the GE Logiq E ultrasound system (Model BT12, GE Medical Systems, Chicago, IL) and downloaded to separate computer using Movavi Video Editor (Movavi, St Louis, MO). Arterial diameters were analyzed using edge detection software, Brachial Analyzer for Research (Medical Imaging Applications, Coralville, IA). The highest 10 s interval throughout the 2 min collection period represented the true peak hyperemic diameter. FMD reported is the percent increase in diameter from baseline. The ICC for baseline diameter, peak diameter, and FMD are 0.94, 0.94, and 0.73 respectively. Intra-observer reliability for the image analysis using the analysis software has been established at 99.2%.
On the same day as FMD measurements, carotid artery IMT images were recorded and automatically calculated as previously described (Feairheller et al., 2014). Images were obtained and measurements made using the GE Logiq E ultrasound system and automated calculation software (Auto-IMT Software Option, GE Medical Systems, Chicago, IL). Three measures of the posterior wall of the right and left common carotid arteries were collected, as per established guidelines (Roman et al., 2006), and the average of all readings is reported. In our laboratory, we have calculated the ICC for IMT measurements at >0.90, with interobserver variability < 0.04 mm and intraobserver variability < 0.02 mm.
2.5. Plasma glucose & cholesterol measurements
Fasted plasma glucose and cholesterol levels were obtained using the Alere Cholestech LDX® lipid profile system (San Diego, CA). Blood was obtained by finger stick using a 35 μl lithium heparin-coated capillary tube, and tested immediately. Alere Cholestech lipid profile values are correlated (r > 0.95) with venous plasma measured in clinical diagnostic laboratories, which meets the cholesterol criteria (Expert Panel, 2001).
2.6. Body composition measurements
Body composition was measured by whole-body Bioelectrical Impedance Analysis (BIA) (ImpediMed DF50, San Diego, CA). Height and weight were measured using a calibrated electronic scale without shoes. BIA was measured in accordance with the manufacturer's instructions at 50 kHz on the right side of the body, two electrodes placed on the dorsal right hand and foot while the participants were lying in a supine position. Three measurements were taken, and the mean values of impedance, phase, resistance, and reactance were used for calculations.
2.7. Fitness testing
Separately, participants reported to the laboratory to complete fitness testing. A maximal symptom-limited treadmill stress test was performed with continuous ECG monitoring (Nasiff CardioCard, Nasiff Associates Inc., New York, NY). BP and perceived exertion were assessed at each stage, and HR was recorded each minute. The treadmill test was terminated according to guidelines, and VO2max was calculated using the Bruce protocol test time formula (Fletcher et al., 2013; Foster et al., 1984).
Following the treadmill test, participants completed a stair climb test, which is reported as a quality measure of overall fitness in FF (Calavalle et al., 2013). Participants were required to continuously climb up and down a set of steps for 2 min, and the number of steps was recorded. Generally, FF activities have been found to affect balance (Colburn et al., 2017), so to measure balance participants stood on one leg at a time for as long as possible. The data collected from right and left leg were combined and total time is reported. Next, until exhaustion, participants held a plank position and then a “wall-sit”. Test results from plank and wall sit times were combined, and this is reported as muscular endurance in the results.
A Fitness Index was calculated for both pre- and post-fitness test data. This index was calculated as a means of assessing volunteer FF fitness. Studies in our lab have begun to investigate ways that volunteer FF can be engaged in their fitness. A simple fitness index calculation may provide fire stations a simple way to assess individual FF fitness. It may also provide a way for each volunteer FF to be motivated, if they see this number improving with implementation of a fitness program. The patient's prior exercise value, reported during initial intake, was combined with the fitness testing stair-climb and balance test results. The sum of these three numbers made up 1/3 of the fitness index. Cardiovascular endurance (VO2max) and muscular endurance made up the other 2/3 of the fitness index. The value of a lifestyle or fitness index was seen in the recent Multisite Cardiac Lifestyle Intervention Program study (Dod et al., 2010).
2.8. Statistical analyses
Data are expressed as mean ± the standard deviation. All data were tested for distribution with the Shapiro-Wilk test of normality. Nonparametric tests were used when appropriate. Pre- and post- exercise values were compared using the paired samples t-test or the paired samples Wilcoxon signed-rank test, as appropriate. Independent t-tests were used to compare differences between volunteer FF and Non-FF groups. Repeated measures ANOVA were used to evaluate time by group interactions, and within-group Tukey's post hoc analysis was performed. Bivariate Pearson's correlation analysis was completed to determine if there were relationships between the variables and was further examined by linear regression analysis. Alpha level of P < 0.05 was required for statistical significance. All statistical analyses were performed using SPSS version 19.0 (SPSS Inc., Chicago, IL, USA).
3. Results
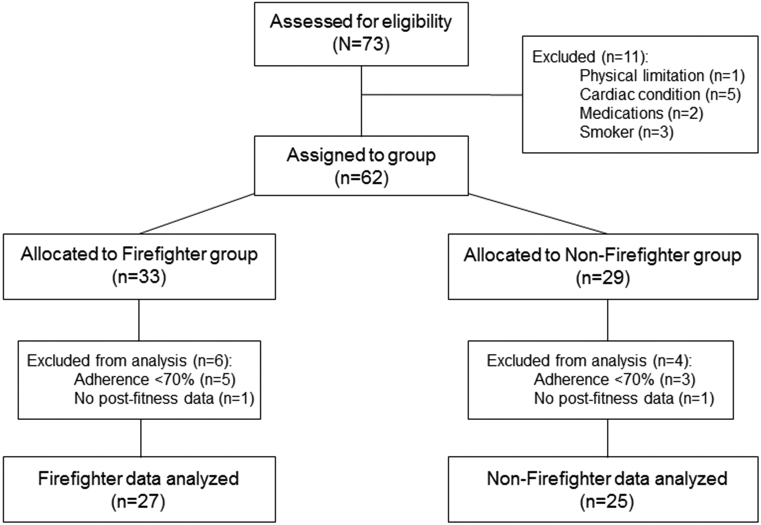
A total of 73 participants were assessed for eligibility, 62 were assigned to groups, and data from 52 adults, 25 Non-FF and 27 FF, was used for the analysis (Fig. 1). In our study, the number of female volunteer FF was low, which is similar to the consistent gender ratio in the overall FF population. According to the NFPA's recent statistics, the annual average number of female FF is very low, around 5%. While the percentage of female adults in the United States is around 50%. We have kept our groups with similar differences, the Non-FF group has a higher percentage of females compared to the FF group, which has a lower percentage. This keeps the study group comparison numbers similar to what the overall population comparison would be. Adherence to the exercise program was 95.8% overall, similar between both groups. Baseline (pre-exercise) and final (post-exercise) health data is presented in Table 1. No differences exist at baseline, but volunteer FF had improvements in body composition and lipid levels with exercise.
Fig. 1.
Study flow diagram.
Table 1.
Physiological changes with exercise training.
| Variable |
Non-firefighters (N = 25) |
Firefighters (N = 27) |
||
|---|---|---|---|---|
| Baseline | Final | Baseline | Final | |
| Age, years | 34.4 ± 15.2 | – | 36.2 ± 13.7 | – |
| Male/female | 18/7 | – | 24/3 | – |
| Body mass, kg | 81.81 ± 20.5 | 81.63 ± 20.1 | 91.54 ± 17.2 | 91.4 ± 17.6 |
| BMI, kg/m2 | 28.8 ± 6.8 | 28.7 ± 6.6 | 30.9 ± 5.3 | 30.8 ± 5.4 |
| Body FAT, % | 27.9 ± 12.2 | 27.4 ± 12.0 | 33.5 ± 6.7 | 32.1 ± 7.4⁎ |
| Total cholesterol, mg/dl | 166.6 ± 33.3 | 163.7 ± 32.5 | 156.1 ± 29.1 | 150.3 ± 27.4⁎ |
| Triglycerides, mg/dl | 94.0 ± 60.2 | 105.3 ± 73.4 | 118.2 ± 59.0 | 97.3 ± 55.4⁎ |
| HDL-C, mg/dl | 45.4 ± 13.1 | 47.5 ± 12.8 | 39.0 ± 11.8 | 40.3 ± 11.2β |
| LDL-C, mg/dl | 105.3 ± 31.5 | 97.6 ± 24.9 | 96.3 ± 28.8 | 93.0 ± 27.8 |
| Glucose, mg/dl | 88.5 ± 9.1 | 90.1 ± 8.9 | 90.9 ± 10.1 | 90.1 ± 6.9 |
Data are presented as mean ± SD. Significance set at p < 0.05. BMI, body mass index; HDL, high density lipoprotein; LDL, low density lipoprotein.
p < 0.05 with training.
p < 0.05 between groups.
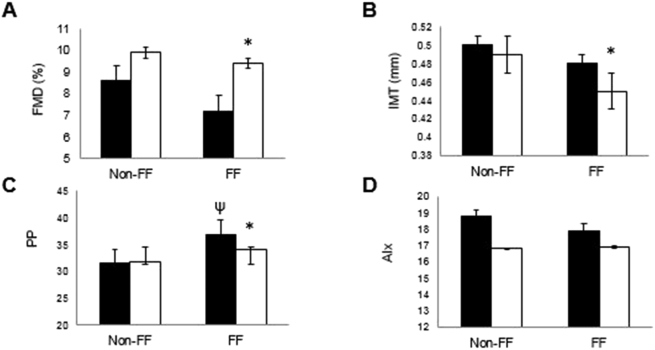
Vascular health changes are reported in Fig. 2. Volunteer FF had higher PP compared to Non-FF. We found significant improvements in FMD, IMT, and PP. FMD increased 2.2% in volunteer FF and 1.3% in Non-FF, common carotid IMT decreased 4.0% in volunteer FF and 1.7% in Non-FF, while PP decreased 4.1% in volunteer FF. There was a positive relationship between IMT and LDL levels in the FF group only (r = 0.455, p < 0.05).
Fig. 2.
Vascular health changes with exercise in non-firefighter (Non-FF) and FF. Values reported are means, pre-test (filled bars) and post-test (open bars). A. Flow Mediated Dilation (FMD) B. Carotid artery Intima Media Thickness (IMT) C. Pulse Pressure (PP) D. Augmentation Index (AIx). *Significant p < 0.05, with training. ψSignificant p < 0.05, between groups.
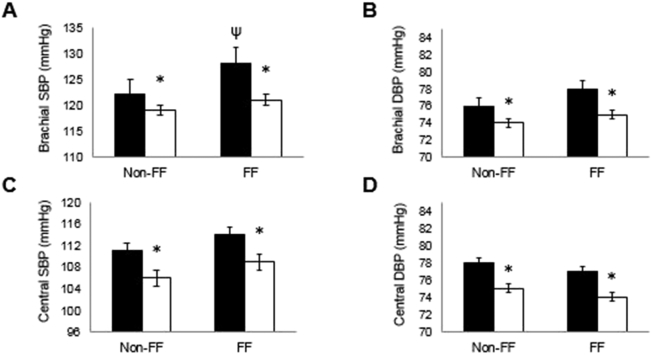
BP improvements with training are shown in Fig. 3. At baseline, volunteer FF had significantly higher systolic BP compared to Non-FF. With CT training, we found significant improvements in brachial and central BP for both groups. Systolic BP (brachial) decreased 5.0% in volunteer FF and 2.7% in Non-FF, while diastolic BP (brachial) decreased 4.2% in volunteer FF and 3.2% in Non-FF. Central BP improvements were similar; systolic BP (central) decreased 3.4% in volunteer FF and 3.3% in Non-FF, diastolic BP (central) decreased 2.8% in volunteer FF and 4.8% in Non-FF. Overall, CT exercise reduced clinical BP to normotensive levels in 19 and to pre-hypertensive range in 16 participants.
Fig. 3.
Blood pressure changes with exercise in non-firefighter (Non-FF) and FF. Values reported are means, pre-test (filled bars) and post-test (open bars). A. Brachial Systolic Blood Pressure (SBP) B. Brachial Diastolic Blood Pressure (DBP) C. Central SBP D. Central DBP. *Significant p < 0.05, within group with training. ψSignificant p < 0.05, between groups.
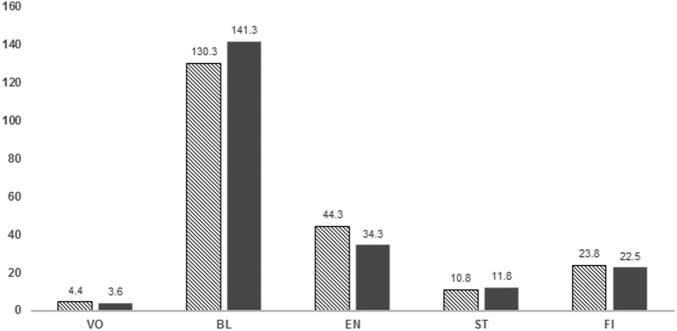
Table 2 shows baseline (pre-exercise) fitness levels. Volunteer FF had higher muscular endurance and overall fitness compared to Non-FF. The percent improvements in fitness are shown in Fig. 4. All fitness measures improved significantly with no between group interactions.
Table 2.
Baseline fitness measures.
| Variable | Non-FF (N = 25) | FF (N = 27) |
|---|---|---|
| VO2max (ml/kg/min) | 37.1 ± 9.0 | 35.7 ± 4.3 |
| Balance, min | 1.93 ± 1.6 | 2.47 ± 1.9 |
| Muscular Endurance, min | 2.12 ± 1.1 | 3.68 ± 1.9β |
| Stair-Climbing test, # steps | 297.7 ± 59.9 | 319.3 ± 45.2 |
| Fitness Index | 0.83 ± 0.2 | 1.21 ± 0.4β |
Data are presented as mean ± SD. Non-FF, Non-firefighter; FF, Firefighter; VO2max, volume of oxygen; Balance, sum of right and left leg balance; Muscular Endurance, sum of core strength measured plank pose and leg strength measured by wall sit; Stair-Climbing, count of steps climbed in 2 min; Fitness Index, composite fitness calculation (see Methods).
p < 0.05 between groups.
Fig. 4.
Percent improvements in fitness markers with exercise in non-firefighter (hashed bars) and firefighters (solid bars). Values reported are percent changes with the circuit training program. VO, Volume of Oxygen consumption max test; BL, Balance sum of right and left leg balance test; EN, Muscular Endurance sum of core strength/endurance measured by plank pose and leg strength/endurance measured by wall sit; ST, Stair-Climb total count of steps; FI, Fitness Index composite fitness calculation (see methods) training. Significant within-group changes with training for all.
4. Discussion
To the best of our knowledge, this was the first CT intervention that compared vascular health responses to exercise between volunteer FF and Non-FF, and the results compare well with studies of 3–6 times longer. The primary novel findings of the present study are that 4 weeks of CT improved vascular health measures FMD, IMT, and PP in a group of volunteer FF. The current study also found that 4 weeks of CT similarly reduced brachial and central BP levels in both groups.
Endothelial function is known to predict clinical events, and endothelial function testing with FMD is associated with the progression of IMT seen in subclinical atherosclerosis (Halcox et al., 2009). Between clinical research studies, change differences in arterial stiffness or vascular function may be due to several factors, including training programs and exercise volume. The majority of research on exercise effects on endothelial function focus on the improvements seen with aerobic training; however, there is some evidence that FMD may also improve with resistance or combination training (Beck et al., 2013; Collier et al., 2008).
It is established that atherosclerotic disease develops slowly, is related to cholesterol and BP levels, and can be imaged prior to the development of clinically apparent disease. At baseline, FMD and IMT were lower and all BP measures were higher in volunteer FF, suggesting altered endothelial function and augmented vascular resistance. Previously we found that 6 months of aerobic exercise training improved FMD and reduced inflammation (Babbitt et al., 2013). In clinical exercise studies, 8 or 10 weeks of exercise improved FMD (Okamoto et al., 2011; Luk et al., 2011). In each of these studies, FMD increased around 2% with exercise. The volunteer FF in our study had similar improvements. Due to differences in ultrasound technology and imaging protocols, it is difficult to directly compare measured IMT values among studies. The IMT measurements in our study were similar to measures reported by Fahs et al., where the authors reported that FF with increased BMI had higher BP and arterial stiffness (Fahs et al., 2009). The volunteer FF in our study were larger than Non-FF. Increased carotid IMT is associated with cholesterol levels, studies have reported that LDL cholesterol may be a predictor of IMT. Also, clinical trials have found that statin therapy reduces subclinical atherosclerosis, as measured by IMT (Bots et al., 2016). We found a direct relationship between IMT and LDL in our group of volunteer FF. All of this vascular data suggests that the FF population may have unique cardiovascular profiles indicative of sub-clinical atherosclerosis.
Reduction of clinical BP levels into the prehypertensive or normotensive range remains the primary clinical goal for hypertension therapy (Chobanian et al., 2013). Plus, exercise remains the recommended non-pharmacologic therapy for hypertension. We confirm this by reporting similar BP improvements as other studies with 4 weeks of exercise (Collier et al., 2008). Brachial BP measurements alone do not provide clinical information about overall systemic BP; therefore, measurement of central BP has gained attention. In the present study, the improvement in central pressures reported are in agreement with others who found reductions in central BP after short-term RT in adults (Heffernan et al., 2009; Taaffe et al., 2007) While mechanism was not examined, it can be hypothesized that reduced central BP may be attributed to a reduced vascular resistance relating to the improved endothelial function (FMD) and structure (IMT).
We found improvements fitness. Exercise studies in FF are limited but some have reported improved fitness and fireground performance (Roberts et al., 2002; Pawlak et al., 2015). Yet lack of physical activity remains a problem in the fire service, and volunteer fire departments are not required to have established fitness programs. NFPA recommends that FF participate in exercise programs but has no requirements (NFPA 1583, 2008). Therefore, more studies in volunteer FF are needed that report on CVD risk reduction with exercise.
This study has several limitations. First, the population for our study group was from the Philadelphia suburban region. This may not be generalizable to all volunteer FF, but this novel study provides valuable clinical exercise research findings. Secondly, to allow analysis of the effects of CT on vascular health, we chose to use a control group of adults who were Non-FF that completed the same exercise intervention. Recent commentaries have suggested that the sedentary control group is unrealistic and can lead to misinterpretation that an inactive condition is healthy enough. This allows our data to direct future research that investigates potential mechanisms for why FF have vascular health improvements. Finally, the present study does not provide causations for the improvements seen in the volunteer FF group. Future studies should examine plasma levels of inflammatory or oxidative stress markers. By the shear nature of what FF do, it can be assumed they may have high inflammation levels which may be associated with the improvements seen in vascular health in the current study.
In conclusion, cardiovascular health may be worse in volunteer FF compared to Non-FF, but with a short 4 week CT program, CVD risk was reduced. The public health and financial burden on communities with volunteer fire departments continues to increase; the number of volunteer FF per population is decreasing and costs of maintaining an active fire company are increasing (Haynes and Stein, 2017). Therefore, exercise interventions aimed at improving health and well-being of FF will prove valuable because cardiac-related LODD could potentially be avoided.
Funding
No funding to disclose.
Disclosure
We have no conflicts of interest to declare.
Acknowledgments/disclosures
Thank you to the volunteer FF and other adults for their participation in the study.
The authors received no outside funding for this research study, and there were no conflicts of interest to report.
References
- Ashor A.W., Lara J., Siervo M. Effects of exercise modalities on arterial stiffness and wave reflection: a systematic review and meta-analysis of randomized controlled trials. PLoS ONE. 2014;9(10) doi: 10.1371/journal.pone.0110034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babbitt D.M., Diaz K.M., Feairheller D.L. Endothelial activation microparticles and inflammation status improve with exercise training in African americans. Int. J. Hypertens. 2013;2013 doi: 10.1155/2013/538017. (8 pages) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck D.T., Casey D.P., Martin J.S. Exercise training improves endothelial function in young prehypertensives. Exp. Biol. Med. 2013;238(4):433–441. doi: 10.1177/1535370213477600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bots M.L., Evans G.W., Tegeler C.H. Carotid intima media thickness measurements: relations with atherosclerosis, risk of cardiovascular disease and application in randomized controlled trails. Chin. Med. J. 2016;129(2):215–226. doi: 10.4103/0366-6999.173500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calavalle A.R., Sista D., Mennelli G. A simple method to analyze overall individual physical fitness in firefighters. J. Strength Cond. Res. 2013;27(3):769–775. doi: 10.1519/JSC.0b013e3182600554. [DOI] [PubMed] [Google Scholar]
- Casey D.P., Beck D.T., Braith R.W. Progressive resistance training without volume increases does not alter arterial stiffness and aortic wave reflection. Exp. Biol. Med. 2007;232(9):1228–1235. doi: 10.3181/0703-RM-65. [DOI] [PubMed] [Google Scholar]
- Chobanian A.V., Bakris G.L., Black H.E. The seventh report of the joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2013;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- Colburn D., Suyama J., Reis S.E. Cardiorespiratory fitness is associated with gait changes among firefighters after a live burn training evolution. Saf. Health Work. 2017;8:183–188. doi: 10.1016/j.shaw.2016.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collier S.R., Kanaley J.A., Carhart R. Effect of 4 weeks of aerobic or resistance exercise training on arterial stiffness, blood flow and blood pressure in pre- and stage-1 hypertensives. J. Hum. Hypertens. 2008;22:678–686. doi: 10.1038/jhh.2008.36. [DOI] [PubMed] [Google Scholar]
- Corretti M.C., Anderson T.J., Benjamin E.J. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery. J. Am. Coll. Cardiol. 2002;39(2):257–265. doi: 10.1016/s0735-1097(01)01746-6. [DOI] [PubMed] [Google Scholar]
- Crilly M., Coch C., Bruce M. Indices of cardiovascular function derived from peripheral pulse wave analysis using radial applanation tonometry: a measurement repeatability study. Vasc. Med. 2007;12:189–197. doi: 10.1177/1358863X07081134. [DOI] [PubMed] [Google Scholar]
- Dod H.S., Bhardwaj R., Sajja V. Effect of lifestyle changes on endothelial function on inflammatory markers of atherosclerosis. Am. J. Cardiol. 2010;105:362–367. doi: 10.1016/j.amjcard.2009.09.038. [DOI] [PubMed] [Google Scholar]
- Expert Panel on Detection, Evaluation, and Treatment of High Cholesterol in Adults Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high cholesterol in adults (adult treatment panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- Fahs C.A., Smith D.L., Horn G.P. Impact of excess body weight on arterial structure, function, and blood pressure in firefighters. Am. J. Cardiol. 2009;104:1441–1445. doi: 10.1016/j.amjcard.2009.07.009. [DOI] [PubMed] [Google Scholar]
- Feairheller D.L. Blood pressure and heart rate responses in volunteer firefighters while wearing personal protective equipment. Blood Press. Monit. 2015;20:194–198. doi: 10.1097/MBP.0000000000000120. [DOI] [PubMed] [Google Scholar]
- Feairheller D.L., Diaz K.M., Kashem M.A. Effects of moderate aerobic exercise training on vascular health and blood pressure in African Americans. J. Clin. Hypertens. 2014;16(7):504–510. doi: 10.1111/jch.12328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher G.F., Ades P.A., Kligfield P. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013;128(8):873–934. doi: 10.1161/CIR.0b013e31829b5b44. [DOI] [PubMed] [Google Scholar]
- Foster C., Jackson A.S., Pollock M.L. Generalized equations for predicting functional capacity from treadmill performance. Am. Heart J. 1984;107(6):1229–1234. doi: 10.1016/0002-8703(84)90282-5. [DOI] [PubMed] [Google Scholar]
- Geibe J.R., Holder J.H., Peeples L. Predictors of on-duty coronary events in male firefighters in the United States. Am. J. Cardiol. 2008;101:585–589. doi: 10.1016/j.amjcard.2007.10.017. [DOI] [PubMed] [Google Scholar]
- Halcox J.P., Donald A.E., Ellins E. Endothelial function predicts progression of carotid intima-media thickness. Circulation. 2009;119:1005–1012. doi: 10.1161/CIRCULATIONAHA.108.765701. [DOI] [PubMed] [Google Scholar]
- Harris R.A., Nishiyama S.K., Wray D.W. Ultrasound assessment of flow-mediated dilation. Hypertension. 2010;55(5):1075–1085. doi: 10.1161/HYPERTENSIONAHA.110.150821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynes H.J., Stein G.P. U.S. Fire Department Profile - 2015. 2017. http://www.nfpa.org/news-and-research/fire-statistics-and-reports/fire-statistics/the-fire-service/administration/us-fire-department-profile Downloaded from.
- Heffernan K.S., Fahs C.A., Iwamoto G.A. Resistance exercise training reduces central blood pressure and improves microvascular function in African American and white men. Atherosclerosis. 2009;207:220–226. doi: 10.1016/j.atherosclerosis.2009.03.043. [DOI] [PubMed] [Google Scholar]
- Ho S.S., Bagatini S.R., Dhaliwal S.S. Resistance, aerobic, and combination training on vascular function in overweight and obese adults. J. Clin. Hypertens. 2012;14:848–854. doi: 10.1111/j.1751-7176.2012.00700.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodama S., Saito K., Tanaka S. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women. JAMA. 2009;301(19):2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- Luk T.H., Dai Y.L., Siu C.W. Effect of exercise training on vascular endothelial function in patients with stable coronary artery disease: a randomized controlled trial. Eur. J. Prev. Cardiol. 2011;19(4):830–839. doi: 10.1177/1741826711415679. [DOI] [PubMed] [Google Scholar]
- Maessen M.F., Verbeek A.L., Bakker E.A. Lifelong exercise patterns and cardiovascular health. Mayo Clin. Proc. 2016;91(6):745–754. doi: 10.1016/j.mayocp.2016.02.028. [DOI] [PubMed] [Google Scholar]
- National Fire Protection Association. NFPA 1582 . 2007. Standard on Comprehensive Occupational Medical Program for Fire Departments. Quincy, MA. [Google Scholar]
- National Fire Protection Association. NFPA 1583 . 2008. Standard on Health-related Fitness Programs for Firefighters. Quincy, MA. [Google Scholar]
- Okamoto T., Masuhara M., Ikuta K. Effect of low-intensity resistance training on artereial function. Eur. J. Appl. Physiol. 2011;111:743–748. doi: 10.1007/s00421-010-1702-5. [DOI] [PubMed] [Google Scholar]
- Park E., Lee Y.-J., Lee S.-W. Changes of oxidative/antioxidative parameters and DNA damage in firefighters wearing personal protective equipment during treadmill walking training. J. Phys. Ther. Sci. 2016;28:3173–3177. doi: 10.1589/jpts.28.3173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawlak R., Clasey J.L., Palmer T. The effect of a novel tactical training program on physical fitness and occupational performance in firefighters. J. Strength Cond. Res. 2015;29(3):578–588. doi: 10.1519/JSC.0000000000000663. [DOI] [PubMed] [Google Scholar]
- Perk J., DeBacker G., Gohlke H. European guidelines on cardiovascular disease prevention in clinical practice: the fifth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice. Atherosclerosis. 2012;223(1):1–68. doi: 10.1016/j.atherosclerosis.2012.05.007. [DOI] [PubMed] [Google Scholar]
- Polak J.F., OLeary D.H. Carotid intima-media thickness as surrogate for and predictor of CVD. Glob. Heart. 2016;11(3):295–312. doi: 10.1016/j.gheart.2016.08.006. [DOI] [PubMed] [Google Scholar]
- Poston W.S., Haddock K., Jahnke S.A. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. JOEM. 2011;53(3):266–273. doi: 10.1097/JOM.0b013e31820af362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhea M.R., Alvar B.A., Gray R. Physical fitness and job performance of firefighters. J. Strength Cond. Res. 2004;18(2):348–352. doi: 10.1519/R-12812.1. [DOI] [PubMed] [Google Scholar]
- Roberts M.A., O'Dea J., Boyce A. Fitness levels of firefighter recruits before and after a supervised exercised training program. J Strength Cond. Res. 2002;16(2):271–277. [PubMed] [Google Scholar]
- Roman M.J., Naqvi T.Z., Gardin J.M. Clinical application of noninvasive vascular ultrasound in cardiovascular risk stratification: a report from the American Society of Echocardiography and the Society for Vascular Medicine and Biology. Vasc. Med. 2006;11(3):201–211. doi: 10.1177/1358863x06070511. [DOI] [PubMed] [Google Scholar]
- Taaffe D.R., Galvao D.A., Sharman J.E. Reduced central blood pressure in older adults following progressive resistance training. J. Hum. Hypertens. 2007;21(1):96–98. doi: 10.1038/sj.jhh.1002115. [DOI] [PubMed] [Google Scholar]
- Williams-Bell M., Villar R., Sharratt M.T. Physiological demands of the firefighter candidate physical ability test. Med. Sci. Sports Exerc. 2009;41(3):653–662. doi: 10.1249/MSS.0b013e31818ad117. [DOI] [PubMed] [Google Scholar]
- Yoo H.L., Franke W.D. Prevalence of cardiovascular disease risk factors in volunteer firefighters. JOEM. 2009;51:958–962. doi: 10.1097/JOM.0b013e3181af3a58. [DOI] [PubMed] [Google Scholar]