Abstract
Sit-stand workstations are a popular workplace intervention. Organizations often require a medical professional's guidance for implementation. Therefore, it is important to understand potential negative outcomes associated with standing work, such as lower limb discomfort and peripheral vascular issues. The objective of this study was to compare changes in lower limb discomfort, blood pressure and blood flow accumulation during a light-load repetitive upper limb work task accomplished from seated and standing postures. At the Jewish Rehabilitation Hospital (Laval, Quebec, Canada), 16 participants were outfitted with Laser Doppler Flow (LDF) electrodes to measure blood flow in the lower limb, and a sphygmomanometer to measure lower limb mean arterial blood pressure (MAP). Participants completed simulated work over 34 min in standing and seated conditions. Repeated measures ANOVAs (Posture x Time) were used to assess the differences. There were significant effects for both Posture (p = 0.003) and Time (p = 0.007) for LDF-measured of blood flow accumulation in the soleus and the foot, with a mean increase of 77% blood flow over time in the standing posture, when compared to seated work. There was a significant ‘Posture × Time’ (p = 0.0034) interaction effect and a significant Posture (p = 0.0001) effect for MAP, with higher values in the standing posture by a mean of 37.2 mmHg. Posture had a significant effect (p < 0.001) on lower limb discomfort, with standing posture reporting higher levels. These results suggest that recommendations for using static standing work postures should be tempered, and physicians' guidance on workstation changes should consider the impacts on the lower limb.
Keywords: Work postures, Standing, Sitting, Vascular outcomes, Lower limb discomfort
Highlights
-
•
Standing work has become popular as a mean of reducing sedentary seated work.
-
•
Very little research on lower limb outcomes during standing work has been completed.
-
•
We compared standing/seated lower limb blood flow, blood pressure and discomfort.
-
•
Standing work led to mean 77% greater lower limb blood flow and 37.2 mm Hg greater MAP.
-
•
This suggests that recommendations for stationary standing work should be tempered.
1. Introduction
Sedentary workplace sitting has become associated with musculoskeletal pain, obesity, cardiovascular disease, diabetes and other chronic health concerns (Buckley et al., 2015; Choi et al., 2010; Wilmot et al., 2012). Media coverage of the impact of sitting at work on an individual's health and wellness has led to a proliferation of height adjustable sit-stand workstations as an intervention to improve health outcomes (Callaghan et al., 2015; Karol and Robertson, 2015). To control costs for new workstations, many organizations require a medical recommendation from an employee outlining why they require a height adjustable sit-stand workstation. Research on the potential health benefits of using standing workstations can help physicians make informed decisions pertaining to sit-stand desks for patients.
Despite standing work having an association with a reduction in upper limb and trunk musculoskeletal symptoms (Callaghan et al., 2015; Husemann et al., 2009), strong causal links between occupational sitting and development of cardiovascular disease and other morbidities have not been conclusively proven (Hayashi et al., 2016; Van Uffelen et al., 2010), and seated work was noted to have no association with all-cause mortality in a recent review (Pulsford et al., 2015). It is likely that there is no extra cardio-metabolic benefit from sedentary standing work compared to sedentary sitting (Tudor-Locke et al., 2014). This has led to calls to temper recommendations for reducing seated behaviour as a means of improving health and reducing mortality (Pulsford et al., 2015). Instead, a focus on physical activity levels both in and outside the workplace form a better set of recommendations (Pulsford et al., 2015; Tudor-Locke et al., 2014). Still, standing work interventions to replace sitting remain very popular workplace health initiatives.
While there may be comfort and musculoskeletal benefits for the trunk and upper limb associated with standing work, physiological outcomes in the lower limb during prolonged standing are often overlooked. Prolonged standing is associated with increased discomfort in the lower limb (Antle et al., 2015; Messing et al., 2008, Messing et al., 2009; Reid et al., 2010), symptoms of lower limb vascular disorder (Laurikka et al., 2002; Raffetto and Khalil, 2008; Sudol-Szopinska et al., 2011; Tuchsen et al., 2005), and varicose veins (Kroeger et al., 2004; Tuchsen et al., 2005). Standing has been previously noted to cause marked increases in mean arterial pressure (MAP) in the lower limb, and it was noted that such increases may lead to peripheral arterial disease (Malhotra et al., 2002). However, these changes in lower limb blood pressure were not tracked during work tasks. Earlier work tracking brachial blood pressure changes during standing occupations did note a reduction in MAP in the upper limb (Ngomo et al., 2008), but such benefits may be offset if there are increases in MAP in the lower limb. In addition to increases in arterial pressure in the lower limb, we must also consider venous back flow and pooling in the lower limb due to gravity during standing work. Standing longer than 75% of the average workday leads to increased hydrostatic venous pressure (Kroeger et al., 2004), which may in turn lead to biochemical changes that cause venous valves and surrounding tissues to become damaged and less functional (Bergan et al., 2006; Raffetto and Khalil, 2008). Increased arterial and venous blood pressures and pooling are likely to induce discomfort, and may contribute to vascular damage and diseases that are often reported in epidemiologic literature (D'Souza et al., 2005; Tabatabaeifar et al., 2015). It is reasonable to assume that seated work would lead to reduced levels of lower limb vascular pooling and pressure, as muscle recruitment demands would be reduced or absent while sitting when compared to static standing. Therefore, less pressure from lower limb musculature would lead to reduced opposition to blood flow in the surrounding vasculature. From a lower limb vascular perspective, seated work may therefore be preferred to standing work. However, studies have yet to evaluate lower limb blood pressure and pooling changes during prolonged standing and seated work postures, and without a comparison it is difficult to include lower limb outcomes in the assessment of appropriate workplace posture interventions.
The objective of this study was to quantitatively compare changes in lower limb MAP and measures of blood pooling during a light-load repetitive upper limb work task accomplished from seated and stationary standing postures. These results are intended to inform further research and considerations for policies around workplace posture adaptations and the impact that such changes might have on physiological changes that may link to health outcomes.
2. Methods
2.1. Participants
16 participants (8 men, 8 women) were recruited for this project and completed the protocol in 2012 or 2013 at the Occupational Biomechanics Laboratory within the Jewish Rehabilitation Hospital in Laval, Quebec. The exclusion criteria were any history of neurological, musculoskeletal, or vascular disorders during the 3 previous years, or currently pregnant. Participants signed an informed consent form, approved by the ethics committee of the Centre for Interdisciplinary Research in Rehabilitation (CRIR) of Greater Montreal. Mean age was 32.4 years (SD = 8.7 years), mean weight was 76.2 kg (SD = 8.9), and mean height was 172.4 cm (SD = 10.7). All participants worked in sedentary desk-based occupations, and potential participants were excluded if they worked in in an occupation which required them to stand for >25% of their working time. While this sample size is not extensive, the experimental research approach allowed for high resolution data using a repeated-measures approach. Adequacy of the data collection procedures and sample size are detailed in previous publications and pilot work (Antle et al., 2013a; Antle et al., 2015; Antle et al., 2013b)
2.2. Apparatus and procedures
Participants were barefoot and outfitted with Laser Doppler Flowmetry (LDF) (floLAB Monitor, Moor Instruments, Devon, England, sampling frequency: 1080 Hz) electrodes to measure skin blood flow; one electrode was placed on the distal third of the soleus, and another over the 4th metatarsal of the foot. This measure provides indication of blood flow and pooling from arterial and venous sources. Lower limb arterial blood pressure, measured as MAP, was measured using an automated digital sphygmomanometer at the left ankle region, which has been noted as having adequate reliability and validity (MacDonald et al., 2008; Verberk et al., 2012). This measure was used to assess arterial pressures as a potential risk factor for peripheral arterial disease.
Participants completed a repetitive box-folding task as the experimental task. This task was selected because it included very light weight loads (<200 g/box), and it would be representative of light repetitive work in both office and industrial work contexts. Participants performed this task during two randomly assigned sessions on separate days within a 2-week timeframe; one session in the seated posture and one in a standing posture. Participants practiced the box-folding task for 10 min prior to beginning the standardization procedure. After a 5-minute rest period following the practice session, participants were instrumented and reference levels for each measure were taken. Baseline measures for blood flow and blood pressure were taken in the seated position, after the subject was seated for 5 min in a chair, with their back and feet supported.
After the standardization procedures, a comfortable work posture was determined. A work surface was placed in front of the participants and adjusted to their knuckle height, based on workstation design guidelines for non-precision work in both standing and seated positions. (Kromer and Grandjean, 2005). The participants then began the experimental work task. For both the standing and seated postures, the task required participants to construct one box every 9 s during four, 8.5 minute work bouts, totaling 34 min. Participants reached for individual pieces of cardboard placed 30 cm to their left, moved it in front of them, folded it into a box, and placed the completed box on a line 30 cm from the near edge of the work table. For standing work, we attempted to control for the effect of different levels of stepping and movement between participants by setting the task to be a stationary standing task. Participants were instructed that while they could shift their weight distribution between the feet at will, they could not move their feet or lift them from their set standing position during the 34 min of work. After each 8.5 minute work bout, the participants were asked to stop working and remain static for 30s, with both arms abducted 45°, to allow collection of vascular data. Movement of the feet was also not allowed during these collection periods. Participants rated their level of reported lower limb discomfort using a 10-point visual analog scale with rooted verbal anchors, which was included in previous publications (Antle et al., 2015).
2.3. Data analysis
Data collected from the LDF at each collection period were normalized to the levels measured during the seated standardization trial. After normalization, the data were integrated over non-overlapping 3s windows for the 30s time series. The ten 3s windows were averaged to attain one value representing blood flow accumulation levels, which would be analogous to accumulation, for each of the work bouts. Ankle blood pressures were reported using the mean arterial pressure (MAP).
Changes in blood flow and blood pressure were assessed using repeated measures ANOVAs with two within-subject factors: Posture and Time. Post-hoc tests (Tukey) were used to identify time(s) when outcomes significantly changed from their time 1 values. Changes in discomfort in the lower limb were assessed using Friedman ANOVAs. Mann-Whitney tests were used as post-hoc tests to determine where significant postural and time-based changes occurred.
3. Results
3.1. Lower limb vascular outcomes
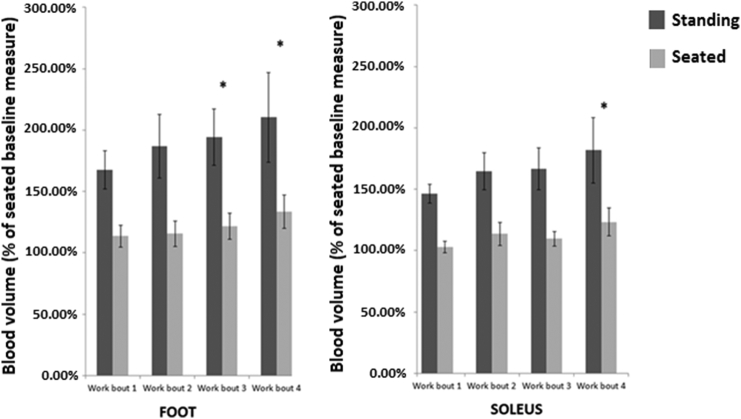
There were significant effects for both Posture and Time for LDF measures of blood flow/volume collected at both the soleus and the foot (Table 1). The foot LDF measures showed significant increases from work bout 1 during work bouts 3 and 4; for the soleus, a significant increase from work bout 1 was found after work bout 4. In the standing condition, the average foot and soleus blood flow accumulation during the final work bout was 77% and 55% higher, respectively, than the final seated work bout (Fig. 1).
Table 1.
Summary of results from ANOVAs with Time and Posture as within-subjects factors*. Data was collected from the Occupational Biomechanics Laboratory within the Jewish Rehabilitation Hospital in Laval, Quebec in 2012/2013.
| Measure | Posture | Time | Posture × time | |
|---|---|---|---|---|
| Vascular | LDF foot | F(1,15) = 12.55, p-0.003⁎ | F(3,45) = 4.58, p = 0.007⁎ | F(3,45) = 0.457, p = 0.714 |
| LDF soleus | F(1,15)-13.52, p-0.002⁎ | F(3,45)-4.43, p-0.008⁎ | F(3,45)-0.276, p-0.843 | |
| MAP | F(1,15)-190.34, p < 0.00001⁎ | F(3, 45)-2.31, p = 0.089 |
F(3,45)-5.26, p = 0.0034⁎ |
|
| Discomfort | Lower limb | Friedman ANOVA-78.69 p < 0.001⁎ | – | – |
Denotes p < 0.05.
Fig. 1.
Change in lower limb LDF accumulation measures, expressed as a percentage of baseline seated values. Data was collected from the Occupational Biomechanics Laboratory within the Jewish Rehabilitation Hospital in Laval, Quebec in 2012/2013.
*Denotes a significant time-based change from baseline. There were main posture effects.
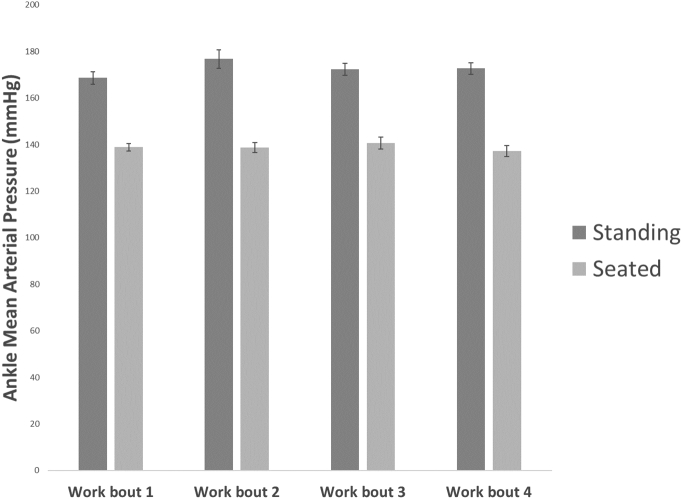
There was a significant ‘Posture × Time’ interaction effect and a significant Posture effect for MAP (Table 1). The post-hoc tests showed that time-based changes occurred only in the standing posture, where MAP increased after work bout 2, slightly decreased after work bout 3, and increased again after work bout 4. At the end, MAP was, on average, 37.2 mmHg higher when standing than when seated (Fig. 2).
Fig. 2.
Change in lower limb mean arterial blood pressure. Data was collected from the Occupational Biomechanics Laboratory within the Jewish Rehabilitation Hospital in Laval, Quebec in 2012/2013.
*Denotes a significant time-based change from baseline. There were main posture effects.
3.2. Lower limb discomfort
There was a significant effect of Posture on lower limb discomfort (Table 1). Post-hoc tests showed that time-based effects also existed during the standing condition, with increases after each work bout. Of the 16 participants, while standing, 13 reported some lower limb discomfort. While seated, 1 reported some lower limb discomfort.
4. Discussion
4.1. Seated and standing work impacts on lower limb vascular outcomes
Both sitting and stationary standing work lead to increases in vascular pooling at approximately 26 min of exposure (main Time effect), but the indicators of vascular pooling were greater in the stationary standing condition. Discomfort was also higher in the stationary standing condition. Previous work had noted that increases in foot blood flow/pooling have association with the development of lower limb discomfort during stationary standing work (Antle and Côté, 2013; Antle et al., 2013b), and this may underscore the lack of discomfort in the seated posture where blood pooling levels are much lower. Given the static nature of this task and the impact of gravity without dynamic movements to aid in venous return, the source of the blood pooling is likely to have a large venous back flow component, which may relate to the noted increases in peripheral venous issues in standing occupations (D'Souza et al., 2005; Tabatabaeifar et al., 2015).
The results also demonstrated higher MAP in the lower limb, and greater increases in MAP over time in the stationary standing condition. This may be a consequence of increased vascular pooling and sustained muscular pressure, and serve as an indicator of vascular tissue stress that underlies risk of peripheral arterial disease. MAP increased from work bout 1 to 2, decreased from work bout 2 to 3, before following an additional increase towards the end of the stationary standing session. This might be interpreted as an indicator of postural compensatory strategies as a means of reducing peripheral vascular stresses. Previous research on stationary standing work provided evidence showing that increased postural shifting was associated with a decrease in MAP, suggesting increases in postural shifting may be a strategy to promote venous return (Antle and Côté, 2013).This study offers supports that indicators of vascular damage and risk of vascular disease are specific to this standing posture, since no statistically significant time-related changes in MAP and lower limb discomfort were observed in the seated condition.
4.2. Potential considerations for workplace posture recommendations
Back and shoulder region musculoskeletal pain is a common reason for employees to request sit-stand workstations and to move away from sitting postures (Grunseit et al., 2013). However, any benefits for the upper body may be offset by the potential consequences for the lower limb. It is possible that without dynamic actions of lower limb agonist/antagonist muscles during walking and body movement, there is a decreased ability to move pooled blood in the lower limb back up the leg against gravity.
For physicians and those who provide guidance on work posture changes in relation to health, it seems logical that patients/employees who have pre-existing peripheral vascular issues should avoid prolonged bouts of static standing work. Excessive standing beyond 30 continuous minutes in a workplace may aggravate these conditions when compared to seated work, based on the outcomes seen in this experimental study. Intermittent standing for bouts of approximately 15 min have been recommended as a means of improving back comfort in office-based tasks, with durations exceeding 15 min and without appropriate breaks in standing time leading to standing-related back discomfort (Callaghan et al., 2015). From the present study, we see that standing durations that exceeded 2 work bouts (17 min) began to lead to unwanted lower limb vascular and discomfort outcomes that continued until the end of the work sessions at 34 min. A recent study found that there were no increases in lower limb discomfort from implementation of a standing workstation following education and training on avoiding standing work (Danquah et al., 2017). While they did not report on their suggested postural rotation scheduling or strategies specifically, this may speak to the importance of proper training when attempting to avoid seated work consequences. Based on previous research, and the results presented in this manuscript continuous stationary standing without seated or movement breaks should not exceed 15–30 min, however more research on dose-response relationships for work postures are clearly needed.
In industrial work, where stationary standing work can be required for much longer periods (for example: on production lines, cashier stations and service stations), the project demonstrates some evidence for negative lower limb vascular and discomfort consequences that should be considered carefully, especially given the longer durations of exposure and cumulative standing time and its association with lower limb discomfort (Messing et al., 2008). Adaptation of this work to allow intermittent seating, or potentially walking periods might be recommended by health care providers.
Many private companies and public institutions have launched programs to combat sedentary behaviour among public sector employees by providing standing desks and the ability to track time standing. These initiatives, while promoting the negative health effects of sedentary sitting behaviors, ignore the potential implications of standing for extended periods of time beyond what would be comfortable for most individuals (15–30 min). In may be more appropriate that any such initiative involve the promotion of a variety of workplace postures with proper rotation between them, and the promotion of regular workplace movement (Castillo-Retamal and Hinckson, 2011; Jancey et al., 2016; Tudor-Locke et al., 2014). Avoiding prolonged stationary standing or sitting by including regular movement breaks, and promoting leisure time physical activity is likely a better alternative to a reliance on primarily using static sitting or standing work postures (Holtermann et al., 2012).
4.3. Future research and policy directions related to health outcomes and working posture
This project suggests that prolonged standing may present some risks for negative lower limb vascular and discomfort outcomes, and that recommendations for prolonged standing work to benefit health outcomes may need to be tempered. However, this project included asymptomatic participants who completed sedentary work. Results for physiological changes during standing and seated postures will likely need to be investigated for populations who have different cardiovascular risk profiles, including those with hypertension, smokers and aging workers. Furthermore, studies with workers who use a greater variety of postures and movement levels throughout the workday should also be investigated.
Another tool to combat sedentary workplace behavior is the implementation of active workstations, such as treadmill or pedal desks, which promote movement throughout the day without decreasing the amount of time spent at a desk (Tudor-Locke et al., 2014). Active workstations increase the daily energy expenditure with minimal disruption to the work day (Cao et al., 2016). Studies have found active workstations decrease job performance, particularly in older adults, but overall there seems to be little overall impact on efficiency (Straker et al., 2009). The challenge of these stations is how to maintain adherence to proper usage (Black et al., 2015). Future research should look at the long-term changes to sedentary behavior after the implementation of movement based workstations and how to increase adherence.
Changing the physical environment and layout of the office in a way that induces more worker displacements through the work day is another potential way to combat sedentary behavior (Jancey et al., 2016). Changing the physical environment has the potential advantage of relying less on worker motivation to initiate movement, thus creating more sustainable change. Currently there is insufficient research to draw any conclusions on the efficacy of changing the environment. Further research is necessary to understand the effect of changing the environment to promote movement in the workplace.
4.4. Limitations of this project
One limitation of this study was the small sample size of 16 participants. This sample may not be representative of the general population and caution is needed when applying these results. However, this study allowed tracking of specific markers for vascular changes throughout an extended work simulation, which is novel. With this study in place, and now with a procedural model to follow, larger studies with more participants may now be possible. Also, by repeating the protocol with the same participants across both standing and seated posture conditions, it allows for stronger and more valid analysis of the data.
Another recognized limitation of the experiment is that the experimental study did not allow for intermittent steps and movement during the work task, while a real-world workplace using a standing workstation would allow for steps, perhaps some seated breaks, and perhaps shifting of leg posture through the work day. These small breaks and movements may offset some of the vascular effects seen in this experiment during real-world work. Yet, the amount of movement and dynamic nature of the steps in a workplace would remain limited by a need to remain in a relatively stationary position during productive work tasks. Therefore, the general physiological effects found in this experiment would very likely apply to the workplace as well.
We also acknowledge that the experiment, having been conducted over 34 min, does not give an indication of the cumulative effects which may be seen across full work days. Future studies should aim to track these outcomes over an entire work shift, and potentially measure additive effects of repeated standing bouts, and the potential impact of rotations between sitting and standing on vascular outcomes.
4.5. Conclusions
Combating sedentary behavior in the workplace is a complex and difficult challenge, and standing work postures are often used as an intervention in the workplace. However, this research notes that stationary standing work postures increase discomfort, MAP and blood pooling in the lower limb, when compared to static seated work. Based on these outcomes, recommendations for individuals to use exclusively standing, or high proportions of the work day at a standing workstation, as a means of dealing with sedentary work places or musculoskeletal discomfort should be tempered. While this study offers a preliminary set of insights using an experimental research approach, further workplace experimental investigations and epidemiologic studies are warranted. Still, physicians and health advocates that provide recommendations and guidance on workstation changes should consider the impacts on the lower limb as well as the back and upper limb. Future directions for research and workplace modifications should focus on the long-term benefits of active workstations and changes to the workplace environment. The long-term effects on both workplace efficacy and the adherence of workers to usage also warrant investigation.
Declarations
Ethics approval and consent to participate/publish
This project was reviewed and approved for human investigations by the Centre for Interdisciplinary Research in Rehabilitation (CRIR) of Greater Montreal. No personal information or patient data were obtained, only biometric outcomes that were coded without identifying information, and raw signals stored and processed with encryption.
Participants signed an informed consent form, approved by the ethics committee, noting that summary data would be published without reference to their identity or individual information.
Availability of data and materials:
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Author contributions
DA, PhD – DA was the lead author on the paper and was the primary individual responsible for methodology development, data collection and data processing. Signal processing procedures, statistical analysis and production of the methodological and results sections of this manuscript were his primary role, which mentorship by J. Côté. He also made contributions to the introduction and discussion sections.
LC, BSc,– LC was a volunteer research student assigned to this project and assisted with preparation of the data using the signal processing approaches developed by DA and JC. LC also completed literature review synthesis and assisted with production of the introduction and discussion sections of the paper.
MF, BSc – MF was also a volunteer research student assigned to this project and assisted with preparation of the data using the signal processing approaches developed by DA and JC. MF also completed literature review synthesis and assisted with production of the introduction and discussion sections of the paper.
LM, OT(D) – LM is an industrial health consultant and her experiences in knowledge translation and application of health research in industry were useful to interpreting the data and its applications. LM helped with review and planning of the discussion section, and provided editing and feedback on the manuscript.
JC, PhD – JC is the director of the laboratory where the research was conducted, and oversaw this project. Julie contributed to the development and refinement of the methodological approaches, data analysis and statistical approaches used in the project. Julie also contributed to the editing and review of the final manuscript.
Acknowledgements
We would like to acknowledge the financial support of the Institut de recherche Robert-Sauvé en santé et en sécurité du travail (IRSST) in the form of a PhD fellowship (http://www.irsst.qc.ca/en/index.html).
References
- Antle D.M., Côté J.N. Relationships between lower limb and trunk discomfort and vascular, muscular and kinetic outcomes during stationary standing work. Gait Posture. 2013;37:615–619. doi: 10.1016/j.gaitpost.2012.10.004. [DOI] [PubMed] [Google Scholar]
- Antle D.M., Vézina N., Côte J.N. Whistler Conference Centre; Whistler, BC, Canada: 2013. An Investigation of Vascular Outcomes and Reports of Discomfort in a Sit-Standing Work Posture, Association of Canadian Ergonomists 44th Annual Conference - From Sea to Sky: Expanding the Reach of Ergonomics. [Google Scholar]
- Antle D.M., Vézina N., Messing K., Côté J.N. Development of discomfort and vascular and muscular changes during a prolonged standing work task. Occup. Ergon. 2013;11:21–33. [Google Scholar]
- Antle D.M., Vézina N., Côté J.N. Comparing standing posture and use of a sit-stand stool: analysis of vascular, muscular and discomfort outcomes during simulated industrial work. Int. J. Ind. Ergon. 2015;45:98–106. [Google Scholar]
- Bergan J.J., Schmid-Schonbein G.W., Smith P.D.C., Nicolaides A.N., Boisseau M.R., Eklof B. Mechanisms of disease: chronic venous disease. N. Engl. J. Med. 2006;355:488–498. doi: 10.1056/NEJMra055289. [DOI] [PubMed] [Google Scholar]
- Black N., Fortin A.-P., Handrigan G.A. Postural and perception variations when using manually adjustable and programmable sit–stand workstations in an emergency call center. IIE Trans. Occup. Ergon. Hum. Factors. 2015;3:127–138. [Google Scholar]
- Buckley J.P., Hedge A., Yates T. The sedentary office: a growing case for change towards better health and productivity. Expert statement commissioned by Public Health England and the Active Working Community Interest Company. Br. J. Sports Med. 2015;49:353–1353. doi: 10.1136/bjsports-2015-094618. [DOI] [PubMed] [Google Scholar]
- Callaghan J.P., De Carvalho D., Gallagher K., Karakolis T., Nelson-Wong E. Is standing the solution to sedentary office work? Ergon. Des. Q. Hum. Factors Appl. 2015;23:20–24. [Google Scholar]
- Cao C., Liu Y., Zhu W., Ma J. Effect of active workstation on energy expenditure and job performance: a systematic review and meta-analysis. J. Phys. Act. Health. 2016;13:562–571. doi: 10.1123/jpah.2014-0565. [DOI] [PubMed] [Google Scholar]
- Castillo-Retamal M., Hinckson E.A. Measuring physical activity and sedentary behaviour at work: a review. Work-A J. Prev. Assess. Rehabil. 2011;40:345–357. doi: 10.3233/WOR-2011-1246. [DOI] [PubMed] [Google Scholar]
- Choi B., Schnall P.L., Yang H. Sedentary work, low physical job demand, and obesity in US workers. Am. J. Ind. Med. 2010;53:1088–1101. doi: 10.1002/ajim.20886. [DOI] [PubMed] [Google Scholar]
- Danquah I.H., Kloster S., Holtermann A., Aadahl M., Tolstrup J.S. Effects on musculoskeletal pain from “Take a Stand!” - a cluster-randomized controlled trial reducing sitting time among office workers. Scand. J. Work Environ. Health. 2017;43:350–357. doi: 10.5271/sjweh.3639. [DOI] [PubMed] [Google Scholar]
- D'Souza J.C., Franzblau A., Werner R.A. Review of epidemiologic studies on occupational factors and lower extremity musculoskeletal and vascular disorders and symptoms. J. Occup. Rehabil. 2005;15:129–165. doi: 10.1007/s10926-005-1215-y. [DOI] [PubMed] [Google Scholar]
- Grunseit A.C., Chau J.Y.-Y., Van der Ploeg H.P., Bauman A. “Thinking on your feet”: a qualitative evaluation of sit-stand desks in an Australian workplace. BMC Public Health. 2013;13 doi: 10.1186/1471-2458-13-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi R., Iso H., Cui R.Z., Tamakoshi A., Grp J.S. Occupational physical activity in relation to risk of cardiovascular mortality: the Japan Collaborative Cohort Study for Evaluation for Cancer Risk (JACC Study) Prev. Med. 2016;89:286–291. doi: 10.1016/j.ypmed.2016.06.008. [DOI] [PubMed] [Google Scholar]
- Holtermann A., Hansen J., Burr H., Søgaard K., Sjøgaard G. The health paradox of occupational and leisure-time physical activity. Br. J. Sports Med. 2012;46:291–295. doi: 10.1136/bjsm.2010.079582. [DOI] [PubMed] [Google Scholar]
- Husemann B., Von Mach C.Y., Borsotto D., Zepf K.I., Scharnbacher J. Comparisons of musculoskeletal complaints and data entry between a sitting and a sit-stand workstation paradigm. Hum. Factors. 2009;51:310–320. doi: 10.1177/0018720809338173. [DOI] [PubMed] [Google Scholar]
- Jancey J.M., McGann S., Creagh R., Blackford K.D., Howat P., Tye M. Workplace building design and office-based workers' activity: a study of a natural experiment. Aust. N. Z. J. Public Health. 2016;40:78–82. doi: 10.1111/1753-6405.12464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karol S., Robertson M.M. Implications of sit-stand and active workstations to counteract the adverse effects of sedentary work: a comprehensive review. WORK-A J. Prev. Assess. Rehab. 2015;52:255–267. doi: 10.3233/WOR-152168. [DOI] [PubMed] [Google Scholar]
- Kroeger K., Ose C., Rudofsky G., Roesener J., Hirche H. Risk factors for varicose veins. Int. Angiol. 2004;23:29–34. [PubMed] [Google Scholar]
- Kromer K., Grandjean E. 2005. Fitting the Task to the Human. A Textbook of. [Google Scholar]
- Laurikka J.O., Sisto T., Tarkka M.R., Auvinen O., Hakama M. Risk indicators for varicose veins in forty- to sixty-year-olds in the Tampere varicose vein study. World J. Surg. 2002;26:648–651. doi: 10.1007/s00268-001-0283-1. [DOI] [PubMed] [Google Scholar]
- MacDonald E., Froggatt P., Lawrence G., Blair S. Are automated blood pressure monitors accurate enough to calculate the ankle brachial pressure index? J. Clin. Monit. Comput. 2008;22:381–384. doi: 10.1007/s10877-008-9146-8. [DOI] [PubMed] [Google Scholar]
- Malhotra A., Cohen D., Syms C., Townsend R.R. Blood pressure changes in the leg on standing. J. Clin. Hypertens. 2002;4:350–354. doi: 10.1111/j.1524-6175.2002.00767.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messing K., Tissot F., Stock S.R. Distal lower-extremity pain and work postures in the Quebec population. Am. J. Public Health. 2008;98:705–713. doi: 10.2105/AJPH.2006.099317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messing K., Tissot F., Stock S.R. Should studies of risk factors for musculoskeletal disorders be stratified by gender? Lessons from the 1998 Quebec Health and Social Survey. Scand. J. Work Environ. Health. 2009;35:96–112. doi: 10.5271/sjweh.1310. [DOI] [PubMed] [Google Scholar]
- Ngomo S., Messing K., Perrault H., Comtois A. Orthostatic symptoms, blood pressure and working postures of factory and service workers over an observed workday. Appl. Ergon. 2008;39:729–736. doi: 10.1016/j.apergo.2007.11.004. [DOI] [PubMed] [Google Scholar]
- Pulsford R.M., Stamatakis E., Britton A.R., Brunner E.J., Hillsdon M. Associations of sitting behaviours with all-cause mortality over a 16-year follow-up: the Whitehall II study. Int. J. Epidemiol. 2015;44:1909–1916. doi: 10.1093/ije/dyv191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raffetto J.D., Khalil R.A. Mechanisms of varicose vein formation: valve dysfunction and wall dilation. Phlebology. 2008;23:85–98. doi: 10.1258/phleb.2007.007027. [DOI] [PubMed] [Google Scholar]
- Reid C.R., Bush P.M., Karwowski W., Durrani S.K. Occupational postural activity and lower extremity discomfort: a review. Int. J. Ind. Ergon. 2010;40:247–256. [Google Scholar]
- Straker L., Levine J., Campbell A. The effects of walking and cycling computer workstations on keyboard and mouse performance. Hum. Factors. 2009;51:831–844. doi: 10.1177/0018720810362079. [DOI] [PubMed] [Google Scholar]
- Sudol-Szopinska I., Bogdan A., Szopinski T., Panorska A.K., Kolodziejczak M. Prevalence of chronic venous disorders among employees working in prolonged sitting and standing postures. Int. J. Occup. Saf. Ergon. 2011;17:165–173. doi: 10.1080/10803548.2011.11076887. [DOI] [PubMed] [Google Scholar]
- Tabatabaeifar S., Frost P., Andersen J.H., Jensen L.D., Thomsen J.F., Svendsen S.W. Varicose veins in the lower extremities in relation to occupational mechanical exposures: a longitudinal study. Occup. Environ. Med. 2015;72:330–337. doi: 10.1136/oemed-2014-102495. [DOI] [PubMed] [Google Scholar]
- Tuchsen F., Hannerz H., Burr H., Krause N. Prolonged standing at work and hospitalisation due to varicose veins: a 12 year prospective study of the Danish population. Occup. Environ. Med. 2005;62:847–850. doi: 10.1136/oem.2005.020537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor-Locke C., Schuna J.M., Frensham L.J., Proenca M. Changing the way we work: elevating energy expenditure with workstation alternatives. Int. J. Obes. 2014;38:755–765. doi: 10.1038/ijo.2013.223. [DOI] [PubMed] [Google Scholar]
- Van Uffelen J.G.Z., Wong J., Chau J.Y. Occupational sitting and health risks a systematic review. Am. J. Prev. Med. 2010;39:379–388. doi: 10.1016/j.amepre.2010.05.024. [DOI] [PubMed] [Google Scholar]
- Verberk W.J., Kollias A., Stergiou G.S. Automated oscillometric determination of the ankle-brachial index: a systematic review and meta-analysis. Hypertens. Res. 2012;35:883–891. doi: 10.1038/hr.2012.83. [DOI] [PubMed] [Google Scholar]
- Wilmot E.G., Edwardson C.L., Achana F.A. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55:2895–2905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.