Abstract
This single arm prospective study assessed the impact of individualized wellness coaching intervention for primary care patients with prediabetes on self-reported changes in physical activity level and food choices. Five hundred sixty adult patients 18 years and older with prediabetes, seen in primary care clinic, were invited to participate in 12 weeks wellness coaching sessions delivered by certified coaches. Responses from questionnaires at baseline, 6 and 12 weeks were analyzed. Of 168 consented patients, 99 completed at least one coaching session; majority was elderly, female, overweight or obese. At baseline, 50% had <60 min aerobic exercise/week. At 6 and 12 weeks, average aerobic exercise time significantly increased from 117 min to 166 and 199 min respectively. Effect was sustained at 24 weeks. Success in making healthy eating choices also statistically improved from baseline. Significant effects on both activity level and eating behavior persisted even after adjusting for age, sex and baseline glucose/A1c values. Secondary outcomes of self-efficacy and quality of life likewise showed significant improvement. Results suggest that integration of wellness coaching in primary care practice among individuals at high risk for diabetes is feasible and may be useful as part of diabetes prevention management strategies in target populations. Future randomized clinical trials are needed to further explore this issue.
Keywords: Wellness coaching, Primary care, Prediabetes, Preventive health, Health behavior
Highlights
-
•
Wellness coaching alone as an effective preventive strategy in patients with prediabetes is proposed.
-
•
It can be incorporated in primary care practice.
-
•
A 12 weeks session resulted in improved physical activity and healthy eating behavior.
-
•
Self-efficacy and quality of life were also increased with coaching.
-
•
Significant changes were seen in 6 weeks with sustained effect up to 24 weeks.
1. Introduction
About 37% of U.S. adults have prediabetes based on fasting glucose or hemoglobin A1C levels (National Diabetes Statistics Report, 2014). These individuals are at high risk of progressing to type 2 diabetes; about 70% are expected to develop diabetes within 10 years (Tabak et al., 2012). Our recent study which involved a cohort of 10,000 individuals with prediabetes, showed an estimated incidence rate of progression to diabetes of 40.24 per 1000 person years at 5 years (DeJesus et al., 2017).
Fortunately, progression of prediabetes to diabetes may be prevented or delayed with moderate weight loss (5–7% total body weight) achieved through positive lifestyle interventions (Knowler et al., 2002; Perreault et al., 2014; Stevens et al., 2015). The US Diabetes Prevention Program (DPP), the largest study conducted to date, reported a 58% risk reduction in diabetes onset after interventions aimed at weight loss, dietary change and increased physical activity (Knowler et al., 2002). However, given the high recidivism in weight management, the challenge is to enable individuals to initiate and maintain healthy lifestyle changes.
Wellness coaching is a novel approach to diabetes prevention that offers a focused self-management support program. Health education alone may not sufficiently initiate and sustain long term behavioral change; there are situations where wellness coaches can better enhance motivation, and guide patients towards behavior change. As a patient-centered intervention, wellness coaching has been shown to achieve sustained behavioral change and clinical outcomes (McGowan, 2011; Tang et al., 2012).
Previous research has demonstrated that when used in chronic disease management, wellness coaching enhances self-management skills in patients with diabetes and helps reduce readmissions in those with chronic obstructive lung disease (Wong-Rieger and Rieger, 2013; Benzo et al., 2016). In a review of 15 randomized health coaching interventions, six were able to demonstrate significant improvements in targeted behaviors such as physical activity and medication adherence (Olsen and Nesbitt, 2010). A study conducted by Clark and colleagues concluded that wellness coaching was associated with improvement in 3 areas of psychosocial functioning: quality of life, mood and perceived stress (Clark et al., 2014). Participants also improved their self-reported health behaviors, and goal setting skills (Clark et al., 2016). Integrating wellness coaching within primary care practice has been found to be a feasible model for diabetes care which can be done without significant additional resources (Liddy et al., 2014). It has also been shown to be well received by patients and physicians in primary care setting (Neuner-Jehle et al., 2013).
While wellness coaching conducted in health care settings has been shown to be effective in chronic disease and weight management, (Wong-Rieger and Rieger, 2013; Benzo et al., 2016; Schmittdiel et al., 2017) its use among patients who do not have a chronic disease but who are at high risk for it has not been widely explored. The DPP focused on a well-structured curriculum that included supervised physical activity sessions supported by individual case managers who functioned as “lifestyle coaches”(Knowler et al., 2002). As health care systems in the U.S. transition to population health care delivery approaches, there is need to create programs that will help prevent chronic diseases progression among high risk population group without creating additional burden to practice and available resources. Therefore, this project's aim was to examine the feasibility of engaging our high risk patients towards healthy lifestyle behavior solely with wellness coaching. We conducted a cohort study to assess whether an individualized 12-week wellness coaching intervention would improve self-reported changes in physical activity level and food choices among primary care patients with prediabetes. We hypothesized that a 12-week wellness coaching intervention would result in positive lifestyle changes demonstrated by increased self-reported level of physical activity and healthier food choices.
2. Design
2.1. Study population
Approximately 10% of the population served by our primary care practice has prediabetes (DeJesus et al., 2017). In this prospective study, five hundred sixty patients with prediabetes, paneled to a provider in Primary Care Internal Medicine (PCIM), in Mayo Clinic Rochester, were invited to participate through mailed-out recruitment letters. Inclusion criteria were: adults 18–80 years of age with prediabetes based on the American Diabetes Association's definition of fasting plasma glucose 100 to <126 mg/dL or HbA1c 5.7–6.4% (Diagnosis and classification of diabetes mellitus, 2013) as the most recent value in the electronic medical record within 12 months of recruitment date, able to participate fully in all aspects of the study and able to provide written informed consent. Laboratory result values from blood draws obtained in the inpatient setting or during pregnancy were excluded. Also excluded were: patients with a diagnosis of diabetes, based on two documented ICD-9 codes for diabetes at least 30 days apart in the past five years, individuals who did not speak and read English, were institutionalized, had cognitive impairment, had an active untreated clinically significant psychiatric condition (psychosis, bipolar disorder, or depression) or had newly diagnosed clinical depression based on Physician Health Questionnaire (PHQ-9) score ≥10. The PHQ-9 is a well validated screening tool for depression in the general population with an accepted diagnostic cut-off point of 10 (Gilbody et al., 2007; Moriarty et al., 2015).
Baseline questionnaires and HIPAA authorization forms were mailed with the recruitment letters; consented participants were requested to complete and mail them back. A Clinical Research Coordinator (CRC) contacted invited patients who did not opt out to verify completion of study questionnaires including the PHQ-9 and initiate enrollment. Patients with score of 10 or higher who were not actively being followed for depression or had not been previously diagnosed with depression, were instructed by the CRC to meet with the study physician for clinical assessment and referral for treatment as appropriate. If they refused, they were recommended to contact their primary care physician. Once inclusion criteria were met, participants were scheduled for an initial wellness coaching session. The study was approved by the institutional review board of the Mayo Clinic Rochester.
2.2. Intervention
Four certified wellness coaches delivered the intervention. Wellness coaches in this project had at least a four year degree and had received training and certification from the Mayo Clinic Wellness Coaching Training Program. Training included skill building in goal setting, communication skills, motivational interviewing techniques and professional ethics (Neuner-Jehle et al., 2013). Wellness coaches learned a strength based approach which incorporated the 5 E's: engage, explore, envision, experiment and evolve. The wellness coaching program consisted of 12 sessions which were completed within 16 weeks and were conducted at the participants' primary clinic site. The coaches were asked to complete a fidelity checklist during each session; this ensured intervention standardization. The checklist included agenda setting, progress review, collaborative problem-solving, engaging education, setting/refining goals, teaching back and completing intervention on time. While coaching was individualized and centered on participants' wellness goals, the coaches were requested to primarily address goals related to physical activity, healthy eating behavior or both. This was specified under “engaging education” step in the checklist. The initial wellness coaching session was conducted face-to-face to assess the participant's strengths, motivation to change and perceived barriers. Participants then determined their preferred approach for the subsequent visits: in-person or telephone-based wellness coaching. In-person coaching sessions were all conducted within the primary care clinic setting which enabled the coaches to interface with the primary care providers. Consistent with clinical practice, wellness coaches collected adherence data throughout the study period, including attendance and discussion points. Participants needed to complete 6 of 12 wellness coaching sessions to be classified as study completer.
3. Methods
3.1. Data collection
Study participants were asked to complete mailed out study questionnaires before their first wellness coaching session (baseline, week 0), at 6 weeks, at the end of wellness coaching (12 weeks) and at 24 weeks. A satisfaction survey was also administered after the last wellness coaching session.
3.2. Study questionnaires
The Stanford Patient Education Research Center 6-item exercise behavior questionnaire was used to measure both aerobic and combination stretching/strengthening exercise (Lorig et al., 1996; Stanford chronic disease self-management education program, n.d.). Item 1 asked how much total time the past week were spent doing non-aerobic exercises (stretching, weight lifting, range of motion) and items 2–6 focused on aerobic exercises (walking, swimming, bicycling, exercise equipment). Responses were ranked as 0 (none), 1 (<30 min/week), 2 (30–60 min/week), 3 (1–3 h/week), and 4 (>3 h/week). For scoring, each rank was converted to mean number of minutes: 0 (none), 15 (<30 min/week), 45 (30–60 min/week), 120 (1–3 h/week) and 180 (>3 h/week).
A five item questionnaire on Current Health Behavior was adapted from a questionnaire used in the Happy Heart Study at Mayo Clinic (Thomas et al., 2010). The first item asked patients to rate their current general health (poor to excellent), the next 3 items asked them to rate their confidence level in their ability to make healthy eating choices and exercise regularly on a scale of 1–9 (not at all confident to very confident) and how successful (on scale of 1–9) they were within the past week in making healthy choices (not at all successful to very successful). The 5th item inquired how often they engaged in physical activity “long enough to work up a sweat” during a typical week (1 = often, 2 = sometimes, 3 = never/rarely).
A validated 5-item self-efficacy scale consisting of 5-point scales ranging from 0 (disagree very much) to 4 (agree very much) was used to measure changes in self-efficacy (Lee et al., 2008). Items scored were: having confidence in ability to have a positive effect on one's health, being able to set some definite goals to improve one's health, having been able to meet set goals to improve one's health, actively working to improve one's health and feeling in control of how and what is learned about one's health.
Quality of life assessment was done using a Mayo Clinic tool that asks adults to rate their level of functioning on scale from 0 (as bad as it can be) to 10 (as good as it can be). The six item questionnaire inquires about overall quality of life, and then covers the five domains of quality of life: mental, physical, emotional, social, and spiritual well-being (Locke et al., 2007). Items have been validated in a sample of 9295 individuals (Singh et al., 2014) and in a sample of over 13,000 worksite wellness members (Clark et al., 2011). Copies of the questionnaires are included as appendices to this manuscript.
3.3. Statistical analysis
Data were summarized as means and standard deviations (SD) for continuous variables and frequencies and percentages for categorical variables. Changes in each outcome from baseline were summarized by effect sizes (absolute difference from baseline divided by the SD) for each time period. Wilcoxon-signed ranked tests were used to compare each follow-up time period (6, 12 and 24 week) to the baseline (referent) time period for each outcome. Additional Wilcoxon-signed ranked tests were used to compare consecutive time periods with the previous time period. Generalized estimating equations (GEE) logistic regression models were used to assess changes over time for each outcome. Each outcome was categorized into a binary variable using the baseline mean level as the cut point. For sensitivity analysis, associations were assessed using GEE linear regression on the untransformed data. GEE, along with robust standard errors (SE), was utilized to control for correlated outcomes within each patient. Multivariable models were used to adjust for baseline age, sex and glucose status.
P-values of ≤0.05 were considered statistically significant. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC).
4. Results
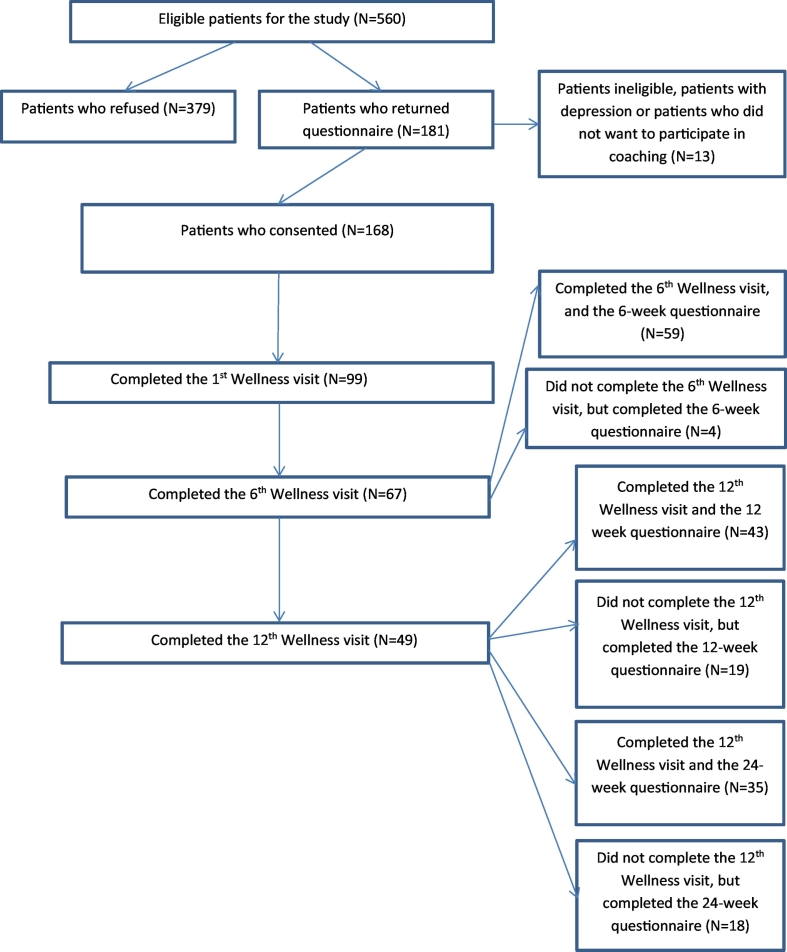
Of the 560 patients who were invited to participate in the study through mailed out recruitment letters, 168 (30%) consented. Overall, 99 (18% of total, and 59% of those expressing interest in the study) were eventually enrolled in the wellness coaching program and completed at least one session (Fig. 1). There were 67 participants (68% completion rate) who completed at least 6 sessions. Study participants and study non-participants did not differ significantly in age, sex, baseline glucose, or hemoglobin A1C level. Demographic characteristics between those who completed at least 6 sessions and those who did not were also not statistically different (data not shown).
Fig. 1.
Flow diagram.
Table 1 shows the demographic characteristics of participants who completed at least 1 wellness coaching session. Median participant age was 67 years, with 56% being 65 years and older. Majority were white, either overweight or obese, and married or lived with a partner. Fifty percent were retired; only 5% were smokers. The level of literacy among participants was high based on extreme confidence in completing medical forms. When participants were asked at baseline “during a typical week, how often do you engage in any regular activity long enough to work up a sweat”, 88% responded sometimes, rarely or never. In addition, participants engaged in stretching/strengthening activities at baseline for a mean of 26.5 min/week; about 117.7 min/week was devoted to aerobic exercise such as swimming, walking, or bicycling. The mean confidence level in “ability to engage in regular exercise and make healthy eating choices” was moderately high (5.9 and 6.5 on a scale of 1–9). However, the mean success rate in actually making healthy eating choices was lower at 5.5. Baseline composite scores for both self-efficacy and quality of life scores were also high (Table 2).
Table 1.
Demographic and baseline characteristics of Wellness Coaching participantsa.
| Age | |
| 18–<40 | 5, 5.1% |
| 40–<65 | 39, 39.4% |
| ≥65 | 55, 55.6% |
| BMI | |
| Under/normal weight | 20, 22.2% |
| Overweight | 32, 35.6% |
| Obese | 38, 42.2% |
| Marital Status | |
| Married/living together | 74, 75.5% |
| Single/widowed/divorced | 24, 24.5% |
| Race/ethnicity | |
| White | 93, 93.9% |
| Non White | 6, 6.1% |
| Education | |
| 12–16 years | 67, 68.4% |
| >16 years | 31, 32.6% |
| Employment | |
| Employed | 38, 38.4% |
| Retired | 50, 50.5% |
| Other | 11, 11.1% |
| Smoking status | |
| Yes | 5, 5.1% |
| No | 94, 94.9% |
| Confidence filling out form | |
| Median (Q1, Q3) | 11(11,11) |
Participant defined as anyone who had at least one Wellness visit.
Table 2.
Changes in exercise, healthy eating and quality of life.
| Baseline (N = 99) | 6 weeks (N = 63) | 12 weeks (N = 62) | 24 weeks (N = 53) | |
|---|---|---|---|---|
| Stretching or strengthening exercises | ||||
| Mean (SD) | 26.5 (48.6) | 48.6 (58.9) | 64.8 (56.8) | 54.2 (49.4) |
| Effect sizea | – | 0.5 | 0.8 | 0.6 |
| P-valueb | Reference | 0.0007 | <0.0001 | <0.0001 |
| P-valuec | – | – | 0.017 | 0.2561 |
| Aerobic exercise | ||||
| Mean (SD) | 117.7 (115.2) | 166.7 (116.3) | 199.1 (118.1) | 186.5 (136.7) |
| Effect sizea | – | 0.4 | 0.7 | 0.6 |
| P-valueb | Reference | 0.0063 | <0.0001 | 0.0011 |
| P-valuec | – | – | 0.0052 | 0.5524 |
| Self-efficacy (composite score) | ||||
| Mean (SD) | 63.9 (17.2) | 84.4 (12.5) | 83.3 (12.3) | 81.9 (12.8) |
| Effect sizea | – | 1.2 | 1.1 | 1.0 |
| P-valueb | Reference | <0.0001 | <0.0001 | <0.0001 |
| P-valuec | – | – | 0.7090 | 0.9308 |
| Quality of life (composite score) | ||||
| Mean (SD) | 73.3 (14.6) | 79.8 (12.8) | 83.8 (9.3) | 80.9 (13.8) |
| Effect sizea | – | 0.4 | 0.7 | 0.5 |
| P-valueb | Reference | 0.0003 | <0.0001 | <0.0001 |
| P-valuec | – | – | 0.0320 | 0.2218 |
| Healthy eating | ||||
| Mean (SD) | 6.5 (1.6) | 7.2 (1.3) | 7.5 (1.2) | 7.5 (1.3) |
| Effect sizea | – | 0.4 | 0.6 | 0.6 |
| P-valueb | Reference | 0.0006 | 0.0001 | <0.0001 |
| P-valuec | – | – | 0.0277 | 0.5526 |
| Regular exercise | ||||
| Mean (SD) | 5.9 (2.2) | 7.2 (1.4) | 7.5 (1.3) | 7.1 (1.6) |
| Effect sizea | – | 0.6 | 0.7 | 0.5 |
| P-valueb | Reference | <0.0001 | 0.0052 | 0.0006 |
| P-valuec | – | – | 0.0386 | 0.1505 |
| Successful snack choices | ||||
| Mean (SD) | 5.5 (1.7) | 6.7 (1.4) | 7.0 (1.1) | 7.0 (1.1) |
| Effect sizea | – | 0.7 | 0.9 | 0.9 |
| P-valueb | Reference | <0.0001 | 0.0458 | <0.0001 |
| P-valuec | – | – | 0.0386 | 0.4686 |
Effect size is defined as the absolute value (difference from baseline to follow-up measure) divided by the SD at baseline.
P-value from Wilcoxon-signed ranked test comparing the time period to baseline.
P-value from Wilcoxon-signed ranked test comparing the time period to previous time period.
At 6 weeks, mean aerobic exercise time among participants increased to 166.7 min with statistically significant observed change in mean duration of both aerobic and non-aerobic exercises when compared to baseline (p value: <0.01). This effect was sustained or further increased at 12 weeks. Statistically significant improvement in self-reported health behaviors (confidence level and success with engaging in regular exercise and having healthy snack choices) was also noted at 6 and 12 weeks as well as in composite self-efficacy and quality of life scores. At 24 weeks, the difference from baseline of all outcome measures remained significant. Sustained results were seen between 12 and 24 weeks in all areas (Table 2).
In logistic regression models adjusted for age, sex, and baseline glucose or hemoglobin A1C levels, increases in physical activity, healthy eating behavior, self-efficacy and quality of life remained significantly different from baseline at 6, 12 and 24 weeks.
5. Discussion
In this study, we assessed the impact of wellness coaching on healthy lifestyle behaviors among primary care patients with prediabetes. We observed a statistically significant increase in exercise level, both non-aerobic and aerobic, healthy eating behavior, self-efficacy and composite quality of life scores among wellness coaching participants as early as 6 weeks into the program.
At 6 weeks, mean exercise time increased to >150 min/week with sustained effect at 12 weeks. This observation has strong clinical relevance since risk reduction in diabetes progression has been associated with at least 150 min of exercise per week (Knowler et al., 2002). A meta-analysis of 33 observational studies to determine the dose-response between levels of physical activity and risk for coronary artery disease also showed that persons who had at least 150 min per week of physical activity had a 14% lower CAD risk (Sattelmair et al., 2011). The results of this study suggest that wellness coaching alone delivered in primary care setting may effectively help high risk patients meet recommended guidelines for level of physical activity.
In terms of self-efficacy in eating behavior, participants at baseline rated their confidence at being able to make healthy snack choices to be moderately high; however, scores for successfully doing so were lower. Wellness coaching resulted in both increased confidence and success at making healthy snack choices from baseline. This finding support the premise that improved health behaviors further enhance self-efficacy which then promotes lifestyle changes.
There are several plausible explanations as to how wellness coaching helped participants achieved improvement in both behaviors and self-efficacy. Wellness coaching has been shown to unlock positive self-intrinsic motivation and self-competency beliefs for healthy lifestyle adjustment thus propelling individuals into action (Cinar and Schou, 2014). Participants also had regular contacts with the wellness coaches which could have heightened their self-monitoring awareness. It is, however, interesting to note that sustained effects were seen even 12 weeks after completion of the wellness coaching sessions. While the reported change in participants' success at making healthy snack choices was statistically significant, it was less striking than the observed increased in the amount of reported physical activity. This difficulty in enhancing autonomous motivation for healthy dietary behavior has previously been observed; a study by Rutten and colleagues showed that lifestyle coaching led to improved physical activity more than healthy eating (Rutten et al., 2014). Other factors may potentially be contributing to unhealthy dietary choices that warrant further exploration.
A significant increase from baseline in both composite self-efficacy and quality of life measures was likewise seen after 6 and 12 weeks of wellness coaching. These findings are consistent with other studies that showed the effectiveness of wellness coaching in enhancing goal setting skills and quality of life domains (Olsen and Nesbitt, 2010; Clark et al., 2014). Health coaching also has been shown to be more effective in enhancing self-efficacy than health education (Cinar and Schou, 2014).
Usual lifestyle modification programs in diabetes prevention combined motivational interviewing with supervised physical activity sessions, health education and dietitian delivered dietary counseling (Knowler et al., 2002; Ma et al., 2013). Our study solely utilized wellness coaching to enhance participants' motivation to engage in healthy behaviors in domains of nutrition and physical activity level. The intervention was delivered by certified wellness coaches who have no clinical background. No specific physical activity program or dietary intervention was followed. This is a unique approach to diabetes prevention among patients with prediabetes that differs from other diabetes prevention programs. A systematic review of counseling interventions to change diet and physical activity behaviors among obese and overweight persons with cardiovascular disease risk factors showed decreased diabetes incidence and improved intermediate cardiovascular health outcomes up to 2 years (Lin et al., 2014). Our participants were likewise mostly obese or overweight with moderately high baseline self-efficacy scores which may have contributed to positive wellness coaching outcomes. Interestingly, we saw an independent association of wellness coaching to each of our measured outcomes after adjusting for age, sex and baseline glucose or hemoglobin A1C level, an observation which suggests the feasibility of modifying and streamlining more robust diabetes prevention programs to one that primarily focus on enhancing self-motivation to change behavior.
Studies that solely involved behavioral counseling to promote healthy lifestyle, had not shown consistent benefit for intermediate health outcomes such as blood pressure, cholesterol level and BMI (Lin et al., 2014). While a statistically significant increase in self-reported health behaviors among participants in this study was observed, the correlation of wellness coaching to intermediate health outcomes could not be determined as clinical data such as blood pressure and cholesterol level were not measured in this study; among participants with available BMI data (n = 71), there was a non-statistically significant decrease in BMI seen at the end of 12 weeks wellness couching. Future wellness coaching studies that capture clinical outcome data will help determine the correlation between wellness coaching and intermediate health outcomes.
This study involved 12 weeks of one to one coaching conducted mainly on a face to face basis. Alternative methods of delivering behavioral interventions by web or mobile devices are showing promise (Block et al., 2015) as well as combination of personal and group coaching (Leahy and Wing, 2013). Other wellness coaching studies (Knowler et al., 2002; Ma et al., 2013) consisted of at least 12 weeks sessions; we saw significant changes in outcome measures as early as 6 weeks into coaching which poses the feasibility of a shorter program duration. Continued efforts to further refine wellness coaching programs will help optimize their role in population based diabetes prevention measures.
5.1. Study limitations
Our study is not without limitations. This was a single arm prospective cohort study and participants where not randomized to a control group; hence, causality cannot be established. Outcome measures were self-reported and since the primary aim was to evaluate the impact of wellness coaching on health behaviors among patients with prediabetes, clinical outcome measures were not captured which would have further strengthened study results.
In addition, overall participation in this study was relatively low when compared to other wellness coaching studies (Clark et al., 2014; Thom et al., 2015); 30% (n = 168) consented to participate, and 18% (n = 99) completed at least 1 coaching session. It has been reported that participation rates in epidemiologic studies have been declining in the last 30 years with even steeper decline in the recent years. Plausible explanations to this observation are proliferation of research studies which tend to overwhelm potential participants, a general decline of volunteerism and increasing demands from multiple fronts on people's time (Galea and Tracy, 2007). However, while the number of consenters to the wellness coaching program was low, participant characteristics did not differ significantly from non-participants, and response rates reflect similar recruitment challenge seen in other studies. For example, Kaiser Permanente's encouragement trial that evaluated outreach methods (secured email, letter or phone) to recruit patients into Wellness Coaching Centers (SCC) showed a 1.9% overall uptake rate across the three intervention arms (Xiao et al., 2015). Reaching out to potential subjects during clinic visits and bringing wellness coaching into the community are ways of possibly increasing participation rates among the high risk individuals who may benefit from it; further research on identifying barriers and facilitators to recruitment would be helpful.
Finally, participants were community dwellers in a Midwestern suburban region served by an academic medical center based primary care clinic and results may not be generalized to populations with dissimilar characteristics.
6. Conclusions
In this study, a 12-week wellness coaching program delivered in primary care setting among individuals with prediabetes led to significant improvement in self-reported behaviors of physical activity and healthy eating choices as early as 6 weeks with continued improvement at 12 weeks and sustained results at 24 weeks. Similar trends were also observed with self-efficacy and quality of life measures. The results suggest that the integration of wellness coaching in primary care practice among individuals at high risk for diabetes is feasible and may be useful as part of diabetes prevention management strategies in target populations. Future randomized clinical trials are needed to further explore this issue.
Conflicts of interest
All authors report no conflict of interest.
Funding
This project was supported by funding from the Population Health Scholar Program of the Robert D. and Patricia E. Kern Center of the Science of Health Care Delivery. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Robert D. and Patricia E. Kern Center of the Science of Health Care Delivery.
Acknowledgments
This project was supported by several individuals. We express our appreciation to Ashley Quinnell who was our study coordinator, Julie Hathaway and Debra Judy for their assistance in data entry and retrieval, Dr. Kristin Vickers Douglas for her expertise and guidance in wellness coaching process. We are also grateful to our four wellness coaches: Mohamed Osman, Melissa Mapes, Karin Pyan and Sara Link, as well as our colleagues in primary care, Dr. Sarah Crane and Dr. Deborah McWilliams.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2018.02.012.
Supplementary data
Study Questionnaires
References
- Benzo R., Vickers K., Novotny P.J. Health coaching and chronic obstructive pulmonary disease rehospitalization: a randomized study. Am. J. Respir. Crit. Care Med. 2016;194(6):672–680. doi: 10.1164/rccm.201512-2503OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block G., Azar K.M., Romanelli R.J. Diabetes prevention and weight loss with a fully automated behavioral intervention by email, web and mobile phone: a randomized controlled trial among persons with prediabetes. J. Med. Internet Res. 2015;17(10) doi: 10.2196/jmir.4897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cinar A.B., Schou L. The role of self-efficacy in health coaching and health education for patients with type 2 diabetes. Int. Dent. J. 2014;64(3):155–163. doi: 10.1111/idj.12093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark M.M., Warren B.A., Hagen P.T. Stress level, health behaviors and quality of life in employees joining the wellness center. Am. J. Health Promot. 2011;26(1):21–25. doi: 10.4278/ajhp.090821-QUAN-272. [DOI] [PubMed] [Google Scholar]
- Clark M.M., Bradley K.L., Jenkins S.M. The effectiveness of wellness coaching for improving quality of life. Mayo Clin. Proc. 2014 Nov;89(11):1537–1544. doi: 10.1016/j.mayocp.2014.04.028. [DOI] [PubMed] [Google Scholar]
- Clark M.M., Bradley K.L., Jenkins S.M. Improvement in health behaviors, eating self-efficacy and goal-setting skills following participation in wellness coaching. Am. J. Health Promot. 2016;30(6):458–464. doi: 10.4278/ajhp.140627-QUAL-304. [DOI] [PubMed] [Google Scholar]
- DeJesus R.S., Radecki Breitkopf C., Rutten L.J. Incidence rate of prediabetes progression to diabetes: modeling an optimum target group for intervention. Popul. Health Manag. 2017;20(3):216–233. doi: 10.1089/pop.2016.0067. [DOI] [PubMed] [Google Scholar]
- Diagnosis and classification of diabetes mellitusDiabetes Care. 2013;36(Suppl. 1):S67–74. doi: 10.2337/dc13-S067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Tracy M. Participation rates in epidemiologic studies. Ann. Epidemiol. 2007;17:643–653. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Gilbody S., Richards D., Brealey S., Hewitt C. Screening for depression in medical settings with the patient health questionnaire (PHQ-9): a diagnostic meta-analysis. J. Gen. Intern. Med. 2007;22(11):1596–1602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowler W.C., Barrett-Connor E., Fowler S.E. For the diabetes prevention program research group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leahy T.M., Wing R.R. A randomized controlled pilot study testing three types of health coaches for obesity treatment: professional, peer, and mentor. Obesity (Silver Spring) 2013;21(5):928–934. doi: 10.1038/oby.2012.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.Y., Hwang H., Hawkins R., Pingree S. Interplay of negative emotion and health self-efficacy on the sue of health information and its outcomes. Commun. Res. 2008;35(2):358–381. [Google Scholar]
- Liddy C., Johnston S., Nash K. Health coaching in primary care: a feasibility model for diabetes care. BMC Fam. Pract. 2014;15:60. doi: 10.1186/1471-2296-15-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J.S., O'Connor E.A., Evans C.V. Agency for Healthcare Research and Quality (US) 2014. Behavioral counseling to promote a healthy lifestyle for cardiovascular disease prevention in persons with cardiovascular risk factors: an updated systematic evidence review for the U.S. Preventive Services Task Force [Internet] (Report No. 13-05179-EF-1.36). [PubMed] [Google Scholar]
- Locke D.E., Decker P.A., Sloan J.A. Validation of single-item linear analog scale assessment of quality of life in neuro-oncology patients. J. Pain Symptom Manag. 2007;34(6):628–638. doi: 10.1016/j.jpainsymman.2007.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig K., Stewart A., Ritter P. Vol. 25. Sage Publications; Thousand Oaks CA: 1996. Outcome Measures for Health Education and other Health Care Interventions; pp. 37–38. [Google Scholar]
- Ma J., Yank V., Xiao L. Translating the diabetes prevention program lifestyle intervention for weight loss into primary care: a randomized trial. JAMA. 2013;173(2):113–121. doi: 10.1001/2013.jamainternmed.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan P. The efficacy of diabetes patient education and self-management education in type 2 diabetes. Can. J. Diabetes. 2011;35:46–53. [Google Scholar]
- Moriarty A.S., Gilbody S., McMillan D., Menea L. Screening and case finding for major depressive disorder using the Patient Health Questionnaire (PHQ-9): a meta-analysis. Gen. Hosp. Psychiatry. 2015;37(6):567–576. doi: 10.1016/j.genhosppsych.2015.06.012. [DOI] [PubMed] [Google Scholar]
- National Diabetes Statistics Report National Center for Chronic Disease Prevention and Health Promotion. 2014. https://www.cdc.gov/diabetes/data/statistics/2014statisticsreport.html
- Neuner-Jehle S., Schmid J., Gruninger U. The health coaching programme: a new patient-centered and visually supported approach for health behavior change in primary care. BMC Fam. Pract. 2013;14:100. doi: 10.1186/1471-2296-14-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen J.M., Nesbitt B.J. Health coaching to improve healthy lifestyle behaviors: an integrative review. Am. J. Health Promot. 2010;25:e1–e12. doi: 10.4278/ajhp.090313-LIT-101. [DOI] [PubMed] [Google Scholar]
- Perreault L., Temprosa M., Mather K.J. Regression from prediabetes to normal glucose regulation is associated with reduction in cardiovascular risk: results from the Diabetes Prevention Program outcomes study. Diabetes Care. 2014;37(9):2622–2631. doi: 10.2337/dc14-0656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutten G.M., Meis J.J., Handriks M.R. The contribution of lifestyle coaching of overweight patients in primary care to more autonomous motivation for physical activity and healthy dietary behavior: results of a longitudinal study. Int. J. Behav. Nutr. Phys. Act. 2014;11:86. doi: 10.1186/s12966-014-0086-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattelmair J., Pertman J., Ding E.L. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124(7):789–795. doi: 10.1161/CIRCULATIONAHA.110.010710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittdiel J.A., Adams R.A., Goler N. The impact of telephonic wellness coaching on weight loss: a “natural experiments for translation in diabetes (NEXT-D)” study. Obesity. 2017;25:352–356. doi: 10.1002/oby.21723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh J.A., Satele D., Suneetha P. Normative data and clinically significant effect sizes for single-item numerical linear analogue self-assessment (LASA) scales. Health Qual. Life Outcomes. 2014;12:187. doi: 10.1186/s12955-014-0187-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanford chronic disease self-management education program. http://patienteducation.stanford.edu/research/exercise.html
- Stevens J.W., Khunti K., Harvey R. Preventing the progression to type 2 diabetes mellitus in adults at high risk: a systematic review and network meta-analysis of lifestyle, pharmacological and surgical interventions. Diabetes Res. Clin. Pract. 2015;107(3):320–331. doi: 10.1016/j.diabres.2015.01.027. [DOI] [PubMed] [Google Scholar]
- Tabak A.G., Herder C., Rathmann W. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379:2279–2290. doi: 10.1016/S0140-6736(12)60283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang T.S., Funnel M.M., Oh M. Lasting effects of a 2-year diabetes self-management support intervention: outcomes at 1 year follow-up. Prev. Chronic Dis. 2012;9 doi: 10.5888/pcd9.110313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thom D.H., Willard-Grace R., Hessler D. The impact of health coaching on medication adherence in patients with poorly controlled diabetes, hypertension, and/or hyperlipidemia: a randomized controlled trial. J. Am. Board Fam. Med. 2015;28(1):38–45. doi: 10.3122/jabfm.2015.01.140123. [DOI] [PubMed] [Google Scholar]
- Thomas R.J. 2010. Happy Heart Pilot Study. Unpublished raw data. [Google Scholar]
- Wong-Rieger D., Rieger F.P. Health coaching in diabetes: empowering patients to self-manage. Can. J. Diabetes. 2013 Feb;37(1):41–44. doi: 10.1016/j.jcjd.2013.01.001. [DOI] [PubMed] [Google Scholar]
- Xiao H., Adams S.R., Goler N. Wellness coaching for people with prediabetes: a randomized encouragement trial to evaluate outreach methods at Kaiser Permanente, Northern California, 2013. Prev. Chronic Dis. 2015;12 doi: 10.5888/pcd12.150251. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Study Questionnaires