Abstract
Background
The influence of pulmonary vein (PV) anatomy on cryo kinetics during cryoballoon (CB) ablation is unclear.
Objective
To investigate the relationship between PV anatomy and cryo kinetics during CB ablation for atrial fibrillation (AF).
Methods
Sixty consecutive patients were enrolled. PV anatomy, including ostial diameters (long, short and corrected), ratio between short and long diameters, ostium shape (round, oval, triangular, and narrow), and drainage pattern (typical, with common trunk, common antrum, ostial branch and supernumerary PV) were evaluated on multi-detector computed tomography (MDCT) images pre-procedure. Cryo kinetics parameters [balloon freeze time from 0 to -30ºC (BFT), balloon nadir temperature (BNT) and balloon warming time from -30 to +15ºC (BWT)] were recorded during procedure. All p values are two-sided, with values of p < 0.05 considered to be statistically significant.
Results
606 times of freezing cycle were accomplished. Moderate negative correlation was documented between BNT and corrected PV diameter (r = -0.51, p < 0.001) when using 23-mm CBs, and mild negative correlation (r = - 0.32, p = 0.001) was found when using 28-mm CBs. Multivariate logistic regression analysis revealed that PV corrected ostial diameter (OR, 1.4; p = 0.004) predicted a BNT < -51ºC when using 23-mm CBs, while PV ostium oval shape (OR, 0.3; p = 0.033) and PV locations (left inferior PV: OR, 0.04; p = 0.005; right superior PV: OR, 4.3; p = 0.025) predicted BNT < -51ºC when using 28-mm CBs.
Conclusions
MDCT can provide PV anatomy accurate evaluation prior CB ablation. PV anatomy is associated with cryo kinetics during ablation.
Keywords: Pulmonary Veins / anatomy & histology, Atrial Fibrillation, Catheter Ablation, Multidetector Computed Tomography, Cost-Benefit Analysis
Introduction
CB ablation has an increasing clinical application worldwide, it has been proved a comparable technique to radiofrequency (RF) ablation in safety and efficacy for the AF treatment,1 and maybe more cost-effective.2 By achieving appropriate occlusion in targeted PVs with the balloon and getting good balloon - PV ostium contact, it can simplify the procedure with a “single-shot” approach to get circumferential PV isolation.3 It is reported that some parameters of cryo kinetics, such as balloon temperature,4 balloon warming time,5 can predict acute PV isolation or late PVs reconnection. Some parameters of PV anatomy have been used to predict occlusion,6 or acute, mid- and long-term success of CB ablation.7-9 It is reasonable to imaging that PV anatomy plays a role in cryo kinetics, thus exerting an influence on ablation efficacy. However, limited data exist regarding the association between PV anatomy and cryo kinetics during CB ablation. We aimed to investigate the relationship between PV anatomy parameters and cryo kinetic parameters in patients undergoing CB ablation using either 23- or 28-mm CB for AF.
Methods
Patients
Between January and October 2014, a prospective study was carried out at our institution. Sixty consecutive patients with symptomatic and drug-refractory AF underwent CB ablation. In these patients, pre-procedural MDCT images and complete recordings of cryoballoon temperature during each CB ablation were available. All patients provided written informed consent. The study followed the ethical standards of the Declaration of Helsinki of 1975, revised in 2008 and was approved by the local institutional ethics committee.
PV Anatomy Assessment
Image acquisition
Prior to the procedure, MDCT studies were performed on a MDCT scanner (SOMATOM Definition Flash, Siemens). Scanning parameters were the following: tube voltage 100 - 120 kV, 3D automatic tube current modulation, thickness / increment of reconstruction 0.625 / 0.625 mm. ECG-gating was not used, and patient breath holding was required during image acquisition. A bolus tracking protocol with 50 ~ 70 mL i.v. contrast agent (Ultravist 370, Bayer Schering) and 3 ~ 5 mL/s flow rate was applied.
Image analysis
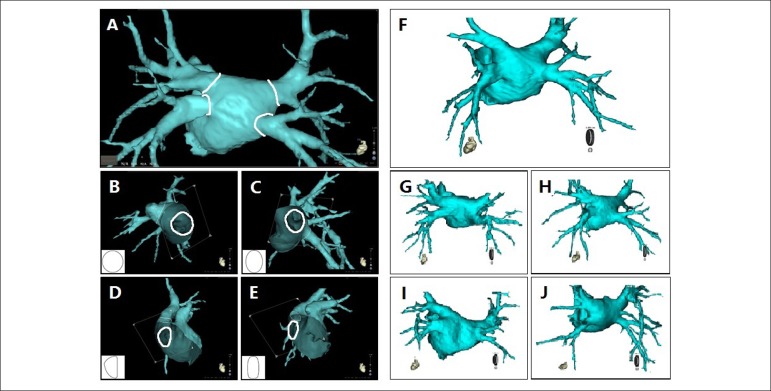
MDCT images were reconstructed and analyzed using CartoMerge software (Biosense Webster, Diamond Bar, CA, USA) right before the procedure. PV ostia were defined anatomically at the parietal pericardium point of reflection10 and were depicted semi-automatically (Figure 1A), together with ostia perimeters calculated automatically by computerized image analysis. Long (Dlong) and short (Dshort) ostia diameters were then measured. Corrected ostial diameters (Dcorrected) were calculated using the formula Dcorrected = perimeter / π. The ratio between Dshort and Dlong (Dshort / Dlong) was also calculated for analysis. Taking consideration of Dshort / Dlong values, PV ostium shapes were divided into 4 types: type I (round), ostia with value between 0.90 ~ 1.00; type II (oval), value between 0.60 ~ 0.90 and a smoothly curved edge; type III (triangular), value between 0.60 ~ 0.90 and an obviously straight part at the edge; and type IV (narrow), value less than 0.60. (Figure 1B-E).
Figure 1.
PV ostium shapes category and PV drainage patterns. A) PV ostia depicted semi-automatically using CartoMerge software. Four shapes of PV ostium; B) Type I (round); C) Type II (oval); D) Type III (triangular); and E) Type IV (narrow). Five patterns of PV drainage; F) Four PVs drains into LA in a typical pattern; G) Left superior and inferior PVs drains into LA both in a pattern of with common trunk; H) Left superior and inferior PVs drains into LA both in a pattern of with common antrum; I) Right inferior PV drains into LA in a pattern of with ostial branch; J) Right superior and inferior PVs drains in LA with supernumerary vein (middle vein).
Five PV drainage patterns were defined for the targeted superior/inferior PVs based on the definition by Marom et al.11 When the superior and inferior PVs on the same side joined together to form a common trunk vein and drained into LA through a common ostium, the superior and inferior PV were defined as “with common trunk”. If the superior and inferior PVs on the same side drained into LA through two independently trunk but drained into LA through ostia hardly separated by LA wall (the minimum distance between the two ostia was less than 2 mm on MDCT images), the two PVs were then defined as “with common antrum”. PV “with ostial branch” was defined as a PV branch joining within 10 mm from the ostium. PV “with supernumerary vein” was defined as the superior or inferior PV with neighboring additional vein(s), when a middle PV existed, both the superior and inferior PV on the same side were defined as “with supernumerary vein”. PV “with typical drainage” was defined as a superior or inferior PV drained into LA independently, through neither a common trunk nor antrum, and that did not have an ostial branch or supernumerary vein. (Figure 1F-J)
Anatomical assessment reproducibility
In order to assess evaluating methods reproducibility of diameters described above, 40 PVs ostial diameter of first 10 patients were measured on CT images by two blind experienced observers at the beginning of the study. One observer measured two times in different moments to study the inter-observer reproducibility. The other observer measured one time, and the intra-observer reproducibility between the two observers was studied. The ostium shapes and drainage patterns were also assessed by two experienced observers in consensus during the study.
Ablation procedure
The ablation procedures were carried out as previously reported.12 Briefly, an octapolar electrode catheter was placed into the coronary sinus and a phrenic nerve (PN) pacing electrode catheter into the superior vein cava (SVC). After a single transseptal puncture, selective PV angiography was carried out and a CB catheter (Arctic Front, Medtronic, Quebec, Canada) was inserted into LA together with a spiral catheter (SC) (Achieve, Medtronic, CA, USA). There are currently two sizes of balloon catheters (23 or 28 mm) and two sizes of SCs (15 or 20 mm) available. PV ostia diameters were determined from MDCT images; CB and SC size were selected accordingly: If long diameters of three or four PVs were < 22 mm, 23-mm CB a 15-mm SC were selected; If that ≥ 22 mm, a 28-mm CB and a 20-mm SC were preferred; otherwise the choice would be made by the operator temporaly. As soon as good contact of balloon to PV ostium indicated by the contrast retention in PV was obtained, freezing cycle was started with two to three applications per vein. Generally each freeze lasted 240s, and ideal freezing temperature was between -45ºC and -55ºC. If exists a common PV, freezing was analyzed separately as in superior or inferior PV based on location of balloon distal end during freezing. Supernumerary PVs were not taken as targeted PV as there are usually too small in dimension.
PN was constantly paced (10 mA, 2 ms, 50/min) with PN pacing catheter in SVC when freezing at right PVs. After each freeze, PV conduction was re-evaluated by adjusting SC position within the PV. In all patients, PVI of all targeted PVs with primary use of CB only was the procedural endpoint. If PVI was not achieved for a particular vein following a minimum of two freezing, either further cryoablation would be performed or conventional RF ablation would be undertaken, depending on the initial contrast-guided occlusion and the minimum temperature achieved.
Cryo kinetics
Three parameters of cryo kinetics5 were introduced: balloon freezing time from 0 to -30ºC (BFT), balloon nadir temperature (BNT) and balloon warming time from -30 to +15ºC (BWT). Freezing cycles with a BNT lower than -30ºCwere taken into analysis.
Statistical analysis
After being tested for normality distribution and variances equality using One-Sample Kolmogorov-Smirnov test and Levene’s test, continuous variables were presented as mean ± standard deviation (SD) or median (interquartile range), and were compared using the unpaired Student’s t-test or nonparametric variables Mann-Whitney U test as appropriate. Categorical variables were expressed as number (percentage) and were compared by means of c2 analysis or Fisher exact test. Measuring reproducibility of PV ostial diameters was assessed using intra-class correlation coefficient (ICC). Pearson or Spearman correlation was used to evaluate the association between two variables based on its distributions. Logistic regression was performed to investigate the predictive values of PV anatomic parameters for cryo kinetic effect. Variables with a p value < 0.10 in univariate analysis were included into the multivariate analysis, which was performed using an enter approach with criteria of p < 0.05 for inclusion in and p > 0.05 for exclusion from the model. A two-sided p < 0.05 was considered statistically significant. All statistical analysis were performed using IBM SPSS statistical software (Version 20.0, SPSS).
Results
Study population and procedural data
The study population baseline characteristics and ablation procedure parameters are presented in Table 1.Compared with 28-mm CB only, the acute PVI rates were not significantly different when ablation was using 23-mm CB only either on PV level (92.5% vs. 96.9%, p = 0.16) or on patient level (79.4% vs. 91.7%, p = 0.28). No significant difference was found in total complication rate between 28- or 23-mm CBs (8.8% vs. 4.2%, p = 0.64). One case of PN palsy, taken as major, was detected during freezing in a right inferior PV using a 28-mm CB and did not recover until discharge. One case of pericardial and pleural effusion, two cases of left groin hematomas were all resolved within one month post-procedure.
Table 1.
Baseline Characteristics of study population and CB PVI Procedure Parameters
| Baseline Characteristics | |
|---|---|
| Age (years) | 56.8 ± 12.5 |
| Gender, male | 32(53.3) |
| BMI (kg/m2) | 24.6 ± 3.1 |
| AF type, paroxysmal AF | 58 (96.7) |
| AF duration (months) | 25.5 (12, 69) |
| CHA2DS2-VASc score | 1(0, 2) |
| LAD (mm) | 35.2 ± 4.8 |
| LVEF (%) | 65.6 ± 5.4 |
| Procedure Parameters | |
| Balloon type, 28-mm /23-mm/double | 34 (56.7) / 24(40) / 2(3.3) |
| Nº. of freeze | 10.8 ± 3.2 |
| Acute PVI | |
| Patient level * | 60(100) |
| With CB only, PV level# | 225 (94.5) |
| With CB only, patient level | 51(85) |
| Complications | 4 (6.7) |
| Phrenic nerve palsy | 1 (1.7) |
| Pericardial & pleural effusion | 1 (1.7) |
| Left groin hematomas | 2 (3.3) |
Values are n (%), mean ± SD, or median (interquartile range). CB: cryoballoon; PVI: pulmonary vein isolation; PV: pulmonary vein; AF: atrial fibrillation; BMI: body mass index; LAD: left atrial diameter; LVEF: left ventricular ejection fraction (measured from transthoracic echocardiography); CHA2DS2-VASc score = stroke risk score [cardiac failure, hypertension, age ≥ 75 years (doubled), diabetes, stroke (doubled)‑vascular disease, age of 65-74 years and sex category (female)].
PVI with CB ablation only or plus conventional RF ablation.
1 right superior and 1 right inferior PV has no potential
Anatomy data
The pre-analysis on reproducibility revealed that inter-observer ICC of Dlong, Dshort and Dcorrected was 0.93, 0.95 and 0.96 (all p < 0.001), and intra-observer ICC of three measured diameters was 0.90, 0.96 and 0.93 respectively (all p < 0.001).
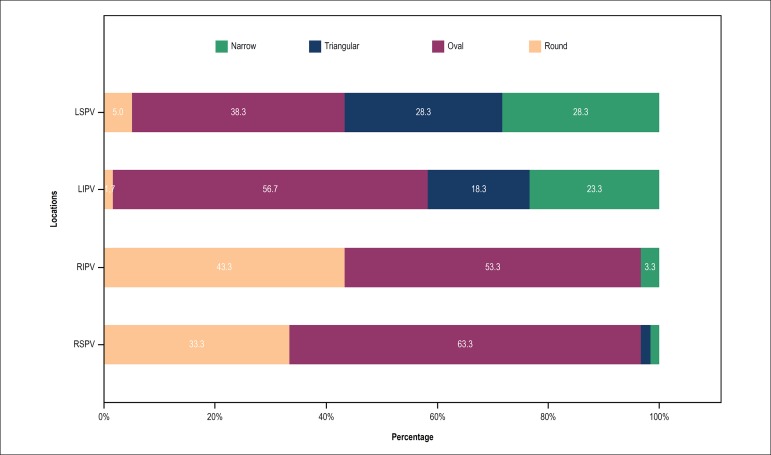
Diameters of 240 PVs measured on CT images were listed in Table 2. Compared with ablation using 23-mm CBs, ratio of Dcorrected and CB diameter was much smaller when frozen using 28-mm CBs (0.76 ± 0.14 vs. 0.68 ± 0.13, p < 0.001). Linear correlation analysis showed that Dcorrected was strongly correlated with Dlong (correlation coefficient: 0.93, p < 0.001) and Dshort (correlation coefficient: 0.90, p < 0.001), while the latter two were moderately correlated with each other (correlation coefficient: 0.74, p < 0.001). Values of Dshort / Dlong were between 0.38 and 1.00. Proportions of different ostium shapes and drainage patterns of four targeted PVs are presented in Figure 2 and Table 3.
Table 2.
PV ostia diameters measured on CT images
| PV location | Dlong (mm) | Dshort (mm) | Dcorrected (mm) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 23-mm CB | 28-mm CB | p | 23-mm CB | 28-mm CB | p | 23-mm CB | 28-mm CB | p | |
| LSPV | 20.3 ± 3.0 | 21.7 ± 2.8 | 0.06 | 13.5 ± 2.7 | 15.2 ± 3.3 | .04 | 17.7 ± 2.7 | 19.3 ± 2.5 | 0.02 |
| LIPV | 17.4 ± 3.4 | 17.6 ± 2.1 | 0.80 | 11.7 ± 3.3 | 12.9 ± 2.1 | .13 | 15.3 ± 3.2 | 15.9 ± 1.9 | 0.41 |
| RIPV | 18.3 ± 3.0 | 19.6 ± 3.0 | 0.09 | 15.6 ± 2.9 | 17.1 ± 3.0 | .054 | 17.3 ± 2.6 | 18.8 ± 2.7 | 0.046 |
| RSPV | 21.2 ± 3.0 | 24.3 ± 3.4 | 0.001 | 18.0 ± 3.7 | 20.4 ± 3.8 | .02 | 20.0 ± 3.0 | 22.7 ± 3.4 | 0.01 |
| Total | 19.2 ± 3.4 | 20.8 ± 3.8 | 0.001 | 14.6 ± 3.9 | 16.4 ± 4.1 | .001 | 17.6 ± 3.3 | 19.1 ± 3.6 | 0.001 |
Values are mean ± SD. p: p-value (unpaired Student's t-test). Dlong: PV ostium long diameter; Dshort: PV ostium short diameter; Dcorrected: Corrected diameter calculated from PV ostium perimeter PV ostium; CB: cryoballoon; LSPV: left superior pulmonary vein; LIPV: left inferior pulmonary vein; RIPV: right inferior pulmonary vein; RSPV: right superior pulmonary vein.
Figure 2.
Proportions of different ostium shapes of the four targeted PVs. Dlong: PV ostium long diameter; Dshort: PV ostium short diameter; Dcorrected: Corrected diameter calculated from PV ostium perimeter PV ostium; CB: cryoballoon; LSPV: left superior pulmonary vein; LIPV: left inferior pulmonary vein; RIPV: right inferior pulmonary vein; RSPV: right superior pulmonary vein.
Table 3.
Proportion of PV drainage patterns
| Location | typical | with common trunk | with common antrum | with ostial branch | with supernumerary vein (MPV) |
|---|---|---|---|---|---|
| LSPV | 23(38.3) | 11(18.3) | 25(41.7) | 2(3.3) | 0 |
| LIPV | 23(38.3) | 11(18.3) | 25(41.7) | 3(5.0) | 0 |
| RIPV | 24(40) | 0 | 6(10) | 27(45) | 4(6.7) |
| RSPV | 37(61.7) | 0 | 6(10) | 14(23.3) | 4(6.7) |
| Total | 107(44.6) | 22(9.2) | 62(25.8) | 46(19.2) | 8(3.3) |
Values are n (%). MPV: middle pulmonary vein; LSPV: left superior pulmonary vein; LSPV: left superior pulmonary vein; LIPV: left inferior pulmonary vein; RIPV: right inferior pulmonary vein; RSPV: right superior pulmonary vein.
Cryo kinetics
238 targeted PVs were frozen 606 times. Of which, 102 PVs were frozen 254 times using 23-mm CB, and 141 PVs 352 times using 28-mm CB. Compared with 28 mm CBs, BFT was shorter and BNT was lower when using 23-mm CBs in all PV locations (all p < 0.001), while BWT was shorter only in superior PVs (see Table 4).
Table 4.
Parameters of cryo kinetics
| PV location | BFT (s) | BNT (ºC) | BWT (s) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 23-mm CB | 28-mm CB | p | 23-mm CB | 28-mm CB | p | 23-mm CB | 28-mm CB | p | |
| LSPV | 13.7 ± 4.2 | 23.8 ± 9.1 | < 0.001 | -52.8 ± 6.5 | -46.8 ± 7.1 | < 0.001 | 19.8 ± 7.7 | 25.3 ± 11.0 | 0.001 |
| LIPV | 14.5 ± 3.4 | 27.3 ± 7.8 | < 0.001 | -50.2 ± 4.9 | -42.0 ± 4.8 | < 0.001 | 17.5 ± 5.7 | 17.9 ± 5.9 | 0.656 |
| RIPV | 13.9 ± 4.0 | 28.1 ± 8.9 | < 0.001 | -52.6 ± 5.9 | -42.3 ± 6.9 | < 0.001 | 20.0 ± 7.6 | 18.4 ± 8.4 | 0.237 |
| RSPV | 12.1 ± 3.0 | 21.3 ± 7.6 | < 0.001 | -56.8 ± 5.1 | -49.7 ± 6.7 | < 0.001 | 26.0 ± 6.8 | 30.4 ± 11.5 | 0.008 |
| Total | 13.6 ± 3.8 | 25.2 ± 8.8 | < 0.001 | -53.1 ± 6.1 | -45.1 ± 7.1 | < 0.001 | 20.8 ± 7.6 | 22.7 ± 10.6 | 0.014 |
Values are mean ± SD. p: p-value (unpaired Student's t-test). CB: cryoballoon; BFT: balloon freezing time from 0 to -30ºC; BNT: balloon nadir temperature; BWT: balloon warming time from -30 to +15ºC; LSPV: left superior pulmonary vein; LIPV: left inferior pulmonary vein; RIPV: right inferior pulmonary vein; RSPV: right superior pulmonary vein.
Correlation between BNT and BFT (correlation coefficient: 0.77, p < 0.001), and between BNT and BWT (correlation coefficient: - 0.85, p < 0.001) was stronger than that between BFT and BWT (correlation coefficient: - 0.60, p < 0.001) when using 23-mm CB. The same result was found when using 28-mm CB (correlation coefficient: 0.79, - 0.86, and - 0.62, respectively; all p < 0.001).
PV anatomy and BNT
As mentioned above, Dcorrected has much stronger correlations with both Dlong and Dshort, and BNT has much stronger correlations with the two other kinetic parameters as well, Dcorrected and BNT were chosen as parameters to investigate the relationship between PV diameter and cryo kinetic parameter. To reflect the maximal biological effect and avoid the confounding effect caused by manipulation between different cycles (e.g., occlusion degree, time of freezing circle), the lowest BNT achieved by using the same size of balloon was chosen to analyze each PV.
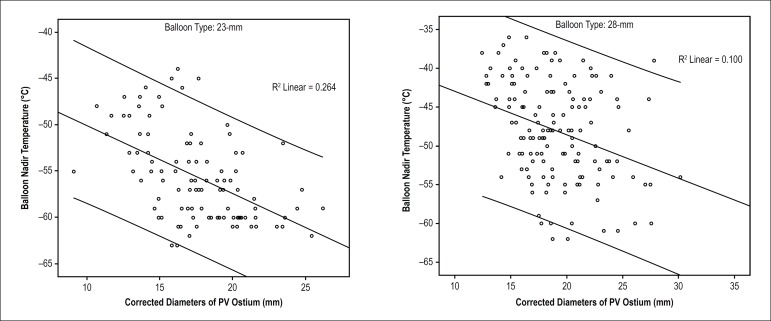
Correlation analysis revealed that the correlation coefficient between Dcorrected and BNT was -0.51 when ablation was with 23-mm CB, and it was -0.32 with 28-mm CB (both p < 0.001). Correlation between the two parameters was stronger when using 23-mm CB (see Figure 3). However, there was no significant correlation between value of Dshort / Dlong and BNT either using 23- (correlation coefficient: -0.11, p = 0.23) or 28-mm CB (correlation coefficient: -0.09, p = 0.30).
Figure 3.
Scatterplot of PV ostium corrected diameters and balloon nadir temperature using two sizes of cryoballoon.
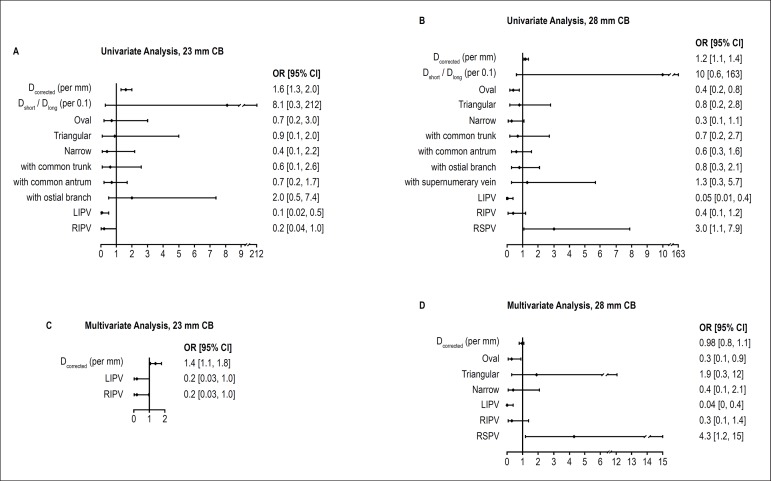
In order to investigate the predict value of PV anatomic parameters for cryo kinetic effect, BNT was transformed into a binary variable with a cut-point of -51ºC (< -51ºC and ≥ -51ºC)4 and taken as dependent variable. PV anatomic parameters including Dcorrected, value of Dshort / Dlong, ostium shape, drainage pattern and location were included in logistic regression model as independent variables. Univariate and multivariate analyses revealed that, among the above-mentioned variables, Dcorrected [OR, 1.4(95% CI: 1.1 - 1.8), p = 0.004] predicted a BNT of < -51ºC when using 23-mm CBs, while an oval shape of PV ostium [OR, 0.3(95% CI: 0.1 - 0.9), p = 0.033] and PV locations [left inferior PV: OR, 0.04(95% CI: 0.004 - 0.4), p = 0.005; right superior PV: OR, 4.3(95% CI: 1.2 - 15), p = 0.025] predicted a BNT of < -51ºC when using 28-mm CB. However, PV drainage patterns did not predict it when using either 23- or 28-mm CBs. (see Figure 4).
Figure 4.
Univariate and multivariate logistic regression analysis for BNT (< -51ºC and ≥ -51ºC). A and C. Univariate and multivariate analysis of 23mm CB. B and D. Univariate and multivariate analysis of 28 mm CB. Dlong: PV ostium long diameter; Dshort: PV ostium short diameter; Dcorrected: Corrected diameter calculated from PV ostium perimeter PV ostium; CB: cryoballoon; LSPV: left superior pulmonary vein; LIPV: left inferior pulmonary vein; RIPV: right inferior pulmonary vein; RSPV: right superior pulmonary vein.
Discussion
Main findings
This study aimed to investigate the relationship between PV anatomy and cryo kinetics during CB ablation. The present study main findings can be summarized as follows: Firstly, MDCT was accurate and useful in pre-procedural evaluation of PV anatomy for CB ablation of AF; Dcorrected was a better parameter for ostial measurement than Dlong and Dshort. Secondly, BNT, BFT and BWT were associated to each other, BNT was a better parameter for evaluating cryo kinetics effect than the latter two. Thirdly, there is an association between Dcorrected and BNT both when using 23- and 28-mm CBs; Dcorrected predicted cryo kinetic effect with a BNT of < -51ºC when using 23-mm CB, while PV ostial shape and location predicted the effect when using the 28-mm CB.
PV anatomy evaluated with MDCT
MDCT images can provide accurate and detailed PVs anatomic information.10 Our study found that variations existed in dimensions, ostial shapes and drainage patterns of PVs among different patients and PV locations, which was consistent with prior studies.11,13,14 Values of PV ostia Dshort / Dlong that we studied were between 0.38~1.00, and only 20.8% PVs (50/240) had a round-shape ostia. Therefore, it is a partial evaluation using only Dlong or Dshort as PV ostial dimension. Considering PVs compliance and deformation to adapt the CB during procedure, Dcorrected, diameter calculated from the perimeter was more reliable. Correlation analysis on PV ostial dimension measurement also demonstrated Dcorrected was more representative than the two others.
CB ablation and cryo kinetics
Cryo kinetics can be evaluated from two aspects: freezing temperature and time course. Furnkranz et al.4 found that BNT could predict acute PVI when using 28-mm CB. Ghosh et al.5 reported that -30~+15ºC BWT was a strong predictor for pulmonary vein reconnection. The current study revealed that BFT, BNT and BWT had significant correlations to each other, which was higher between BNT and the two others. For this reason, we chose BNT as the representative cryo kinetic parameter for analyzing the relationship between PV anatomy and cryo kinetics. A cut-point of < -51ºC was selected for logistic regression because BNT < -51ºC was invariably associated with PVI, as Ghosh et al.5 concluded.
Relationship between PV Anatomy and Cryo Kinetics
The CB ablation basic technique is to achieve cryoenergy-induced PVI on a condition of appropriate occlusion of PV blood flow and circumferential contact between PV ostia and CB surface, ideally the equatorial region of CB.15 Sorgente et al.6 found that PV ostium shape was useful in predicting the degree of occlusion. PV ovality16 and drainage patterns9 were reported to have an impact on AF recurrence in some studies. In this study, though a mild to moderate association was found between BNT and Dcorrected, no association existed either between BNT and PV ostium shape or between BNT and PV drainage pattern. The main reasons for this may be as follows: (1) PV ostia had certain compliance and could deform to adapt to the CB during procedure; (2) Different definitions of PV ostium shape and drainage pattern between studies; (3) cryo kinetic effect is associated with but not equal to occlusion degree or ablation effect.
Compared with 23-mm CB, the association between BNT and Dcorrected was weaker when using the 28-mm CB. This may be because: (1) 28-mm CB had a higher requirement for PV compliance and “free space” to handle (e.g., PV location, puncturing site of interatrial septum); (2) PV ablated using the 28-mm CB had a smaller ratio of Dcorrected and diameter of CB in this study, which limited the comparability.
Efficacy and safety of two CB sizes
Some studies reported that 23-mm CBs was associated with higher success rates but came at the cost of safety, referring mainly to the complication of PN palsy.15,17,18 PN palsy occurs more frequently in right PVs with an incidence of 2.0% ~ 24.4%.12,19,20 Our study demonstrated that the overall complication rate were not significantly different between using the two CBs, while ablation using 23-mm CB only had a similar rate of acute PVI on PV level and nonsignificant higher rate on patient level comparing with using 28-mm CB only. It is worth mention that the only one case of PN palsy (1.7%) occurred when using 28-mm balloon, this indicates that, with the improvement of operators’ skills and monitoring methods, smaller CB can be just as safe as the bigger CB while achieving comparable or even higher efficacy when using for the selected patients.
Study limitation
In this single-center study with a small sample, PV anatomy variations might only partially represent the universal situation among population; BNT cut-point < -51ºC was just used to facilitate the analysis and it is not a cut-point between effective and non-effective ablation, so was the cryo kinetic effect not equal to ablation effect. As SCs were used not only to record PV potentials, but also to support the CBs, real-time PV isolation recording, a more direct and better parameter to evaluate acute ablation effect, could only be achieved in some of the patients. However, this situation is expected to change with the progress of technology and manipulation skills,21 and investigation of relationship between PV anatomy and real time isolation will be the future research direction. Current results only apply to the use of first-generation CB. With the spreading use of CB second generation, cryo kinetics needs further discussion. In addition, the evaluation of PV anatomy was carried out with Carto system in electrophysiological lab for convenience and efficiency. Other post processing platforms and reconstructing software could also be used for analysis.
Conclusions
MDCT images can provide accurate evaluation of PV ostial anatomy and preprocedural guidance for CB ablation. PV anatomy is associated with cryo kinetics, and PV diameter plays a more prominent role when using 23-mm CBs, while PV location is more prominent when using 28-mm CBs.
Footnotes
Sources of Funding
There were no external funding sources for this study
Study Association
This study is not associated with any thesis or dissertation work.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Fuwai Hospital under the protocol number 2013078. All the procedures in this study were in accordance with the 1975 Helsinki Declaration, updated in 2013. Informed consent was obtained from all participants included in the study.
Author contributions
Conception and design of the research: Xiongbiao C, Pihua F, Tang M; Acquisition of data and Critical revision of the manuscript for intellectual content: Xiongbiao C, Pihua F, Zheng L, Jia H, Tang M, Jun L, Bin L, Shu Z; Analysis and interpretation of the data: Xiongbiao C, Pihua F, Zheng L, Jia H, Tang M, Jun L, Bin L; Statistical analysis: Xiongbiao C, Pihua F, Zheng L, Jun L; Writing of the manuscript: Xiongbiao C.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Kuck KH, Brugada J, Furnkranz A, Metzner A, Ouyang F, Chun KR, et al. FIRE AND ICE Investigators Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374(23):2235–2245. doi: 10.1056/NEJMoa1602014. [DOI] [PubMed] [Google Scholar]
- 2.Chun KR, Brugada J, Elvan A, Geller L, Busch M, Barrera A, et al. FIRE AND ICE Investigators The impact of cryoballoon versus radiofrequency ablation for paroxysmal atrial fibrillation on healthcare utilization and costs: an economic analysis from the FIRE AND ICE trial. J Am Heart Assoc. 2017;6(8) doi: 10.1161/JAHA.117.006043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kojodjojo P, Wyn Davies D. How to perform antral pulmonary venous isolation using the cryoballoon. Heart Rhythm. 2011;8(9):1452–1456. doi: 10.1016/j.hrthm.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 4.Furnkranz A, Koster I, Chun KR, Metzner A, Mathew S, Konstantinidou M, et al. Cryoballoon temperature predicts acute pulmonary vein isolation. Heart Rhythm. 2011;8(6):821–825. doi: 10.1016/j.hrthm.2011.01.044. [DOI] [PubMed] [Google Scholar]
- 5.Ghosh J, Martin A, Keech AC, Chan KH, Gomes S, Singarayar S, et al. Balloon warming time is the strongest predictor of late pulmonary vein electrical reconnection following cryoballoon ablation for atrial fibrillation. Heart Rhythm. 2013;10(9):1311–1317. doi: 10.1016/j.hrthm.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 6.Sorgente A, Chierchia GB, de Asmundis C, Sarkozy A, Namdar M, Capulzini L, et al. Pulmonary vein ostium shape and orientation as possible predictors of occlusion in patients with drug-refractory paroxysmal atrial fibrillation undergoing cryoballoon ablation. Europace. 2011;13(2):205–212. doi: 10.1093/europace/euq388. [DOI] [PubMed] [Google Scholar]
- 7.Knecht S, Kuhne M, Altmann D, Ammann P, Schaer B, Osswald S, et al. Anatomical predictors for acute and mid-term success of cryoballoon ablation of atrial fibrillation using the 28 mm balloon. J Cardiovasc Electrophysiol. 2013;24(2):132–138. doi: 10.1111/jce.12003. [DOI] [PubMed] [Google Scholar]
- 8.Schmidt M, Dorwarth U, Straube F, Daccarett M, Rieber J, Wankerl M, et al. Cryoballoon in AF ablation: Impact of PV ovality on AF recurrence. Int J Cardiol. 2013;167(1):114–120. doi: 10.1016/j.ijcard.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 9.Kubala M, Hermida JS, Nadji G, Quenum S, Traulle S, Jarry G. Normal pulmonary veins anatomy is associated with better AF-free survival after cryoablation as compared to atypical anatomy with common left pulmonary vein. Pacing Clin Electrophysiol. 2011;34(7):837–843. doi: 10.1111/j.1540-8159.2011.03070.x. [DOI] [PubMed] [Google Scholar]
- 10.Schwartzman D, Lacomis J, Wigginton WG. Characterization of left atrium and distal pulmonary vein morphology using multidimensional computed tomography. J Am Coll Cardiol. 2003;41(8):1349–1357. doi: 10.1016/s0735-1097(03)00124-4. https://doi.org/10.1016/S0735-1097(03)00124-4 [DOI] [PubMed] [Google Scholar]
- 11.Marom EM, Herndon JE, Kim YH, McAdams HP. Variations in pulmonary venous drainage to the left atrium: implications for radiofrequency ablation. Radiology. 2004;230(3):824–829. doi: 10.1148/radiol.2303030315. [DOI] [PubMed] [Google Scholar]
- 12.Vogt J, Heintze J, Gutleben KJ, Muntean B, Horstkotte D, Nolker G. Long-term outcomes after cryoballoon pulmonary vein isolation: results from a prospective study in 605 patients. J Am Coll Cardiol. 2013;61(16):1707–1712. doi: 10.1016/j.jacc.2012.09.033. [DOI] [PubMed] [Google Scholar]
- 13.Mansour M, Holmvang G, Sosnovik D, Migrino R, Abbara S, Ruskin J, et al. Assessment of pulmonary vein anatomic variability by magnetic resonance imaging: implications for catheter ablation techniques for atrial fibrillation. J Cardiovasc Electrophysiol. 2004;15(4):387–393. doi: 10.1046/j.1540-8167.2004.03515.x. [DOI] [PubMed] [Google Scholar]
- 14.Kaseno K, Tada H, Koyama K, Jingu M, Hiramatsu S, Yokokawa M, et al. Prevalence and characterization of pulmonary vein variants in patients with atrial fibrillation determined using 3-dimensional computed tomography. Am J Cardiol. 2008;101(11):1638–1642. doi: 10.1016/j.amjcard.2008.01.053. Erratum in: Am J Cardiol. 2008;102(4):508. [DOI] [PubMed] [Google Scholar]
- 15.Sarabanda AV, Bunch TJ, Johnson SB, Mahapatra S, Milton MA, Leite LR, et al. Efficacy and safety of circumferential pulmonary vein isolation using a novel cryothermal balloon ablation system. J Am Coll Cardiol. 2005;46(10):1902–1912. doi: 10.1016/j.jacc.2005.07.046. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt M, Dorwarth U, Straube F, Daccarett M, Rieber J, Wankerl M, et al. Cryoballoon in AF ablation: impact of PV ovality on AF recurrence. Int J Cardiol. 2013;167(1):114–120. doi: 10.1016/j.ijcard.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 17.Van Belle Y, Janse P, Rivero-Ayerza MJ, Thornton AS, Jessurun ER, Theuns D, et al. Pulmonary vein isolation using an occluding cryoballoon for circumferential ablation: feasibility, complications, and short-term outcome. Eur Heart J. 2007;28(18):2231–2237. doi: 10.1093/eurheartj/ehm227. [DOI] [PubMed] [Google Scholar]
- 18.Furnkranz A, Chun KR, Nuyens D, Metzner A, Koster I, Schmidt B, et al. Characterization of conduction recovery after pulmonary vein isolation using the “single big cryoballoon” technique. Heart Rhythm. 2010;7(2):184–190. doi: 10.1016/j.hrthm.2009.10.038. [DOI] [PubMed] [Google Scholar]
- 19.Martins RP, Hamon D, Cesari O, Behaghel A, Behar N, Sellal JM, et al. Safety and efficacy of a second-generation cryoballoon in the ablation of paroxysmal atrial fibrillation. Heart Rhythm. 2014;11(3):386–393. doi: 10.1016/j.hrthm.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 20.Casado-Arroyo R, Chierchia GB, Conte G, Levinstein M, Sieira J, Rodriguez-Manero M, et al. Phrenic nerve paralysis during cryoballoon ablation for atrial fibrillation: a comparison between the first- and second-generation balloon. Heart Rhythm. 2013;10(9):1318–1324. doi: 10.1016/j.hrthm.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 21.Reissmann B, Wissner E, Deiss S, Heeger C, Schlueter M, Wohlmuth P, et al. First insights into cryoballoon-based pulmonary vein isolation taking the individual time-to-isolation into account. Europace. 2017;19(10):1676–1680. doi: 10.1093/europace/euw233. [DOI] [PubMed] [Google Scholar]