Abstract
Problem:
Medical school curriculum continues to search for methods to develop a conceptual educational framework that promotes the storage, retrieval, transfer, and application of basic science to the human experience. To achieve this goal, we propose a metacognitive approach that integrates basic science with the humanistic and health system aspects of medical education.
Intervention:
During the week, via problem-based learning and lectures, first-year medical students were taught the basic science underlying a disease. Each Friday, a patient with the disease spoke to the class. Students then wrote illness scripts, which required them to metacognitively reflect not only on disease pathophysiology, complications, and treatments but also on the humanistic and health system issues revealed during the patient encounter. Evaluation of the intervention was conducted by measuring results on course exams and national board exams and analyzing free responses on the illness scripts and student course feedback. The course exams and National Board of Medical Examiners questions were divided into 3 categories: content covered in lecture, problem-based learning, or patient + illness script. Comparisons were made using Student t-test. Free responses were inductively analyzed using grounded theory methodology.
Context:
This curricular intervention was implemented during the first 13-week basic science course of medical school. The main objective of the course, Scientific Principles of Medicine, is to lay the scientific foundation for subsequent organ system courses. A total of 150 students were enrolled each year. We evaluated this intervention over 2 years, totaling 300 students.
Outcome:
Students scored significantly higher on illness script content compared to lecture content on the course exams (mean difference = 11.1, P = .006) and national board exams given in December (mean difference = 21.8, P = .0002) and June (mean difference = 12.7, P = .016). Themes extracted from students’ free responses included the following: relevance of basic science, humanistic themes of empathy, resilience, and the doctor-patient relationship, and systems themes of cost, barriers to care, and support systems.
Lessons learned:
A metacognitive approach to learning through the use of patient encounters and illness script reflections creates stronger conceptual frameworks for students to integrate, store, retain, and retrieve knowledge.
Keywords: Illness scripts, metacognition, patient encounters, basic science
Introduction
Cognitive integration of basic science with clinical experience improves diagnostic reasoning.1 An illness script is a schema by which clinicians integrate information to understand a clinical presentation and link formal knowledge with experiential clinical encounters.2 Expert clinicians often depend on this method to make memory connections that aid in recognizing possible differential diagnoses.3,4 Medical students do not usually get this training until third year of medical school during clinical rotations. We propose that illness scripts can be used early in medical school training, in basic science courses. By linking science to the human experience, a metacognitive approach can reinforce conceptual scaffolding with personal, emotional connections.
The 4 main pillars of medical education at our institution are scientific knowledge, clinical practice, humanities, and health systems.5,6 Although the exact themes may vary between institutions, the challenge many medical schools face is finding an effective way to integrate similar themes into their curriculum.7,8 Although some courses may easily lend themselves to such integration,9 other courses, for example those heavy in the basic sciences, find it difficult. Our research analyzes the use of illness scripts to integrate humanistic and health system issues in the basic science course, Scientific Principles of Medicine (SPM).
Illness scripts were first introduced into the medical literature by Professor Clancey10 in the 1980s. These scripts were designed as an educational tool for clinical rotations. Students would describe a disease’s pathogenesis, presentation, diagnosis, and treatment and then correlate this information to a specific, real-life patient they observed during their rotation. Scripts are believed to facilitate information storage in long-term memory which can then be activated by trainees at subsequent encounters either on a test or in a clinical setting.11 In other words, they guide student information selection, memorization, and interpretation.12 The effectiveness of this tool is supported by today’s current medical educational theory, which suggests that students learn material through gists and schema rather than pure memorization of facts and figures.13 Indeed, learning medicine in this manner prepares students to become expert clinicians14 because medical diagnoses are an explanation and correlation of symptoms made on the basis of biomedical knowledge.15 Integrating basic science with clinical sessions is felt to increase understanding and application of the scientific material.16
The first objective of this article is to compare the understanding and retention of medical knowledge learned through the 3 educational methods used in the SPM class: lecture-based pedagogy, constructivist learning with problem-based learning (PBL), and the metacognitive approach with patient encounters and illness scripts. We used the results of the SPM midterm and final exams to represent short-term learning and the results of the standardized National Board of Medical Examiners (NBME) exam 3 and 8 months later to represent learning retention and retrieval.
The second objective of this article was to explore the ability of patient encounters and illness scripts to integrate clinical medicine, humanities, and health systems into a basic science course. Humanities and health systems education are crucial themes for a well-rounded medical education.17–19 Integrating these themes into a basic science course can be challenging. To address this problem, free response humanities and health system sections were added to the illness scripts. The free responses were inductively analyzed using grounded theory methodology.
Methods
The data used in this study were approved as part of the education research registry, which was approved by the College of Medicine Institutional Review Board (#STUDY00000123).
Each year from August through October, 150 first-year medical students take SPM, a basic science course whose main objective is to lay the scientific foundation for the subsequent organ system blocks. SPM is 13 weeks in duration. There is a formative midterm assessment and a summative final assessment composed of multiple-choice and short answer responses.
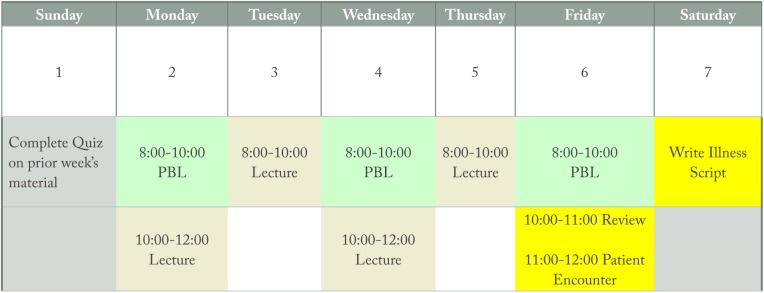
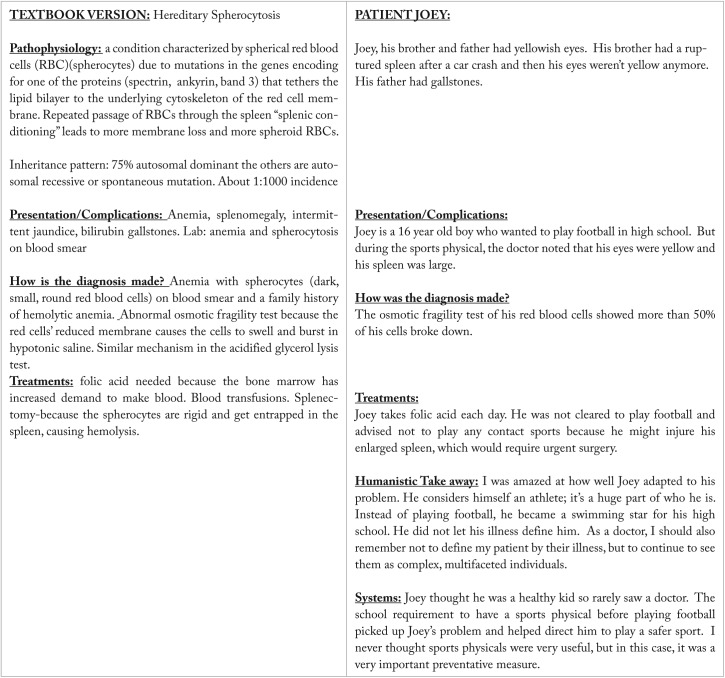
The SPM curriculum is organized by week. Each week covers 2 active-learning PBLs for 2 hours every Monday, Wednesday, and Friday. There are 2 hours of lecture each day from Monday through Thursday. On Friday, a 1-hour integration/review session with questions and answers is followed by a 1-hour patient encounter (Figure 1). The patient encounter is mandatory, it is not videotaped, students dress professionally and wear their white coats, computers are closed, note taking is discouraged, and listening and interacting is encouraged. The patients who speak have an illness that was discussed either in PBL or in lecture. For example, 1 week in PBL, students learned about the cystic fibrosis transmembrane regulator (CFTR) protein and sodium-chloride-water transport. On Friday, a patient with cystic fibrosis spoke to the class. An illness script regarding this encounter was due by Sunday evening. The illness script was formatted with the textbook version in column 1 and the patient version in column 2 (Figure 2). The categories addressed in each version were pathophysiology, presentation, diagnosis, treatment, humanistic take-away, and health systems issues.
Figure 1.
Weekly SPM schedule template. PBL indicates problem-based learning; SPM, Scientific Principles of Medicine.
Figure 2.
Example of illness script.
Patients had the following illnesses: celiac disease, cystic fibrosis, diabetes mellitus, multidrug-resistant infection, HIV, lynch syndrome, myasthenia gravis, osteogenesis imperfecta, glycogen storage disease, muscular dystrophy, and phenylketonuria. Often spouses, family, the patient’s physician, or nurse-coordinator accompanied the patient. The patient was given the opportunity to describe how they were diagnosed, the life adjustments that were required to live with their condition, and the issues that arose during treatment. Time was allotted for questions from the student audience.
The results of this study are presented in a sequential exploratory mixed-methods approach.
Qualitative data from 300 students over 2 years were acquired via written student illness scripts which included the free response sections addressing humanism and health systems and the end of the course student feedback. The scripts were evaluated with a thematic analysis approach.20 Team members developed ideas about patterns and meanings. One team member developed a codebook by randomly selecting 15 representative illness scripts from each of the patient sessions over the 2 years and assigning codes to repetitive ideas. The team extrapolated from the literature that approximately 12 field interviews were sufficient to obtain data saturation.21 ATLAS.ti 8.0 software was used to manage the data. Once verified, codes were grouped into themes according to similarities. Using the newly developed codebook, 2 other team members each independently coded sections of relevant text from the 15 random illness scripts. Updating and changing the codebook was done among the 3 members until consensus was achieved and theoretical saturation was reached.
Quantitative data was obtained over 2years from 300 students, 4 SPM exams, and 4 practice NBME exams. The SPM midterm and final exams were administered 6 and 13 weeks into the course, respectively. We considered the SPM exams a measurement of short-term memory. The exams were 60% multiple choice questions and 40% short answer responses. The NBME exams were administered in December, 2 months after the SPM course ended, and June, 8 months after SPM. We considered the NBME exams results to be an indicator of more long-term memory. The NBME exams were 100% multiple choice questions. Students took the NMBE exams as Step 1 practice, with no additional preparation.
A team member, blinded from exam question scores, identified the category of each exam question’s content. Each question on the SPM and NBME exams was selected into 1 of 3 categories based on where the content was taught during the SPM course: lecture only, PBL only, or patient + illness script. The SPM exam data are given as the class total correct cumulative points. The NBME data are given as the percentage of students who answered the question correctly. For statistical analysis, the lecture based questions served as the standard baseline. Averages were compared using a paired student’s t-test with significance defined as p<0.05. Mean differences compared to the lecture group were then calculated with a confidence interval set at 95%.
Results
Qualitative results revealed 7 main themes: patients make the basic science relevant, empathy and awareness, patient resilience, the doctor-patient relationship, cost of care, barriers to care, and support systems.Tables 1 to 3 outline the themes that were derived from the qualitative free response portion of the illness scripts matched with representative quotes.
Table 1.
Qualitative theme of relevance with representative quotes.
| Theme | Subtheme | Representative quotes |
|---|---|---|
| Relevance | Patients bring relevance to the basic sciences | Because of this encounter, if just one of us remembers and considers Lynch syndrome when we see a patient with multiple cancers, that may be one more life saved. |
| The patient encounter was insightful and solidified my learning. It furthered my knowledge of cystic fibrosis and how it can affect both the medical and emotional aspects of a person’s life. | ||
| The encounter allowed us to put a face and interaction to a disease. | ||
| If it wasn’t for this presentation, I would not have understood the full gravity of the more severe forms of osteogenesis imperfecta. | ||
| The system of newborn screening has clearly shown excellent results for the PKU patients. It correctly identified the disease and allowed them to immediately restrict diets and avoid complications. | ||
| They taught me the importance of using the patient as a resource for better understanding their disease. |
Abbreviation: PKU, phenylketonuria.
Table 3.
Qualitative health system themes with representative quotes.
| Theme | Subtheme | Representative quotes |
|---|---|---|
| Cost of care | Insurance and payments | The patient was fortunate to be covered by insurance through his mom, who is a nurse, until he was able to work himself and be covered under his employment. |
| He notes that his insurance, with supplemental insurance from the government, has covered all of his procedures and treatments well. | ||
| Maintaining health coverage due to all her medical issues was a concern. The variation in insurance between employers can make things difficult. | ||
| The family had many problems with insurance. She complains that she wants to be healthy and treat herself properly, but must pay a copay for every visit and every surgical procedure and it has become a major financial burden. | ||
| He is insured by Medicaid and has a lot of difficulty “proving that he has a disease,” and so has struggled financially. The other patient with OI has had a very different experience. Her parents both have very good insurance plans and have been able to cover all of her surgeries and treatments easily. | ||
| He lives in a trailer home with his mom. His mattress is worn through, but he can’t get another one until the end of the year. When his wheelchair broke, he had to wait and go through a lot of hoops to get a new one. | ||
| Barriers to care | Waiting for a transplant | The progression of the transplant list is no longer linear like in the past when he was very sick, waiting to get his lung transplant. Rather than waiting for the person ahead of you to get a lung transplant or die to move up the list, the system now takes into account many factors such as quality of life and severity of the condition. |
| The major barrier he faced in the healthcare system was waiting for organs for transplantation. He was placed on a waiting list for a kidney transplant for many years. | ||
| He’s been waiting for a kidney transplant, but he got taken off the list when he had diabetic foot infections. Now he’s back on, but he can’t travel to his daughter’s college graduation or see his grandchildren out of state because if he leaves the state and a kidney becomes available, he’ll miss it. | ||
| Interference with daily living | One of the main barriers was the difficulty finding a location for dialysis, as he worked the night shift and most places were already closed by the time he would be able to arrive. | |
| It’s difficult to travel because he has to find a dialysis unit and set up M/W/F dialysis wherever he goes. | ||
| Showering with the port in was difficult since he couldn’t let the catheters get wet. | ||
| It was difficult scheduling plans around all the hospital visits. | ||
| She needed lab work and pyridostigmine for her myasthenia gravis. But she was away at college in a rural community where her prescription was not on the formulary and lab work had a two-week turnaround time. | ||
| Personal responsibility | The patient blames himself for not getting good care. He said that he knew about diabetes. His mother and father had diabetes, his father lost a leg to it. He was told how to take care of it, but he was a kid, he forgot about it and it caught up to him. | |
| As HIV treatments progressed, she experienced different side effects and she had a hard time getting herself to take the meds everyday. | ||
| Patients are apt to not take their medications daily if they are feeling well and do not understand the importance of consistent therapy. | ||
| Monitoring her diet and maintaining the cornstarch regimen every 4 hours takes a great deal of self-control, which is really hard for a teenager who wants to keep up with her friends. | ||
| Support systems | Health professionals | The patient emphasized the importance of a strong support network and a strong team of healthcare professionals in helping her manage her chronic illness. |
| She explained that it was very helpful to have a consistent team of doctors who understood her chronic illnesses and found it comforting to see the same nurses and healthcare professionals each time that she was admitted to the hospital. | ||
| He frequently uses the help of the CF foundation, that advocates for CF patients and their families. They provide legal advice/information, help deal with insurance companies, offer nutritional advice and help CF patients enroll in various assistance programs. This foundation also reviews and provides guidelines to CF-specialists. | ||
| B’s care team has assisted with his home care, so he can live at home and have his needs met with family assistance. B has also found support and resources through MDA (Muscular Dystrophy Association), through which he attended camp for 10 years. | ||
| B has an interdisciplinary care team consisting of neurology, physical therapy, orthopedics, pulmonology, cardiology, bracing and wheelchair makers. | ||
| Family and community | Mr. S has the support of his wife who makes sure that his wound is bandaged and taken care of. | |
| She also stressed the importance of peer and family support and being willing to ask friends for help rather than trying to do everything alone. | ||
| She acknowledges how much her support system has helped her overcome challenges. Her story emphasizes the role of community in maintaining the physical and emotional health of a patient. | ||
| I’m amazed at the strength and fortitude of these mothers. They adjust their lives to provide a daily routine for their children so it is just part of life: whether it’s getting up every 4 hours to give her daughter with von Gierkes disease corn starch, or teaching her child to be “PKU strong” with a special diet or managing the insulin on her type I diabetic child, or attending school everyday pushing the wheelchair for her child with osteogenesis imperfecta. | ||
| 19 year old Z. with PKU is now the person who comes to the clinic to talk to parents to calm their fears and prove that their child will be OK and grow up normally. They have become mentors to others families with PKU. |
Abbreviations: OI, osteogenesis imperfecta; PKU, phenylketonuria; CF, cystic fibrosis.
Table 2.
Qualitative humanities themes with representative quotes.
| Theme | Subtheme | Representative quotes |
|---|---|---|
| Developing Empathy | Student self-awareness | The most important thing is to empathize rather than pass judgment. Judgment leads to sadness/depression which eventually leads to poorer outcomes. |
| This made me see how a disease can impact so many aspects of an individual’s life. | ||
| Prior to this encounter I think it was easy to think that people like her were the cause of their own complications. However, it is not that simple. | ||
| There is a lot of science to learn in medical school, but it’s quintessential that in the process of trying to become doctors that the basic human need to connect to another person is not forgotten. | ||
| I took away from this the importance of connecting with your patients. Patients are people and do better when they are seen as such, instead of a condition. | ||
| He reminded all of the students about the idea that the patient knows their disease very well, so listen to them and observe them before you act. He specifically mentioned instances when nurses and doctors would grab his arms and legs and break bones without taking a moment to assess the situation or think. | ||
| When I heard that a patient with HIV was to speak at our patient encounter, I didn’t know what to expect. Even though I try to avoid stereotyping patients or defining them by their illnesses, it was difficult not to picture someone with an HIV diagnosis as emaciated, sickly, and/or bitter about their situation and fate. Yet T fit none of these descriptions. In fact, she was vibrant, passionate, diplomatic, and frankly very healthy looking. Her demeanor made me completely rethink my previous conceptions about patients with HIV or AIDS. It is one thing to read about a condition in a textbook, and quite another to look it straight in the face. Her words certainly had an effect on me. | ||
| Her words certainly had an effect on me. In the future, I will try to approach all my interactions with HIV patients with a new and fresh outlook, distancing myself from any biases or preconceived notions that could obscure my view of the patients as individuals. | ||
| Doctor-Patient Relationship | Continuity | The patient mentioned just how significant the “physician-patient” relationship was, and how it played a major role in his ability to overcome his complications. |
| He received most of his care from 2 physicians in particular, which allowed him to received continuity of care and better quality treatment. | ||
| He spoke very highly of his doctor of the last 20 years. He said that he would often call his doctor on weekends and at night, and his doctor was always willing to take the time to help. | ||
| Trust | He was fortunate to have a physician who understood how the system works and knew to place him on the renal/pancreatic transplant list. | |
| Best experiences have been when physicians treat patients more than “science on slides” and more like real people. Good physicians are those with “hopes and plans.” Going the extra mile for a patient does wonders for the patient’s mind and body. | ||
| She loved her doctor for his integrity and education and for the fact that he will share with her anything new or recently discovered about HIV and keep her updated about everything. | ||
| She felt that some healthcare professionals were discriminatory against her HIV status and that some doctors were too overworked to spend time to deeply care about her. | ||
| I think it is important to never lose sight of the patient. Being able to see past the disease is of utmost importance when anyone comes to you for assistance as a physician. Listen to the patient, look them in the eyes when they are talking to you, and form that lifelong relationship built on trust. | ||
| Advocacy | Dr. B played a pivotal role by reassuring the mothers that everything was going to be okay. There are many people (physicians and staff alike) working within local hospitals who weren’t able to explain PKU to these concerned mothers. A’s mother emphasized the importance of doctors being the patient’s number one advocate. | |
| As a doctor, we are our patients’ first advocate. We have the power to reassure our patients through difficult times and also to advocate for legislation that would support them. | ||
| Lab values are just numbers, and it is up to the provider to keep the patient on track with managing the disease and encourage them not to give up hope. | ||
| RD is so grateful to his doctor who went out of his way and pushed hard to keep him on the transplant list. | ||
| Resilience | Appreciation of life | He is someone who appreciates life, and it was apparent that he wanted us to understand why he felt that way. |
| All three patients have been appreciating their quality of life despite their cancer/high probability of developing cancers. | ||
| As an individual with a chronic illness sometimes he wondered “why me” but he overall has learned to live with his disease and is very thankful for his “second chance” at life after his transplantation. He took a moment to mention that he still has a very fulfilling life. He got to meet his lung donor’s family and still keeps in contact with them and he is very thankful for that. | ||
| I was blown away by this patient encounter. His determination to use his life as a means to better the world, despite what unfortunate circumstances define his own is absolutely amazing. It puts everything into perspective. No matter how bad things seem sometimes, there’s always someone who has it worse. We take things for granted, the ability to talk, to play, to sneeze without breaking ribs. If he can find the motivation to live and enjoy life at least to some extent, then those of us here, healthy and able, need to find that motivation too. This patient embodied resilience in every way, and I drew much motivation from him to make the most out of my life. | ||
| She was very honest with us, discussing her past substance abuse, prostitution, and what some would define as poor choices without shame or regret. She even went so far as to classify herself as fortunate for contracting HIV. For T, having AIDS was her “purpose in life.” In this respect, she is very inspirational. I don’t think that I would similarly be able to have such a diagnosis yet remain so positive. She is dedicated to her family, her husband, and her calling to educate others about HIV to remove the stigma surround the diagnosis. | ||
| Disease does not define the person | He is a strong believer that your disease doesn’t have to hold you back if you don’t let it, which he proved by becoming an athletic trainer with many athletic organizations. This makes me realize that the tiny setbacks in my life should never trip me up. | |
| Mr. V seems committed to not allowing his disease prevent him from living his life in the way he desires. The only difference between a healthy individual and the patient is a single amino acid. | ||
| He does not want his disease to define who he is. He tries to maintain a normal life and wants to be treated just like everyone else. | ||
| Both patients have lives beyond their disease that are just as important to know about. | ||
| D has to basically live his life on egg shells and the way that he handles the pain of constantly breaking bones is remarkable. If someone wants to see the face of resilience and what it means to overcome suffering, they should look at him. | ||
| R exemplified how important it was to her to not let the symptoms of OI get in the way of leading a healthy, active lifestyle. Although she takes caution in her pursuits, R still runs and swims regularly, and considers sports to be a major part of her lifestyle. She has not let the disease limit her boundaries of enjoyment and fulfillment. |
Abbreviations: OI, osteogenesis imperfecta; PKU, phenylketonuria.
The quantitative data revealed that patient + illness script SPM questions were answered significantly more correctly than lecture questions. PBL question results were not significantly different than lecture question results on the SPM exams. Both PBL and patient + illness script NBME questions were answered correctly more often than lecture questions in both the December and June exams. The patient + illness script questions scored better than the PBL questions. As would be expected, the average percent correct for all question categories declined over time. There was a 7% to 16% decrease in all test scores from the December exam to the June exam, 6 months later.
Discussion
John Dewey the father of pragmatist teaching theory believed that “School should be less about preparation for life and more like life itself.”22,23 Although we set out to address 2 objectives, the first: best methods for learning retention and retrieval and the second: integrating humanities and health sciences into a basic science medical school course, we completed this research project with a more complete understanding that these objectives are not separate entities but are one integrated objective. The multiple learning contexts used in the SPM course created a conceptual framework that enhanced abstraction of relevant features, promoted transfer to new situations, and improved retrieval and application of knowledge.
What we found was that each of our learning methods added a new beam of support to our students’ educational scaffolding. Lectures, considered a “banking model” where faculty make deposits that students receive, lay down the foundation of factual knowledge.24 First-year students, novices to medicine, tend to approach this learning style with memorization and surface level understanding committed to short-term memory, frequently failing to extract the meaning and relevance of the information. Next, we added on the constructivist approach with PBLs, where students are at the center of learning; where they create their own knowledge. With this approach, students explore, investigate, make connections, and collaborate.25,26 What we added, that most medical schools fail to do, is the final beam to complete the scaffolding, metacognition. Through our patient encounters and illness scripts, we discovered that students developed internal conversations reconciling their preconceived notions with new knowledge, connecting and applying knowledge, as John Dewey23 would say, to “life itself.”
We learned from the free response section of the illness scripts that the human element experienced in the patient encounter created an emotional connection to the subject matter (Tables 1 to 3). We know that emotion stimulates an entire system of cerebral connections involving memory consolidation, memory encoding and formation, and memory retention.27,28 Patients told very personal and often emotional stories to which we saw students empathize with and reflect upon. Adding the illness scripts prompted the students to reflect on and write about the human experience, the medical science and the health systems that led to that experience. But most importantly, the students reflected on how they will approach such an experience as a future physician.
As seen in Table 4, adding on PBL (constructivist learning method) improved test scores especially in the retrieval from long-term memory, compared to lecture based only. Although the literature is mixed regarding specific grade differences between PBL and lecture (ie, students with a PBL-based curriculum do not necessarily score higher on standardized exams compared with students with a lecture-based curriculum), the idea that PBL increases long-term knowledge retention and enhances self-directed learning is well founded.29,30 Adding on the level of metacognition with the patient encounters/illness scripts, we see an even better effect on both short-term and long-term knowledge retrieval. There is currently limited research on live patient encounters with illness scripts and learning retention in basic science classes. Scripts increase clinical reasoning and performance, but their effect on exams is relatively unstudied.3,31 Our results demonstrate that students transferred their learning from the conceptual framework in SPM that included PBL and patient encounters/illness scripts to questions asked on a national standardized test. We believe that this additional layer of emotional-humanistic metacognition focuses the students’ attention to better understand, integrate, store, retrieve, transfer, and apply their learning.
Table 4.
Test scores divided by content: lecture based, PBL based, and patient/illness script based.
| Lecture | PBL | Patient/illness script | Lecture vs PBL |
P-value | Lecture vs patient/illness script |
P-value | |
|---|---|---|---|---|---|---|---|
| Mean difference 95% CI |
Mean difference 95% CI |
||||||
| SPM 2015/2016 | N = 101 | N = 27 | N = 57 | ||||
| Average number correct | 117.3 ± 26 | 124.8 ± 18 | 128.4 ± 20 | 7.4 (−16.20, 31.0) | .162 | 11.1 (3.02, 19.80) | .006 |
| December 2015-2016 NBME | N = 100 | N = 17 | N = 15 | ||||
| Average percent correct | 60.3 ± 21 | 77.7 ± 15 | 82.1 ± 13 | 17.4 (0.064, 0.28) | .002 | 21.8 (0.10, 0.33) | .0002 |
| June 2016-2017 NBME | N = 100 | N = 23 | N = 16 | ||||
| Average percent correct | 53.5 ± 20 | 63.2 ± 19 | 66.3 ± 16 | 9.6 (0.004, 0.18) | .038 | 12.7 (0.02, 0.23) | .016 |
Abbreviations: CI, confidence interval; NBME, National Board of Medical Examiners; PBL, problem-based learning; SPM, Scientific Principles of Medicine.
Not only did this added layer of metacognition in our educational framework improve test scores, it was enjoyable. Student feedback was unanimously positive with frequent comments that the patient encounter was their favorite part of SPM and that they looked forward to it every Friday. After moving on from SPM, students inquire, why doesn’t every course have a Friday patient encounter? Students also appreciate that they are not to take notes and that they are to listen and interact. The patient portion of the illness scripts comes from the memory of the event, what they recall, not what they wrote notes about. On class feedback, the most common remark was that the patient encounter made their week of studies relevant to their purpose of becoming a doctor.
Limitations to this study include the differences in quantitative data points. In all exams, there were more lecture-content questions than PBL or patient/illness script content questions. Unfortunately, this limitation was unavoidable since more testable content is packed into 1 hour of lecture than 1 hour of PBL or 1 hour with a patient. Since it is impossible to bring a patient in for every illness studied each week, it is important to find a patient who embodies the essence of the week.
Patients who have taught in our class for a number of years now return with stories about their more recent hospitalizations. These patients feel fulfilled when the team of white coats exits the hospital room but a medical student lingers behind to personally thank the patient for his or her presentation in the SPM class years earlier and inform the patient that he or she is still remembered. Future studies plan to not only analyze if students keep these illness scripts and find them helpful when seeing such patients on clinical rotations or for studying for the board exams years later but also to look at the effects that patient encounters have upon the patients themselves.
In conclusion, this study supports the concept that applying metacognition through the use of patient encounters and illness scripts can be successfully employed in a basic science medical school class. Reflecting upon a patient’s experience not only promotes learning connections and retrieval of knowledge but also enhances integration of clinical medicine, humanities, and health systems into a basic science curriculum.
Acknowledgments
The authors alone are responsible for the content and writing of the article.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: Eileen F Hennrikus, MD devised and implemented the curricular design. All authors were involved in the analysis and interpretation of the curricular design, and writing and editing the manuscript.
References
- 1. Lisk K, Agur AMR, Woods NN. Exploring cognitive integration of basic science and its effect on diagnostic reasoning in novices. Perspect Med Educ. 2016;5:147-153. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4908035/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brush JE, Jr, Sherbino J, Norman G. How expert clinicians intuitively recognize a medical diagnosis. Am J Med. 2017;130:629-634. https://www.ncbi.nlm.nih.gov/pubmed/28238695. [DOI] [PubMed] [Google Scholar]
- 3. Schmidt HG, Norman GR, Boshuizen HP. A cognitive perspective on medical expertise: theory and implication. Acad Med. 1990;65:611-621. https://www.ncbi.nlm.nih.gov/pubmed/2261032. [DOI] [PubMed] [Google Scholar]
- 4. Woods NN, Brooks LR, Norman GR. It all make sense: biomedical knowledge, causal connections and memory in the novice diagnostician. Adv Health Sci Educ Theory Pract. 2007;12:405-415. https://www.ncbi.nlm.nih.gov/pubmed/17318360. [DOI] [PubMed] [Google Scholar]
- 5.http://med.psu.edu/md/hershey.
- 6. Gonzalo JD, Thompson BM, Haidet P, Mann K, Wolpaw DR. A constructive reframing of student roles and systems learning in medical education using a communities of practice lens. Acad Med. 2017;92:1687-1694. doi: 10.1097/ACM.0000000000001778 https://www.ncbi.nlm.nih.gov/pubmed/28640036. [DOI] [PubMed] [Google Scholar]
- 7. Dienstag JL. Evolution of the new pathway curriculum at Harvard Medical School: the new integrated curriculum. Perspect Biol Med. 2011;54:36-54. https://www.ncbi.nlm.nih.gov/pubmed/21399382. [DOI] [PubMed] [Google Scholar]
- 8. Wilkerson L, Stevens CM, Krasne S. No content without context: integrating basic, clinical, and social sciences in a pre-clerkship curriculum. Med Teach. 2009;31:812-821. https://www.ncbi.nlm.nih.gov/pubmed/19811186. [DOI] [PubMed] [Google Scholar]
- 9. Muller JH, Jain S, Loeser H, Irby DM. Lessons learned about integrating a medical school curriculum: perceptions of students, faculty and curriculum leaders. Med Educ. 2008;42:778-785. https://www.ncbi.nlm.nih.gov/pubmed/18627445. [DOI] [PubMed] [Google Scholar]
- 10. Clancey WJ. The epistemology of a rule-based expert system—a framework for explanation. Artif Intell. 1983;20:215-251. https://pdfs.semanticscholar.org/d0ea/2a37ebfb1323e11e809cf407904db0d4680a.pdf. [Google Scholar]
- 11. Custers EJ. Thirty years of illness scripts: theoretical origins and practical applications. Med Teach. 2015;37:457-462. https://www.ncbi.nlm.nih.gov/pubmed/25180878. [DOI] [PubMed] [Google Scholar]
- 12. Charlin B, Boshuizen HP, Custers EJ, Feltovich PJ. Scripts and clinical reasoning. Med Educ. 2007;41:1178-1184. https://www.ncbi.nlm.nih.gov/pubmed/18045370. [DOI] [PubMed] [Google Scholar]
- 13. Bobrow CG, Norman DA. Some principles of memory schemata. In: Bobrow DB, Collins A. eds. Representation and Understanding. New York: Academic Press; 1975:72-92. https://doi.org/10.1016%2FB978-0-12-108550-6.50010-0. [Google Scholar]
- 14. Schmidt HG, Rikers RM. How expertise develops in medicine: knowledge encapsulation and illness script formation. Med Educ. 2007;41:1133-1139. https://www.ncbi.nlm.nih.gov/pubmed/18004989. [DOI] [PubMed] [Google Scholar]
- 15. Custers E, Boshuizen H, Schmidt H. The role of illness scripts in the development of medical diagnostic expertise: results from an interview study. Cognition Instruct. 1998;16:4367-4398. doi: 10.1207/s1532690xci1604_1 http://doi.org/10.1207/s1532690xci1604_1. [DOI] [Google Scholar]
- 16. Peiman S, Mirzazadeh A, Alizadeh M, et al. A case based-shared teaching approach in undergraduate medical curriculum: a way for integration in basic and clinical sciences. Acta Med Iran. 2017;55:259-264. http://acta.tums.ac.ir/index.php/acta/article/view/5513. [PubMed] [Google Scholar]
- 17. Gonzalo JD, Haidet P, Papp KK, et al. Educating for the 21st-century health care system: an interdependent framework of basic, clinical, and systems sciences. Acad Med. 2017;92:35-39. doi: 10.1097/ACM.0000000000000951. [DOI] [PubMed] [Google Scholar]
- 18. Halperin EC. Preserving the humanities in medical education. Med Teach. 2010;32:76-79. doi: 10.3109/01421590903390585 https://www.ncbi.nlm.nih.gov/pubmed/20095779. [DOI] [PubMed] [Google Scholar]
- 19. Barron L. The impact of baccalaureate medical humanities on subsequent medical training and practice: a physician-educator’s perspective. J Med Humanit. 2017;38:473-483. doi: 10.1007/s10912-017-9457-1. [DOI] [PubMed] [Google Scholar]
- 20. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77-101. eprints.uwe.ac.uk/11735/2/thematic_analysis_revised. [Google Scholar]
- 21. Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18:59-82. doi: 10.1177/1525822X05279903. [DOI] [Google Scholar]
- 22. National Research Council. How People Learn: Brain, Mind, Experience, and School. Washington, DC: National Academy Press; 2000. http://www.csun.edu/~SB4310/How%20People%20Learn.pdf. [Google Scholar]
- 23. Dewey J. My pedogogic creed. Article II: what the school is; 1897. dewey.pragmatism.org/creed.htm. [Google Scholar]
- 24. Freire Paulo. The banking model of education. In: Provenzo EF. ed. Critical Issues in Education: An Anthology of Readings. Thousand Oaks, CA: SAGE; 2006:105-117. https://eric.ed.gov/?id=ED500192. [Google Scholar]
- 25. Dennick R. Constructivism: reflections on twenty five years teaching the constructivist approach in medical education. Int J Med Educ. 2016;7:200-205. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4939219/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jonassen D. Designing constructivist learning environments. In: Reigeluth CM, ed. Instructional-Design Theories and Models. 2nd ed. Mahwah, NJ: Lawrence Erlbaum Associates; https://www.savoiabenincasa.gov.it/wp-content/uploads/2016/04/1999-Jonassen.pdf. [Google Scholar]
- 27. Tyng CM, Amin HU, Saad MNM, Malik AS. The influences of emotion on learning and memory. Front Psychol. 2017;8:1454 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5573739/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Phelps EA. Human emotion and memory: interactions of the amygdala and hippocampal complex. Curr Opin Neurobiol. 2004;14:198-202. https://www.ncbi.nlm.nih.gov/pubmed/15082325. [DOI] [PubMed] [Google Scholar]
- 29. Norman GR, Schmidt HG. The psychological basis of problem-based learning: a review of the evidence. Acad Med. 1992;67:557-565. https://www.ncbi.nlm.nih.gov/pubmed/1520409. [DOI] [PubMed] [Google Scholar]
- 30. Thomas RE. Problem-based learning: measurable outcomes. Med Educ. 1997;31:320-329. https://www.ncbi.nlm.nih.gov/pubmed/9488851. [DOI] [PubMed] [Google Scholar]
- 31. Jones B, Brzezinski WA, Estrada CA, Rodriguez M, Kraemer RR. A 22-year-old woman with abdominal pain. J Gen Intern Med. 2014;29:1074-1078. doi: 10.1007/s11606-013-2747-z.10.1007/s11606-013. [DOI] [PMC free article] [PubMed] [Google Scholar]