Abstract
Context:
Interactions among muscle strength, pain, and self-reported outcomes in patients with anterior cruciate ligament reconstruction (ACLR) are not well understood. Clarifying these interactions is of clinical importance because improving physical and psychological function is thought to optimize outcomes after ACLR.
Objective:
To examine the relationships among neuromuscular quadriceps function, pain, self-reported knee function, readiness to return to activity, and emotional response to injury both before and after ACLR.
Design:
Descriptive laboratory study.
Patients or Other Participants:
Twenty patients (11 females and 9 males; age = 20.9 ± 4.4 years, height = 172.4 ± 7.5 cm, weight = 76.2 ± 11.8 kg) who were scheduled to undergo unilateral ACLR.
Main Outcome Measure(s):
Quadriceps strength, voluntary activation, and pain were measured at presurgery and return to activity, quantified using maximal voluntary isometric contractions (MVICs), central activation ratio, and the Knee Injury and Osteoarthritis Outcome Score pain subscale, respectively. Self-reported knee function, readiness to return to activity, and emotional responses to injury were evaluated at return to activity using the International Knee Documentation Committee questionnaire (IKDC), ACL Return to Sport After Injury scale (ACL-RSI), and Psychological Response to Sport Injury Inventory (PRSII), respectively. Pearson product moment correlations and linear regressions were performed using raw values and percentage change scores.
Results:
Presurgical levels of pain significantly predicted 31% of the variance in the ACL-RSI and 29% in the PRSII scores at return to activity. The MVIC and pain collected at return to activity significantly predicted 74% of the variance in the IKDC, whereas only MVIC significantly predicted 36% of the variance in the ACL-RSI and 39% in the PRSII scores. Greater increases in MVIC from presurgery to return to activity significantly predicted 49% of the variance in the ACL-RSI and 59% of the variance in the IKDC scores.
Conclusion:
Decreased quadriceps strength and higher levels of pain were associated with psychological responses in patients with ACLR. A comprehensive approach using traditional rehabilitation that includes attention to psychological barriers may be an effective strategy to improve outcomes in ACLR patients.
Key Words: quadriceps strength, return to sport, self-reported function, psychology of injury
Key Points
Quadriceps weakness, knee pain, and self-reported disability are commonly observed at many stages of recovery in patients with anterior cruciate ligament (ACL) reconstruction.
Presurgical levels of knee pain were associated with a participant's readiness to return to functional activity and his or her emotional response to ACL injury.
Knee pain and quadriceps strength at return to activity were associated with self-reported knee function, readiness to return to sport, and emotional response to injury in participants when cleared for unrestricted activity.
Anterior cruciate ligament (ACL) ruptures are common sporting injuries that occur in more than 250 000 Americans each year, many of whom elect to undergo surgical reconstruction (ACLR).1 Anterior cruciate ligament reconstruction is typically performed to restore static knee-joint stability and is traditionally followed by therapeutic rehabilitation focused on minimizing symptoms, restoring neuromuscular function, decreasing the risk of reinjury, and allowing patients to return to preinjury physical-activity levels.2,3 Unfortunately, quadriceps dysfunction persists, with quadriceps strength4,5 and voluntary activation6 deficits surpassing 20% at return to activity. Furthermore, approximately 23% of patients with ACLR will sustain a second ACL rupture,7,8 given that these individuals continue to exhibit alterations in lower extremity biomechanics that increase the risk of future ACL injury.9 Knee-joint pain after ACL injury is also common and can persist for years after surgery.10 In addition, individuals with ACLR describe deficits in self-reported outcomes, which are often overlooked.11 In particular, individuals with ACLR experience impaired quality of life12,13 and self-reported knee-joint dysfunction14 at return to activity and in the years after surgery. Emotional distress,15 such as changes in mood and motivation, is common and may hinder the recovery process.16,17 Also, only 54% to 63% of individuals returned to preinjury activity levels after ACLR.18,19
Interestingly, pain is one of the most commonly cited reasons for individuals not returning to preinjury activity levels,19 and quadriceps strength outcomes collected before surgery20 and at return to activity21 have been associated with a patient's self-reported knee function. These data have led researchers11,22 to theorize that self-reported responses to injury are associated with rehabilitation outcomes, such as measures of quadriceps function and pain; however, these associations are not well understood. Therefore, it seems likely that rehabilitation outcomes have the potential to influence self-reported function and that this interaction plays an important role in patients with ACL injury.11,18
Although not thoroughly investigated after musculoskeletal injury, specifically ACL injury, other areas of medicine have benefited from understanding the interaction between physical symptoms and psychological function, such as emotional responses to injury. In particular, psychological interventions have had positive effects on physical symptoms such as pain, swelling, and nausea in a wide range of patients diagnosed with cancer,23,24 osteoarthritis,25 rheumatoid arthritis,25,26 and low back pain.27 Understanding the interactions among quadriceps muscle strength, pain, and self-reported outcomes in patients with ACLR may aid clinicians in creating optimal treatment approaches, which may include both therapeutic rehabilitation and psychological counseling, to ensure that optimal physical and psychological recovery can occur. Given that psychological recovery occurs simultaneously with the restoration of physical function after ACLR, it is important to know whether the quadriceps muscle dysfunction and pain that athletes experience throughout rehabilitation are related to psychological responses when they return to activity.
Therefore, the purpose of our investigation was to examine the contributions of (1) presurgical levels of quadriceps strength, pain, and activation to self-reported knee function and readiness to return to functional activity collected when individuals with an ACLR returned to unrestricted physical activity; (2) levels of quadriceps strength, pain, and activation collected when individuals with an ACLR returned to activity on self-reported knee function, readiness to return to functional activity, and emotional response to the injury collected at the same time point; and (3) the changes in levels of pain, quadriceps strength, and activation from presurgery to return to activity on self-reported knee function, readiness to return to functional activity, and emotional response to the injury collected at return to activity. We hypothesized that pain and quadriceps function would contribute to the self-reported outcomes in individuals with ACLR in all 3 of our aims.
METHODS
Participants
Twenty participants who sustained a unilateral ACL injury and were currently scheduled to undergo surgical reconstruction were recruited via 3 orthopaedic physicians at the University of Toledo Medical Center Orthopedic Clinic. After ACLR, all participants were entered in a standardized rehabilitation program by the orthopaedic surgeon and physical therapy clinic at the University of Toledo Medical Center. Participants with a history of a lower extremity injury other than ACLR in the last 6 months or history of any other orthopaedic surgery to either lower extremity were excluded. Before enrollment, the Biomedical Institutional Review Board at the University of Toledo approved all procedures and all participants provided written informed consent.
Procedures
Participants reported to the laboratory on 2 occasions: before surgery (presurgery: 37.1 ± 15.3 days post-initial ACL injury) and once fully cleared for unrestricted physical activity by their orthopaedic surgeon (return to activity: 28.3 ± 2.9 weeks postsurgical reconstruction). At the presurgery and return-to-activity time points, quadriceps strength, voluntary activation, and levels of pain associated with their injury were assessed. Additionally, at the return-to-activity time point, participants completed self-reported outcome questionnaires to assess their responses to injury, including self-reported knee-joint function, readiness to return to functional activity, and their emotional response to the injury.
Quadriceps Strength and Voluntary Activation
Quadriceps strength was quantified bilaterally via maximal voluntary isometric contractions (MVICs). Participants were secured in an isokinetic dynamometer (model III Pro; Biodex Medical Systems, Inc, Shirley, NY) with their knees and hips in 90° of flexion. After a warm-up, participants performed MVIC trials until peak torque no longer increased, with at least 1 minute of rest between trials. To ensure maximal effort, the torque generated by the contraction was depicted in real time on a custom computer software program (Visual Basic; Microsoft Corp, Redmond, WA) and provided to the participant for visual feedback. The analog torque signal was collected from the dynamometer using a 16-bit, 1.25-millisecond samples/s A-to-D conversion board (model USB-6251; National Instruments, Austin, TX), sampled at 1000 samples/s, and displayed to the participant on a 55-cm LCD monitor.28 Torque data were low-pass filtered at 150 Hz using a second-order Butterworth filter. The absolute peak force of the trial that yielded the highest MVICs for both the injured and uninjured limbs was used for analysis and normalized to participant body mass.21 In addition, to provide a measure of symmetry, a quadriceps strength index was calculated by dividing the MVIC of the injured ACL limb by that of the uninjured limb and multiplying by 100.29
Voluntary activation was measured using the central activation ratio (CAR).30,31 Immediately after MVIC testing, two 7- × 13-cm self-adhesive stimulating electrodes were positioned on the proximal vastus lateralis and the distal vastus medialis muscles.30 An automated system was used to trigger 125 V (100-millisecond train of 10 stimuli, at 100 pulses per second, with a pulse duration of 0.6 milliseconds and a 0.01-millisecond pulse delay) of electrical stimulation to the quadriceps via a square-wave stimulator (model S48; Grass-Telefactor Corp, West Warwick, RI) and a stimulation-isolation unit (model SIU8T; Grass-Telefactor Corp) while the participant performed an MVIC.32,33 The CAR was calculated for both limbs, using the maximal torque produced by the participant divided by the maximal torque produced with the electrical stimulation and multiplying by 100. To provide a measure of symmetry, a quadriceps activation index was also calculated by dividing the CAR of the injured ACL limb by that of the uninjured limb and multiplying by 100.
Pain
The pain subscale of the Knee Injury and Osteoarthritis Outcome Score (KOOS) was used to quantitatively assess joint pain. The 42-item KOOS is a valid and reliable instrument that assesses disease-specific outcomes in young and active participants with knee injuries34 using a 5-item Likert Scale. The pain subscale (Cronbach α = 0.91; Cronbach α is a widely used, objective measure of reliability and internal consistency for a questionnaire scale, and a value >0.70 is considered satisfactory35)36 is normalized and represented as a range from 0 to 100, with greater KOOS scores representing less pain. The KOOS pain subscale was completed during all testing sessions (presurgery and return to activity).
Self-Reported Knee Function
When participants were cleared for unrestricted physical activity, the International Knee Documentation Committee self-reported questionnaire (IKDC) was used as a measure of knee function. The IKDC is a 10-item, valid, and reliable (Cronbach α = 0.95) questionnaire that is used as a global assessment of self-reported knee-joint function.37 A transformed score is calculated for each participant using the following equation and is represented as a single value ranging from 0 to 100, with greater IKDC scores representing greater self-reported knee function.38 The IKDC was completed only during the last testing session, when participants were cleared for unrestricted activity. To calculate the transformed IKDC score,
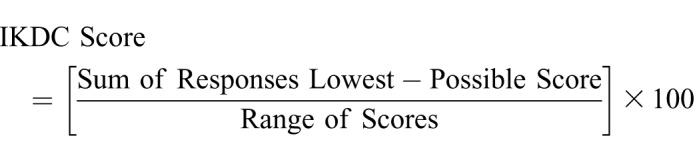 |
Readiness to Return to Activity
The ACL Return to Sport After Injury scale (ACL-RSI) was used to assess the participant's readiness to return to functional activities. It is a 12-item, valid, and reliable (Cronbach α = 0.92) questionnaire designed to evaluate specific elements associated with an athlete's readiness to return to functional activity, including his or her confidence in performance and risk appraisal.39 Each of the 12 items is scored on a scale from 0 to 100, and a final score is calculated by averaging all 12 items, with greater ACL-RSI scores indicating that participants are more ready to return to athletic activities. The ACL-RSI was completed only during the last testing session, when participants were cleared for unrestricted activity.
Emotional Response to Injury
The 19-item Psychological Response to Sport Injury Inventory (PRSII) was used to evaluate the participant's psychological health and emotional response to his or her ACL injury, surgical reconstruction, and therapeutic rehabilitation process. It is a 19-item, valid, and reliable (Cronbach α = 0.86) assessment of an individual's psychological response to a sport injury, using a 5-item Likert scale.40 The PRSII was designed to evaluate psychological factors including feelings of devastation, dispiritedness, reorganization, feeling cheated, and restlessness. Items are summed for a representative score, with lower PRSII scores representing more positive emotions associated with the injury.40 The PRSII was completed only during the last testing session, when participants were cleared for unrestricted activity.
Statistical Analysis
Initial bivariate Pearson product moment correlations were performed between independent predictor variables (MVIC of the injured limb, MVIC of the uninjured limb, MVIC of the quadriceps index, CAR of the injured limb, CAR of the uninjured limb, CAR of the quadriceps index, KOOS pain score) at each time point and the self-reported functional outcomes collected at return to activity (IKDC, ACL-RSI, and PRSII scores). The correlation coefficient (r) was classified as weak (0–0.4), moderate (0.4–0.7), or strong (0.7–1.0).41 Pearson product moment correlations were also performed between all predictor variables (Appendix).
Stepwise hierarchical multiple linear regression analyses were performed to examine the amount of variance in IKDC, ACL-RSI, and PRSII scores at return to activity that could be explained by the variance in each appropriate outcome collected either at presurgery or at return to activity (ie, multivariate predictors). The order in which the predictor variables were entered into the respective regression model was determined by the magnitude of the individual simple Pearson product moment correlations. Only predictor variables that demonstrated significant Pearson product moment correlations were entered into the regression models. The total R2 of the model was reported, as well as the change in R2 that each additional variable provided to the model.
Percentage change scores were calculated for all variables between the time points at which they were collected. Additional Pearson product moment correlations and stepwise hierarchical multiple linear regression analyses were performed in the same manner as described earlier, using the percentage change scores to determine how changes in pain and quadriceps function throughout the injury process affected self-reported outcomes collected at the return-to-activity time point.
All statistical analyses were performed using SPSS (version 23.0; IBM Corp, Armonk, NY), and the level of significance was established a priori at P ≤ .05.
RESULTS
A total of 20 participants were included in this investigation (11 females and 9 males; age = 20.9 ± 4.4 years, height = 172.4 ± 7.5 cm, mass = 76.2 ± 11.8 kg). Of the 20 participants, 11 underwent reconstruction using bone-patellar tendon-bone autografts and the remaining 9 participants, hamstrings/gracilis tendon autografts. Thirteen participants sustained concomitant meniscal damage; 7 participants underwent simultaneous meniscectomy and 6 underwent repair. Means and standard deviations, as well as percentage change scores, for all main outcome measures are found in Table 1.
Table 1.
Main Outcome Variables and Percentage Change Scores (Mean ± SD)
| Variable |
Presurgery (37.1 ± 15.3 d Postinjury) |
Return to Activity (28.3 ± 2.9 wk Postsurgery) |
Percentage Change (Presurgery to Return to Activity) |
| Maximal voluntary isometric contractions, Nm/kg | |||
| Injured limb | 2.04 ± 0.52 | 2.55 ± 0.66 | 35 ± 60 |
| Uninjured limb | 2.54 ± 0.62 | 2.77 ± 0.81 | 11 ± 36 |
| Quadriceps index maximal voluntary isometric contractions | 81.1 ± 14.2 | 90.0 ± 10.3 | 13 ± 19 |
| Central activation ratio, % | |||
| Injured limb | 0.83 ± 0.08 | 0.91 ± 0.06 | 10 ± 15 |
| Uninjured limb | 0.88 ± 0.07 | 0.93 ± 0.05 | 6 ± 10 |
| Quadriceps index central activation ratio | 94.4 ± 10.6 | 98.1 ± 7.3 | 4 ± 12 |
| Knee Injury and Osteoarthritis Outcome Score, pain | 49.8 ± 9.6 | 82.7 ± 16.5 | 73 ± 59 |
| International Knee Documentation Committee score | 77.1 ± 17.9 | ||
| Anterior Cruciate Ligament Return to Sport After Injury score | 67.2 ± 28.1 | ||
| Psychological Response to Sport Injury Inventory score | 28.5 ± 5.8 | ||
Effects of Presurgical Pain and Quadriceps Function on Self-Reported Outcomes at Return to Activity
No presurgical independent predictor variables were associated with IKDC at return to activity. However, pain at presurgery was moderately associated with both ACL-RSI and PRSII scores collected at return to activity (Table 2.1), indicating that less pain at presurgery was associated with a greater readiness to return to functional activity and more positive emotions associated with the ACL injury when participants were cleared for unrestricted activity.
Table 2.
Pearson Product Moment Correlations
| Variable |
Score at Return to Activity (P Value) |
||
| International Knee Documentation Committee |
Anterior Cruciate Ligament Return to Sport After Injury |
Psychological Response to Sport Injury Inventory |
|
| Table 2.1: Presurgery Pain and Quadriceps Function | |||
| Maximal voluntary isometric contractions | |||
| Injured limb | 0.36 (.16)a | 0.32 (.15) | −0.09 (.68) |
| Uninjured limb | 0.33 (.15) | 0.37 (.10) | −0.08 (.72) |
| Quadriceps index | 0.07 (.75) | 0.08 (.72) | −0.11 (.63) |
| Central activation ratio | |||
| Injured limb | 0.26 (.34) | 0.24 (.29) | −0.35 (.12) |
| Uninjured limb | 0.04 (.84) | 0.35 (.13) | −0.16 (.50) |
| Quadriceps index | 0.25 (.28) | 0.06 (.78) | −0.22 (.35) |
| Knee Injury and Osteoarthritis Outcome Score, pain | 0.25 (.28) | 0.56 (.01)b | −0.54 (.01)b |
| Table 2.2: Return-to-Activity Pain and Quadriceps Function | |||
| Maximal voluntary isometric contractions | |||
| Injured limb | 0.72 (<.001)b | 0.60 (.005)b | −0.59 (.01)b |
| Uninjured limb | 0.51 (.02)b | 0.51 (.02)b | −0.50 (.02)b |
| Quadriceps index | 0.14 (.54) | 0.08 (.73) | −0.02 (.92) |
| Central activation ratio | |||
| Injured limb | 0.11 (.64) | 0.02 (.92) | −0.09 (.67) |
| Uninjured limb | 0.09 (.70) | 0.02 (.92) | −0.05 (.83) |
| Quadriceps index | 0.02 (.93) | 0.01 (.97) | −0.12 (.60) |
| Knee Injury and Osteoarthritis Outcome Score, pain | 0.79 (<.001)b | 0.52 (.01)b | −0.51 (.02)b |
Correlation coefficients (r) classified as weak (0–0.4), moderate (0.4–0.7), or strong (0.7–1.0).
Significant at P ≤ .05.
Given that no presurgical variables were associated with IKDC, no regression analysis was performed. Presurgical KOOS pain was the only presurgical independent predictor variable that significantly correlated with ACL-RSI (R2 = 0.31, P = .01) and PRSII (R2 = 0.29, P = .01) scores; therefore, regression models were not performed.
Effects of Pain and Quadriceps Function Collected at Return to Activity on Self-Reported Outcomes Collected at Return to Activity
Correlation analyses indicated that less pain and greater levels of both injured- and uninjured-limb quadriceps strength collected at return to activity were associated with greater knee-joint function, greater readiness to return to functional activity, and more positive emotions connected to the injury process (Table 2.2). The multiple regression model using the injured- and uninjured-limb KOOS pain score and MVIC collected at return to activity significantly predicted 74% of the variance in IKDC; however, the KOOS pain score and injured-limb MVIC significantly predicted 73% of the variance, with the uninjured-limb MVIC adding an insignificant 1% to the model (Table 3.1). The same 3 variables also collectively explained 37% of the variance in ACL-RSI score; however, this model was driven by injured-limb MVIC values (36%), with insignificant contributions from the KOOS pain score (0%) and uninjured-limb MVIC (1%; Table 3.2). Last, the same variables collectively explained 42% of the variance in PRSII; however, this model was also driven by injured-limb MVIC values (35%), with insignificant contributions from the KOOS pain score (4%) and uninjured-limb MVIC (3%; Table 3.3).
Table 3.
Regression Analyses Performed Using Predictor Variables at the Return-to-Activity Time Point to Explain Variance in the International Knee Documentation Committee Form, Anterior Cruciate Ligament Return to Sport After Injury Inventory, and Psychological Response to Sport Injury Inventory Results
| Step |
Variable |
R2 Value |
ΔR2 Value (P Value) |
P Value |
| 3.1 International Knee Documentation Committee Form | ||||
| 1 | KOOS pain | 0.63a | 0.63a (<.001) | <.001 |
| 2 | MVIC injured limb | 0.73a | 0.10a (.02) | <.001 |
| 3 | MVIC uninjured limb | 0.74a | 0.01 (.40) | <.001 |
| 3.2 Anterior Cruciate Ligament Return to Sport After Injury Inventory | ||||
| 1 | MVIC injured limb | 0.36a | 0.36a (.005) | .005 |
| 2 | KOOS pain | 0.36a | 0.00 (.72) | .02 |
| 3 | MVIC uninjured limb | 0.37a | 0.01 (.75) | .05 |
| 3.3 Psychological Response to Sport Injury Inventory | ||||
| 1 | MVIC injured limb | 0.35a | 0.35a (.01) | .01 |
| 2 | KOOS pain | 0.39a | 0.04 (.32) | .01 |
| 3 | MVIC uninjured limb | 0.42a | 0.03 (.44) | .03 |
Abbreviations: KOOS, Knee Injury and Osteoarthritis Outcome Score; MVIC, maximal voluntary isometric contraction.
Significant at P ≤ .05.
Effects of Changes in Pain and Quadriceps Function on Self-Reported Outcomes Collected at Return to Activity
Independent predictors of the changes in KOOS pain score (r = 0.50, P = .02) and injured-limb (r = 0.77, P < .001) and uninjured-limb (r = 0.70, P < .001) MVIC were correlated with IKDC score, indicating that greater reductions in pain and greater increases in both injured- and uninjured-limb quadriceps strength from presurgery to return to activity were associated with greater self-reported knee function collected at return to activity. The overall regression model, using multivariate predictors of percentage change in pain and injured- and uninjured-limb quadriceps strength predicted 59% (R2 = 0.59, P = .02) of the variance in IKDC score collected at return to activity. However, this model was driven by the change in injured-limb MVIC (59%), with insignificant contributions from the KOOS pain score (0%) and uninjured-limb MVIC (0%; Table 4.1).
Table 4.
Regression Analyses Performed Using Change in Level of Pain and Quadriceps Strength to Explain Variance in the International Knee Documentation Committee Form, and Anterior Cruciate Ligament Return to Sport After Injury Inventory at the Return-to-Activity Time Point
| Step |
Variable |
R2 Value |
ΔR2 Value (P Value) |
P Value |
| 4.1 International Knee Documentation Committee Form | ||||
| 1 | ΔMVIC injured limb | 0.59a | 0.59a (<.001) | <.001 |
| 2 | ΔMVIC uninjured limb | 0.59a | 0.00 (.82) | .01 |
| 3 | ΔKOOS pain | 0.59a | 0.00 (.84) | .02 |
| 4.2 Anterior Cruciate Ligament Return to Sport After Injury Inventory | ||||
| 1 | ΔMVIC injured limb | 0.46a | 0.46a (.004) | .004 |
| 2 | ΔMVIC uninjured limb | 0.49a | 0.03 (.38) | .03 |
Abbreviations: KOOS, Knee Injury and Osteoarthritis Outcome Score; MVIC, maximal voluntary isometric contraction.
Significance at P ≤ .05.
Independent predictors of the changes in injured-limb (r = 0.68, P = .004) and uninjured-limb (r = 0.60, P = .001) MVIC were correlated with the ACL-RSI score, indicating that greater increases in the strength of both the injured and uninjured quadriceps from presurgery to return to activity were also associated with a greater readiness to return to functional activity collected at return to activity. The overall regression model using the percentage change in injured- and uninjured-limb quadriceps strength predicted 49% (R2 = 0.492, P = .03) of the variance in ACL-RSI scores; however, this model was driven by the change in injured-limb MVIC (46%), with an insignificant contribution from uninjured-limb MVIC (3%; Table 4.2).
DISCUSSION
The purpose of our investigation was to examine the contributions of pain and function on self-reported outcomes in participants with ACL injuries. Specifically, we sought to identify the contributions of pain and quadriceps function, individually at presurgery and at return to activity, on self-reported knee function, readiness to return to functional activity, and emotional response to ACL injury, collected at return to activity. We observed that lower levels of presurgical pain were associated with a participant being more ready to return to functional activity and having more positive emotions about the ACL injury process. Furthermore, lower levels of pain in addition to greater levels of quadriceps strength at return to activity were associated with greater knee-joint function. Greater levels of injured-limb quadriceps strength at return to activity also significantly contributed to a greater readiness to return to functional activity and more positive emotions connected to the injury. We observed that those who experienced greater increases in quadriceps strength from presurgery to return to activity were more ready to return to functional activity and reported greater levels of knee function.
Previous researchers20 observed that presurgical quadriceps strength was associated with IKDC scores at 6 months postsurgery; however, we did not find a significant association between presurgical levels of pain or quadriceps function and IKDC scores at return to activity. The strength of the association found in the current study between preoperative quadriceps strength and IKDC score at return to activity (R2 = 0.13) was similar to that reported by Logerstedt et al20 (R2 = 0.11). In addition, we observed a significant relationship between the change in the strength of both the injured and uninjured quadriceps from presurgery to return to activity and IKDC scores at return to activity, highlighting the potential clinical effect of presurgical quadriceps strength as well as the importance of intervening and maximizing muscle strength from presurgery to return to activity.
The pain score and injured- and uninjured-limb quadriceps strength collected at return to activity were all independent predictors of a participant's self-reported knee function, also collected at return to activity. However, levels of pain (partial r = 0.655) and quadriceps strength (partial r = 0.501) of the involved limb appeared to be the most influential factors, because the addition of uninjured-limb strength provided an insignificant increase of 1% of the predictive capabilities of the regression model (final regression equation: y = 0.014 + 0.617 [KOOS pain score] + 10.196 [Injured MVIC]; Table 3.1), likely due to the collinearity of quadriceps strength between limbs (r = 0.82, P = .001).
Pain has previously been associated with IKDC scores at various time points during ACL rehabilitation.42 Chmielewski et al42 reported a correlation between pain and self-reported knee function when ACLR participants returned to full physical activity (R2 = 0.67) that was similar to what we found (R2 = 0.62). However, ours is the first investigation to identify both pain and quadriceps strength at return to activity as significant contributors to self-reported knee disability, collectively predicting 73% of the variance in IKDC scores. This is an important clinical observation, given that nearly three-quarters of a participant's self-reported disability, at the time he or she was cleared for unrestricted physical activity by the physician, could be explained by the 2 clinically modifiable factors of pain and quadriceps strength.
Additionally, pain before surgery contributed to both a participant's readiness to return to functional activity and his or her emotional response to injury after ACLR. This finding implies that a participant may self-reflect on pre-operative symptoms when considering his or her perceived ability to return to functional activity and emotions regarding the injury once ultimately cleared for unrestricted physical activity.15,17,42 We find it interesting that a participant may have psychological reactions at return to activity in response to physical factors that were measured at presurgery, even though the factors and reaction were separated by surgical reconstruction and therapeutic rehabilitation. Quadriceps strength at return to activity, similar to level of pain at presurgery, was an independent predictor of a participant's readiness to return to functional activity and his or her emotional response to injury. In fact, quadriceps strength at the return-to-activity time point appeared to be a more influential predictor than level of pain at this time point, because pain insignificantly contributed 0% to 4% to IKDC and PRSII scores at return to activity (Table 3.2 and 3.3). Therefore, quadriceps strength is an important component of a participant's self-reported knee function, and it appears to be more important than pain to a participant's readiness to return to activity and emotional response to that injury. Quadriceps strength and voluntary activation have been shown to contribute to physical function43; therefore, adequate quadriceps function may lead to greater participant confidence in performance of functional activities. It is logical to assume that a greater ability to complete functional tasks would lead to an increase in a participant's perceived readiness to return to activity after injury. For instance, previous investigators15,17,43 have linked functional ability to more positive emotions associated with the injury, thus increasing athlete self-confidence in the ability to return fully. Sports medicine professionals have been encouraged to consider multiple factors when making return-to-play decisions,44 and the evidence presented here suggests that quadriceps strength and level of pain may be important components in a successful return to physical activity. In contrast, approximately 60% of the variance in readiness to return to activity was not explained by pain and strength alone. Further research is warranted to evaluate other physical (eg, past medical history, functional tests, range of motion, extent of damage) and psychological (eg, type of sport and position played, competition level, fear of reinjury, external pressure) outcomes that may influence a participant's perceived ability to return to activity.
Aside from isometric quadriceps strength, no measure of quadriceps function was associated with any of the psychological outcomes. Quadriceps activation has previously been identified as a moderator of the relationship between quadriceps strength and physical function43; thus, it was plausible to expect a significant association in the current study. Furthermore, symmetry in quadriceps strength has previously been associated with performance during hopping tasks29; however, we were unaware of any investigation that has established a relationship between symmetry in voluntary activation and levels of self-reported function. Hence, it is possible that maximal strength output is a better indicator of patient-reported outcomes; however, additional study is needed to understand the influences of voluntary activation and quadriceps strength limb symmetry on psychological function.
Our results provide further evidence for an association among pain related to quadriceps strength and self-reported outcomes after ACL injury and reconstruction. Others16,45 have suggested that improving psychological outcomes in ACL participants, such as self-reported knee function, readiness to return to functional activity, fear of reinjury, and emotional responses to injury, would help to increase the percentage of athletes who return to preinjury activity levels and aid in decreasing reinjury rates. These findings and others16,45,46 offer evidence that physical and psychological factors interact in patients with ACL injuries, further supporting the view that clinicians should gain a stronger understanding of the interventions that directly affect the patient's psychological outcomes, while also understanding when psychological referral may be necessary.45–47 Previous research on patients with arthritis25 and low back pain27 has demonstrated that those participating in psychological counseling experienced better outcomes than those who did not. It is interesting that psychological counseling not only improved psychological measures, such as anxiety and quality of life, but also appeared to have beneficial effects on pain and swelling.25–27 Although the exact mechanism behind this association remains unknown, the observed relationship between physical and psychological factors ultimately suggests that collaboration between medical and psychological professionals may be the most beneficial approach to ensuring holistic recovery and successful return to activity. Whereas some psychological interventions have demonstrated positive benefits (eg, guided imagery, relaxation training, acceptance, and commitment therapy), we need to develop effective and realistic interventions that athletic trainers, physicians, and physical therapists, as well as other health care providers, can implement to improve post-ACL physical and psychological outcomes.45 Future investigations are needed to fully explore the role of psychological interventions in rehabilitation for patients with ACL injuries.
Although we obtained a psychological assessment of each participant's readiness to return to functional activity, we did not assess whether participants returned to their preinjury level of physical activity. Instead, our data assessed how the participant perceived his or her readiness to accomplish functional tasks at the time point of clearance for unrestricted physical activity. However, participants did complete a Tegner Activity Level Scale48 at the return-to-activity time point, with a reported mean score of 5.4 ± 0.60, indicating that, on average, participants in the current study returned to some level of competitive or recreational sport. Also, we included only participants who had sustained their first ACL injury. First-time injured athletes are predisposed to experiencing more stress and are overall less confident than athletes who have had a history of injury.49 Future researchers could examine the association between physical and psychological factors among first-time injured participants and those with repetitive injuries.
CONCLUSIONS
Presurgical levels of pain were associated with a participant's readiness to return to functional activity and his or her emotional response to ACL injury. In addition, pain and quadriceps strength at return to activity were independently, but not collectively, associated with self-reported knee function, readiness to return to sport, and emotional response to injury in ACLR participants when cleared for unrestricted activity by their orthopaedic surgeon. These results provide evidence that the level of pain and MVIC at the time of return to activity collectively contributed to the IKDC score.
Appendix.
Pearson Product Moment Correlation Matrix for All Predictor Variables, r (P) a
| Variable |
Presurgery |
Postsurgery |
||||||||||||
| MVIC |
CAR |
QI |
KOOS Pain |
MVIC |
QI |
CAR |
QI |
KOOS Pain |
||||||
| Injured Limb |
Uninjured Limb |
QI |
Injured Limb |
Uninjured Limb |
Injured Limb |
Uninjured Limb |
Injured Limb |
Uninjured Limb |
||||||
| Presurgery | ||||||||||||||
| MVIC | ||||||||||||||
| Injured limb | ||||||||||||||
| Uninjured limb | 0.57 (.05) | |||||||||||||
| QI | 0.54 (.10) | −0.14 (.53) | ||||||||||||
| CAR | ||||||||||||||
| Injured limb | 0.18 (.42) | −0.14 (.55) | 0.30 (.19) | |||||||||||
| Uninjured limb | 0.13 (.57) | 0.20 (.33) | 0.00 (.99) | 0.38 (.09) | ||||||||||
| QI | 0.06 (.79) | −0.33 (.15) | 0.39 (.08) | 0.74 (.01) | −0.20 (.39) | |||||||||
| KOOS pain | 0.01 (.96) | −0.07 (.74) | –0.09 (.68) | −0.31 (.18) | −0.34 (.13) | −0.20 (.39) | ||||||||
| Postsurgery | ||||||||||||||
| MVIC | ||||||||||||||
| Injured limb | 0.19 (.41) | −0.02 (.93) | −0.06 (.77) | 0.12 (.59) | 0.06 (.79) | −0.0 (1.94) | 0.21 (.38) | |||||||
| Uninjured limb | 0.13 (.57) | 0.24 (.29) | −0.17 (.47) | −0.05 (.87) | 0.02 (.90) | −0.18 (.44) | 0.15 (.52) | 0.82 (.00) | ||||||
| QI | 0.38 (.09) | −0.07 (.75) | 0.31 (.18) | 0.25 (.28) | 0.35 (.12) | −0.08 (.71) | 0.14 (.53) | 0.30 (.19) | −0.08 (.73) | |||||
| CAR | ||||||||||||||
| Injured limb | 0.00 (1.0) | −0.08 (.73) | 0.06 (.77) | 0.04 (.86) | 0.11 (.63) | −0.07 (.74) | −0.03 (.88) | 0.37 (.10) | 0.20 (.38) | 0.10 (.66) | ||||
| Uninjured limb | 0.23 (.31) | −0.06 (.78) | 0.31 (.18) | 0.11 (.61) | 0.28 (.21) | −0.12 (.59) | −0.14 (.55) | −0.34 (.14) | 0.34 (.14) | 0.26 (.25) | 0.46 (.03) | |||
| QI | 0.23 (.31) | 0.04 (.95) | −0.23 (.31) | −0.21 (.35) | −0.17 (.47) | −0.12 (.58) | −0.01 (.95) | 0.00 (.98) | −0.05 (.51) | −0.17 (.40) | 0.54 (.02) | −0.34 (.13) | ||
| KOOS pain | 0.07 (.75) | −0.33 (.12) | 0.33 (.15) | 0.13 (.58) | 0.04 (.86) | 0.18 (.43) | 0.04 (.85) | 0.38 (.14) | 0.36 (.11) | 0.40 (.07) | 0.22 (.33) | 0.12 (.59) | 0.22 (.34) | |
Abbreviations: CAR, central activation ratio; MVIC, maximal voluntary isometric contraction; QI, quadriceps index.
Significant at P ≤ .05. Correlation coefficient (r) classified as weak (0–0.4), moderate (0.4–0.7), or strong (0.7–1.0). Boldface text indicates a significant correlation at P < .05.
REFERENCES
- 1. Griffin LY., Albohm MJ., Arendt EA., et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II Meeting, January 2005. . 2006; 34 9: 1512– 1532. [DOI] [PubMed] [Google Scholar]
- 2. Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. . 2004; 34 4: 269– 280. [DOI] [PubMed] [Google Scholar]
- 3. Daniel DM., Stone ML., Dobson BE., Fithian DC., Rossman DJ., Kaufman KR. Fate of the ACL-injured patient: a prospective outcome study. . 1994; 22 5: 632– 644. [DOI] [PubMed] [Google Scholar]
- 4. Ingersoll CD., Grindstaff TL., Pietrosimone BG., Hart JM. Neuromuscular consequences of anterior cruciate ligament injury. . 2008; 27 3: 383– 404, vii. [DOI] [PubMed] [Google Scholar]
- 5. Palmieri-Smith RM., Thomas AC., Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. . 2008; 27 3: 405– 424. [DOI] [PubMed] [Google Scholar]
- 6. Hart JM., Pietrosimone B., Hertel J., Ingersoll CD. Quadriceps activation following knee injuries: a systematic review. . 2010; 45 1: 87– 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paterno MV., Rauh MJ., Schmitt LC., Ford KR., Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. . 2012; 22 2: 116– 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wiggins AJ., Grandhi RK., Schneider DK., Stanfield D., Webster KE., Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. . 2016; 44 7: 1861– 1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Goerger BM., Marshall SW., Beutler AI., Blackburn JT., Wilckens JH., Padua DA. Anterior cruciate ligament injury alters preinjury lower extremity biomechanics in the injured and uninjured leg: the JUMP-ACL study. . 2015; 49 3: 188– 195. [DOI] [PubMed] [Google Scholar]
- 10. Lohmander LS., Ostenberg A., Englund M., Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. . 2004; 50 10: 3145– 3152. [DOI] [PubMed] [Google Scholar]
- 11. Langford JL., Webster KE., Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. . 2009; 43 5: 377– 381. [DOI] [PubMed] [Google Scholar]
- 12. Filbay SR., Ackerman IN., Russell TG., Macri EM., Crossley KM. Health-related quality of life after anterior cruciate ligament reconstruction: a systematic review. . 2014; 42 5: 1247– 1255. [DOI] [PubMed] [Google Scholar]
- 13. Filbay SR., Culvenor AG., Ackerman IN., Russell TG., Crossley KM. Quality of life in anterior cruciate ligament-deficient individuals: a systematic review and meta-analysis. . 2015; 49 16: 1033– 1041. [DOI] [PubMed] [Google Scholar]
- 14. Lepley LK. Deficits in quadriceps strength and patient-oriented outcomes at return to activity after ACL reconstruction: a review of the current literature. . 2015; 7 3: 231– 238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Morrey MA., Stuart MJ., Smith AM., Wiese-Bjornstal DM. A longitudinal examination of athletes' emotional and cognitive responses to anterior cruciate ligament injury. . 1999; 9 2: 63– 69. [DOI] [PubMed] [Google Scholar]
- 16. Brewer BW., Cornelius AE., Sklar JH., et al. Pain and negative mood during rehabilitation after anterior cruciate ligament reconstruction: a daily process analysis. . 2007; 17 5: 520– 529. [DOI] [PubMed] [Google Scholar]
- 17. Kvist J., Ek A., Sporrstedt K., Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. . 2005; 13 5: 393– 397. [DOI] [PubMed] [Google Scholar]
- 18. Ardern CL., Webster KE., Taylor NF., Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. . 2011; 45 7: 596– 606. [DOI] [PubMed] [Google Scholar]
- 19. Flanigan DC., Everhart JS., Pedroza A., Smith T., Kaeding CC. Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. . 2013; 29 8: 1322– 1329. [DOI] [PubMed] [Google Scholar]
- 20. Logerstedt D., Lynch A., Axe MJ., Snyder-Mackler L. Pre-operative quadriceps strength predicts IKDC2000 scores 6 months after anterior cruciate ligament reconstruction. . 2013; 20 3: 208– 212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pietrosimone BG., Lepley AS., Ericksen HM., Gribble PA., Levine J. Quadriceps strength and corticospinal excitability as predictors of disability after anterior cruciate ligament reconstruction. . 2013; 22 1: 1– 6. [DOI] [PubMed] [Google Scholar]
- 22. Brewer BW. Developmental differences in psychological aspects of sport-injury rehabilitation. . 2003; 38 2: 152– 153. [PMC free article] [PubMed] [Google Scholar]
- 23. Luebbert K., Dahme B., Hasenbring M. The effectiveness of relaxation training in reducing treatment-related symptoms and improving emotional adjustment in acute non-surgical cancer treatment: a meta-analytical review. . 2001; 10 6: 490– 502. [DOI] [PubMed] [Google Scholar]
- 24. Syrjala KL., Donaldson GW., Davis MW., Kippes ME., Carr JE. Relaxation and imagery and cognitive-behavioral training reduce pain during cancer treatment: a controlled clinical trial. . 1995; 63 2: 189– 198. [DOI] [PubMed] [Google Scholar]
- 25. Dixon KE., Keefe FJ., Scipio CD., Perri LM., Abernethy AP. Psychological interventions for arthritis pain management in adults: a meta-analysis. . 2007; 26 3: 241– 250. [DOI] [PubMed] [Google Scholar]
- 26. Bradley LA., Alberts KR. Psychological and behavioral approaches to pain management for patients with rheumatic disease. . 1999; 25 1: 215– 232, viii. [DOI] [PubMed] [Google Scholar]
- 27. Hoffman BM., Papas RK., Chatkoff DK., Kerns RD. Meta-analysis of psychological interventions for chronic low back pain. . 2007; 26 1: 1– 9. [DOI] [PubMed] [Google Scholar]
- 28. Lepley AS., Gribble PA., Thomas AC., Tevald MA., Sohn DH., Pietrosimone BG. Quadriceps neural alterations in anterior cruciate ligament reconstructed patients: a 6-month longitudinal investigation. . 2015; 25 6: 838– 839. [DOI] [PubMed] [Google Scholar]
- 29. Schmitt LC., Paterno MV., Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. . 2012; 42 9: 750– 759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pietrosimone BG., Selkow NM., Ingersoll CD., Hart JM., Saliba SA. Electrode type and placement configuration for quadriceps activation evaluation. . 2011; 46 6: 621– 628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Stackhouse SK., Dean JC., Lee SC., Binder-MacLeod SA. Measurement of central activation failure of the quadriceps femoris in healthy adults. . 2000; 23 11: 1706– 1712. [DOI] [PubMed] [Google Scholar]
- 32. Krishnan C., Allen EJ., Williams GN. Torque-based triggering improves stimulus timing precision in activation tests. . 2009; 40 1: 130– 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pietrosimone BG., Saliba SA., Hart JM., Hertel J., Kerrigan DC., Ingersoll CD. Effects of transcutaneous electrical nerve stimulation and therapeutic exercise on quadriceps activation in people with tibiofemoral osteoarthritis. . 2011; 41 1: 4– 12. [DOI] [PubMed] [Google Scholar]
- 34. Roos EM., Roos HP., Lohmander LS., Ekdahl C., Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure. . 1998; 28 2: 88– 96. [DOI] [PubMed] [Google Scholar]
- 35. Connelly LM. Cronbach's alpha. . 2011; 20 1: 45, 44. [PubMed] [Google Scholar]
- 36. Salavati M., Akhbari B., Mohammadi F., Mazaheri M., Khorrami M. Knee Injury and Osteoarthritis Outcome Score (KOOS); reliability and validity in competitive athletes after anterior cruciate ligament reconstruction. . 2011; 19 4: 406– 410. [DOI] [PubMed] [Google Scholar]
- 37. Irrgang JJ., Anderson AF., Boland AL., et al. Development and validation of the international knee documentation committee subjective knee form. . 2001; 29 5: 600– 613. [DOI] [PubMed] [Google Scholar]
- 38. Irrgang JJ., Anderson AF., Boland AL., et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. . 2006; 34 10: 1567– 1573. [DOI] [PubMed] [Google Scholar]
- 39. Webster KE., Feller JA., Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. . 2008; 9 1: 9– 15. [DOI] [PubMed] [Google Scholar]
- 40. Evans L., Hardy L., Mitchell I., Rees T. The development of a measure of psychological responses to injury. . 2008; 17 1: 21– 37. [DOI] [PubMed] [Google Scholar]
- 41. Cohen J. . New York, NY: Academic Press; 1977. [Google Scholar]
- 42. Chmielewski TL., Jones D., Day T., Tillman SM., Lentz TA., George SZ. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. . 2008; 38 12: 746– 753. [DOI] [PubMed] [Google Scholar]
- 43. Fitzgerald GK., Piva SR., Irrgang JJ., Bouzubar F., Starz TW. Quadriceps activation failure as a moderator of the relationship between quadriceps strength and physical function in individuals with knee osteoarthritis. . 2004; 51 1: 40– 48. [DOI] [PubMed] [Google Scholar]
- 44. Creighton DW., Shrier I., Shultz R., Meeuwisse WH., Matheson GO. Return-to-play in sport: a decision-based model. . 2010; 20 5: 379– 385. [DOI] [PubMed] [Google Scholar]
- 45. Schwab Reese LM, Pittsinger R, Yang J. Effectiveness of psychological intervention following sport injury. . 2012; 1 2: 71– 79. [Google Scholar]
- 46. Cormier ML., Zizzi SJ. Athletic trainers' skills in identifying and managing athletes experiencing psychological distress. . 2015; 50 12: 1267– 1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mann BJ., Grana WA., Indelicato PA., O'Neill DF., George SZ. A survey of sports medicine physicians regarding psychological issues in patient-athletes. . 2007; 35 12: 2140– 2147. [DOI] [PubMed] [Google Scholar]
- 48. Tegner Y., Lysholm J. Rating systems in the evaluation of knee ligament injuries. . 1985; 198: 43– 49. [PubMed] [Google Scholar]
- 49. Johnson U. The multiply injured versus the first-time-injured athlete during rehabilitation: a comparison of nonphysical characteristics. . 1996; 5 4: 293– 304. [Google Scholar]


