Abstract
Context:
Despite the high frequency of knee injuries in athletes, few researchers have studied the effects of chronologic age and stage of maturation on knee-joint kinematics in male youth soccer players.
Objective:
To use a coach-friendly screening tool to examine knee-valgus scores for players of different ages and at different stages of maturation.
Design:
Cross-sectional study.
Setting:
Academy soccer clubs.
Patients or Other Participants:
A total of 400 elite male youth soccer players aged 10 to 18 years categorized by chronologic age and stage of maturation based on their years from peak height velocity (PHV).
Main Outcome Measure(s):
Knee valgus was evaluated during the tuck-jump assessment via 2-dimensional analysis. Frontal-plane projection angles were subjectively classified as minor (<10°), moderate (10°–20°), or severe (>20°), and using these classifications, we scored knee valgus in the tuck jump as 0 (no valgus), 1 (minor), 2 (moderate), or 3 (severe).
Results:
A trend toward higher valgus scores was observed in the younger age groups and the pre-PHV group. The lowest frequency of no valgus occurred in the U18 and post-PHV groups. The highest percentages of severe scores were in the U13 and pre-PHV groups for the right limb. Knee-valgus scores were lower for both lower extremities in the U18 group than in all other age groups (P < .001) except the U16 group. Scores were lower for the post-PHV than the pre-PHV group for the right limb (P < .001) and both pre-PHV and circa-PHV groups for the left limb (P < .001). Noteworthy interlimb asymmetries were evident in the U14, U15, and circa-PHV groups.
Conclusions:
Reductions in knee valgus with incremental age and during the later stages of maturation indicated that this risk factor was more prevalent in younger players. Interlimb asymmetry may also emerge around the time of the peak growth spurt and early adolescence, potentially increasing the risk of traumatic injury.
Key Words: knee valgus, injury risk, asymmetry
Key Points
The knee-valgus mode score decreased with advancing chronologic age and during the later stages of maturation, which could be linked to enhanced relative strength and motor control.
Greater knee-valgus scores for the right limb for the sample and certain age and maturation groups indicated the potential emergence of limb dominance in elite male youth soccer players.
Quantifying the effects of chronologic age and stage of maturation on knee-valgus motion during the tuck-jump assessment will assist coaches in identifying players who demonstrate high-risk kinematics in an affordable and easy-to-administer way.
Aberrant landing mechanics appear to be more pronounced during periods of rapid growth and subsequent gains in body mass, specifically in the U13 to U15 groups and circa-peak height velocity group.
Practitioners should adopt an integrative neuromuscular training approach to program design, particularly for the U13 to U15 groups and circa-peak height velocity group, to develop fundamental movement skills and muscular strength through resistance training, balance activities, and plyometrics.
Recent data1,2 have shown a trend toward increased lower extremity injury with each sequential playing level in youth soccer players, indicating their relevance as a specific target group for injury-risk–reduction strategies. Peak height velocity (PHV) has been defined as the age at which the maximum rate of growth occurs during the adolescent growth spurt.3 A period of heightened risk occurs around this time,4 which may be due in part to rapid changes in stature and mass but is also associated with altered movement and motor-control strategies.4–6
In male youth soccer players, approximately 71% to 80% of injuries affected mainly the lower extremities, predominantly the upper thigh, knee, and ankle.1,7 The highest proportion of injuries to the knee are ligamentous, largely to the medial collateral ligament.1,7,8 Moore et al8 reported a rate of 0.71 knee injuries per player per year, equating to an absence of 17 training days and 2 matches per knee injury. Furthermore, the most frequent site of severe injury (time absent >28 days) was the anterior cruciate ligament (ACL).9 Primary injury mechanisms for these structures have been identified, including a noncontact incident whereby the knee is positioned in valgus during landing and deceleration.10,11 Using appropriate screening protocols to prospectively identify players who demonstrate high-risk movement patterns may help prevent traumatic events via targeted neuromuscular-training techniques.12
Kinematic assessments are considered useful in identifying the noncontact knee-injury risk.12–17 A major focus has often been placed on female athletes13,14,18; however, aberrant landing kinematics have also been seen in male youth soccer players who subsequently sustained an ACL injury versus uninjured control individuals.16 Yet few researchers have analyzed the effects of age and maturation on knee-joint kinematics in this cohort. Boys appear to demonstrate kinematic changes at the knee, with reductions in valgus alignment as they progress through maturation.19–21 Male youth soccer players who participated in the U14 to U16 chronologic age groups also appeared to be at greater risk of knee injury,8 which may have been due to periods of rapid growth. In the context of a soccer academy, players compete and are typically screened in their respective chronologic age groups; however, Schmitz et al20 indicated that knee valgus may be influenced by the stage of maturity. Therefore, quantifying the effects of age and maturation on knee-valgus motion during repeated jumping tasks may help coaches identify players who demonstrate high-risk kinematics and developmental trends associated with age and different stages of maturity.
Cumulatively, despite the high frequency of knee injuries, limited evidence is available to determine the influence of age and maturation on knee-joint kinematics using coach-friendly diagnostics in male youth soccer players. Therefore, the purpose of our study was to examine possible age- and maturity-related differences in dynamic knee valgus using the tuck-jump assessment (TJA) in elite male youth soccer players.
METHODS
Experimental Design
We used a cross-sectional design to assess the effects of chronologic age and stage of maturation on dynamic knee valgus during the TJA. Participants were required to attend their respective club's training sessions on 2 occasions separated by a period of 7 days. We used the first session for familiarization and collected data during the second session. Standardization procedures, including the warm-up, test setup, and participant instructions, were replicated at each test session. We instructed participants to eat their normal diets, refrain from drinking substances other than water 1 hour before testing, and refrain from strenuous exercise for at least 48 hours before testing.
Participants
Four hundred elite male youth soccer players from the academies of 6 professional English soccer clubs volunteered to participate. Descriptive statistics are provided for each chronologic age and maturation group in Tables 1 and 2, respectively. Maturation was calculated using a previously suggested regression analysis.3 All players undertook regular neuromuscular training, including skill, balance, plyometrics, and resistance training, as these modes are a requirement of the clubs to maintain their academy status. No players reported injuries at the time of testing, and all were participating regularly in football training and competitions. We collected physical activity readiness questionnaires before testing. All participants and their parents or guardians provided written informed assent or consent, respectively, and the study was approved by the Cardiff Metropolitan University Ethics Committee.
Table 1.
Participant Characteristics for Each Chronologic Age Group
| Age Group |
No. |
Mean ± SD |
||||
| Age, y |
Body Mass, kg |
Height, cm |
Sitting Height, cm |
Maturity Offset |
||
| U11 | 58 | 11.2 ± 0.6 | 37.8 ± 5.8 | 144.0 ± 6.7 | 75.9 ± 4.8 | −2.6 ± 0.5 |
| U12 | 45 | 12.1 ± 0.6 | 40.3 ± 5.7 | 149.2 ± 5.9 | 79.3 ± 4.7 | −2.0 ± 0.6 |
| U13 | 56 | 12.8 ± 0.6 | 44.7 ± 8.8 | 155.8 ± 9.1 | 83.8 ± 6.8 | −1.2 ± 0.7 |
| U14 | 74 | 14.0 ± 0.5 | 50.2 ± 9.2 | 162.8 ± 9.4 | 84.2 ± 13.0 | −0.1 ± 0.9 |
| U15 | 64 | 15.3 ± 0.6 | 60.9 ± 8.4 | 172.2 ± 7.6 | 91.6 ± 5.3 | 1.0 ± 0.6 |
| U16 | 60 | 16.1 ± 0.6 | 65.3 ± 8.1 | 175.8 ± 7.0 | 92.1 ± 5.7 | 1.8 ± 0.6 |
| U18 | 43 | 17.5 ± 0.8 | 72.0 ± 6.5 | 178.9 ± 5.9 | 93.2 ± 4.2 | 2.9 ± 0.7 |
Table 2.
Participant Characteristics for Each Maturation Group
| Maturation Group |
No. |
Mean ± SD |
||||
| Age, y |
Body Mass, kg |
Height, cm |
Limb Length, cm |
Maturity Offset |
||
| Pre-PHV | 135 | 11.9 ± 1.1 | 39.7 ± 6.4 | 148.2 ± 7.5 | 74.6 ± 3.5 | −2.2 ± 0.6 |
| Circa-PHV | 83 | 14.4 ± 0.9 | 51.8 ± 6.7 | 164.8 ± 7.6 | 82.3 ± 3.6 | 0.0 ± 0.3 |
| Post-PHV | 129 | 16.1 ± 1.1 | 66.8 ± 8.0 | 176.6 ± 6.7 | 88.6 ± 4.7 | 2.0 ± 0.8 |
Abbreviation: PHV, peak height velocity.
Procedures
Anthropometry
Body mass in kilograms was measured on a calibrated physician scale (model 786 Culta; Seca, Milan, Italy). Standing and sitting height in centimeters was recorded on a measurement platform (model 274; Seca).
Biological Maturity
Stage of maturation was calculated in a noninvasive manner using a regression equation comprising measures of age, body mass, standing height, and sitting height taken during the data-collection period.3 Using this method, maturity offset (calculation of years from PHV) was completed (Equation 1). The equation has been used to predict maturation status with a standard error of approximately 6 months in pediatric participants.3
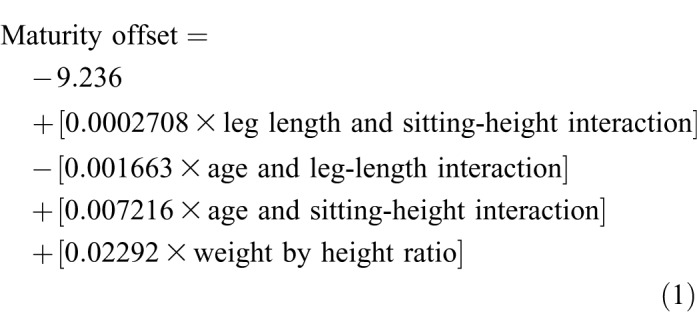 |
Tuck-Jump Assessment
Tuck jumps were performed in place for 10 consecutive repetitions, and each participant's technique was visually graded for the presence of knee valgus based on previous recommendations.17 A 2-dimensional video camera (model H200HD; Samsung, Ridgefield Park, NJ) was positioned in the frontal plane at a height of 0.70 m and a distance of 5 m from the landing area to capture the test. Knee valgus was estimated by measuring the angle created by lines drawn between the hip-, knee-, and ankle-joint centers.19 Frontal-plane projection angles at the point of maximum knee flexion were subjectively classified as minor (<10°), moderate (10°–20°), or severe (>20°). The classifications were determined using pilot data and agreement among expert raters (n = 5), including experienced strength and conditioning coaches and rehabilitation specialists (all authors). Researchers22 have also shown that frontal-plane projection valgus angles ranging from 1° to 9° are to be expected for physically active adults during drop-jump tasks in uninjured participants. Using these classifications, knee valgus in the tuck jump was scored as follows: 0 (no valgus), 1 (minor), 2 (moderate), or 3 (severe). Recorded deficits were marked if the respective knee-valgus score was present on 2 or more repetitions,23 and the maximum score was used for the analysis. Scores were marked retrospectively by the same rater (P.J.R.), a certified strength and conditioning specialist who was part of the research team.
Statistical Analysis
Descriptive statistics were calculated for each subgroup. We performed a Kruskal-Wallis test to determine whether tuck-jump knee-valgus scores differed between groups. Separate analyses were performed to compare a range of chronologic age groups that represented those in an elite soccer academy (U11–U18). A secondary analysis was also employed, grouping players by their stages of maturation (pre-PHV, circa-PHV, or post-PHV). To account for the reported error (approximately 6 months) in the equation,3 players were grouped into discrete bands based on their maturational offset (pre-PHV [<−1], circa-PHV [−0.5 to 0.5], post-PHV [>1]). Players who recorded a maturational offset from −1 to −0.5 or 0.5 to 1 were subsequently removed from the dataset when players were analyzed by stage of maturation. We conducted post hoc analyses using Mann-Whitney U tests to determine between-groups differences. Further analysis included a Wilcoxon signed rank test to assess differences in performance between limbs for the whole sample and for each subgroup. The frequencies of knee-valgus scores were also calculated for each limb for each chronologic age and maturation group. All data were computed through Excel (version 2010; Microsoft Corp, Redmond, WA). Kruskal-Wallis and Wilcoxon signed rank tests were processed using SPSS (version 21; IBM Corp, Armonk, NY). We set the α level at ≤.05. Intrarater reliability for knee-valgus scores in the repeated TJA was assessed using the κ coefficient. To do this, we evaluated the videos of 50 participants on 2 occasions separated by 1 week to determine the accuracy and repeatability of subjectively classified scores.
RESULTS
Median and mode knee-valgus scores for the right and left limbs for all chronologic age and maturation groups are displayed in Table 3. The U18 group had lower knee-valgus scores for the right limb than all other age groups (P < .001) except for the U16 group. For the left limb, knee-valgus scores were higher in the U11 and U12 groups than in all age groups (P < .05) except the U13 group, and lower scores were recorded in the U18 group (P < .001). A trend toward a difference was shown with lower right-limb knee-valgus scores in the U16 than in the U13 (P = .058) and U12 (P = .08) groups. When analyzed by maturation, right-limb scores were highest in the pre-PHV group; however, these differences were only significant when comparing the pre-PHV and post-PHV groups (P < .001). For the left limb, the post-PHV group had a lower score than both the circa-PHV and pre-PHV groups (P < .001).
Table 3.
Knee-Valgus Median (Interquartile Range) and Mode Scores and Mean Rank for Each Group
| Group |
Valgus Right Limb |
Valgus Left Limb |
||||
| Median |
Mode |
Mean Rank |
Median |
Mode |
Mean Rank |
|
| U11 | 2 (1–2) | 2 | 212.98 | 2 (1–2) | 2 | 239.59 |
| U12 | 2 (1–2) | 2 | 218.77 | 2 (1–2) | 2 | 241.70 |
| U13 | 2 (1–2) | 2 | 220.87 | 2 (1–2) | 2 | 220.80 |
| U14 | 2 (1–2) | 2 | 207.06 | 1 (1–2) | 1 | 194.50 |
| U15 | 2 (1–2) | 2 | 189.34 | 1 (0–1) | 1 | 170.56 |
| U16 | 1 (1–2) | 1 | 182.15 | 1 (1–2) | 1 | 184.99 |
| U18 | 1 (0–1) | 1 | 126.11 | 0 (0–1) | 0 | 109.73 |
| Pre-PHV | 2 (1–2) | 2 | 178.43 | 2 (1–2) | 2 | 193.87 |
| Circa-PHV | 2 (1–2) | 2 | 159.71 | 1 (1–2) | 1 | 171.42 |
| Post-PHV | 1 (1–2) | 1 | 138.38 | 1 (0–1) | 0 | 117.40 |
Abbreviation: PHV, peak height velocity.
With all players combined, between-limbs comparisons revealed that knee-valgus scores were higher for the right limb (P < .001). The same pattern was observed in the U14 to U18 groups and for the circa-PHV and post-PHV groups, with no between-limbs differences in the U11 (P = .75), U13 (P = .21), and pre-PHV (P = .88) groups. As shown in Table 3, interlimb asymmetry median and mode scores were evident in the U14, U15 (2 : 1 right versus left), and U18 (1 : 0 right versus left) groups. The same pattern of interlimb differences was observed when analyzed by maturation (Table 3).
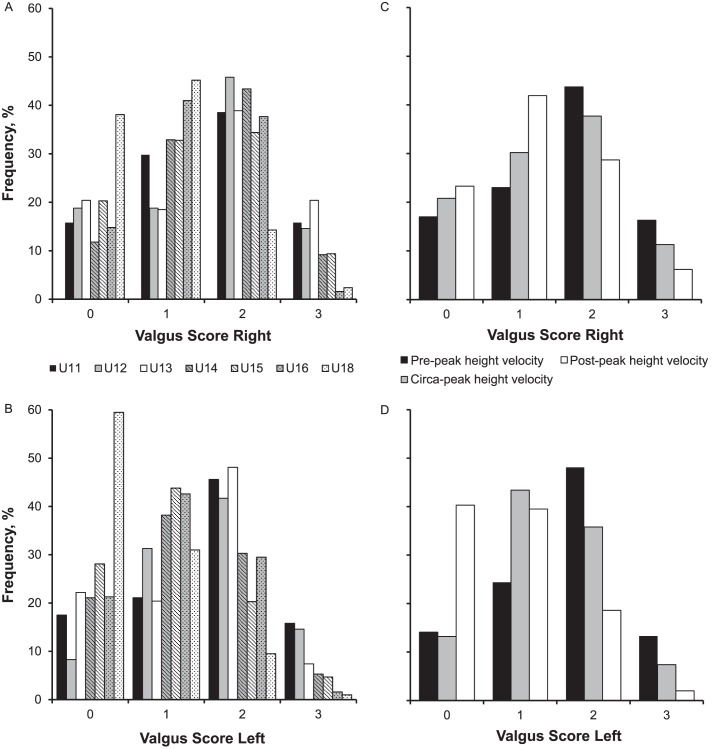
The distribution of knee-valgus scores for each chronologic age and maturation group is displayed in the Figure. The greatest frequencies of no-valgus scores were recorded in the U18 and post-PHV groups. The frequencies of moderate and severe scores were greater in the younger chronologic age groups and in players who were pre-PHV and circa-PHV. The combined percentage of moderate and severe scores was also lower in the older chronologic age groups for both limbs. This pattern was consistent when the data were analyzed by maturation stage, with the circa-PHV and post-PHV groups displaying reductions in combined moderate and severe knee-valgus scores compared with the pre-PHV group. We observed the highest percentages of severe scores in the U13 and pre-PHV groups for the right limb. Intrarater reliability for knee-valgus scores was deemed strong (κ = 0.89).
Figure.
A–D, Frequency (%) of knee-valgus scores for each group.
DISCUSSION
We assessed the effects of chronologic age and stage of maturation on the presence of knee valgus in elite male youth soccer players during the TJA. Results showed reductions in knee-valgus mode scores and lower frequencies of moderate and severe valgus scores with advancing age and stage of maturation. The highest percentages of severe scores were in the U13 and pre-PHV groups for the right limb. Knee-valgus scores were also greater for the right limb when all the players were combined, with subgroup analysis showing noteworthy interlimb asymmetry in the U14 to U15 chronologic age groups and the circa-PHV group.
All chronologic age groups except the U18 group recorded knee-valgus mode scores greater than 1 during the TJA as measured via frontal-plane projection angles, indicating that this risk factor was present to some degree in most of the elite male youth soccer players. Greater valgus motion on landing is a high-risk mechanism for ACL and medial collateral ligament injury,18,24,25 and the latter has been reported as the most frequently occurring knee injury in this cohort.1,8 Untrained youths who did not regularly undertake strength- and plyometric-training activities were more likely to demonstrate knee-valgus malalignment.19 Our results reinforce the need for age-appropriate neuromuscular training to target strength and motor-control deficits to reduce the athletes' relative risk of injury.23,26
We observed a trend toward reduced knee-valgus scores with advancing age and stage of maturation. These findings are consistent with those of researchers21 who examined male recreational youth soccer players. Investigators27 have observed reduced ground reaction forces relative to body weight with maturation during a drop-jump maneuver. These data indicate that, with advancing age and maturation, athletes are better able to attenuate landing forces by using more effective movement strategies to dissipate force.28 Reductions in valgus could be due to the benefits of maturation in terms of increased strength and motor control,29 or chronologic age may be a surrogate of training age, whereby older players have adapted positively from a greater training history.
When the data from all players were pooled, knee-valgus scores were greater for the right limb. The same pattern was observed for all chronologic age and maturation groups, notwithstanding the U11 to U13 and pre-PHV groups. Movement variability during jumping tasks is more evident in younger athletes,30 which may explain the discrepancy in our study between players who were prepubertal and players who were older and at a later stage of maturation. Greater knee-valgus scores for the right limb may indicate that limb dominance is evident in elite male youth soccer players: this appears to emerge at the onset of the U14 chronologic age group (as indicated by asymmetric median and mode scores) and continue through PHV and into early adolescence. Interlimb asymmetry in foundational movement tasks has been reported5 to increase during this period due to physiological adaptations of the dominant limb in youth soccer players.31 Therefore, increases in limb dominance may be an age- and maturity-related injury risk factor. A plausible explanation is that most participants in this study preferred to use their right foot for kicking actions; with greater exposure to soccer-specific practice and competitions, players may become more accustomed to and competent at landing and stabilizing on their left limbs. Whereas no data are available to confirm this in youth athletes, the distribution of noncontact ACL injuries has shown that 74.1% of adult male elite soccer players injured their dominant (kicking) limbs.32 Further research is required to analyze prospective relationships between limb dominance and injury risk in elite male youth soccer players.
Interlimb asymmetric median and mode scores were evident in the U14, U15, and U18 groups and the circa-PHV and post-PHV groups. The asymmetry scores for the U14 and U15 groups and the circa-PHV group may reflect an increased injury risk (2 : 1 right versus left comparison). The highest frequency of severe knee-valgus scores was also recorded in the U13 group. Recent data4,33 showed that elite male youth soccer players were particularly susceptible to injury from the ages of 13.5 to 14.5 years. This could be attributed to potential alterations in motor control that may emerge during periods of rapid growth.6 Subsequently, heightened risk and the potential for a greater incidence of overuse or traumatic knee injury may also be present for players in these groups.4,33 However, further investigation is needed to examine if greater valgus scores and asymmetry between limbs increase the risk of injury in this cohort.
CONCLUSIONS AND PRACTICAL APPLICATIONS
To our knowledge, we are the first to provide cross-sectional data from elite male youth soccer players using the TJA to examine the effects of chronologic age and stage of maturation on knee-joint kinematics during a dynamic jump-landing task. We observed reductions in knee-valgus mode scores with advancing chronologic age and during later stages of maturation, which could be linked to enhanced relative strength and motor control. Greater knee-valgus scores for the right limb in the sample and in certain age and maturation groups suggested the potential emergence of limb dominance in elite male youth soccer players. Furthermore, noteworthy interlimb knee-valgus asymmetries were present in the U14 to U15 chronologic age groups and in the circa-PHV group, indicating that these groups should be targets for injury-risk–reduction strategies. This aberrant movement pattern, which appears to emerge during periods associated with rapid growth in stature, may increase the risk of traumatic injury due to asymmetric loading of passive knee structures.
Quantifying the effects of chronologic age and stage of maturation on knee-valgus motion during the TJA will help coaches identify players who demonstrate high-risk kinematics in an easy and affordable way. Aberrant landing mechanics appear to be more pronounced during periods of rapid growth and subsequent gains in body mass, specifically in the U13 to U15 and circa-PHV groups. These groups should be considered important targets for injury-prevention strategies, with practitioners addressing any neuromuscular deficits through developmentally appropriate and technique-driven exercise prescriptions. Specifically, practitioners are advised to adopt an integrative neuromuscular-training approach to program design15,34,35 that develops fundamental movement skills and muscular strength through resistance training, balance activities, and plyometrics. Researchers35,36 have shown that this form of training should be initiated during preadolescence and maintained through adolescence to enhance skill-related fitness and reduce the risk of sport-related injury.
ACKNOWLEDGMENT
Gregory D. Myer, PhD, acknowledges funding support from the National Institutes of Health/NIAMS Grant No. U01AR067997.
REFERENCES
- 1. Price RJ., Hawkins RD., Hulse MA., Hodson A. The Football Association and medical research programme: an audit of injuries in academy youth football. . 2004; 38 4: 466– 471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schmikli SL., de Vries WR., Inklaar H., Backx FJ. Injury prevention target groups in soccer: injury characteristics and incidence rates in male junior and senior soccer players. . 2011; 14 3: 199– 203. [DOI] [PubMed] [Google Scholar]
- 3. Mirwald RL., Baxter-Jones AD., Bailey DA., Beunen GP. An assessment of maturity from anthropometric measurements. . 2002; 34 4: 689– 694. [DOI] [PubMed] [Google Scholar]
- 4. van der Sluis A., Elferink-Gemser MT., Coelho-e-Sliva MJ., Nijboer JA., Brink MS., Visscher C. Sports injuries aligned to peak height velocity in talented pubertal soccer players. . 2014; 35 4: 351– 355. [DOI] [PubMed] [Google Scholar]
- 5. Atkins SJ., Bentley I., Hurst HT., Sinclair JK., Hesketh C. The presence of bilateral imbalance of the lower limbs in elite youth soccer players of different ages. . 2016; 30 4: 1007– 1013. [DOI] [PubMed] [Google Scholar]
- 6. Philippaerts RM., Vaeyens R., Janssens M., et al. The relationship between peak height velocity and physical performance in youth soccer players. . 2006; 24 3: 221– 230. [DOI] [PubMed] [Google Scholar]
- 7. Le Gall F., Carling C., Reilly T., Vandewalle H., Church J., Rochcongar P. Incidence of injuries in elite French youth soccer players: a 10-season study. . 2006; 34 6: 928– 938. [DOI] [PubMed] [Google Scholar]
- 8. Moore O., Cloke DJ., Avery PJ., Beasley I., Deehan DJ. English Premiership Academy knee injuries: lessons from a 5 year study. . 2011; 29 14: 1535– 1544. [DOI] [PubMed] [Google Scholar]
- 9. Volpi P., Pozzoni R., Galli M. The major traumas in youth football. . 2003; 11 6: 399– 402. [DOI] [PubMed] [Google Scholar]
- 10. Waldén M., Krosshaug T., Bjørneboe J., Andersen TE., Faul O., Hägglund M. Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: a systematic video analysis of 39 cases. . 2015; 49 22: 1452– 1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wijdicks CA., Griffith CJ., LaPrade RF., et al. Medial knee injury: part 2, load sharing between the posterior oblique ligament and superficial medial collateral ligament. . 2009; 37 9: 1771– 1776. [DOI] [PubMed] [Google Scholar]
- 12. Read PJ., Oliver JL., De Ste Croix MB., Myer GD., Lloyd RS. Neuromuscular risk factors for knee and ankle ligament injuries in male youth soccer players. . 2016; 46 8: 1059– 1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Myer GD., Paterno MV., Ford KR., Quatman CE., Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. . 2006; 36 6: 385– 402. [DOI] [PubMed] [Google Scholar]
- 14. Myer GD., Ford KR., Khoury J., Succop P., Hewett TE. Development and validation of a clinic-based prediction tool to identify female athletes at high risk of anterior cruciate ligament injury. . 2010; 38 10: 2025– 2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Myer GD., Brent JL., Ford KR., Hewett TE. Real-time assessment and neuromuscular training feedback techniques to prevent ACL injury in female athletes. . 2011; 33 3: 21– 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Padua DA., DiStefano LJ., Beutler AI., de la Motte SJ., DiStefano MJ., Marshall SW. The Landing Error Scoring System as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. . 2015; 50 6: 589– 595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Read PJ., Oliver JL., de Ste Croix MB., Myer GD., Lloyd RS. Reliability of the tuck jump injury risk screening assessment in elite male youth soccer players. . 2016; 30 6: 1510– 1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hewett TE., Myer GD., Ford KR., et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. . 2005; 33 4: 492– 501. [DOI] [PubMed] [Google Scholar]
- 19. Noyes FR., Barber-Westin SD., Fleckenstein C., Walsh C., West J. The drop-jump screening test: difference in lower limb control by gender and effect of neuromuscular training in female athletes. . 2005; 33 2: 197– 207. [DOI] [PubMed] [Google Scholar]
- 20. Schmitz RJ., Schultz SJ., Nguyen AD. Dynamic valgus alignment and functional strength in males and females during maturation. . 2009; 44 1: 26– 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yu B., McClure SB., Onate JA., Guskiewicz KM., Kirkendall DT., Garrett WE. Age and gender effects on lower extremity kinematics of youth soccer players in a stop-jump task. . 2005; 33 9: 1356– 1364. [DOI] [PubMed] [Google Scholar]
- 22. Herrington L., Munro A. Drop jump landing knee valgus angle: normative data in a physically active population. . 2010; 11 2: 56– 59. [DOI] [PubMed] [Google Scholar]
- 23. Myer GD., Stroube BW., DiCesare CA., et al. Augmented feedback supports skill transfer and reduces high-risk injury landing mechanics: a double-blind, randomized controlled laboratory study. . 2013; 41 3: 669– 677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ford KR., Myer GD., Hewett TE. Valgus knee motion during landing in high school female and male basketball players. . 2003; 35 10: 1745– 1750. [DOI] [PubMed] [Google Scholar]
- 25. Indelicato PA. Isolated medial collateral ligament injuries in the knee. . 1995; 3 1: 9– 14. [DOI] [PubMed] [Google Scholar]
- 26. Stroube BW., Myer GD., Brent JL., Ford KR., Heidt RS, Jr,, Hewett TE. Effects of task-specific augmented feedback on deficit modification during performance of the tuck-jump exercise. . 2013; 22 1: 7– 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Quatman CE., Ford KR., Myer GD., Hewett TE. Maturation leads to gender differences in landing force and vertical jump performance: a longitudinal study. . 2006; 34 5: 806– 813. [DOI] [PubMed] [Google Scholar]
- 28. Swartz EE., Decoster LC., Russell PJ., Croce RV. Effects of developmental stage and sex on lower extremity kinematics and vertical ground reaction forces during landing. . 2005; 40 1: 9– 14. [PMC free article] [PubMed] [Google Scholar]
- 29. Jones MA., Hitchen PJ., Stratton G. The importance of considering biological maturity when assessing physical fitness measures in girls and boys aged 10 to 16 years. . 2000; 27 1: 57– 65. [DOI] [PubMed] [Google Scholar]
- 30. Gerodimos V., Zafeiridis A., Perkos S., Dipla K., Manou V., Kellis S. The contribution of stretch-shortening cycle and arm-swing to vertical jumping performance in children, adolescents, and adult basketball players. . 2008; 20 4: 379– 389. [DOI] [PubMed] [Google Scholar]
- 31. Daneshjoo A., Rahnama N., Mokhtar AH., Yusof A. Bilateral and unilateral asymmetries of isokinetic strength and flexibility in male young professional soccer players. . 2013; 36: 45– 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Brophy R., Silvers HJ., Gonzales T., Mandelbaum BR. Gender influences: the role of leg dominance in ACL injury among soccer players. . 2010; 44 10: 694– 697. [DOI] [PubMed] [Google Scholar]
- 33. van der Sluis A., Elferink-Gemser MT., Brink MS., Visscher C. Importance of peak height velocity timing in terms of injuries in talented soccer players. . 2015; 36 4: 327– 332. [DOI] [PubMed] [Google Scholar]
- 34. Myer GD., Ford KR., Palumbo JP., Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. . 2005; 19 1: 51– 60. [DOI] [PubMed] [Google Scholar]
- 35. Myer GD., Faigenbaum AD., Ford KR., Best TM., Bergeron MF., Hewett TE. When to initiate integrative neuromuscular training to reduce sports-related injuries and enhance health in youth? . 2011; 10 3: 155– 166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Faigenbaum AD., Farrell A., Fabiano M., et al. Effects of integrative neuromuscular training on fitness performance in children. . 2011; 23 4: 573– 584. [DOI] [PubMed] [Google Scholar]