Abstract
Introduction:
Identifying trajectories of tobacco use is critical for understanding its natural history and targeting interventions, but research on trajectories of smokeless tobacco and dual use of smokeless tobacco and cigarettes is very limited. This study identified tobacco use trajectories from adolescence to midlife and tested correlates of trajectory group membership.
Methods:
This study included all male participants in a longitudinal study who reported cigarette smoking or smokeless tobacco use in 1987, 1993, 1999, 2005, or 2011 (N = 2230). Group-based trajectory analyses were conducted with zero-inflated Poisson models. Analysis of covariance was used to test adolescent health beliefs associated with trajectory group membership.
Results:
Five smoking trajectory groups were identified: (1) consistent abstinence from cigarettes; (2) late onset intermittent, then cessation; (3) early onset regular, then cessation; (4) delayed onset regular, then cessation; and (5) consistent regular. Four smokeless tobacco trajectory groups were identified: (1) early onset, then cessation; (2) consistent abstinence from smokeless tobacco; (3) late onset, escalating; and (4) consistent regular. The proportion of participants in trajectory groups representing dual use was low. Adolescent beliefs favorable to smoking and smokeless tobacco were associated with membership in consistent regular use groups.
Conclusions:
The prevalence of dual use of cigarettes and smokeless tobacco was low, and there was little evidence to suggest switching between tobacco products. Participants who held more positive beliefs about smoking and smokeless tobacco as adolescents were more likely to be consistent regular users of cigarettes and smokeless tobacco into adulthood.
Introduction
The identification of multiple developmental trajectories of tobacco use is critical for understanding its natural history and pinpointing targets for intervention.1 Although several studies have identified multiple cigarette smoking trajectories from adolescence to adulthood,1–5 there has been little work done on identifying similar trajectories of smokeless tobacco use. In fact, the only published work to date on trajectories of smokeless tobacco use did not extend beyond adolescence.6 In their study of Swedish adolescents, Rosendahl et al.6 found early and steep escalation of snus use only among males but early and steep escalation of cigarette smoking only among females. Among both sexes, exposure to tobacco in the social environment was associated with membership in the early escalating trajectory groups for cigarette smoking. However, only parents’ tobacco use behavior was a significant predictor of membership in the early escalating trajectory group for snus use. The three identified trajectory groups of dual use of cigarettes and smokeless tobacco were early escalation, late escalation, and sustained trial, but predictors of membership in these groups were not reported. Dual users are particularly important because they have been shown to differ from smokers and smokeless tobacco users.7 For instance, they may escalate more quickly to heavy tobacco use and nicotine dependence than do users of a single tobacco product.6
Although there is a lack of research on empirically identified trajectories of smokeless tobacco use and dual use of smokeless tobacco and cigarettes, there has been a lively debate in the literature between researchers who report that smokeless tobacco use increases the risk of future cigarette smoking8–10 and those who claim that no such link exists.11–13 The lack of consensus has been attributed to differences in definitions of nonsmoking at baseline (eg, never smoker vs. current nonsmoker) and exclusion of established predictors of tobacco use that point to a common vulnerability to both forms of tobacco use. Differences in findings may also be due to methodological limitations of these studies. For instance, some of the studies are retrospective,11,13 and prospective longitudinal studies are better-suited to answering this question. However, even the prospective studies that have been done are limited to two time points with only 1 year,8 2 years,9 and 4 years10,12 between baseline and follow-up. Therefore, the studies are limited in the developmental range that they cover, which makes it difficult to distinguish developmentally limited experimentation with tobacco, which generally occurs in adolescence and young adulthood, from long-term regular use that extends into adulthood. Also, these studies are unable to describe long-term patterns, which are important from a health perspective.
Aside from Rosendahl et al.,6 no study has utilized longitudinal data to identify correlates of cigarette smoking, smokeless tobacco use, and dual use trajectory group membership. Prior cross-sectional studies have reported characteristics of dual users compared to users of a single tobacco product. For example, dual users were younger,14,15 had lower levels of education,15 had less income,14 and had less intention to quit14 compared to other tobacco users. In terms of health beliefs, dual users did not perceive smokeless tobacco as less harmful than cigarettes.14
The current study is the first to identify trajectories of smokeless tobacco use and cigarette smoking that start in adolescence and extend into midlife. Utilizing a sample that spans 35 years allows us to differentiate predictors of use limited to adolescence from predictors of long-term regular use and also distinguish potentially important heterogeneity in age of onset and cessation. A key question in this study is the extent to which tobacco users in this sample engage in dual use of cigarettes and smokeless tobacco. It is important to explicitly model the dual use of smokeless tobacco and cigarettes, because univariate approaches (smokeless tobacco only or cigarettes only) may hide relations that can only be seen with dual use models. In terms of these dual use trajectories, there are alternative possible outcomes, which have different implications for tobacco prevention and cessation programs. One possibility is a common vulnerability to tobacco use, such that the use of both cigarettes and smokeless tobacco remains positively linked over time. If trajectories of smokeless tobacco use and cigarette smoking are positively related, then prevention and cessation messages that target tobacco use in general should be most useful (rather than smokeless tobacco or cigarette-specific messages). For example, messages about the dangers of nicotine addiction, regardless of the source, may be best for such a trajectory group. A second possibility is a common vulnerability to tobacco use in adolescence or young adulthood that produces broad experimentation with multiple forms of tobacco but then specialization in either smoking or smokeless tobacco use at some point later in life. One study’s findings suggest that individuals who are dual users at an early age tend to move toward cigarettes later in life.16 If this pattern is most common, then prevention messages that target all tobacco use are appropriate at younger ages, but messages that focus on cigarettes would be needed at older ages. Third, individuals may initiate with one type of tobacco product and then switch altogether to another form of tobacco. A trajectory group characterized by smokeless tobacco use in adolescence and later switching to cigarette smoking provides evidence that smokeless tobacco use is a “gateway” to cigarette smoking and informs the debate discussed previously. On the other hand, a trajectory group characterized by switching from smoking to smokeless tobacco use may suggest that use of smokeless tobacco functions as a perceived safer alternative to smoking. This could include both perceived personal safety as well as perceived safety for family members who would no longer be exposed to environmental tobacco smoke. One prior study found little evidence that male smokers switched to smokeless tobacco or that male smokeless tobacco users switched to smoking cigarettes, but these transitions were tested over a 1-year period.17 In contrast, a study of smokers in Minnesota reported an increase in smokeless tobacco use between 2007 and 2010 suggesting that smokers may be adopting smokeless tobacco.18 In the current study, we tested for switching tobacco products over a 35-year period.
In addition to identifying trajectories of cigarette smoking and smokeless tobacco use, we examined adolescent health beliefs associated with membership in trajectory groups. Specifically, we tested health beliefs, normative beliefs, and perceived prevalence measured at baseline as correlates of membership in trajectories of smoking, smokeless tobacco use, and dual use going forward for up to 35 years.
Methods
Participants
Participants were from the Indiana University Smoking Survey, an ongoing cohort-sequential study of the natural history of cigarette smoking and other tobacco use.2 A total of 8487 participants were enrolled in the study. Follow-up surveys were conducted in 1987, 1993, 1999, 2005, and 2011. At each wave, 70% or more of the original sample has been retained. In 1987, survey data were collected with group-administered questionnaires in school for cohorts who were still in high school. For older cohorts and for all participants in 1993, 1999, 2005, and 2011, a survey was sent by mail followed by telephone interviews, and an online survey in 2011, if surveys were not returned. Participants were paid $15 to $35 over the waves, and in 1999, 2005, and 2011 they were also entered into lottery drawings for cash prizes up to $500. The research protocol was approved by the Institutional Review Board at Indiana University, and informed consent was obtained for participation in the research.
For the current study, we selected all male participants who reported any cigarette smoking or smokeless tobacco use in 1987, 1993, 1999, 2005, or 2011. Only males were selected because of the low prevalence of smokeless tobacco use among females. A total of 4399 males completed questionnaires in 1987, 1993, 2005, and 2011. We sequentially excluded participants with missing values on age across all five survey waves (n = 525), those with missing data on cigarette smoking and smokeless tobacco use at all five waves (n = 2), and those who reported not smoking and not using smokeless tobacco at all five waves (n = 1642). We excluded study participants who abstained from all tobacco products across all five waves of measurement because the objective of this study was to identify patterns of use rather than differences between users and nonusers. This resulted in a total sample size of 2230 for the trajectory analyses. In terms of the demographic characteristics of the sample, 93% were white, and 1% was Hispanic. In 2011, 34% reported educational attainment of a bachelor’s degree or higher, 63% were married, 74% had at least one child, and 80% worked full-time. This sample is representative of the community from which it was drawn, one that is predominately non-Hispanic white and well-educated. For the tests of health beliefs associated with trajectory group membership, the sample size was 1650 due to missing data on health belief variables, all of which were measured in 1987.
Measures
Cigarette Smoking
At each wave, participants reported their smoking status and the number of cigarettes usually smoked in a day. These two items were used to create a seven-level smoking variable at each wave: noncurrent smoker; current smoker, but no more than one a month; current smoker, but no more than one a week; current smoker, but no more than one a day; current smoker, up to nine cigarettes per day; current smoker, 10–20 cigarettes per day; and current smoker, more than 20 cigarettes per day.
Smokeless Tobacco Use
At each wave, participants self-reported their smokeless tobacco use. Because there was little variability in the distribution of use in this sample, a three-level variable was created: noncurrent smokeless tobacco user; current smokeless tobacco user, less than daily; and current smokeless tobacco user, daily.
Parent Education
In 1987, participants reported the highest level of education completed by their mother and father. For analyses, we created a binary parent education variable (at least one parent with college education or higher vs. no parent with college education).
Personally Relevant Health Beliefs
All health belief variables were measured in 1987. For beliefs about smoking, participants responded to two items (“If I smoke cigarettes, I will get lung cancer.” and “If I smoke cigarettes, I will get heart disease.”) measured on a five-point scale from strongly agree to strongly disagree. Responses to the two items were averaged, and a higher score reflected pro-smoking beliefs (mean = 2.43, SD = 0.81, range: 1–5, Cronbach’s α = 0.90). For beliefs about smokeless tobacco, participants responded to two items (“If I chew or dip tobacco, I will get mouth cancer.” and “If I chew or dip tobacco, I will get heart disease.”) measured on a five-point scale from strongly agree to strongly disagree. Responses to the two items were averaged, and a higher score reflected pro-smokeless tobacco beliefs (mean = 2.86, SD = 0.67, range: 1–5, Cronbach’s α = 0.51).
Personalized Risk of Addiction
Participants reported risk of addiction by responding to one item about smoking (“If I smoke cigarettes, I will be hooked.”) and one item about smokeless tobacco (“If I chew or dip tobacco, I will get hooked.”), both measured on a five-point scale from strongly agree to strongly disagree. A higher score reflected a lower level of perceived risk (mean = 2.74, SD = 1.17, range: 1–5 for smoking; mean = 2.73, SD = 1.00, range: 1–5 for smokeless tobacco).
General Health Beliefs
For beliefs about smoking, participants responded to five items (eg, “Smoking cigarettes is OK as long as you don’t smoke too many.”) measured on a five-point scale from strongly agree to strongly disagree. Responses to the five items were averaged, and a higher score reflected pro-smoking beliefs (mean = 2.21, SD = 0.69, range: 1–5, Cronbach’s α = 0.81). For beliefs about smokeless tobacco, participants responded to five items (eg, “Chewing or dipping tobacco is OK as long as you don’t chew or dip too much.”) measured on a five-point scale from strongly agree to strongly disagree. Responses to the five items were averaged, and a higher score reflected pro-smokeless tobacco beliefs (mean = 2.30, SD = 0.77, range: 1–5, Cronbach’s α = 0.89).
Normative Beliefs
Participants responded to four items (eg, “My friends think that I should not smoke cigarettes.”) measured on a five-point scale from strongly agree to strongly disagree to assess normative beliefs about smoking and four items (eg, “My friends think that I should not chew or dip tobacco.”) measured on a five-point scale from strongly agree to strongly disagree to assess normative beliefs about smokeless tobacco. In both cases, a higher score reflected more positive beliefs (mean = 2.09, SD = 0.78, range: 1–5, Cronbach’s α = 0.83 for smoking; mean = 2.17, SD = 0.84, range: 1–5, Cronbach’s α = 0.86 for smokeless tobacco).
Perceived Prevalence
We measured perceived prevalence of cigarette smoking by asking participants how many boys and how many men out of 100 did they think smoked cigarettes in their city. We averaged the responses to the two questions to create a perceived prevalence of smoking score (mean = 47.69, SD = 19.65, range: 5–93). The same method was followed for perceived prevalence of smokeless tobacco use (mean = 36.38, SD = 21.23, range: 5–93).
Health Dangers of Smoking Versus Smokeless Tobacco
Participants responded to a single item, “Compare the health dangers of smoking cigarettes and chewing/dipping tobacco.” Response options were “smoking is much more dangerous” (scored as −2), “smoking is somewhat more dangerous” (scored as −1), “smoking and chewing/dipping are equally dangerous (scored as 0), “chewing/dipping is somewhat more dangerous” (scored as 1), and “chewing/dipping is much more dangerous” (scored as 2). The mean value for this item was −0.82 (SD = 0.91, range: −2 to 2).
Data Analyses
Group-based trajectory analyses were conducted on cigarette smoking and smokeless tobacco separately and then jointly over age by using zero-inflated Poisson models.19 Although the nature of the data supported the use of zero-inflated Poisson models, we also conducted analyses with CNORM models. These findings were similar to those from the zero-inflated Poisson models, suggesting the patterns identified are robust to the selected models. For the dual trajectory analysis, we did two additional sensitivity analyses using a seven-level cigarette smoking variable and a two-level smokeless tobacco use variable: (1) zero-inflated Poisson model for smoking and logistic regression model for smokeless and (2) CNORM for smoking and logistic regression model for smokeless. Again, both sensitivity analyses showed similar dual trajectory patterns as reported in this manuscript.
The optimum number of groups was chosen based on the combined information of scree plots based on the Bayesian information criterion and Akaike information criterion, Jeffrey’s scale of the evidence method using Bayes Factor, and model interpretability. The group probabilities were determined for each individual based on the estimated parameters of a trajectory model given a specified number of groups. Each individual was assigned to the group with the maximal group membership probability among all group membership probabilities. These models were fitted using the “TRAJ” command in Stata Version 13 (StataCorp, College Station, TX). Two-sided P ≤ .05 was considered statistically significant.
Correlates of trajectory group membership were tested with a series of five (smoking trajectory group) by four (smokeless tobacco trajectory group) analysis of covariances with age in 1987 and parent education included as covariates. Pairwise comparisons were only assessed when the omnibus F-test was statistically significant. A Bonferroni correction was used for pairwise comparisons among groups to address the issue of multiple comparisons.20 Membership in a dual use group was determined by the interaction of smoking trajectory group by smokeless tobacco trajectory group in each two-way analysis of covariance. These analyses were done with SPSS Version 22 (IBM Corp., Armonk, NY).
Results
Study Participant Characteristics
Sample characteristics overall and by cigarette smoking and smokeless tobacco trajectory group are shown in Table 1. Those in the early onset, then cessation smokeless tobacco trajectory group were significantly younger in 1987 than those in the other smokeless tobacco trajectory groups. In terms of parent education, those in the regular use trajectory groups for both cigarette smoking and smokeless tobacco were the least likely to have at least one parent with a college education.
Table 1.
Sample Characteristics in 1987 Overall and by Smoking and Smokeless Tobacco Trajectory Group
| Characteristic in 1987 | Overall, n = 2230, % or mean (SD) | Smoking trajectory groups, % or mean (SD) | Smokeless trajectory groups, % or mean (SD) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) consistent abstainer from cigarettes, n = 649 | (2) late onset, cessation, n = 214 | (3) early onset, cessation, n = 235 | (4) delayed onset regular, cessation, n = 270 | (5) regular, n = 862 | P (ANOVA or chi-square) | (1) early onset, cessation, n = 367 | (2) consistent abstainer from smokeless tobacco, n = 1070 | (3) late onset, n = 139 | (4) regular n = 654 | P (ANOVA or chi-square) | ||
| Age | 20.1 (2.7) | 20.2 (2.7) | 20.5 (2.9) | 19.7 (2.8) | 20.1 (2.8) | 20.1 (2.7) | .096 | 19.5 (2.8) | 20.3 (2.7) | 20.3 (2.8) | 20.1 (2.7) | <.001 |
| At least one parent with college education or higher | 40.5 | 38.2 | 43.6 | 53.1 | 48.5 | 34.4 | <.001 | 40.6 | 47.2 | 32.4 | 32.3 | <.001 |
ANOVA = analysis of variance.
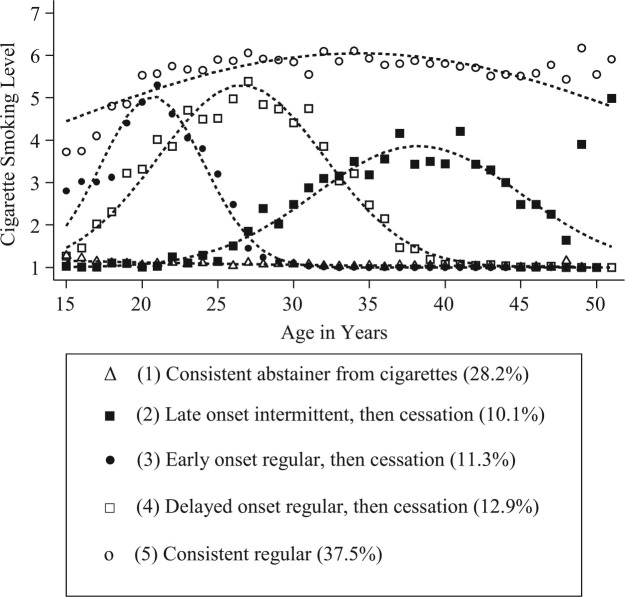
Smoking Trajectories
Figure 1 displays the cigarette smoking trajectory groups. Based on the criteria mentioned above, five groups were identified: (1) consistent abstinence from cigarettes (28.2%); (2) late onset intermittent, then cessation (10.1%); (3) early onset regular, then cessation (11.3%); (4) delayed onset regular, then cessation (12.9%); and (5) consistent regular (37.5%).
Figure 1.
Trajectories of cigarette smoking. Note: The points represent calculated average cigarette smoking scores for participants at a fixed age within one trajectory group. The large deviation of the observed points from the fitted values for the late onset intermittent, then cessation group is a result of small sample sizes at ages 49 and above that produce low precision of estimation.
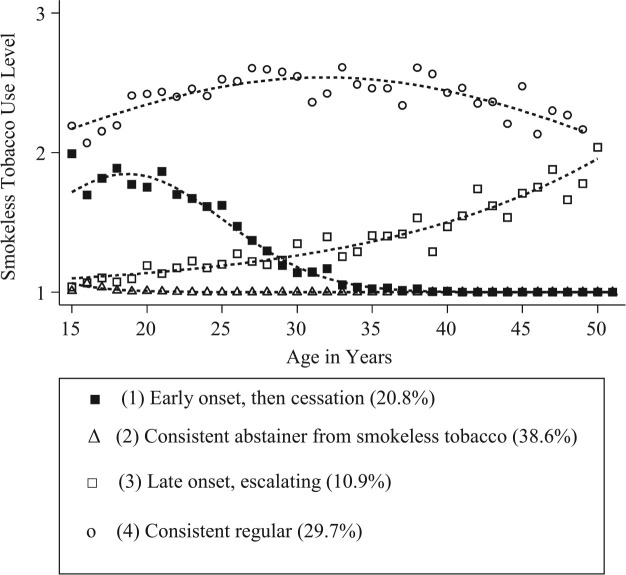
Smokeless Tobacco Trajectories
Smokeless tobacco trajectory groups are in Figure 2. Four groups were optimal: (1) early onset, then cessation (20.8%); (2) consistent abstinence from smokeless tobacco (38.6%); (3) late onset, escalating (10.9%); and (4) consistent regular (29.7%).
Figure 2.
Trajectories of smokeless tobacco use. Note: The points represent calculated average smokeless tobacco use scores for participants at a fixed age within one trajectory group.
Dual Trajectories
Results of the dual trajectory analysis are in Table 2. The cells with the highest proportion of participants were those indicating consistent regular use of one product and abstinence from the other product (26.8% consistent regular smoking and abstinence from smokeless tobacco and 20.6% consistent regular smokeless tobacco use and abstinence from smoking).
Table 2.
Joint Classification Membership Based on a Dual Trajectory Model of Cigarette Smoking and Smokeless Tobacco
| Smokeless tobacco, n (%) | Total | |||||
|---|---|---|---|---|---|---|
| (1) early onset, then cessation | (2) consistent abstainer from smokeless tobacco | (3) late onset, escalating | (4) consistent regular | |||
| Cigarette smoking, n (%) | (1) consistent abstainer from cigarettes | 166 (7.44) | 3 (0.13)a | 20 (0.90) | 460 (20.63) | 649 (29.10) |
| (2) late onset intermittent, then cessation | 13 (0.58) | 129 (5.78) | 24 (1.08) | 48 (2.15) | 214 (9.60) | |
| (3) early onset regular, then cessation | 40 (1.79) | 150 (6.73) | 13 (0.58) | 32 (1.43) | 235 (10.54) | |
| (4) delayed onset regular, then cessation | 4 (0.18) | 191 (8.57) | 18 (0.81) | 57 (2.56) | 270 (12.11) | |
| (5) consistent regular Total | 144 (6.46) | 597 (26.77) | 64 (2.87) | 57 (2.56) | 862 (38.65) | |
| 367 (16.46) | 1070 (47.98) | 139 (6.23) | 654 (29.33) | 2230 (100.00) | ||
The model was constructed using dual trajectory analysis under the assumption of zero-inflated Poisson distributions for both variables.
aThis value of 3 represents error in the model.
In terms of dual use of both cigarettes and smokeless tobacco, 2.6% of the sample belonged to trajectory groups representing consistent regular use of both cigarettes and smokeless tobacco. An additional 2.9% were consistent regular for smoking and late onset, escalating for smokeless; 1.1% were late onset intermittent, then cessation for smoking and late onset, escalating for smokeless; and 2.2% were late onset intermittent, then cessation for smoking and consistent regular for smokeless. Thus, a total of 8.7% were members of trajectory groups that represented any dual use over the 35-year time period. We were also interested in dual trajectories that suggested switching from one product to the other. The two groups that indicated switching from cigarettes to smokeless tobacco were early onset regular, then cessation for smoking and late onset, escalating for smokeless (0.6%) and delayed onset regular, then cessation for smoking and late onset, escalating for smokeless (0.8%) for a total of 1.4%. Finally, the one group that indicated switching from smokeless tobacco to cigarettes was early onset, then cessation for smokeless and late onset intermittent, then cessation for smokeless (0.6%).
Correlates of Trajectory Group Membership
Results from the analysis of covariance models testing the adolescent health beliefs associated with trajectory group membership are shown in Table 3. The table displays the estimated marginal mean level of the health beliefs for each smoking and smokeless trajectory group, the omnibus F-values for the main effects of smoking and smokeless trajectory group and the interaction between smoking and smokeless trajectory groups, and significant pairwise differences. The consistent regular smoking trajectory group had the highest levels for all smoking-related beliefs with the exception of personalized risk of addiction to smoking, and the mean difference compared to the consistent abstainer group was statistically significant for all beliefs except personalized risk of addiction to smoking and perceived prevalence of smoking. Also, the consistent regular smoking group had higher levels on these beliefs than the trajectory groups that included cessation from smoking, although the significant pairwise differences varied among the beliefs (Table 3).
Table 3.
Correlates of Trajectory Group Membership Measured in 1987
| Predictor | Smoking trajectory group meana | Omnibus F-value | Significant pairwise differencesb | Smokeless trajectory group meana | Omnibus F-value | Significant pairwise differencesb | Smoking by smokeless interaction F-value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) consistent abstainer from cigarettes | (2) late onset, cessation | (3) early onset, cessation | (4) delayed onset regular, cessation | (5) regular | (1) early onset, cessation | (2) consistent abstainer from smokeless tobacco | (3) late onset | (4) regular | ||||||
| Personally relevant health beliefs about smoking | 2.04 | 2.17 | 2.51 | 2.46 | 2.64 | 8.51*** | 1,5**; 2,3*; 2,5*** | 2.44 | 2.28 | 2.29 | 2.45 | 1.23 | None | 0.57 |
| Personally relevant health beliefs about smokeless | 2.90 | 2.72 | 3.08 | 2.67 | 2.93 | 4.50** | 2,3**; 3,4* | 2.80 | 2.79 | 2.79 | 3.07 | 5.52** | 3,4** | 1.03 |
| Personalized risk of addiction to smoking | 2.97 | 2.78 | 3.11 | 2.48 | 2.70 | 2.98* | 3,5* | 2.57 | 2.93 | 2.85 | 2.88 | 1.19 | None | 1.90* |
| Personalized risk of addiction to smokeless | 2.56 | 2.53 | 2.83 | 2.35 | 2.85 | 3.63** | 4,5* | 2.42 | 2.74 | 2.66 | 2.68 | 1.16 | None | 1.20 |
| General health beliefs about smoking | 1.80 | 1.94 | 2.38 | 2.16 | 2.41 | 13.29*** | 1,3***; 1,5***; 2,3***; 2,5*** | 2.13 | 2.07 | 2.17 | 2.19 | 0.53 | None | 0.80 |
| General health beliefs about smokeless | 1.87 | 2.16 | 2.44 | 2.20 | 2.50 | 7.56*** | 1,3**; 1,5***; 2,5** | 2.27 | 1.94 | 2.22 | 2.50 | 8.12*** | 2,4***; 3,4* | 0.87 |
| Normative beliefs about smoking | 1.86 | 1.73 | 2.23 | 1.92 | 2.42 | 18.66*** | 1,5**; 2,3***; 2,5***; 4,5** | 1.95 | 2.10 | 1.97 | 2.10 | 1.09 | None | 0.66 |
| Normative beliefs about smokeless | 2.02 | 1.82 | 2.36 | 1.99 | 2.40 | 11.40*** | 2,3***; 2,5***; 4,5* | 2.19 | 1.87 | 2.00 | 2.42 | 9.50*** | 2,4***; 3,4*** | 1.91* |
| Perceived prevalence of smoking | 42.42 | 45.77 | 47.53 | 46.50 | 52.73 | 4.46** | 2,5* | 45.87 | 43.59 | 49.12 | 49.38 | 1.57 | None | 0.53 |
| Perceived prevalence of smokeless | 39.26 | 37.47 | 35.09 | 33.77 | 38.93 | 1.07 | None | 35.17 | 32.69 | 37.74 | 42.01 | 3.95** | 2,4* | 0.68 |
| Health dangers of smoking versus smokeless | −0.73 | −0.89 | −0.87 | −0.99 | −0.77 | 0.82 | None | −1.06 | −0.65 | −0.79 | −0.89 | 2.04 | None | 0.80 |
aEstimated marginal means.
bSignificant pairwise differences after Bonferroni adjustment.
*P < .05; **P < .01; ***P < .001.
Similarly, for smokeless tobacco-related beliefs, the consistent regular use trajectory group had the highest levels for all beliefs except personalized risk of addiction to smokeless tobacco. In terms of pairwise comparisons, with the exception of personally relevant health beliefs about smokeless tobacco, the consistent regular use trajectory group had significantly higher mean values than the consistent abstainer group on all health beliefs related to smokeless tobacco.
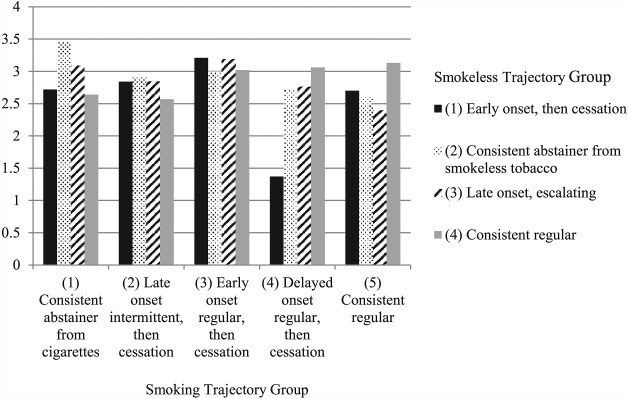
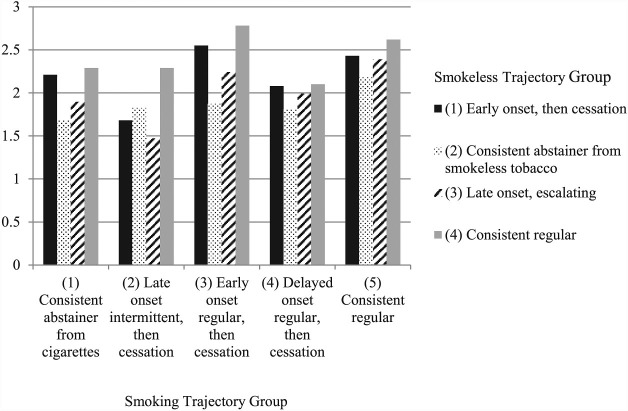
There were two significant interactions between smoking trajectory group and smokeless trajectory group. Figure 3 shows that for personalized risk of addiction to smoking, individuals who were in both the delayed onset regular, then cessation smoking group and the early onset, then cessation smokeless tobacco use group had the lowest mean value, indicating a high level of perceived risk. Figure 4 shows that for normative beliefs about smokeless tobacco, participants in the consistent regular smokeless tobacco use group and the early onset regular, then cessation cigarette smoking group had the highest mean level of normative beliefs.
Figure 3.
Estimated marginal mean level of personalized risk of addiction to smoking jointly stratified by smokeless trajectory group and smoking trajectory group.
Figure 4.
Estimated marginal mean level of normative beliefs about smokeless tobacco jointly stratified by smokeless trajectory group and smoking trajectory group.
Discussion
This study is the first to empirically identify trajectories of cigarette smoking and smokeless tobacco among men from adolescence to mid-life. A better understanding of long-term tobacco use patterns is important for tailoring interventions to reduce tobacco use. The first finding of note was that dual use of cigarettes and smokeless tobacco was relatively uncommon in this sample of Midwestern US males. This is consistent with previous studies conducted in the United States16 and in Norway.21 Our finding of low rates of dual use may be partially due to the age of the sample as studies have reported that dual use is more common among adolescent and young adult males than among older males.16,22 The sample for the current study was in young adulthood in 1987 and had an average age of 44 in 2009. Thus, dual use may be a more recent phenomenon, and its prevalence among young tobacco users should continue to be monitored. However, for older adults, these findings suggest that cessation interventions should focus on specific types of tobacco products rather than tobacco in general.
We were also interested in exploring patterns of tobacco use that suggested switching of tobacco products. One possibility was switching from smokeless tobacco to cigarettes in support of the notion that smokeless tobacco use in adolescence acts as a “gateway” to later cigarette smoking in adulthood. Another possibility was that cigarette smokers switched to smokeless tobacco in adulthood because of the increase in smoking restrictions in workplaces and public places or because of the belief that smokeless tobacco products are less harmful than cigarette smoking. However, in these data, there was very little evidence of switching in either direction. A 1-year study of a national US sample also reported that switching was infrequent.17 The current study provides additional evidence over a much longer period of time that tobacco users are unlikely to switch to a different product. Instead, they are more likely to stay with the same product or quit altogether.
An additional objective of this study was to test adolescent health beliefs associated with trajectory group membership. In general, adolescents who held the most favorable beliefs toward cigarette smoking were most likely to be members of the consistent regular smoking group into adulthood. This was the case for personally relevant health beliefs about smoking, general health beliefs about smoking, normative beliefs about smoking, and perceived prevalence of smoking. Prior studies of correlates of smoking trajectories into young adulthood similarly found that pro-smoking beliefs were related to membership in the highest risk groups.2,4 These beliefs represent targets for change for antismoking interventions. Interestingly, the one belief for which this pattern did not hold true was personalized risk of addiction to smoking. Thus, the current findings suggest that, for adolescents, messages related to the risk of addiction may not be as effective as messages about health beliefs or normative beliefs.
Because this is the first study to empirically identify trajectories of smokeless tobacco use that extend into adulthood, it is also the first to test correlates of long-term smokeless trajectory group membership. Similar to the findings for cigarette smoking, adolescents who were most favorable to smokeless tobacco for personally relevant health beliefs, general health beliefs, normative beliefs, and perceived prevalence were most likely to be members of the consistent regular smokeless tobacco use trajectory group. Also, personalized risk of addiction to smokeless tobacco use did not distinguish membership in the smokeless tobacco trajectory groups. Therefore, adolescent smokeless tobacco prevention programs should make use of existing successful intervention strategies that focus on changing health beliefs, normative beliefs, and perceived prevalence.
Finally, we tested for correlates of membership in the dual cigarette smoking and smokeless tobacco use groups. In one instance, personalized risk of addiction to smoking, study participants who were in both the delayed onset regular, then cessation smoking trajectory group and the early onset, then cessation smokeless tobacco use group had a high level of perceived risk compared to the other groups. All other groups were similar in terms of their perceived risk of addiction to smoking. This group may have been at elevated risk of any tobacco use, and their high level of personalized risk of addiction to smoking led them to start with smokeless tobacco but then later initiate cigarette smoking. A second significant interaction indicated that individuals in the consistent regular smokeless tobacco use group and the early onset regular, then cessation smoking group had more pro-smokeless tobacco normative beliefs compared to the other groups. It is important to note that these were very small groups as were all of the dual use groups. Thus, we may have been limited in our ability to identify correlates of dual trajectory group membership. Moreover, the lack of significant interactions in the present analyses may be because the health beliefs were measured at a static point during adolescence, so they may be more reflective of the adolescent experience with tobacco products. Nonetheless, these beliefs may still be important because adolescent experiences may influence later decisions made during adulthood.
Although this study is the first to use longitudinal data to identify dual trajectories of cigarette smoking and smokeless tobacco use among men from adolescence to mid-life, there are limitations to note. First, the community from which this representative sample was drawn is predominantly white, non-Hispanic, and located in the Midwestern United States. Thus, these findings may not generalize to other racial and ethnic groups and other geographic regions or countries. However, smokeless tobacco use is more prevalent among white, non-Hispanic males in the Midwestern United States than among other groups,14 so the findings may be generalizable to groups at elevated risk of dual use of cigarettes and smokeless tobacco. Second, because waves of data collection in this study were separated by 6 years, we were unable to detect any short-term changes in tobacco use behaviors that may have taken place. For example, we may have missed instances of cigarette smokers switching to smokeless tobacco between waves of data collection and then reporting abstinence from both at the next wave. Third, the missing data from 1987 on health beliefs should be taken into account as those in the regular use trajectory groups for both cigarettes and smokeless tobacco were more likely to be missing these data compared to the other groups. Fourth, dual use was defined using seven sub-categories of smoking but only three sub-categories of smokeless tobacco use. More refined definitions of smokeless tobacco use, and therefore dual use, may identify a higher prevalence of dual use. Finally, as noted previously, the health beliefs tested in this study were measured during adolescence predicting future use, and beliefs may change over time.
This study adds to the literature on trajectories of tobacco use in important ways. No prior study has identified trajectories of smokeless tobacco use and dual use of cigarettes and smokeless tobacco from adolescence to adulthood. The analyses presented here found little evidence of dual use in this Midwestern US sample. Moreover, there appeared to be little switching from one tobacco product to another. These findings support the use of product-specific messaging in prevention and cessation interventions. Finally, adolescent health beliefs and normative beliefs were important correlates of subsequent patterns of cigarette smoking and smokeless tobacco use. These beliefs are potentially useful targets in campaigns to prevent adolescents’ use of cigarettes and smokeless tobacco.
Funding
This work was supported by the National Institute on Drug Abuse at the National Institutes of Health (DA013555).
Declaration of Interests
None declared.
References
- 1. Colder CR, Mehta P, Balanda K, Campbell RT, Mayhew KP, Stanton WR. Identifying trajectories of adolescent smoking: an application of latent growth mixture modeling. Health Psychol. 2001;20(2):127–135. doi:10.1037/0278-6133.20.2.127. [DOI] [PubMed] [Google Scholar]
- 2. Chassin L, Presson CC, Sherman SJ, Pitts S. The natural history of cigarette smoking from adolescence to adulthood in a midwestern community sample: multiple trajectories and their psychosocial correlates. Health Psychol. 2000;19(3):223–231. doi:10.1037/0278-6133.19.3.223. [PubMed] [Google Scholar]
- 3. Karp I, O’Loughlin J, Paradis G, Hanley J, Difranza J. Smoking trajectories of adolescent novice smokers in a longitudinal study of tobacco use. Ann Epidemiol. 2005;15(6):445–452. doi:10.1016/j.annepidem.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 4. Orlando M, Tucker JS, Ellickson PL, Klein DJ. Developmental trajectories of cigarette smoking and their correlates from early adolescence to young adulthood. J Consult Clin Psychol. 2004;72(3):400–410. doi:10.1037/0022-006X.72.3.400. [DOI] [PubMed] [Google Scholar]
- 5. Stanton WR, Flay BR, Colder CR, Mehta P. Identifying and predicting adolescent smokers’ developmental trajectories. Nicotine Tob Res. 2004;6(5):843–852. doi:10.1080/14622200410001734076. [DOI] [PubMed] [Google Scholar]
- 6. Rosendahl KI, Galanti MR, Gilljam H. Trajectories of smokeless tobacco use and of cigarette smoking in a cohort of Swedish adolescents: differences and implications. Nicotine Tob Res. 2008;10(6):1021–1027. doi:10.1080/14622200802097522. [DOI] [PubMed] [Google Scholar]
- 7. Wetter DW, McClure JB, de Moor C, et al. Concomitant use of cigarettes and smokeless tobacco: prevalence, correlates, and predictors of tobacco cessation. Prev Med. 2002;34(6):638–648. doi:10.1006/pmed.2002.1032. [DOI] [PubMed] [Google Scholar]
- 8. Haddock CK, Weg MV, DeBon M, et al. Evidence that smokeless tobacco use is a gateway for smoking initiation in young adult males. Prev Med. 2001;32(3):262–267. doi:10.1006/pmed.2000.0802. [DOI] [PubMed] [Google Scholar]
- 9. Severson HH, Forrester KK, Biglan A. Use of smokeless tobacco is a risk factor for cigarette smoking. Nicotine Tob Res. 2007;9(12):1331–1337. doi:10.1080/14622200701705209. [DOI] [PubMed] [Google Scholar]
- 10. Tomar SL. Is the use of smokeless tobacco a risk factor for cigarette smoking? The U.S. experience. Nicotine Tob Res. 2003;5(4):561–569. doi:10.1080/14622200307249. [DOI] [PubMed] [Google Scholar]
- 11. Kozlowski LT, O’Connor RJ, Edwards BQ, Flaherty BP. Most smokeless tobacco use is not a causal gateway to cigarettes: using order of product use to evaluate causation in a national US sample. Addiction. 2003;98(8):1077–1085. doi:10.1046/j.1360-0443.2003.00460.x. [DOI] [PubMed] [Google Scholar]
- 12. O’Connor RJ, Flaherty BP, Edwards BQ, Kozlowski LT. Regular smokeless tobacco use is not a reliable predictor of smoking onset when psychosocial predictors are included in the model. Nicotine Tob Res. 2003;5(4):535–543. doi:10.1080/1462220031000118676. [DOI] [PubMed] [Google Scholar]
- 13. O’Connor RJ, Kozlowski LT, Flaherty BP, Edwards BQ. Most smokeless tobacco use does not cause cigarette smoking: results from the 2000 National Household Survey on Drug Abuse. Addict Behav. 2005;30(2):325–326. doi:10.1080/1462220031000118676. [DOI] [PubMed] [Google Scholar]
- 14. McClave-Regan AK, Berkowitz J. Smokers who are also using smokeless tobacco products in the US: a national assessment of characteristics, behaviours, and beliefs of ‘dual users.’ Tob Control. 2011;20(3):239–242. doi:10.1136/tc.2010.039115. [DOI] [PubMed] [Google Scholar]
- 15. Mushtaq N, Williams MB, Beebe L. Concurrent use of cigarettes and smokeless tobacco among US males and females. J Environ Public Health. 2012;2012:1–11. doi:10.1155/2012/984561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tomar SL, Alpert HR, Connolly GN. Patterns of dual use of cigarettes and smokeless tobacco among US males: findings from national surveys. Tob Control. 2010;19(2):104–109. doi:10.1136/tc.2009.031070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhu SH, Wang JB, Hartman A, et al. Quitting cigarettes completely or switching to smokeless tobacco: do US data replicate the Swedish results? Tob Control. 2009;18(2):82–87. doi:10.1136/tc.2008.028209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Boyle RG, Claire AW, St, Kinney AM, D’Silva J, Carusi C. Concurrent use of cigarettes and smokeless tobacco in Minnesota. J Environ Public Health. 2012;2012:1–6. doi:10.1155/2012/493109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jones BL, Nagin DS. A Stata Plugin for Estimating Group-Based Trajectory Models 2012. www.indiana.edu/~wim/docs/Info%20about%20STATA%20plugin.pdf Accessed December 22, 2014.
- 20. Bland JM, Altman DG. Multiple significance tests: the Bonferroni method. BMJ. 1995;310(6973):170 www.ncbi.nlm.nih.gov/pmc/articles/PMC2548561/pdf/bmj00576-0038.pdf Accessed December 29, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lund KE, McNeill A. Patterns of dual use of snus and cigarettes in a mature snus market. Nicotine Tob Res. 2013;15(3):678–684. doi:10.1093/ntr/nts185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rath JM, Villanti AC, Abrams DB, Vallone DM. Patterns of tobacco use and dual use in US young adults: the missing link between youth prevention and adult cessation. J Environ Public Health. 2012;2012:1–9. doi:10.1155/2012/679134. [DOI] [PMC free article] [PubMed] [Google Scholar]