Abstract
Mycobacterium tuberculosis (Mtb), the causative agent of tuberculosis (TB), has infected over 1.7 billion people worldwide and causes 1.4 million deaths annually. Recently, genome sequence analysis has allowed the reconstruction of Mycobacterium tuberculosis complex (MTBC) evolution, with the identification of seven phylogeographic lineages: four referred to as evolutionarily “ancient”, and three “modern”. The MTBC strains belonging to “modern” lineages appear to show enhanced virulence that may have warranted improved transmission in humans over ancient lineages through molecular mechanisms that remain to be fully characterized. To evaluate the impact of MTBC genetic diversity on the innate immune response, we analyzed intracellular bacterial replication, inflammatory cytokine levels, and autophagy response in human primary macrophages infected with MTBC clinical isolates belonging to the ancient lineages 1 and 5, and the modern lineage 4. We show that, when compared to ancient lineage 1 and 5, MTBC strains belonging to modern lineage 4 show a higher rate of replication, associated to a significant production of proinflammatory cytokines (IL-1β, IL-6, and TNF-α) and induction of a functional autophagy process. Interestingly, we found that the increased autophagic flux observed in macrophages infected with modern MTBC is due to an autocrine activity of the proinflammatory cytokine IL-1β, since autophagosome maturation is blocked by an interleukin-1 receptor antagonist. Unexpectedly, IL-1β-induced autophagy is not disadvantageous for the survival of modern Mtb strains, which reside within Rab5-positive phagosomal vesicles and avoid autophagosome engulfment. Altogether, these results suggest that autophagy triggered by inflammatory cytokines is compatible with a high rate of intracellular bacilli replication and may therefore contribute to the increased pathogenicity of the modern MTBC lineages.
Introduction
Mycobacterium tuberculosis (Mtb) emerged as a human pathogen 75–150 thousand years ago and spread by clonal expansion among human communities since then, giving rise to seven phylogeographic lineages which show a relatively limited genetic variability, consisting of large-sequence polymorphisms (LSPs) and single-nucleotide polymorphisms (SNPs)1–3. The lineages present in the Mtb complex (MTBC) are distinguished as ancient and modern. The ancient ones comprise two Mtb lineages (lineage 1 and the recently identified lineage 7) causing tuberculosis (TB) in humans, and two M. africanum lineages, one of which includes bacilli responsible for TB in animal species4. The modern lineages 2, 3, and 4 consist of Mtb strains responsible for the largest and deadliest epidemics of the last few centuries and that are driving the current pandemics in Sub-Saharan Africa, Southeast Asia, and Eastern Europe, while the ancient lineage 1 causes TB mainly in the Indo-Oceanic regions and the Philippines5. Despite the limited genetic variability within MTBC, the strains belonging to different lineages show significant differences in terms of pathogenicity, transmissibility, and host specificity, as highlighted by the differences between M. tuberculosis, M. africanum, and M. bovis strains. Even human-adapted MTBC strains (Mtb) show phenotypic differences in terms of intracellular survival and transcriptional profile in macrophages6–10 and virulence in mice9,10. The impact of these phenotypic differences between the human-adapted strains on TB disease and transmission remains elusive, although the observed sympatric association between Mtb lineages and ethnic human groups supported the continuous adaptive process between Mtb and its host11,12.
The balance between immune activation and inflammation influences the outcome of Mtb infection. Interferon-γ (IFN-γ) and tumor necrosis factor-α (TNF-α), mainly produced by type-1 T helper cells, are key cytokines to contrast Mtb infection13,14. IFN-γ production is regulated by interleukin (IL) 12, which is secreted by activated phagocytes. Other important proinflammatory cytokines are IL-1β and IL-6, which may lead to the Th17-differentiation, as a subset of T cells essential for the formation of mature pulmonary granulomas13,15. Although both inflammatory and adaptive responses are crucial for contrasting mycobacteria infection16–18, the extensive immune activation may be self-defeating for the host, paving the way to active TB development and aggravation13,19,20.
Mtb has developed elaborate survival mechanisms to persist in the host cells, being able to avoid the immune system but, at the same time, chronically stimulating it. The main immune evasion strategies adopted by Mtb are based on the inhibition of (a) phagolysosomes formation; (b) antigen processing and presentation to escape from T-cell surveillance; (c) IFN-γ-signaling pathway; and (d) autophagy15,21–25.
The role of autophagy during Mtb infection has been extensively investigated in the last few years. It is well-known that, besides controlling the turnover of intracellular components, autophagy captures invading pathogens and delivers them to the lysosome for elimination26. In this process, target materials are engulfed by double-membrane vesicles, termed autophagosomes, which eventually fuse to lysosomes27,28. A specific set of genes, called ATGs, are dedicated to the regulation of autophagy29. Among them, members of the Atg8 family, e.g., LC3, are required for autophagosomal membranes expansion and closure, as for the selective recognition of autophagy substrates, including viruses and bacteria, by interacting with adaptor proteins, such as the sequestosome 1/p62-like receptors, which directly bind to cargos30.
Both the innate and adaptive responses required a functional autophagic process in order to accomplish their goals31,32. Accordingly, autophagy is strictly regulated by a variety of immune sensors, such as Toll-like receptors, Nod-like receptors, IRGM, and nucleic-acid sensors33. Moreover, proinflammatory Th1 cytokines, such as IFN-γ, TNF-α, and IL-1β, induce autophagy, while anti-inflammatory Th2 cytokines, such as IL-4 and IL-13 are inhibitory34,35. On the other hand, autophagy generally plays an inhibitory role on inflammation, either by eliminating the infectious agent or by physical interaction of ATG proteins with components of the inflammatory pathways, contributing in this way to temporally limit the inflammation response26.
Several evidences show that Mtb can avoid autophagic degradation and may actually exploit this process to its own advantage by using multiple strategies36,37. The type-VII secretion system ESX-1 plays a central role in the modulation of autophagy by Mtb H37Rv, being responsible for a rapid activation of autophagy by bacterial DNA through the cytosolic DNA sensor STING38,39, as well as for the inhibition of autophagosome–lysosome fusion when infection is established40,41. Importantly, autophagy stimulation mediated by cytokines and T cells is able to rescue the block imposed by Mtb and favors its killing36,41.
Unexpectedly, recent studies show that, apart from ATG5, autophagy-deficient mice do not show increased susceptibility to Mtb42. Although these data appear to diminish the contribution of basal autophagy in controlling Mtb, they are consistent with the reported ability of this bacterium to effectively inhibit autophagy during infection25.
Since most of the studies on the host immune response to Mtb infection have been performed using the laboratory strain H37Rv, we decided to characterize whether genetic variability of Mtb may account for a different ability to modulate the inflammatory response and autophagy flux in primary macrophages.
Results
Selection of MTBC strains
To investigate the impact of MTBC genetic diversity on intracellular growth, inflammatory response, and autophagy, six MTBC strains were randomly chosen from a collection of clinical strains based on their genotype determined by spoligotyping (Fig. 1a). We selected two Mtb strains of the ancient phylogeographic lineage 1, belonging to clades EAI1_SOM and EAI2_Manilla, and a strain of M. africanum, belonging to the ancient lineage 5, which includes strains causing TB in a restricted area of West Africa or in recent immigrants from those regions5,43. Two strains belonging to the highly successful phylogeographic lineage 4, of clades H3 and T1, and one strain from lineage 3, clade CAS1-Kili, were selected as representative of the modern Mtb strains. We also included the Mtb reference strain H37Rv, that, while belonging to the modern lineage 4, has been subjected to many in vitro passages that may have altered its virulence properties44. These strains were chosen because they may fairly represent the genetic diversity of MTBC at the global level.
Fig. 1. Genetic characterization and replication properties of MTBC strains from ancient and modern lineages in human primary macrophages.
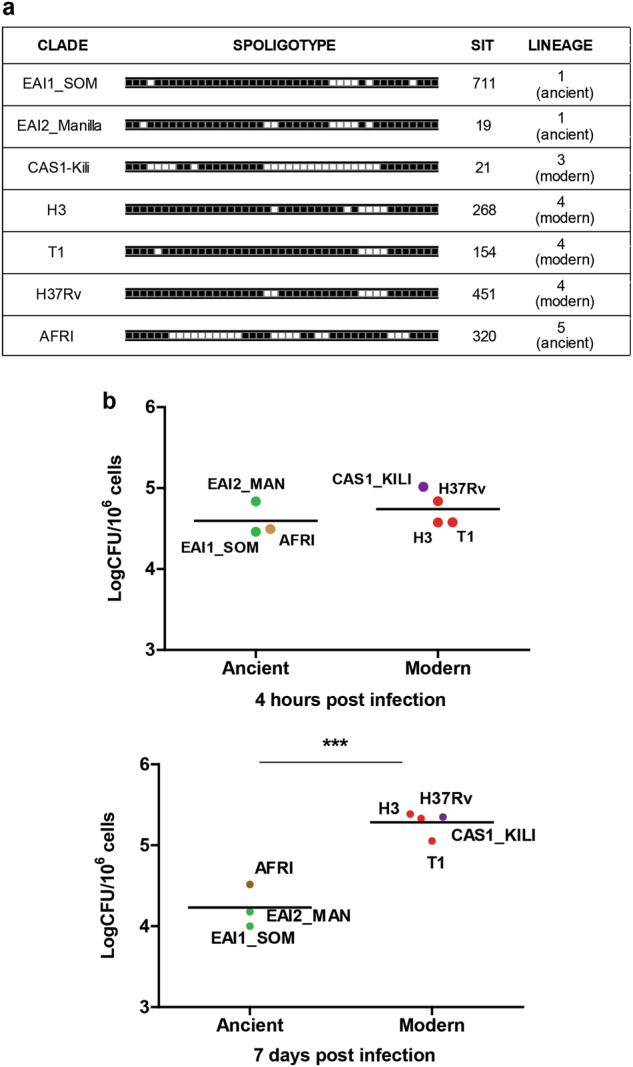
a Characterization of MTBC lineages by spoligotyping. b Macrophages were infected with the indicated MTBC strains. Four hours (upper panel) and 7 days (lower panel) after infection, cells were lysed to measure the number of viable bacteria by plating for determining CFU. Values are expressed as a mean of three independent experiments
Mtb strains belonging to the modern lineage show a higher rate of intracellular replication
To characterize the virulence properties of the selected MTBC strains, human monocyte-derived macrophages (MDM) were infected at MOI 1:1 and intracellular CFUs were determined at 4 h and 7 days post infection. As shown in Fig. 1b (upper panel), no significant differences were observed in the intracellular CFUs at 4 h post infection, indicating a similar ability of ancient and modern strains to gain access to macrophages. Analysis of the intracellular CFUs at day 7 post infection (Fig. 1b, lower panel) indicated a poor capacity of the two EAI strains to survive and replicate intracellularly and also the M. africanum strain showed limited ability to persist in macrophages. Conversely, all Mtb strains of the modern clades were capable of replicating intracellularly, with a similar level of intracellular CFUs. Macrophages infected with different Mtb strains showed similar viability, as indicated by evaluating LDH release (data not shown), indicating that cytotoxicity may not account for the observed differences of CFUs.
Taken together, these results indicate that the MTBC strains of the modern clades show enhanced ability to replicate intracellularly compared to the strains belonging to the ancient clades.
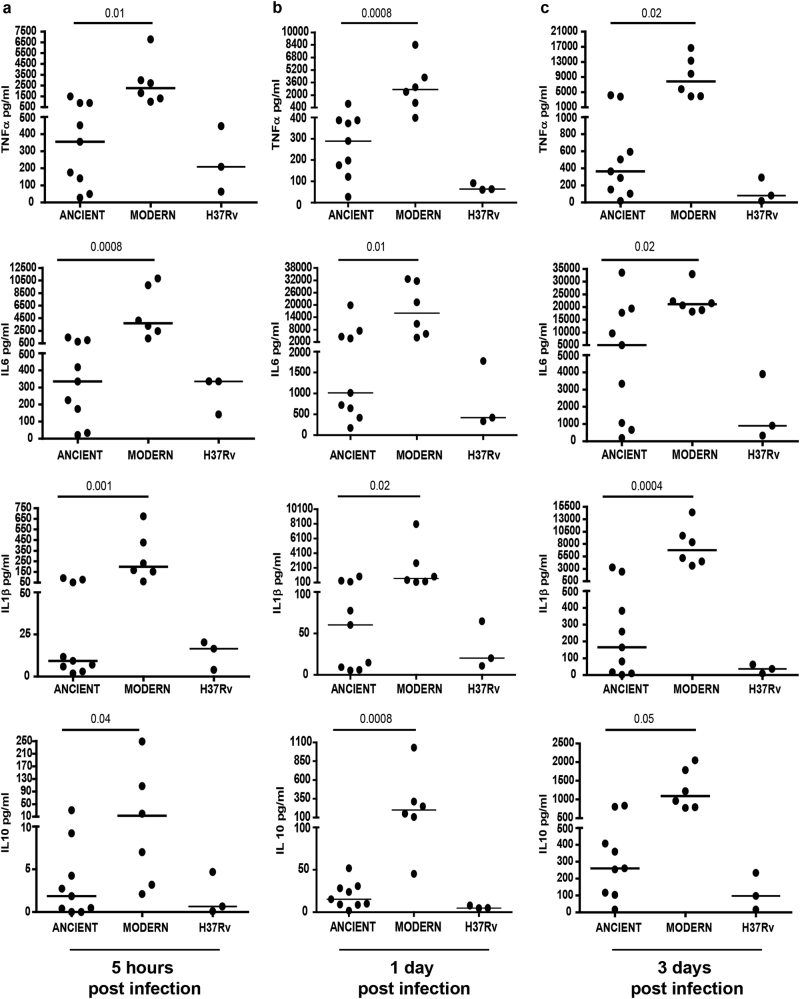
Mtb strains of modern lineages produce higher levels of inflammatory cytokines
The levels of inflammatory cytokines upon infection of human primary macrophages with modern and ancient MTBC strains were evaluated by cytometry. As shown in Fig. 2 and S1, infection with the modern lineage strains induced a higher production of TNF-α, IL-6, IL-1β, and IL-10 compared to the ancient strains at 5 h (Fig. 2a: p = 0.01, p = 0.0008, p = 0.001, and p = 0.04, respectively), 1 day (Fig. 2b: p = 0.0008, p = 0.01, p = 0.02, and p = 0.0008, respectively) and 3 days post infection (Fig. 2c: p = 0.02, p = 0.02, p = 0.0004, and p = 0.05, respectively).
Fig. 2. Evaluation of inflammatory cytokine production in human primary macrophages infected with MTBC strains of ancient and modern lineages.
Cell culture supernatants were collected from macrophages infected with MTBC (MOI 1:1) at 5 h (a), 1 (b), and 3 (c) days. The production of TNF-α, IL-6, IL-1β, and IL-10 was measured by CBA Flex Set. The results are represented as median of data obtained from modern (H3 and T1) and ancient (EAI1_SOM, EAI2_MANILLA) Mtb strains. Data obtained from individual MTBC strain infections are reported in Figure S1
These data indicate that a proinflammatory signature is induced by macrophage infection with modern Mtb strains.
Mtb strains of the modern lineage 4 induce a functional autophagy flux
Autophagy flux was analyzed in human primary macrophages infected with the different Mtb strains described in Fig. 1a by comparing the levels of the autophagosome protein LC3-II in the presence or absence of lysosome inhibitors. In macrophages infected for 24 h with the ancient Mtb strains, EAI1_SOM, EAI2_Manilla (lineage 1), and AFRI (lineage 5), the inhibition of lysosomal activity does not result in a significant accumulation of LC3-II compared to the untreated cells, indicating that the fusion of autophagosomes with the lysosomes is impaired (Fig. 3a), similar to what was previously reported for the laboratory strain H37Rv40,41. Conversely, in macrophages infected with the modern Mtb strains H3 and T1, the lysosome inhibitors significantly increased LC3-II levels compared to the untreated cells (Fig. 3b), indicating that newly formed autophagosomes are efficiently delivered to the lysosomes in these cells. Similar results were obtained when autophagic flux was analyzed at 5 h after infection with ancient and modern Mtb strains (Figure S2a). Autophagy induction following infection was prevented by using the phosphatidylinositol 3-kinase inhibitor wortmannin, indicating that modern Mtb strains trigger a canonical autophagic pathway (Figure S2b).
Fig. 3. Analysis of autophagy flux in human primary macrophages infected with MTBC strains of ancient and modern lineages.
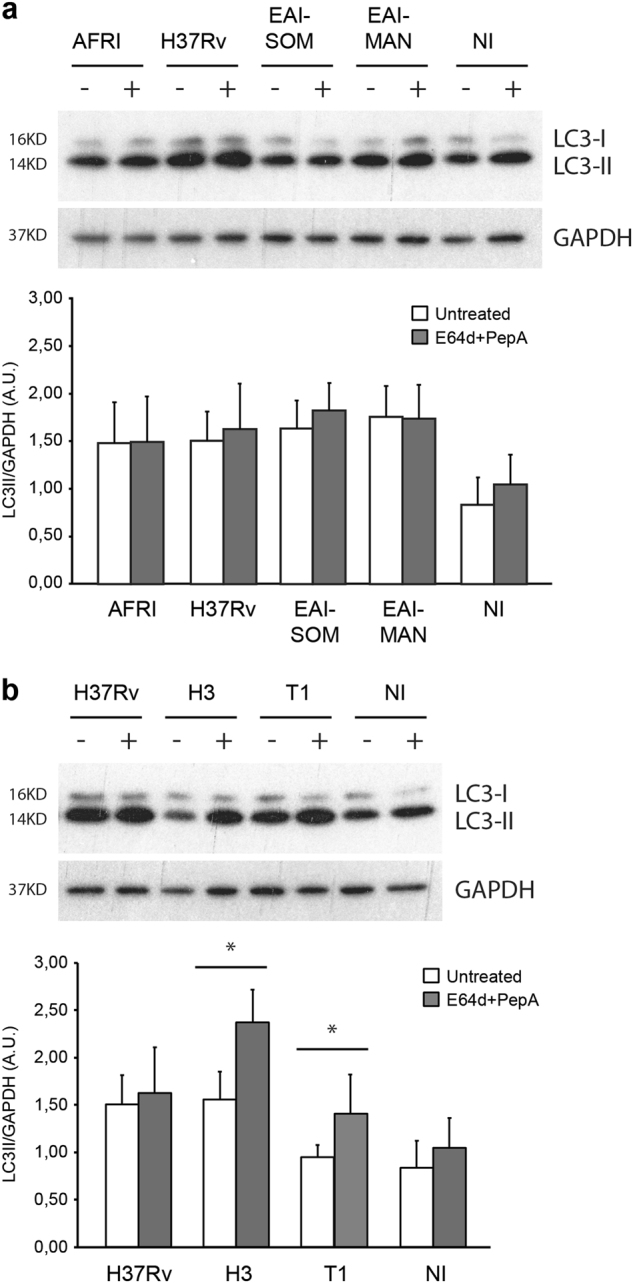
Macrophages were infected with the indicated ancient (a) or modern (b) MTBC strains and with H37Rv as a reference strain. After 20 h, cells were either incubated with E64d + PepA to inhibit lysosome activity or left untreated. Autophagy levels were analyzed for LC3 expression by immunoblotting. GAPDH levels were analyzed to normalize the amount of protein loaded (upper panels). LC3-II/GAPDH ratios were quantified by densitometric analysis using the ImageQuant software. Each point value represents the mean ± SD from three independent experiments (lower panels). NI: not infected
The Mtb H3 strain of lineage 4 evades the autophagy sequestration
Considering the important contribution of autophagy in Mtb clearance24, the increased autophagy flux observed in macrophages infected with the modern strains appeared to be in contrast with their high rate of replication. These data prompted us to investigate whether modern Mtb strains are spared from the autophagosome-mediated degradation, despite their ability to trigger autophagy.
To this aim, confocal analysis was carried out to evaluate the colocalization of mycobacteria with the autophagic marker LC3, as well as with ubiquitin and the ubiquitin-binding autophagy adaptors NDP52 and NBR1, which have been reported to mediate the engulfment of Mtb in autophagosomes39,45. Mtb H3 was chosen as a representative strain for the modern lineage and compared to H37Rv. As shown in Fig. 4a and S3, Mtb H3 shows low levels of colocalization with LC3, ubiquitin, NDP52 and NBR1, indicating that Mtb H3 is not targeted by autophagy.
Fig. 4. Analysis of Mtb H3 localization within autophagosomal/autolysosomal vesicles.
Primary macrophages were infected with H3 and H37Rv Mtb. Cells were fixed and analyzed for LC3 (a) or LAMP1 (b) localization by immunofluorescence using specific antibodies, while Mtb was detected by auramine staining. The images show that the merging of the two fluorescence signals is shown on the left panels. Green: Mtb; red: LC3 in (a), LAMP1 in (b). Scale bar, 6 μm. Colocalization rate was measured by Mander’s coefficient calculated by ImageJ software. Graphics reporting a quantification of the experiments is shown in the right panels. The results represent the mean ± SD of three independent experiments
Moreover, we tested the ability of Mtb H3 to prevent the lysosomal degradation, which may occur by the maturation of either phagosomal or autophagosomal compartments. As shown in Fig. 4b, Mtb H3 showed a low level of colocalization with the lysosomal marker LAMP1, similar to what was observed in H37Rv-infected cells.
Altogether, our data indicate that, although macrophage infection with modern Mtb strains leads to an increased autophagy flux, these bacteria are able to elude the autophagy machinery.
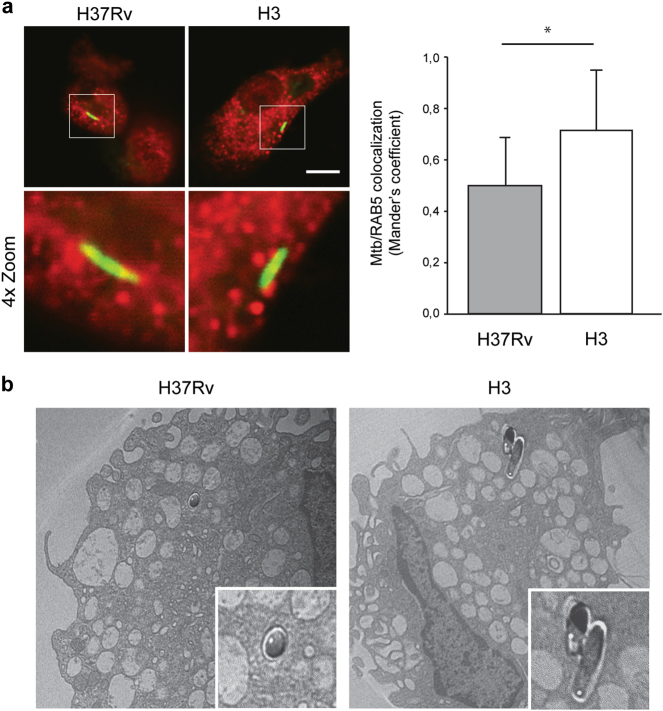
Recently, Mtb strains belonging to the modern lineages were reported to have a preferential cytosolic residence in the infected macrophages, which was proposed as an alternative adaptation mechanism to avoid the autophagy degradation46. Thus, we investigated if the autophagy-resistant properties of the modern Mtb H3 were due to an increased cytosolic localization. To this aim, confocal analyses were performed to evaluate the localization of H37Rv and H3 mycobacteria within Rab5-positive or CD63-positive endosomal/phagosomal compartments (Fig. 5a and S4). Our data show that Mtb H3 has a predominant phagosomal localization, similar to what was observed in H37Rv-infected cells. Phagosomal localization of Mtb H3 was also confirmed by performing electron microscopy analysis (Fig. 5b).
Fig. 5. Analysis of localization Mtb H3 within the endosomal compartment.
a Primary macrophages were infected with H3 and H37Rv Mtb. Cells were fixed and analyzed for Rab5 localization by immunofluorescence using a specific antibody, while Mtb was detected by auramine staining (left panel). The images show that the merging of the two fluorescence signals is shown on the left panels. Green: Mtb; red: RAB5. Scale bar, 6 μm. Colocalization rate was measured by Mander’s coefficient calculated by Image J software. Graphics reporting a quantification of the experiments is shown in the right panel. The results represent the mean ± SD of three independent experiments. b Ultrastructural analysis of Mtb H37Rv and H3-infected macrophages 24 h post infection. Mycobacteria are indicated by asterisks (×1.500). A magnification of Mtb-containing vesicles is shown in the panels below (×4.000)
Taken together, these results suggest that, similar to H37Rv, Mtb H3 is able to prevent its autophagosomal engulfment by hiding within the phagosomes.
Mtb H3 strain of lineage 4 induces a functional autophagy flux through IL-1β-dependent signaling
Our data show that modern Mtb strains of lineage 4 induce high levels of IL-1β production and autophagy. Since IL-1β has been demonstrated to be a powerful inducer of autophagy in human macrophages47, we investigated the functional relationship between IL-1β and autophagy in Mtb H3-infected macrophages.
To this aim, IL-1β activity was blocked using an IL-1 receptor antagonist (IL-1-RA) and autophagy flux evaluated by western blot analysis. Notably, IL-1-RA treatment inhibited the autophagic flux in macrophages infected with Mtb H3, as shown by the reduced increase of the autophagy markers LC3-II and p62 observed after the inhibition of the lysosomal activity (Fig. 6). According to the capability of Mtb H3 to escape the autophagic response, the inhibition of either IL-1β signaling by IL-1-RA or the IL-1β-induced autophagic flux by a lysosome inhibitor did not have an impact on bacterial growth in infected macrophages (Figure S5).
Fig. 6. Role of IL-1β on the induction of autophagy triggered by Mtb H3.

Macrophages were infected with the Mtb H3 and H37Rv strains. After 2 h, uninfected and infected cells were treated with an IL-1β receptor antagonist or left untreated. After 20 h, cells were incubated with E64d + PepA to inhibit lysosome activity or left untreated. Autophagy levels were analyzed by evaluating LC3 and p62 expression by immunoblotting. GAPDH levels were analyzed to verify protein amount loading (upper panels). LC3-II/GAPDH ratios were quantified by densitometric analysis using the ImageQuant software. Each point value represents the mean ± SD from three independent experiments (lower panel)
These data suggest that the different ability of ancient and modern Mtb to modulate the autophagy flux in macrophages is associated with their inflammatory properties.
Discussion
Recent studies have shown the presence of lineage-specific effects on the outcome of Mtb infection and disease11. However, how the differences of Mtb genomes impact on the host response remains poorly characterized. Here, we compared ancient and modern MTBC strains with regard to their ability to replicate in human macrophages and to modulate innate immune responses in terms of proinflammatory cytokines and autophagy. We found that strains of the modern lineages 3 and 4 have an improved ability to grow in human primary infected macrophages compared to strains of the ancient lineages 1 and 5. These results are in line with previous findings showing an enhanced intracellular survival and replication rate of the strains belonging to the modern lineages when compared to the reference strains (H37Rv and CDC1551) and the MTBC strains of the ancient lineages (EAI and M. africanum), which showed an even less efficient intracellular survival6,10. However, it should be noted that differences in the intracellular replication rate have also been observed between strains belonging to the same lineage, indicating the presence of both intra-lineage or intra-genotype variability48,49.
Unexpectedly, a more efficient intracellular replication is paralleled by an increased production of inflammatory cytokines and higher levels of autophagy. In detail, we found that TNF-α, IL-1β, IL-6, and IL-10 levels are higher in H3 and T1 strains of lineage 4 than in the two EAI strains from lineage 1 and M. africanum. To note, the anti-inflammatory cytokine IL-10 is also increased after H3 and T1 infection. This observation is in agreement with the important role proposed for this cytokine in counterbalancing an excessive innate and adaptive immune response against Mtb, and could represent an important target to alter the survival rate of the modern Mtb strains in macrophages16,50.
It has been previously reported that mycobacteria belonging to the modern lineages induce a lower immune response compared to the ancient ones8. In fact, Portevin and colleagues observed a reduction of proinflammatory cytokine levels in both macrophages, monocyte-derived dendritic cells, and murine bone marrow-derived macrophages. Possible differences that may account for this discrepancy could be represented by the procedure we used for the ex vivo differentiation of macrophages, which does not include GM-CSF8, or the difference in the clinical isolates tested51. In fact, it has been observed that distinct clinical isolates from the same lineages may differently modulate the immune response51.
Activation of proinflammatory responses by Mtb infection depends on the binding of bacterial components to extracellular PRRs52 and to the intracellular activation of the NLRP3 inflammasome53. It has been shown that differences in surface lipids, sugars, and protein compositions among Mtb strains may impact the innate immune responses54–56. Moreover, intracellular pathogen recognition pathways, including IL-1β production via the NLRP-3 inflammasome and type-I IFNs via the cGAS/STING pathway, can be differently stimulated according to the level of secreted EsxA57. It follows that differential expression or polymorphisms affecting ESX-1 may have an impact on IL-1β secretion, probably by influencing the translocation of proteins and other Mtb metabolites to the cytosol of infected macrophages58. However, since MTBC strains belonging to modern and ancient lineages were shown to differentially induce type-I IFN, despite the fact that these strains were equally capable of accessing the cytosol59, it is likely that multiple factors may contribute to the inflammatory response to different MTBC strains, as, for example, the extent of the mitochondrial damage.
Activation of IL-1β has been previously shown to promote Mtb killing through the activation of the TNF-α signaling, which culminates with caspase-3-induced apoptosis followed by the uptake and the lysosomal degradation of Mtb-containing apoptotic bodies by uninfected neighbors, a process defined as efferocytosis60,61. In addition, IL-1β is also known to induce autophagy that in turn has been shown to restrict Mtb replication in macrophages47. In line with these observations, the H3 and T1 strains, which trigger a higher level of IL-1β compared with ancient and reference strains, induce a functional autophagic process, as shown by analyzing the degradation rate of the autophagosomal marker LC3II. Conversely, cells infected with ancient MTBC strains and H37Rv, secrete lower levels of IL-1β and show an inhibited autophagic flux. Notably, we found that the increased production of IL-1β was indeed responsible for the induction of autophagy, since an inhibitor of IL-1β prevented autophagy flux in H3-infected macrophages, reestablishing the block of autophagosome maturation observed with H37Rv and the ancient strains. However, despite the higher autophagy induction and consistent with its increased ability to survive in macrophages, Mtb H3 strain is able to hide within endosomal compartments and to elude autophagosome engulfment and consequent lysosomal degradation. Understanding the molecular mechanisms that allow modern Mtb strains to escape IL-1β-induced autophagy degradation will be relevant to design novel therapeutic strategies aimed at preventing their intracellular survival. The fact that several drugs specifically targeting autophagy, inflammation, and immunometabolism have been shown to exert anti-TB activity highlights the potential consequences of these studies in terms of development of new host-directed therapies against TB62–64.
Modulation of IL-1β and autophagy levels may have a relation with the increased virulence observed in strains of modern lineages. In fact, IL-1β is required for protection against TB but a chronic high level of IL-1β is associated with pathology, likely causing a non-protective response65. At the same time, IL-1β-induced autophagy could turn out to be beneficial for chronic infection by sustaining macrophages metabolism66 and protecting against excessive inflammation during Mtb infection67. In this line, it has been recently proposed that Mtb may selectively regulate autophagy to extend survival in infected macrophages68. This hypothesis is also supported by our observation that infection with modern Mtb strains does not result in decreased macrophage viability, which would have been expected in cells infected with highly replicating Mtb strains. Hence, the ability of modern Mtb strains to efficiently replicate intracellularly in macrophages, while inducing autophagy, may represent an advantage acquired during evolution to enhance bacilli persistence in inflammed host tissues. Potential limitations of the present study should be considered. We analyzed a relatively small number of clinical isolates. However, although larger studies are needed to confirm these observations, the data generated here on the modulation of the autophagy process are confirmed by different approaches such as immunoblotting, confocal, and electron microscopy.
In view of these findings, it will be important to test how the different ability of modern Mtb strains to alter autophagy and inflammation impacts on the regulation of specific T-cell response. This is expected to uncover new aspects on the complex mechanism that allows Mtb to escape the immune response and be protected from vaccinal approaches. The results of this study may have translational implications for the design of new TB vaccines or host-directed therapies, which should take into account both the autophagic and immunogenic characteristics of the lineage of the Mtb candidate.
Materials and methods
MTBC strains
The MTBC strains used in this study were selected from a collection of clinical strains isolated at the Università Cattolica del Sacro Cuore in Rome and Mtb H37Rv was used as a reference strain. The MTBC strains were grown in Middlebrook 7H9 (Difco BD, NY) medium supplemented with 0.2% glycerol, 10% ADC (bovine albumin fraction V, dextrose, and catalase; Microbiol [Cagliari, Italy]), and 0.05% Tween 80 (Sigma-Aldrich, St. Louis, MO) at 37 °C. Mycobacterial cultures were harvested at late log phase, glycerol was added at 20% final concentration, and 1-ml aliquots were stored at –80 °C. Genomic DNA was extracted from liquid cultures by using the CTAB method, as previously described69.
Phylogenetic analysis of MTBC strains
The genomic DNA of each MTBC clinical strain was genotyped by spoligotyping70. For each experimental session, genomes of Mtb H37Rv and M. bovis BCG were used as positive controls and water as negative control.
Macrophage culture
Peripheral blood mononuclear cells (PBMCs) were obtained from healthy donors. PBMCs were isolated by density-gradient centrifugation. Monocytes were purified from PBMCs by positive sorting, using anti-CD14-conjugated magnetic microbeads (Miltenyi Biotec, Auburn, CA). After the selection, the level of purification was verified by flow cytometry (FACS Canto II flow cytometer; Becton Dickinson, Milan, Italy): 99% of CD14 + monocytes and 1% of CD3 + T cells. Macrophage-derived monocytes (MDM) were obtained by cultivating adherent monocytes for 5–6 days in X-Vivo 15 medium (Lonza, Walkersville, MD) and 2% human serum (Euroclone, Paignton, UK) at 37 °C in a 5% humidified atmosphere until macrophage differentiation.
Depending on the experimental requirements, different amount of cells were used. In detail, for the western blot experiments, the cells were seeded in six-well flat-bottom tissue culture plates (3 × 106 cells/well, 2 ml/well; Corning, New York, NJ). For the confocal experiments, cells were seeded in glass slide chambers (Nunc, Lab-Tek, Waltham, Massachusetts, USA) (5 × 105 cells/well, 2 ml/well). For the colony-forming unit (CFU) experiment, cells were seeded in 24-well flat-bottom tissue culture plates (5 × 105 cells/well, 1 ml/well; Corning, New York, NJ). For electron microscopy, cells were seeded in 60-mm tissue culture plates (5.5 × 106 cells; Corning, New York, NJ).
Autophagy was evaluated both 5 and 24 h after infection. To assess the autophagy flux, the lysosomal inhibitors E64d/pepstatin A (5 µg/ml; Sigma-Aldrich, St. Louis, MO), were added 4 h before lysis. Wortmannin (20 nM Sigma-Aldrich, St. Louis, MO) was added 5 h before lysis. To inhibit IL-1b activity, soluble antagonist for IL-1 receptor (IL-1-RA) at 1 µg/ml (R&D, Minneapolis, MN) was added to the macrophage cultures before infection. IL-1-RA was added again after the infection, concomitantly to the medium change; the uninfected cells followed the same treatment71.
To evaluate the viability of the MTBC-infected macrophages, the LDH Cytotoxicity Assay Kit (Thermo Fisher, Waltham, MA, USA) was used. The LDH Cytotoxicity Assay Kit is a reliable colorimetric assay to quantitatively measure lactate dehydrogenase (LDH) released into the media from damaged cells as a biomarker for cellular cytotoxicity and cytolysis.
MTBC infection of macrophages and colony-forming unit assay
Macrophages were infected with different MTBC strains (HR7Rv, EAI1_SOM, EAI2_MANILLA, AFRI, H3, and T1) at a multiplicity of infection (MOI) of 1:1 for western blot analysis and CFU and at a MOI of 2:1 for confocal experiments and electron microscopy. Two hours after the in vitro infection, macrophages were washed once with phosphate-buffered saline (PBS) and then fresh medium was added.
To determine the intracellular bacterial load, CFUs of infected macrophages were measured in triplicate and determined at 4 h and 7 day post infection55. Briefly, infected cell cultures were lysed in PBS 0.1%, Triton X (Sigma-Aldrich, St. Louis, MO), and the serial dilution was prepared in PBS 0.05% Tween 80 (Sigma-Aldrich, St. Louis, MO). Fifty-microliter aliquots of each dilution were plated on 7H11/OADC (Difco BD, NY) agar plates. The plates were incubated for 3 weeks.
Western blot assays
Cells were collected 5 and 24 h post infection and lysed in CelLytic buffer (Sigma-Aldrich, St. Louis, MO) plus the following protease and phosphatase inhibitors: protease inhibitor cocktail, 1 mM sodium fluoride, 1 mM sodium orthovanadate, and 1 mM sodium molybdate; 1 mM phenylmethylsulfonyl fluoride (Sigma-Aldrich, St. Louis, MO). Proteins were resolved on 12% NuPAGE Bis-Tris gel (Life Technologies, Carlsbad, CA) and electroblotted onto PVDF membranes (Millipore, Billerica, MA). Blots were incubated with primary antibodies in 5% nonfat dry milk in PBS plus 0.1% Tween-20 (Sigma-Aldrich, St. Louis, MO) overnight at 4 °C. Proteins were detected using horseradish peroxidase-conjugated secondary antibody (Jackson Laboratory, Bar Harbor, ME) and visualized with ECL plus (GE Healthcare, Little Chalfont, UK).
The primary antibodies used in this study were rabbit anti-LC3 (Cell Signaling, Danvers, MA) (1:2000), mouse anti-p62 (Santa Cruz Biotech, Santa Cruz, CA) (1:1000), and goat anti-GAPDH (Santa Cruz Biotech, Santa Cruz, CA) (1:50,000).
Confocal microscopy
Twenty-four hours after infection, cells were fixed with 4% paraformaldehyde (Sigma-Aldrich, St. Louis, MO) in PBS followed by permeabilization with 0.2% Triton X-100 (Sigma-Aldrich, St. Louis, MO) in PBS. Mycobacteria were stained with auramine for 20 min and destained for 10 min (TB Fluorescent Stain Kit BD, Sparks, MD). Cells were then labeled with the primary antibody anti-LC3 (L7543, Sigma-Aldrich, St. Louis, MO), anti-LAMP1 (Ab-24170, Abcam, Cambridge, UK) and anti-Rab5a (S-19, Santa Cruz Biotech, Santa Cruz, CA), anti-NDP52 (Ab-184688, Abcam, Cambridge, UK), anti-CD63 (MX-49.129.5, Santa Cruz Biotech, CA), anti-NBR1 (NBP1-71703, Novus Biological, Littleton, Colorado, CA), and anti-ubiquitin (FK2) (ST1200, Millipore, Billerica, MA) for 1 h at room temperature and visualized by means of Cy3-conjugated secondary antibodies (Jackson Immunoresearch). Coverslips were mounted in Prolong Gold antifade (Life Technologies, Carlsbad, CA) and examined under a confocal microscope (Leica TCS SP2, Wetzlar, Germany). Digital images were acquired with the Leica software and the image adjustments and merging were performed by using the appropriated tools of ImageJ software. Quantification of colocalization, expressed in terms of Mander’s coefficient, was calculated using the JacoP plugin of ImageJ software. A minimum of 50 cells per sample experimental condition were counted for triplicate samples per condition in each experiment.
Cytokine detection
Supernatants from MTBC-infected macrophage cultures were collected at different time points after in vitro infection and cytokines were evaluated by a cytometric bead array (BD Biosciences, San Jose, CA).
Electron microscopy
Twenty-four hours after infection, cells were fixed on ice with 2.5% glutaraldehyde in 0.1 M cacodylate buffer, pH 7.4, for 120 min and postfixed with 1% osmium tetraoxide for 120 min at 4 °C. After an extensive washing with cacodylate buffer at 0.1 M, pH 7.4, cells were dehydrated in graded concentrations of ethanol (30, 50, 70, 90, and 100%) and finally embedded in Spurr resin (TAAB). Ultrathin sections (60 nm) were subsequently cut with a PT-PC PowerTome ultramicrotome (RMC Boeckeler). Sections, collected on copper grids, were stained with saturated aqueous uranyl acetate and counterstained with 4% lead citrate, and then observed with HT-7700 TEM (Hitachi, Tokyo, Japan).
Statistical analysis
Data were analyzed by the GraphPad Prism software, version 4.00 for Windows (GraphPad Software, San Diego, CA). For all the experiments shown, with the exception of the cytokine results, the data were evaluated by analyzing the mean and standard deviation. The statistical significance of the differences between two groups was determined using the Student’s t-test. For the cytokine results, data are analyzed evaluating the median and P-values were calculated using the Mann–Whitney test. Differences were considered significant if P-values were ≤0.05.
Electronic supplementary material
Acknowledgements
This work was supported in part by grants from the Italian Ministry of University and Research (PRIN 20152CB22L), from the Italian Ministry of Health “Ricerca Corrente” and “Ricerca Finalizzata” (GR-2011-02350886; RF-2011-02348713; RF-2011-02349394), from the European Union (HEALTH-F3-2009-241642, contract no. HEALTH.F3.2009 241745, and EC FP7 NEWTBVAC), and from “Accordo Programma Quadro––Ricerca Regione Puglia” Future in Research VPSBGE1.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
These authors contributed equally: Alessandra Romagnoli, Elisa Petruccioli.
Edited by B. Zhivitovsky
Electronic supplementary material
Supplementary Information accompanies this paper at 10.1038/s41419-018-0640-8.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Giovanni Delogu, Email: giovanni.delogu@unicatt.it.
Delia Goletti, Email: delia.goletti@inmi.it.
Gian Maria Fimia, Email: gianmaria.fimia@inmi.it.
References
- 1.Brosch R, et al. A new evolutionary scenario for the Mycobacterium tuberculosis complex. Proc. Natl Acad. Sci. USA. 2002;99:3684–3689. doi: 10.1073/pnas.052548299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wirth T, et al. Origin, spread and demography of the Mycobacterium tuberculosis complex. PLoS Pathog. 2008;4:e1000160. doi: 10.1371/journal.ppat.1000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hershberg R, et al. High functional diversity in Mycobacterium tuberculosis driven by genetic drift and human demography. PLoS Biol. 2008;6:e311. doi: 10.1371/journal.pbio.0060311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brites D, Gagneux S. Co-evolution of Mycobacterium tuberculosis and Homo sapiens. Immunol. Rev. 2015;264:6–24. doi: 10.1111/imr.12264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coscolla M, Gagneux S. Consequences of genomic diversity in Mycobacterium tuberculosis. Semin. Immunol. 2014;26:431–444. doi: 10.1016/j.smim.2014.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Homolka S, Niemann S, Russell DG, Rohde KH. Functional genetic diversity among Mycobacterium tuberculosis complex clinical isolates: delineation of conserved core and lineage-specific transcriptomes during intracellular survival. PLoS Pathog. 2010;6:e1000988. doi: 10.1371/journal.ppat.1000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sarkar R, Lenders L, Wilkinson KA, Wilkinson RJ, Nicol MP. Modern lineages of Mycobacterium tuberculosis exhibit lineage-specific patterns of growth and cytokine induction in human monocyte-derived macrophages. PLoS ONE. 2012;7:e43170. doi: 10.1371/journal.pone.0043170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Portevin D, Gagneux S, Comas I, Young D. Human macrophage responses to clinical isolates from the Mycobacterium tuberculosis complex discriminate between ancient and modern lineages. PLoS Pathog. 2011;7:e1001307. doi: 10.1371/journal.ppat.1001307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krishnan N, et al. Mycobacterium tuberculosis lineage influences innate immune response and virulence and is associated with distinct cell envelope lipid profiles. PLoS ONE. 2011;6:e23870. doi: 10.1371/journal.pone.0023870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reiling, N. et al. Clade-specific virulence patterns of Mycobacterium tuberculosis complex strains in human primary macrophages and aerogenically infected mice. MBio4, 10.1128/mBio.00250-13 (2013). [DOI] [PMC free article] [PubMed]
- 11.Gagneux S. Host-pathogen coevolution in human tuberculosis. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2012;367:850–859. doi: 10.1098/rstb.2011.0316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gagneux S. Ecology and evolution of Mycobacterium tuberculosis. Nat. Rev. Microbiol. 2018;16:202–213. doi: 10.1038/nrmicro.2018.8. [DOI] [PubMed] [Google Scholar]
- 13.Lyadova IV, Panteleev AV. Th1 and Th17 cells in tuberculosis: protection, pathology, and biomarkers. Mediat. Inflamm. 2015;2015:854507. doi: 10.1155/2015/854507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prezzemolo T, et al. Functional signatures of human CD4 and CD8 T cell responses to Mycobacterium tuberculosis. Front. Immunol. 2014;5:180. doi: 10.3389/fimmu.2014.00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ottenhoff TH. New pathways of protective and pathological host defense to mycobacteria. Trends Microbiol. 2012;20:419–428. doi: 10.1016/j.tim.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Flynn JL, Chan J, Lin PL. Macrophages and control of granulomatous inflammation in tuberculosis. Mucosal Immunol. 2011;4:271–278. doi: 10.1038/mi.2011.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boom WH, et al. Human immunity to M. tuberculosis: T cell subsets and antigen processing. Tuberculosis. 2003;83:98–106. doi: 10.1016/S1472-9792(02)00054-9. [DOI] [PubMed] [Google Scholar]
- 18.Kaufmann SH. Tuberculosis: Back on the immunologists’ agenda. Immunity. 2006;24:351–357. doi: 10.1016/j.immuni.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 19.Fletcher HA, et al. T-cell activation is an immune correlate of risk in BCG vaccinated infants. Nat. Commun. 2016;7:11290. doi: 10.1038/ncomms11290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petruccioli E, et al. Correlates of tuberculosis risk: predictive biomarkers for progression to active tuberculosis. Eur. Respir. J. 2016;48:1751–1763. doi: 10.1183/13993003.01012-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flynn JL, Chan J. Immune evasion by Mycobacterium tuberculosis: living with the enemy. Curr. Opin. Immunol. 2003;15:450–455. doi: 10.1016/S0952-7915(03)00075-X. [DOI] [PubMed] [Google Scholar]
- 22.Rohde K, Yates RM, Purdy GE, Russell DG. Mycobacterium tuberculosis and the environment within the phagosome. Immunol. Rev. 2007;219:37–54. doi: 10.1111/j.1600-065X.2007.00547.x. [DOI] [PubMed] [Google Scholar]
- 23.Sahiratmadja E, et al. Dynamic changes in pro- and anti-inflammatory cytokine profiles and gamma interferon receptor signaling integrity correlate with tuberculosis disease activity and response to curative treatment. Infect. Immun. 2007;75:820–829. doi: 10.1128/IAI.00602-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gutierrez MG, et al. Autophagy is a defense mechanism inhibiting BCG and Mycobacterium tuberculosis survival in infected macrophages. Cell. 2004;119:753–766. doi: 10.1016/j.cell.2004.11.038. [DOI] [PubMed] [Google Scholar]
- 25.Goletti D, Petruccioli E, Romagnoli A, Piacentini M, Fimia GM. Autophagy in Mycobacterium tuberculosis infection: a passepartout to flush the intruder out? Cytokine Growth Factor Rev. 2013;24:335–343. doi: 10.1016/j.cytogfr.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Deretic V, Saitoh T, Akira S. Autophagy in infection, inflammation and immunity. Nat. Rev. Immunol. 2013;13:722–737. doi: 10.1038/nri3532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mizushima N, Komatsu M. Autophagy: renovation of cells and tissues. Cell. 2011;147:728–741. doi: 10.1016/j.cell.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 28.Antonioli M, Di Rienzo M, Piacentini M, Fimia GM. Emerging mechanisms in initiating and terminating autophagy. Trends Biochem. Sci. 2017;42:28–41. doi: 10.1016/j.tibs.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 29.Mizushima N, Yoshimori T, Ohsumi Y. The role of Atg proteins in autophagosome formation. Annu. Rev. Cell. Dev. Biol. 2011;27:107–132. doi: 10.1146/annurev-cellbio-092910-154005. [DOI] [PubMed] [Google Scholar]
- 30.Rogov V, Dotsch V, Johansen T, Kirkin V. Interactions between autophagy receptors and ubiquitin-like proteins form the molecular basis for selective autophagy. Mol. Cell. 2014;53:167–178. doi: 10.1016/j.molcel.2013.12.014. [DOI] [PubMed] [Google Scholar]
- 31.Kuballa P, Nolte WM, Castoreno AB, Xavier RJ. Autophagy and the immune system. Annu. Rev. Immunol. 2012;30:611–646. doi: 10.1146/annurev-immunol-020711-074948. [DOI] [PubMed] [Google Scholar]
- 32.Shibutani ST, Saitoh T, Nowag H, Munz C, Yoshimori T. Autophagy and autophagy-related proteins in the immune system. Nat. Immunol. 2015;16:1014–1024. doi: 10.1038/ni.3273. [DOI] [PubMed] [Google Scholar]
- 33.Deretic V. Autophagy as an innate immunity paradigm: expanding the scope and repertoire of pattern recognition receptors. Curr. Opin. Immunol. 2012;24:21–31. doi: 10.1016/j.coi.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harris J. Autophagy and cytokines. Cytokine. 2011;56:140–144. doi: 10.1016/j.cyto.2011.08.022. [DOI] [PubMed] [Google Scholar]
- 35.Harris J, et al. T helper 2 cytokines inhibit autophagic control of intracellular Mycobacterium tuberculosis. Immunity. 2007;27:505–517. doi: 10.1016/j.immuni.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 36.Deretic V, et al. Immunologic manifestations of autophagy. J. Clin. Invest. 2015;125:75–84. doi: 10.1172/JCI73945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stanley SA, Cox JS. Host-pathogen interactions during Mycobacterium tuberculosis infections. Curr. Top. Microbiol. Immunol. 2013;374:211–241. doi: 10.1007/82_2013_332. [DOI] [PubMed] [Google Scholar]
- 38.Watson RO, et al. The cytosolic sensor cGAS detects Mycobacterium tuberculosis DNA to induce type I interferons and activate autophagy. Cell. Host. Microbe. 2015;17:811–819. doi: 10.1016/j.chom.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Watson RO, Manzanillo PS, Cox JS. Extracellular M. tuberculosis DNA targets bacteria for autophagy by activating the host DNA-sensing pathway. Cell. 2012;150:803–815. doi: 10.1016/j.cell.2012.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Romagnoli A, et al. ESX-1 dependent impairment of autophagic flux by Mycobacterium tuberculosis in human dendritic cells. Autophagy. 2012;8:1357–1370. doi: 10.4161/auto.20881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Petruccioli E, et al. Specific T cells restore the autophagic flux inhibited by Mycobacterium tuberculosis in human primary macrophages. J. Infect. Dis. 2012;205:1425–1435. doi: 10.1093/infdis/jis226. [DOI] [PubMed] [Google Scholar]
- 42.Kimmey JM, et al. Unique role for ATG5 in neutrophil-mediated immunopathology during M. tuberculosis infection. Nature. 2015;528:565–569. doi: 10.1038/nature16451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Jong BC, Antonio M, Gagneux S. Mycobacterium africanum–review of an important cause of human tuberculosis in WestAfrica. PLoS Negl. Trop. Dis. 2010;4:e744. doi: 10.1371/journal.pntd.0000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Collins FM. Tuberculosis research in a cold climate. Tuber. Lung Dis. 1997;78:99–107. doi: 10.1016/S0962-8479(98)80002-6. [DOI] [PubMed] [Google Scholar]
- 45.Franco LH, et al. The ubiquitin ligase Smurf1 functions in selective autophagy of Mycobacterium tuberculosis and anti-tuberculous host defense. Cell Host Microbe. 2017;21:59–72. doi: 10.1016/j.chom.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jamwal SV, et al. Mycobacterial escape from macrophage phagosomes to the cytoplasm represents an alternate adaptation mechanism. Sci. Rep. 2016;6:23089. doi: 10.1038/srep23089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pilli M, et al. TBK-1 promotes autophagy-mediated antimicrobial defense by controlling autophagosome maturation. Immunity. 2012;37:223–234. doi: 10.1016/j.immuni.2012.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ribeiro SC, et al. Mycobacterium tuberculosis strains of the modern sublineage of the Beijing family are more likely to display increased virulence than strains of the ancient sublineage. J. Clin. Microbiol. 2014;52:2615–2624. doi: 10.1128/JCM.00498-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Theus SA, et al. Differences in the growth of paired Ugandan isolates of Mycobacterium tuberculosis within human mononuclear phagocytes correlate with epidemiological evidence of strain virulence. Infect. Immun. 2006;74:6865–6876. doi: 10.1128/IAI.00561-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Etna MP, Giacomini E, Severa M, Coccia EM. Pro- and anti-inflammatory cytokines in tuberculosis: a two-edged sword in TB pathogenesis. Semin. Immunol. 2014;26:543–551. doi: 10.1016/j.smim.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 51.Tientcheu LD, et al. Immunological consequences of strain variation within the Mycobacterium tuberculosis complex. Eur. J. Immunol. 2017;47:432–445. doi: 10.1002/eji.201646562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mortaz E, et al. Interaction of pattern recognition receptors with Mycobacterium Tuberculosis. J. Clin. Immunol. 2015;35:1–10. doi: 10.1007/s10875-014-0103-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mishra A, Akhtar S, Jagannath C, Khan A. Pattern recognition receptors and coordinated cellular pathways involved in tuberculosis immunopathogenesis: Emerging concepts and perspectives. Mol. Immunol. 2017;87:240–248. doi: 10.1016/j.molimm.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 54.Reed MB, et al. A glycolipid of hypervirulent tuberculosis strains that inhibits the innate immune response. Nature. 2004;431:84–87. doi: 10.1038/nature02837. [DOI] [PubMed] [Google Scholar]
- 55.Palucci I, et al. PE_PGRS33 contributes to Mycobacterium tuberculosis entry in macrophages through interaction with TLR2. PLoS ONE. 2016;11:e0150800. doi: 10.1371/journal.pone.0150800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Manca C, et al. Mycobacterium tuberculosis CDC1551 induces a more vigorous host response in vivo and in vitro, but is not more virulent than other clinical isolates. J. Immunol. 1999;162:6740–6746. [PubMed] [Google Scholar]
- 57.Wassermann R, et al. Mycobacterium tuberculosis differentially activates cGAS- and inflammasome-dependent intracellular immune responses through ESX-1. Cell Host Microbe. 2015;17:799–810. doi: 10.1016/j.chom.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 58.Simeone R, Bottai D, Frigui W, Majlessi L, Brosch R. ESX/type VII secretion systems of mycobacteria: Insights into evolution, pathogenicity and protection. Tuberculosis. 2015;95(Suppl 1):S150–S154. doi: 10.1016/j.tube.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 59.Wiens KE, Ernst JD. The mechanism for type I interferon induction by Mycobacterium tuberculosis is bacterial strain-dependent. PLoS. Pathog. 2016;12:e1005809. doi: 10.1371/journal.ppat.1005809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Martin CJ, et al. Efferocytosis is an innate antibacterial mechanism. Cell Host Microbe. 2012;12:289–300. doi: 10.1016/j.chom.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jayaraman P, et al. IL-1beta promotes antimicrobial immunity in macrophages by regulating TNFR signaling and caspase-3 activation. J. Immunol. 2013;190:4196–4204. doi: 10.4049/jimmunol.1202688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zumla A, et al. Towards host-directed therapies for tuberculosis. Nat. Rev. Drug. Discov. 2015;14:511–512. doi: 10.1038/nrd4696. [DOI] [PubMed] [Google Scholar]
- 63.Kaufmann SHE, Dorhoi A, Hotchkiss RS, Bartenschlager R. Host-directed therapies for bacterial and viral infections. Nat. Rev. Drug. Discov. 2018;17:35–56. doi: 10.1038/nrd.2017.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Palucci I, et al. Transglutaminase type 2 plays a key role in the pathogenesis of Mycobacterium tuberculosis infection. J. Intern. Med. 2018;283:303–313. doi: 10.1111/joim.12714. [DOI] [PubMed] [Google Scholar]
- 65.Bradfute SB, et al. Autophagy as an immune effector against tuberculosis. Curr. Opin. Microbiol. 2013;16:355–365. doi: 10.1016/j.mib.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.O’Neill LA, Pearce EJ. Immunometabolism governs dendritic cell and macrophage function. J. Exp. Med. 2016;213:15–23. doi: 10.1084/jem.20151570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Castillo EF, et al. Autophagy protects against active tuberculosis by suppressing bacterial burden and inflammation. Proc. Natl Acad. Sci. USA. 2012;109:E3168–E3176. doi: 10.1073/pnas.1210500109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chandra P, et al. Mycobacterium tuberculosis inhibits RAB7 recruitment to selectively modulate autophagy flux in macrophages. Sci. Rep. 2015;5:16320. doi: 10.1038/srep16320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.van Embden JD, et al. Strain identification of Mycobacterium tuberculosis by DNA fingerprinting: recommendations for a standardized methodology. J. Clin. Microbiol. 1993;31:406–409. doi: 10.1128/jcm.31.2.406-409.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kamerbeek J, et al. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J. Clin. Microbiol. 1997;35:907–914. doi: 10.1128/jcm.35.4.907-914.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Goletti D, Kinter AL, Hardy EC, Poli G, Fauci AS. Modulation of endogenous IL-1 beta and IL-1 receptor antagonist results in opposing effects on HIV expression in chronically infected monocytic cells. J. Immunol. 1996;156:3501–3508. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.