Abstract
Background
The mental health treatment gap for youth in low- and middle-income countries (LMICs) is substantial; strategies for redress are urgently needed to mitigate the serious health and social consequences of untreated mental illness in youth.
Aims
To estimate the burden of major depressive episode (MDE) and posttraumatic stress disorder (PTSD) as well as utilization of care among Haitian youth in order to describe the mental health treatment gap in a LMIC setting.
Methods
We estimated the point prevalence of MDE, PTSD, and subthreshold variants in a school-based sample of youth (n=120, ages 18–22) using a modified SCID-based interview and examined treatment utilization among those receiving one of these diagnoses. We assessed additional psychopathology with self-report measures to examine validity of study diagnostic assignments.
Results
The combined prevalence of full-syndrome or subthreshold MDE or PTSD was high (36.7%). A large majority of affected individuals (88.6%) had accessed no mental health services in the health sector and 36.4% had accessed no care of any kind in either the health or folk sectors in the past year.
Conclusions
Findings demonstrate a high mental health burden among Haiti’s youth and that many youth with MDE and PTSD are not accessing mental health care.
Keywords: mental health treatment gap, low-income countries, youth, mental health burden, Haiti
Introduction
Mental and substance use disorders remain the leading health contributors to disability both globally and in low- and middle-income countries (LMICs) (IHME, 2016) but the majority of affected individuals in LMICs do not receive care for serious mental illness (Demyttenaere et al., 2004). For example, only one in 27 individuals with major depression in a LMIC receives minimally adequate treatment (Thornicroft et al., 2016). Although reasons underpinning the mental health treatment gap—the proportion of those with mental illness who do not receive care—are multi-factorial, developing and deploying strategies to expand access to quality mental health services are a focus for its redress (Becker & Kleinman, 2013). Strategies for improving care access across diverse regions and populations can be enhanced by understanding patterns of treatment utilization and particular barriers to care within demographics defined by age and local social context.
Mental disorders are also the greatest contributor to disability in youth worldwide (Gore et al., 2011), but the majority of affected youth do not receive care for their mental illness (Patton et al., 2012). Unfortunately, untreated mental disorders in youth carry the risk for serious downstream health and social consequences. For example, a longer duration of mental disorder in adolescence is among the strongest predictors of adult disorder (Patton et al., 2014). Moreover, adolescent mental illness is associated with poorer social and economic outcomes ten years later and greater risk for other non-communicable diseases (Ngo et al., 2013). Because early detection and treatment can reduce the chronicity and severity of the primary mental disorder and prevent secondary disorders (Ghio et al., 2014; McGorry et al., 2011; Patton et al., 2014), timely intervention for youth is critical for their future health and well-being. This treatment gap, moreover, is most pronounced in LMICs where an estimated 10–20% of adolescents have a mental disorder (Kieling et al., 2011; Patel et al., 2008). Barriers to care include health systems constraints relating to an inadequate mental health workforce and public sector budget allocation to meet needs, as well as a variety of factors that influence help-seeking for mental illness. For example, relevant cultural factors include local idioms of distress and explanatory models that render care-seeking in the health or folk sectors germane (e.g., Kleinman, 1980). Likewise, social structural factors, such as political and economic disenfranchisement, impede help-seeking (Farmer, 2010). Impacts of the latter—such as legal factors, unaffordable costs, and poor access to transportation—are more pronounced for youth (Patton et al., 2016). Understanding factors underpinning user demand and accessibility of services are salient to optimizing interventional approaches and targets to reduce the mental health treatment gap in LMICs.
The present study seeks to characterize the local mental health treatment gap among youth in Haiti, a low-income country in the Caribbean. In 2010, a major earthquake centered near Port-au-Prince resulted in devastating casualties, infrastructural damage, and displacement in Haiti. Given the elevated risk for depression and PTSD following humanitarian emergencies and disasters (Goldmann & Galea, 2014; Marquez, 2016) and the likely impacts of this “acute-on-chronic” event (Farmer, 2011) on mental health in the setting of longstanding social adversities (WHO, 2010; Raviola et al., 2012), we expected depression and PTSD to be prevalent among youth in Haiti’s Central Plateau. Further, although rigorous epidemiologic data on mental disorders in Haiti are quite limited (cf. WHO, 2010), post-earthquake data from self-report or inventory assessments support a high burden of depression and posttraumatic stress disorder among youth (Blanc et al., 2014; Cénat & Derivois, 2014, 2015) and adults (Cerda et al., 2013) living in Port-au-Prince as well as prevalent depressive symptoms among adults in Haiti’s Central Plateau (Wagenaar et al., 2012). Similar to the situation in other LMICs, accessibility to mental health services in Haiti has been severely constrained by resource shortfalls of all types and centralization of services in urban areas (WHO, 2010; WHO, 2011). Significant stigma towards mental illness also exists in Haiti, and there is little exposure to and endorsement of biomedical explanations of mental illness (Khoury et al., 2012; Wagenaar et al., 2013). Nonetheless, there is inadequate understanding about help-seeking for mental illness among Haitian youth to inform development of community-based mental health care in Central Haiti to serve them (Raviola et al., 2012).
The present study’s aims are to 1) estimate the point prevalence of depression and PTSD among a community-based sample of secondary school youth in the Central Plateau of Haiti; 2) estimate 12-month utilization of health-system based care for mental health; and 3) describe the unmet need for mental health treatment in this sample. An empirical understanding of local mental health burden and associated unmet need can strategically inform further development of approaches for promoting the mental health of Haitian youth, and also has potential application for understanding and closing the mental health treatment gap for youth in other low-income settings.
Methods
Cross-sectional study data were collected during the baseline assessment phase of the Teacher-Accompagnateur Pilot Study (TAPS), a school-based pilot mental health intervention in Haiti’s Central Plateau in October and November 2013 (Eustache et al., 2014; Eustache et al,. 2017b). The corresponding study protocols—including components presented here—were approved by both the Institutional Review Board (IRB) of the Harvard Faculty of Medicine and the Zanmi Lasante (ZL) Ethics Committee. Methods described here represent those most relevant to the present study’s aims (see Eustache et al, 2017a for additional details about study procedures).
Study Sample
The study sample was drawn from four participating schools in Haiti’s Central Plateau. Students meeting eligibility criteria (actively enrolled in a participating school, ages 18 to 22 years) were randomly selected within each school from school registers (n=33 to 41 per school). Across all schools, 145 eligible students were invited to participate and of these, 121 students were enrolled in the study and completed the assessment. Subsequently, one participant withdrew consent and requested that his/her study data be discarded, yielding a revised study sample of n=120. The response rate was 82.8% in total, and at least 78.0% in each school. Study participants received lunch but there was no monetary compensation for participation.
Procedures
After providing informed consent, participants responded to a battery of self-report psychosocial assessments and subsequently underwent a structured research interview. Assessments were in Haitian Creole at the students’ respective schools. The self-report assessments were proctored by members of the study team and completed during a single day. Research interviews were conducted by (or co-facilitated with) clinician-investigators with local experience in diagnostic assessment of mental disorders. 85.8% of the interviews were completed within two days of the student’s self-report assessment, and all interviews were completed within 15 days of the self-report assessment. Following the research interview and independently of the study, study participants were encouraged to undergo an onsite clinical interview with a mental health clinician to follow up on clinical concerns or questions and facilitate a path to care, if appropriate.
Assessments
With the exception of questions about healthcare utilization developed for this study, study psychosocial assessments were drawn from or adapted for use from existing measures (Table 1). Written self-report assessments were translated from English to Haitian Creole using an iterative process involving contributions by three or more members of the study team as follows (cf. Bhui et al., 2003): forward translation and independent back translation by two or more bilingual members of the study team, comparison for discrepancies by one or more native English-speaking investigators, and adjustments by one or more investigators to optimize idiomatic and readily comprehensible usage. Assessments were finalized after a piloting them with an independently selected sample of Haitian students (n=12).
Table 1.
Measures used for assessment
| Construct | Source measure and method of assessment | Description of measure, study-specific usage or adaptation, and psychometric properties |
|---|---|---|
| Sociodemographic characteristics |
Unstandardized measure/questions used in previous research in Haiti (Smith Fawzi et al., 2003, 2012) Self-report |
|
|
| ||
| Health care utilization, barriers to care |
None; item content developed for this study Self-report |
|
|
| ||
| Depressive symptoms |
Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, 1977) Self-report |
|
|
| ||
| Signs of mental distress and/or associated impairment |
Global School-based Health Survey (GSHS) (World Health Organization, 2013a, 2013b) Self-report |
|
|
| ||
| Stressful life events/traumatic exposures |
Stressful Life Events (SLE) Checklist (Bean et al., 2004b) Self-report |
|
|
| ||
| Post-traumatic Stress Disorder symptoms |
Reaction of Adolescents to Traumatic Stress (RATS) (Bean et al., 2004a, 2006) Self-report |
|
|
| ||
| Major Depressive Episode (MDE), Post-traumatic Stress Disorder (PTSD), subthreshold MDE, subthreshold PTSD |
Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID) (First et al., 2010) Structured interview |
|
Data Analyses
All statistical analyses were conducted in SPSS 23 (IBM Corp, 2015). Descriptive statistics were calculated as frequencies for categorical data and means with standard deviations for continuous variables. For all diagnostic categories corresponding 95% confidence intervals were calculated using the Wald method except when n≤5, in which case the exact method was used. Chi-square tests were used to test for differences in prevalence by gender. In order to examine construct convergent validity of the DSM-based study diagnostic assignments, we used self-report data from the following assessments (as adapted for this study; Table 1): Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977), Global School-based Health Survey (GSHS; WHO, 2013a, 2013b), Reaction of Adolescents to Traumatic Stress (RATS; Bean et al., 2004b), and Stressful Life Events Checklist (SLE; Bean et al., 2004a).
Data management
Raw self-report data were entered into an Excel file and verified. Missing data for the CES-D and RATS were handled as follows. We used mean imputation for observations missing 10% or fewer of responses and excluded observations missing greater than 10% of responses (n=9 and n=5, respectively for CES-D and RATS). Complete data were available for healthcare utilization analyses. All other deviations from the sample size of n=120 for individual items are noted in tables and text.
Interviews were completed by each respondent. Written ratings data recorded on the paper copies of the interview guides were entered into an Excel spreadsheet for analysis. In addition, we transcribed and translated all narrative responses as well as summary and margin notes recorded on the interview guides; these were also entered into a spreadsheet for review alongside numeric ratings. Our algorithm for diagnostic assignment handled missing data from the research interview as described below.
Procedures for study diagnostic assignment
We used data from interviews based on content adapted and abridged from the MDE and PTSD modules of the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID; First et al., 2010) to make study diagnostic assignments. The interviewer’s summary assessment was the primary basis for a diagnostic assignment as MDE or PTSD. Members of the study team also considered all written information recorded on the interview form about symptoms, presentation, and context—including any narrative data, margin notes, and summary ratings data—to reach consensus about diagnostic assignments. In addition to the standard SCID diagnostic summary rating questions in the respective MDE and PTSD modules, we added a second study-specific item asking the interviewer to affirm whether the diagnosis was present. This item allowed additional response options (e.g., to indicate that only partial criteria were met or a diagnosis could not be ascertained). The interviewer’s summary assessment of the presence of a disorder in response to at least one of these items was required for a study diagnostic assignment as MDE or PTSD. In addition, we reviewed and considered interview margin and summary notes for contradictory or qualifying information.
Next we systematically reviewed all of these interview data—including written summary ratings, narrative responses, and margin notes recorded on the paper copies of the SCID-based interview guides—for evidence of subthreshold MDE or PTSD. We followed study operational criteria (described below and in Table 2) and reached consensus among three or more study investigators regarding presence of each these subthreshold diagnoses for each participant.
Table 2.
Study criteria for diagnostic assignment of subthreshold MDE and subthreshold PTSD among participants not meeting full-syndrome criteria
| Conservative | Broad | |
|---|---|---|
| Subthreshold MDE |
|
|
| Subthreshold PTSD |
|
|
Present refers to a rating of 3 on signs, symptoms, or criteria assessed during the SCID-based research interview, consistent with scoring on the SCID (First et al., 2010); likewise “subthreshold” refers to a rating of 2 on these criteria.
Criteria referenced in the table refer to the DSM-IV-TR criteria rated in the SCID for MDE and PTSD, respectively (American Psychiatric Association, 2000; First et al., 2010).
Diagnostic assignments of subthreshold MDE
When participants did not meet study criteria for MDE, we assigned a study diagnosis of subthreshold MDE to participants who nonetheless met either of the two sets of corresponding study criteria (Table 2). These criteria are based on guidance in SCID instructions that subthreshold diagnosis can be assigned when an individual is deemed likely to meet full criteria (First et al., 2002). We operationalized our ‘conservative’ criteria to assign a subthreshold diagnosis of MDE when Criteria A, B, and C were met, except for the presence of only 4 of the 5 required neurovegetative symptoms. In addition, we assigned a study diagnosis of subthreshold MDE when clinicians had given a rating of at least subthreshold for signs and symptoms of Criteria A-C that would have, if all present, been consistent with full syndrome MDE (cf. Schnurr et al., 1993).
Diagnostic assignments of subthreshold PTSD
When participants did not meet study criteria for PTSD, we assigned a study diagnosis of subthreshold PTSD to participants who nonetheless met either of the two sets of corresponding study criteria (Table 2). Criteria sets were based on practices described in the literature. The first, which we termed “Subthreshold PTSD (Conservative)”, was based on the approach described by Blanchard et al., (1994). We selected this approach given its established use (see Franklin et al., 2002; Brancu et al., 2016) and that it is conservative in requiring two full symptom clusters to be met (Cukor et al., 2010). The second, which we termed “Subthreshold PTSD (Broad)”, is based on the approach described by Schnurr and colleagues (1993). This method allows for a subthreshold diagnosis to be assigned when signs and symptoms otherwise adequate to meet diagnostic criteria are present but do not reach threshold levels.
Validation of study diagnostic assignments
To assess the validity of study diagnostic assignments, we exmined convergent validity by examining between group differences (case vs. non-case) with respect to measures of depressed mood and trauma exposure generated by self-report assessments. First, internal consistency reliability for the CES-D and RATS was estimated with Cronbach’s alpha. Wilcoxon-Mann-Whitney tests were used to compare 1) MDE cases versus non-cases and 2) MDE cases and/or subthreshold variants versus non-cases on CES-D- and GSHS-based measures of depressive symptomatology. A parallel set of Wilcoxon-Mann-Whitney tests were used to compare 1) PTSD cases versus PTSD non-cases and 2) PTSD cases and/or subthreshold variants versus non-cases on SLE and RATS measures of trauma exposure and PTSD-related symptomatology.
Assessment of the gap between identified mental health needs and care utilization
We used self-report responses concerning healthcare utilization to calculate the proportion of participants within each of these study diagnostic categories who had not accessed healthcare for any mental health problem in the past 12 months and who had also not accessed healthcare for any health problem during the same time period. We operationalized “unmet need” for mental health services as the former.
Results
Sociodemographic characteristics, healthcare utilization, and barriers to care
Table 3 displays a summary of socioeconomic characteristics and healthcare utilization among participants. The sample was two-thirds male with a mean age of 19.5 years. Socio-economic indicators consistent with poverty were notable for the prevalence of food insecurity and lack of indoor latrine as well as difficulty affording healthcare, medicines, or transportation to health services. For example, three-quarters of respondents reported having at least one day without any food over the preceding three months and one-quarter did not have a latrine in their home. Moreover, a majority of respondents (59.5%) reported difficulty paying for hospital or clinic-based care or difficulty paying for medicine (50.8%). Likewise, nearly a quarter of participants reported difficulty paying for medicine from a healer or houngan.
Table 3.
Student Sample Characteristics, n=120 unless otherwise indicated
| Measure | n (%), unless otherwise specified |
|---|---|
| Socio-demographic | |
| Age in years, mean (SD) | 19.5 (1.37) |
| Gender | |
| Male | 80 (66.7%) |
| Female | 40 (33.3%) |
| Days of school attended per week, on average, mean (SD), n=118 | 4.7 (1.34) |
| School | |
| Public | 60 (50.0%) |
| Private | 60 (50.0%) |
|
| |
| Household economic status indicators | |
| Latrine at home | 90 (75.0%) |
| Roofing on home, n=119 | |
| Aluminum | 77 (64.7%) |
| Thatched | 2 (1.7%) |
| Concrete | 30 (25.2%) |
| Other | 10 (8.4%) |
| Number of meals per day, on average, mean (SD), n=106 | 2.2 (.63) |
| Days without any food, in last three months, n=113 | |
| None | 28 (24.8%) |
| One | 22 (19.5%) |
| Two | 13 (11.5%) |
| Three | 7 (6.2%) |
| More than three | 43 (38.1%) |
|
| |
| Utilization and access to care | |
| Accessed care for any health problem | |
| Utilized general health care in past 12 months | 63 (52.5%) |
| Accessed care for a mental health problem | |
| Utilized mental health care in lifetime | 30 (25.0%) |
| Utilized mental health care in past 12 months | 15 (12.5%) |
| Accessed care from a healer or houngan for any health problem | |
| Utilized healer or houngan for general health care in past 12 months | 15 (12.5%) |
| Accessed care from a healer or houngan for a mental health problem | |
| Utilized healer or houngan for mental health care in lifetime | 21 (17.5%) |
| Utilized healer or houngan for mental health care in past 12 months | 9 (7.5%) |
| Reported difficulties with care access | |
| Have you ever had difficulty with transport to a health center or clinic?, n=117 | 51 (43.6%) |
| Do you ever have difficulty paying for your health care at a hospital or clinic?, n=116 | 69 (59.5%) |
| Do you ever have difficulty paying for medicine at a hospital, clinic, or pharmacy? | 61 (50.8%) |
| Do you ever have difficulty paying for your health care from a healer? | 32 (26.7%) |
| Do you ever have difficulty paying for medicine from a healer? | 29 (24.2%) |
Health services were only accessed by slightly over half the participants within the past year. During this timeframe, 55.0% of participants accessed either general or mental health care through the health system and an additional 4.2% accessed care only through the folk sector (i.e., by visiting healers or houngans); however, 40.8% of the sample did not access any of these kinds of care within the past 12 months (Table 4). Moreover, only 12.5% of participants had accessed mental health care through the health system and an additional 5.8% had addressed mental health problems with a healer or houngan. Thus, the majority of the participants (81.7%) had not accessed any specific mental health care in the past year.
Table 4.
One-month point prevalence estimates and 95% confidence intervals for MDE, PTSD, MDE and/or PTSD, and comorbid MDE and PTSD
| Overall, n=120 | Male, n=80 | Female, n=40 | p | |
|---|---|---|---|---|
| MDE case | 7.5% (3.7–13.1%), n=9 | 3.8% (.8–10.6%), n=3 | 15.0% (6.3–28.1%), n=6 | .059 |
| MDE case or subthreshold | 25.8% (18.6–34.1%), n=31 | 26.3% (17.5–36.5%), n=21 | 25.0% (13.4–39.7%), n=10 | .88 |
|
| ||||
| PTSD case | 10.8% (6.1%-17.2), n=13 | 10.0% (4.7–17.8%), n=8 | 12.5% (4.2–26.8%), n=5 | .76 |
| PTSD case or subthreshold | 20.8% (14.2–28.7%), n=25 | 21.3% (13.3–31.0%), n=17 | 20.0% (9.7–34.0%), n=8 | .87 |
|
| ||||
| MDE and/or PTSD case | 14.2% (8.7–21.1%), n=17 | 10.0% (4.7–17.8%), n=8 | 22.5% (11.5–36.9%), n=9 | .064 |
| MDE and/or PTSD case or subthreshold | 36.7% (28.4–45.5%), n=44 | 35.0% (25.1–45.8%), n=28 | 40.0% (25.8–55.5%), n=16 | .59 |
|
| ||||
| Comorbidity (MDE and PTSD case) | 4.2% (1.4–9.5%), n=5 | 3.8% (.8–10.6%), n=3 | 5.0% (.6–16.9%), n=2 | 1.00 |
| Comorbidity (MDE and PTSD case or subthreshold) | 10.0% (4.6–15.4%), n=12 | 12.5% (6.5–20.9%), n=10 | 5.0% (.6–16.9%), n=2 | .33 |
Note. Wald method used for 95% confidence intervals except when n ≤5, in which case exact method was used. Significance testing with chi-square, except any cells had expected count <5, in which case Fisher’s exact test was used.
Prevalence of MDE, PTSD, and subthreshold variants
Table 4 displays the one-month point prevalence estimates for MDE, PTSD, and their respective subthreshold variants. The prevalence of MDE was 7.5%; including participants with either MDE or MDE subthreshold variants increased the prevalence considerably to 25.8%. The prevalence of PTSD was 10.8%; the combined prevalence of PTSD and PTSD subthreshold variants was 20.8%. Overall, the one-month prevalence of either MDE or PTSD was 14.2% in our study sample; the prevalence of any one of the study diagnoses (MDE, PTSD, and/or a subthreshold variant) was high at 36.7%. We noted that 4.2% of the study participants had comorbid MDE and PTSD. Although we did not observe a gender difference for either PTSD or comorbid MDE and PTSD cases, we observed a marginally significant higher prevalence of MDE for females (15.0% females vs. 3.8% males; p=0.059).
Convergent Validity
Table 5 shows overall and group means for depressive symptomatology measured by the CES-D and GSHS questions across groups defined by diagnostic assignments relating to MDE. Also displayed are overall and group means for measures of stressful life events/traumatic exposures and PTSD-related symptomatology, across groups defined by diagnostic assignments relating to PTSD. MDE cases had significantly higher levels of depressive symptomatology than non-cases. Similarly, the group comprising MDE case and subthreshold variants also had significantly higher depressive symptomatology than all others. Parallel analysis for PTSD showed similar results: PTSD cases had significantly higher stressful life event/traumatic exposures and PTSD-related symptomatology than non-cases. The group comprising PTSD cases and subthreshold PTSD variants also had significantly higher stressful life event/traumatic exposures and PTSD-related symptomatology than all others.
Table 5.
Convergent validity of MDE and PTSD diagnostic assignments.
| MDE | Overall Mean (SD) (n=120, unless indicated) |
MDE Case, Mean (SD) (n=9) |
All others Mean (SD) (n=111, unless indicated) |
Wilcoxon- Mann- Whitney z, p |
MDE Case or Subthreshold, Mean (SD) (n=31, unless indicated) |
All others Mean (SD) (n=89, unless indicated) |
Wilcoxon- Mann- Whitney z, p |
|---|---|---|---|---|---|---|---|
| CES-D | 22.75 (12.38) (n=111) | 40.63 (11.86) | 21.17 (11.16) (n=102) | z=3.77, p <.001 | 33.17 (11.20) (n=30) | 18.89 (10.45) (n=81) | z=5.20, p <.001 |
| GSHS Worrya | 2.46 (1.08) | 3.89 (0.33) | 2.34 (1.04) | z=4.06, p <.001 | 3.19 (0.87) | 2.20 (1.04) | z=4.37, p <.001 |
| GSHS Social Impairmentb | 2.22 (1.05) | 3.33 (1.12) | 2.13 (0.99) | z=3.02, p=.003 | 2.87 (1.02) | 1.99 (0.96) | z=3.94, p <.001 |
| GSHS Academic Impairmentc | 2.76 (1.18) (n=119) | 3.56 (0.88) | 2.70 (1.19) (n=110) | z=2.18, p=.029 | 3.35 (0.91) | 2.56 (1.20) (n=88) | z=3.44, p=.001 |
|
| |||||||
| PTSD | Overall (n=120, unless indicated) | PTSD Case (n=13) | All others (n=107, unless indicated) | Wilcoxon-Mann-Whitney z, p | PTSD Case or Subthreshold (n=25) | All others (n=95, unless indicated) | Wilcoxon-Mann-Whitney z, p |
|
| |||||||
| SLE | 5.43 (2.20) | 7.00 (2.04) | 5.24 (2.15) | z=2.58, p=.010 | 6.92 (1.93) | 5.04 (2.11) | z=3.77, p <.001 |
| RATS | 47.77 (11.76) (n =115) | 55.16 (9.62) | 46.82 (11.72) (n=102) | z=2.44, p=.015 | 53.73 (8.37) | 46.12 (12.07) (n=90) | z=3.11, p=.002 |
During the past 12 months, how often have you been so worried about something that you could not sleep at night?
During the past 12 months, how often have you felt lonely?
During the past 12 months, how often have you had a hard time staying focused on your homework or other things you had to do?
Utilization of healthcare across groups identified by mental health needs
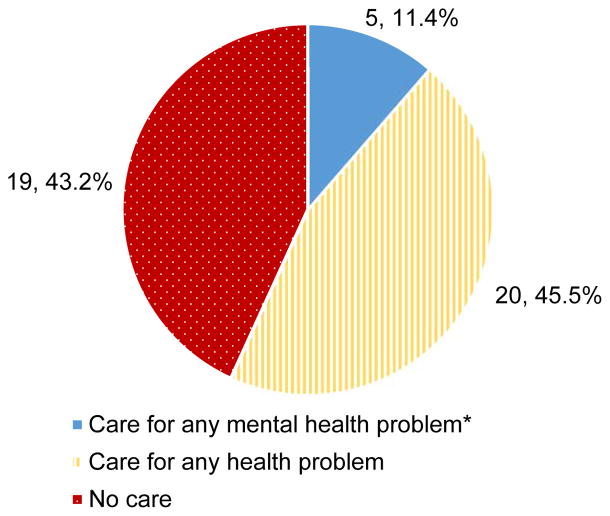
Among participants with a diagnosis of subthreshold or full-syndrome MDE and/or PTSD, 88.6% (n=39) had not accessed healthcare for any mental health problem in the past 12 months; 43.2% (n=19) had not accessed healthcare for any mental or other health problem during the same time period (Figure 1); and 36.4% (n=16) had not accessed mental healthcare, other healthcare, or folk sector care over the same one-year period. Health service utilization patterns were similar among participants with full-syndrome MDE or PTSD (no mental health utilization: 94.1%, n=16; no utilization for any health problem: 41.2%, n=7), MDE cases (no mental health utilization: 88.9%, n=8; no utilization for any health problem: 33.3%, n=3), PTSD cases (no mental health utilization: 100.0%, n=13; no utilization for any health problem: 46.2%, n=6), or not meeting at least subthreshold criteria (no mental health utilization: 86.8%, n=66; no utilization for any health problem: 46.1%, n=35).
Figure 1.
Health-system based care use in the past year among participants with case or subthreshold MDE and/or PTSD, n=44.
*All participants above who indicated receiving care for a mental health problem also indicated receiving care for any health problem
Discussion
In this community-based sample of secondary school youth in Haiti’s Central Plateau, the point-prevalence estimates of MDE and PTSD were 7.5% and 10.8%, respectively, with 14.2% affected by one or both of these disorders. Although the point prevalence of MDE in our sample was just slightly higher than the 5.3% 12-month prevalence of MDE in a community based sample among of 18–34 year old adults in developing countries (Kessler et al., 2010), the prevalence of PTSD was substantially higher than the 0.7–0.8% prevalence of PTSD reported among adults in low and middle income countries (Karam et al., 2014). Further, over one-third of our sample had at least subthreshold MDE and/or PTSD and, therefore, demonstrated clinically significant mental health treatment need. Diagnostic assignments based on the modified, abridged version of the SCID showed good convergent validity in comparisons based on several measures of symptomatology, including depression and PTSD screening tools and an assessment of stressful events/traumatic exposures.
We also found striking evidence of a large mental health treatment gap. Across diagnostic classifications, nearly 90% of participants in need of mental health treatment had not utilized services in the past year for the mental health problems we describe here. The magnitude of unmet need for Haitian youth identified in this study appears to be comparatively large (cf. Demyttenaere et al., 2004; Wang et al., 2007). This is unlikely to be attributable to lack of available mental health services since the participating schools were located in communities with ZL health centers offering mental health care. Nevertheless, participants endorsed difficulties with transportation as well as payment for care and medicine. Future exploration of these difficulties is warranted. Participant reports align with research indicating that accessibility of care is a key determinant of youth utilization (Ambresin et al., 2013; World Psychiatric Association et al., 2005). Attitudes about mental health treatment among Haitian youth may be important to explore, given research suggesting that adults in the Central Plateau prefer non-health system based care for mental disorders (Wagenaar et al., 2013). However, our data did not support that a substantial percentage of individuals with mental health needs who had not accessed mental health care through the health sector were accessing it through the folk sector instead.
Nearly half of participants with full or subthreshold MDE or PTSD who had not utilized health services for a mental health problem, had accessed general healthcare over the same one-year period. Like other rural Haitians (Keys et al., 2012), our participants may be presenting for general health services with somatic problems that could represent idioms of emotional distress. Hence, incorporation of screening and treatment for mental disorders into primary healthcare through collaborative care programs guided by the Mental Health Gap Action Programme may improve case-finding and utilization of mental healthcare (Sharpe & Naylor, 2016; Wang et al., 2007; WHO, 2008).
There are a number of limitations of this study. School-based assessment in central Haiti excludes youth who do not attend school or reside elsewhere in Haiti and limits the generalizability of our findings. Our study sample of transitional age youth within a narrow age range, moreover, does not encompass younger adolescents who may encounter different mental health barriers and needs. Nonetheless, there is growing recognition of a need to focus on early identification of mental health problems and effective interventions for youth who are making the developmental transition to greater independence and adulthood (Patton et al., 2016; Wilens & Rosenbaum, 2013). Although a SCID interview is commonly considered to be a gold standard for research diagnostic assessment, there were limitations to its implementation in this setting. Our study diagnostic assignments could have resulted in misclassification due to the use of SCID-based interviews in a setting for which it was not developed. Moreover, our use of an abridged interview for MDE meant that we were unable to discern the impact of medical illness, bereavement, food insecurity, and poverty on symptoms. Finally, because SCID content aligns with nosologic constructs developed outside of Haiti, it may not have captured clinically significant psychopathology that is expressed or manifested differently in the Haitian cultural context (Farmer, 1992; WHO, 2010; Keys et al., 2012). However, other qualitative research has demonstrated evidence of overlap between symptoms of MDE and PTSD experienced in Haiti and corresponding diagnostic constructs measured by the SCID (Bolton et al., 2012; Rahill et al., 2015; Rasmussen et al., 2015). Our approach integrating interviewer clinical judgment— based on local diagnostic experience—into our procedure for study diagnostic assignment was intended to identify locally salient presentations of MDE and PTSD (cf. Bhui et al., 2003). Likewise, we included subthreshold variants of MDE and PTSD in our analyses so as to encompass a broader range of psychopathology than is reflected in SCID-generated full syndrome diagnoses. Our finding that groups defined by a study diagnostic assignment of MDE, PTSD, and subthreshold variants had greater levels of psychopathology as measured by standardized self-report assessments, supports the validity of these assignments. Finally, our cross-sectional study design does not illuminate possible temporal trends in prevalence, either relative to the 2010 earthquake or many chronic social adversities confronting Haitian youth.
Notwithstanding these limitations, our finding of prevalent MDE, PTSD, and clinically significant psychopathology in our study population warrants concern and action. The remediation of unmet burden of mental disease arguably requires broad intervention beyond the clinical domain given the myriad impacts of poverty on health (e.g., Farmer, 1992). Like Haitian youth, many youth residing in LMICs face harsh social vulnerabilities that increase risk for poor mental health (Patel et al., 2008; Lund et al., 2010), such as absence of caregivers, poor physical health and nutrition, and low levels of education (Walker et al., 2007; Kieling et al., 2011; Smith Fawzi et al., 2012)., Nonetheless, study findings underscore the importance of ensuring access to mental health services for youth in Haiti, and by extension, in other LMICs.
Conclusion
We observed a high prevalence of PTSD and substantial prevalence of MDE in this sample of secondary school youth in rural Haiti. Moreover, mental health care utilization was low among youth with clinically significant levels of MDE or PTSD symptomatology, suggesting a large mental health treatment gap for this population. This underscores the need to reduce barriers to help-seeking and increase human resources to provide mental health treatment for youth in Haiti and similar resource-limited settings.
Acknowledgments
We are grateful to the leadership of Zanmi Lasante as well as at the four schools who so generously accommodated the planning and implementation of the mental health training and its accompanying school-based pilot study. We thank Kate Boyd, Shin Daimyo, Georges Alexis, Elysee Noesil, Ernst Origene, Handy Petit-Homme, and other colleagues at Partners In Health and Zanmi Lasante as well as Claire Pernar and Megan Benson Stack at Harvard Medical School for their support of the planning, management and implementation of the study and trainings. We thank Marie-Christine Ouellet Ph.D. and her team, École de psychologie, Université Laval, Québec, Canada for providing the French translation of the SCID. We express here our profound gratitude to the student study participants for their time and generous feedback, and from whom we learned so much.
Funding
Research reported in this publication was supported by National Institute of Mental Health of the National Institutes of Health under award number R21MH093298 (Co-PIs, Becker and Eustache). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Ambresin AE, Bennett K, Patton GC, Sanci LA, Sawyer SM. Assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. Journal of Adolescent Health. 2013;52(6):670–681. doi: 10.1016/j.jadohealth.2012.12.014. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Text. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Bean T, Eurelings-Bontekoe E, Derluyn I, Spinhoven P. Oegstgeest: Centrum ‘45. 2004a. Reactions of Adolescents to Traumatic Stress questionnaire (RATS): User’s manual. [DOI] [PubMed] [Google Scholar]
- Bean T, Eurelings-Bontekoe E, Derluyn I, Spinhoven P. Centrum’45, Oegstgeest. 2004b. Stressful life events (SLE): User’s Manual. [Google Scholar]
- Bean T, Derluyn I, Eurelings-Bontekoe E, Broekaert E, Spinhoven P. Validation of the multiple language versions of the reactions of adolescents to traumatic stress questionnaire. Journal of traumatic stress. 2006;19(2):241–255. doi: 10.1002/jts.20093. [DOI] [PubMed] [Google Scholar]
- Becker AE, Kleinman A. Mental health and the global agenda. New England Journal of Medicine. 2013;369(1):66–73. doi: 10.1056/NEJMra1110827. [DOI] [PubMed] [Google Scholar]
- Bhui K, Mohamud S, Warfa N, Craig TJ, Stansfeld SA. Cultural adaptation of mental health measures: improving the quality of clinical practice and research. British Journal of Psychiatry. 2003 Sep;183(3):184–186. doi: 10.1192/bjp.183.3.184. [DOI] [PubMed] [Google Scholar]
- Blanc J, Bui E, Mouchenik Y, Derivois D, Birmes P. Prevalence of post-traumatic stress disorder and depression in two groups of children one year after the January 2010 earthquake in Haiti. Journal of affective disorders. 2015;172:121–126. doi: 10.1016/j.jad.2014.09.055. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Hickling EJ, Taylor AE, Loos WR, Gerardi RJ. Psychological morbidity associated with motor vehicle accidents. Behaviour research and therapy. 1994;32(3):283–290. doi: 10.1016/0005-7967(94)90123-6. [DOI] [PubMed] [Google Scholar]
- Bolton P, Surkan PJ, Gray AE, Desmousseaux M. The mental health and psychosocial effects of organized violence: A qualitative study in northern Haiti. Transcultural psychiatry. 2012;49(3–4):590–612. doi: 10.1177/1363461511433945. [DOI] [PubMed] [Google Scholar]
- Brancu M, Mann-Wrobel M, Beckham JC, Wagner HR, Elliott A, Robbins AT, … Runnals JJ. Subthreshold posttraumatic stress disorder: A meta-analytic review of DSM–IV prevalence and a proposed DSM–5 approach to measurement. Psychological trauma: theory, research, practice, and policy. 2016;8(2):222–232. doi: 10.1037/tra0000078. [DOI] [PubMed] [Google Scholar]
- Cénat JM, Derivois D. Assessment of prevalence and determinants of posttraumatic stress disorder and depression symptoms in adult survivors of earthquake in Haiti after 30 months. Journal of affective disorders. 2014;159:111–117. doi: 10.1016/j.jad.2014.02.025. [DOI] [PubMed] [Google Scholar]
- Cénat JM, Derivois D. Long-term outcomes among child and adolescent survivors of the 2010 Haitian earthquake. Depression and anxiety. 2015;32(1):57–63. doi: 10.1002/da.22275. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Global Student Health Survey (GSHS) 2013 Retrieved from: http://www.cdc.gov/gshs/background/pdf/gshsoverview.pdf.
- Cerdá M, Paczkowski M, Galea S, Nemethy K, Péan C, Desvarieux M. Psychopathology in the aftermath of the Haiti earthquake: A population-based study of posttraumatic stress disorder and major depression. Depression and anxiety. 2013;30(5):413–424. doi: 10.1002/da.22007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukor J, Wyka K, Jayasinghe N, Difede J. The nature and course of subthreshold PTSD. Journal of anxiety disorders. 2010;24(8):918–923. doi: 10.1016/j.janxdis.2010.06.017. [DOI] [PubMed] [Google Scholar]
- Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine J, … Polidori G. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291(21):2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- Eustache E, Becker AE, Wozo Ekip. Developing Research Capacity for Mental Health Interventions for Youth in Haiti. In. Frontiers in Neuroscience for Global Health/Tenth Anniversary of Brain Disorders in the Developing World: Research across the Lifespan 2014 [Google Scholar]
- Eustache E, Gerbasi ME, Severe J, Fils-Aimé JR, Smith Fawzi MC, Raviola GJ, … Becker AE. Formative research on a teacher accompaniment model to promote youth mental health in Haiti: Relevance to mental health task-sharing in low-resource school settings. International Journal of Social Psychiatry. 2017a Jun;63(4):314–24. doi: 10.1177/0020764017700173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eustache E, Gerbasi ME, Fawzi MS, Fils-Aimé JR, Severe J, Raviola GJ, … Becker AE. Mental health training for secondary school teachers in Haiti: a mixed methods, prospective, formative research study of feasibility, acceptability, and effectiveness in knowledge acquisition. Global Mental Health. 2017b;4 doi: 10.1017/gmh.2016.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer P. The Birth of the Klinik: A Cultural History of Haitian Professional Psychiatry. In: Gaines A, editor. Ethnopsychiatry: The cultural construction of professional and folk psychiatries. Albany: SUNY Press; 1992. pp. 251–272. [Google Scholar]
- Farmer P. On suffering and structural violence. In: Farmer P, Saussy H, editors. Partner to the poor: a Paul Farmer reader. Vol. 23. Univ of California Press; 2010. pp. 328–349. [Google Scholar]
- Farmer P. Haiti after the earthquake. Public Affairs. 2011 Jul 10; [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW. User’s Guide for the Structured Clinical Interview for DSM-IV-TR Axis I Disorders - Research Version - (SCID-I for DSM-IV-TR, November 2002 Revision) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- First MB, Spitzer R, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition. New York, NY: Biometrics Research, New York State Psychiatric Institute; 2010. SCID-I/NP, January 2010 Revision. [Google Scholar]
- Franklin CL, Sheeran T, Zimmerman M. Screening for trauma histories, posttraumatic stress disorders (PTSD) and subthreshold PTSD in psychiatric outpatients. Psychological Assessment. 2002;14(4):467–471. doi: 10.1037//1040-3590.14.4.467. [DOI] [PubMed] [Google Scholar]
- Ghio L, Gotelli S, Marcenaro M, Amore M, Natta W. Duration of untreated illness and outcomes in unipolar depression: a systematic review and meta-analysis. Journal of affective disorders. 2014;152:45–51. doi: 10.1016/j.jad.2013.10.002. [DOI] [PubMed] [Google Scholar]
- Goldmann E, Galea S. Mental health consequences of disasters. Annual review of public health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, … Mathers CD. Global burden of disease in young people aged 10–24 years: a systematic analysis. The Lancet. 2011;377(9783):2093–2102. doi: 10.1016/S0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows (Version 23.0) Armonk, NY: IBM Corp; 2015. [Google Scholar]
- Institute for Health Metrics and Evaluation (IHME) GBD Compare. Seattle, WA: IHME, University of Washington; 2016. Retrieved from: http://vizhub.healthdata.org/gbd-compare. [Google Scholar]
- Karam EG, Friedman MJ, Hill ED, Kessler RC, McLaughlin KA, Petukhova M, … Girolamo G. Cumulative traumas and risk thresholds: 12-month PTSD in the World Mental Health (WMH) surveys. Depression and Anxiety. 2014;31(2):130–142. doi: 10.1002/da.22169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Keys HM, Kaiser BN, Kohrt BA, Khoury NM, Brewster ART. Idioms of distress, ethnopsychology, and the clinical encounter in Haiti’s central plateau. Social Science & Medicine. 2012;75(3):555–564. doi: 10.1016/j.socscimed.2012.03.040. [DOI] [PubMed] [Google Scholar]
- Khoury NM, Kaiser BN, Keys HM, Brewster ART, Kohrt BA. Explanatory models and mental health treatment: is vodou an obstacle to psychiatric treatment in rural Haiti? Culture, Medicine, and Psychiatry. 2012;36(3):514–534. doi: 10.1007/s11013-012-9270-2. [DOI] [PubMed] [Google Scholar]
- Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, … Rahman A. Child and adolescent mental health worldwide: evidence for action. The Lancet. 2011;378(9801):1515–1525. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- Kleinman A. Patients and healers in the context of culture: An exploration of the borderland between anthropology, medicine, and psychiatry. Vol. 3. Univ of California Press; 1980. [Google Scholar]
- Lund C, Breen A, Flisher AJ, Kakuma R, Corrigall J, Joska JA, … Patel V. Poverty and common mental disorders in low and middle income countries: A systematic review. Social science & medicine. 2010;71(3):517–528. doi: 10.1016/j.socscimed.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquez PV. Mental Health Among Displaced People and Refugees. World Bank; 2016. Retrieved from: https://openknowledge.worldbank.org/bitstream/handle/10986/25854/111164-WP-P145350-PUBLIC-Mental-health-displaced-people-edit-Dec-19-2016.pdf?sequence=1. [Google Scholar]
- Martsolf D. Childhood maltreatment and mental and physical health in Haitian adults. Journal of Nursing Scholarship. 2004;36(4):293–299. doi: 10.1111/j.1547-5069.2004.04054.x. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Purcell R, Goldstone S, Amminger GP. Age of onset and timing of treatment for mental and substance use disorders: implications for preventive intervention strategies and models of care. Current opinion in psychiatry. 2011;24(4):301–306. doi: 10.1097/YCO.0b013e3283477a09. [DOI] [PubMed] [Google Scholar]
- Ngo VK, Rubinstein A, Ganju V, Kanellis P, Loza N, Rabadan-Diehl C, Daar AS. Grand challenges: integrating mental health care into the non-communicable disease agenda. PLoS Med. 2013;10(5):e1001443. doi: 10.1371/journal.pmed.1001443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opoliner A, Blacker D, Fitzmaurice G, Becker A. Challenges in assessing depressive symptoms in Fiji: A psychometric evaluation of the CES-D. International Journal of Social Psychiatry. 2014;60(4):367–376. doi: 10.1177/0020764013490871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Flisher AJ, Nikapota A, Malhotra S. Promoting child and adolescent mental health in low and middle income countries. Journal of Child Psychology and Psychiatry. 2008;49(3):313–334. doi: 10.1111/j.1469-7610.2007.01824.x. [DOI] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Cappa C, Currie D, Riley L, Gore F, … Mokdad A. Health of the world’s adolescents: a synthesis of internationally comparable data. The Lancet. 2012;379(9826):1665–1675. doi: 10.1016/S0140-6736(12)60203-7. [DOI] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Romaniuk H, Mackinnon A, Carlin JB, Degenhardt L, … Moran P. The prognosis of common mental disorders in adolescents: a 14-year prospective cohort study. The Lancet. 2014;383(9926):1404–1411. doi: 10.1016/S0140-6736(13)62116-9. [DOI] [PubMed] [Google Scholar]
- Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, … Kakuma R. Our future: a Lancet commission on adolescent health and wellbeing. The Lancet. 2016;387(10036):2423–2478. doi: 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- Rahill GJ, Joshi M, Lescano C, Holbert D. Symptoms of PTSD in a sample of female victims of sexual violence in post-earthquake Haiti. Journal of Affective disorders. 2015;173:232–238. doi: 10.1016/j.jad.2014.10.067. [DOI] [PubMed] [Google Scholar]
- Rasmussen A, Eustache E, Raviola G, Kaiser B, Grelotti DJ, Belkin GS. Development and validation of a Haitian Creole screening instrument for depression. Transcultural psychiatry. 2015;52(1):33–57. doi: 10.1177/1363461514543546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raviola G, Eustache E, Oswald C, Belkin GS. Mental health response in Haiti in the aftermath of the 2010 earthquake: a case study for building long-term solutions. Harvard review of psychiatry. 2012;20(1):68–77. doi: 10.3109/10673229.2012.652877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Rosenberg SD. Preliminary MMPI scores as predictors of combat-related PTSD symptoms. American Journal of Psychiatry. 1993;150(3):479–483. doi: 10.1176/ajp.150.3.479. [DOI] [PubMed] [Google Scholar]
- Sharpe M, Naylor C. Integration of mental and physical health care: from aspiration to practice. The Lancet Psychiatry. 2016;3(4):312–313. doi: 10.1016/S2215-0366(16)00062-6. [DOI] [PubMed] [Google Scholar]
- Smith Fawzi MC, Lambert W, Singler JM, Koenig SP, Leandre F, Nevil P, … Louissaint M. Prevalence and risk factors of STDs in rural Haiti: implications for policy and programming in resource-poor settings. International journal of STD & AIDS. 2003;14(12):848–853. doi: 10.1258/095646203322556200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith Fawzi MC, Eustache E, Oswald C, Louis E, Surkan PJ, Scanlan F, … Mukherjee JS. Psychosocial support intervention for HIV-affected families in Haiti: implications for programs and policies for orphans and vulnerable children. Social science & medicine. 2012;74(10):1494–1503. doi: 10.1016/j.socscimed.2012.01.022. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, … Bruffaerts R. Undertreatment of people with major depressive disorder in 21 countries. The British Journal of Psychiatry. 2016:bjp-bp. doi: 10.1192/bjp.bp.116.188078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagenaar BH, Hagaman AK, Kaiser BN, McLean KE, Kohrt BA. Depression, suicidal ideation, and associated factors: a cross-sectional study in rural Haiti. BMC psychiatry. 2012;12(1):149. doi: 10.1186/1471-244X-12-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagenaar BH, Kohrt BA, Hagaman AK, McLean KE, Kaiser BN. Determinants of care seeking for mental health problems in rural Haiti: culture, cost, or competency. Psychiatric Services. 2013;64(4):366–372. doi: 10.1176/appi.ps.201200272. [DOI] [PubMed] [Google Scholar]
- Walker SP, Wachs TD, Gardner JM, Lozoff B, Wasserman GA, Pollitt E … International Child Development Steering Group. Child development: risk factors for adverse outcomes in developing countries. The Lancet. 2007;369(9556):145–157. doi: 10.1016/S0140-6736(07)60076-2. [DOI] [PubMed] [Google Scholar]
- Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, … Haro JM. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. The Lancet. 2007;370(9590):841–850. doi: 10.1016/S0140-6736(07)61414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilens TE, Rosenbaum JF. Transitional aged youth: a new frontier in child and adolescent psychiatry. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(9):887–890. doi: 10.1016/j.jaac.2013.04.020. [DOI] [PubMed] [Google Scholar]
- World Health Organization. mhGAP Mental Health Gap Action Programme: Scaling up care for mental, neurological, and substance use disorders. Geneva: World Health Organization; 2008. [PubMed] [Google Scholar]
- World Health Organization. Culture and Mental Health in Haiti: A Literature Review. Geneva: WHO; 2010. Retrieved from: http://www.who.int/mental_health/emergencies/culture_mental_health_haiti_eng.pdf. [Google Scholar]
- World Health Organization. Mental Health Atlas 2011. Geneva: World Health Organization; 2011. Retrieved from: http://www.who.int/mental_health/evidence/atlasmnh/en/ [Google Scholar]
- World Health Organization. Global School-based Student Health Survey (GSHS) Core-Expanded Questions. 2013a http://www.who.int/chp/gshs/GSHS_Core_Expanded_Questions_2013_English.pdf?ua=1.
- World Health Organization. Global school-based student health survey 2013 core questionnaire modules. 2013b http://www.who.int/chp/gshs/GSHS_Core_Modules_2013_English.pdf?ua=1.
- World Psychiatric Association, World Health Organization and International Association for Child and Adolescent Psychiatry and Allied Professions. Atlas: Child and adolescent mental health resources: global concerns, implications for the future. Geneva: World Health Organization; 2005. [Google Scholar]