SUMMARY
Clostridium difficile is the main causative agent of antibiotic-associated and health care-associated infective diarrhea. Recently, there has been growing interest in alternative sources of C. difficile other than patients with Clostridium difficile infection (CDI) and the hospital environment. Notably, the role of C. difficile-colonized patients as a possible source of transmission has received attention. In this review, we present a comprehensive overview of the current understanding of C. difficile colonization. Findings from gut microbiota studies yield more insights into determinants that are important for acquiring or resisting colonization and progression to CDI. In discussions on the prevalence of C. difficile colonization among populations and its associated risk factors, colonized patients at hospital admission merit more attention, as findings from the literature have pointed to their role in both health care-associated transmission of C. difficile and a higher risk of progression to CDI once admitted. C. difficile colonization among patients at admission may have clinical implications, although further research is needed to identify if interventions are beneficial for preventing transmission or overcoming progression to CDI.
KEYWORDS: Clostridium difficile, health care-associated infections, intestinal colonization
INTRODUCTION
Clostridium difficile is a spore-forming, Gram-positive rod that causes Clostridium difficile infection (CDI), whose symptoms range from mild diarrhea to life-threatening pseudomembranous colitis. Clostridium difficile infection has been considered a health care-associated infection transmitted primarily from other symptomatic CDI patients. Recent studies, notably based on highly discriminatory techniques, such as whole-genome sequencing, have emphasized that assumptions about the sources and transmission of C. difficile may not be correct (1–3). The realization that a large proportion of CDI cases are not due to transmission from other CDI cases has underlined the need to reexamine the many diverse potential sources of C. difficile and to determine their contributions to the epidemiology of this disease. Paramount to our understanding is the issue of colonization of C. difficile, which is the subject of this review.
DEFINITIONS
Definition of C. difficile Colonization
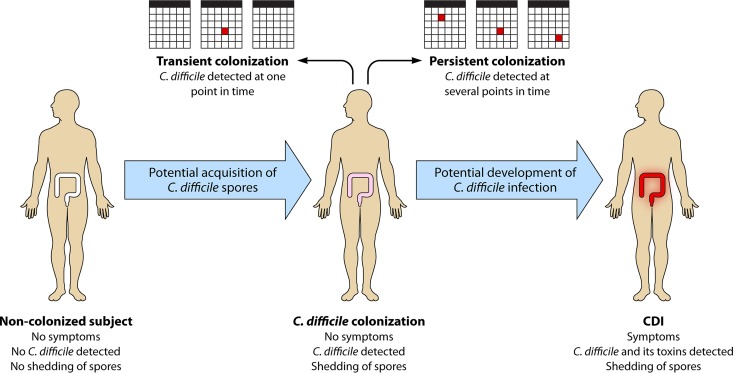
We define “C. difficile colonization” as the detection of the organism in the absence of CDI symptoms and “C. difficile infection” as the presence of C. difficile toxin (ideally) or a toxigenic strain type and clinical manifestations of CDI (Fig. 1). Clinical presentations compatible with CDI include diarrhea (defined as Bristol stool chart types 5 to 7 plus a stool frequency of three stools in 24 or fewer consecutive hours, or more frequently than is normal for the individual), ileus (defined as signs of severely disturbed bowel function, such as vomiting and absence of stool with radiological signs of bowel distention), and toxic megacolon (defined as radiological signs of distention of the colon, usually to ≥10 cm in diameter, and signs of a severe systemic inflammatory response) (4).
FIG 1.
C. difficile colonization versus C. difficile infection. CDI, Clostridium difficile infection.
However, as a previous review highlighted, the definitions for CDI used in the Infectious Diseases Society of America (IDSA) and European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines differ (5–7). IDSA guidelines accept a CDI diagnosis if C. difficile symptoms are identified in combination with either the presence of a toxigenic strain, free toxin in the stool, or histopathological evidence of pseudomembranous colitis, whereas recent ESCMID guidelines require the additional exclusion of alternative etiologies for diarrhea. Differences in definitions for CDI may affect the proportion of patients regarded as asymptomatically or symptomatically colonized instead of having symptomatic CDI.
Moreover, the criteria used to define asymptomatic carriage/colonization vary considerably among studies. Strict definitions of colonization have been described (8, 9) and include classifying asymptomatic carriers as those testing positive for C. difficile toxins but having no signs of CDI for 12 weeks pre- or post-specimen collection, based on a retrospective record review (2). Highly restrictive definitions are difficult to apply in practice, and therefore use of a simplified definition of multiple positive stools from multiple time points to determine colonization has been recommended (10). In contrast, other studies utilized the less strict definition of colonization as a single C. difficile-positive stool and the absence of diarrhea (11–13). Clearly, this has implications for who is classified as colonized by C. difficile and how asymptomatic cohorts are perceived as potential transmission sources. Donskey and colleagues demonstrated that a single C. difficile-positive fecal sample may imply either colonization, transient carriage, or even “passing through” (10). We thus indicate the importance of further delineation of asymptomatic carriage into transient and persistent colonization, as outlined in a transmission study by Curry et al. (2). Differentiating repeat, persistent detection (carriage) and point detection (colonization) would enable a greater understanding of transmission events and the infection control practices necessary to prevent CDI spread. However, at the moment, longitudinal studies on this topic are lacking.
Assessing Asymptomatic Colonization
The rates of asymptomatic colonization vary considerably due to different definitions of diarrhea and laboratory methodological differences.
Standardization of the definition of diarrhea is essential, since McFarland et al. defined diarrhea as ≥3 unformed stools for at least two consecutive days (14), while others accepted the same number of loose stools, but over a single 24-h period (12, 15). Therefore, the absence of diarrhea is not synonymous with a lack of loose stools, potentially resulting in inconsistent designations of asymptomatic patients.
Besides the disparate definitions of diarrhea, assays or methodologies to test for CDI or C. difficile colonization also vary and affect the incidence rates of both conditions (13) (Table 1). Methods used for CDI diagnosis can sometimes also be used to diagnose C. difficile colonization, but on the other hand, some methods used for routine diagnosis of CDI may falsely classify colonized patients with diarrhea (due to a non-C. difficile cause) as CDI patients.
TABLE 1.
Diagnostic methodologies for detecting C. difficile or its toxinsa
| Diagnostic test | Detection target | Ability to detect colonization | Remarks |
|---|---|---|---|
| Direct culture | C. difficile | Yes | Does not differentiate between colonization and infection by C. difficile, does not differentiate between toxigenic and nontoxigenic C. difficile |
| Enrichment culture | C. difficile | Yes | Does not differentiate between colonization and infection by C. difficile, does not differentiate between toxigenic and nontoxigenic C. difficile, thought to be more sensitive than direct culture when small numbers of vegetative cells or spores are present |
| GDH EIA | GDH | Yes | Does not differentiate between colonization and infection by C. difficile, does not differentiate between toxigenic and nontoxigenic C. difficile |
| Toxigenic culture | Toxigenic C. difficile | Yes | Does not differentiate between infection and colonization by toxigenic C. difficile |
| PCR assay of toxin genes | tcdA, tcdB, binary toxin genes | Yes | Does not differentiate between infection and colonization by toxigenic C. difficile |
| Toxin A/B EIA | Toxins A and B | No | Detects toxins A and B, not the presence of the organism, and therefore cannot be utilized to identify asymptomatic colonization |
| CCNA | Toxin B | No | Detects toxin B, not the presence of the organism, and therefore cannot be utilized to identify asymptomatic colonization |
GDH, glutamate dehydrogenase; EIA, enzyme immunoassay; CCNA, cell cytotoxicity neutralization assay.
Despite its labor-intensive and time-consuming characteristics and susceptibility to toxin degradation in stool samples with incorrect storage, the cell cytotoxicity neutralization assay (CCNA) is frequently considered the gold standard for CDI diagnosis due to its high specificity and direct detection of the main virulence factor (toxin) (16, 17). However, as CCNA detects C. difficile toxins, not the presence of the organism itself, its utility is limited in detecting C. difficile colonization. Nonetheless, in infants, a positive CCNA result without clinical symptoms has been used to consider these infants colonized by C. difficile (18), indicating the aberrant association between toxin presence and clinical symptoms in this age group.
An alternative gold standard for CDI is toxigenic culture, which includes culture of the organism followed by detection of its in vitro toxin-producing capacity by a toxin enzyme immunoassay (Tox A/B EIA), CCNA, or a nucleic acid amplification test (NAAT) for detection of the toxin genes. A major study of >12,000 fecal specimens by Planche et al. highlighted no increase in mortality in patients harboring a toxigenic C. difficile strain without the presence of detectable toxin (19), suggesting that free toxin positivity reflects CDI, while toxigenic culture positivity encompasses some patients with colonization. Therefore, the use of toxigenic culture to diagnose CDI may lead to overdiagnosis of CDI, and hence an underestimation of C. difficile colonization. However, if the goal is detection of toxigenic C. difficile colonization in asymptomatic patients, toxigenic culture is a suitable option.
As both gold standard methods for diagnosing CDI are time-consuming and laborious, rapid assays are more appealing for CDI testing in daily practice. If rapid assays are used to test for CDI, it is recommended that they be used in an algorithm in order to optimize positive and negative predictive values. Concerning the relationship between free toxins and true disease as described above, the algorithm should include a Tox A/B EIA to test for free toxins in stool. However, in clinical practice, rapid assays (especially NAATs) are often used as stand-alone tests instead of as part of an algorithm, and this may again lead to C. difficile colonization erroneously being classified as CDI. A study by Polage et al. demonstrated that 39.9% of NAAT-positive specimens tested negative for toxin by cell cytotoxicity assay (20), showing that reliance on a stand-alone NAAT may lead to overdiagnosis of CDI, and consequently an underestimation of asymptomatic colonization, similar to the situation described above for toxigenic culture.
There are some specific limitations that have to be taken into account in assessing C. difficile colonization. With C. difficile colonization, bacterial loads can be lower than those for CDI. Direct culture of the organism is quite sensitive, although detection rates will differ as the sensitivities of the culture media vary. Nonetheless, culture-independent detection techniques, such as enzyme immunoassays, have lower sensitivity and specificity than those of culture methods. As stools with lower counts of C. difficile may be deemed falsely negative, these assays may lead to underestimation of the asymptomatic colonization rate, making them less suitable for detection of colonization. For example, glutamate dehydrogenase (GDH) screening is regarded as highly specific for detection of C. difficile in clinical specimens (7, 21); however, potential issues have been highlighted with the use of this methodology for reporting asymptomatic colonization (22). In a study by Miyajima et al., only one of five positive cases determined by an enrichment culture method was positive by GDH assay (22), probably due to low levels of GDH antigen (below the lower limit of detection for this assay) in nondiarrheal stools.
As the above observations illustrate, the diagnosis of CDI should not be based on laboratory results alone but should always be supported by clinical signs and symptoms suggestive of CDI (7, 23). This is especially important in cases where methodologies which cannot discern CDI from colonization (stand-alone NAATs and toxigenic culture) are applied for routine CDI testing.
Likewise, we suggest that an optimal diagnostic method for the determination of asymptomatic colonization should include a confirmation of the absence of clinical symptoms (i.e., absence of diarrhea, ileus, and toxic megacolon per the criteria described above) or the presence of an alternative explanation for these clinical symptoms. The laboratory methods should include (enrichment) stool culture and either toxigenic culture or PCR confirmation. This combination of sensitive techniques, although expensive, will yield more reliable data and support interstudy comparisons.
MECHANISMS OF C. DIFFICILE COLONIZATION
After the definition of C. difficile colonization, a closer look at mechanisms that underlie C. difficile colonization is needed. Key factors in acquiring or resisting colonization (and subsequent infection) are the gut microbiota and the host immune response against C. difficile.
Disruptions in the Microbiota
The gut microbiota has a prominent role in the whole life cycle of C. difficile, from germination and colonization to establishing symptomatic disease. Results from studies on the differences in microbial composition in patients with CDI, asymptomatic carriers, and noninfected patients can elucidate which alterations determine either susceptibility to colonization and/or disease development or colonization resistance (defined as the resistance to colonization by ingested bacteria or inhibition of overgrowth of resident bacteria normally present at low levels within the intestinal tract) (24, 25). The optimal method for studying the impact of the microbiota in spore germination, colonization, and toxin production by C. difficile would be to take luminal samples and biopsy specimens to study both the microbiota attached to the intestinal wall and that present in the lumen, as C. difficile was actually found in biofilm-like structures in the mucus layer of the murine gut and in a human CDI gut model (26, 27). Also, ideally, samples from different locations along the intestine should be examined, because it was demonstrated that in mice C. difficile spores did germinate and grow in ileal contents, while this was not possible in cecal contents unless the mice had been treated with specific antibiotics (28). Obtaining these samples from human subjects is not feasible, though ingestible, remotely controlled capsules that are capable of taking samples from the small intestinal tract are in development. However, most human studies use easy-to-obtain fecal samples to analyze the intestinal microbiota, although these may not actually optimally reflect the microbial composition in the more proximal intestine, where bile acid-induced germination of ingested spores occurs (see below).
Alterations in gut microbial composition that have been described for CDI patients include a lower species richness and lower microbial diversity than those in healthy controls (29–31). Greater heterogeneity was observed between samples from CDI patients than between individual samples from healthy controls (31). At the phylum level, Bacteroidetes was less prevalent in CDI patients than in healthy controls, while there was an increase in the Proteobacteria. Within the Firmicutes phylum, a decrease in the Clostridia, especially from the Ruminococcaceae and Lachnospiraceae families and butyrate-producing anaerobic bacteria from Clostridium clusters IV and XIVa, was noted in CDI patients (31). In addition to these depletions, increases in bacteria of the orders Enterobacteriales, Pseudomonadales (Proteobacteria), and Lactobacillales (Firmicutes) were observed (30, 31). Also, in human fecal samples collected prior to onset of a first CDI episode, decreased diversity, a decrease in the phylum Bacteroidetes, and changes within the phylum Firmicutes (a decrease in Clostridiales family XI incertae sedis and an increase in Enterococcaceae from the order Lactobacillales) were observed in comparison to those for samples from hospitalized patients who did not develop CDI (32). A reduction in Clostridiales family XI incertae sedis in these samples was demonstrated to be independently associated with CDI development. Moreover, changes in microbial composition comparable to those found in CDI patients have been described for patients with nosocomial diarrhea who tested negative for C. difficile or its toxins. These changes included comparable decreases in species richness and microbial diversity and, again, a decrease in butyrate-producing bacteria from the Ruminococcaceae and Lachnospiraceae families in comparison to those in healthy controls (30, 31, 33). This may indicate that patients with nosocomial diarrhea not due to CDI are also susceptible to development of CDI once they are exposed to C. difficile spores. It also suggests that CDI itself did not much alter the gut microbial composition (31). For mice that were given clindamycin to render them susceptible to CDI development, luminal samples and biopsy specimens generally confirmed the findings for humans and demonstrated a decreased species richness (34). Mice without antibiotic preexposure, and therefore with an undisturbed microbiota, do not develop CDI symptoms after administration of C. difficile spores (34). Also, a microbiota dominated by Proteobacteria was demonstrated for mice with CDI, instead of a Firmicutes- and Bacteroidetes-dominated microbiota like that found in healthy mice (34, 35).
Alterations in gut microbial composition in C. difficile carriers are less well described but may give more insight into the mechanisms that allow for colonization while protecting against the development of overt disease. One of the few available studies reports a decreased species richness and decreased microbial diversity not only in samples from 8 CDI patients but also in samples from 8 asymptomatic carriers compared to those in samples from 9 healthy subjects (29). However, the structures of the microbial communities were significantly different among CDI patients and carriers, and therefore it is suggested that the absence or presence of certain bacterial taxa is more important in determining the development of CDI or C. difficile colonization than the diversity or species richness alone. Fewer Proteobacteria and a larger proportion of Firmicutes and Bacteroidetes were found for carriers than for CDI patients, so this distribution more closely resembled that of healthy individuals (29). Another study of 98 hospitalized patients (including 4 CDI patients and 4 C. difficile-colonized patients) showed that compared to that in CDI patients, a higher level of Clostridiales family XI incertae sedis, Clostridium, or Eubacterium was found just before C. difficile colonization was detected, also supporting the notion that the presence of certain bacterial taxa is important for preventing overgrowth or progression from colonization to overt infection (36). Evidence from murine studies also indicates that colonization with certain bacterial taxa may prevent the progression from colonization to CDI; mice precolonized with a murine Lachnospiraceae isolate showed significantly reduced C. difficile colonization (37). Similarly, administration of Clostridium scindens to antibiotic-treated mice was associated with resistance to CDI (38). Moreover, in antibiotic-exposed mice challenged with C. difficile spores, different patterns of microbiota composition were seen for those that developed severe CDI symptoms versus animals that became only colonized by C. difficile (35). In the first group, a shift toward Proteobacteria was noted, while the latter group had a microbiota that was dominated by Firmicutes (including Lachnospiraceae), resembling that of mice who had not been exposed to antibiotics. The presence of a Firmicutes-dominated microbiota seemed to be protective against the development of clinical symptoms in this experiment (35).
Interestingly, a recent longitudinal study of a C. difficile-colonized infant showed important changes in microbiota composition during weaning. An increase in the relative abundance of Bacteroides, Blautia, Parabacteroides, Coprococcus, Ruminococcus, and Oscillospira was noted, suggesting that these bacterial genera likely account for the expulsion of C. difficile (39).
In conclusion, there are only a few studies on the intestinal microbiota in patients with asymptomatic C. difficile colonization, which also have very limited sample sizes. However, these studies and findings from mouse studies support the idea that decreased species richness and decreased microbial diversity appear to allow for colonization, although the presence of certain bacterial taxa seems to protect from progression to CDI. Mechanisms by which the microbiome, and in particular the presence of certain bacterial taxa, may offer colonization resistance and protection against infection are described below.
Roles of the Microbiota
Bile acid metabolism.
The first step in establishing C. difficile colonization is the germination of spores. Primary bile acids are known to stimulate this germination process (40). The physiological function of primary bile acids is to assist in digesting fat. To be able to do so, after being produced in the liver, primary bile acids are released into and reabsorbed from the small intestine. However, a small amount of the primary bile acids is not reabsorbed and is passed into the colon. In the colon, these primary bile acids are metabolized into secondary bile acids by certain members of the normal gut microbiota. Secondary bile acids inhibit C. difficile growth (40). The capacity to metabolize primary bile acids into secondary bile acids by the production of bile acid 7α-dehydroxylating enzymes has been shown for members of the Lachnospiraceae, Ruminococcaceae, and Blautia families, all of which belong to the phylum Firmicutes (28, 41). A disruption in the intestinal microbiota and depletion of Firmicutes may therefore cause an increase in primary bile acids and a decrease in secondary bile acids. This was shown in antibiotic-treated mice, in which loss of members of the Lachnospiraceae and Ruminococcaceae families was found to be correlated with a significant loss of secondary bile acids (28). More specifically, this was also shown for one of the members of the Lachnospiraceae family, C. scindens; the administration of this bacterium was shown to restore physiological levels of secondary bile acid synthesis (38). Loss of secondary bile acids and an increase in primary bile acids create a favorable environment for C. difficile. Support for the role of bile acid metabolism in susceptibility to C. difficile colonization is obtained from both in vitro and in vivo studies. In vitro, spores were able to germinate in the presence of bile acid concentrations found in feces of CDI patients; however, spore germination and vegetative growth were inhibited in the presence of bile acids at concentrations found in patients after fecal microbiota transplant (FMT) or in mice resistant to C. difficile (28, 42). In vivo, significantly higher levels of primary bile acids and lower levels of secondary bile acids were found in feces from CDI patients than in those from controls, especially for patients with a recurrent CDI episode (43). Notably, the amount of germination in response to bile acids seems to vary between strains, which may be related to mutations in the CspC germinant receptor that recognizes the primary bile acids (42). A C. difficile mutant completely deficient in the CspC receptor gene was demonstrated to cause less severe clinical symptoms in a hamster model (40).
Other mechanisms.
Apart from the altered bile acid composition, other mechanisms also induced by disruptions of the microbiota are suggested to play a role in conferring susceptibility to C. difficile.
First, disruptions in the microbiota that lead to diminished production of short-chain fatty acids (SCFAs) may be important. SCFAs are produced from dietary and host-derived carbohydrates, mainly by Lachnospiraceae and Ruminococcaceae, the families that were less abundant in CDI patients and carriers. They may have an effect on colonization resistance through reducing the luminal pH (and thereby creating an unfavorable environment for C. difficile) (44) and stimulating the defensive barrier, as one of the SCFAs (butyrate) is the main energy source of the gut epithelium (45, 46). Amino acids may also play a role in susceptibility to C. difficile colonization, as they can enhance germination in the presence of secondary bile acids and may influence the immune system. Moreover, the digestion of carbohydrates in the gut may have an impact on susceptibility to CDI development. The Bacteroidetes are mainly responsible for this carbohydrate digestion, which results in production of substrates essential for homeostasis of colonocytes (47). A reduction in the level of Bacteroidetes may therefore have a negative impact on colonic health.
Besides the indirect mechanisms described above, the microbiota may also have direct resistance mechanisms against C. difficile. These include competition for niches and nutrients and the production of antimicrobials (48, 49).
Roles of the Immune System
Innate immunity.
The precise protective factors of innate immunity that prevent colonization and progression to CDI are unknown but are probably less important than the role of the microbiota and bile acid metabolism. Virulence factors of C. difficile induce a rapid innate immune response that results in an inflammatory response which is necessary to induce adaptive immunity.
CDI is characterized by a severe intestinal inflammatory response in which neutrophils infiltrate the mucosa. TcdA and TcdB play an important role in eliciting this inflammatory response (50). After epithelial barrier disruption, TcdA and TcdB trigger inflammatory signaling cascades through activation of NF-κB, AP-1, and inflammasomes, and they stimulate production of proinflammatory cytokines and chemokines in epithelial cells. This promotes the recruitment of immune cells, including neutrophils, and induces the production of defensins. Surface proteins also trigger an innate immune response. Challenge of macrophages with C. difficile surface proteins (surface layer proteins [SLPs]) leads to production of proinflammatory cytokines, such as tumor necrosis factor alpha (TNF-α), interleukin-1β (IL-1β), and IL-8 (51).
Additionally, C. difficile SLPs interact in vitro with Toll-like receptor 4 (TLR4), leading to dendritic cell (DC) maturation, robust Th1 and Th17 responses with production of gamma interferon (IFN-γ) and IL-17, and a weak Th2 response leading to antibody production (52). Ryan et al. showed that TLR4- and myeloid differentiation primary response protein 88 (MyD88)-deficient mice were more prone to C. difficile infection (53). The C. difficile flagellin FliC also activates an innate immune response via its interaction with TLR5, inducing activation predominantly of p38 mitogen-activated protein kinase (MAPK) and, to a lesser extent, NF-κB, resulting in upregulation of the expression of proinflammatory cytokine genes and the production of proinflammatory factors (54, 55). In vivo, Batah et al. showed a synergic effect of C. difficile flagellin and toxins in inducing mucosal inflammation (56).
In summary, the innate immune response induces an inflammatory response which promotes an adaptive immune response with memory and long-lasting immunity (see below), but its effects on C. difficile colonization are unknown.
Adaptive immunity.
Adaptive immunity against C. difficile colonization or CDI has been studied mainly for its antibody-mediated response, whereas the role of the cell-mediated immune response remains unknown.
Serum antibodies against somatic antigens and surface components have been found in asymptomatic carriers and patients who recovered from CDI (57, 58), which suggests that surface proteins induce an immune response and modulate disease outcome. Vaccination assays with these proteins have been performed in animal models. Parenteral or mucosal vaccination with the S-layer proteins led to specific antibody production but only partial protection in the hamster model (59, 60). Immunization studies with Cwp84 and the flagellar proteins FliC and FliD administered to animals by the mucosal route resulted in a significant decrease in intestinal C. difficile colonization in the mouse model and partial protection in the hamster model (61, 62). Likewise, Ghose et al. immunized mice and hamsters intraperitoneally with FliC adjuvanted with alum, inducing a high circulating anti-FliC IgG response in animal sera and full protection in mice against the clinical 072/NAP1 strain but only partial protection in hamsters against the 630Δerm strain (63). All these results suggest that antibodies against C. difficile surface proteins have a protective role against colonization. At the moment, studies with surface protein-based vaccines to prevent colonization in humans are lacking.
Antibodies to TcdA and TcdB do not protect from colonization, but they influence disease susceptibility and, subsequently, the progression from colonization to CDI. Kyne et al. studied anti-TcdA IgG antibody levels in patients who became colonized after C. difficile exposure. They found that patients who remained asymptomatically colonized had greater increases in anti-TcdA IgG antibodies than patients who progressed from colonization to CDI (64).
Monoclonal antibody (MAb)-based passive immunotherapy directed to toxins was able to protect hamsters from CDI. In humans, two MAbs, one targeting TcdA (actoxumab) and another targeting TcdB (bezlotoxumab), were tested in human clinical trials aimed at the prevention of recurrent disease (65). Bezlotoxumab prevented approximately 40% of recurrences. A recently published hypothesis suggested that this reduction in recurrences is presumably due to limiting epithelial damage and facilitating rapid microbiome recovery (66), suggesting that reduced (re)colonization may be an important factor, although this should be explored further. Currently, two pharmaceutical firms (Pfizer and Valneva) have vaccine clinical trial development programs, with the two toxins (toxoids or toxin fragments) but no colonization factors as antigens (67); Sanofi Pasteur recently announced the cessation of its vaccine development program, which was also based on toxin antigens alone. Therefore, these vaccines protect against the toxic effects of C. difficile on the intestinal mucosa and can thereby hinder the progression from colonization to CDI.
In conclusion, a rapid innate immune response induces adaptive immunity to CDI, for which the antibody-mediated response is best understood. Antibodies against C. difficile surface proteins are thought to protect against colonization, while antibodies against C. difficile toxins protect against disease, directly by a toxin neutralizing effect and possibly also indirectly by limiting epithelial damage and restoring colonization resistance.
HUMAN SOURCES OF C. DIFFICILE
Patients with CDI can shed C. difficile not only during the diarrheal episode but also after completion of therapy. In a study of 52 patients receiving treatment for CDI, samples from stool, skin, and environmental sites were cultured for C. difficile before treatment, every 2 to 3 days during treatment, and weekly after therapy was completed (68). Prior to treatment, 100% of stool samples and approximately 90% of skin and environmental samples were culture positive for C. difficile. Stool cultures became C. difficile negative in most patients by the time diarrhea resolved at a mean of 4.2 days. However, at the same time, skin and environmental contamination levels with C. difficile remained high, at 60% and 37%, respectively. In addition, stool detection of C. difficile was 56% at 1 to 4 weeks posttreatment among asymptomatic patients recovering from CDI. Moreover, 58% had skin contamination with C. difficile 1 to 4 weeks after completion of treatment, and 50% had sustained environmental shedding. Persistent skin and environmental contamination was associated with receipt of additional antibiotic therapy. Prior to treatment, the mean density of C. difficile in stool samples was significantly higher than that at the time that the diarrhea resolved, at the end of treatment, and at 1 to 6 weeks posttreatment. This study highlights that patients with CDI can be a source of C. difficile spores and that they can potentially transmit C. difficile to other patients even after diarrhea has resolved. In addition, similar to the case in animal models, continued antibiotic treatment can trigger a “supershedder” state in patients, in which there is C. difficile overgrowth and excretion of high concentrations of spores (69).
CDI was historically regarded as a health care-associated infection transmitted primarily (directly or indirectly) by symptomatic patients, but a growing body of evidence demonstrates that asymptomatic carriers can also transmit the disease.
One study using multilocus sequence typing (MLST) could link only 25% of patients with symptomatic CDI to a previously identified CDI patient (1). A follow-up study of the same large patient cohort (>1,200 cases) used whole-genome sequencing and was able to link, at most, only 55% (and more likely only 35%) of new cases to previous patients with CDI (3). A much smaller study (∼50 cases) using multilocus variable-number tandem-repeat analysis (MLVA) found that only 30% of new cases could be linked to previously identified cases (2). One could argue that the inability to link new cases to previous ones might be caused by patients with CDI who are clinically undetected. However, strict criteria were used to determine which samples should be tested for CDI in the large UK study (1, 3); although the study used a toxin EIA, which is not as sensitive as a reference test, repeat sampling was carried out according to clinical suspicion of CDI. Depending on the reference test used, the sensitivity of toxin EIA is approximately 60 to 85%, which means that 15 to 40% of patients with CDI may go undetected. Nonetheless, this does not account completely for the 45 to 75% of cases that were not closely linked to symptomatic patients (1, 3). This raises the question of what source(s) accounts for approximately half of new CDI cases. Curry et al. examined patients for C. difficile carriage who were selected to undergo screening for vancomycin-resistant enterococci. They found that 29% of CDIs could be linked to asymptomatic C. difficile carriers (2).
As asymptomatic carriers and the associated shedding of spores usually go undetected because of a lack of routine screening, they can play a role in spread of C. difficile to the environment and other patients. Although transmission events from one individual asymptomatic carrier may be rare, as shown in a relatively small study (15), asymptomatic carriers may still importantly contribute to the transmission of the disease, as they likely outnumber symptomatic CDI patients. A recent study showed that 2.6% of patients who were not exposed to C. difficile-colonized patients developed CDI, while this percentage increased to 4.6% for patients who were exposed (70). Unfortunately, however, the case definition of CDI in this study was based on detection of a toxin gene rather than toxin, so overdiagnosis of true cases likely occurred. Asymptomatic carriers who are colonized at admission appear to contribute to sustaining transmission in the ward. Already in 1992, it was recognized that C. difficile strains introduced to the ward by asymptomatic carriers were important sources of onwards health care-associated transmission (71), although definitive proof of linkage was hampered by use of a nonspecific typing technique. More recently, using an epidemiological model of C. difficile transmission in health care settings, Lanzas et al. confirmed that patients colonized on admission likely play a significant role in sustaining ward-based transmission (72).
ANIMAL AND ENVIRONMENTAL SOURCES OF C. DIFFICILE
Animals
Similar to that in humans, CDI or asymptomatic carriage can occur among domestic, farm, and wild animals (73–80). Carriage rates in these studies range from 0 to 100%. These varied observed rates may be related to different culture methodologies and different study settings. Much of this subject has been reviewed in this journal, but new information has emerged on possible transmission from domestic and farm animals (81, 82).
C. difficile can cause diarrhea in domestic companion animals, such as dogs and cats, but asymptomatic transient carriage of C. difficile by household pets is common (11 to 40%) (73, 78, 83, 84). However, many of these studies did not analyze isolates from humans and pets within the same household. A recent study examined the potential for transmission to pets from 8 patients with recurrent CDI (85), but in that study C. difficile was not found in any of the pets. In contrast, Loo et al. studied 51 families with 15 domestic pets that included 9 cats, 5 dogs, and 1 bird (86). During follow-up visits, toxigenic C. difficile was found in cultures of 2 cats and 2 dogs. Probable transmission occurred in 3 of the 15 domestic pet contacts. None of the domestic pets had diarrhea. Typing by pulsed-field gel electrophoresis (PFGE) showed that the profiles of all 4 domestic pet isolates were indistinguishable or closely related to those of their respective index patients. It is conceivable that household pets can serve as a potential source of C. difficile for humans.
Transmission from farm animals to humans has been examined by whole-genome sequencing of 40 Australian ribotype 014/NAP4 isolates of human or porcine origin (87). A clonal relationship with one or more porcine strains was demonstrated among 42% of human strains, underscoring the potential for interspecies transmission. Similar findings were obtained in a study of 65 C. difficile 078/NAP7 isolates collected between 2002 and 2011 that included 12 pairs of human and pig isolates from 12 different pig farms (88). Five (41.7%) of the 12 farmer-pig pairs were colonized with identical and nearly identical C. difficile clones (88); the remaining 7 (58.3%) farmer-pig isolate pairs were not clonal, suggesting exposure to different sources, such as the environment.
Food
With reports that C. difficile can be detected among farm animals, studies of C. difficile detection in retail food products appeared.
Studies from Canada and the United States report that C. difficile can be recovered from retail meat, including ground beef, ready-to-eat beef, ground pork, ground turkey, pork sausage, summer sausage, pork chorizo, and pork braunschweiger, with prevalences ranging from 20 to 63% (89–92).
However, the prevalences of C. difficile in retail meat products were lower in European countries, ranging from 0 to 6.3% (93–95). The observed differences in prevalence of C. difficile culture positivity in retail meats in North America and Europe are striking. These may be related to seasonal and temporal changes or may be true observed geographical differences.
Using both quantitative and enrichment culture methods, Weese et al. sought to provide a measure of the degree of contamination of 230 samples of retail ground beef and pork (96). C. difficile was isolated from 28 (12%) samples, and notably, approximately 70% of these samples were positive by enrichment culture only. Among the samples that were positive on direct culture, the concentrations of spores ranged from 20 to 240 spores/g. Although the infectious dose of C. difficile is not known, these findings suggest that while C. difficile can readily be recovered from retail meat products, the concentration of C. difficile spores is low.
Stabler et al. investigated the MLST profiles of 385 C. difficile isolates from human, animal, and food sources and from geographically diverse regions (97). Animal and food strains were associated with the ST-1 and ST-11 profiles, and these strains have been associated with CDI outbreaks in humans. Although the majority of C. difficile isolates recovered from retail food products are toxigenic and are of the same ribotypes or MLST types as those of human isolates, there have not been any human CDI cases that have been confirmed to be foodborne in origin.
Environment
C. difficile spores can survive in the environment for months or years due to their resistance to heat, drying, and certain disinfectants. Within hospitals, the surface environment is frequently contaminated with C. difficile. C. difficile has been cultured from many surfaces, including floors, commodes, toilets, bedpans, and high-touch surfaces, such as call bells and overbed tables (14, 98). The frequency of environmental contamination depends on the C. difficile status of the patient: fewer than 8% of rooms of culture-negative patients, 8 to 30% of rooms of patients with asymptomatic colonization, and 9 to 50% of rooms of CDI patients were found to be contaminated with C. difficile (14, 99, 100).
To examine environmental sources outside the health care milieu, al Saif and Brazier undertook a large study in Cardiff, South Wales, of 2,580 samples from various sources, including water, domestic and farm animals, soil, raw vegetables, surface samples from health care facilities, veterinary clinics, and private residences (101). One hundred eighty-four (7.1%) samples were positive. Water samples gave the highest yield of culture positivity (36%), followed by soil (21%) and health care environments (20%). C. difficile was found in 59% of lawn samples collected in public spaces in Perth, Australia, and toxigenic ribotypes 014/NAP4 and 020/NAP4 were predominant (102). A Canadian study demonstrated that C. difficile was found in 39% of sediments sampled from rivers connected to the discharge effluent pipes of wastewater treatment plants (103). The most common PCR ribotype was 078/NAP7.
In summary, C. difficile has been isolated from animals, retail food, and the environment. Based on results obtained by ribotyping and whole-genome sequencing techniques, there appears to be interspecies and environmental transmission, but the directionality of the transmission remains to be elucidated.
EPIDEMIOLOGY OF ASYMPTOMATIC COLONIZATION
After the discussion of possible sources of C. difficile and underlying mechanisms of colonization, a description of the epidemiology of colonization, including the prevalence of colonization rates among different populations, is essential.
Infants (0 to 24 Months)
Asymptomatic colonization rates in neonates and infants (<2 years) are widely reported as high but range from 4 to 71% (18, 104–108). Although the clinical relevance of C. difficile colonization in infants is considered less significant due to low rates of disease in this population (109), its potential as a transmission reservoir for adult populations remains.
An early study researching the prevalence of C. difficile in the neonate population found that approximately 30% of all newborns were asymptomatically colonized within their first month of life (18). However, these data included four specimens deemed positive but with no identifiable organism, only toxin. Nonetheless, the transient nature of colonization at this early stage was highlighted, with only 4 of 10 babies who were culture positive in the first week of life remaining positive at 14 and 28 days. A more recent review corroborated these early figures, pooling data from 5,887 subjects to determine a colonization rate of approximately 35% of infants under 1 year of age (105). This large-scale analysis suggests that colonization peaks at 6 to 12 months before substantially decreasing toward adult rates. Although that major review provides a valuable assemblage of data, the variability across methodologies used by the included studies should be taken into consideration.
Geographical differences in infant colonization rates have been identified, with one study indicating variances of 4 to 35% across Estonian and Swedish infant populations (108). The colonization rate was inversely associated with an elevated presence of inhibitory lactobacilli in Estonian subjects, which may be determined by variations in diet and environmental exposure. A U.S. study of hospitalized infants demonstrated a 20% colonization rate (110), whereas Furuichi et al. found no evidence of C. difficile colonization among Japanese newborns (111). However, the Japanese data were based on culture only, with no attempt to utilize an EIA or NAAT to detect low levels of organism. These studies emphasize the variable epidemiology among diverse geographical populations.
The source of infant colonization is uncertain, with suggestions that the presence of C. difficile in the urogenital tract implicated vaginal delivery as a potential route of transmission to neonates (112). However, later work contradicted this suggestion, failing to detect any C. difficile-positive vaginal swabs from postpartum mothers (18, 104). Molecular analysis of both infant and environmental isolates demonstrated likely acquisition from environmental sources and patient-to-patient transmission (113).
Infants are rarely diagnosed with CDI. Bolton and colleagues found that almost 50% of colonized infants carried toxin-positive strains but showed no sign of diarrhea, suggesting that although the relevant toxin genes may be present, they may be minimally (or not) expressed and so fail to cause disease; alternatively, absent or immature toxin receptors may explain the infrequency of CDI despite high colonization rates (18). However, understanding toxigenic strain colonization rates may provide greater insight into the relevance of this population as a reservoir for transmission to adults. Isolates from infants have shown a predominance of ribotypes associated with CDI (106). Adlerberth et al. found that 71% of colonized infants had toxigenic strains, with more than half identified as ribotypes 001/NAP2 and 014/NAP4, which can cause endemic CDI (114). A comparison of C. difficile strains in children (<30 months) and those circulating in the adult (≥18 years) CDI population within the same institution determined nine shared sequence types among the 20% asymptomatic pediatric subjects (115). This may further implicate infants as a potential reservoir for C. difficile dissemination; nonetheless, no direct transmission events were documented in that limited pilot study. Potential community-based transmission from infant carriers to the adult population was alluded to in a longitudinal study demonstrating colonization in all 10 infants at some point in the first year of life, with 3 infants colonized for 4 to 9 months (116).
Children (2 to 16 Years)
A meta-analysis of studies examining pediatric C. difficile epidemiology reported an asymptomatic colonization rate of 15% for children older than 1 year of age, with the prevalence reduced to 5% in those older than 2 years of age (117). One explanation for the reduction in colonization rates after infancy is that, by 12 months, the distribution of gut flora begins to closely resemble that of a healthy adult, providing a colonization resistance effect. Nonetheless, contemporaneous studies have reported higher rates (up to 30%) of asymptomatic colonization among noninfant pediatric populations (111, 118, 119). Similarly, Merino and colleagues found that around a quarter of U.S. children aged 1 to 5 years were colonized asymptomatically by C. difficile (120). By using a molecular identification method to classify groups by the presence of the toxin A gene (tcdA), the toxin B gene (tcdB), and the binary toxin genes (cdtA/B), they found that although 3/37 asymptomatically colonized children harbored a strain with the toxigenic genes (tcdA and tcdB), none carried the binary toxin genes (cdtA/cdtB). Ferreira et al. (121) found low levels of toxigenic C. difficile in Brazilian children, arguing that the majority of cases of acute diarrhea in this cohort are likely to be associated with entirely different enteropathogens. These epidemiological variations should be considered in the context of widely differing enteric pathogen populations between developing and developed countries.
Healthy Adults
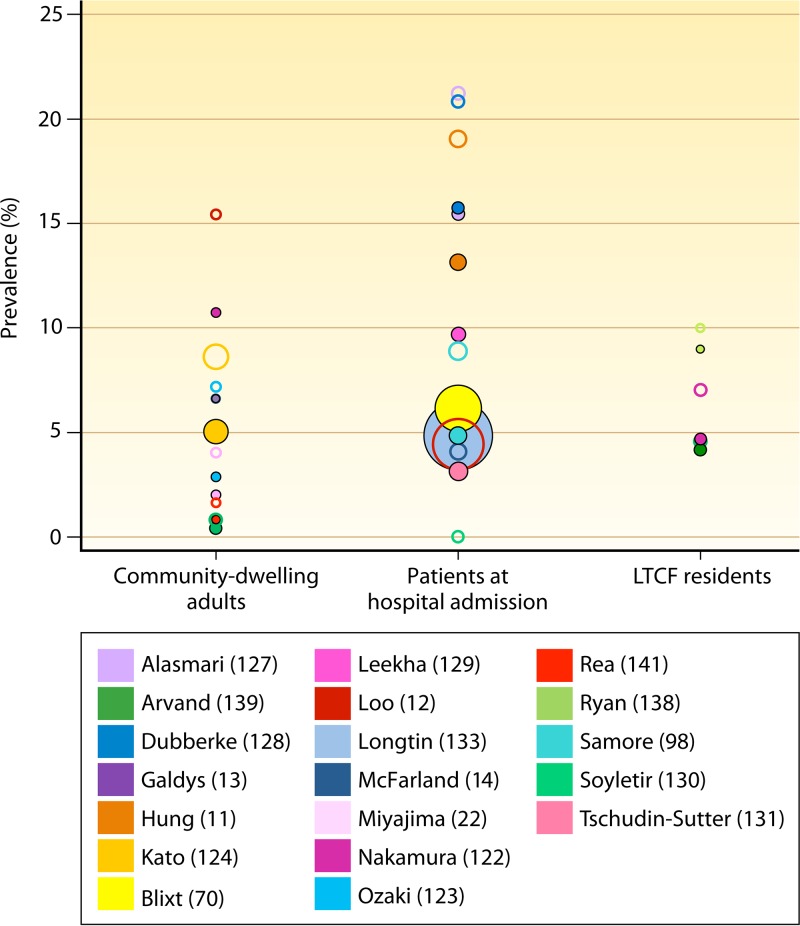
Previous studies indicated that the asymptomatic colonization rates among healthy individuals range from 4 to 15% (Fig. 2). However, these studies were often based on point prevalence detection of C. difficile, making the true carriage rate difficult to ascertain. Nevertheless, such a prevalence of even transient colonization by C. difficile suggests significant potential for exposure to the bacterium in the community setting among healthy populations.
FIG 2.
Prevalence of colonization among community-dwelling adults, patients at hospital admission, and LTCF residents. Hollow circles represent C. difficile colonization (including nontoxigenic and toxigenic strains) prevalences, and solid circles represent toxigenic C. difficile colonization prevalences. Sizes of the circles represent sample sizes. The different colors represent the different studies (see the legend). See references 11 to 14, 22, 70, 98, 122 to 124, 127 to 131, 133, 138, 139, and 141.
It is important to note the proportions of toxigenic strains because of their importance for transmission and potential for causing CDI. Work carried out among healthy Japanese adults reported a high colonization rate (15.4%), with around 70% of colonized individuals harboring toxigenic strains (122). However, a more recent U.S. study discovered that all strains contributing to a 6.6% asymptomatic colonization rate were toxigenic (13). This rate is higher than those seen in large patient transmission studies (2, 12, 71), suggesting that the healthy adult data may be skewed by relatively small study cohorts (n = 149 [122] and n = 139 [123]).
Ozaki identified matching PCR ribotypes among a cohort of healthy company employees as a potential indication of a shared workplace as a common source or representing human cross-transmission within this cohort (123). In addition, they highlighted the transient nature of colonization, with only 37.5% of individuals demonstrating carriage with the same strain within a follow-up period of 1 year. Galdys et al. also found that approximately 33% of participants remained positive with the same strain in samples submitted 1 month apart (13). Another study used cluster analysis to highlight that although colonization among healthy groups acts as a reservoir for community-acquired CDI, it may only occur infrequently between families (124). Although a previous study implicated the family environment as a source of transmission of C. difficile (125), Kato et al. (124) found only one instance of a shared strain type among family members across 22 families with 1 C. difficile-colonized index patient.
Patients at Admission to Hospital
Patients at admission to a hospital are a considerable reservoir for C. difficile and, importantly, a potential source of nosocomial transmission. Asymptomatic colonization rates among patients at admission to a hospital range from 3 to 21% (11, 12, 14, 98, 126–131) (Fig. 2). A large study by Clabots and colleagues reported that 9.6% of patients admitted to the study ward were colonized; admissions from home had the lowest colonization rate (6%) but nonetheless accounted for the second most prevalent method of C. difficile introduction due to their larger numbers (71). A major Canadian study of over 5,000 admissions demonstrated a lower C. difficile prevalence rate, with 4.05% of patients colonized asymptomatically (132); this rate was very similar in a more recent large-scale study (4.8%) (133). Kong et al. suggested that these low rates may be due to regional distribution, as the majority of C. difficile-colonized patients in this multi-institution study were based in hospitals with larger proportions of NAP1-associated CDI (132).
A recent meta-analysis of studies reporting toxigenic C. difficile colonization rates upon hospital admission reported a rate of 8.1% among almost 9,000 patients (134). Although this overall rate provides a strong insight into the prevalence of toxigenic C. difficile colonization, the meta-analysis excluded certain large studies due to methodology differences in order to attain maximum compatibility of the data sets. Such exclusions may well have had an impact on the reported colonization rates.
Two considerably smaller studies reported higher C. difficile colonization rates, highlighting the potential for sampling bias. Hung et al. found that 20% of 441 patients admitted to a Taiwanese hospital were C. difficile positive, with two-thirds of these carrying toxigenic C. difficile (11), while Alasmari and colleagues reported a rate of 21.2% (n = 259), with almost 75% of carriers harboring toxigenic strains (127). Prior health care exposure was very common and not statistically different between patients colonized with a toxigenic strain and noncolonized patients (prevalences of prior health care exposure were 90% and 85%, respectively). However, Leekha and colleagues demonstrated recent health care exposure as a significant risk factor, reporting a 9.7% toxigenic C. difficile colonization rate on admission (129).
Hospitalized Patients
Determination of hospital C. difficile colonization rates is helpful for understanding the potential for nosocomial transmission. Rates of asymptomatic acquisition during hospital admission have generally been demonstrated to range from 3 to 21% (11, 12, 14, 71, 98, 130, 135, 136). McFarland et al. were able to separate their study cohort into groups with early (<2 weeks) and late (>2 weeks) acquisition relative to hospital admission (14). The majority of patients had early colonization, with a significant increase in disease severity associated with subjects progressing to CDI after late acquisition. However, this understandably correlates with significant increases in other recognized CDI risk factors, including exposure to antibiotics and multiple comorbidities.
Nevertheless, a study that involved mainly HIV-positive (and young) participants demonstrated that all 44 C. difficile-negative patients remained noncolonized throughout the period of hospitalization (137). This study population was largely accommodated in single rooms, which may have diminished the impact of positive carriers on transmission. In addition, Guerrero et al. demonstrated that rectal and skin swabs from hospitalized, colonized patients yielded much lower counts than those from subjects with diarrhea, suggesting a reduced transmission potential associated with colonized individuals (8). Furthermore, Longtin and colleagues were able to show a significant decreasing trend in health care-associated CDI cases after the implementation of contact isolation precautions for colonized patients identified upon admission (133).
Length of hospital stay, not surprisingly, is related to the risk of C. difficile colonization: a large study reported a 50% acquisition rate for patients with a length of stay greater than 4 weeks. For patients who screened negative on admission, average durations of hospital stay before a positive C. difficile culture ranged from 12 to 71 days (11, 14, 136).
Patients in LTCF
Previous reports of C. difficile colonization rates among residents of long-term health care facilities (LTCF) have ranged widely (4 to 51%) (138–141). A major caveat in the study reporting the highest colonization rate was that it was conducted during a CDI outbreak (142). Furthermore, two studies that found high rates examined relatively small cohorts (n = 68 [142] and n = 32 [140]). Interestingly, data from the work of Riggs and colleagues showed that 37% of colonized residents harbored the outbreak strain (RT027/NAP1) asymptomatically (142), while Rea et al. also isolated a range of outbreak-associated strains, including RT027/NAP1, 078/NAP7, 018, 014/NAP4, and 026, from an asymptomatic group (141). These rates must be considered with caution, as the presence of an epidemic strain in a given community is likely to inflate asymptomatic colonization rates. For example, the asymptomatic colonization rates before and after a CDI outbreak were reported to be 6.5% and 30.1%, respectively (P = 0.01) (143).
Arvand et al. identified colonization rates that ranged from 0 to 10% across 11 nursing homes in Germany and concluded that additional factors influenced the asymptomatic colonization prevalence, including antibiotic exposure rates, comorbidities of residents, and individual facilities' infection control procedures (139). Ryan et al. found similar distributions, likely reflecting differing resident morbidities and regional strain prevalences (138). Arvand and colleagues found that nursing home residents were 10 times more likely to be colonized with toxigenic strains than with nontoxigenic types (139), similar to the results of other reports (122, 138) demonstrating the presence of the toxin genes tcdA and tcdB in 70% of strains from the asymptomatic cohorts. Conversely, Rogers et al. found only toxigenic C. difficile in those with asymptomatic colonization (140). In one study where follow-up samples from colonized residents (1 to 3 months after initial screening) were tested, 10/12 individuals displayed persistent carriage of the same C. difficile PFGE type, possibly indicating a less transient nature among individuals in LTCFs (142). These data demonstrate the variability across studies, which likely reflects multiple confounders, including the stringency of infection control procedures, strain type, antibiotic use, comorbidities, and issues such as single-room versus shared accommodation.
HCWs
Asymptomatic gut colonization of health care workers (HCWs) is a potential but unproven source of C. difficile transmission. HCWs may well have a role in transmission due to their frequent patient contact, but this may simply be due to transient hand contamination.
Kato et al. carried out a large-scale study of Japanese groups, including two cohorts of HCWs, and identified 4.2% of hospital employees as colonized by C. difficile (124). Van Nood et al. attempted to clarify whether intestinal colonization was related to the presence of spores on HCW's hands. Of 50 Dutch hospital workers, 0% and 13% were C. difficile culture positive based on handprint agar plates and fecal samples, respectively (144). Also, in demonstrating that colonization rates were similar across staff working on wards with and without CDI patients, they highlighted the potential for acquisition and/or transmission by means other than HCW's hands. Unfortunately, no strain typing was carried out in this study, and definitive transmission relationships therefore could not be determined.
Several studies demonstrated low to nonexistent intestinal colonization levels, with 0 to 1% of health care workers being C. difficile positive (145–148). Friedman et al. did, however, point out the voluntary nature of study recruitment, in which case HCWs with poorer hand hygiene may have opted out, leading to a nonrepresentative cohort (146). Furthermore, these studies sampled subjects only once.
Landelle et al. detected C. difficile spores on the hands of 24% of HCWs who were directly caring for CDI patients (149). Other studies have also shown that after caring for patients with CDI, the proportions of health care workers with hand contamination when gloves are not worn range from 8 to 59% (14, 150). This highlights the challenge in determining the relative importance of patients' fecal C. difficile burden versus HCW hand or environmental contamination as a potential source of transmission.
Duration of Carriage
There is a paucity of research reporting the duration of asymptomatic C. difficile carriage. Large-scale longitudinal studies are required to investigate length of carriage and the associated determinants. Nonetheless, some research does provide follow-up data on asymptomatic hosts.
Several studies have assessed the duration of short-term carriage (98, 151, 152). During weekly follow-up of 32 asymptomatic subjects, Samore et al. found that 84% remained positive until discharge, although the mean duration of sampling was only 8.5 days (range, 7 to 29 days) (98). Johnson et al. continued surveillance on 51 asymptomatic patients with long-term hospital stays for up to 9 weeks, with no development of CDI during this time (151). Later, on investigating treatment efficacies for asymptomatic carriage, the same investigators found that 60, 80, and 100% of carriers had lost C. difficile colonization after 40, 70, and >90 days, respectively (in the absence of a targeted intervention) (152). Contemporaneous research demonstrated that only two of six healthy, colonized volunteers retained the same strain 1 month later (13). Although the data are limited, they indicate the short-term, transient nature of symptomless C. difficile colonization, at least in the absence of repeated exposure to C. difficile risk factors, such as antibiotics. Nonetheless, variation among patient cohorts and environments must be considered.
Longitudinal studies of healthy Japanese populations have monitored asymptomatic carriers among students, employees, and hospital workers. Kato et al. performed a longitudinal surveillance study of 38 asymptomatic carriers for 5 to 7 months and determined that 12 (31.6%) remained C. difficile positive during this time (124). Half of these maintained the same PFGE type, while 5 had acquired a new strain. The remaining participant retained the original strain and acquired a new type. Therefore, only 18.4% of participants retained the same strain after 6 months, again implying a high rate of transient colonization. Nonetheless, analysis of a single, 6-month follow-up sample does not permit in-depth analysis of the dynamics of carriage, and it remains unclear if carriage was lost after a few days, weeks, or months. Testing of 18 asymptomatic subjects in 3-month intervals over a 1-year period found that 10 participants (55.6%) tested positive for C. difficile on only a single sampling occasion, indicating loss of carriage within 3 months; only 3 participants (16.7%) were persistently colonized throughout the study (123). This further supports the suggestion that intestinal colonization in healthy adults is largely a transient phenomenon. Of those testing positive in three or four instances, 5 individuals harbored the same strain on consecutive sampling occasions (3 students and 2 employees), potentially indicating an element of cross-transmission within cohorts sharing common physical areas, and even the possibility of a subject contaminating his or her own environment and reacquiring the strain later.
A recent study of healthy subjects from Pittsburgh, PA, provided an analysis of participant demographics and dietary data in relation to the duration of C. difficile carriage (13). No correlations were found between previous CDI, prior antibiotic use, health care exposure, race, ethnicity, consumption of uncooked meat or seafood, and duration of carriage.
Ribotype-Specific Differences
Determining the prevalences of ribotypes among asymptomatically colonized individuals may help to improve the understanding of potential sources of C. difficile, and specifically which toxigenic and common strain types originate from such individuals. Studies of colonizing strains have shown a broad distribution of PCR ribotypes, with reports of 37 ribotypes among 94 isolates (124) and 29 diverse sequence types from 112 carriers (115). While it might be expected that there is a diverse strain distribution among asymptomatically colonized individuals, as with CDI patients the prevalences of individual strain types are likely to vary depending on the virulence potential of specific ribotypes. Nonetheless, the relationship between ribotype prevalence in CDI patients and strain distribution among asymptomatic carriers remains unclear.
In the context of outbreaks, colonization rates by hypervirulent strains appear to be markedly increased. Loo et al. and Riggs et al. found very similar (asymptomatic) colonization rates for PCR ribotype 027/NAP1 strains (36.1% and 37%, respectively) (12, 142). Contemporaneous research highlighted the persistence of PCR ribotype 027/NAP1 in a New York long-term health care facility, where half of the asymptomatic population (19.3% of all residents) carried this strain (153). This is likely to be due to increased prevalence in the patient populations and consequent spore shedding into the environment (154). Interestingly, three of the five asymptomatically colonized patients that developed subsequent CDI harbored the epidemic 027/NAP1 strain, hinting at its potential superiority in progression from colonization to symptomatic disease.
Other ribotypes have also been implicated as dominant colonizing strains. Earlier work reported that 51.7% of asymptomatically colonized elderly patients were positive for ribotype 001/NAP2 on admission, with the remaining 48.3% of colonizers consisting of 12 other ribotypes (155). As ribotype 001/NAP2 was deemed to predominate in Welsh hospitals at the time, this may be as expected. Other prevalent European ribotypes (156), including 012/NAPcr1, 014/NAP4, and 020/NAP4, have also been reported as predominant strains among asymptomatic populations (127, 139).
Conversely, in recent studies covering a period of marked reduction in PCR ribotype 027/NAP1-associated CDI (156), asymptomatic colonization rates of this strain were considerably lower (139, 141). These data were supported by a large-scale UK transmission study (15) which also found no evidence of PCR ribotype 027/NAP1 colonization in hospitalized UK patients; no single strain predominated in this study.
RISK FACTORS FOR C. DIFFICILE COLONIZATION
Clinical and epidemiological risk factors for CDI are well known, but risk factors for colonization with C. difficile have only recently come to attention. An important distinction has to be made between risk factors for being colonized in the community or at admission to a hospital and risk factors for acquiring colonization during hospital admission.
Colonization in a Community Setting
Risk factors for being or becoming colonized in the community are not extensively studied. Clusters of colonized patients with identical C. difficile types have been identified within community settings (e.g., employees or students) and families, indicating cross-transmission from colonized individuals or acquisition from a common source (124). A study of 106 healthy adults in Pennsylvania found no statistically significant differences in patient characteristics or exposures between 7 colonized and 99 noncolonized subjects, but this may have been due to the small sample size (13). Living in the proximity of livestock farms was not found to be a risk factor in a recent study of 2,494 adults in the Netherlands (157). Antibiotic exposure in the 3 preceding months was, however, associated with a 3.7-fold increased risk of C. difficile colonization in the same study (157). A recent study of 338 predominantly healthy infants (≤2 years of age) showed that the risk of C. difficile colonization was increased in those with pet dogs (158).
Colonization at Hospital Admission
Recognition of risk factors for being colonized at admission is important, as patients with these risk factors may introduce and spread C. difficile in the hospital. Epidemiological and clinical risk factors for (overall or toxigenic) colonization at the time of admission include recent hospitalization (15, 129, 132), chronic dialysis (129), corticosteroid/immunosuppressant use (15, 129, 132), gastric acid suppressant medication (15), and antibodies against toxin B (132) (Table 2). The consistent association between previous health care contact and colonization by C. difficile likely means that hospitals remain important sources of C. difficile, with relationships to host factors at the time of admission (e.g., altered microbiota composition due to antibiotic use) and increased exposure to strains. However, patients colonized at admission may have acquired C. difficile from diverse sources. Notably, the health care-associated C. difficile ribotype 027/NAP1 is found less frequently in carriers at admission than in those who become colonized during admission (128, 132).
TABLE 2.
Studies investigating risk factors for C. difficile colonization at hospital admission or acquisition of C. difficile during admissiona
| Condition | Identified risk factor | Reference(s) |
|---|---|---|
| Risk factors for colonization at admission | ||
| C. difficile colonization | Previous hospitalization | 15, 132 |
| Previous CDI episode | 132 | |
| Previous use of corticosteroids or other immunosuppressant medication | 15, 132 | |
| Presence of antibodies against toxin B | 132 | |
| Current loose stools/diarrhea not meeting CDI criteria | 15 | |
| Toxigenic C. difficile colonization | Previous hospitalization | 129 |
| Chronic dialysis | 129 | |
| Use of corticosteroids | 129 | |
| Risk factors for acquiring colonization during admission | ||
| C. difficile colonization | Previous hospitalization | 12 |
| Use of chemotherapy | 12 | |
| Use of proton pump inhibitors or H2 blockers | 12 | |
| Presence of antibodies against toxin B | 12 | |
| Toxigenic C. difficile colonization | TLR4 polymorphism | 11 |
| Cefepime use during admission | 11 |
Studies were included if they were published since 1994, investigated either risk factors for colonization at admission or risk factors for colonization acquisition during admission (studies investigating risk factors for being colonized at a certain time point during hospitalization were excluded), had a sample size of >100 patients, and assessed risk factors by multivariate regression.
Acquiring C. difficile during Hospital Admission
Previous hospitalization in the last 2 months, use of proton pump inhibitors, H2 blockers, or chemotherapy (within the 8 weeks preceding the hospitalization or during hospitalization but before colonization was acquired), and cephalosporin use during admission were significant risk factors for becoming colonized (with toxigenic or nontoxigenic strains) during admission (12, 128) (Table 2). In one study, cefepime use and a Toll-like receptor 4 polymorphism were risk factors for acquiring toxigenic C. difficile colonization during admission (11). The presence of toxin B antibodies was associated with asymptomatic colonization during admission (12). Interestingly, antibodies against toxin B may have a protective effect against the development of CDI. Likewise, compared to patients who acquired C. difficile and subsequently developed CDI, patients who acquired C. difficile colonization but remained asymptomatic had higher levels of IgG antibody against toxin A at the time of colonization (64). These observations may indicate that antibodies and/or acquired immunity (e.g., due to previous hospitalizations) confers resistance to the development of symptomatic CDI (as discussed above). Patients who acquired C. difficile and developed asymptomatic colonization were less frequently colonized with the hypervirulent ribotype 027/NAP1 strain than those who developed CDI (12, 64, 128). This suggests that the virulence of the acquired strain can influence the development of colonization or infection.
Colonization by Toxigenic versus Nontoxigenic Strains
A recent study showed that hospitalized patients colonized by toxigenic strains and nontoxigenic strains do not share risk factors. Risk factors for colonization by a toxigenic strain included a larger number of admissions in the previous year, antimicrobial exposure during the current admission, and the presence of gastroesophageal reflux disease. Risk factors for colonization by a nontoxigenic strain were chronic kidney failure and chronic obstructive pulmonary disease. Unfortunately, the design of the study was cross-sectional, and therefore the period of C. difficile acquisition (i.e., before admission or during admission) could not be established for these patients (159). Another study tried to determine if the type of antibiotics used during admission affects the risk for acquisition of either toxigenic or nontoxigenic C. difficile. That study found that the use of cephalosporins was a risk factor for both conditions: acquisition of a toxigenic strain was associated with the use of cefepime, while the acquisition of a nontoxigenic strain was associated with the use of cefuroxime. Moreover, the use of glycopeptides was a risk factor for acquiring a nontoxigenic strain during admission (11). For patients colonized on admission, associations between classes of antibiotics used and the colonization of either toxigenic or nontoxigenic C. difficile have also been reported, but multivariate analyses to identify independent risk factors have not yet been performed (127).
C. DIFFICILE COLONIZATION AND SUBSEQUENT CDI
One of the major questions at present is the following: do C. difficile-colonized individuals have an increased risk of developing subsequent CDI, or are they protected against disease? A lower risk of subsequently developing CDI was found for C. difficile-colonized patients in a frequently cited but older meta-analysis of four studies (160). The major drawback of that review, however, is that patients colonized by toxigenic or nontoxigenic strains were not analyzed separately; this difference may be important, as 44% of colonized patients in the meta-analysis harbored a nontoxigenic strain. Also, all four studies were performed pre-1994, before the emergence of hypervirulent strains and recognition of community-associated CDI. Furthermore, colonization was determined at different time points: at admission (71, 98); at the start of tube feeding, with patients colonized at admission excluded (161); and after a hospital stay of at least 7 days (151). Colonized patients therefore included some patients that acquired colonization during admission. The risk of the latter patients going on to develop CDI during the hospital stay may be different from that for individuals already colonized at admission. A recent meta-analysis aimed to include studies in which patients were colonized at admission with toxigenic strains only (11, 15, 98, 127, 130, 134, 162–164). However, not all included studies succeeded in obtaining samples within 48 or 72 h of admission (15, 98). Also, a study that included patients at admission to a rehabilitation unit (after an average stay of 30 days in an acute care facility) was included (164). In one study, the distinction between colonization of a toxigenic strain and CDI was difficult to establish, as all patients received a hematopoietic stem cell transplantation and donor lymphocyte infusion; almost all such patients subsequently develop diarrhea. For patients known to carry a toxigenic C. difficile strain, diarrhea may have been falsely attributed to CDI (162). Notwithstanding these limitations, all studies pointed to an increased risk for patients colonized with toxigenic C. difficile at admission to progress to CDI: overall, the relative risk was 5.86 (95% confidence interval [CI], 4.21 to 8.16) (Table 3). Some recent studies were not included in the meta-analysis. A recent large study which screened 3,605 of 4,508 hospital admissions found that patients carrying toxigenic strains on admission were at a much higher risk of developing CDI (CDI rate of 9.4% versus 2.3% for nontoxigenic C. difficile carriers) (70). The risk of CDI in noncolonized patients who were exposed to subjects colonized by a toxigenic strain was also significantly increased (4.6% versus 2.6% for nonexposed patients) (odds ratio for CDI if exposed to carrier, 1.79; 95% CI, 1.16 to 2.76). However, the study appeared to diagnose CDI based on the presence of toxigenic C. difficile strains rather than toxin, so the case incidence is likely to have been overestimated. In turn, the association between colonization by or exposure to toxigenic strains and subsequent CDI may have been exaggerated (70). A much smaller study did not report any CDI cases among 37 patients colonized on admission (128) (Table 3).
TABLE 3.
Studies investigating the risk of development of CDI among patients with toxigenic C. difficile colonization on hospital admissiona
| Study authors (reference) | Country, yr(s) | Setting and patients | Follow-up period | No. of included patients | Prevalence (no. of positive patients/total no. of patients [%]) |
RR for CDI (95% CI) | Remarks | ||
|---|---|---|---|---|---|---|---|---|---|
| Toxigenic C. difficile colonization | CDI among patients with toxigenic C. difficile colonization | CDI among controls | |||||||
| Samore et al. (98) | USA, 1991 | Patients with an anticipated LOS of at least 5 days admitted or transferred to general medical and surgical wards and ICUs | Until discharge | 496 | 24/496 (4.8) | 1/24 (4.2) | 8/472 (1.7) | 2.46 (0.32–18.87) | 90 of 496 samples (18.1%) were not obtained within 72 h of admission |
| Soyletir et al. (130) | Turkey, published 1996 | Patients admitted to a general medical ward with an LOS of at least 48 h | Until discharge | 202 | 0/202 (0) | 0/0 (0) | 0/202 (0) | NA | None of the patients were colonized at admission |
| Gupta et al. (163) | USA and Canada, 2009–2011 | Patients of >60 yr admitted to general medical and surgical units and on antibiotics | Until 30 days after discharge or 60 days in hospital (whichever came first) | 1,099 | 91/1,099 (8.3) | 9/91 (9.9) | 11/1,008 (1.1) | 9.06 (3.86–21.30) | Asymptomatic carriage was diagnosed by culture and REA typing but could have included both toxigenic C. difficile colonization and nontoxigenic C. difficile colonization |
| Alasmari et al. (127) | USA, 2010–2011 | Adult patients with an anticipated LOS of >48 h admitted to general medical and surgical wards | Until 60 days after discharge | 259 | 40/259 (15.4) | 1/40 (2.5) | 2/219 (0.9) | 2.74 (0.25–29.48) | |
| Dubberke et al. (128) | USA, 2010–2012 | Adult patients admitted to medical or surgical wards with an anticipated LOS of >48 h | Until 60 days after discharge | 235 | 37/235 (15.7) | 0/37 (0) | 2/198 (1.0) | NA | Partly the same patient cohort as that in the work of Alasmari et al. |
| Bruminhent et al. (162) | USA, 2011–2012 | Patients admitted to a bone marrow transplant unit for HSCT | Until 100 days after HSCT | 150 | 16/150 (10.7) | 14/16 (87.5) | 23/134 (17.2) | 5.10 (3.36–7.72) | Distinction between CDI and colonization by toxigenic strains is difficult to establish because almost all patients develop diarrhea after HSCT, and CDI testing did not include free toxin detection in all cases |
| Hung et al. (11) | Taiwan, 2011–2012 | Adult patients with an anticipated LOS of at least 5 days admitted to a general medical ward | Until discharge from last hospitalization | 441 | 58/441 (13.2) | 8/58 (13.8) | 6/383 (1.6) | 8.80 (3.17–24.46) | |
| Blixt et al. (70) | Denmark, 2012–2013 | Patients admitted to medical departments at 2 university hospitals | 1 mo (in and outside hospitals) | 3,464 | 213/3,464 (6.1) | 20/213 (9.4) | 76/3,251 (2.3) | 4.02 (2.50–6.44) | |
| Tschudin-Sutter et al. (131) | USA, 2013 | Patients admitted to an ICU within 48 h of hospital admission | Until discharge | 542 | 17/542 (3.1) | 2/17 (11.8) | 6/525 (1.1) | 10.29 (2.24–47.3) | |
Studies were included if they were published since 1994, had a sample size of >100 patients, compared patients with toxigenic C. difficile colonization on admission to controls (patients with nontoxigenic C. difficile colonization and noncolonized patients together). Relative risks were calculated as the risk for toxigenic C. difficile-colonized patients compared to the risk for noncolonized and nontoxigenic C. difficile-colonized patients together and were unadjusted. RR, relative risk; HSCT, hematopoietic stem cell transplantation; CDI, Clostridium difficile infection; LOS, length of stay; ICU, intensive care unit; NA, not available; REA, restriction endonuclease analysis.
Two other recent studies described the risk of developing CDI for colonized intensive care unit (ICU) patients. A study by Tschudin-Sutter et al. with a cohort of 542 ICU patients described a relative risk of developing CDI of 8.6 for patients colonized on admission and a relative risk of 10.9 for patients who became colonized during hospitalization (131). Zhang and colleagues, however, identified 6 patients who were colonized on admission to the ICU, but none of them developed CDI. During the study period, 4 patients developed CDI, but all were not colonized on admission to the ICU (165). These conflicting results are probably caused by small sample sizes, a relatively rare outcome event (3 versus 0 colonized patients who progressed to CDI), and different predominant strains.
From the above-mentioned observations, we can conclude that patients asymptomatically colonized by toxigenic strains may progress to CDI during admission. However, for patients asymptomatically colonized by nontoxigenic strains, there seems to be no increased risk of progressing to CDI, and these patients may even be protected from developing CDI.
INFECTION CONTROL AND ANTIMICROBIAL STEWARDSHIP IMPLICATIONS FOR ASYMPTOMATIC CARRIERS
Symptomatic CDI patients are believed to be the main source of nosocomial transmission, and current guidelines recommend their systematic detection and isolation (5). Due to a paucity of data at the time of writing of this review, the isolation of asymptomatic carriers is not recommended. Whether these carriers should be isolated remains an important clinical question stemming from the growing body of literature on the subject. Mathematical modeling of C. difficile transmission and simulation of screening and isolation of carriers have shown the intervention to be effective at reducing CDI rates (166, 167). However, a clinically based study to directly answer this question was not conducted until recently (133).
Longtin et al. explored the effect of isolating asymptomatic C. difficile carriers on the incidence of hospital-acquired CDI in an acute care hospital in Quebec, Canada, with high baseline rates of CDI (133). A quasi-experimental design was employed, using changes in CDI incidence in other Quebec hospitals as controls. The effect of the intervention (isolation of carriers) was evaluated through a time series analysis. Compared with that in the preintervention period, the incidence of CDI decreased significantly after the intervention. In addition, the effect was confirmed using two methods of analysis, segmented regression analysis and autoregressive integrated moving average (ARIMA) modeling, indicating the robustness of the results. Incidence rates of CDI in the study hospital remained low a year after the study terminated, demonstrating the sustained effect of this intervention.
This study provides the most convincing evidence, to date, for the significant effect of isolating carriers. The authors assessed confounding elements, such as the intensity of CDI testing, total antimicrobial use, and proton pump inhibitor use, which remained stable during the study period. Concurrently, a significant decrease in the use of metronidazole and oral vancomycin suggested a true clinical impact from the observed decrease in incidence. Compliance with hand hygiene increased but utilized an alcohol-based solution not effective against C. difficile spores. Some potential confounders that were not assessed include compliance with isolation precautions, environmental cleaning, improvement in appropriate antibiotic use, and knowledge of C. difficile carrier status for the management of a patient (168).
Ultimately, these promising findings need to be reproduced in a multicenter cluster randomized trial prior to being considered for widespread implementation. If these results are confirmed in various hospital settings, adoption of screening and isolation of asymptomatic carriers may be an important strategy for decreasing CDI rates. However, this will raise several practical questions, such as whether universal versus targeted screening should be adopted and which screening method is optimal. Given the known risk factors for colonization on admission, a reasonable approach may be to selectively target high-risk patients and to isolate them on admission to hospital (132). Other issues that would need to be addressed include the frequency of screening during hospitalization, the optimal isolation protocol, the impact on patient perception of care, and the additional workload burden on frontline health care workers and the microbiology laboratory.
Reducing inappropriate antimicrobial use through antimicrobial stewardship programs (ASPs) has been shown to decrease rates of CDI (169–171), but given the lack of widespread screening for asymptomatic carriers, ASPs targeted at this population have not been studied. It does not necessarily follow that targeting colonized patients as a whole group would decrease CDI rates, as some of these patients may be long-term-colonized patients with immunity and a decreased risk of developing symptomatic CDI. These patients are likely different from patients who may still be colonized with C. difficile after an episode of symptomatic CDI (10, 68). One study showed a 3-fold increase in recurrence of CDI in patients exposed to antimicrobials after resolved CDI compared to that in patients who were not exposed (172). Therefore, patients with prior CDI, an easily identifiable subset of asymptomatic carriers, probably represent colonized patients at the highest risk of developing infection and may represent suitable targets for focused stewardship efforts.
CONCLUDING REMARKS AND FUTURE DIRECTIONS
The intriguing concept of C. difficile colonization has garnered much attention during the last decade. Gut microbiota studies and immunologic studies have provided some insight into the conditions that allow for colonization and protect against disease progression. However, more studies are needed to assess the precise role of changes in the microbiota and the precise triggers of spore germination and colonization, as well as changes and initiators that lead to toxin production. Why some individuals transition to C. difficile carrier status and what interventions can terminate colonization or block the progression to CDI also need to be explored.
The realization that C. difficile-colonized patients may be the most important unexplained reservoir for C. difficile transmission has led to epidemiological studies investigating colonization rates among different populations and risk factors for this condition. Colonized patients at hospital admission appear to play an important role in introducing and maintaining transmission in the ward, and hence, risk factors for colonization on admission are of specific interest. To further study the acquisition and transmission of C. difficile, all patients admitted to the hospital should be screened for colonization by (and preferably sustained carriage of) C. difficile. C. difficile-positive individuals should be questioned about risk factors for acquisition and should be monitored during admission for the development of symptomatic CDI. Epidemiological investigations and molecular typing methods should be applied to examine possible linkage of C. difficile-colonized individuals to CDI cases. In this way, risk factors for C. difficile colonization can be identified, and the role of C. difficile-positive individuals in transmission of the disease can be elucidated. It would be interesting to determine if there are host and pathogen factors that affect the transmissibility of C. difficile. More evidence from different settings is needed to determine whether specific control measures targeting colonized patients may be justified to prevent spread. In addition, the protective effects of C. difficile vaccines are being examined, but information on the consequences of colonization and spread to nonvaccinated individuals would be relevant.
ACKNOWLEDGMENTS
M.H.W. has received consulting fees from Actelion, Astellas, bioMerieux, MedImmune, Merck, Pfizer, Qiagen, Sanofi-Pasteur, Seres, Summit, Synthetic Biologics, and Valneva; lecture fees from Alere, Astellas, Merck, and Pfizer; and grant support from Actelion, Astellas, bioMerieux, Da Volterra, Merck, Sanofi-Pasteur, Seres, and Summit. V.G.L. has received consulting fees from Merck. M.J.T.C., J.J.V., L.Y.K., S.P., and E.J.K. have no conflicts of interest.
Biographies

Monique J. T. Crobach obtained her medical degree from Leiden University, the Netherlands. She subsequently started her internal medicine residency in The Bronovo Hospital, The Hague, and the Leiden University Medical Centre in the Netherlands. Currently, she is combining this training with her work as a Ph.D. student in the Department of Medical Microbiology at the Leiden University Medical Centre. Her research focuses on diagnostics of C. difficile infections and asymptomatic C. difficile colonization. She took the lead in the development of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) diagnostic guidance document for CDI, is conducting a multicenter study on asymptomatic C. difficile colonization, and is involved in the Dutch national CDI surveillance.

Jonathan J. Vernon is currently a final-year Ph.D. research student at the Leeds Institute of Biomedical and Clinical Sciences at the University of Leeds. His research interests are in the development of multidrug resistance in Clostridium difficile, particularly by epidemiological investigations of resistance determinants and phenotypes. He has been involved in the Healthcare-Associated Infection (HCAI) Research Group in Leeds for over 5 years, working primarily with C. difficile as part of a large-scale, longitudinal, pan-European surveillance study. His other research involvements include in vitro gut modeling of C. difficile infections for investigation of treatment regimens and infection recurrence, efficacy testing of novel compounds for antimicrobial activity, and work as part of the Clostridium difficile Ribotyping Network (CDRN) reference laboratory. Before joining the HCAI research group, he acquired his B.Sc. (Honors) at the University of Lincoln and previously worked as a forensic DNA analyst for the Forensic Science Service, United Kingdom.

Vivian G. Loo is currently a Professor of Medicine at McGill University and Director of the Infectious Disease Clinic at the McGill University Health Centre. Dr. Loo received her medical degree, M.S. in epidemiology, and internal medicine residency training from McGill University. She completed her clinical fellowships in infectious diseases and medical microbiology at the University of Toronto. In 1991, Dr. Loo joined the Faculty of Medicine of McGill University in the Division of Infectious Diseases. At the McGill University Health Centre, she was the Director of the Infection Control and Prevention Service for 10 years as well as the Chief of the Department of Microbiology for 9 years. Dr. Loo's research interests include the epidemiology, transmission, and laboratory diagnosis of Clostridium difficile infections.

Ling Yuan Kong is an infectious diseases and medical microbiology fellow in her final year of training at McGill University, Montreal, Canada. She completed medical school and residency in internal medicine at McGill University. During her residency and fellowship, she developed an interest in infection control and conducted research on C. difficile colonization risk factors and transmission dynamics. She plans to pursue further training in epidemiology and a career combining clinical infectious diseases, medical microbiology, and hospital epidemiology research.

Séverine Péchiné, Pharm.D., Ph.D., has been an Assistant Professor in the Faculty of Pharmacy, Department of Microbiology, Paris-Sud University, since 2006. From 1998 to 2001, she worked for chemical and pharmaceutical companies (Schweizerhall-France and Inalco-Italy). During her Ph.D. training, she studied Clostridium difficile, especially the surface proteins and their use in the development of vaccine strategies, at the Paris-Sud University. She has developed expertise on Clostridium difficile colonization factors, immune responses of the host, and vaccine strategies in animal models. She has published in the field of Clostridium and acts as a referee for peer-reviewed journals.

Mark H. Wilcox is a Consultant Microbiologist, Head of Research and Development in Microbiology at the Leeds Teaching Hospitals (LTHT), Professor of Medical Microbiology at the University of Leeds (Leeds Institute of Biomedical and Clinical Sciences), Lead on Clostridium difficile and Head of the UK C. difficile Reference Laboratory for Public Health England (PHE), and Medical Advisor to the National Infection Prevention & Control Lead (NHS Improvement), England. He was formerly a Director of Infection Prevention (4 years), Infection Control Doctor (8 years), Clinical Director of Pathology (6 years), and Head of Microbiology (15 years) at LTHT. Professor Wilcox heads a health care-associated infection research team at the University of Leeds; projects include multiple aspects of Clostridium difficile infection, diagnostics, antibiotic resistance and the gut microbiome, staphylococcal infection, and the clinical development of new antimicrobial agents.

Ed J. Kuijper is Professor and Head of Experimental Bacteriology at the Department of Medical Microbiology, Leiden University Medical Center. He received his education at the University of Amsterdam and obtained a medical degree in 1982. His Ph.D. was achieved in 1987 with the thesis “Aeromonas-associated diarrhoea in the Netherlands.” In 1987, he also completed his training as a medical microbiologist, and he worked as a researcher on the topics of meningococcal infections, fungal infections, and mycobacterial infections until 2000. In 2001, he was appointed at Leiden University and started a research group on Clostridium difficile infections (CDI), in close collaboration with the National Center for Infectious Diseases at the RIVM. The research group focuses on the pathogenesis, epidemiology, and treatment of CDI.
REFERENCES
- 1.Walker AS, Eyre DW, Wyllie DH, Dingle KE, Harding RM, O'Connor L, Griffiths D, Vaughan A, Finney J, Wilcox MH, Crook DW, Peto TE. 2012. Characterisation of Clostridium difficile hospital ward-based transmission using extensive epidemiological data and molecular typing. PLoS Med 9:e1001172. doi: 10.1371/journal.pmed.1001172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Curry SR, Muto CA, Schlackman JL, Pasculle AW, Shutt KA, Marsh JW, Harrison LH. 2013. Use of multilocus variable number of tandem repeats analysis genotyping to determine the role of asymptomatic carriers in Clostridium difficile transmission. Clin Infect Dis 57:1094–1102. doi: 10.1093/cid/cit475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eyre DW, Cule ML, Wilson DJ, Griffiths D, Vaughan A, O'Connor L, Ip CL, Golubchik T, Batty EM, Finney JM, Wyllie DH, Didelot X, Piazza P, Bowden R, Dingle KE, Harding RM, Crook DW, Wilcox MH, Peto TE, Walker AS. 2013. Diverse sources of C. difficile infection identified on whole-genome sequencing. N Engl J Med 369:1195–1205. doi: 10.1056/NEJMoa1216064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Debast SB, Bauer MP, Kuijper EJ, European Society of Clinical Microbiology and Infectious Diseases. 2014. European Society of Clinical Microbiology and Infectious Diseases: update of the treatment guidance document for Clostridium difficile infection. Clin Microbiol Infect 20(Suppl 2):S1–S26. doi: 10.1111/1469-0691.12418. [DOI] [PubMed] [Google Scholar]
- 5.Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, Pepin J, Wilcox MH, Society for Healthcare Epidemiology of America, Infectious Diseases Society of America. 2010. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol 31:431–455. doi: 10.1086/651706. [DOI] [PubMed] [Google Scholar]
- 6.Galdys AL, Curry SR, Harrison LH. 2014. Asymptomatic Clostridium difficile colonization as a reservoir for Clostridium difficile infection. Expert Rev Anti Infect Ther 12:967–980. doi: 10.1586/14787210.2014.920252. [DOI] [PubMed] [Google Scholar]
- 7.Crobach MJ, Planche T, Eckert C, Barbut F, Terveer EM, Dekkers OM, Wilcox MH, Kuijper EJ. 2016. European Society of Clinical Microbiology and Infectious Diseases: update of the diagnostic guidance document for Clostridium difficile infection. Clin Microbiol Infect 22(Suppl 4):S63–S81. doi: 10.1016/j.cmi.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 8.Guerrero DM, Becker JC, Eckstein EC, Kundrapu S, Deshpande A, Sethi AK, Donskey CJ. 2013. Asymptomatic carriage of toxigenic Clostridium difficile by hospitalized patients. J Hosp Infect 85:155–158. doi: 10.1016/j.jhin.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Freter R, Brickner H, Fekete J, Vickerman MM, Carey KE. 1983. Survival and implantation of Escherichia-coli in the intestinal-tract. Infect Immun 39:686–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Donskey CJ, Kundrapu S, Deshpande A. 2015. Colonization versus carriage of Clostridium difficile. Infect Dis Clin North Am 29:13–28. doi: 10.1016/j.idc.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Hung YP, Lin HJ, Wu TC, Liu HC, Lee JC, Lee CI, Wu YH, Wan L, Tsai PJ, Ko WC. 2013. Risk factors of fecal toxigenic or non-toxigenic Clostridium difficile colonization: impact of Toll-like receptor polymorphisms and prior antibiotic exposure. PLoS One 8:e69577. doi: 10.1371/journal.pone.0069577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loo VG, Bourgault AM, Poirier L, Lamothe F, Michaud S, Turgeon N, Toye B, Beaudoin A, Frost EH, Gilca R, Brassard P, Dendukuri N, Beliveau C, Oughton M, Brukner I, Dascal A. 2011. Host and pathogen factors for Clostridium difficile infection and colonization. N Engl J Med 365:1693–1703. doi: 10.1056/NEJMoa1012413. [DOI] [PubMed] [Google Scholar]
- 13.Galdys AL, Nelson JS, Shutt KA, Schlackman JL, Pakstis DL, Pasculle AW, Marsh JW, Harrison LH, Curry SR. 2014. Prevalence and duration of asymptomatic Clostridium difficile carriage among healthy subjects in Pittsburgh, Pennsylvania. J Clin Microbiol 52:2406–2409. doi: 10.1128/JCM.00222-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McFarland LV, Mulligan ME, Kwok RY, Stamm WE. 1989. Nosocomial acquisition of Clostridium difficile infection. N Engl J Med 320:204–210. doi: 10.1056/NEJM198901263200402. [DOI] [PubMed] [Google Scholar]
- 15.Eyre DW, Griffiths D, Vaughan A, Golubchik T, Acharya M, O'Connor L, Crook DW, Walker AS, Peto TE. 2013. Asymptomatic Clostridium difficile colonisation and onward transmission. PLoS One 8:e78445. doi: 10.1371/journal.pone.0078445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Planche T, Wilcox M. 2011. Reference assays for Clostridium difficile infection: one or two gold standards? J Clin Pathol 64:1–5. doi: 10.1136/jcp.2010.080135. [DOI] [PubMed] [Google Scholar]
- 17.Freeman J, Wilcox MH. 2003. The effects of storage conditions on viability of Clostridium difficile vegetative cells and spores and toxin activity in human faeces. J Clin Pathol 56:126–128. doi: 10.1136/jcp.56.2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bolton RP, Tait SK, Dear PRF, Losowsky MS. 1984. Asymptomatic neonatal colonization by Clostridium-difficile. Arch Dis Child 59:466–472. doi: 10.1136/adc.59.5.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Planche TD, Davies KA, Coen PG, Finney JM, Monahan IM, Morris KA, O'Connor L, Oakley SJ, Pope CF, Wren MW, Shetty NP, Crook DW, Wilcox MH. 2013. Differences in outcome according to Clostridium difficile testing method: a prospective multicentre diagnostic validation study of C difficile infection. Lancet Infect Dis 13:936–945. doi: 10.1016/S1473-3099(13)70200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polage CR, Gyorke CE, Kennedy MA, Leslie JL, Chin DL, Wang S, Nguyen HH, Huang B, Tang YW, Lee LW, Kim K, Taylor S, Romano PS, Panacek EA, Goodell PB, Solnick JV, Cohen SH. 2015. Overdiagnosis of Clostridium difficile infection in the molecular test era. JAMA Intern Med 175:1792–1801. doi: 10.1001/jamainternmed.2015.4114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eastwood K, Else P, Charlett A, Wilcox M. 2009. Comparison of nine commercially available Clostridium difficile toxin detection assays, a real-time PCR assay for C. difficile tcdB, and a glutamate dehydrogenase detection assay to cytotoxin testing and cytotoxigenic culture methods. J Clin Microbiol 47:3211–3217. doi: 10.1128/JCM.01082-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miyajima F, Roberts P, Swale A, Price V, Jones M, Horan M, Beeching N, Brazier J, Parry C, Pendleton N, Pirmohamed M. 2011. Characterisation and carriage ratio of Clostridium difficile strains isolated from a community-dwelling elderly population in the United Kingdom. PLoS One 6:e22804. doi: 10.1371/journal.pone.0022804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burnham C-AD, Carroll KC. 2013. Diagnosis of Clostridium difficile infection: an ongoing conundrum for clinicians and for clinical laboratories. Clin Microbiol Rev 26:604–630. doi: 10.1128/CMR.00016-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lawley TD, Walker AW. 2013. Intestinal colonization resistance. Immunology 138:1–11. doi: 10.1111/j.1365-2567.2012.03616.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Theriot CM, Young VB. 2015. Interactions between the gastrointestinal microbiome and Clostridium difficile. Annu Rev Microbiol 69:445–461. doi: 10.1146/annurev-micro-091014-104115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Semenyuk EG, Poroyko VA, Johnston PF, Jones SE, Knight KL, Gerding DN, Driks A. 2015. Analysis of bacterial communities during Clostridium difficile infection in the mouse. Infect Immun 83:4383–4391. doi: 10.1128/IAI.00145-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crowther GS, Chilton CH, Todhunter SL, Nicholson S, Freeman J, Baines SD, Wilcox MH. 2014. Comparison of planktonic and biofilm-associated communities of Clostridium difficile and indigenous gut microbiota in a triple-stage chemostat gut model. J Antimicrob Chemother 69:2137–2147. doi: 10.1093/jac/dku116. [DOI] [PubMed] [Google Scholar]
- 28.Theriot CM, Bowman AA, Young VB. 2016. Antibiotic-induced alterations of the gut microbiota alter secondary bile acid production and allow for Clostridium difficile spore germination and outgrowth in the large intestine. mSphere 1:e00045-15. doi: 10.1128/mSphere.00045-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang L, Dong D, Jiang C, Li Z, Wang X, Peng Y. 2015. Insight into alteration of gut microbiota in Clostridium difficile infection and asymptomatic C. difficile colonization. Anaerobe 34:1–7. doi: 10.1016/j.anaerobe.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 30.Gu S, Chen Y, Zhang X, Lu H, Lv T, Shen P, Lv L, Zheng B, Jiang X, Li L. 2016. Identification of key taxa that favor intestinal colonization of Clostridium difficile in an adult Chinese population. Microbes Infect 18:30–38. doi: 10.1016/j.micinf.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 31.Antharam VC, Li EC, Ishmael A, Sharma A, Mai V, Rand KH, Wang GP. 2013. Intestinal dysbiosis and depletion of butyrogenic bacteria in Clostridium difficile infection and nosocomial diarrhea. J Clin Microbiol 51:2884–2892. doi: 10.1128/JCM.00845-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vincent C, Stephens DA, Loo VG, Edens TJ, Behr MA, Dewar K, Manges AR. 2013. Reductions in intestinal Clostridiales precede the development of nosocomial Clostridium difficile infection. Microbiome 1:18. doi: 10.1186/2049-2618-1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schubert AM, Rogers MA, Ring C, Mogle J, Petrosino JP, Young VB, Aronoff DM, Schloss PD. 2014. Microbiome data distinguish patients with Clostridium difficile infection and non-C. difficile-associated diarrhea from healthy controls. mBio 5:e01021-14. doi: 10.1128/mBio.01021-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Buffie CG, Jarchum I, Equinda M, Lipuma L, Gobourne A, Viale A, Ubeda C, Xavier J, Pamer EG. 2012. Profound alterations of intestinal microbiota following a single dose of clindamycin results in sustained susceptibility to Clostridium difficile-induced colitis. Infect Immun 80:62–73. doi: 10.1128/IAI.05496-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reeves AE, Theriot CM, Bergin IL, Huffnagle GB, Schloss PD, Young VB. 2011. The interplay between microbiome dynamics and pathogen dynamics in a murine model of Clostridium difficile infection. Gut Microbes 2:145–158. doi: 10.4161/gmic.2.3.16333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vincent C, Miller MA, Edens TJ, Mehrotra S, Dewar K, Manges AR. 2016. Bloom and bust: intestinal microbiota dynamics in response to hospital exposures and Clostridium difficile colonization or infection. Microbiome 4:12. doi: 10.1186/s40168-016-0156-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reeves AE, Koenigsknecht MJ, Bergin IL, Young VB. 2012. Suppression of Clostridium difficile in the gastrointestinal tracts of germfree mice inoculated with a murine isolate from the family Lachnospiraceae. Infect Immun 80:3786–3794. doi: 10.1128/IAI.00647-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Buffie CG, Bucci V, Stein RR, McKenney PT, Ling L, Gobourne A, No D, Liu H, Kinnebrew M, Viale A, Littmann E, van den Brink MR, Jenq RR, Taur Y, Sander C, Cross JR, Toussaint NC, Xavier JB, Pamer EG. 2015. Precision microbiome reconstitution restores bile acid mediated resistance to Clostridium difficile. Nature 517:205–208. doi: 10.1038/nature13828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davis MY, Zhang H, Brannan LE, Carman RJ, Boone JH. 2016. Rapid change of fecal microbiome and disappearance of Clostridium difficile in a colonized infant after transition from breast milk to cow milk. Microbiome 4:53. doi: 10.1186/s40168-016-0198-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Francis MB, Allen CA, Shrestha R, Sorg JA. 2013. Bile acid recognition by the Clostridium difficile germinant receptor, CspC, is important for establishing infection. PLoS Pathog 9:e1003356. doi: 10.1371/journal.ppat.1003356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wells JE, Hylemon PB. 2000. Identification and characterization of a bile acid 7alpha-dehydroxylation operon in Clostridium sp. strain TO-931, a highly active 7alpha-dehydroxylating strain isolated from human feces. Appl Environ Microbiol 66:1107–1113. doi: 10.1128/AEM.66.3.1107-1113.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weingarden AR, Dosa PI, DeWinter E, Steer CJ, Shaughnessy MK, Johnson JR, Khoruts A, Sadowsky MJ. 2016. Changes in colonic bile acid composition following fecal microbiota transplantation are sufficient to control Clostridium difficile germination and growth. PLoS One 11:e0147210. doi: 10.1371/journal.pone.0147210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Allegretti JR, Kearney S, Li N, Bogart E, Bullock K, Gerber GK, Bry L, Clish CB, Alm E, Korzenik JR. 2016. Recurrent Clostridium difficile infection associates with distinct bile acid and microbiome profiles. Aliment Pharmacol Ther 43:1142–1153. doi: 10.1111/apt.13616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gupta P, Yakubov S, Tin K, Zea D, Garankina O, Ghitan M, Chapnick EK, Homel P, Lin YS, Koegel MM. 2016. Does alkaline colonic pH predispose to Clostridium difficile infection? South Med J 109:91–96. doi: 10.14423/SMJ.0000000000000414. [DOI] [PubMed] [Google Scholar]
- 45.Ross CL, Spinler JK, Savidge TC. 2016. Structural and functional changes within the gut microbiota and susceptibility to Clostridium difficile infection. Anaerobe 41:37–43. doi: 10.1016/j.anaerobe.2016.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wong JM, de Souza R, Kendall CW, Emam A, Jenkins DJ. 2006. Colonic health: fermentation and short chain fatty acids. J Clin Gastroenterol 40:235–243. doi: 10.1097/00004836-200603000-00015. [DOI] [PubMed] [Google Scholar]
- 47.Bibbo S, Lopetuso LR, Ianiro G, Di Rienzo T, Gasbarrini A, Cammarota G. 2014. Role of microbiota and innate immunity in recurrent Clostridium difficile infection. J Immunol Res 2014:462740. doi: 10.1155/2014/462740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rea MC, Sit CS, Clayton E, O'Connor PM, Whittal RM, Zheng J, Vederas JC, Ross RP, Hill C. 2010. Thuricin CD, a posttranslationally modified bacteriocin with a narrow spectrum of activity against Clostridium difficile. Proc Natl Acad Sci U S A 107:9352–9357. doi: 10.1073/pnas.0913554107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sambol SP, Merrigan MM, Tang JK, Johnson S, Gerding DN. 2002. Colonization for the prevention of Clostridium difficile disease in hamsters. J Infect Dis 186:1781–1789. doi: 10.1086/345676. [DOI] [PubMed] [Google Scholar]
- 50.Popoff MR, Geny B. 2011. Rho/Ras-GTPase-dependent and -independent activity of clostridial glucosylating toxins. J Med Microbiol 60:1057–1069. doi: 10.1099/jmm.0.029314-0. [DOI] [PubMed] [Google Scholar]
- 51.Pechine S, Collignon A. 2016. Immune responses induced by Clostridium difficile. Anaerobe 41:68–78. doi: 10.1016/j.anaerobe.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 52.Vohra P, Poxton IR. 2012. Induction of cytokines in a macrophage cell line by proteins of Clostridium difficile. FEMS Immunol Med Microbiol 65:96–104. doi: 10.1111/j.1574-695X.2012.00952.x. [DOI] [PubMed] [Google Scholar]
- 53.Ryan A, Lynch M, Smith SM, Amu S, Nel HJ, McCoy CE, Dowling JK, Draper E, O'Reilly V, McCarthy C, O'Brien J, Ni Eidhin D, O'Connell MJ, Keogh B, Morton CO, Rogers TR, Fallon PG, O'Neill LA, Kelleher D, Loscher CE. 2011. A role for TLR4 in Clostridium difficile infection and the recognition of surface layer proteins. PLoS Pathog 7:e1002076. doi: 10.1371/journal.ppat.1002076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yoshino Y, Kitazawa T, Ikeda M, Tatsuno K, Yanagimoto S, Okugawa S, Yotsuyanagi H, Ota Y. 2013. Clostridium difficile flagellin stimulates Toll-like receptor 5, and toxin B promotes flagellin-induced chemokine production via TLR5. Life Sci 92:211–217. doi: 10.1016/j.lfs.2012.11.017. [DOI] [PubMed] [Google Scholar]
- 55.Batah J, Deneve-Larrazet C, Jolivot PA, Kuehne S, Collignon A, Marvaud JC, Kansau I. 2016. Clostridium difficile flagella predominantly activate TLR5-linked NF-kappaB pathway in epithelial cells. Anaerobe 38:116–124. doi: 10.1016/j.anaerobe.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 56.Batah J, Kobeissy H, Bui Pham PT, Deneve-Larrazet C, Kuehne S, Collignon A, Janoir-Jouveshomme C, Marvaud JC, Kansau I. 2017. Clostridium difficile flagella induce a pro-inflammatory response in intestinal epithelium of mice in cooperation with toxins. Sci Rep 7:3256. doi: 10.1038/s41598-017-03621-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Drudy D, Calabi E, Kyne L, Sougioultzis S, Kelly E, Fairweather N, Kelly CP. 2004. Human antibody response to surface layer proteins in Clostridium difficile infection. FEMS Immunol Med Microbiol 41:237–242. doi: 10.1016/j.femsim.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 58.Wright A, Drudy D, Kyne L, Brown K, Fairweather NF. 2008. Immunoreactive cell wall proteins of Clostridium difficile identified by human sera. J Med Microbiol 57:750–756. doi: 10.1099/jmm.0.47532-0. [DOI] [PubMed] [Google Scholar]
- 59.Bruxelle JF, Mizrahi A, Hoys S, Collignon A, Janoir C, Pechine S. 2016. Immunogenic properties of the surface layer precursor of Clostridium difficile and vaccination assays in animal models. Anaerobe 37:78–84. doi: 10.1016/j.anaerobe.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 60.Ni Eidhin DB, O'Brien JB, McCabe MS, Athie-Morales V, Kelleher DP. 2008. Active immunization of hamsters against Clostridium difficile infection using surface-layer protein. FEMS Immunol Med Microbiol 52:207–218. doi: 10.1111/j.1574-695X.2007.00363.x. [DOI] [PubMed] [Google Scholar]
- 61.Pechine S, Janoir C, Boureau H, Gleizes A, Tsapis N, Hoys S, Fattal E, Collignon A. 2007. Diminished intestinal colonization by Clostridium difficile and immune response in mice after mucosal immunization with surface proteins of Clostridium difficile. Vaccine 25:3946–3954. doi: 10.1016/j.vaccine.2007.02.055. [DOI] [PubMed] [Google Scholar]
- 62.Pechine S, Deneve C, Le Monnier A, Hoys S, Janoir C, Collignon A. 2011. Immunization of hamsters against Clostridium difficile infection using the Cwp84 protease as an antigen. FEMS Immunol Med Microbiol 63:73–81. doi: 10.1111/j.1574-695X.2011.00832.x. [DOI] [PubMed] [Google Scholar]
- 63.Ghose C, Eugenis I, Sun X, Edwards AN, McBride SM, Pride DT, Kelly CP, Ho DD. 2016. Immunogenicity and protective efficacy of recombinant Clostridium difficile flagellar protein FliC. Emerg Microbes Infect 5:e8. doi: 10.1038/emi.2016.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kyne L, Warny M, Qamar A, Kelly CP. 2000. Asymptomatic carriage of Clostridium difficile and serum levels of IgG antibody against toxin A. N Engl J Med 342:390–397. doi: 10.1056/NEJM200002103420604. [DOI] [PubMed] [Google Scholar]
- 65.Wilcox MH, Gerding DN, Poxton IR, Kelly C, Nathan R, Birch T, Cornely OA, Rahav G, Bouza E, Lee C, Jenkin G, Jensen W, Kim YS, Yoshida J, Gabryelski L, Pedley A, Eves K, Tipping R, Guris D, Kartsonis N, Dorr MB. 2017. Bezlotoxumab for prevention of recurrent Clostridium difficile infection. N Engl J Med 376:305–317. doi: 10.1056/NEJMoa1602615. [DOI] [PubMed] [Google Scholar]
- 66.Dieterle MG, Young VB. 2017. Reducing recurrence of C. difficile infection. Cell 169:375. doi: 10.1016/j.cell.2017.03.039. [DOI] [PubMed] [Google Scholar]
- 67.Pechine S, Janoir C, Collignon A. 2017. Emerging monoclonal antibodies against Clostridium difficile infection. Expert Opin Biol Ther 17:415–427. doi: 10.1080/14712598.2017.1300655. [DOI] [PubMed] [Google Scholar]
- 68.Sethi AK, Al-Nassir WN, Nerandzic MM, Bobulsky GS, Donskey CJ. 2010. Persistence of skin contamination and environmental shedding of Clostridium difficile during and after treatment of C. difficile infection. Infect Control Hosp Epidemiol 31:21–27. doi: 10.1086/649016. [DOI] [PubMed] [Google Scholar]
- 69.Lawley TD, Clare S, Walker AW, Goulding D, Stabler RA, Croucher N, Mastroeni P, Scott P, Raisen C, Mottram L, Fairweather NF, Wren BW, Parkhill J, Dougan G. 2009. Antibiotic treatment of Clostridium difficile carrier mice triggers a supershedder state, spore-mediated transmission, and severe disease in immunocompromised hosts. Infect Immun 77:3661–3669. doi: 10.1128/IAI.00558-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Blixt T, Gradel KO, Homann C, Seidelin JB, Schonning K, Lester A, Houlind J, Stangerup M, Gottlieb M, Knudsen JD. 2017. Asymptomatic carriers contribute to nosocomial Clostridium difficile infection: a cohort study of 4508 patients. Gastroenterology 152:1031.e2–1041.e2. doi: 10.1053/j.gastro.2016.12.035. [DOI] [PubMed] [Google Scholar]
- 71.Clabots CR, Johnson S, Olson MM, Peterson LR, Gerding DN. 1992. Acquisition of Clostridium difficile by hospitalized patients: evidence for colonized new admissions as a source of infection. J Infect Dis 166:561–567. doi: 10.1093/infdis/166.3.561. [DOI] [PubMed] [Google Scholar]
- 72.Lanzas C, Dubberke ER, Lu Z, Reske KA, Grohn YT. 2011. Epidemiological model for Clostridium difficile transmission in healthcare settings. Infect Control Hosp Epidemiol 32:553–561. doi: 10.1086/660013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stone NE, Sidak-Loftis LC, Sahl JW, Vazquez AJ, Wiggins KB, Gillece JD, Hicks ND, Schupp JM, Busch JD, Keim P, Wagner DM. 2016. More than 50% of Clostridium difficile isolates from pet dogs in Flagstaff, USA, carry toxigenic genotypes. PLoS One 11:e0164504. doi: 10.1371/journal.pone.0164504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pelaez T, Alcala L, Blanco JL, Alvarez-Perez S, Marin M, Martin-Lopez A, Catalan P, Reigadas E, Garcia ME, Bouza E. 2013. Characterization of swine isolates of Clostridium difficile in Spain: a potential source of epidemic multidrug resistant strains? Anaerobe 22:45–49. doi: 10.1016/j.anaerobe.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 75.Schneeberg A, Neubauer H, Schmoock G, Baier S, Harlizius J, Nienhoff H, Brase K, Zimmermann S, Seyboldt C. 2013. Clostridium difficile genotypes in piglet populations in Germany. J Clin Microbiol 51:3796–3803. doi: 10.1128/JCM.01440-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Knight DR, Squire MM, Riley TV. 2015. Nationwide surveillance study of Clostridium difficile in Australian neonatal pigs shows high prevalence and heterogeneity of PCR ribotypes. Appl Environ Microbiol 81:119–123. doi: 10.1128/AEM.03032-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Riley TV, Adams JE, O'Neill GL, Bowman RA. 1991. Gastrointestinal carriage of Clostridium difficile in cats and dogs attending veterinary clinics. Epidemiol Infect 107:659–665. doi: 10.1017/S0950268800049359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Borriello SP, Honour P, Turner T, Barclay F. 1983. Household pets as a potential reservoir for Clostridium difficile infection. J Clin Pathol 36:84–87. doi: 10.1136/jcp.36.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bojesen AM, Olsen KE, Bertelsen MF. 2006. Fatal enterocolitis in Asian elephants (Elephas maximus) caused by Clostridium difficile. Vet Microbiol 116:329–335. doi: 10.1016/j.vetmic.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 80.Orchard JL, Fekety R, Smith JR. 1983. Antibiotic-associated colitis due to Clostridium difficile in a Kodiak bear. Am J Vet Res 44:1547–1548. [PubMed] [Google Scholar]
- 81.Freeman J, Bauer MP, Baines SD, Corver J, Fawley WN, Goorhuis B, Kuijper EJ, Wilcox MH. 2010. The changing epidemiology of Clostridium difficile infections. Clin Microbiol Rev 23:529–549. doi: 10.1128/CMR.00082-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Knight DR, Elliott B, Chang BJ, Perkins TT, Riley TV. 2015. Diversity and evolution in the genome of Clostridium difficile. Clin Microbiol Rev 28:721–741. doi: 10.1128/CMR.00127-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Weese JS, Staempfli HR, Prescott JF, Kruth SA, Greenwood SJ, Weese HE. 2001. The roles of Clostridium difficile and enterotoxigenic Clostridium perfringens in diarrhea in dogs. J Vet Intern Med 15:374–378. [PubMed] [Google Scholar]
- 84.Weese JS, Weese HE, Bourdeau TL, Staempfli HR. 2001. Suspected Clostridium difficile-associated diarrhea in two cats. J Am Vet Med Assoc 218:1421, 1436–1439. doi: 10.2460/javma.2001.218.1421. [DOI] [PubMed] [Google Scholar]
- 85.Shaughnessy MK, Bobr A, Kuskowski MA, Johnston BD, Sadowsky MJ, Khoruts A, Johnson JR. 2016. Environmental contamination in households of patients with recurrent Clostridium difficile infection. Appl Environ Microbiol 82:2686–2692. doi: 10.1128/AEM.03888-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Loo VG, Brassard P, Miller MA. 2016. Household transmission of Clostridium difficile to family members and domestic pets. Infect Control Hosp Epidemiol 37:1342–1348. doi: 10.1017/ice.2016.178. [DOI] [PubMed] [Google Scholar]
- 87.Knight DR, Squire MM, Collins DA, Riley TV. 2017. Genome analysis of Clostridium difficile PCR ribotype 014 lineage in Australian pigs and humans reveals a diverse genetic repertoire and signatures of long-range interspecies transmission. Front Microbiol 7:2138. doi: 10.3389/fmicb.2016.02138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Knetsch CW, Connor TR, Mutreja A, van Dorp SM, Sanders IM, Browne HP, Harris D, Lipman L, Keessen EC, Corver J, Kuijper EJ, Lawley TD. 2014. Whole genome sequencing reveals potential spread of Clostridium difficile between humans and farm animals in the Netherlands, 2002 to 2011. Euro Surveill 19:20954. doi: 10.2807/1560-7917.ES2014.19.45.20954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rodriguez-Palacios A, Staempfli HR, Duffield T, Weese JS. 2007. Clostridium difficile in retail ground meat, Canada. Emerg Infect Dis 13:485–487. doi: 10.3201/eid1303.060988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Loo VG, Poirier L, Miller MA, Oughton M, Libman MD, Michaud S, Bourgault AM, Nguyen T, Frenette C, Kelly M, Vibien A, Brassard P, Fenn S, Dewar K, Hudson TJ, Horn R, Rene P, Monczak Y, Dascal A. 2005. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. N Engl J Med 353:2442–2449. doi: 10.1056/NEJMoa051639. [DOI] [PubMed] [Google Scholar]
- 91.Rodriguez-Palacios A, Reid-Smith RJ, Staempfli HR, Daignault D, Janecko N, Avery BP, Martin H, Thomspon AD, McDonald LC, Limbago B, Weese JS. 2009. Possible seasonality of Clostridium difficile in retail meat, Canada. Emerg Infect Dis 15:802–805. doi: 10.3201/eid1505.081084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Songer JG, Trinh HT, Killgore GE, Thompson AD, McDonald LC, Limbago BM. 2009. Clostridium difficile in retail meat products, USA, 2007. Emerg Infect Dis 15:819–821. doi: 10.3201/eid1505.081071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.de Boer E, Zwartkruis-Nahuis A, Heuvelink AE, Harmanus C, Kuijper EJ. 2011. Prevalence of Clostridium difficile in retailed meat in the Netherlands. Int J Food Microbiol 144:561–564. doi: 10.1016/j.ijfoodmicro.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 94.Hoffer E, Haechler H, Frei R, Stephan R. 2010. Low occurrence of Clostridium difficile in fecal samples of healthy calves and pigs at slaughter and in minced meat in Switzerland. J Food Prot 73:973–975. doi: 10.4315/0362-028X-73.5.973. [DOI] [PubMed] [Google Scholar]
- 95.Bouttier S, Barc MC, Felix B, Lambert S, Collignon A, Barbut F. 2010. Clostridium difficile in ground meat, France. Emerg Infect Dis 16:733–735. doi: 10.3201/eid1604.091138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Weese JS, Avery BP, Rousseau J, Reid-Smith RJ. 2009. Detection and enumeration of Clostridium difficile spores in retail beef and pork. Appl Environ Microbiol 75:5009–5011. doi: 10.1128/AEM.00480-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Stabler RA, Dawson LF, Valiente E, Cairns MD, Martin MJ, Donahue EH, Riley TV, Songer JG, Kuijper EJ, Dingle KE, Wren BW. 2012. Macro and micro diversity of Clostridium difficile isolates from diverse sources and geographical locations. PLoS One 7:e31559. doi: 10.1371/journal.pone.0031559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Samore MH, DeGirolami PC, Tlucko A, Lichtenberg DA, Melvin ZA, Karchmer AW. 1994. Clostridium difficile colonization and diarrhea at a tertiary care hospital. Clin Infect Dis 18:181–187. doi: 10.1093/clinids/18.2.181. [DOI] [PubMed] [Google Scholar]
- 99.Kim KH, Fekety R, Batts DH, Brown D, Cudmore M, Silva J Jr, Waters D. 1981. Isolation of Clostridium difficile from the environment and contacts of patients with antibiotic-associated colitis. J Infect Dis 143:42–50. doi: 10.1093/infdis/143.1.42. [DOI] [PubMed] [Google Scholar]
- 100.Biswas JS, Patel A, Otter JA, van Kleef E, Goldenberg SD. 2015. Contamination of the hospital environment from potential Clostridium difficile excretors without active infection. Infect Control Hosp Epidemiol 36:975–977. doi: 10.1017/ice.2015.79. [DOI] [PubMed] [Google Scholar]
- 101.al Saif N, Brazier JS. 1996. The distribution of Clostridium difficile in the environment of South Wales. J Med Microbiol 45:133–137. doi: 10.1099/00222615-45-2-133. [DOI] [PubMed] [Google Scholar]
- 102.Moono P, Lim SC, Riley TV. 2017. High prevalence of toxigenic Clostridium difficile in public space lawns in western Australia. Sci Rep 7:41196. doi: 10.1038/srep41196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Xu C, Weese JS, Flemming C, Odumeru J, Warriner K. 2014. Fate of Clostridium difficile during wastewater treatment and incidence in Southern Ontario watersheds. J Appl Microbiol 117:891–904. doi: 10.1111/jam.12575. [DOI] [PubMed] [Google Scholar]
- 104.Al-Jumaili IJ, Shibley M, Lishman AH, Record CO. 1984. Incidence and origin of Clostridium-difficile in neonates. J Clin Microbiol 19:77–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Enoch DA, Butler MJ, Pai S, Aliyu SH, Karas JA. 2011. Clostridium difficile in children: colonisation and disease. J Infect 63:105–113. doi: 10.1016/j.jinf.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 106.Rousseau C, Lemee L, Le Monnier A, Poilane I, Pons JL, Collignon A. 2011. Prevalence and diversity of Clostridium difficile strains in infants. J Med Microbiol 60:1112–1118. doi: 10.1099/jmm.0.029736-0. [DOI] [PubMed] [Google Scholar]
- 107.Burgner D, Siarakas S, Eagles G, McCarthy A, Bradbury R, Stevens M. 1997. A prospective study of Clostridium difficile infection and colonization in pediatric oncology patients. Pediatr Infect Dis J 16:1131–1134. doi: 10.1097/00006454-199712000-00006. [DOI] [PubMed] [Google Scholar]
- 108.Naaber P, Klaus K, Sepp E, Bjorksten B, Mikelsaar M. 1997. Colonization of infants and hospitalized patients with Clostridium difficile and lactobacilli. Clin Infect Dis 25:S189–S190. doi: 10.1086/516183. [DOI] [PubMed] [Google Scholar]
- 109.Zilberberg MD, Tillotson GS, McDonald C. 2010. Clostridium difficile infections among hospitalized children, United States, 1997–2006. Emerg Infect Dis 16:604–609. doi: 10.3201/eid1604.090680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Guido K, Khattab H, Bay C, Ostovar GA. 2015. Clostridium difficile colonization in asymptomatic infants 1 to 12 months old, admitted to a community hospital. Clin Pediatr 55:1176–1179. doi: 10.1177/0009922815614354. [DOI] [PubMed] [Google Scholar]
- 111.Furuichi M, Imajo E, Sato Y, Tanno S, Kawada M, Sato S. 2014. Characteristics of Clostridium difficile colonization in Japanese children. J Infect Chemother 20:307–311. doi: 10.1016/j.jiac.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 112.Hafiz S, Morton RS, McEntegart MG, Waitkins SA. 1975. Clostridium difficile in urogenital tract of males and females. Lancet i:420–421. [DOI] [PubMed] [Google Scholar]
- 113.Delmee M, Verellen G, Avesani V, Francois G. 1988. Clostridium-difficile in neonates—serogrouping and epidemiology. Eur J Pediatr 147:36–40. doi: 10.1007/BF00442608. [DOI] [PubMed] [Google Scholar]
- 114.Adlerberth I, Huang HH, Lindberg E, Aberg N, Hesselmar B, Saalman R, Nord CE, Wold AE, Weintraub A. 2014. Toxin-producing Clostridium difficile strains as long-term gut colonizers in healthy infants. J Clin Microbiol 52:173–179. doi: 10.1128/JCM.01701-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Stoesser N, Crook DW, Fung R, Griffiths D, Harding RM, Kachrimanidou M, Keshav S, Peto TE, Vaughan A, Walker AS, Dingle KE. 2011. Molecular epidemiology of Clostridium difficile strains in children compared with that of strains circulating in adults with Clostridium difficile-associated infection. J Clin Microbiol 49:3994–3996. doi: 10.1128/JCM.05349-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rousseau C, Poilane I, De Pontual L, Maherault AC, Le Monnier A, Collignon A. 2012. Clostridium difficile carriage in healthy infants in the community: a potential reservoir for pathogenic strains. Clin Infect Dis 55:1209–1215. doi: 10.1093/cid/cis637. [DOI] [PubMed] [Google Scholar]
- 117.Lees EA, Miyajima F, Pirmohamed M, Carrol ED. 2016. The role of Clostridium difficile in the paediatric and neonatal gut—a narrative review. Eur J Clin Microbiol Infect Dis 35:1047–1057. doi: 10.1007/s10096-016-2639-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Leibowitz J, Soma VL, Rosen L, Ginocchio CC, Rubin LG. 2015. Similar proportions of stool specimens from hospitalized children with and without diarrhea test positive for Clostridium difficile. Pediatr Infect Dis J 34:261–266. doi: 10.1097/INF.0000000000000556. [DOI] [PubMed] [Google Scholar]
- 119.Matsuki S, Ozaki E, Shozu M, Inoue M, Shimizu S, Yamaguchi N, Karasawa T, Yamagishi T, Nakamura S. 2005. Colonization by Clostridium difficile of neonates in a hospital, and infants and children in three day-care facilities of Kanazawa, Japan. Int Microbiol 8:43–48. [PubMed] [Google Scholar]
- 120.Merino VR, Nakano V, Finegold SM, Avila-Campos MJ. 2014. Genes encoding toxin of Clostridium difficile in children with and without diarrhea. Scientifica 2014:594014. doi: 10.1155/2014/594014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ferreira CEA, Nakano V, Durigon EL, Avila-Campos MJ. 2003. Prevalence of Clostridium spp. and Clostridium difficile in children with acute diarrhea in Sao Paulo City, Brazil. Mem Inst Oswaldo Cruz 98:451–454. doi: 10.1590/S0074-02762003000400003. [DOI] [PubMed] [Google Scholar]
- 122.Nakamura S, Mikawa M, Nakashio S, Takabatake M, Okado I, Yamakawa K, Serikawa T, Okumura S, Nishida S. 1981. Isolation of Clostridium-difficile from the feces and the antibody in sera of young and elderly adults. Microbiol Immunol 25:345–351. doi: 10.1111/j.1348-0421.1981.tb00036.x. [DOI] [PubMed] [Google Scholar]
- 123.Ozaki E. 2004. Clostridium difficile colonization in healthy adults: transient colonization and correlation with enterococcal colonization. J Med Microbiol 53:167–172. doi: 10.1099/jmm.0.05376-0. [DOI] [PubMed] [Google Scholar]
- 124.Kato H, Kita H, Karasawa T, Maegawa T, Koino Y, Takakuwa H, Saikai T, Kobayashi K, Yamagishi T, Nakamura S. 2001. Colonisation and transmission of Clostridium difficile in healthy individuals examined by PCR ribotyping and pulsed-field gel electrophoresis. J Med Microbiol 50:720–727. doi: 10.1099/0022-1317-50-8-720. [DOI] [PubMed] [Google Scholar]
- 125.Sutphen JL, Grand RJ, Flores A, Chang TW, Bartlett JG. 1983. Chronic diarrhea associated with Clostridium difficile in children. Am J Dis Child 137:275–278. [DOI] [PubMed] [Google Scholar]
- 126.Koo HL, Van JN, Zhao M, Ye X, Revell PA, Jiang ZD, Grimes CZ, Koo DC, Lasco T, Kozinetz CA, Garey KW, DuPont HL. 2014. Real-time polymerase chain reaction detection of asymptomatic Clostridium difficile colonization and rising C. difficile-associated disease rates. Infect Control Hosp Epidemiol 35:667–673. doi: 10.1086/676433. [DOI] [PubMed] [Google Scholar]
- 127.Alasmari F, Seiler SM, Hink T, Burnham CA, Dubberke ER. 2014. Prevalence and risk factors for asymptomatic Clostridium difficile carriage. Clin Infect Dis 59:216–222. doi: 10.1093/cid/ciu258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Dubberke ER, Reske KA, Seiler S, Hink T, Kwon JH, Burnham CA. 2015. Risk factors for acquisition and loss of Clostridium difficile colonization in hospitalized patients. Antimicrob Agents Chemother 59:4533–4543. doi: 10.1128/AAC.00642-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Leekha S, Aronhalt KC, Sloan LM, Patel R, Orenstein R. 2013. Asymptomatic Clostridium difficile colonization in a tertiary care hospital: admission prevalence and risk factors. Am J Infect Control 41:390–393. doi: 10.1016/j.ajic.2012.09.023. [DOI] [PubMed] [Google Scholar]
- 130.Soyletir G, Eskiturk A, Kilic G, Korten V, Tozun N. 1996. Clostridium difficile acquisition rate and its role in nosocomial diarrhoea at a university hospital in Turkey. Eur J Epidemiol 12:391–394. doi: 10.1007/BF00145303. [DOI] [PubMed] [Google Scholar]
- 131.Tschudin-Sutter S, Carroll KC, Tamma PD, Sudekum ML, Frei R, Widmer AF, Ellis BC, Bartlett J, Perl TM. 2015. Impact of toxigenic Clostridium difficile colonization on the risk of subsequent C. difficile infection in intensive care unit patients. Infect Control Hosp Epidemiol 36:1324–1329. doi: 10.1017/ice.2015.177. [DOI] [PubMed] [Google Scholar]
- 132.Kong LY, Dendukuri N, Schiller I, Bourgault AM, Brassard P, Poirier L, Lamothe F, Beliveau C, Michaud S, Turgeon N, Toye B, Frost EH, Gilca R, Dascal A, Loo VG. 2015. Predictors of asymptomatic Clostridium difficile colonization on hospital admission. Am J Infect Control 43:248–253. doi: 10.1016/j.ajic.2014.11.024. [DOI] [PubMed] [Google Scholar]
- 133.Longtin Y, Paquet-Bolduc B, Gilca R, Garenc C, Fortin E, Longtin J, Trottier S, Gervais P, Roussy JF, Levesque S, Ben-David D, Cloutier I, Loo VG. 2016. Effect of detecting and isolating Clostridium difficile carriers at hospital admission on the incidence of C difficile infections: a quasi-experimental controlled study. JAMA Intern Med 176:796–804. doi: 10.1001/jamainternmed.2016.0177. [DOI] [PubMed] [Google Scholar]
- 134.Zacharioudakis IM, Zervou FN, Pliakos EE, Ziakas PD, Mylonakis E. 2015. Colonization with toxinogenic C. difficile upon hospital admission, and risk of infection: a systematic review and meta-analysis. Am J Gastroenterol 110:381–390. doi: 10.1038/ajg.2015.22. [DOI] [PubMed] [Google Scholar]
- 135.Rudensky B, Rosner S, Sonnenblick M, Vandijk Y, Shapira E, Isaacsohn M. 1993. The prevalence and nosocomial acquisition of Clostridium-difficile in elderly hospitalized-patients. Postgrad Med J 69:45–47. doi: 10.1136/pgmj.69.807.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hung YP, Tsai PJ, Hung KH, Liu HC, Lee CI, Lin HJ, Wu YH, Wu JJ, Ko WC. 2012. Impact of toxigenic Clostridium difficile colonization and infection among hospitalized adults at a district hospital in southern Taiwan. PLoS One 7:e42415. doi: 10.1371/journal.pone.0042415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Mainardi JL, Lacassin F, Guilloy Y, Goldstein FW, Leport C, Acar JF, Vilde JL. 1998. Low rate of Clostridium difficile colonization in ambulatory and hospitalized HIV-infected patients in a hospital unit: a prospective survey. J Infect 37:108–111. doi: 10.1016/S0163-4453(98)80162-X. [DOI] [PubMed] [Google Scholar]
- 138.Ryan J, Murphy C, Twomey C, Ross RP, Rea MC, MacSharry J, Sheil B, Shanahan F. 2010. Asymptomatic carriage of Clostridium difficile in an Irish continuing care institution for the elderly: prevalence and characteristics. Irish J Med Sci 179:245–250. doi: 10.1007/s11845-009-0361-1. [DOI] [PubMed] [Google Scholar]
- 139.Arvand M, Moser V, Schwehn C, Bettge-Weller G, Hensgens MP, Kuijper EJ. 2012. High prevalence of Clostridium difficile colonization among nursing home residents in Hesse, Germany. PLoS One 7:e30183. doi: 10.1371/journal.pone.0030183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rogers DS, Kundrapu S, Sunkesula VC, Donskey CJ. 2013. Comparison of perirectal versus rectal swabs for detection of asymptomatic carriers of toxigenic Clostridium difficile. J Clin Microbiol 51:3421–3422. doi: 10.1128/JCM.01418-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Rea MC, O'Sullivan O, Shanahan F, O'Toole PW, Stanton C, Ross RP, Hill C. 2012. Clostridium difficile carriage in elderly subjects and associated changes in the intestinal microbiota. J Clin Microbiol 50:867–875. doi: 10.1128/JCM.05176-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Riggs MM, Sethi AK, Zabarsky TF, Eckstein EC, Jump RL, Donskey CJ. 2007. Asymptomatic carriers are a potential source for transmission of epidemic and nonepidemic Clostridium difficile strains among long-term care facility residents. Clin Infect Dis 45:992–998. doi: 10.1086/521854. [DOI] [PubMed] [Google Scholar]
- 143.Ziakas PD, Zacharioudakis IM, Zervou FN, Grigoras C, Pliakos EE, Mylonakis E. 2015. Asymptomatic carriers of toxigenic C. difficile in long-term care facilities: a meta-analysis of prevalence and risk factors. PLoS One 10:e0117195. doi: 10.1371/journal.pone.0117195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.van Nood E, van Dijk K, Hegeman Z, Speelman P, Visser CE. 2009. Asymptomatic carriage of Clostridium difficile among HCWs: do we disregard the doctor? Infect Control Hosp Epidemiol 30:924–925. doi: 10.1086/605642. [DOI] [PubMed] [Google Scholar]
- 145.Carmeli YVL, DeGirolami PC, Lichtenberg DA, Karchmer AW, Samore MB. 1998. Stool colonization of healthcare workers with selected resistant bacteria. Infect Control Hosp Epidemiol 19:38–40. [DOI] [PubMed] [Google Scholar]
- 146.Friedman ND, Pollard J, Stupart D, Knight DR, Khajehnoori M, Davey EK, Parry L, Riley TV. 2013. Prevalence of Clostridium difficile colonization among healthcare workers. BMC Infect Dis 13:459. doi: 10.1186/1471-2334-13-459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Hell M, Sickau K, Chmelizek G, Kern JM, Maass M, Huhulescu S, Allerberger F. 2012. Absence of Clostridium difficile in asymptomatic hospital staff. Am J Infect Control 40:1023–1024. doi: 10.1016/j.ajic.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 148.Sall O, Johansson K, Noren T. 2015. Low colonization rates of Clostridium difficile among patients and healthcare workers at Orebro University Hospital in Sweden. APMIS 123:240–244. doi: 10.1111/apm.12353. [DOI] [PubMed] [Google Scholar]
- 149.Landelle C, Verachten M, Legrand P, Girou E, Barbut F, Brun Buisson C. 2014. Contamination of healthcare workers' hands with Clostridium difficile spores after caring for patients with C. difficile infection. Infect Control Hosp Epidemiol 35:10–15. doi: 10.1086/674396. [DOI] [PubMed] [Google Scholar]
- 150.Samore MH, Venkataraman L, DeGirolami PC, Arbeit RD, Karchmer AW. 1996. Clinical and molecular epidemiology of sporadic and clustered cases of nosocomial Clostridium difficile diarrhea. Am J Med 100:32–40. doi: 10.1016/S0002-9343(96)90008-X. [DOI] [PubMed] [Google Scholar]
- 151.Johnson S, Clabots CR, Linn FV, Olson MM, Peterson LR, Gerding DN. 1990. Nosocomial Clostridium-difficile colonization and disease. Lancet 336:97–100. doi: 10.1016/0140-6736(90)91605-A. [DOI] [PubMed] [Google Scholar]
- 152.Johnson S, Homann SR, Bettin KM, Quick JN, Clabots CR, Peterson LR, Gerding DN. 1992. Treatment of asymptomatic Clostridium difficile carriers (fecal excretors) with vancomycin or metronidazole. A randomized, placebo-controlled trial. Ann Intern Med 117:297–302. [DOI] [PubMed] [Google Scholar]
- 153.Prasad N, Labaze G, Kopacz J, Chwa S, Platis D, Pan CX, Russo D, LaBombardi VJ, Osorio G, Pollack S, Kreiswirth BN, Chen L, Urban C, Segal-Maurer S. 2016. Asymptomatic rectal colonization with carbapenem-resistant Enterobacteriaceae and Clostridium difficile among residents of a long-term care facility in New York City. Am J Infect Control 44:525–532. doi: 10.1016/j.ajic.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 154.Akerlund T, Persson I, Unemo M, Noren T, Svenungsson B, Wullt M, Burman LG. 2008. Increased sporulation rate of epidemic Clostridium difficile type 027/NAP1. J Clin Microbiol 46:1530–1533. doi: 10.1128/JCM.01964-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Brazier JS, Fitzgerald TC, Hosein I, Cefai C, Looker N, Walker M, Bushell AC, Rooney P. 1999. Screening for carriage and nosocomial acquisition of Clostridium difficile by culture: a study of 284 admissions of elderly patients to six general hospitals in Wales. J Hosp Infect 43:317–319. doi: 10.1016/S0195-6701(99)90431-0. [DOI] [PubMed] [Google Scholar]
- 156.Freeman J, Vernon J, Morris K, Nicholson S, Todhunter S, Longshaw C, Wilcox MH, Pan-European Longitudinal Surveillance of Antibiotic Resistance among Prevalent Clostridium difficile Ribotypes' Study Group. 2015. Pan-European longitudinal surveillance of antibiotic resistance among prevalent Clostridium difficile ribotypes. Clin Microbiol Infect 21:248.e9–248.e16. doi: 10.1016/j.cmi.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 157.Zomer TP, Van Duijkeren E, Wielders CCH, Veenman C, Hengeveld P, Van Der Hoek W, De Greeff SC, Smit LAM, Heederik DJ, Yzermans CJ, Kuijper EJ, Maassen CBM. 2017. Prevalence and risk factors for colonization of Clostridium difficile among adults living near livestock farms in the Netherlands. Epidemiol Infect 145:2745–2749. doi: 10.1017/S0950268817001753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Stoesser N, Eyre DW, Quan TP, Godwin H, Pill G, Mbuvi E, Vaughan A, Griffiths D, Martin J, Fawley W, Dingle KE, Oakley S, Wanelik K, Finney JM, Kachrimanidou M, Moore CE, Gorbach S, Riley TV, Crook DW, Peto TEA, Wilcox MH, Walker AS. 2017. Epidemiology of Clostridium difficile in infants in Oxfordshire, UK: risk factors for colonization and carriage, and genetic overlap with regional C. difficile infection strains. PLoS One 12:e0182307. doi: 10.1371/journal.pone.0182307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Furuya-Kanamori L, Clements AC, Foster NF, Huber CA, Hong S, Harris-Brown T, Yakob L, Paterson DL, Riley TV. 2017. Asymptomatic Clostridium difficile colonisation in two Australian tertiary hospitals, 2012–2014: a prospective, repeated cross-sectional study. Clin Microbiol Infect 23:48.e1–48.e7. doi: 10.1016/j.cmi.2016.08.030. [DOI] [PubMed] [Google Scholar]
- 160.Shim JK, Johnson S, Samore MH, Bliss DZ, Gerding DN. 1998. Primary symptomless colonisation by Clostridium difficile and decreased risk of subsequent diarrhoea. Lancet 351:633–636. doi: 10.1016/S0140-6736(97)08062-8. [DOI] [PubMed] [Google Scholar]
- 161.Bliss DZ, Johnson S, Savik K, Clabots CR, Willard K, Gerding DN. 1998. Acquisition of Clostridium difficile and Clostridium difficile-associated diarrhea in hospitalized patients receiving tube feeding. Ann Intern Med 129:1012–1019. doi: 10.7326/0003-4819-129-12-199812150-00004. [DOI] [PubMed] [Google Scholar]
- 162.Bruminhent J, Wang ZX, Hu C, Wagner J, Sunday R, Bobik B, Hegarty S, Keith S, Alpdogan S, Carabasi M, Filicko-O'Hara J, Flomenberg N, Kasner M, Outschoorn UM, Weiss M, Flomenberg P. 2014. Clostridium difficile colonization and disease in patients undergoing hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 20:1329–1334. doi: 10.1016/j.bbmt.2014.04.026. [DOI] [PubMed] [Google Scholar]
- 163.Gupta SB, Mehta V, Herring TA, Dubberke E, Gerding DN, Saddier P, Sambol SP, Walter T, Kaslow DC, Miller M. 2012. A large prospective North American epidemiologic study of hospital-associated Clostridium difficile colonization & infection, abstr 020. 4th Int Clostridium difficile Symp, Bled, Slovenia. [Google Scholar]
- 164.Marciniak C, Chen D, Stein AC, Semik PE. 2006. Prevalence of Clostridium difficile colonization at admission to rehabilitation. Arch Phys Med Rehab 87:1086–1090. doi: 10.1016/j.apmr.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 165.Zhang X, Wang X, Yang J, Liu X, Cai L, Zong Z. 2016. Colonization of toxigenic Clostridium difficile among ICU patients: a prospective study. BMC Infect Dis 16:397. doi: 10.1186/s12879-016-1729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Grigoras CA, Zervou FN, Zacharioudakis IM, Siettos CI, Mylonakis E. 2016. Isolation of C. difficile carriers alone and as part of a bundle approach for the prevention of Clostridium difficile infection (CDI): a mathematical model based on clinical study data. PLoS One 11:e0156577. doi: 10.1371/journal.pone.0156577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Lanzas C, Dubberke ER. 2014. Effectiveness of screening hospital admissions to detect asymptomatic carriers of Clostridium difficile: a modeling evaluation. Infect Control Hosp Epidemiol 35:1043–1050. doi: 10.1086/677162. [DOI] [PubMed] [Google Scholar]
- 168.Crobach MJ, Terveer EM, Kuijper EJ. 2016. Effect of detecting and isolating asymptomatic Clostridium difficile carriers. JAMA Intern Med 176:1572–1573. doi: 10.1001/jamainternmed.2016.5339. [DOI] [PubMed] [Google Scholar]
- 169.Feazel LM, Malhotra A, Perencevich EN, Kaboli P, Diekema DJ, Schweizer ML. 2014. Effect of antibiotic stewardship programmes on Clostridium difficile incidence: a systematic review and meta-analysis. J Antimicrob Chemother 69:1748–1754. doi: 10.1093/jac/dku046. [DOI] [PubMed] [Google Scholar]
- 170.Wenzler E, Mulugeta SG, Danziger LH. 2015. The antimicrobial stewardship approach to combating Clostridium difficile. Antibiotics (Basel) 4:198–215. doi: 10.3390/antibiotics4020198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Davey P, Brown E, Charani E, Fenelon L, Gould IM, Holmes A, Ramsay CR, Wiffen PJ, Wilcox M. 2013. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev 2013:CD003543. doi: 10.1002/14651858.CD003543.pub3. [DOI] [PubMed] [Google Scholar]
- 172.Drekonja DM, Amundson WH, Decarolis DD, Kuskowski MA, Lederle FA, Johnson JR. 2011. Antimicrobial use and risk for recurrent Clostridium difficile infection. Am J Med 124:1081.e1–1081.e7. doi: 10.1016/j.amjmed.2011.05.032. [DOI] [PubMed] [Google Scholar]