Abstract
Background
The Pacific Islands have environmental conditions highly favourable for transmission of leptospirosis, a neglected zoonosis with highest incidence in the tropics, and Oceania in particular. Recent reports confirm the emergence and outbreaks of leptospirosis in the Pacific Islands, but the epidemiology and drivers of transmission of human and animal leptospirosis are poorly documented, especially in the more isolated and less developed islands.
Methodology/Principal findings
We conducted a systematic review of human and animal leptospirosis within 25 Pacific Islands (PIs) in Polynesia, Melanesia, Micronesia, as well as Easter Island and Hawaii. We performed a literature search using four international databases for articles published between January 1947 and June 2017. We further included grey literature available on the internet. We identified 148 studies describing leptospirosis epidemiology, but the number of studies varied significantly between PIs. No data were available from four PIs. Human leptospirosis has been reported from 13 PIs, with 63% of all studies conducted in Hawaii, French Polynesia and New Caledonia. Animal leptospirosis has been investigated in 19 PIs and from 14 host species, mainly pigs (18% of studies), cattle (16%) and dogs (11%). Only 13 studies provided information on both human and animal leptospirosis from the same location. Serology results were highly diverse in the region, both in humans and animals.
Conclusions/Significance
Our study suggests that, as in other tropical regions, leptospirosis is widespread in the PIs while showing some epidemiological heterogeneity. Data are scarce or absent from many PIs. Rodents, cattle, pigs and dogs are all likely to be important carriers, but the relative importance of each animal species in human infection needs to be clarified. Epidemiological surveys with appropriate sampling design, pathogen typing and data analysis are needed to improve our understanding of transmission patterns and to develop effective intervention strategies.
Author summary
Leptospirosis is an important bacterial zoonosis that affects people and animals worldwide. It is common in tropical areas, especially in island ecosystems. Because islands are relatively small, isolated, and have limited health and diagnostic facilities, the disease burden is often underestimated. In this systematic review, we aimed to describe the extent of leptospirosis in the Pacific Islands, including the diversity of pathogens and animal reservoirs. We identified 148 studies from 21 Pacific islands that described Leptospira infection in humans or animals. In hospitalized febrile patients, leptospirosis was a common cause of the acute febrile illness, but accurate diagnosis was challenging and often delayed because symptoms overlapped with many other infectious diseases, and access to laboratory diagnosis was limited. A wide variety of animal hosts of Leptospira were identified, with rodents, cattle, pigs and dogs reported as important hosts; however, their relative importance in human infection remains unclear. Our review demonstrates that the epidemiology of leptospirosis varies across the Pacific Islands, but information about risk factors and transmission routes is currently limited. We recommend more integrated studies, using an eco-epidemiological approach that includes human, veterinary and environmental factors, and interactions between factors at different ecological scales.
Introduction
Leptospira is a genus of bacteria belonging to the phylum of Spirochaetes causing leptospirosis in humans and other mammals [1]. Leptospirosis is the most widespread and potentially fatal bacterial zoonosis worldwide [2], with an estimated 1.03 million human cases and 58,900 deaths worldwide each year [3]. The majority of the disease burden occurs in tropical regions where large epidemics can occur after heavy rainfall and flooding [4]. Leptospirosis is a neglected disease in most of the tropics, especially in the Pacific region [5], and a recent systematic review found that Oceania was the region most impacted by leptospirosis in terms of morbidity (150.68 cases per 100,000 per year), mortality (9.61 deaths per 100,000 per year) [3], and disability adjusted life years (DALY) [6]. Incidence of up to 1,945 cases per 100,000 population has been reported in 2008 in Futuna (a Polynesian island) during a multi-year outbreak [7]. The health impacts of leptospirosis have been predominantly attributed to acute infections and early complications such as pulmonary haemorrhage and renal failure. However, leptospirosis can also cause subacute and chronic complications and long-term sequelae [8].
Two classification schemes are used for Leptospira, one based on serology with the serovar as the basic taxon, and another which uses molecular taxonomy to identify the species, sometimes referred to as genomospecies [2]. Leptospira have been classified serologically into over 300 serovars grouped in almost 30 serogroups (both saprophytic and pathogenic) using Microscopic Agglutination Test (MAT) and Cross Agglutination Absorption Test (CAAT) [9, 10]. Phylogenetically, the genus Leptospira is divided into 23 species based on 16S rRNA phylogeny and DNA-DNA hybridization, and clustered into saprophytic, intermediate and pathogenic groups [11]. Laboratory diagnosis of leptospirosis may be accomplished by direct detection of the organism or its components in body fluid or tissues, by isolation of leptospires in cultures, or by detection of specific antibodies [12, 13]. Molecular diagnosis is based on Leptospira DNA amplification from serum, urine, aqueous humour, cerebrospinal fluid (CSF) or post-mortem tissue samples [14]. Historically, most cases of leptospirosis have been diagnosed by serology, because capacity for culture and PCR were limited. IgM antibodies are detectable in the blood from 5–7 days after the onset of symptoms [2]. The use of agglutination tests was described soon after the first isolation of the organism, and the MAT remains the definitive serological investigation technique in both humans and animals [15].
Human infections range from, most commonly, a mild ‘flu-like illness, to severe complications including acute renal failure and pulmonary haemorrhagic syndrome associated with high fatality rates. Infection results from direct or indirect exposure to urine from infected reservoir host animals that carry the pathogen in their renal tubules and shed pathogenic leptospires which contaminate soils, surface waters, streams and rivers [2]. Humans are infected via mucous membranes, abrasions or cuts in the skin. Prolonged immersion in, or swallowing of, contaminated water can also result in infection. Numerous animal species, including rodents (often considered as the main reservoir), domestic mammals (including livestock and companion animals) and wildlife, have been shown to be reservoirs for Leptospira [15]. In food-producing animals, cattle and pigs are relatively susceptible to clinical infection, resulting in production losses including reduced milk yield, reproductive failure, abortions, premature birth or stillbirth [16].
The Oceania region includes Australia, New Zealand and the Pacific Islands Countries and Territories (PICTs), these latter all falling within the tropics. Poverty, remoteness and tropical climate all contribute to vulnerability to, and significant burden of, infectious diseases in the PICTs [17]. Global emergence of leptospirosis has been associated with environmental factors including rainfall, flooding, poverty, and urbanization [18–20], all of which are important drivers of transmission in the Pacific Islands. Recent reports confirm the emergence of leptospirosis in the Pacific region, with increase in incidence and reports of unprecedented outbreaks [5, 21]. However, the incidence of leptospirosis is unfortunately not well-documented from many Pacific Islands, mainly because of the unavailability of laboratory diagnosis [22, 23], poor medical awareness, and non-specific symptoms that overlap with many other tropical infectious diseases, especially arbovirus infections [24]. As a consequence, little is known about the ecological, epidemiological and clinical characteristics of leptospirosis in the region, and the burden of the disease might be even higher than recognized.
To tackle these gaps in current knowledge and understanding of human and animal leptospirosis infection in the Pacific Islands, we conducted a systematic review of both peer-reviewed and grey literature following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [25]. Our aims were to summarise and compare human and animal leptospirosis within and between the Pacific Islands.
Methods
Geographic scope
The selection of the countries and territories to be included in this review was based on the official list of the United Nations Statistics Division for the geographical region #009 Oceania (http://unstats.un.org/unsd/methods/m49/m49regin.htm#oceania). We excluded Australia and New Zealand (#053) and focused on the small islands of the PICTs including five in Melanesia (Fiji, New Caledonia, Papua New Guinea, Solomon Islands, Vanuatu), eight in Micronesia (Guam, Kiribati, Marshall Islands, Federated States of Micronesia, Nauru, Mariana Islands, Palau, United States Minor Outlying Islands) and ten in Polynesia (American Samoa, Cook Islands, French Polynesia, Niue, Pitcairn Islands, Samoa, Tokelau, Tonga, Tuvalu, and Wallis and Futuna). The “United States Minor Outlying Islands” were restricted to Wake Island in our study. We further included Easter Island (Chile) as well as Hawaii (U.S.A.) (Fig 1). Except for Papua New Guinea and Hawaii, the included PIs had populations of less than one million inhabitants and represented significant diversity in economies, geography, culture and living conditions. For ease of reference, the 25 countries and territories included in this review will be referred to as ‘Pacific Islands’ (PIs).
Fig 1. Map of the South Pacific region.
All countries in Oceania were included in this review with the exception of Australia and New Zealand. Easter Island does not appear on the map but was included in our study. ‘W&F’: Wallis and Futuna. ‘Am.Sam.’: American Samoa. The map was provided by the Pacific Community (SPC) and is available online at: http://pacific.popgis.spc.int.
Search strategy
Peer-reviewed studies were sought in June 2017 from four international databases (PubMed, Web of Science, Scopus, and Embase (Ovid)) for resources published between January 1947 and June 2017 inclusively, either in English or in French, and following the PRISMA guidelines [25] (S1 Appendix). The search strategy is presented in detail in S2 Appendix. Secondly, additional peer-reviewed studies were retrieved by examining the references from the papers identified by the initial electronic search. Thirdly, grey literature (i.e. print and electronic formats that have not been formally published by commercial publishers) were reviewed by scrutinising the websites of government health departments and other relevant administrative bodies of the Pacific Islands (see S2 Appendix for the list of websites browsed), and by bibliography hand searches of relevant articles from Google Scholar (https://scholar.google.com).
Eligibility criteria
Inclusion criteria
A publication was included in this review if it contained qualitative and/or quantitative information on human or/and animal leptospirosis in the PIs, including environmental studies, case reports, outbreak description or epidemiologic surveys. Conference papers were included if they contained relevant information not published in a peer-reviewed journal.
Exclusion criteria for title and abstract review
Reviews or summary articles, editorials, letters to the editor, opinions or commentaries without original data were excluded, as well as lay media publications or broadcasts. We further excluded publications focusing on (i) the wrong geographic location, (ii) the wrong agent/disease, (iii) experimental data (in vitro or in vivo cellular, molecular, biochemical or other studies that did not include naturally occurring cases of leptospirosis in humans or animals), and (iv) descriptions or studies of laboratory methods. The inclusion and exclusion criteria were applied to the title and abstract of all retrieved references. References for which no abstract was available were included in the next stage of full text review.
Exclusion criteria during full-text review
The full texts of articles classified as eligible for inclusion were retrieved and assessed against the same exclusion criteria as per abstract review. Any articles where the country was not specified were excluded, as well as references for which the methods or study population were not described in sufficient detail to determine whether the study met inclusion or exclusion criteria. When more than one reference was retrieved for the same study, or when the same data were retrieved under different formats (publications, project reports, conference presentation), only the most comprehensive one was retained. We included reports of returned travellers despite a potential uncertainty around the specific location where infection was acquired, because for some of the Pacific Islands considered, this was the only information/evidence available. Studies for which the full text was not available were excluded except when relevant data (qualitative or quantitative) were available from the abstract or from a later published study.
Data collection process
The data collection process was undertaken in two steps. First, abstracts and titles were compiled in EndNote (Thomson Reuters, Philadelphia, PA, USA) and reviewed by one researcher (VG) on the basis of the abstract and title. Second, the articles identified through the pre-selection process were retrieved in full text format and reviewed independently by two researchers for the full text (VG and either CG, JB or CLL). A third researcher served as a tiebreaker for any discordant decisions.
Following the inclusion/exclusion process, qualitative and quantitative data were extracted from each of the included articles. Papers were classified into human clinical studies, human community-based studies, and animal population studies (no animal clinical studies were identified). For human studies, information was compiled on the country, year(s) of study, study design, target population, inclusion criteria, number enrolled, diagnostic tests used, confirmed leptospirosis cases and risk factors. For animal studies, information was compiled on country, year(s) of study, species investigated, methodology, number of samples, and confirmed positivity for Leptospira. When available, data on serology and genetic typing of isolates from humans and animals were also compiled and summarised by country and by animal species.
Case definition and strength of evidence of results
MAT is a serogroup-specific assay and does not provide reliable information on the infecting serovar [26, 27]; results were therefore summarised at the serogroup level even if studies reported MAT results at the serovar level. Although serogroups are no longer used in the taxonomic classification of serovars, they remain useful for laboratory purposes and epidemiological comparisons.
As the definition of a “positive” serology result differed between studies, we standardised results across the studies by using the following case definitions:
For the human clinical studies, a confirmed case was defined based on the recommendations of the WHO LERG report [28] as follows: clinical signs and symptoms consistent with leptospirosis and one or more of the following: (i) positive PCR or isolation by culture; (ii) seroconversion or fourfold increase in MAT titre between acute and convalescent serum samples; (iii) MAT titre ≥ 1:400 in single serum sample. Cases that fitted the confirmed case definition were considered “strong evidence” whereas others were considered “weak evidence”.
For the seroprevalence studies (human or animal), any positive MAT result (as defined by the individual studies, from 1:50 upwards) was considered to indicate previous infection. However, opportunistic sampling of animals with less than ten individuals of a species was considered as “weak evidence”.
Any result based on Leptospira isolates was considered “strong evidence”.
When MAT results were detailed, the serogroup with the highest titre was reported as putatively involved. If equally high titres were reported for more than one serogroup, MAT was considered positive but serogroup results were not reported. If data were not detailed enough to allow interpretation (especially in the case of cross-reactions), serogroup results were not reported.
Critical assessment of data quality and possible bias
Because of the great heterogeneity in the methodology and the quality of the data between studies, most of the data reported in our review are qualitative rather than quantitative. As detailed in the previous paragraph, methodological quality was assessed for serology studies by comparison to pre-determined case definition criteria to control for heterogeneity in study design and diagnostic methodology. Evidence of Leptospira infection was assessed for each study as ‘strong’ or ‘weak’. The sample sizes (number of animal tested, number of clinical cases reported) are reported in our review when necessary, as an indication of the degree of confidence of the results. Exposure and risk factors are reported as per the included studies, and are considered mostly as untested hypotheses. Epidemiological studies providing risk factors based on robust analyses are highlighted.
Results
Selected studies
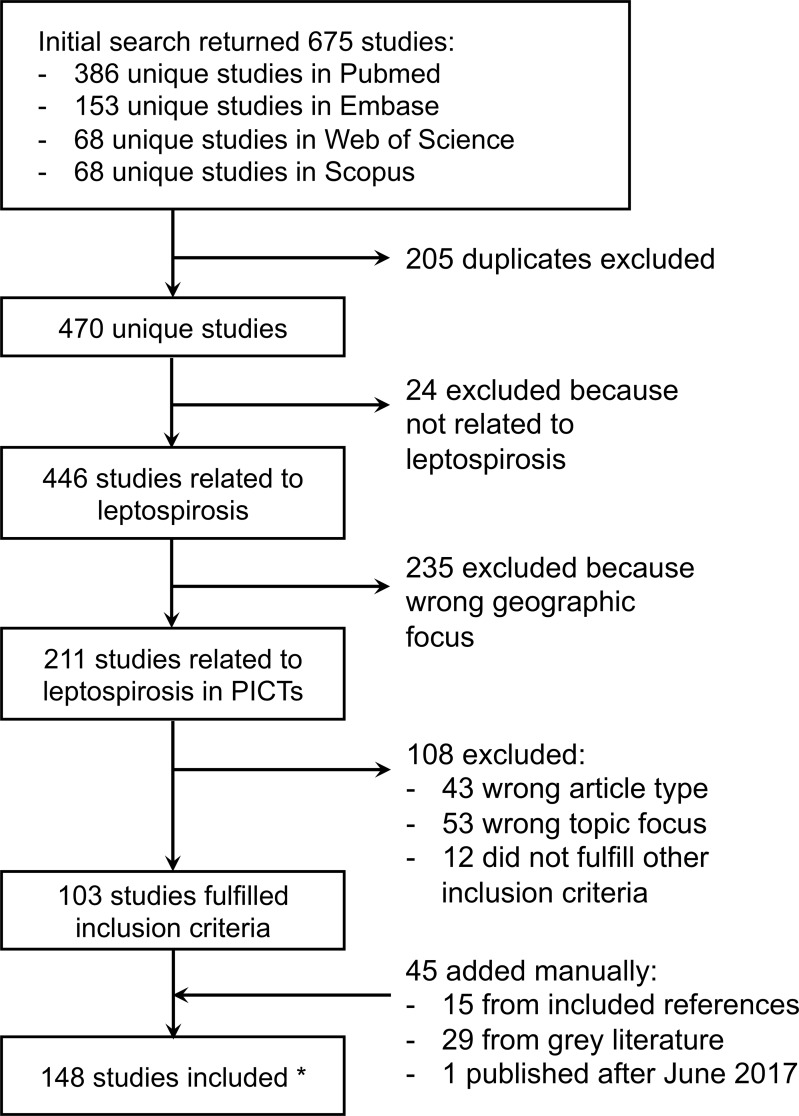
The initial search retrieved a total of 675 studies, including 386 on PubMed, 68 on Scopus, 68 on Web of Science, and 153 on Embase respectively. After removing 205 duplicates, 103 met the inclusion and exclusion criteria. A further 44 studies were identified, either from the reference list of already included papers (n = 15), or when searching internet websites for grey literature (n = 29). One publication from the last author of the present review (CL) that was accepted for publication after the search in June was also added, making a final list of 148 studies. For 11 studies, the full text document could not be retrieved but quantitative and/or qualitative data were available from the abstract, or from the full text of later published papers. The flow diagram of the search strategy is summarised in Fig 2.
Fig 2. Flow diagram of the systematic review and identification of studies.
*Among the 148 included studies, 11 full texts could not be retrieved but quantitative and/or qualitative data were collected from the abstract or from the full text of later published studies.
The included leptospirosis studies were conducted in 21 out of the 25 PIs within the scope of our study. No information about leptospirosis was retrieved from Nauru, Pitcairn Islands, Tuvalu and Wake Island. Included studies were mostly either dedicated to animals (n = 54, 36.5%) or humans (n = 79, 53.4%), while very few studies (n = 13, 8.7%) provided information on both animals and humans. The remaining two studies (1.4%) focused on Leptospira in the environment [29, 30]. Detailed information on each study is provided in S1 Table.
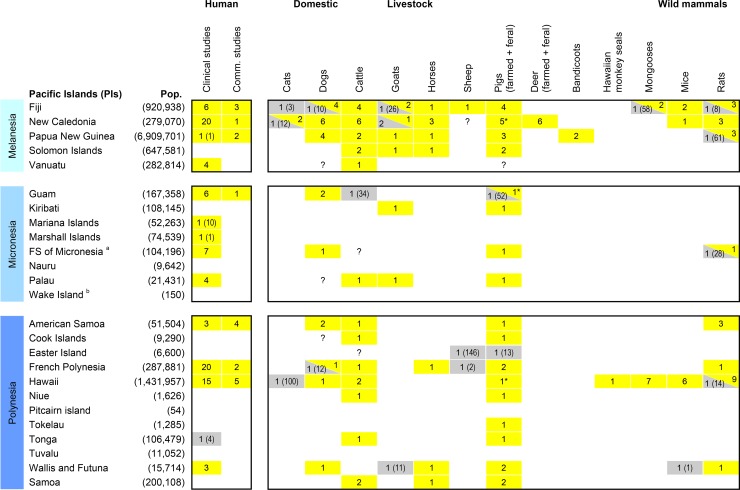
Human leptospirosis studies
Human leptospirosis was investigated in 92 eligible studies from 14 PIs. We classified human studies into two categories: community-based studies (investigating healthy people) and clinical studies (investigating people who were unwell) (see Fig 3 and S1 Table). Community-based studies consisted of 19 (21%) seroprevalence studies, of which six were “mixed” studies that also included clinical case reports. The remaining 73 studies (79%) were clinical, including surveillance data, case reports or leptospirosis investigation in sick and/or hospitalised patients). Clinical studies were reported as strong or weak evidence of leptospirosis following the criteria detailed in the methods section (see S1 Table for detailed classification). French Polynesia was the most frequently represented PI with a total of 22 studies [5, 24, 31–48], followed by 20 from New Caledonia [32, 36, 42, 49–65] and 19 from Hawaii [66–84]. Of the 14 PIs investigated, confirmed cases were reported from 13 PIs only as four suspected leptospirosis cases investigated in Tonga were later reported as negative [5].
Fig 3. Number of studies that reported Leptospira infection from humans and/or animals in the Pacific Islands (PIs).
Empty cells correspond to PIs/species for which no studies were retrieved; coloured cells and numbers correspond to PIs/species for which studies were retrieved, and the number of studies included in this review. The presence or absence of Leptospira is reported in yellow or grey respectively. For animal studies that provided no evidence of Leptospira infection, the number of tested animals is given in brackets to provide an indication of the degree of confidence of the negative results. Similarly, when only one human clinical study was conducted in a specific PI, the number of reported cases is given in brackets. a Federated States of Micronesia; b Wake Island is part of the United States Minor Outlying Islands. ‘Pop’: July 2016 estimated population size reported from the CIA World Factbook (https://www.cia.gov/library/) except for Hawaii, Wake Island and Easter Island for which data were retrieved from different internet sources. ‘Comm. studies’: human community-based studies. ‘*’: includes one study on feral pigs. ‘?’: inconclusive results (reported from [85]).
Animal leptospirosis studies
Past infection with, or renal carriage of, leptospires in animals was investigated in 66 eligible studies from 19 PIs, plus one paper that reported animal leptospirosis from 22 PIs [85] (S1 Table). In total, 13 different animal species were tested: bandicoots (Echymipera kalubu), cats (Felis catus), cattle (Bos spp.), deer (Rusa timorensis), dogs (Canis lupus), pigs (Sus scrofa), goats (Capra aegagrus), horses (Equus ferus), mongooses (Herpestes auropunctatus), mice (Mus musculus), rats (Rattus spp.), sheep (Ovis aries), and in one case, Hawaiian monkey seals (Monachus schauinslandi). Both feral and farmed populations of pigs and deer were investigated. Livestock represented the majority of the investigations, i.e. farmed pigs (29 studies from 18 PIs) and cattle (27 studies from 14 PIs), followed by rats (28 studies from 8 PIs) and domestic dogs (24 studies from 9 PIs).
The majority of animal studies (n = 54, 82%) were seroprevalence studies. Renal carriage was also investigated (n = 14, 21%) especially in rats, either alone or in combination with serology. Older studies reported the presence of leptospires in kidneys from microscopic examination of tissues or by experimental infection of guinea pigs (e.g. by injection of crushed rat kidneys), while more recent studies used real-time PCR for confirmation of infection. Evidence of past or present Leptospira infection was most commonly found in farmed pigs (27 studies from 15 PIs) followed by cattle (24 studies from 13 PIs), rats (24 studies from 8 PIs) and dogs (22 studies from 9 PIs) (Fig 3). There was variation in the sample sizes between studies, ranging from one animal tested in some studies that reported on opportunistic sampling of animals to about 9,000 animals in a study of cattle in the Solomon Islands [86].
Serology results by serogroup
Studies reported a total of 21 putative Leptospira serogroups in humans or animals across the Pacific, the most common being Icterohaemorrhagiae (15 PIs), Pomona (15 PIs), Australis (14 PIs) and Sejroe (13 PIs). Table 1 summarises the serogroups reported for humans and animal species for each PI. However, this finding should be interpreted with caution because of the many limitations of the MAT, including cross-reactions between serovars and serogroups, paradoxical reactions or anamnestic responses [2, 87]. MAT results might also vary depending on the panel of serovars used.
Table 1. Summary of serology results.
Results are reported at the serogroup level. Human studies include both clinical and seroprevalence studies, while animal studies are seroprevalence only. A specific serogroup is reported as present in a PI if it was reported from at least one study over the 1947–2017 period, meaning that studies classified as ‘weak evidence’ for leptospirosis were also included. For this reason, and because of the limitations of the MAT, results should be interpreted with caution.
| Pacific Islands (PIs) | Serogroups | Australis | Autumnalis | Ballum | Bataviae | Canicola | Celledoni | Cynopteri | Djasiman | Grippotyphosa | Hebdomadis | Icterohaemorrhagiae | Javanica | Mini | Panama | Pomona | Pyrogenes | Santarosai | Sarmin | Sejroe | Shermani | Tarassovi | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Melanesia | Fiji | human | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||||||||||||
| animal | mice, cattle, goat, rat, mongoose, pig, sheep, cattle, dog, rat, horse | mice, pig, sheep, cattle, goat, rat, mongoose, horse, dog | cattle, pig, horse, dog, mice, mongoose | cattle, goat, rat, horse | cattle, horse, dog, pig | pig, horse | cattle, pig, horse | cattle, pig, horse | cattle, mongoose | cattle, goat, pig, horse, dog, rat | pig | cattle, mongoose | cattle | pig, goat, cattle, horse | cattle, goat, pig, horse, dog | cattle | pig, horse | cattle, goat, pig, horse, mongoose | cattle, horse, dog | ||||
| New Caledonia | human | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||||
| animal | cattle, deer, horse, dog | cattle, deer, horse, dog | cattle, deer, horse, dog, cat | cattle, deer, cat | cattle, deer, horse, dog, cat | cattle, deer, horse, dog, cat | rat, cattle, pig, deer, horse, dog, cat | cattle, horse, cat | pig, deer, horse | cattle, horse, dog | pig, cattle, deer, dog | cattle, deer | |||||||||||
| Papua New Guinea | human | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||||||||
| animal | dog, pig, goat, rat, cattle, bandicoot | dog, pig, goat, rat | goat, cattle, horse | rat, dog, pig, goat, horse | dog, pig | dog, pig | dog, pig, horse, rat | dog, pig, rat, cattle | dog, pig, rat | dog, pig, rat, cattle | dog, pig, goat, rat, cattle | dog, pig, bandicoot | dog, pig, cattle, horse, rat | dog, pig, cattle, horse, rat, bandicoot | |||||||||
| Solomon Is. | animal | cattle, pig, horse | cattle | cattle, horse | cattle, pig | pig | cattle, goat, horse | cattle, horse | |||||||||||||||
| Vanuatu | human | ✔ | ✔ | ✔ | ✔ | ✔ | |||||||||||||||||
| animal | cattle | cattle | cattle | cattle | |||||||||||||||||||
| Micronesia | Guam | animal | feral pig | feral pig, dog | feral pig | feral pig | |||||||||||||||||
| Kiribati | animal | pig? | goat, pig? | goat | goat | ||||||||||||||||||
| FSM | human | ✔ | ✔ | ✔ | ✔ | ||||||||||||||||||
| animal | dog, rat, pig | rat, pig | pig | pig | pig | pig | pig | dog, pig | pig | pig | pig | pig | dog | ||||||||||
| Palau | human | ✔ | ✔ | ||||||||||||||||||||
| animal | goat | pig | pig | pig | pig | pig | pig | pig | goat, pig | cattle, pig | pig | ||||||||||||
| Polynesia | American Samoa | human | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||||||||||||||
| animal | rat? | dog | dog | ||||||||||||||||||||
| Cook Is. | animal | pig | cattle | cattle | |||||||||||||||||||
| French Polynesia | human | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||
| animal | cattle, pig, horse | cattle, pig | cattle, pig | pig | pig | cattle | cattle, pig, horse | cattle, pig, horse | cattle | cattle, pig | |||||||||||||
| Hawaii | human | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||||||||
| animal | mongoose, feral pig, rat, cattle, HMS | feral pig | rat, mice, mongoose | cattle | mongoose | feral pig | feral pig | rat, feral pig, mongoose, mice, HMS | feral pig | feral pig, HMS | feral pig | cattle, HMS, rat, mice, mongoose | |||||||||||
| Tokelau | animal | pig | pig | ||||||||||||||||||||
| Tonga | animal | pig | cattle | cattle | pig | cattle, pig | cattle | cattle | |||||||||||||||
| Wallis and Futuna | human | ✔ | ✔ | ✔ | ✔ | ||||||||||||||||||
| animal | dog, pig | dog, pig | dog, pig | dog | dog, pig | dog, pig | pig | dog, pig | pig | pig | pig | ||||||||||||
| Samoa | animal | cattle, horse, pig | cattle, pig | cattle, pig | horse, pig | cattle, horse, pig | horse, pig | pig | cattle, horse | cattle, horse, pig | cattle, horse | cattle, horse, pig | cattle, horse | cattle, pig | cattle, horse, pig | cattle, pig | cattle | cattle, pig |
Hawaii
Human leptospirosis was recognised as early as 1936 in Hawaii; seroprevalence studies investigated the general population in Honolulu [66] and sugar cane workers [67] in 1936–1942, and revealed seroprevalence rates of 3.8% (13/344) and 12.2% (105/860) respectively, using a cut-off titre of 1:100. A seroprevalence study of US army blood bank donors conducted in 2002 in Oahu found a positivity rate of 1.4% (7/488) [79]. Sixteen publications reported leptospirosis cases from surveillance data and clinical studies between 1962 and 2008. Information by island was not always available as surveillance data generally included cases from all islands, but a few studies were dedicated to Kauai and Oahu, reporting sporadic cases. One study investigated cases of leptospirosis during an outbreak of murine typhus on Kauai (1998) and reported two cases of co-infection with both diseases [76]. The complete list of human studies from Hawaii is reported in Table 2.
Table 2. Summary of publications reporting human leptospirosis in Hawaii, 1947–2017.
| Citation | Study years | Case reports | Seroprevalence studies | Exposure/risk factors |
|---|---|---|---|---|
| [66] | 1936–42 | Hawaii: 59 cases; Kanai: 4 cases; Lanai: 14 cases; Maui: 1; Oahu: 4 | Honolulu residents: 13/344 (3.8%) | N/A |
| [67] | 1943? | Workers from sugar cane plantations: 105/860 (13.0%) | Outdoor work, field work; heavy rainfall | |
| [68] | 1962–63 | 3 cases | Exposure: Waded barefoot in a creek | |
| [69] | 1960–75 | Hawaii: 100 cases; Oahu: 21 cases; Kauai: 7 cases; 19 cases hospitalized | N/A | |
| [70] | 1970–84 | 186 confirmed cases | Prior to 1950: occupational risk (sugar industry); after 1950: recreational risk | |
| [71] | 1987 | Kauai: 16 cases | Swimming in the Waimea river | |
| [72] | 1988–89 | Hawaii: 20 confirmed / 172 suspects Kauai: 13 confirmed / 100 suspects | Use of water catchment systems, skin wounds, handling animal tissues (especially cattle) | |
| [73] | 1992 | Oahu: 2 confirmed cases | Recreational exposure (falls); not linked to rats | |
| [74] | 1989–97 | 7 cases | N/A | |
| [75] [77] | 1974–98 | 353 confirmed / 752 suspects | Decrease of occupational exposures over time; increase of recreational exposures. Animal exposure: dogs 71%, rats 30%. Largest outbreak: swimming in a river | |
| [76] | 1998 | Kauai: 2 cases / 5 murine typhus cases | N/A | |
| [78] | 1979–98 | 74 confirmed cases | N/A | |
| [79] | 2002 | US Army blood donors, Oahu: 7/488 (1.4%) | N/A | |
| [80] | 2004 | Oahu: 2 confirmed / 48 tested | Flooding event on a university campus | |
| [81] | 2001–2 | 54 confirmed /1206 febrile illness * | N/A | |
| [83] | 2011? | 1 case | Cliff-diving in Maunawili Falls | |
| [82] | 1992–2004 | 18 confirmed cases | Freshwater exposure (83%); 50% of cases acquired infection in Hawaii, others were infected in Japan, Malaysia and other PIs. | |
| [84] | 1999–2008 | 198 confirmed / 345 suspects | Recreational exposure 45%; Occupational exposures 44%; Habitational exposure 11% |
N/A: no information available from the study.
*The study was conducted during a dengue outbreak.
In Hawaii, the epidemiology and relative importance of risk factors for human leptospirosis have evolved over the past few decades. Leptospirosis in Hawaii has historically been considered an occupationally-acquired disease affecting primarily sugarcane labourers and farmers, but a shifting trend in exposure has been observed since the 1970s, with increasing importance of recreational exposure (freshwater swimming, hunting, fishing, hiking) [70, 75, 77]. During 1989–2008, the frequency of recreational exposures plateaued while frequency of occupational exposures seemed to increase (at least for the island of Hawaii). At the same time, a significant shift in the seasonal occurrence of leptospirosis from the drier summer months to the wetter winter months was observed [84]. An increase in “habitational risks”, especially gardening at home, was suspected to be linked to the resurgence of traditional taro farming. Lastly, exposure to feral pigs, although not investigated per se in the epidemiological surveys, was suspected to be responsible for the changing trend in the infecting serogroup in human cases, shifting from Icterohaemorrhagiae to Australis.
Animals were first investigated for leptospirosis in Hawaii during the same 1936–1942 investigation targeting humans. Dogs, cats, rats and mongooses were serologically screened for leptospirosis, and revealed evidence of infection in all three species [66, 88]. Between 1943 and 2009, more animal studies followed, investigating six animal species. Seropositive rats and mongooses were reported from nine and seven more studies respectively. Evidence of leptospirosis infection was also found in cattle (2/2 studies), mice (6/6), feral swine (1/1) and Hawaiian monkey seals (1/1). Surprisingly, dogs and cats were never further investigated. The complete list of animal studies from Hawaii is reported in Table 3.
Table 3. Summary of publications reporting animal leptospirosis in Hawaii, 1947–2017.
| Citation | Study years | Animal species | Test | N | Positive cases (%) |
|---|---|---|---|---|---|
| [88] | N/A | Dogs | S | 100 | 39 (39%) |
| [66] | 1936–42 | Cats | S | 100 | 0 |
| Rats | DF | 447 | 18 (4%) | ||
| Mongooses | DF | 12 | 4 (33%) | ||
| [67] | 1943 | Rats | S, DF | 96 | 17.2% (Kohala district), 31.3% (Olaa district) |
| Mongooses | S, DF | 86 | 20% (Kohala district), 23% (Olaa district) | ||
| [89] | 1950s-60s | Rats, mice, mongooses | S | 1238 | 558 (45%) |
| [90] | 1959–61 | Rats (RR, RN, RE) | S | 1705 | 587 (34%) |
| Mice | S | 170 | 98 (58%) | ||
| Mongooses | S | 152 | 49 (32%) | ||
| [91] | 1970–73 | Rats (RR, RN, RE) | S, DF, IC | 819 | 201 (25%) |
| Mice | S, DF, IC | 26 | 5 (19%) | ||
| Mongooses | S, DF, IC | 282 | 65 (23%) | ||
| [92] | 1969–74 | Rats (RR, RN, RE) | S, IC | 305 | 50% RN, 55% RR, 34% RE |
| Mice | S, IC | 53 | 33% | ||
| Mongooses | S, IC | 180 | 23% | ||
| [93] | 1969–73 | Rats (RR, RN, RE) | S | 2389 | 722 (30%) |
| Mice | S | 95 | 41 (43%) | ||
| Mongooses | S | 473 | 136 (29%) | ||
| [71] | 1987 | Rats | DF | 14 | 0 |
| Cattle | S | 139 | 89 (64%) | ||
| [94] | N/A | Cattle | S, IC | - | 1 isolation from kidney |
| [73] | 1992 | Rats (RR, RN, RE) | S, IC | 85 | 4/77 RR, 1/2 RN, 0/6 RE |
| [76] | 1992–98 | Mongooses, rats, mice | S, IC | 12501 | 2391 (19%) |
| [95] | 1997–2001 | Hawaiian monkey seals | S | 308 | 19 (6%) |
| [96] | 1990–2003 | Rats, mice | S, DF, IC | 15171 | 2766 (18.2%) |
| [97] | 2007–2009 | Feral swine | S | 804 | 33.8% |
N/A: information unavailable from the study; N: number of animals tested; RR: Rattus rattus; RN: Rattus norvegicus; RE: Rattus exulans; S: serology test; DF: microscopic examination of kidney tissues with a dark field microscope; IC: isolation by culture.
Hawaii is one of the two places (with New Caledonia) where leptospires were investigated in the environment. A molecular study from 2011 focused on environmental samples collected in 22 tropical streams of Oahu near the point at which they discharge to the coastal ocean, showing evidence of Leptospira in 87 of 88 samples. All of the sequenced amplicons (n = 42) were characterised as pathogenic Leptospira wolffii.
New Caledonia
Human leptospirosis was first reported in 1954 and 1957. A total of 20 articles from New Caledonia were identified. Two seroprevalence studies were conducted in 1985–86 [53, 54], and the majority of articles were clinical studies (n = 18) including case reports, routine surveillance data, and case investigations. Clinical studies were conducted from 1973 to 2012, with frequent reports except between 1990–1998, suggesting endemic transmission. Three clinical studies focused on severe leptospirosis: severe icteric leptospirosis cases with cardiac manifestations [55], the influence of age on the development of severe leptospirosis in children [63], and risk factors and predictors of severe leptospirosis [64]. The complete list of human leptospirosis studies from New Caledonia is reported in Table 4.
Table 4. Summary of publications reporting human leptospirosis in New Caledonia, 1947–2017.
| Citation | Study years | Case reports | Seroprevalence studies | Exposure/risk factors |
|---|---|---|---|---|
| [32] | 1954, 1957 | 7 confirmed cases | N/A | |
| [36] | 1974–79 | 24 confirmed cases | N/A | |
| [49] | 1973–80 | 32 cases | N/A | |
| [50] | 1973–80 | 37 confirmed / 286 suspects | Possible drivers: Poor hygiene, rivers | |
| [51] | 1973–81 | 39 confirmed cases 1981: 5 cases (1 infected in Vanuatu) |
Possible exposure: Streams, occupational activities | |
| [52] | 1983–85 | 57 cases | Living in rural areas, in tribes | |
| [53] | 1985–86 | 193 cases | Around cases: 63/210 | Cases: 72% live in flood plains |
| Occupational risk: 124/669 | Around cases: farmers most at risk | |||
| Control population: 26/260 | Occupational risk: farmers most at risk | |||
| [54] | 1985–86 | La Néra: 60 cases | Around cases: Néra = 16/41; Coulée = 5/20 | Cases: 85% live in a muddy place; 95% in frequent contact with rivers |
| La Coulée: 26 cases | Occupational risk: Néra = 16/41; Coulée = 16/93 | |||
| [55] | 1983–85 | 57 cases, 15 with cardiac symptoms | N/A | |
| [42] | 1987 | 46 cases | N/A | |
| [56] | 1989–93 | 192 confirmed cases Peak in 1990 (51 cases) |
Temporality: 4-fold increase in March 65.9% cases: Melanesian leading a tribal lifestyle; subsistence farming Recreational risks: bathing in running fresh water, fishing, hunting |
|
| [57] | 1989 | 144 confirmed cases | Exposure: ditch or river water; living in a rural area. Contacts with rats, dogs | |
| [58] | 1989–90 | Bourail: 78 confirmed cases | Exposure: Swimming, poor hygiene, hunting, fishing, contact with animals | |
| [60] | 1989–2001 | 156 cases | ||
| [59] | 2005 | 37 confirmed and 3 probable / 1059 suspects | Exposure: Swimming, hunting, fishing, contact with animals | |
| [61] | 2001–05 | 239 confirmed / 6690 suspects | Contacts with animals, recreational activities | |
| [62] | 2008 | Outbreak: 135 confirmed cases | Suspected driver: heavy rainfalls associated with floods. Exposure: Contact with animals (OR>2), swimming, fishing, hunting (OR>3) | |
| [63] | 2006–12 | 60 cases under 18yo | Age-dependant association with severity of leptospirosis | |
| [64] | 2008–11 | 72 severe leptospirosis / 306 cases | Delay in diagnosis, tabacco use, infection by L. interrogans Icterohaemorragiae | |
| [65] | 2000–12 | 731 confirmed and 432 probable/ 1163 suspects | SST anomaly, rainfall, temperature |
N/A: information unavailable from the study.
The risk factors for human leptospirosis in New Caledonia varied little between the 1980s and today. The disease was more frequent among young men and during the wet season. The main risk factors identified were recreational exposure (fishing and swimming in fresh water, hunting) and contact with animals, with populations living in rural areas and local tribes being at highest risk. However, the probable source of infection was difficult to ascertain because of the multiplicity of potential infecting sources and exposure pathways, and the overlap between professional and recreational activities [56]. Also, identification of the animal source of leptospires in these (human only) studies was only presumptive as people were frequently exposed to multiple species, including cattle, pigs, horses, dogs, rats and, less commonly, deer [56, 61].
Eleven studies were published on animal leptospirosis in New Caledonia between 1983 and 2004. Leptospira spp. infection was demonstrated in a wide range of animal hosts, including cattle (6/6 studies), dogs (6/6), deer (6/6), horses (3/3), pigs (4/5, including one study of feral pigs), rats (3/3) and cats (2/3). Results on goats largely lacked detail, however one study reported five seropositive animals. Results on sheep (one study) were inconclusive. The complete list of studies on animal leptospirosis in New Caledonia is reported in Table 5.
Table 5. Summary of publications reporting animal leptospirosis in New Caledonia, 1947–2017.
For study [54] the number of tested animals ‘N’ is provided separately for the two areas of interest, i.e. La Néra basin first and La Coulée basin then. Studies [60] and [98] targeted positive animals only, so ‘N’ equals ‘positive cases’.
| Citation | Study years | Animal species | Test | N | Positive cases (%) |
|---|---|---|---|---|---|
| [99] | 1982–83 | Cattle | S | 136 | 84 (61.8%) seropositive |
| Dogs | S | 38 | 12 (31.6%) seropositive | ||
| Horses | S | 25 | 13 (52%) seropositive | ||
| Pigs | S | 43 | 10 (23.3%) seropositive | ||
| Sheep/goats | S | 2 | 1 (suspected) seropositive | ||
| [100] | 1986 | Cattle | S | 5 | 5 seropositive |
| [53] Grande Terre and Islands |
1985–86 | Rats (RR, RN, RE) | S, DF, IC | 18 | 11 (61.1%) seropositive |
| Cattle | S, DF, IC | 70 | 69 (98.7%) seropositive | ||
| Pigs | S, DF, IC | 36 | 21 (58.3%) seropositive | ||
| Horses | S, DF, IC | 18 | 9 (50%) seropositive | ||
| Goats | S, DF, IC | 13 | N/A | ||
| Dogs | S, DF, IC | 81 | 48 (59.3%) seropositive | ||
| Cats | S, DF, IC | 12 | NA | ||
| [54] La Néra + La Coulée |
1985–86 | Rats (RR, RN, RE) | S | 12 + 4 | 8 + 3 seropositive |
| Cattle | S | 15 + 0 | 15 seropositive | ||
| Pigs | S | 14 + 0 | ? | ||
| Horses | S | 4 + 0 | ? | ||
| Goats | S | 9 + 4 | 1 + 2 seropositive | ||
| Dogs | S | 46 + 7 | 29 + 2 seropositive | ||
| Cats | S | 6 + 5 | 0 + 1 seropositive | ||
| Deer | S | 1 + 0 | 1 seropositive | ||
| [101] | 1984 | Cattle | S | 350 | 58.3% seropositive |
| [60] | 1989–2001 | Dogs | TY | 1 | 1 |
| Pigs | TY | 7 | 7 | ||
| Deer | TY | 5 | 5 | ||
| [98] | 2010 | Introduced deer | TY | 12 | 12 |
| [102] Poster summary |
Introduced deer | yes | |||
| Rats (same as [103]) | yes | ||||
| [103] | 2008–10 | Rats, mice (Bourail area) | MT | 210 | 56 (26.7%) renal carriage |
| [104] | 2009 | Cattle | S | 30 | 43% seropositive |
| Deer | S | 29 | 72% seropositive | ||
| Horses | S | 25 | 80% seropositive | ||
| Dogs | S | 51 | 43% seropositive | ||
| Cats | S | 8 | 100% seropositive | ||
| [105] | 2013 | Dogs (urban + rural) | S, MT | 95 | 30.8% seropositive; 4.4% renal carriage |
| Pigs (feral + farmed) | MT, TY | 94 + 138 | 6.4% (feral); 10.2% (farmed) | ||
| Deer (feral + farmed) | MT, TY | 85 + 107 | 13.02% |
N/A: information unavailable from the study; N: number of animals tested; RR: Rattus rattus; RN: Rattus norvegicus; RE: Rattus exulans; S: serology test; DF: microscopic examination of tissues with a dark field microscope; IC: isolation by culture; MT: molecular testing (PCR); TY: molecular typing.
In one study from 2016 in New Caledonia, leptospires were investigated in the environment [29]. The study focused on environmental samples collected around human cases, showing that 58% of soil samples were contaminated with pathogenic leptospires.
French Polynesia
The first human leptospirosis cases were reported from Tahiti in the 1950s [31]. Two serological surveys in the general population were conducted in French Polynesia: one in Tahiti in 1970–71 [34] found a seroprevalence of 29.5%, and another in Marquesas in 1981 [39] where a lower seroprevalence (9.5%) was found. In addition, 20 clinical studies from 1952 to 2015 provided evidence of human leptospirosis, suggesting endemic transmission throughout the archipelago. Available reports generally covered the whole of French Polynesia, a vast archipelago of 118 islands and atolls, because diagnostic laboratories received samples from clinically-suspected cases from all islands, but a few studies were dedicated to specific Islands, i.e. Marquesas [5, 39, 46] and Raiatea [5, 46]. The complete list of human studies from French Polynesia is reported in Table 6.
Table 6. Summary of publications reporting human leptospirosis in French Polynesia, 1947–2017.
| Citation | Study years | Case reports | Seroprevalence studies | Exposure/risk factors |
|---|---|---|---|---|
| [31] | 1952–53 | Tahiti: 2 cases | Rats trapped in the same suburbs are infected; pigs and dogs might be | |
| [32] | 1952–57 | 7 confirmed + 4 probable / 35 suspects | N/A | |
| [33] | 1969–70 | Tahiti: 36 cases | N/A | |
| [34] | 1970–71 | Tahiti: 224/759 (29.5%) | N/A | |
| [35] | 1955–68 1969–72 |
22 confirmed cases 66 confirmed cases |
Possible drivers: favorable climatic conditions; flood-risk areas; lots of rats and roaming dogs | |
| [36] | 1970–79 | 77 severe cases | N/A | |
| [37] | 1975–80 | 43 confirmed / 60 hospitalized | Occupational risk (16), rodents around (most); 50% of cases don't swim in rivers | |
| [38] | 1975–80 | 60 cases | Thrombocytopenia (16), renal failure (15), both (10) | |
| [39] | 1981 | Marquesas: 24/253 (9.5%) | Exposure: contacts with dogs, rats; walking bare-foot | |
| [40] | 1983 | 11 cases | N/A | |
| [41] | 1985–87 | Tahiti: 6 cases with pulmonary complications | N/A | |
| [42] | 1987 | 36 cases | N/A | |
| [43] | 1984–90 | 114 confirmed / 120 hospitalized | Exposure: living in rural or semi-rural areas in contact with livestock (pigs) | |
| [44] | 1994–2000 | 360 confirmed cases / 2525 suspects | N/A | |
| [45] | 2004–05? | Tahiti: 71 severe cases | Severe outcome linked to hypotension, oliguria, abnormal chest auscultation at the first examination | |
| [5] | 2003–05 | Marquesas: 13 confirmed /47 suspects | Marquesas: hunting (75% cases) | |
| Raiatea: 16 confirmed /68 suspects | Raiatea: bathing if freshwater (64% cases) | |||
| [46] | 2004–05 | Marquesas: 13 confirmed /47 suspects | Possible drivers: Contact with dogs, hunting in Marquesas; contacts with rats in Raiatea | |
| Raiatea: 20 confirmed /66 suspects | ||||
| [47] | 2006–08 | 165 confirmed cases + 107 probable | Swimming in river (30%), farmers (22%), contact with rats (24%) dogs (21%) or cats (17%), walking barefoot (21%), gardening (18%) | |
| [106] | 2010 | 81 confirmed cases | Contact with rats (40%) or domestic animal (60%), walking barefoot in water or mud (77%); swimming in rivers (43%), gardening (50%); working in piggeries (17.5%), farmer (52%) | |
| [107] | 2006–10 | 502 cases, 100 serotyped | Contact with rats (34%) or domestic animal (60%), walking barefoot in water or mud (33%); swimming in rivers (35%), gardening (30%); working in piggeries (14%), farmer (29%) | |
| [24] | 2014–15 | 2 cases (co-infection with chikungunya) | N/A | |
| [48] | 2014–15 | 44 confirmed cases | Possible risk factors: rats and dogs (as they share common types of leptospires with human cases) |
N/A: information unavailable from the study.
Three clinical studies included case investigations (through questionnaires) that aimed to identify risk factors associated with human leptospirosis (2006–2010), and important factors common between the studies included contact with rats or domestic animals, walking barefoot in water or mud, swimming in rivers, gardening, and occupational risks (working in piggeries, farming) [47, 106, 107]. In Marquesas, hunting and contact with dogs have been reported as possible sources of infection [5, 46]. Risk factors in French Polynesia were mostly recreational rather than occupational, but potential infecting sources were numerous.
Only three studies investigated animal leptospirosis in French Polynesia. The first study (1952–53) investigated renal carriage in rats from Tahiti by experimental infection of guinea pigs with crushed rat kidneys; four guinea pigs became icteric [31]. The second was a seroprevalence study (1981–86) targeting four host species from Tahiti, and cattle from both Tahiti and Marquesas [108]. Positive serology results were found in 15.5% (23/148) of cattle, 32.2% (37/115) of pigs, and all five horses tested. Serology results were not detailed by island, but only seven tested cattle originated from Marquesas. The two sheep and twelve dogs tested were found to be seronegative. The last study investigated animal leptospirosis in dogs, pigs and rats from Tahiti [48]. Renal carriage of pathogenic leptospires was demonstrated from 26.5% (48/181) of farmed pigs, 20.4% (23/113) of rats, and four sick dogs.
Fiji
The first study reporting human leptospirosis in Fiji was published in 1978 [109], describing 240 cases between 1969 and 1977. Since then, two community-based seroprevalence studies were published [110, 111], as well as five studies reporting clinical cases [5, 112–115]. The first seroprevalence study in the 1980s identified 264 seropositive out of 300 healthy volunteers (88%) from a rural area in the main island of Viti Levu [110]. A second seroprevalence study was conducted in 2013 and included 2,152 healthy individuals from 81 communities on the three main islands of Fiji, of whom 19.4% were seropositive [111]. Risk factors associated with infection included living in villages (OR 1.64), lack of treated water at home (OR 1.52), working outdoors (1.64), living in rural areas (OR 1.43), high poverty rate (OR 1.74), living <100m from a major river (OR 1.41), pigs in the community (OR 1.54), high cattle density in the district (OR 1.04 per head/km2) and high maximum rainfall in the wettest month. Using the data from the 2013 seroprevalence study (which included questionnaire data about contact with animals as well as livestock data from the Fiji Ministry of Agriculture), a third study [116] showed significant heterogeneity in the relative importance of animal species in leptospirosis transmission in different ethnic groups and residential settings.
Five studies have been published on animal leptospirosis in Fiji [113, 117–120], exploring a wide range of host species, including dogs, goats, mongooses, cattle, pigs, rats, sheep, mice, horses and cats. Except for cats (only three animals tested), the studies identified seropositive animals in all species that were tested. Thus, Leptospira infection seems common in multiple animal species in Fiji.
Papua New Guinea
Studies on human leptospirosis in Papua New Guinea (PNG) were published between 1955 and 1968 [121–124], including three seroprevalence studies targeting healthy volunteers, showing high seroprevalence of 53.0% to 57.5%, with Australis and Hebdomadis the most common serogroups. One study explored risk factors for human infections and found that leptospirosis in PNG was common in both males and females, and in both adults and children, reflecting high risk in the whole population from shared occupational, domestic, and other environmental exposures [123]. People have close contact with domestic animals, particularly dogs and pigs, as well as native fauna in gardens and uncleared areas surrounding the villages. Rats were suspected to be of less importance compared to other animal species because human studies in PNG found that serogroup Icterohaemorrhagiae (commonly associated with rodents) was relatively uncommon [122, 125].
Leptospira infection in animals was explored in the 1960s and 1970s, with seven publications exploring infection in rats, cattle, dogs, pigs, goats and marsupial bandicoots [122, 123, 125–129]. Seropositive animals were identified from all tested species, but sample size was small for bandicoots (n = 5). After the 1970s, no further studies were published until a seroprevalence study investigated cattle (n = 1,452) and pigs (n = 326) in 2004, and dogs and livestock in 2006 (111 cattle, 69 pigs, 22 dogs, 15 horses) [130]. Seropositive animals were identified from all species, but seroprevalence was low in dogs (1/22 in 2006) and pigs (0/362 in 2004, 1/69 in 2006).
Guam
The first study published in 1974 identified three seropositive stray dogs out of 180 tested (1.7% seroprevalence) [131]. More recent studies investigated cattle (n = 34) and pigs (n = 52) in 1999 [132], and feral pigs (n = 46) in 2015 [133]. All livestock tested seronegative but the seroprevalence in feral pigs was 23.9%.
The first human clinical study was published in 1998, describing two human leptospirosis cases with pancreatitis [74]. Three human clinical studies in the 2000s reported sporadic cases only [5, 74, 134, 135]. In addition, two leptospirosis cases reported in Hawaii for the period 1999–2008 were suspected to have been acquired in Guam [84]. One mixed study included both clinical data and a seroprevalence study conducted following an outbreak that occurred after an outdoor multisport athletic event: out of 46 participants surveyed, 21 reported being ill and three of them were confirmed with recent leptospirosis infections [136]. Reported exposures were often recreational activities involving swimming in fresh water or waterfalls, but water buffaloes were also reported as a suspected source of contamination.
Wallis and Futuna
No seroprevalence study has been conducted in Wallis and Futuna. A multicentre survey of suspect clinical cases recruited by general practitioners conducted in 2003–2005 identified 3 cases out of 14 (21%) and 31 cases out of 71 (44%) in Wallis Island and Futuna Island respectively [5]. Another clinical study conducted in 2005 identified one case in Wallis and 21 cases in Futuna [137], and reported some exposure information: one case swam in a river few days before the occurrence of the disease, and all the other cases were involved in breeding pigs (at home for the Futuna cases, at work in a pig farm for the one Wallis case). A third study conducted over the period 2004–2014 reported 382 cases in Futuna, with a peak incidence in 2008 [7]. Serogroup Australis was predominant until 2007, when Icterohaemorrhagiae became the most common. Despite similar cultural and socio-economical patterns between the islands, human leptospirosis was considered endemic in Futuna while it only occurred sporadically in Wallis.
Three studies focused on animal leptospirosis in Wallis and Futuna. A first study focusing on livestock only reported the detection of specific Leptospira serogroups in pigs, with no prevalence provided [138]. A seroprevalence study was conducted in the 1990s on different animal species: 14% (12/88) of pigs were found to be seropositive in 1985, and 33% (54/163) in 1997 but a wider range of serogroups was tested in 1997. In 1998, two dogs out of 10 and three horses out of six also tested seropositive, while all 11 goats tested were seronegative [138, 139]. In 2008–2012, Leptospira prevalence in three rat species was investigated [140]. Renal carriage of Leptospira interrogans was confirmed in 84 rats out of 286 in Futuna (36.4% Rattus rattus, 42.8% Rattus norvegicus and 18.8% Rattus exulans), while only one R. exulans out of 56 rats (1.8%) was positive in Wallis; 15 rats were found negative in the uninhabited island of Alofi, 2 km from Futuna.
Risk factors associated with human leptospirosis have not been formally investigated, but rodents in Futuna have a much higher Leptospira carriage rate than on Wallis. It has been hypothesised that this variation could be explained by differences in taro farming practices; people on Wallis irrigate their fields by ditches, while those on Futuna flood their fields. This practice in Futuna might facilitate the spread of Leptospira among rats and subsequently to humans [140].
American Samoa
Human leptospirosis was first investigated in American Samoa in 1948 [141]; ten patients hospitalised for jaundice were tested, but none were seropositive against four Leptospira serogroups. Thirty patients hospitalised for reasons other than jaundice were also tested, and three were found to be seropositive for serogroup Australis. Leptospirosis cases were later occasionally reported, including three cases of co-infection with dengue in 2008 [142] and one severe case in 2011 of a 15 year old boy who frequently slept in the rainforest and had recently waded through freshwater [143].
Four community-based seroprevalence studies were conducted in American Samoa. Two studies reported seroprevalence rates of 17% in 2004 (n = 341) [144] and 15.5% in 2010 (n = 807) [145]. Australis was the main serogroup in 2004 (71%) while Hebdomadis, Australis and Pyrogenes were the most common serogroups in 2010. The 2010 survey found that outdoor occupation (OR = 3.25), piggeries around the house (OR = 2.63) and recreational exposure (swimming at beach OR = 2.01, fishing OR = 1.78) were significantly associated with seropositivity, but infections with each of the three main serogroups were associated with different behavioural and environmental exposures [145]. A third study compared the serogroups between the 2004 and 2010 surveys [146] and showed epidemiological evidence of serogroup emergence, possibly as a result of ecological and environmental change. The fourth study produced a predictive risk map using environmental variables from 2010 study and demonstrated the importance of environmental drivers of transmission [147].
Two studies focused on animal leptospirosis. Renal carriage of leptospires by rats was examined on Tutuila Island in 1948; out of 126 individuals from four rat species trapped, 24 (19%) Rattus norvegicus kidney tissues stained by silver precipitation technique were found positive under microscopic examination [141]. One out of twelve dogs was also found seropositive by MAT. A more recent study published in 2005 reported data ‘from animal studies and literature’ (with no date specified) showing seropositive results from pigs, rats, dogs and cattle [135]. The authors suggested that, even though the animal studies were not conducted at the same time as the human studies (2004), it appeared that Australis was the most common serogroup infecting people, and pigs were the most likely reservoir hosts.
Federated States of Micronesia
Seven clinical studies reported information about human leptospirosis in the Federated States of Micronesia (FSM), which consists of the four states of Yap, Chuuk, Kosrae and Pohnpei in the Northwestern Pacific Ocean. In 1989–1997, eight confirmed leptospirosis cases identified in Hawaii were acquired from Kosrae and Pohnpei [74], and from 1999–2008 one reported case in Hawaii was acquired from FSM [84]. A multi-centre survey of patients with suspected leptospirosis conducted in 2003–2005 reported no seropositive case from Yap (0/1 suspected) or Pohnpei (0/27 suspected) [5]. In 2010, an investigation of 10 febrile patients in Chuuk revealed two confirmed cases of leptospirosis [148]. In 2011, a hospital-based survey conducted in Pohnpei on 54 patients presenting with undifferentiated fever found that 20.4% showed serologic evidence of acute infection by MAT [149]. In 2012 in Yap, 172 patients with suspected dengue were investigated by qPCR and five (2.9%) were confirmed as acute leptospirosis infections [150]. Lastly, one study investigated the health risks associated with climate change in FSM using a time series distribution of monthly leptospirosis outpatient cases in Pohnpei. This study was based on hospital records and is assumed to represent close to all of the reported cases [151]. Taken together, those studies suggest that leptospirosis is endemic in FSM.
Rats were the first animal species to be investigated in 1947, but microscopic examination of kidney tissues stained by silver precipitation technique did not reveal any leptospires from 28 rats trapped in Chuuk and Pohnpei [152]. However, a seroprevalence study conducted in 1995–1996 on pigs (in four states), dogs (Pohnpei, Chuuk) and rats of three species (Pohnpei, Chuuk, Yap) showed positive results from all species [153].
Solomon Islands
No papers on human leptospirosis were identified from the Solomon Islands, and only three papers on animal leptospirosis have been published. Between 1967 and 1977, a large veterinary survey investigated cattle diseases from all the cattle herds listed in 1967 (165 herds with a total of 8,930 cattle) plus some of the 650 herds established after 1967 [86]. For leptospirosis, only the female cattle over one year of age were tested, of which 62 were found seropositive. In 1985, pigs were reported positive with serogroup Pomona, but detailed results were not available [154, 155]. A seroprevalence study conducted in 1998 reported that 83% of 226 cattle, 12% of 298 pigs, 16% of 63 goats, and 71% of 31 horses tested were seropositive by MAT [155].
Vanuatu
Only sporadic cases of human leptospirosis have been reported in Vanuatu in the 1990s [156, 157] and the 2000s [5]. No human seroprevalence studies have been conducted. Two cases in travellers returning from Vanuatu were also reported in New Caledonia [51] and Australia [158]. The latter swam in a river in Vanuatu with an injured foot, and developed a fatal illness with acute renal failure, jaundice, respiratory failure, myocarditis and rhabdomyolysis.
During an extensive survey of livestock diseases conducted between 1971 and 1981 throughout the Vanuatu archipelago, 6,719 cattle from 131 herds were investigated by MAT; 92 cattle (1.4%) were found positive [159].
Palau
Following the presentation of three cases of Weil’s disease in 2000, 171 patients presenting with a ‘viral syndrome’ were investigated in Palau, of whom seven were serologically confirmed as leptospirosis [160]. Over the period 2000–2006, the disease surveillance system recorded 81 cases, all living in the most populated areas of the country [161]. In 2003–2005, a multi-centre survey of patients with clinically suspected leptospirosis reported one seropositive out of eight tested [5]. In 2014, two Japanese travellers developed leptospirosis after returning from Palau; the suspected exposure was swimming in Ngardmau falls [15].
Cattle (n = 20), goats (n = 7) and pigs (n = 55) were serologically investigated by MAT between 1993 and 1996 in Palau [162]. All three investigated species were found seropositive for Leptospira, i.e. 9 cattle (45%), 3 goats (43%) and 22 pigs (40%).
Other Pacific Islands
In Tonga, a multi-centre survey of clinically suspected cases was conducted in 2003–2005; four patients were tested by PCR or MAT but none were confirmed as leptospirosis [5]. Cattle (n = 171) and pigs (n = 244) from different Tongan islands (Tongatapu, 'Eua, Ha'apai, Vava'u) were serologically investigated by MAT between 1992 and 1994 [163]. Seroprevalence varied between the islands, from 19.6% to 45.0% in cattle, and from 5.0% to 16.7% in pigs.
In the Commonwealth of the Northern Mariana Islands (CNMI), leptospirosis has been reported as endemic, but our search retrieved only one study; in 2000–2001, 10 cases of leptospirosis were reported in Saipan, of which eight were severe, and three were fatal [164]. In none of the cases was laboratory diagnosis available to the medical staff until weeks after patient was hospitalized or had died. Case reports available for four of the patients identified possible exposures as swimming in freshwater, cleaning out roadside sewers after a tropical storm, slaughtering pigs, and occupational gardening.
In 1989–1997, one confirmed leptospirosis case identified in Hawaii was acquired from the Marshall Islands [74].
For the remaining Pacific Islands, our search retrieved no studies on human leptospirosis, but few animal studies were available for Easter Island, Kiribati, Niue, Cook Islands, Samoa and Tokelau. The results are summarised in Table 7.
Table 7. Summary of publications reporting animal leptospirosis in the Pacific Islands for which no studies on human leptospirosis were reported, 1947–2017.
| Citation | PICTs | Study years | Host | N | Confirmed cases (%) |
|---|---|---|---|---|---|
| [165] | Easter Island | 1946–65 | Cattle | 57 | 46 low-grade reactions with MAT |
| Sheep | 146 | 0 | |||
| Pigs | 13 | 0 | |||
| [166] | Kiribati | 1975–80 | Pigs | 172 | 0 |
| 1985 | Goats | 51 | 8 (15.7%) seropositive | ||
| 1992–94 | Pigs | 193 | 6 (3.1%) seropositive | ||
| [167] | Niue | 1992–94 | Cattle | 60 | Inconclusive serology |
| Pigs | 60 | Inconclusive serology | |||
| [168] | Cook Islands (Raratonga) |
1982–83 | Cattle | 48 | 3 (6.3%) seropositive |
| Pigs | 60 | 1 positive, 6 inconclusive (11.7%) | |||
| [141] | Samoa | 1948? | Rats | 36 | 8 (22.2%) renal carriage |
| [169] | Samoa | ? | Cattle | 629 | 414 (65.8%) seropositive |
| Pigs | 108 | 27 (25%) seropositive | |||
| [170] | Samoa | 1997 | Cattle | 316 | 125 (40%) seropositive |
| Horses | 63 | 28 (44%) seropositive | |||
| Pigs | 161 | 37 (23%) seropositive | |||
| [171] | Tokelau | 1998 | Pigs | 88 | 3 (3.4%) seropositive |
Discussion
This systematic review is the first to synthesize and compile data on the epidemiology of human leptospirosis and pathogenic Leptospira spp. infection in animals in the PIs. Considering the limited population and economic resources in those mostly small and isolated islands, the number of studies retrieved was impressive (n = 148). Overall, the systematic review demonstrates that leptospirosis is an important cause of acute febrile illness across the PIs, with evidence of human disease demonstrated in 13 of 14 PIs where investigations have been conducted. Community-based seroprevalence studies were conducted in seven PIs and provided heterogeneous results, with prevalence ranging from 10% to 88%. Taken together, these findings reflect the public health importance of leptospirosis in the region, and corroborate recent estimates of very high disease burden in Oceania [3]. A wide range of domestic and wildlife species (n = 13 when counting rats as a single species) from across the PIs showed evidence of present and/or past infection with Leptospira. In some PIs, infected animals were mainly livestock (cattle and pigs in particular), indicating the potentially important role of non-rodent reservoir species in human infections, especially in islands where backyard subsistence livestock are common. However, rats were investigated in fewer studies and less islands than livestock, even in islands where serogroup Icterohaemorrhagiae was identified from human cases (e.g. Palau).
Even though many studies on human leptospirosis in the PIs were retrieved, these studies probably under-estimate the true burden as leptospirosis is thought to be under-reported globally, particularly in developing countries such as the majority of PIs. Several studies included in our review were conducted during outbreaks of dengue [81, 142, 150], chikungunya [24] or murine typhus [76], and coincidentally identified leptospirosis cases that might otherwise have remained undetected. On the contrary, the co-circulation of different infectious diseases sharing similar clinical presentation in the PIs might lead to leptospirosis under-diagnosis, sometimes resulting in a fatal outcome [24]. In the reviewed human clinical studies, diagnosis for leptospirosis often occurred very late, in already hospitalised (n = 21 studies where hospitalisation is specified) or even deceased patients [164]. A case report from American Samoa highlighted some of the leptospirosis diagnostic challenges faced by clinicians in the PIs [143]. There is still a need to raise awareness and to reinforce diagnostic capabilities for leptospirosis in the PIs. These have to go hand in hand with better agreement about the use of diagnostic tools and interpretation of the results. The development of clinical guidelines for the management of febrile patients with suspected leptospirosis should be a priority.
Serological studies suggested a wide variety of Leptospira serogroups (n = 21) in humans and animals across the PIs, including common as well as rare serogroups. Reported serogroups varied between PIs, between humans and animals, and between animal species. Across the PIs, seropositive animal hosts were reported for all the serogroups detected in human cases. However, it was difficult to make serogroup links between animals and humans because data were reported from multiple studies with variable study designs. Also, MAT results were difficult to interpret because of the intrinsic limitations of the test, as well as the heterogeneity in data quality between the studies. MAT has limited sensitivity, especially with early acute-phase specimens, and with chronically infected animals (reservoirs) that may be serologically negative even while shedding the bacteria in their urine [173]. Also, MAT results may vary depending on subjective interpretation by laboratory personnel and the panel of serovars used [2]. Interpretation is further complicated by the high degree of cross-reactions that occurs between Leptospira of the same serogroup or even between serogroups [173]. Apart from those intrinsic limitations, many studies included in our review were classified as “weak evidence” because they did not comply with our case definition and/or provide the minimal information required to assess the quality of the results. Even in studies complying with our case definition, some MAT results were still overstated. For example, one study from New Caledonia [57] reported 12 different serogroups in severe cases identified in 1989, while studies using Leptospira isolates or genotyping techniques have provided evidence that only six serogroups have been responsible for human cases in New Caledonia [60, 98]. Therefore, tables of serology results provided in this review (Table 1 and S2 Table) should be taken as summaries of the reports from the studies, but interpreted with great caution. To ensure a proper quality assessment of the results and accurate interpretation, it is crucial that in the future MAT results are reported in detail, especially providing information regarding the panel of serovars used, MAT titres, and detailed and appropriate case definition criteria. In cases where serology is expected to be of poor sensitivity, the use of molecular methods might be more appropriate. In our review, a limited number of studies relied on a molecular diagnosis (n = 14 in animals; n = 15 in humans).
Studies including both animal and clinical data were uncommon (n = 13 in 11 PIs) in this review. Also, molecular characterization of Leptospira spp. diversity that allows human Leptospira infection to be traced back to the probable source of contamination [172] was attempted in very few studies. When Leptospira infection was investigated in separate studies for animals and humans in a same PI, it was generally not possible to link the results, for example because of a time gap between animal and human studies, and/or different study designs, and/or the use of different MAT panels. In some PIs, human leptospirosis was not investigated, even though Leptospira infection was demonstrated in animals, i.e. in the Solomon Islands, Cook Islands, Kiribati, Niue, Tokelau, Samoa, and to a lesser extent Tonga where only four suspect human cases were tested. Also, we retrieved livestock studies from 19 PIs while rodent studies were available from only eight of these 19 PIs, which might bias our understanding of leptospirosis infection in humans in the PIs.
This review identified common behavioural risk factors and environmental drivers for leptospirosis infection across the region. Environmental drivers were mostly climate-related (flooding, extreme events), while individual risk factors included backyard subsistence livestock, farming, lifestyle (walking bare-foot, fishing, hunting), contact with animals and contact with fresh water sources (recreational use, washing laundry). Our review only identified a few epidemiological surveys that conducted robust statistical analyses of risk factors associated with human leptospirosis. Many studies reported some “possible drivers” of infection, or some “possible exposure” but the hypotheses were rarely properly evaluated. Even where surveys on clinical cases were conducted with detailed questionnaires, the probable source of infection was difficult to ascertain because of the multiplicity of potential infecting exposures (e.g. people who have been in contact with rats and pigs and dogs, and have been swimming in fresh water), the overlapping of professional and recreational activities and the lack of a comparator or control group.
Leptospirosis as a human disease is the result of complex interactions between humans, animal reservoirs/carriers, and the environment where the bacteria can survive. Our findings suggest that the major animal reservoirs of human-infecting leptospires may vary across the PIs, but that livestock (especially cattle and pigs), dogs and rodents may all play important roles in disease transmission to humans. However, intra-island heterogeneity has not been explored. In Fiji, the difference between habitats has been specifically investigated, showing that the relative importance of animal species in human infections varied between urban, peri-urban and rural settings [111]. We also showed a wide heterogeneity of leptospirosis serogroups and individual risk factors within and between islands. Combined with the already discussed limitations of the MAT and the limited number of studies combining animal, human and environmental investigations, overall the epidemiology of the disease is still unclear for most of the PIs.
As already advocated in other studies [174, 175], eco-epidemiological studies following an integrated “One Health” approach are needed to understand the exposure pathways for leptospirosis in humans, including the specific role and relative importance of each animal species in different environmental settings. Future studies should further explore how disease transmission to humans is influenced by the complex interactions between humans, animals, and the environment, including interactions within as well as between ecological scales. Also, better integration of environmental studies (only two in our search), inclusion of health economics evaluations and application of novel epidemiological methods such as mathematical modelling would be valuable next steps. This is crucial in a context where climate change, increased risk of flooding, population growth, urbanization, loss of biodiversity and agricultural intensification could individually, or possibly synergistically, lead to further increases in the burden of human leptospirosis in the Pacific. In the future, guidelines for a proper framework for leptospirosis research may help to improve our understanding of local epidemiology and complex transmission dynamics of leptospirosis worldwide.
Supporting information
(DOC)
A list of electronic databases browsed is provided, as well as the complete search strategy, including search terms.
(DOC)
The complete reference is provided for each study, as well as the island(s) where the study took place, the target (human vs animal) and the type of study. Human clinical studies were reported as strong or weak evidence of leptospirosis following the criteria detailed in the methods section. The 11 studies for which the full text document could not be retrieved are indicated.
(XLSX)
The results are reported per study, indicating where (island(s)) and when (year(s)) the study was conducted, the target (human vs animal), the animal species investigated when relevant and the serogroup. Serology results are reported as in the study, i.e. potentially including cross-reactions between serovars and serogroups, paradoxical reactions or anamnestic responses. For this reason, and because of the limitations of the MAT, some results were considered as “weak evidence” of leptospirosis following the criteria detailed in the methods section; thus this table should be interpreted with caution.
(XLS)
Acknowledgments
We gratefully acknowledge the Pacific Community (SPC)—Statistics for Development Division for providing the regional map. We thank Nicky Foxlee (University of Queensland Library) for advice on database and search strategies. We also thank Institut Pasteur de Paris library and Nicky Foxlee for providing many full-text documents.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
CLL was supported by an Australian National Health and Medical Research Council (NHMRC) Fellowship (1109035). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Human leptospirosis: guidance for diagnosis, surveillance and control. Geneva: 2003.
- 2.Levett PN. Leptospirosis. Clin Microbiol Rev. 2001;14(2):296–326. doi: 10.1128/CMR.14.2.296-326.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Costa F, Hagan JE, Calcagno J, Kane M, Torgerson P, Martinez-Silveira MS, et al. Global Morbidity and Mortality of Leptospirosis: A Systematic Review. PLoS Negl Trop Dis. 2015;9(9):e0003898 doi: 10.1371/journal.pntd.0003898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pappas G, Papadimitriou P, Siozopoulou V, Christou L, Akritidis N. The globalization of leptospirosis: worldwide incidence trends. Int J Infect Dis. 2008;12(4):351–7. doi: 10.1016/j.ijid.2007.09.011 [DOI] [PubMed] [Google Scholar]
- 5.Berlioz-Arthaud A, Kiedrzynski T, Singh N, Yvon JF, Roualen G, Coudert C, et al. Multicentre survey of incidence and public health impact of leptospirosis in the Western Pacific. Trans R Soc Trop Med Hyg. 2007;101(7):714–21. doi: 10.1016/j.trstmh.2007.02.022 [DOI] [PubMed] [Google Scholar]
- 6.Torgerson PR, Hagan JE, Costa F, Calcagno J, Kane M, Martinez-Silveira MS, et al. Global Burden of Leptospirosis: Estimated in Terms of Disability Adjusted Life Years. PLoS Negl Trop Dis. 2015;9(10):e0004122 doi: 10.1371/journal.pntd.0004122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Massenet D, Yvon JF, Couteaux C, Goarant C. An Unprecedented High Incidence of Leptospirosis in Futuna, South Pacific, 2004–2014, Evidenced by Retrospective Analysis of Surveillance Data. PLoS One. 2015;10(11):e0142063 doi: 10.1371/journal.pone.0142063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goris MG, Kikken V, Straetemans M, Alba S, Goeijenbier M, van Gorp EC, et al. Towards the burden of human leptospirosis: duration of acute illness and occurrence of post-leptospirosis symptoms of patients in the Netherlands. PLoS One. 2013;8(10):e76549 doi: 10.1371/journal.pone.0076549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cerqueira GM, Picardeau M. A century of Leptospira strain typing. Infect Genet Evol. 2009;9(5):760–8. doi: 10.1016/j.meegid.2009.06.009 [DOI] [PubMed] [Google Scholar]
- 10.Hartskeerl RA, Smythe LD. The role of leptospirosis reference laboratories. Curr Top Microbiol Immunol. 2015;387:273–88. doi: 10.1007/978-3-662-45059-8_11 [DOI] [PubMed] [Google Scholar]
- 11.Fouts DE, Matthias MA, Adhikarla H, Adler B, Amorim-Santos L, Berg DE, et al. What Makes a Bacterial Species Pathogenic?:Comparative Genomic Analysis of the Genus Leptospira. PLoS Negl Trop Dis. 2016;10(2):e0004403 doi: 10.1371/journal.pntd.0004403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hartskeerl RA, Collares-Pereira M, Ellis WA. Emergence, control and re-emerging leptospirosis: dynamics of infection in the changing world. Clin Microbiol Infect. 2011;17(4):494–501. doi: 10.1111/j.1469-0691.2011.03474.x [DOI] [PubMed] [Google Scholar]
- 13.Schreier S, Doungchawee G, Chadsuthi S, Triampo D, Triampo W. Leptospirosis: current situation and trends of specific laboratory tests. Expert Rev Clin Immunol. 2013;9(3):263–80. doi: 10.1586/eci.12.110 [DOI] [PubMed] [Google Scholar]
- 14.Levett PN. Leptospirosis: a forgotten zoonosis? Clin Appl Immunol Rev. 2004;4:435–48. [Google Scholar]
- 15.Matono T, Kutsuna S, Koizumi N, Fujiya Y, Takeshita N, Hayakawa K, et al. Imported Flood-Related Leptospirosis From Palau: Awareness of Risk Factors Leads to Early Treatment. Journal of travel medicine. 2015;22(6):422–4. doi: 10.1111/jtm.12241 [DOI] [PubMed] [Google Scholar]
- 16.Zuerner R. Host Response to Leptospira Infection In: Adler B, editor. Leptospira and Leptospirosis. Current Topics in Microbiology and Immunology. 387 Heidelberg, Germany: Springer-Verlag; 2015. p. 223–50. doi: 10.1007/978-3-662-45059-8_9 [DOI] [PubMed] [Google Scholar]
- 17.Lau C. Combating infectious diseases in the Pacific Islands: sentinel surveillance, environmental health, and geospatial tools. Rev Environ Health. 2014;29(1–2):113–7. doi: 10.1515/reveh-2014-0028 [DOI] [PubMed] [Google Scholar]
- 18.Lau CL, Smythe LD, Craig SB, Weinstein P. Climate change, flooding, urbanisation and leptospirosis: fuelling the fire? Trans R Soc Trop Med Hyg. 2010;104(10):631–8. doi: 10.1016/j.trstmh.2010.07.002 [DOI] [PubMed] [Google Scholar]
- 19.Lau C, Smythe L, Weinstein P. Leptospirosis: an emerging disease in travellers. Travel Med Infect Dis. 2010;8(1):33–9. doi: 10.1016/j.tmaid.2009.12.002 [DOI] [PubMed] [Google Scholar]
- 20.Bharti AR, Nally JE, Ricaldi JN, Matthias MA, Diaz MM, Lovett MA, et al. Leptospirosis: a zoonotic disease of global importance. Lancet Infect Dis. 2003;3(12):757–71. [DOI] [PubMed] [Google Scholar]
- 21.ProMED-mail. Leptospirosis—Fiji (02): more cases, flood. ProMED-mail 2016; 11 Aug: 20160813.4413510. Available from: <http://www.promedmail.org>. Accessed 20 September 2017.
- 22.Victoriano AFB, Smythe LD, Gloriani-Barzaga N, Cavinta LL, Kasai T, Limpakarnjanarat K, et al. Leptospirosis in the Asia Pacific region. BMC Infect Dis. 2009;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Musso D, Roche C, Marfel M, Bel M, Nilles EJ, Cao-Lormeau V. Improvement of leptospirosis surveillance in remote Pacific islands using serum spotted on filter paper. Int J Infect Dis. 2014;20:74–6. doi: 10.1016/j.ijid.2013.12.002 [DOI] [PubMed] [Google Scholar]
- 24.Nhan TX, Bonnieux E, Rovery C, De Pina JJ, Musso D. Fatal leptospirosis and chikungunya co-infection: Do not forget leptospirosis during chikungunya outbreaks. IDCases. 2016;5:12–4. doi: 10.1016/j.idcr.2016.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097 doi: 10.1371/journal.pmed.1000097 ; PubMed Central PMCID: PMCPMC2707599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levett PN. Usefulness of serologic analysis as a predictor of the infecting serovar in patients with severe leptospirosis. Clin Infect Dis. 2003;36(4):447–52. doi: 10.1086/346208 [DOI] [PubMed] [Google Scholar]
- 27.Smythe LD, Wuthiekanun V, Chierakul W, Suputtamongkol Y, Tiengrim S, Dohnt MF, et al. The microscopic agglutination test (MAT) is an unreliable predictor of infecting Leptospira serovar in Thailand. Am J Trop Med Hyg. 2009;81(4):695–7. doi: 10.4269/ajtmh.2009.09-0252 [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. Report of the First Meeting of the Leptospirosis Burden Epidemiology Reference Group. Geneva: 2010.
- 29.Thibeaux R, Geroult S, Benezech C, Chabaud S, Soupe-Gilbert ME, Girault D, et al. Seeking the environmental source of Leptospirosis reveals durable bacterial viability in river soils. PLoS Negl Trop Dis. 2017;11(2):e0005414 doi: 10.1371/journal.pntd.0005414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Viau EJ, Boehm AB. Quantitative PCR-based detection of pathogenic Leptospira in Hawai'ian coastal streams. J Water Health. 2011;9(4):637–46. doi: 10.2166/wh.2011.064 [DOI] [PubMed] [Google Scholar]
- 31.Heuls J. [Leptospirosis caused by Leptospira icterohemorrhagiae in Tahiti]. Bull Soc Path Exot. 1959;52(1):22–6. [PubMed] [Google Scholar]
- 32.Mailloux M, Kolochine-Erber B. Leptospirosis in former territories of the Union Francaise. Tropenmedizin und Parasitologie. 1961;12(3):307–25. [PubMed] [Google Scholar]
- 33.Segonne J, Lugagne J, Artus JC. Les aspects cliniques et bactériologiques des leptospires en Polynésie française. Med Afr Noire. 1972;19(2)(131(6)):523–7. [Google Scholar]
- 34.Cinco M, Olivotto M, Segonne J. [Serological research on the presence and spread of human leptospirosis in French Polynesia]. Bull Soc Path Exot. 1973;66(2):273–8. [PubMed] [Google Scholar]
- 35.Segonne J, Mailloux M, Lugagne J, Bernard F. Significance of leptospiroses in Tahiti pathology (a study of 66 cases of human leptospiroses from 1969 to 1972). Bull Soc Path Exot. 1973;66(5):621–7. [Google Scholar]
- 36.Mailloux A. [Human leptospiroses in the overseas departments and territories: 10 years' immunological diagnosis (1970–1979)]. Bull Soc Path Exot. 1980;73(3):229–38. [PubMed] [Google Scholar]
- 37.Jeandel P, Raoult D, Bauduceau B, Rougier Y, Mailloux M, Auger C. [Epidemiological aspects and diagnosis of 60 cases of leptospiroses in French Polynesia]. Bull Soc Path Exot. 1982;75(4):367–74. [PubMed] [Google Scholar]
- 38.Raoult D, Jeandel P, Mailloux M, Rougier Y. Thrombocytopenia and renal failure in leptospirosis. Am J Trop Med Hyg. 1983;32(6):1464 [DOI] [PubMed] [Google Scholar]
- 39.Rougier Y, Mailloux M, Bourget D, Davy R. [Immunologic survey on leptospirosis in the Marquesas Islands]. Med Trop (Mars). 1984;44(1):23–5. [PubMed] [Google Scholar]
- 40.Mailloux M, Raoult D. Leptospiroses in France in 1983. Sem Hop Paris. 1985;61(26):1925–8. [Google Scholar]
- 41.Bourdais A, Lonjon B, Vergez-Pascal R, Fournier A, Ah Lo W. Respiratory complications during leptospirosis. Report on 6 cases including 3 cases with hemodynamic study. Med Trop (Mars). 1988;48(2):149–60. [PubMed] [Google Scholar]
- 42.Perolat P, Baranton G, Postic D. Actuality of leptospirosis in France. Med Mal Infect. 1988;18(11):835–9. [Google Scholar]
- 43.Gendron Y, Prieur J, Gaufroy X, Gras C. [Leptospirosis in French Polynesia: 120 case reports]. Med Trop (Mars). 1992;52(1):21–7. [PubMed] [Google Scholar]
- 44.Hubert B. Infectious diseases in French Polynesia, 2001. Inform'Action. 2001;10(December):8–9. [Google Scholar]
- 45.Doudier B, Garcia S, Quennee V, Jarno P, Brouqui P. Prognostic factors associated with severe leptospirosis. Clin Microbiol Infect. 2006;12(4):299–300. doi: 10.1111/j.1469-0691.2005.01335.x [DOI] [PubMed] [Google Scholar]
- 46.Coudert C, Beau F, Berlioz-Arthaud A, Melix G, Devaud F, Boyeau E, et al. [Human leptospirosis in French Polynesia. Epidemiological, clinical and bacteriological features]. Med Trop (Mars). 2007;67(2):137–44. [PubMed] [Google Scholar]
- 47.Hirschauer C, Daudens E, Coudert C, Frogier E, Melix G, Fleure M, et al. Épidémiologie de la leptospirose en Polynésie française de 2006 à 2008. BEH thématique. 2009;48-49-50(22 Décembre 2009):508–11. [Google Scholar]
- 48.Guernier V, Richard V, Nhan T, Rouault E, Tessier A, Musso D. Leptospira diversity in animals and humans in Tahiti, French Polynesia. PLoS Negl Trop Dis. 2017;11(6):e0005676 doi: 10.1371/journal.pntd.0005676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Joseph-Louisia J, Mailloux M, Daguet GL. [Leptospiroses in New Caledonia. Reports of 32 cases diagnosed between 1973 and 1980]. Bull Soc Path Exot. 1982;75(5):461–5. [PubMed] [Google Scholar]
- 50.Guelain J, Le Gonidec G, Bouchard E, Peghini M. [Leptospiroses in New Caledonia]. Med Trop (Mars). 1983;43(2):137–43. [PubMed] [Google Scholar]
- 51.Mailloux M. Leptospirosis in New Caledonia (Melanesia). Zentralbl Bakteriol Mikrobiol Hyg A. 1984;257(4):540–1. [DOI] [PubMed] [Google Scholar]
- 52.Cointet F, Gilles B, Dussarat G, Le Bris H, Martini L, Brethes B, et al. [Human leptospirosis in New Caledonia and dependencies. Apropos of 57 cases observed between 1 June 1983 and 31 May 1985]. Bull Soc Path Exot. 1987;80(1):28–37. [PubMed] [Google Scholar]
- 53.Brethes B, Puech PL, Fraisse A, Dubois P, Domenech J, Bourdin P, et al. [Epidemiological study of leptospirosis in New Caledonia]. Bull Soc Path Exot. 1988;81(2):189–97. [PubMed] [Google Scholar]
- 54.Brethes B, Puech PL, Fraisse A, Dubois P, Domenech J, Bourdin P, et al. [Leptospirosis and environment. Study of 2 major foci in New Caledonia]. Rev Epidemiol Sante Publique. 1988;36(6):436–42. [PubMed] [Google Scholar]
- 55.Dussarat GV, Cointet F, Capdevielle P, Le Bris H, Brethes B. [Cardiac manifestations in leptospirosis. Apropos of 15 cases observed in New Caledonia]. Ann Cardiol Angeiol (Paris). 1988;37(8):449–53. [PubMed] [Google Scholar]
- 56.Merien F, Perolat P. Public health importance of human leptospirosis in the South Pacific: a five-year study in New Caledonia. Am J Trop Med Hyg. 1996;55(2):174–8. [DOI] [PubMed] [Google Scholar]
- 57.Perrocheau A, Perolat P. Epidemiology of leptospirosis in New Caledonia (South Pacific): a one-year survey. Eur J Epidemiol. 1997;13(2):161–7. [DOI] [PubMed] [Google Scholar]
- 58.Bouree P, Benoist L, Perolat P. [Epidemiologic and clinical study of leptospirosis in Bourail (New Caledonia)]. Bull Soc Path Exot. 1999;92(1):51–5. [PubMed] [Google Scholar]
- 59.Berlioz-Arthaud A, Merien F. Leptospirosis report 2005: New Caledonia. Inform'Action. 2006;23(May):14–8. [Google Scholar]
- 60.Salaun L, Merien F, Gurianova S, Baranton G, Picardeau M. Application of multilocus variable-number tandem-repeat analysis for molecular typing of the agent of leptospirosis. J Clin Microbiol. 2006;44(11):3954–62. doi: 10.1128/JCM.00336-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Berlioz-Arthaud A, Merien F, Baranton G. [Laboratory based human leptospirosis surveillance in New Caledonia (2001–2005)]. Bull Soc Path Exot. 2007;100(2):133–8. [PubMed] [Google Scholar]
- 62.Goarant C, Laumond-Barny S, Perez J, Vernel-Pauillac F, Chanteau S, Guigon A. Outbreak of leptospirosis in New Caledonia: diagnosis issues and burden of disease. Trop Med Int Health. 2009;14(8):926–9. doi: 10.1111/j.1365-3156.2009.02310.x [DOI] [PubMed] [Google Scholar]
- 63.Guerrier G, Hie P, Gourinat AC, Huguon E, Polfrit Y, Goarant C, et al. Association between age and severity to leptospirosis in children. PLoS Negl Trop Dis. 2013;7(9):e2436 doi: 10.1371/journal.pntd.0002436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tubiana S, Mikulski M, Becam J, Lacassin F, Lefevre P, Gourinat AC, et al. Risk factors and predictors of severe leptospirosis in New Caledonia. PLoS Negl Trop Dis. 2013;7(1):e1991 doi: 10.1371/journal.pntd.0001991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Weinberger D, Baroux N, Grangeon JP, Ko AI, Goarant C. El Nino Southern Oscillation and leptospirosis outbreaks in New Caledonia. PLoS Negl Trop Dis. 2014;8(4):e2798 doi: 10.1371/journal.pntd.0002798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Alicata JE, Breaks V. A survey of leptospirosis in Honolulu. Hawaii Med J. 1943;2:137–42. [Google Scholar]
- 67.Alicata JE. A study of leptospirosis in Hawaii. Plant Health. 1944;8:7–32. [Google Scholar]
- 68.Jensen WL Jr., Miller FL, Wong F, Bethlenfalvay N. Clinical leptospirosis in Hawaii. Hawaii Med J. 1965;24:273–6. [PubMed] [Google Scholar]
- 69.Shrader WA Jr. Leptospirosis in Hawaii. Hawaii Med J. 1977;36(5):135–8. [PubMed] [Google Scholar]
- 70.Anderson BS, Minette HP. Leptospirosis in Hawaii: shifting trends in exposure, 1907–1984. Int J Zoonoses. 1986;13(2):76–88. [PubMed] [Google Scholar]
- 71.Katz AR, Manea SJ, Sasaki DM. Leptospirosis on Kauai: investigation of a common source waterborne outbreak. Am J Public Health. 1991;81(10):1310–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sasaki DM, Pang L, Minette HP, Wakida CK, Fujimoto WJ, Manea SJ, et al. Active surveillance and risk factors for leptospirosis in Hawaii. Am J Trop Med Hyg. 1993;48(1):35–43. [DOI] [PubMed] [Google Scholar]
- 73.Katz AR, Sasaki DM, Mumm AH, Escamilla J, Middleton CR, Romero SE. Leptospirosis on Oahu: an outbreak among military personnel associated with recreational exposure. Mil Med. 1997;162(2):101–4. [PubMed] [Google Scholar]
- 74.O'Brien MM, Vincent JM, Person DA, Cook BA. Leptospirosis and pancreatitis: A report of ten cases. Pediatr Infect Dis J. 1998;17(5):436–8. [DOI] [PubMed] [Google Scholar]
- 75.Katz AR, Ansdell VE, Effler PV, Middleton CR, Sasaki DM. Assessment of the clinical presentation and treatment of 353 cases of laboratory-confirmed leptospirosis in Hawaii, 1974–1998. Clin Infect Dis. 2001;33(11):1834–41. doi: 10.1086/324084 [DOI] [PubMed] [Google Scholar]
- 76.Manea SJ, Sasaki DM, Ikeda JK, Bruno PP. Clinical and epidemiological observations regarding the 1998 Kauai murine typhus outbreak. Hawaii Med J. 2001;60(1):7–11. [PubMed] [Google Scholar]
- 77.Katz AR, Ansdell VE, Effler PV, Middleton CR, Sasaki DM. Leptospirosis in Hawaii, 1974–1998: epidemiologic analysis of 353 laboratory-confirmed cases. Am J Trop Med Hyg. 2002;66(1):61–70. [DOI] [PubMed] [Google Scholar]
- 78.Katz AR, Effler PV, Ansdell VE. Comparison of serology and isolates for the identification of infecting leptospiral serogroups in Hawaii, 1979–1998. Trop Med Int Health. 2003;8(7):639–42. [DOI] [PubMed] [Google Scholar]
- 79.Lettieri C, Moon J, Hickey P, Gray M, Berg B, Hospenthal D. Prevalence of Leptospira antibodies in U.S. Army blood bank donors in Hawaii. Mil Med. 2004;169(9):687–90. [DOI] [PubMed] [Google Scholar]
- 80.Gaynor K, Katz AR, Park SY, Nakata M, Clark TA, Effler PV. Leptospirosis on Oahu: an outbreak associated with flooding of a university campus. Am J Trop Med Hyg. 2007;76(5):882–5. [PubMed] [Google Scholar]
- 81.Ellis T, Imrie A, Katz AR, Effler PV. Underrecognition of leptospirosis during a dengue fever outbreak in Hawaii, 2001–2002. Vector Borne Zoonotic Dis. 2008;8(4):541–7. doi: 10.1089/vbz.2007.0241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hurst FP, Neff RT, Katz AR, Buchholz AE, Sasaki DM, Berg BW, et al. Acute kidney injury requiring hemodialysis in patients with anicteric leptospirosis. Clin Nephrol. 2009;72(3):186–92. [DOI] [PubMed] [Google Scholar]
- 83.Duplessis CA, Sklar MJ, Maves RC, Spichler A, Hale B, Johnson M, et al. Hemoptysis associated with leptospirosis acquired in Hawaii, USA. Emerg Infect Dis. 2011;17(12):2375–7. doi: 10.3201/eid1712.110700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Katz AR, Buchholz AE, Hinson K, Park SY, Effler PV. Leptospirosis in Hawaii, USA, 1999–2008. Emerg Infect Dis. 2011;17(2):221–6. doi: 10.3201/eid1702.101109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Saville P. The animal health status of the pacific island countries and territories—1994 Noumea, New Caledonia: South Pacific Commission; 1996. [Google Scholar]
- 86.de Fredrick DF, Reece RL. Diseases of cattle in the Solomon Islands. Australian veterinary journal. 1980;56(11):522–5. [DOI] [PubMed] [Google Scholar]
- 87.Musso D, La Scola B. Laboratory diagnosis of leptospirosis: a challenge. J Microbiol Immunol Infect. 2013;46(4):245–52. doi: 10.1016/j.jmii.2013.03.001 [DOI] [PubMed] [Google Scholar]
- 88.Alicata JE, Breaks V. Incidence of leptospirosis among dogs in Honolulu as determined by serological agglutination tests. Journal of the Washington Academy of Sciences. 1942;32(10):305–8. [Google Scholar]
- 89.Wallace GD, Gross B, Lee R. Leptospirosis survey of small mammals on the island of Hawaii. 10th Pacific Scientific Congress; Honolulu, Hawaii 1961.
- 90.Minette HP. Leptospirosis in rodents and mongooses on the island of Hawaii. Am J Trop Med Hyg. 1964;13:826–32. [DOI] [PubMed] [Google Scholar]
- 91.Higa HH, Fujinaka IT. Prevalence of rodent and mongoose leptospirosis on the Island of Oahu. Public Health Rep. 1976;91(2):171–7. [PMC free article] [PubMed] [Google Scholar]
- 92.Tomich PQ. Studies of leptospirosis in natural host populations. 1. Small mammals of Waipio valley, Island of Hawaii. Pacific Science. 1979;33(3):257–79. [Google Scholar]
- 93.Shimizu MM. Environmental and biological determinants for the prevalence of leptospirosis among wild small mammal hosts, island of Hawaii. Int J Zoonoses. 1984;11(2):173–88. [PubMed] [Google Scholar]
- 94.Miller DA, Wilson MA, Beran GW. Relationships between prevalence of Leptospira interrogans in cattle, and regional, climatic, and seasonal factors. Am J Vet Res. 1991;52(11):1766–8. [PubMed] [Google Scholar]
- 95.Aguirre AA, Keefe TJ, Reif JS, Kashinsky L, Yochem PK, Saliki JT, et al. Infectious disease monitoring of the endangered Hawaiian monk seal. J Wildl Dis. 2007;43(2):229–41. doi: 10.7589/0090-3558-43.2.229 [DOI] [PubMed] [Google Scholar]
- 96.Wong M, Katz AR, Li D, Wilcox BA. Leptospira infection prevalence in small mammal host populations on three Hawaiian islands. Am J Trop Med Hyg. 2012;87(2):337–41. doi: 10.4269/ajtmh.2012.12-0187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Buchholz AE, Katz AR, Galloway R, Stoddard RA, Goldstein SM. Feral Swine Leptospira Seroprevalence Survey in Hawaii, USA, 2007–2009. Zoonoses Public Health. 2016;63(8):584–7. doi: 10.1111/zph.12266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Perez J, Goarant C. Rapid Leptospira identification by direct sequencing of the diagnostic PCR products in New Caledonia. BMC Microbiol. 2010;10:325 doi: 10.1186/1471-2180-10-325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Domenech J, Lechapt M. Animal leptospirosis: prevalence in the South Pacific [in French]. Rev Elev Med Vet Pays Trop Nouvelle-Calédonie. 1983;2:1–8. [Google Scholar]
- 100.Thevenon JG, Morlet B, Costa R, Lambert C. Etude de la cinétique du taux d'anticorps antileptospirosiques sur des bovins du Centre de Recherche Zootechnique de Port-Laguerre. Rev Elev Med Vet Pays Trop Nouvelle-Calédonie. 1987;10:7–12. [Google Scholar]
- 101.Thevenon JG, Lambert C, Desouter D, Costa R, Domenech J. Epidemiologic study of bovine leptospirosis in New Caledonia. Rec Med Vet Ec Alfort. 1990;166(10):903–9. [Google Scholar]
- 102.Perez J, Brescia F, Becam J, Goarant C. Deciphering leptospirosis eco-epidemiology in New Caledonia. BMC Proc. 2011;5:P110 doi: 10.1186/1753-6561-5-S8-P11022373255 [Google Scholar]
- 103.Perez J, Brescia F, Becam J, Mauron C, Goarant C. Rodent abundance dynamics and leptospirosis carriage in an area of hyper-endemicity in New Caledonia. PLoS Negl Trop Dis. 2011;5(10):e1361 doi: 10.1371/journal.pntd.0001361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Roqueplo C, Cabre O, Davoust B, Kodjo A. Epidemiological study of animal leptospirosis in new caledonia. Vet Med Int. 2013;2013:826834 doi: 10.1155/2013/826834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gay N, Soupe MEG, Goarant C. Though not reservoirs, dogs might transmit Leptospira in New Caledonia. Int J Environ Res Public Health. 2014;11(4):4316–25. doi: 10.3390/ijerph110404316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Daudens E, Frogier E, Mallet H-P. Recrudescence of leptospirosis in French Polynesia in early 2010. Inform'Action. 2010;32:3–6. [Google Scholar]
- 107.Daudens E, Mallet H-P, Buluc A, Frogier E. Situation épidémiologique de la leptospirose en Pf (2006–2010). BISES. 2011;Décembre(5):6–8. [Google Scholar]
- 108.Raust P. Animal leptospirosis in French Polynesia. Preliminary serological investigations [in French]. Rev Elev Med Vet Pays Trop Nouvelle-Calédonie. 1988;12:15–9. [Google Scholar]
- 109.Ram P. Epidemiology of leptospirosis in Fiji. Fiji Med J. 1978;6:70–2. [Google Scholar]
- 110.Ram P, Mataika JU, Metcalfe RV, Bettelheim KA. Antibody levels to Brucella abortus, Toxoplasma gondii, and Leptospira serogroups, in sera collected from healthy people in Fiji. Comp Immunol Microbiol Infect Dis. 1982;5(4):397–403. [DOI] [PubMed] [Google Scholar]
- 111.Lau CL, Watson CH, Lowry JH, David MC, Craig SB, Wynwood SJ, et al. Human Leptospirosis Infection in Fiji: An Eco-epidemiological Approach to Identifying Risk Factors and Environmental Drivers for Transmission. PLoS Negl Trop Dis. 2016;10(1):e0004405 doi: 10.1371/journal.pntd.0004405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ram P. Leptospiral meningitis. Fiji Med J. 1982;May-Jun:76–8. [Google Scholar]
- 113.Ram P, Collings DF. Further observations on the epidemiology of leptospirosis in Fiji. Fiji Med J. 1982;May-Jun:71–5. [Google Scholar]
- 114.Ram P, Chandra MS. Unusual electrocardiographic abnormality in leptospirosis: case reports. Angiology. 1985;36(7):477–82. doi: 10.1177/000331978503600711 [DOI] [PubMed] [Google Scholar]
- 115.Gill AC, Allen H, Campbell D. Fever in a teenage traveller. J Paediatr Child Health. 2002;38(6):610–1. [DOI] [PubMed] [Google Scholar]
- 116.Lau CL, Mayfield HJ, Lowry JH, Watson CH, Kama M, Nilles EJ, et al. Unravelling infectious disease eco-epidemiology using Bayesian networks and scenario analysis: A case study of leptospirosis in Fiji. Environ Modell Softw. 2017;97:271–86. [Google Scholar]
- 117.Munro R. Leptospirosis in the animal population in Fiji. Fiji Med J. 1978;6:79–80. [Google Scholar]
- 118.Collings DF. Leptospira interrogans infection in domestic and wild animals in Fiji. N Z Vet J. 1984;32(3):21–4. doi: 10.1080/00480169.1984.35050 [DOI] [PubMed] [Google Scholar]
- 119.Lupo C. Epidemiological study of animal Leptospirosis in Fiji Islands [Veterinary Thesis]. France: Ecole Nationale Veterinaire de Toulouse; 2003.
- 120.Togami E. Animal & Human Leptospirosis In A High Transmission Setting In Fiji [Public Health Thesis]: Yale University; 2016.
- 121.Forbes BRV, Wannan JS. Leptospiral infection in natives of the territory of Papua and New Guinea. Aust Ann Med. 1955;4(1):64–9. [DOI] [PubMed] [Google Scholar]
- 122.Emanuel ML. Leptospiral infections in Papua. Papua N Guinea Med J. 1959;3(3):76–80. [Google Scholar]
- 123.Willis MF, Wannan JS. Some aspects of the epidemiology of leptospirosis in New Guinea. Med J Aust. 1966;53(4):129–36. [DOI] [PubMed] [Google Scholar]
- 124.Kariks J, Stallman ND. Human leptospirosis, proven by culture, in the territory of Papua and New Guinea. Med J Aust. 1968;2(1):20. [DOI] [PubMed] [Google Scholar]
- 125.Forbes BRV, Wannan JS. Examination of domestic and field animals of the territory of Papua and New Guinea for evidence of leptospiral infection. Aust J Sci. 1958;21:121. [Google Scholar]
- 126.Wannan JS. Leptospiral serotypes in Australasia. Aust Vet J. 1955;31(12):297–301. [Google Scholar]
- 127.Morahan RJ. Isolation of leptospires in the tarassovi (Hyos) serogroup from a bandicoot (Marsupialia, peramelidae) from Koil Island, territory of Papua and New Guinea. Med J Aust. 1968;2(1):18–9. [DOI] [PubMed] [Google Scholar]
- 128.Morahan RJ. Further leptospiral isolations in the Sepik district, Territory of Papua and New Guinea. Med J Aust. 1971;1(5):276–7. [DOI] [PubMed] [Google Scholar]
- 129.Babudieri B, D'Aquino A. Systematics of leptospirae strains isolated in the Sepik District, Papua New Guinea. Med J Aust. 1973;1(14):701 [DOI] [PubMed] [Google Scholar]
- 130.Wai’in PM. Epidemiology of infection with Leptospira species in Livestock in Papua New Guinea [PhD Thesis]. Perth, Australia: School of Biomedical and Veterinary Sciences, Murdoch University; 2007.
- 131.Ryu E, Haddock RL. Leptospirosis within the Territory of Guam: prevalence among canines. Micronesica. 1974;10(1):13–5. [Google Scholar]
- 132.Duguies M, Nusbaum S, Saville P. ADAP Animal Health Survey for Guam 1999. 2000.
- 133.Cleveland CA, DeNicola A, Dubey JP, Hill DE, Berghaus RD, Yabsley MJ. Survey for selected pathogens in wild pigs (Sus scrofa) from Guam, Marianna Islands, USA. Vet Microbiol. 2017;205:22–5. doi: 10.1016/j.vetmic.2017.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Dziuban EJ, Liang JL, Craun GF, Hill V, Yu PA, Painter J, et al. Surveillance for waterborne disease and outbreaks associated with recreational water—United States, 2003–2004. MMWR Surveill Summ. 2006;55(12):1–30. [PubMed] [Google Scholar]
- 135.Singh N. Pacific Island Environmental Conference—Guam, 20–24 June 2005. Inform'Action. 2005;21:19–23. [Google Scholar]
- 136.Haddock RL, Gilmore JW, Pimentel F. A leptospirosis outbreak on Guam associated with an athletic event. Pac Health Dialog. 2002;9(2):186–9. [PubMed] [Google Scholar]
- 137.Morisse L, Roualen G, Yvon J-F. Leptospirosis in Wallis and Futuna in 2005. Inform'Action. 2006;23:10–3. [Google Scholar]
- 138.Giraud P, Toutain B, Domenech J, Brégeat D. Présentation de l'élevage aux îles Wallis et Futuna. Rev Elev Med Vet Pays Trop. 1987;40(2):173–9. [Google Scholar]
- 139.Martin T. The animal health status of Wallis & Futuna. Noumea, New Caledonia: Secretariat of the Pacific Community, 2000. [Google Scholar]
- 140.Theuerkauf J, Perez J, Taugamoa A, Niutoua I, Labrousse D, Gula R, et al. Leptospirosis risk increases with changes in species composition of rat populations. Naturwissenschaften. 2013;100(4):385–8. doi: 10.1007/s00114-013-1033-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Alicata JE. Observations on leptospiral infections in Samoa. Hawaii Med J. 1949;9(2):85–9. [PubMed] [Google Scholar]
- 142.Bouslough DB, Partridge R, Thome T. Leptospirosis and dengue fever co-infection: A report of three representative cases. Am J Trop Med Hyg. 2011;85(6 Suppl 1):406–7. [Google Scholar]
- 143.Lau CL, DePasquale JM. Leptospirosis, diagnostic challenges, American Samoa. Emerg Infect Dis. 2012;18(12):2079–81. doi: 10.3201/eid1812.120429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Leptospirosis: A Seroprevalence Survey on American Samoa. [Internet]. 2004. Available from: http://www.botany.hawaii.edu/basch/uhnpscesu/pdfs/sam/Winger2004AS.pdf.
- 145.Lau CL, Dobson AJ, Smythe LD, Fearnley EJ, Skelly C, Clements AC, et al. Leptospirosis in American Samoa 2010: epidemiology, environmental drivers, and the management of emergence. Am J Trop Med Hyg. 2012;86(2):309–19. doi: 10.4269/ajtmh.2012.11-0398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Lau CL, Skelly C, Smythe LD, Craig SB, Weinstein P. Emergence of new leptospiral serovars in American Samoa—ascertainment or ecological change? BMC Infect Dis. 2012;12:19 doi: 10.1186/1471-2334-12-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lau CL, Clements AC, Skelly C, Dobson AJ, Smythe LD, Weinstein P. Leptospirosis in American Samoa—estimating and mapping risk using environmental data. PLoS Negl Trop Dis. 2012;6(5):e1669 doi: 10.1371/journal.pntd.0001669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Pavlin B. Draft Mission Report: Suspected Systemic Febrile Illness Outbreak. Chuuk State, Federated States of Micronesia: World Health Organization, Office of the South Pacific, 2010. [Google Scholar]
- 149.Colt S, Pavlin BI, Kool JL, Johnson E, McCool JP, Woodward AJ. Human leptospirosis in The Federated States of Micronesia: a hospital-based febrile illness survey. BMC Infect Dis. 2014;14:186 doi: 10.1186/1471-2334-14-186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Musso D, Roche C, Marfel M, Bel M, Nilles EJ, Cao-Lormeau VM. Improvement of leptospirosis surveillance in remote Pacific islands using serum spotted on filter paper. Int J Infect Dis. 2014;20:74–6. doi: 10.1016/j.ijid.2013.12.002 [DOI] [PubMed] [Google Scholar]
- 151.McIver L, Hashizume M, Kim H, Honda Y, Pretrick M, Iddings S, et al. Assessment of Climate-sensitive Infectious Diseases in the Federated States of Micronesia. Trop Med Health. 2015;43(1):29–40. doi: 10.2149/tmh.2014-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Hartmann FW. Further Observations on Leptospirosis in Micronesia. Science (New York, NY). 1947;106(2752):294. [DOI] [PubMed] [Google Scholar]
- 153.Simms JR. Animal leptospirosis in the Federated States of Micronesia. Pac Health Dialog. 1998;5(1):30–7. [Google Scholar]
- 154.Baker AA. Annual report of the Chief Veterinary Officer. Solomon Islands Government: Veterinary/Livestock Department, Ministry of Agriculture and Lands, Honiara, 1985. [Google Scholar]
- 155.Martin T, Epstein V. The animal health status of the Solomon Islands Noumea, New Caledonia: Secretariat of the Pacific Community, 1999. [Google Scholar]
- 156.Perolat P, Reeve PA. First evidence of leptospirosis in Vanuatu. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1992;86(5):557–9. [DOI] [PubMed] [Google Scholar]
- 157.Moranne O, Queyrel V. Leptospirosis in Espiritu Santo, Vanuatu, 8 case reports. Med Trop (Mars). 2003;63(6):611–3. [PubMed] [Google Scholar]
- 158.O'Leary FM, Hunjan JS, Bradbury R, Thanakrishnan G. Fatal leptospirosis presenting as musculoskeletal chest pain. Med J Aust. 2004;180(1):29–31. [DOI] [PubMed] [Google Scholar]
- 159.Schandevyl P, Deleu D. Diseases and parasites of cattle in Vanuatu. Aust Vet J. 1985;62(9):297–300. [DOI] [PubMed] [Google Scholar]
- 160.Pineda MD. Leptospirosis in Palau. Inform'Action. 2001;8(May):9–11. [Google Scholar]
- 161.Stevens AM, Carter K, Kiep R, Stevenson K, Schneeweiss R. The epidemiology of leptospirosis in Palau. Pac Health Dialog. 2011;17(1):129–38. [PubMed] [Google Scholar]
- 162.Saville P. The animal health status of Palau Noumea, New Caledonia: Secretariat of the Pacific Community, 1999. [Google Scholar]
- 163.Saville P. The animal health status of Tonga Noumea, New Caledonia: Secretariat of the Pacific Community, 1996. [Google Scholar]
- 164.Villagomez JK, Brostrom R, Diaz EP, Tagabuel J, Habib F. Leptospirosis in the Northern Mariana islands. Inform'Action. 2001;10(December):4–7. [Google Scholar]
- 165.Boulanger P, Gray DP, Gibbs HC, Murphy DA. A serological survey of sera from domestic animals on Easter Island. Can J Comp Med. 1968;32(2):425–9. [PMC free article] [PubMed] [Google Scholar]
- 166.Saville P. The animal health status of Kiribati Noumea, New Caledonia: South Pacific Commission, 1996. [Google Scholar]
- 167.Saville P. The animal health status of Niue Noumea, New Caledonia: South Pacific Comission, 1996. [Google Scholar]
- 168.Saville P. The animal health status of the Cook Islands Suva, Fiji: Secretariat of the Pacific Community / RMC; 1996. [Google Scholar]
- 169.de Rooij RJ. Animal health and production—Western Samoa; end of assignment report. FAO, 1979. [Google Scholar]
- 170.Martin T. The animal health status of Samoa Suva, Fiji Secretariat of the Pacific Community, 1999. [Google Scholar]
- 171.Martin T. The animal health status of Tokelau Noumea, New Caledonia: Secretariat of the Pacific Community, 1999. [Google Scholar]
- 172.Guernier V, Allan KJ, Goarant C. Advances and challenges in barcoding pathogenic and environmental Leptospira. Parasitology. 2017:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Faine S, Adler B, Bolin C, Perolat P. Leptospira and Leptospirosis 2nd Edition ed. Melbourne, Australia: MedSci; 1999. 295 p. [Google Scholar]
- 174.Allan KJ, Biggs HM, Halliday JE, Kazwala RR, Maro VP, Cleaveland S, et al. Epidemiology of Leptospirosis in Africa: A Systematic Review of a Neglected Zoonosis and a Paradigm for 'One Health' in Africa. PLoS Negl Trop Dis. 2015;9(9):e0003899 doi: 10.1371/journal.pntd.0003899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Jancloes M, Bertherat E, Schneider C, Belmain S, Munoz-Zanzi C, Hartskeerl R, et al. Towards a “One Health” Strategy against Leptospirosis. GRF Davos Planet@Risk. 2014;2(3):204–6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
A list of electronic databases browsed is provided, as well as the complete search strategy, including search terms.
(DOC)
The complete reference is provided for each study, as well as the island(s) where the study took place, the target (human vs animal) and the type of study. Human clinical studies were reported as strong or weak evidence of leptospirosis following the criteria detailed in the methods section. The 11 studies for which the full text document could not be retrieved are indicated.
(XLSX)
The results are reported per study, indicating where (island(s)) and when (year(s)) the study was conducted, the target (human vs animal), the animal species investigated when relevant and the serogroup. Serology results are reported as in the study, i.e. potentially including cross-reactions between serovars and serogroups, paradoxical reactions or anamnestic responses. For this reason, and because of the limitations of the MAT, some results were considered as “weak evidence” of leptospirosis following the criteria detailed in the methods section; thus this table should be interpreted with caution.
(XLS)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.