Abstract
Common variable immunodeficiency (CVID) is a heterogeneous disorder with decreased production of immunoglobulins that presents with recurrent and serious infections in ∼90% of cases. Review of the literature showed only 12 cases of gastrointestinal infection of cytomegalovirus in patients with CVID. We present an unusual case of a CVID patient presenting with new-onset hematochezia. With proper clinical suspicion and endoscopic evaluation, cytomegalovirus colitis was diagnosed and acute bleeding was successfully treated endoscopically.
Introduction
Various studies have been published concerning patients with common variable immunodeficiency (CVID), and the incidence of cytomegalovirus (CMV) colitis in such patients was very low. One study reported only 1 case of CMV colitis in 248 patients with CVID,1 and another reported only 1 case of CMV colitis in 313 patients with CVID.2 Although it is rare, it is important to consider CMV in the differential diagnosis in CVID with new or worsening gastrointestinal (GI) symptoms, given that the complications of CMV infection of the GI tract are potentially life-threatening bleeding and perforation.3
Case Report
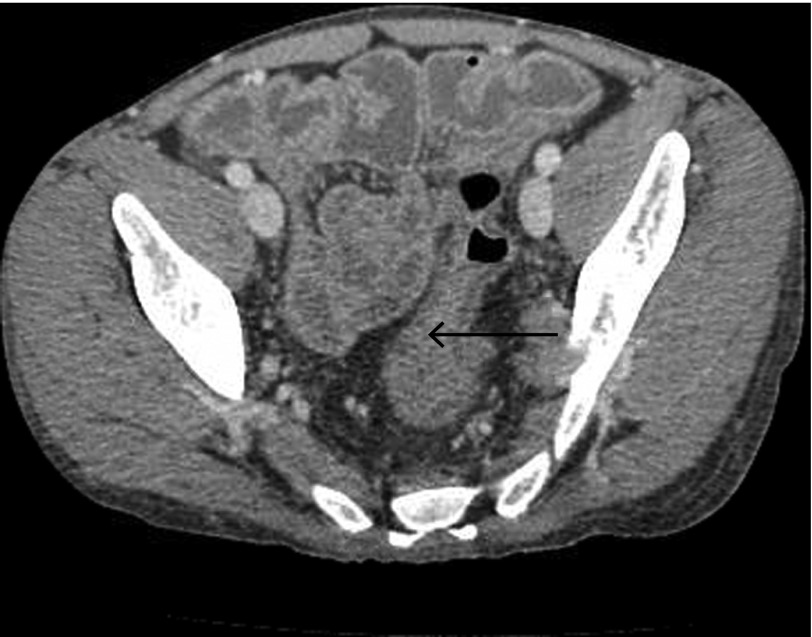
A 27-year-old white man with CVID diagnosed at the age of 10, being treated with intravenous immunoglobulin, was admitted for hematochezia. He had a history of CVID-induced enteropathy with 4–5 bowel movements per day, for which he took low-dose prednisone every other day along with enteral budesonide. He also had CMV proctitis 5 years previously, which was treated medically. Subsequent episodes of viremia were treated intermittently with antivirals. His last episode of viremia, 3 months ago, was successfully suppressed with foscarnet because he developed resistance to ganciclovir. Upon presentation, he complained of generalized abdominal pain along with 4 episodes of hematochezia 1 day prior to admission. Vitals on admission were normal. Examination showed soft, non-distended abdomen with normal bowel sounds and tenderness in the right lower quadrant. Rectal examination showed streaks of blood. Abdominal computed tomography (CT) revealed nodular thickening of the small bowel and circumferential thickening of the rectum, sigmoid, and descending colon, which were unchanged from an abdominal CT done 2 months prior (Figure 1). Pertinent initial labs included hemoglobin 9.9 gm/dL (down from 11.6 gm/dL 2 days before the admission), mean corpuscular volume 68 fL, white blood cell count 13.7 K/mL, platelets 153 K/mL, and lactic acid 2.2 mMol/L. The remainder of the labs were normal.
Figure 1.
Computed tomography showing thickening of sigmoid colon and rectum (arrow).
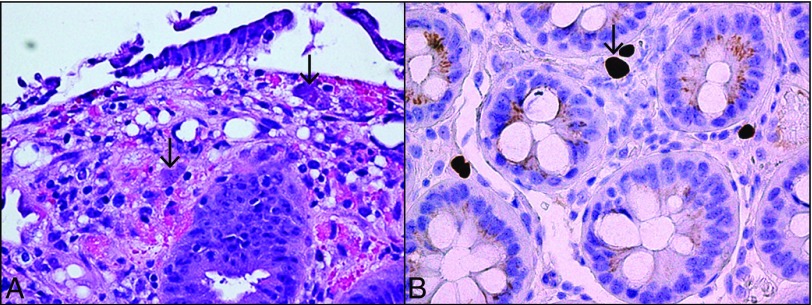
Shortly after admission, the bleeding stopped. Colonoscopy to evaluate the source of hematochezia revealed diffuse colonic wall edema along with a 2-cm ulcer and an overlying clot at the distal end of the ileocecal valve. No active bleeding was seen after suctioning of the clot, but a small visible vessel was cauterized with a bipolar circumactive probe. Biopsies obtained from the center and margins of the ulcer, as well as from random colonic mucosa, demonstrated tissue CMV, and the patient was started on intravenous foscarnet (Figure 2). Six days later, lower GI bleeding returned with a significant decrease in hemoglobin requiring transfusion. At repeat colonoscopy, a large clot was noted along with a bleeding visible vessel on the margin of the previously treated and biopsied ulcer (Figure 3). Epinephrine was injected, and an endoscopic clip was applied with successful hemostasis (Figure 4).
Figure 2.
(A) Hematoxylin and eosin stain showing enlarged endothelial cells (arrows) with intracytoplasmic and nuclear inclusions. (B) Immunohistochemistry showing cytomegalovirus (arrow).
Figure 3.
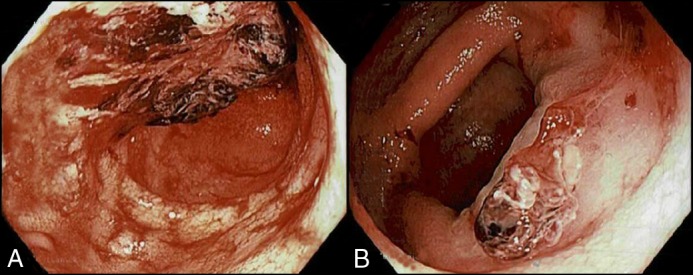
Repeat colonoscopy showing (A) a large ulcer on the ileocecal valve with active bleeding and an overlying clot, and (B) a visible vessel at the margin of the ulcer.
Figure 4.
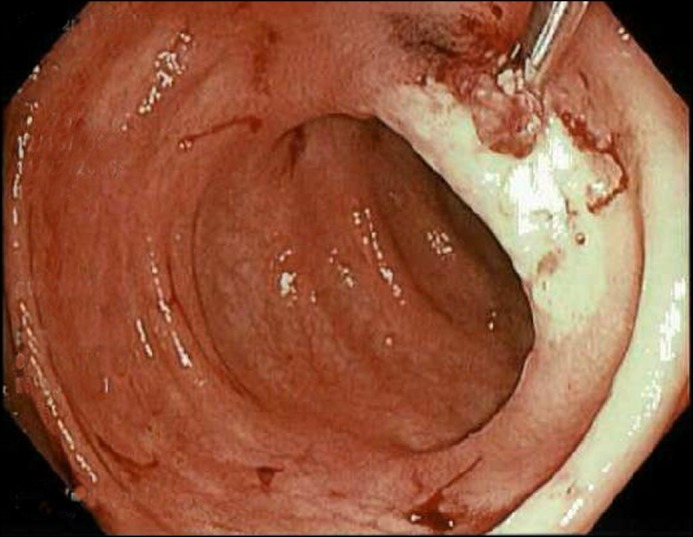
Successful application of an endoscopic clip for hemostasis.
The patient was monitored for several more days with no re-bleeding. However, because of intolerable side effects, including myalgias and electrolyte abnormalities, foscarnet had to be stopped and the CMV immunoglobulin (IG) CytoGam (CSL Behring, King of Prussia, Pennsylvania) was started. The viral load decreased from 30,900 IU/mL to 7,200 IU/mL with no recurrence of GI bleed in the 7-month follow-up period while on CytoGam treatment. Repeat endoscopy was not needed.
Discussion
CVID is the most common primary immunodeficiency syndrome. It is characterized by a defect in IG production. The underlying pathogenic defect affecting terminal B cell differentiation results in a decrease in plasma cells and subsequent hypogammaglobulinemia.4 However, abnormalities with T-lymphocyte proliferation in response to antigens and a low CD4:CD8 ratio have also been reported in subsets of patients.1,5 CMV has been implicated in inducing/worsening CVID enteropathy, which is generally attributed to an exaggerated T-cell response to CMV.6 These observations are based on the findings that CD8+ T cells from patients displaying an inverted CD4:CD8 ratio co-express CD57 and HLA-DR molecules, a phenotype that is also seen in patients infected with viruses like CMV, Epstein-Barr virus, and HIV.4 Our patient also had an inverted CD4:CD8 ratio (0.68).
Common opportunistic infections seen in CVID are Pneumo-cystis jiroveci, scarring Herpes zoster, Mycobacterium species, Aspergillus species, Candida species, and Toxoplasma gondii.2 In addition to the GI tract, CMV infection has been reported as a cause of retinitis, pneumonia, pleuritis, and lymphadenitis in patients with CVID.2 The data available on CMV infection in CVID is scarce, some of which is attributed to underreporting. A search of the English literature showed only 12 cases of CMV affecting the GI tract in patients with CVID for the 1966–2017 period.2,3,6-11 We were able to review 9 of those patients; details of the other cases could not be found.
The average age at presentation was 42 years, with a male predominance. Seven cases out of 10, including the patient described in this case report, had colonic involvement.2,3,6,7,10,11 The most common symptoms included worsening diarrhea and weight loss. CVID-associated enteropathy also presents with chronic diarrhea and weight loss. A history of CMV infection, worsening of baseline symptoms, hematochezia, and histological changes of CMV are clues that favor CMV colitis over CVID enteropathy. Bleeding was the presenting symptom in 2 patients, including the current case; the other patient required colectomy for active GI bleeding and perforation and died during the same admission.3 Endoscopic hemostasis helped our patient avoid surgery.
The diagnosis of CMV organ involvement requires histological and immunohistochemical stain examination on biopsy specimens.12 Serum polymerase chain reaction (PCR) is of limited use, but it may be used as an adjunctive tool to monitor response to antiviral treatment.13 Colonic tissue PCR is considered an overly sensitive test that can detect even mild CMV infections of no clinical significance.14
Intravenous ganciclovir is the treatment of choice, and it can be switched to oral valganciclovir as an outpatient regimen. In patients who develop resistance to ganciclovir, foscarnet may be used as an alternative. Very limited data are available on the role of CytoGam and the duration of use for the treatment of CMV infection in the GI tract in CVID. CMV infection, though rare, should be a part of the differential diagnosis in CVID patients presenting with lower GI bleeding becaues timely endoscopic hemostasis may be helpful as in our patient. This case provides a valuable demonstration of the GI manifestations of CMV in CVID and the challenges in its management with antiviral agents.
Disclosures
Author contributions: P. Kathi wrote the manuscript. M. Tama, V. Reddy, S. Kundumadam, O. Al-Subee, and M. N. Ehrinpreis edited the manuscript. M. Tama is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Cunningham-Rundles C, Bodian C. Common variable immunodeficiency: Clinical and immunological features of 248 patients. Clin Immunol. 1999;92(1):34–48. [DOI] [PubMed] [Google Scholar]
- 2.Kralickova P, Mala E, Vokurkova D, et al. . Cytomegalovirus disease in patients with common variable immunodeficiency: Three case reports. Int Arch Allergy Immunol. 2014;163(1):69–74. [DOI] [PubMed] [Google Scholar]
- 3.Ünal B, Başsorgun CI, Çil Gönülcü S, Uçar A, Çelik F, Elpek GÖ. Cytomegalovirus colitis with common variable immunodeficiency and Crohn’s disease. Case Rep Med. 2015;2015:348204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stack E, Washington K, Avant GR, Eisen GM. Cytomegalovirus enteritis in common variable immunodeficiency. South Med J. 2004;97(1):96–101. [DOI] [PubMed] [Google Scholar]
- 5.Raeiszadeh M, Kopycinski J, Paston SJ, et al. . The T cell response to persistent herpes virus infections in common variable immunodeficiency. Clin Exp Immunol. 2006;146(2):234–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Malphettes M, Gérard L, Carmagnat M, et al. . Late‐onset combined immune deficiency: A subset of common variable immunodeficiency with severe T cell defect. Clin Infect Dis. 2009;49(9):1329–38. [DOI] [PubMed] [Google Scholar]
- 7.Costantino G, Mondello P, Previti M, Fries W, Villanacci V. Pan-digestive tract colonization by cytomegalovirus in common variable immunodeficiency. Int Arch Allergy Immunol. 2014;164(1):30–31. [DOI] [PubMed] [Google Scholar]
- 8.Tahan V, Dobrucali A, Canbakan B, et al. . Cytomegalovirus infection of gastrointestinal tract with multiple ulcers and strictures, causing obstruction in a patient with common variable immunodeficiency syndrome. Dig Dis Sci. 2000;45(9):1781–85. [DOI] [PubMed] [Google Scholar]
- 9.Medlicott SAC, Coderre S, Horne G, Panaccione R. Multimodal immunosuppressant therapy in steroid-refractory common variable immunodeficiency sprue: A case report complicating cytomegalovirus infection. Int J Surg Pathol. 2006;14(1):101–6. [DOI] [PubMed] [Google Scholar]
- 10.Chua I, Standish R, Lear S, et al. . Anti-tumour necrosis factor-α therapy for severe enteropathy in patients with common variable immunodeficiency (CVID). Clin Exp Immunol. 2007;150(2):306–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buckner FS, Pomeroy C. Cytomegalovirus disease of the gastrointestinal tract in patients without AIDS. Clin Infect Dis. 2017;17(4):644–56. [DOI] [PubMed] [Google Scholar]
- 12.Kotton CN, Kumar D, Caliendo AM, et al. . Updated international consensus guidelines on the management of cytomegalovirus in solid-organ transplantation. Transplantation. 2013;96(4):333–60. [DOI] [PubMed] [Google Scholar]
- 13.Razonable RR, Hayden RT. Clinical utility of viral load in management of cytomegalovirus infection after solid organ transplantation. Clin Microbiol Rev. 2013;26(4):703–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beswick L, Ye B, Van Langenberg DR. Toward an algorithm for the diagnosis and management of CMV in patients with colitis. Inflamm Bowel Dis. 2016;22(12):2966–76. [DOI] [PubMed] [Google Scholar]