Abstract
Dried persimmon is a well-known dried fruit in Asian countries such as Japan, Korea, and China. Small bowel obstruction caused by phytobezoar is a rare but interesting pathogenesis that accounts for 2–4% of all small bowel obstructions. We present the case of an 87-year-old female who suffered from small bowel obstruction caused by ingestion of a huge, dried astringent persimmon. She was initially treated conservatively, but removal by enterotomy was performed after relief failed to be achieved with conservative therapy.
Keywords: Small bowel obstruction, Dried persimmon, Phytobezoar
Introduction
Phytobezoar is one type of bezoar encountered in the gastrointestinal tract, including the stomach and small intestine [1, 2, 3, 4]. However, huge phytobezoars are rarely seen clinically because food is usually chewed before swallowing. Most phytobezoars reported in the literature have been 30–50 mm in diameter. Our case represents the second largest phytobezoar reported to date in the English literature. Phytobezoar caused by persimmon is rare [5, 6]. We report successful treatment of a huge phytobezoar caused by a dried persimmon with a diameter of 80 mm.
Case Presentation
An 87-year-old female presented to our hospital complaining of epigastric pain, nausea, and dysorexia. She had a surgical history of enterectomy for small bowel ileus 20 years earlier. On physical examination, vital signs were stable. The abdomen was soft and nondistended with normal bowel sounds, but mild tenderness was identified in the epigastric region. The patient showed markedly poor appetite. Laboratory findings were as follows: white blood cell count, 8,200/μL (normal, 5,000–8,000); aspartate aminotransferase, 20 U/L (normal, 5–35); alanine aminotransferase, 13 U/L (normal, 5–30); alkaline phosphatase, 441 U/L (normal, 115–359); gamma-glutamyl transferase, 25 U/mL (normal, 0–50); lactate dehydrogenase, 264 U/L (normal, 106–211); albumin, 4.7 g/dL (normal, 3.7–5.5); total bilirubin, 1.01 g/dL (normal, 0.2–1.0); and C-reactive protein, 0.7 mg/dL (normal, 0–0.3). Almost all laboratory findings were within normal range.
Abdominal computed tomography (CT) revealed a mass-like lesion in the jejunum with a diameter of 80 mm and air bubbles retained in the interstices (Fig. 1). A tumor of the small intestine with necrosis was suspected, but CT made 4 days later revealed that the lesion had moved to another part of the jejunum. Based on a history of having eaten dried persimmon, ileus caused by a phytobezoar comprising dried persimmon was diagnosed.
Fig. 1.
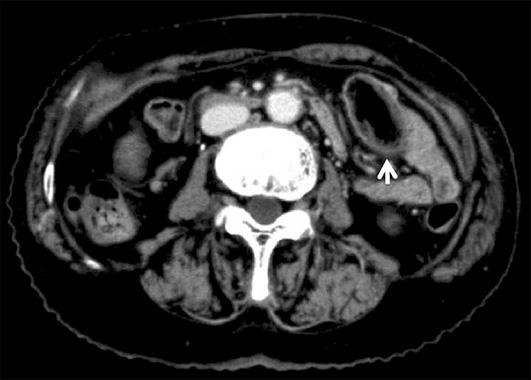
Computed tomography. The white arrow indicates a mass-like lesion in the jejunum (diameter, 80 mm) with air bubbles retained in the interstices.
The patient was hospitalized and treated conservatively, but no improvement of the symptoms was identified. The condition of the patient became more serious. On day 3 after admission, she experienced acute aggravation of epigastric distention and pain, and vomited. Laboratory findings were also further aggravated, with a C-reactive protein level increasing to 4.0 mg/dL (normal, 0–0.3). As no relief had been achieved using conservative therapy, surgical treatment was planned.
Under general anesthesia, laparotomy was performed through a low median incision. The mass was palpable in the dilated small intestine. Enterotomy was performed, and a huge, dark-brown, elliptical bezoar 80 mm in diameter was removed (Fig. 2a). The small intestine was closed using a simple interrupted suture.
Fig. 2.

Surgically exenterated specimen. a The huge, dark-brown, elliptical bezoar (diameter, 80 mm) after removal. b The cut surface of the specimen resembled the image from CT, with empty spaces retained in the interstices.
The surgically exenterated specimen was identified as a dried persimmon. The cut surface of the specimen resembled the image from CT with empty spaces retained in the interstices (Fig. 2b). The specimen was therefore identified as the swallowed dried persimmon. The patient made satisfactory postoperative progress and was discharged without complications.
Discussion
A phytobezoar is one type of bezoar, a concretion of undigested particles that usually forms in the stomach, and descends through the digestive tract where small bowel obstruction can result [1, 7, 8, 9]. Four major types of bezoar have been reported: trichobezoars; pharmacobezoars; lactobezoars; and phytobezoars. A trichobezoar is composed of hair, and is associated with psychiatric disorders such as trichotillomania. A pharmacobezoar usually comprises undigested pills from supplements and/or medications. Lactobezoars are more commonly seen in neonates, resulting from the formation of milk curds in the stomach due to the immaturity of the digestive system. Phytobezoars, as present in this case, are composed of vegetable matter and are the most common cause of bezoars [4, 6, 7, 10]. To the best of our knowledge, this case represents the second largest phytobezoar reported in the English literature and involves the oldest patient.
Phytobezoars typically comprise indigestible cellulose, tannin, and lignin derived from ingested vegetables and fruit [11]. Phytobezoar caused by persimmons have been seen in various countries, with about 50 cases reported in the English literature [5, 6, 12].
Dried persimmon is eaten primarily in Asian countries and is made from Diospyros kaki. This fruit is so bitter that it is unsuitable for being eaten raw. By drying the astringent persimmon, the tannins shift from soluble to insoluble, and the bitter taste turns sweet. Phytobezoars due to persimmons are generally attributed to overingestion of dried astringent persimmons. As dried astringent persimmons are rich in soluble tannin, this tannin is susceptible to polymerization of the cellulose, hemicellulose, and protein in the presence of the dilute hydrochloric acid in the stomach, forming the basis of the bezoar [6, 13].
Phytobezoars due to persimmons are commonly associated with previous gastric surgery (such as truncal vagotomy plus pyloroplasty or subtotal gastrectomy plus gastroenterostomy), dental problems, poor mastication, and overconsumption of persimmons [3, 4, 5]. Gastric operations may reduce gastric motility and delay gastric emptying. Gastric motility disorder and hypoacidity play an important role in the formation of phytobezoars [5, 14]. Diabetes mellitus and hypothyroidism have also been reported as predisposing factors for phytobezoar formation, as they could delay gastric emptying [6, 15]. Our patient had a history of overconsumption of dried persimmon and was using dentures, which most likely contributed to her maldigestion of the dried persimmon. Depending on the location of the phytobezoar, clinical manifestations vary from no symptoms to acute abdomen [6, 16, 17]. Major complications of phytobezoar have been reported to include intestinal obstruction, gastric perforation, gastric ulcer, and gastritis [13]. Abdominal pain (49–100%), epigastric distress (80%), anorexia, vomiting and nausea (35–78%), and small bowel obstruction (94%) are the main clinical symptoms [4, 16]. In this study, the patient presented with epigastric distress, vomiting, and small bowel obstruction.
As for the radiological findings, about 50–75% of all small bowel obstructions due to phytobezoar can be diagnosed from plain abdominal CT [18]. Phytobezoar is demonstrated by CT as a well-defined round mass with internal gas bubbles outlined in the gastrointestinal tract [17]. Conservative treatment (gastric lavage, endoscopic disruption, etc.) and conventional surgery as well as laparoscopic surgery are the therapeutic options for phytobezoar [5]. However, phytobezoars are often resistant to conservative treatment. Gastric lavage has been reported for the treatment of phytobezoars using NaHCO3, which has a mucolytic effect, and penetration of CO2 bubbles into the surface of bezoars could also allow digestion [19, 20]. Interestingly, successful nasogastric Coca-Cola lavage for gastric phytobezoar has been reported [9, 19, 20, 21, 22]. We have tried Coca-Cola lavage in vitro with exenterated specimens, but no dissolution was identified.
In conventional surgery, bezoar removal is commonly achieved by gastrotomy and/or enterotomy. If complicated with small bowel obstruction, gastric perforation, or gastric hemorrhage, patients can be treated by gastric and/or intestinal resection [6]. Our patient showed a huge phytobezoar in the jejunum that was safely extracted by enterotomy. Moreover, a laparoscopic approach may be the treatment of choice when surgery is indicated. In our case, open laparotomy was selected due to the past history of surgery. When suitable expertise is available, laparoscopy is safe and effective in the management of bezoar-induced small bowel obstruction and offers superior postoperative outcomes to the conventional open approach.
In conclusion, phytobezoar due to persimmon is rare. Plain abdominal CT is helpful in the diagnosis of phytobezoar. Treatment can be either conservative or surgical, but surgical treatment is reliable and more rapid than conservative treatment.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- 1.Erzurumlu K, Malazgirt Z, Bektas A, Dervisoglu A, Polat C, Senyurek G, et al. Gastrointestinal bezoars: a retrospective analysis of 34 cases. World J Gastroenterol. 2005 Mar;11((12)):1813–1817. doi: 10.3748/wjg.v11.i12.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ezzat RF, Rashid SA, Rashid AT, Abdullah KM, Ahmed SM. Small intestinal obstruction due to phytobezoar: a case report. J Med Case Reports. 2009 Dec;3((1)):9312. doi: 10.1186/1752-1947-3-9312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yakan S, Sirinocak A, Telciler KE, Tekeli MT, Deneçli AG. A rare cause of acute abdomen: small bowel obstruction due to phytobezoar. Ulus Travma Acil Cerrahi Derg. 2010 Sep;16((5)):459–463. [PubMed] [Google Scholar]
- 4.de Toledo AP, Rodrigues FH, Rodrigues MR, Sato DT, Nonose R, Nascimento EF, et al. Diospyrobezoar as a cause of small bowel obstruction. Case Rep Gastroenterol. 2012 Sep;6((3)):596–603. doi: 10.1159/000343161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gayà J, Barranco L, Llompart A, Reyes J, Obrador A. Persimmon bezoars: a successful combined therapy. Gastrointest Endosc. 2002 Apr;55((4)):581–583. doi: 10.1067/mge.2002.122332. [DOI] [PubMed] [Google Scholar]
- 6.Zhang RL, Yang ZL, Fan BG. Huge gastric disopyrobezoar: a case report and review of literatures. World J Gastroenterol. 2008 Jan;14((1)):152–154. doi: 10.3748/wjg.14.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuo JY, Mo LR, Tsai CC, Yueh SK, Lin RC, Hwang MH. Endoscopic fragmentation of gastric phytobezoar by electrohydraulic lithotripsy. Gastrointest Endosc. 1993 Sep-Oct;39((5)):706–708. doi: 10.1016/s0016-5107(93)70229-1. [DOI] [PubMed] [Google Scholar]
- 8.Roy M, Fendrich I, Li J, Szomstein S, Rosenthal RJ. Treatment option in patient presenting with small bowel obstruction from phytobezoar at the jejunojejunal anastomosis after Roux-en-Y gastric bypass. Surg Laparosc Endosc Percutan Tech. 2012 Aug;22((4)):e243–e245. doi: 10.1097/SLE.0b013e31825d6c07. [DOI] [PubMed] [Google Scholar]
- 9.Ladas SD, Kamberoglou D, Karamanolis G, Vlachogiannakos J, Zouboulis-Vafiadis I. Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatment. Aliment Pharmacol Ther. 2013 Jan;37((2)):169–173. doi: 10.1111/apt.12141. [DOI] [PubMed] [Google Scholar]
- 10.Santos Valenciano J, Nonose R, Bragattini Cruz R, Tiemi Sato D, Monteiro Fernandes F, Fabrício Nascimento E, et al. Tricholithobezoar causing gastric perforation. Case Rep Gastroenterol. 2012 Jan;6((1)):26–32. doi: 10.1159/000336203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gorgone S, Di Pietro N, Rizzo AG, Melita G, Calabrò G, Sanò M, et al. [Mechanical intestinal occlusion due to phytobezoars]. G Chir. 2003 Jun-Jul;24((6-7)):239–242. [PubMed] [Google Scholar]
- 12.Kement M, Ozlem N, Colak E, Kesmer S, Gezen C, Vural S. Synergistic effect of multiple predisposing risk factors on the development of bezoars. World J Gastroenterol. 2012 Mar;18((9)):960–964. doi: 10.3748/wjg.v18.i9.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krausz MM, Moriel EZ, Ayalon A, Pode D, Durst AL. Surgical aspects of gastrointestinal persimmon phytobezoar treatment. Am J Surg. 1986 Nov;152((5)):526–530. doi: 10.1016/0002-9610(86)90221-7. [DOI] [PubMed] [Google Scholar]
- 14.Saeed ZA, Rabassa AA, Anand BS. An endoscopic method for removal of duodenal phytobezoars. Gastrointest Endosc. 1995 Jan;41((1)):74–76. doi: 10.1016/s0016-5107(95)70282-2. [DOI] [PubMed] [Google Scholar]
- 15.Ahn YH, Maturu P, Steinheber FU, Goldman JM. Association of diabetes mellitus with gastric bezoar formation. Arch Intern Med. 1987 Mar;147((3)):527–528. [PubMed] [Google Scholar]
- 16.Toccaceli S, Donfrancesco A, Stella LP, Diana M, Dandolo R, Di Schino C. [Shall bowel obstruction caused by phytobezoar. Case report]. G Chir. 2005 May;26((5)):218–220. [PubMed] [Google Scholar]
- 17.Kim JH, Ha HK, Sohn MJ, Kim AY, Kim TK, Kim PN, et al. CT findings of phytobezoar associated with small bowel obstruction. Eur Radiol. 2003 Feb;13((2)):299–304. doi: 10.1007/s00330-002-1432-0. [DOI] [PubMed] [Google Scholar]
- 18.Ripollés T, García-Aguayo J, Martínez MJ, Gil P. Gastrointestinal bezoars: sonographic and CT characteristics. AJR Am J Roentgenol. 2001 Jul;177((1)):65–69. doi: 10.2214/ajr.177.1.1770065. [DOI] [PubMed] [Google Scholar]
- 19.Ha SS, Lee HS, Jung MK, Jeon SW, Cho CM, Kim SK, et al. Acute intestinal obstruction caused by a persimmon phytobezoar after dissolution therapy with Coca-Cola. Korean J Intern Med (Korean Assoc Intern Med). 2007 Dec;22((4)):300–303. doi: 10.3904/kjim.2007.22.4.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hayashi K, Ohara H, Naitoh I, Okumura F, Andoh T, Itoh T, et al. Persimmon bezoar successfully treated by oral intake of Coca-Cola: a case report. Cases J. 2008 Dec;1((1)):385. doi: 10.1186/1757-1626-1-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kato H, Nakamura M, Orito E, Ueda R, Mizokami M. The first report of successful nasogastric Coca-Cola lavage treatment for bitter persimmon phytobezoars in Japan. Am J Gastroenterol. 2003 Jul;98((7)):1662–1663. doi: 10.1111/j.1572-0241.2003.07563.x. [DOI] [PubMed] [Google Scholar]
- 22.Chung YW, Han DS, Park YK, Son BK, Paik CH, Jeon YC, et al. Huge gastric diospyrobezoars successfully treated by oral intake and endoscopic injection of Coca-Cola. Dig Liver Dis. 2006 Jul;38((7)):515–517. doi: 10.1016/j.dld.2005.10.024. [DOI] [PubMed] [Google Scholar]


