Abstract
Background
In patients with heart failure with preserved ejection fraction (HFpEF), worse kidney function is associated with worse overall cardiac mechanics. Right ventricular stroke work index (RVSWI) is a parameter of right ventricular function. The aim of our study was to determine the relationship between RVSWI and glomerular filtration rate (GFR) in patients with HFpEF.
Method
This was a single-center cross-sectional study. HFpEF is defined as patients with documented heart failure with ejection fraction > 50% and pulmonary wedge pressure > 15 mm Hg from right heart catheterization. RVSWI (normal value 8–12 g/m/beat/m2) was calculated using the formula: RVSWI = 0.0136 × stroke volume index × (mean pulmonary artery pressure – mean right atrial pressure). Univariate and multivariate linear regression analysis was performed to study the correlation between RVSWI and GFR.
Result
Ninety-one patients were included in the study. The patients were predominantly female (n = 64, 70%) and African American (n = 61, 67%). Mean age was 66 ± 12 years. Mean GFR was 59 ± 35 mL/min/1.73 m2. Mean RVSWI was 11 ± 6 g/m/beat/m2. Linear regression analysis showed that there was a significant independent inverse relationship between RVSWI and GFR (unstandardized coefficient = −1.3, p = 0.029). In the subgroup with combined post and precapillary pulmonary hypertension (Cpc-PH) the association remained significant (unstandardized coefficient = −1.74, 95% CI −3.37 to −0.11, p = 0.04).
Conclusion
High right ventricular workload indicated by high RVSWI is associated with worse renal function in patients with Cpc-PH. Further prospective studies are needed to better understand this association.
Keywords: Right ventricular stroke work index, Glomerular filtration rate, Heart failure with preserved ejection fraction
Introduction
In patients with chronic heart failure with reduced ejection fraction (HFrEF), those who had right ventricular dysfunction measured by tricuspid annular plane systolic excursion were more likely to have chronic kidney disease [1]. A cross-sectional study showed that patients with heart failure with preserved ejection fraction (HFpEF) who had worse right ventricular free wall strain by echocardiography had worse glomerular filtration rate (GFR) [2]. However, there is a lack of evidence on the direct relationship between invasive parameters of right ventricular function and kidney function in HFpEF patients.
Right ventricular stroke work index (RVSWI) is an invasive parameter of right ventricular function obtained by right heart catheterization. It is calculated using both pressures and flow through the right ventricle. It is mainly used to determine the need for right-sided assist devices in patients who need left ventricular assist devices [3, 4]. Higher right ventricular workload demonstrated by high RVSWI is associated with worse outcome after lung transplantation. This may be due to the effect of higher mean pulmonary artery pressure [5]. On the contrary, lower RVSWI is associated with worse outcome after heart transplants [6].
The relationship between RVSWI and kidney function in patients with HFpEF patients is not established. This study was conducted to determine the relationship between RVSWI and GFR in patients with HFpEF.
Method
Patients were included through a retrospective chart review of patients who were admitted to our center with a diagnosis of diastolic heart failure or HFpEF between January 2010 and September 2016. HFpEF was defined as documented diagnosis of heart failure, ejection fraction > 50%, and pulmonary capillary wedge pressure > 15 mm Hg from right heart catheterization. Patients with combined post- and precapillary pulmonary hypertension (Cpc-PH) were defined as HFpEF patients with diastolic pressure gradient (DPG) > 7 mm Hg or pulmonary vascular resistance (PVR) > 3 Wood units [7, 8]. Patients with end-stage renal disease, moderate or severe valvular heart disease, prosthetic valves, organ transplants, and significant pericardial effusion were excluded from the study. Data on demographics, comorbidities, echocardiography parameters, right heart catheterization parameters, and kidney functions were obtained through medical record review.
Patients with comorbidities including diabetes mellitus, hypertension, and dyslipidemia were defined as patients with those comorbidities documented in their medical records. Patients with coronary artery disease were defined as those who had documented coronary artery disease on left heart catheterization. Current smokers were defined as those with documented smoking at the time of admission or those who had quit less than 1 year before admission.
RVSWI was calculated by the formula: 0.0136 × stroke volume index × (mean pulmonary artery pres sure – right atrial pressure). Stroke volume index was calculated as cardiac index by the Fick method divided by heart rate. Glomerular filtration rate (GFR) was calculated by the Modification of Diet in Renal Disease (MDRD) study equation.
Statistical Analysis
Baseline characteristics and comorbidities are demonstrated as mean ± SD for continuous variables, and numbers with percentages for categorical variables. Right heart catheterization parameters, and kidney function parameters are described as mean ± SD. Association between RVSWI and kidney function was determined by linear regression analysis. Statistical significance was defined as a p value less than 0.05. Multivariable linear regression analysis was performed to adjust for potential confounders including age, sex, ethnicity, smoking status, and comorbidities. Subgroup analyses were also performed in patients with Cpc-PH using DPG and PVR, to examine the influence of fixed pulmonary hypertension on this association. All statistical analyses were performed using SPSS statistics version 22.
Results
A total of 234 patients admitted to our center with diastolic heart failure or HFpEF who underwent right heart catheterization during the study period met our criteria. There were 112 patients with moderate or severe valvular heart disease, 9 with end-stage renal disease, 11 with prosthetic valves, 4 with significant pericardial effusion, and 7 with organ transplant.
After exclusion, a total of 91 patients were included in this study. Baseline characteristics are shown in Table 1. Thirty percent of the patients (n = 27) were male, and 67% (n = 61) were African American. Sixty-nine percent (n = 63) had diabetes mellitus, 78% (n = 86) had hypertension, 47% (n = 43) had dyslipidemia, and 46% (n = 42) had coronary artery disease. A majority of patients were on β-blockers (74%), statins (76%), and loop diuretics (79%). A significant number of patients were on ACE inhibitors or angiotensin receptor blockers (46%). The participants' medications are listed in Table 2.
Table 1.
Patients' baseline characteristics and right heart catheterization parameters
| Variables | ||
| Age, years | 66±12 | |
| BMI | 39±9 | |
| Male | 30 (27) | |
| Current smoker | 24 (22) | |
| African American | 67 (61) | |
| Dyslipidemia | 47 (43) | |
| Hypertension | 78 (86) | |
| Diabetes mellitus | 69 (63) | |
| History of coronary artery disease | 46 (42) | |
| History of stroke | 14 (13) | |
| Creatinine, mg/dL | 1.6±1 | |
| Glomerular filtration rate, mL/min/1.73 m2 | 59±35 | |
| Right heart catheterization parameters | ||
| Mean right atrial pressure, mm Hg | 16±5.8 | |
| Pulmonary artery systolic pressure, mm Hg | 59±14 | |
| Pulmonary artery diastolic pressure, mm Hg | 27±8 | |
| Mean pulmonary artery pressure, mm Hg | 39±11 | |
| Pulmonary capillary wedge pressure, mm Hg | 25±6.6 | |
| Fick cardiac output, L/min | 5.9±2 | |
| Fick cardiac index, L/min/m2 | 2.8±1 | |
| Pulmonary vascular resistance, Woods units | 1.76±0.85 | |
| Diastolic pulmonary gradient, mm Hg | 2.9±7.1 | |
| Right ventricular stroke work index, g/m2/beat | 11.4±6.2 | |
Values are mean ± SD or % (n), as appropriate. BMI, body mass index.
Table 2.
Common medication prescribed for our participants
| Medication | n (%) |
|---|---|
| Aspirin | 73 (80) |
| ACEI or ARB | 42 (46) |
| β-Blocker | 67 (74) |
| Loop diuretics | 72 (79) |
| Statin | 69 (76) |
ACEI, ACE inhibitor; ARB, aldosterone receptor blocker.
Right heart catheterization parameters are shown in Table 1. Mean Fick cardiac output was 5.9 ± 2 L/min. Mean cardiac index was 2.8 ± 1 L/min/m2. Average mean pulmonary artery pressure was 39 ± 11 mm Hg. Mean RVSWI was 11.4 ± 6.2 g/m/beat/m2. Mean pulmonary vascular resistance was 1.76 ± 0.85 Wood units. Mean MDRD GFR was 59 ± 35 mL/min/1.73 m2.
Linear regression analysis found that there was an inverse relationship between RVSWI and GFR (Fig. 1; unstandardized coefficient = −1.48, p = 0.01). Multivariable linear regression was performed to adjust for age, sex, smoking status, and comorbidities including diabetes mellitus, hyperlipidemia, and hypertension. Multivariable linear regression (Table 3) showed that RVSWI was inversely related to GFR independent of those confounders (unstandardized coefficient = −1.3 p = 0.029).
Fig. 1.
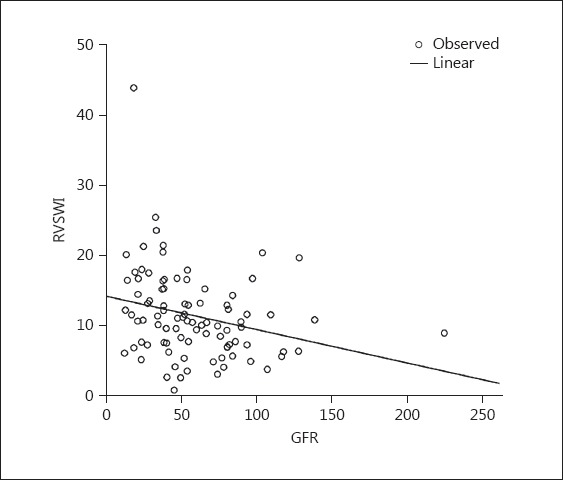
Scatterplot showing inverse relationship between right ventricular stroke work index (RVSWI; g/m2/beat) and glomerular filtration rate (GFR; mL/min/1.73 m2). Unstandardized coefficient = −1.48, p = 0.01.
Table 3.
Multivariate linear regression analysis of the association between RVSWI and glomerular filtration rate
| Variables | Unstandardized coefficient | 95% CI of coefficient | p value |
|---|---|---|---|
| RVSWI | −1.3 | −2.47 to–0.13 | 0.029 |
| Age | −0.23 | −0.85 to 0.39 | 0.45 |
| Sex | 8.68 | −7.37 to 24.74 | 0.29 |
| Race | −3.10 | −10.9 to 4.7 | 0.43 |
| Hypertension | −13.05 | −35.5 to 9.4 | 0.25 |
| Hyperlipidemia | 16.48 | 0.73 to 32.2 | 0.04 |
| Diabetes mellitus | −5.90 | −22.4 to 10.6 | 0.68 |
| Smoking | 9.6 | −8.03 to 27.28 | 0.28 |
RVSWI, right ventricular stroke work index.
Subgroup analyses (Table 4) were carried out to examine this association in patients with features of Cpc-PH. In patients with DPG > 7 mm Hg, there was an independent inverse association between RVSWI and GFR (unstandardized coefficient = −1.8, 95% CI −5 to −0.55, p = 0.046). The association was also significant in the subgroup with PVR > 3 Wood units (unstandardized coefficient = −1.8, 95% CI −3.50 to −0.06, p = 0.04) and the subgroup with either PVR > 3 Wood units or DPG > 7 mm Hg (unstandardized coefficient = −1.74, 95% CI −3.37 to −0.11, p = 0.04). However, there was no independent association observed in the subgroup with PVR ≤3 Wood units or DPG ≤7 mm Hg.
Table 4.
Univariate and multivariate linear regression analyses of subgroups
| Univariate analysis |
Multivariate analysis |
|||||
|---|---|---|---|---|---|---|
| unstandardized coefficient (95% CI) | β | p value | unstandardized-coefficient (95% CI) | β | p value | |
| All subjects (n = 91) | −1.48 (−2.60 to −3.45) | −0.27 | 0.01 | −1.3 (−2.50 to −0.13) | −0.23 | 0.03 |
| PVR >3 Wood units (n = 29) | −1.44 (−3.30 to 0.40) | −0.30 | 0.12 | −1.8 (−3.50 to −0.06) | −0.36 | 0.04 |
| DPG >7 mm Hg (n = 22) | −2.46 (−4.9 to −0.05) | −0.45 | 0.046 | −2.5 (−5 to −0.55) | −0.47 | 0.046 |
| PVR >3 Wood units or DPG >7 mm Hg (n = 32) | −1.51 (−3.33 to 0.31) | −0.30 | 0.1 | −1.74 (−3.37 to −0.11) | −0.34 | 0.04 |
| Diastolic dysfunction grade I and worse (n = 50) | −0.71 (−2.38 to 0.96) | −0.13 | 0.40 | −0.35 (−2.12 to −1.43) | −0.06 | 0.7 |
PVR, pulmonary vascular resistance; DPG, diastolic pulmonary gradient.
Discussion
This study found that RVSWI was inversely related to GFR, and the association remained significant after adjustment of confounders including age, sex, and comorbidities. This association is likely driven by the presence of fixed pulmonary hypertension causing increased right ventricular workload as evidenced by the subgroup analyses of patients with Cpc-PH showing a significant association, while there was no association in subgroups without precapillary hypertension.
RVSWI is an invasive parameter of right ventricular workload. The index takes into account both pressure across the right ventricle and right ventricle stroke volume in the calculation. High RVSWI indicates higher workload on the right ventricle. Higher RVSWI is associated with increased pulmonary artery stiffness in patients with pulmonary hypertension [9]. In patients who underwent lung transplant, higher RVSWI also predicted worse outcomes [5]. Our study is one of the very few studies that demonstrate a relationship between invasive right heart catheterization parameters in patients with HFpEF. This study is also one of the first studies to explore the relationship between RVSWI and kidney function in this population.
It is now well recognized that some patients with HFpEF develop structural remodeling of small pulmonary arteries over time, indicative of a precapillary component of pulmonary hypertension manifested by increased PVR and DPG; this entity is termed “combined post- and precapillary pulmonary hypertension” (Cpc-PH). These patients have reduced pulmonary artery capacitance and increased stiffness of the pulmonary arteries [7]. Elevated stiffness of the pulmonary arteries has been associated with increased right ventricular workload or a higher RVSWI [9]. In our study, patients with Cpc-PH and higher RVSWI had worse renal function, thus suggesting that remodeling of the pulmonary vasculature and its effect on right ventricular function are key players in worsening renal function in HFpEF patients. Patients with Cpc-PH have worse prognosis and develop overt right ventricular dysfunction over time. There are some studies showing that these patients may benefit from targeted therapy for pulmonary hypertension [7, 8]. Whether these therapies have a favorable impact on renal function will need to be evaluated in future studies.
A known mechanism of renal dysfunction in patients with HFpEF is related to right ventricular dysfunction [2], leading to elevated right atrial pressure, renal congestion, and decreased GFR. However, in our study, patients with elevated RV afterload but without overt right ventricular dysfunction had lower GFR, an association that has not been described previously. Larger studies should be carried out to confirm this association and to determine causality.
There are some limitations of this study, the first being that this is a cross-sectional study and causality cannot be established. Our study included patients with HFpEF who were admitted and had clinically indicated right heart catheterization; this population had worse than average baseline clinical status and worse GFR. Many patients also received diuretics prior to right heart catheterization, which could underestimate RVSWI. We were unable to perform right ventricular strain in this cohort and therefore our findings could not be correlated with less invasive parameters. However, a study has shown good correlation between RVSWI and right ventricular free wall strain [10]. This should be explored further in future studies.
Conclusion
Right ventricular workload is inversely associated with kidney function in patients with HFpEF. Larger prospective studies should be carried out to better clarify this mechanism of association.
Statement of Ethics
This study was approved by the institutional review board of the Einstein Medical Center. This investigation was in accordance with the Declaration of Helsinki.
Disclosure Statement
The authors report no relationships that could be construed as a conflict of interest.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Dini FL, Demmer RT, Simioniuc A, Morrone D, Donati F, Guarini G, et al. Right ventricular dysfunction is associated with chronic kidney disease and predicts survival in patients with chronic systolic heart failure. Eur J Heart Fail. 2012;14:287–294. doi: 10.1093/eurjhf/hfr176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Unger ED, Dubin RF, Deo R, Daruwalla V, Friedman JL, Medina C, et al. Association of chronic kidney disease with abnormal cardiac mechanics and adverse outcomes in patients with heart failure and preserved ejection fraction. Eur J Heart Fail. 2016;18:103–112. doi: 10.1002/ejhf.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ochiai Y, McCarthy PM, Smedira NG, Banbury MK, Navia JL, Feng J, et al. Predictors of severe right ventricular failure after implantable left ventricular assist device insertion: analysis of 245 patients. Circulation. 2002;106((12 suppl 1)):I198–I202. [PubMed] [Google Scholar]
- 4.Imamura T, Kinugawa K, Kinoshita O, Nawata K, Ono M. High pulmonary vascular resistance in addition to low right ventricular stroke work index effectively predicts biventricular assist device requirement. J Artif Organs. 2016;19((1)):44–53. doi: 10.1007/s10047-015-0867-4. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong HF, Schulze PC, Kato TS, Bacchetta M, Thirapatarapong W, Bartels MN. Right ventricular stroke work index as a negative predictor of mortality and initial hospital stay after lung transplantation. J Heart Lung Transplant. 2013;32:603–608. doi: 10.1016/j.healun.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kato TS, Stevens GR, Jiang J, Schulze PC, Gukasyan N, Lippel M, et al. Risk stratification of ambulatory patients with advanced heart failure undergoing evaluation for heart transplantation. J Heart Lung Transplant. 2013;32:333–340. doi: 10.1016/j.healun.2012.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenkranz S, Gibbs J, SR, Wachter R, De Marco T, Vonk-Noordegraaf A, Vachiéry J-L. Left ventricular heart failure and pulmonary hypertension. Eur Heart J. 2016;37:942–954. doi: 10.1093/eurheartj/ehv512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vachiéry J-L, Adir Y, Barberà JA, Champion H, Coghlan JG, Cottin V, et al. Pulmonary hypertension due to left heart diseases. J Am Coll Cardiol. 2013;62((suppl 25)):D100–D108. doi: 10.1016/j.jacc.2013.10.033. [DOI] [PubMed] [Google Scholar]
- 9.Stevens GR, Garcia-Alvarez A, Sahni S, Garcia MJ, Fuster V, Sanz J. RV dysfunction in pulmonary hypertension is independently related to pulmonary artery stiffness. JACC Cardiovasc Imaging. 2012;5:378–387. doi: 10.1016/j.jcmg.2011.11.020. [DOI] [PubMed] [Google Scholar]
- 10.Cameli M, Lisi M, Righini FM, Tsioulpas C, Bernazzali S, Maccherini M, et al. Right ventricular longitudinal strain correlates well with right ventricular stroke work index in patients with advanced heart failure referred for heart transplantation. J Card Fail. 2012;18:208–215. doi: 10.1016/j.cardfail.2011.12.002. [DOI] [PubMed] [Google Scholar]


