Abstract
Background
Brugada syndrome (BrS) is considered to be an inherited arrhythmic disease associated with fatal complications and premature sudden unexpected death. The prevalence of the Brugada electrocardiogram pattern (BrP) has been reported in several countries. Nonetheless, the specific worldwide prevalence of BrS has not been reported.
Objective
We estimated the worldwide prevalence of BrS and Type-2/3 BrP in general adult populations using a systematic review and meta-analysis of the existing literature.
Methods
We thoroughly searched MEDLINE and SCOPUS databases up to March 2017. Included studies were population-based electrocardiogram studies in which prevalence was presented or could be calculated from available data. Pooled prevalence by country/region and/or ethnicity was estimated using a random-effect model.
Results
Twenty-eight articles with atotal population of 369,068 were included in this study. The worldwide pooled prevalence of BrS was 0.5 per 1,000 [95% confidence interval (CI): 0.3-0.7]. The highest prevalence was reported in Southeast Asia (3.7 per 1,000, 95% CI: 0.7-6.7); the lowest was found in North Africa (0 per 1,000). BrS in Asians was nine times more common than in Caucasians and 36 times more common than in Hispanics. The worldwide pooled prevalence of Type-2/3 BrP was 6.1 per 1,000 (95% CI: 5.0-7.1). The highest prevalence was also reported in Southeast Asia (35.5 per 1,000, 95% CI: 17.1-53.9).
Conclusions
This study revealed a significant difference in the worldwide prevalence of BrS and Type-2/3 BrP. Brugada electrocardiogram patterns are highly prevalent in Southeast Asia.
Keywords: Brugada electrocardiogram pattern, Brugada syndrome, Prevalence
INTRODUCTION
Brugada syndrome (BrS), first reported in 1992, is an inherited arrhythmic disease associated with ventricular fibrillation (VF), premature sudden arrhythmic death syndrome, and aborted sudden cardiac death (SCD).1-4 It has an autosomal dominant inheritance with variable penetrance. The specific characteristics of BrS are marked ST-segment elevation in right precordial leads without evidence of ischemia, electrolyte imbalance, and other structural heart diseases.5,6 Over 100 mutations have been associated with BrS,7 of which loss-of-function mutations in SCN5A, characterized by inactivation of sodium channels, are the most common, reported in 20% of BrS cases.7,8
The Brugada electrocardiogram pattern (BrP) includes both the coved type (BrS) ST segment elevation ≥ 2 mm in right precordial leads, and the saddle back type (Type-2 BrP).9 The diagnostic criteria of BrS have recently been revised and only the spontaneous coved type is considered diagnostic of BrS.9 The clinical manifestation of BrS varies among patients and includes VF, sudden arrhythmic death syndrome, SCD, syncope, palpitations, nocturnal agonal respiration, and chest discomfort.10 The symptoms usually present during the fourth decade of life.11 However, most patients with BrS have a silent phenotype without malignant symptoms. Nevertheless, it is still considered to be a lethal disease because of its complications and premature sudden unexpected deaths.5
A recent meta-analysis reported the prevalence of the overall composite BrP of Type-1, Type-2, and Type-3 BrP, however a robust evaluation of the prevalence of BrS has not been reported.12 Another study reported the prevalence of BrS by combining data worldwide, however the prevalence was incorrectly estimated by simple summation of cases and subjects without weighting.5 In addition, several studies have been published since the last searches reported in these two studies. The Shanghai Scoring System used more specific criteria and required a score of 3.5 to definitively diagnose BrS. Therefore, we conducted this systematic review and meta-analysis to estimate the prevalence of BrS according to these new diagnostic criteriain the general adult population and in subgroups based on ethnicity, gender, fever, and region.9
METHODS
Eligibility criteria
Observational studies, including cohort and cross-sectional studies published in English were eligible if they met the following criteria: studied adults (age ≥ 18 years) who had electrocardiography (ECG), reported BrP prevalence, and in which the number of BrPs and total number of subjects were available. Authors were contacted when eligible studies had insufficient information reported.
Definitions
Brugada syndrome is characterized by a spontaneous coved-type ST-segment elevation ≥ 2 mm (0.2 mV) in ≥ 1 right precordial leads (V1-V3) positioned in the 4th, 3rd, or 2nd intercostal space according to the recent consensus conference of J wave syndrome in 2016. Finding only Type 1 BrP is the basis of the diagnosis of BrS. However, if Type-1 BrP is unmasked by either fever or drug challenge testing, patients need to also have a clinical history, family history, or genetic test results, as proposed in the Shanghai Scoring System, to achieve a score of 3.5 or greater for the definite diagnosis of BrS.9
Type-2 BrP is characterized by saddleback ST-segment elevation ≥ 0.5 mm in ≥ 1 right precordial lead (V1-V3), followed by a convex ST and a positive T wave in V2 and variable morphology V1.9 Type-3 BrP is characterized by either a saddleback or a coved pattern with an ST-segment elevation < 1 mm.9
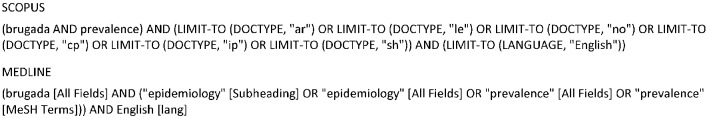
Search strategy
MEDLINE and SCOPUS electronic databases were searched up to March 31, 2017 using PubMed and SCOPUS search engines. A search strategy combining key words and related database-specific subject terms was used to identify relevant studies. The search strategies were constructed by combining search terms related to ECG characteristics (Brugada, right bundle branch block, ST elevation, precordial lead), study design (cohort, cross-sectional study), and statistical parameters (e.g. prevalence, incidence, frequency, proportion).
The titles of the retrieved articles were examined, and any studies that were obviously irrelevant were excluded. Abstracts and then full texts of the remaining articles were reviewed and screened for the inclusion criteria. Additional articles were identified by reviewing the reference lists of full articles to identify publications on the same topic.
Risk of bias assessment
The quality of the studies was independently assessed by two reviewers (PP & WS) using the Newcastle-Ottawa Scale for nonrandomized studies.13 The score was measured using a standardized star allocation system for the representativeness of the sample and outcome. The primary outcome of interest was the prevalence of BrS and Type-2/3 BrP, which was identified by the individual study authors.
Data extraction
A standardized data extraction form was used to extract information from each study. Information extracted included study design, setting, mean age, percentage of males, ethnicity, geographical region (e.g. East Asia, Southeast Asia, South Asia, Europe, North America, North Africa, etc.), type of BrP, number of cases, and the total number of subjects.
Decisions on study selection, data extraction, and risk of bias assessment were independently performed by two reviewers (PP & WS). Disagreements were resolved by discussion and consensus with athird party (WV or AT). Data cleaning and checking were performed separately for each study. Any unclear coding or outlier was clarified by contacting the study authors.
Analysis
Data on the characteristics of the studies and patients were reported using mean, median, or frequency where appropriate. BrS and Type-2/3 BrP were estimated for individual studies. These were then pooled across the studies separately by country/region of setting and/or ethnicity using meta-analysis for pooling prevalence. A random-effect model was applied if heterogeneity was present; otherwise a fixed-effect model was applied. The heterogeneity of BrP prevalence was assessed using the Q-statistic, and its degree of heterogeneity was quantified using the I2 statistic. Heterogeneity was considered to be present if the Q statistic p-value was < 0.1 or I2 > 25%.14 Forrest plots consisting of point and range estimations of prevalence for individual studies were constructed. All analyses were performed using STATA version 14.1 (StataCorp, College Station, Texas).
RESULTS
Description of the included studies
Our search strategy yielded 897 potentially relevant articles (227 articles from Scopus and 670 articles from MEDLINE) (Figure 1). After excluding 204 duplicate articles, 693 articles underwent title and abstract review. Six hundred twenty-eight articles were excluded at this stage as they were not cohort or cross-sectional studies (375 without reported prevalence of BrP, 108 case reports, 45 letters, 23 non-human studies, 8 non-English studies), leaving 69 articles for full-length article review. Thirty-four studies were excluded because they were not ECG screening studies (N = 28), had duplicate reports (N = 2), or had an unclear BrP definitions (N = 5). Thus, the remaining 28 studies (25 cross-sectional and 3 cohort studies) with 369,068 subjects were included in this meta-analysis. Quality assessment was performed using Newcastle-Ottawa scales (see Supplement Table 1).
Figure 1.
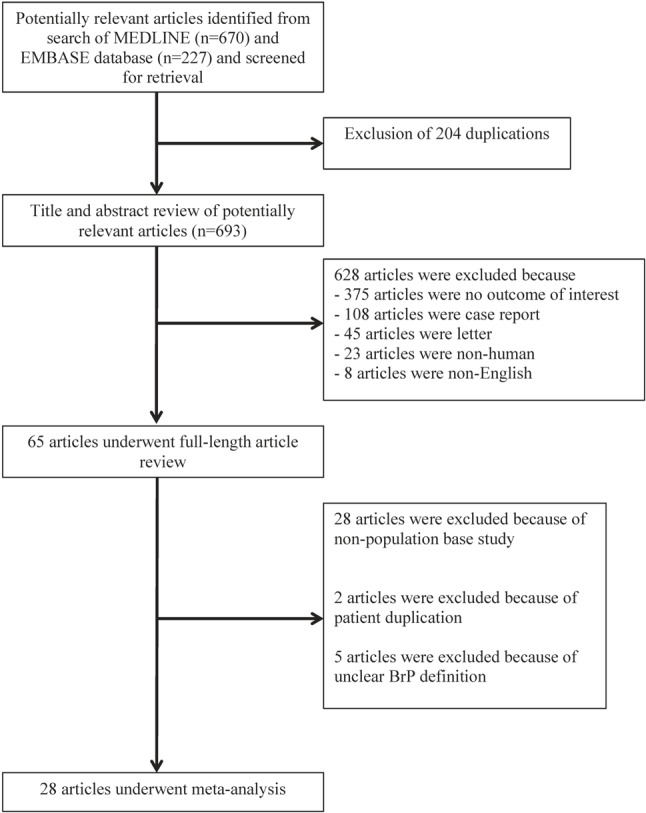
Flowchart showing the meta-analysis studies selection. BrP, Brugada electrocardiogram pattern.
Supplement Table 1. Newcastle-Ottawa quality assessment scale of included studies in the meta-analysis.
| Authors, year | Representativeness of the sample | Outcome | Total score | ||||||
| Truly representative of the average in the target population* (all subjects or random sampling) | Somewhat representative of the average in the target population* (non-random sampling) | Selected group of users | No description of the sampling strategy | Assessment of outcome | |||||
| Independent blind assessment# | Record linkage# | Self report* | No description | ||||||
| Adler, 2013 | 0 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 2 |
| Atarashi, 2001 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 2 |
| Bigi, 2007 | 1 | N/A | N/A | N/A | 1 | N/A | N/A | N/A | 2 |
| Bozkurt, 2006 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Chung. 2014 | 1 | N/A | N/A | N/A | 1 | N/A | N/A | N/A | 2 |
| Donohue, 2008 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Furahashi, 2001 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Gallagher, 2008 | 0 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 2 |
| Gervacio-Domingo, 2008 | 1 | N/A | N/A | N/A | 1 | N/A | N/A | N/A | 2 |
| Hermida, 2000 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Ito,2006 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Juang, 2011 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Juang, 2015 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Junttila, 2004 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Letsas, 2007 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Makarawate, 2015 | 0 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 2 |
| Miyasaka, 2001 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Monroe, 2000 | 0 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 2 |
| Ouali, 2011 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Patel, 2009 | 1 | N/A | N/A | N/A | 1 | N/A | N/A | N/A | 2 |
| Pecini, 2010 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Rattanawong, 2015 | 0 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 2 |
| Rattanawong, 2017 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Sakabe, 2003 | 1 | N/A | N/A | N/A | 1 | N/A | N/A | N/A | 2 |
| Schukro, 2010 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Shin SC, 2005 | 0 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 2 |
| Tsuji, 2008 | 1 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 3 |
| Wajed, 2008 | 0 | N/A | N/A | N/A | 2 | N/A | N/A | N/A | 2 |
Meta-analysis results
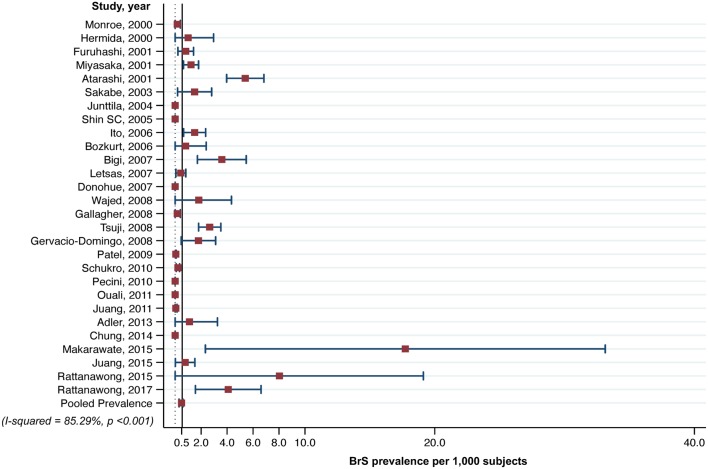
Prevalence of Brugada syndrome
The characteristics of the 28 included studies involving a total population of 369,068 subjects are shown in Table 1. All 28 studies provided the number of cases of BrS, spontaneous Type-1 BrP, at presentation and Type-2/3 BrP. Only two studies provided the numbers of Type-2/3 BrP that were diagnosed as BrS (7 patients). The number of cases and the total number of subjects are reported in Table 1. The prevalence of BrS was estimated from the 28 individual studies, and varied from 0 to 17.7 per 1,000 with high heterogeneity (Q = 224.1, I2 = 85.3%, p < 0.001). The random-effect model showed that the worldwide pooled prevalence was 0.5 per 1,000 [95% confidence interval (CI): 0.3-0.7 per 1,000] (Figure 2). The highest prevalence was reported by Makarawate et al. in Thailand (17.7 per 1,000, 95% CI: 7.6-40.8). The pooled prevalence of BrS in Thailand was 6.8 per 1,000 (95% CI: 0.5-13.2), which was 14 times higher than the worldwide prevalence.
Table 1. Summary and baseline characteristics of included studies in meta-analysis.
| Authors, year | Study | ECG screening population | Ethnicity | Region | n | Mean age | Male (%) | Brugada syndrome | Type-2 BrP | |||
| Age | (SD) | (n) | Male (%) | (n) | Male (%) | |||||||
| Adler, 2013 20 | Cross-sectional | Non-Febrile | White | Middle east | 909 | 61 | 19 | 49 | 1 | N/A | 4 | 100 |
| Atarashi, 2001 21 | Cross-Sectional | Healthy | Asian | East Asia | 10000 | 42 | 9 | 89.1 | 54 | N/A | 51 | N/A |
| Bigi, 2007 22 | Cross-Sectional | Palpitation group | White | Middle east | 3895 | 38.2 | 11.9 | 46 | 14 | 78.6 | 86 | 78.6 |
| Bozkurt, 2006 23 | Cross-sectional | Healthy | White | Middle east | 1238 | 38.9 | 17.6 | 54.2 | 1 | 100 | 5 | 100 |
| Chung, 2014 24 | Cross-Sectional | Healthy | White | North America | 672 | N/A | N/A | 51.3 | 0 | 0 | 76 | N/A |
| Donohue, 2008 25 | Cross-Sectional | Hospital | White | North America | 1348 | 52.7 | 16.2 | 53.6 | 0 | N/A | 2 | N/A |
| Furuhashi, 2001 26 | Cross-Sectional | Healthy | Asian | East Asia | 8612 | 49.2 | N/A | 69.52 | 7 | 100 | 10 | 100 |
| Gallagher, 2008 27 | Cross-Sectional | Healthy | White | Europe | 12012 | 29.88 | 8.99 | 90.8 | 2 | 100 | 29 | 100 |
| Gervacio-Domingo, 2008 28 | Cross-Sectional | Healthy | Asian | Southeast Asia | 3907 | N/A | N/A | N/A | 7 | 85.7 | 87 | 85.7 |
| Hermida, 2000 29 | Cross-Sectional | Healthy | White | Europe | 1000 | 39 | 10 | 63.2 | 1 | 100 | 60 | 100 |
| Ito, 2006 30 | Cross-Sectional | non-cardiac patient | Asian | Hawaii | 8006 | 54.1 | 55 | 100 | 12 | 100 | 11 | 100 |
| Juang, 2011 31 | Cross-Sectional | non-cardiac patient | Asian | East Asia | 20562 | 49 | 21 | 38.8 | 1 | 0 | 25 | 0 |
| Juang, 2015 32 | Cohort | Healthy | Asian | East Asia | 5214 | 69.3 | 8 | 48.5 | 4 | 75 | 169 | 75 |
| Junttila, 2004 33 | Cross-Sectional | Healthy | White | Europe | 3021 | 28.66 | NA | 91 | 0 | 0 | 18 | N/A |
| Letsas, 2007 34 | Cross-Sectional | Healthy | White | Europe | 11488 | 56.5 | NA | 57.8 | 5 | 92 | 20 | N/A |
| Makarawate, 2015 15 | Cross-Sectional | Healthy | Asian | Southeast Asia | 282 | 27.82 | 8.66 | 100 | 5 | N/A | 45 | 100 |
| Miyasaka, 2001 35 | Cross-sectional | Healthy | Asian | East Asia | 13929 | 58 | 10 | 26.5 | 17 | N/A | 81 | N/A |
| Monroe, 2000 36 | Cross-sectional | Hospital(pre-op patient) | White | North America | 12000 | N/A | N/A | N/A | 2 | N/A | 50 | N/A |
| Ouali, 2011 37 | Cross-Sectional | Athletes | White | North Africa | 540 | 18.3 | 2.4 | 64.4 | 0 | N/A | 9 | N/A |
| Patel, 2009 16 | Cross-sectional | Hospital (tertiary) | Hispanic | North America | 162590 | NA | NA | NA | 8 | N/A | 12 | N/A |
| Pecini, 2010 38 | Cross-sectional | Healthy | White | Europe | 18974 | 52 | 12 | 45 | 0 | N/A | 13 | N/A |
| Rattanawong, 2015 39 | Cross-sectional | Non-febrile (emergency room) | Asian | Southeast Asia | 249 | 51.2 | 18 | N/A | 2 | N/A | 7 | 100 |
| Rattanawong, 2017 3 | Cohort | Healthy | Asian | Southeast Asia | 2446 | 40.8 | 7 | 73 | 10 | 100 | 21 | 100 |
| Sakabe, 2003 40 | Cohort | Healthy | Asian | East Asia | 3339 | N/A | N/A | 79.25 | 16 | N/A | 53 | N/A |
| Schukro, 2010 41 | Cohort | General (military) | White | Europe | 47606 | 18 | N/A | N/A | 10 | 77 | N/A | N/A |
| Shin SC, 2005 42 | Cross-sectional | Healthy | Asian | East Asia | 225 | 44 | 13 | 100 | 0 | 0 | 3 | N/A |
| Tsuji, 2008 43 | Cross-sectional | Healthy | Asian | East Asia | 13904 | 58 | 10 | 26.51 | 37 | 84 | 61 | 83.8 |
| Wajed, 2008 44 | Cross-sectional | Hospital | Asian | South Asia | 1100 | 20.7 | 5.92 | 64.73 | 2 | 50 | 7 | 50 |
BrP, Brugada electrocardiogram pattern; ECG, electrocardiography; SD, standard deviation.
Figure 2.
Forest plot of pooled prevalence of Brugada syndrome in adult population according to 28 cross-sectional and cohort studies.
Subgroup analysis was then performed by ethnicity, including Asian (N = 14), Caucasian (N = 13), and Hispanic subjects (N = 1). The prevalence of BrS in the subjects with Asian ethnicity was 1.8 per 1,000 (95% CI: 1.0-2.6); compared to 0.2 per 1,000 (95% CI: 0.0-0.3) for Caucasian and 0.05 per 1,000 (95% CI: 0.0-0.1) for Hispanic subjects (Figure 3B). The heterogeneity of the prevalence among different ethnicities was high (I2 = 98.8%, p < 0.001). Brugada syndrome was nine times more common in Asians than in Caucasians, and 36 times more common in Asians than in Hispanics.
Figure 3.
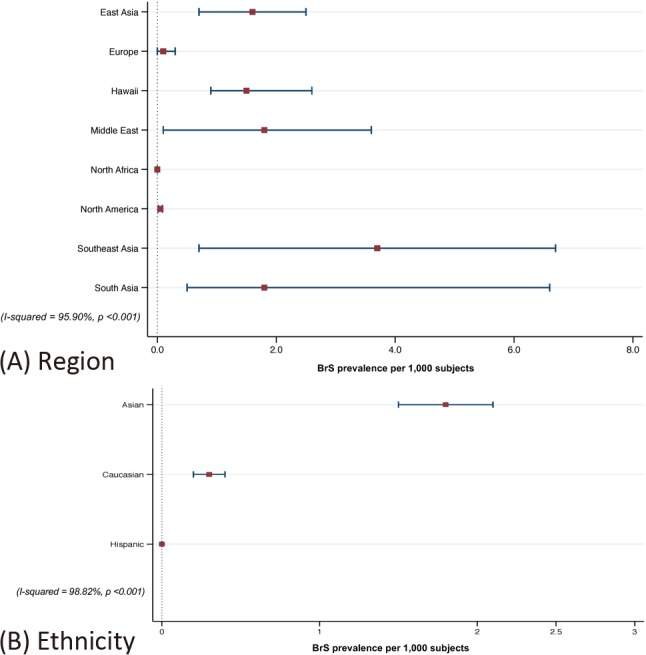
(A) Forest plot of pooled prevalence of Brugada syndrome by region and (B) Forest plot of pooled prevalence of Brugada syndrome by ethnicity.
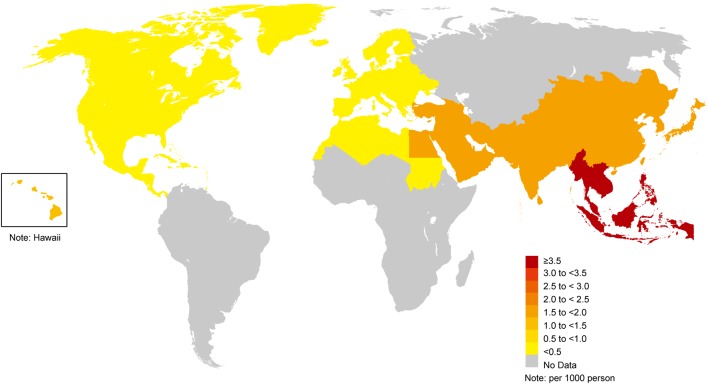
In addition, subgroup analysis by region of setting was also performed. There were 16, 6, 4, 1, and 1 studies conducted in Asia, Europe, North America, Hawaii, and North Africa, respectively. In Asia, there were 4, 8, 1, and 3 studies conducted in Southeast Asia, East Asia, South Asia, and the Middle East, respectively. The pooled BrS prevalence per 1,000 was highest in Southeast Asia (3.7 per 1,000, 95% CI: 0.7-6.7), followed by the Middle East (1.8 per 1,000, 95% CI: 0.1-3.6), South Asia (1.8 per 1,000, 95% CI: 0.5-6.6%), Hawaii (1.5 per 1,000, 95% CI: 0.9-2.6), East Asia (1.6 per 1,000, 95% CI: 0.7-2.5), Europe (0.1 per 1,000, 95% CI: 0.0-0.3), North America (0.05 per 1,000, 95% CI: 0.0-0.1), and North Africa (0 per 1,000) (Figure 3A). The heterogeneity of the prevalence among different regions was high (I2 = 95.9%, p < 0.001).
In Asia, the pooled prevalence of BrS was highest in Southeast Asia with a prevalence of 3.7 per 1,000 (95% CI: 0.7-6.7). The second highest most prevalent regions for BrS in Asia were the Middle East and South Asia with prevalence rates of 1.8 per 1,000 (95% CI: 0.1-3.6) and 1.8 per 1,000 (95% CI: 0.5-6.6), respectively, followed by East Asia (1.6 per 1,000, 95% CI: 0.7-2.5). A worldwide prevalence map of BrS by region is shown in Figure 6.
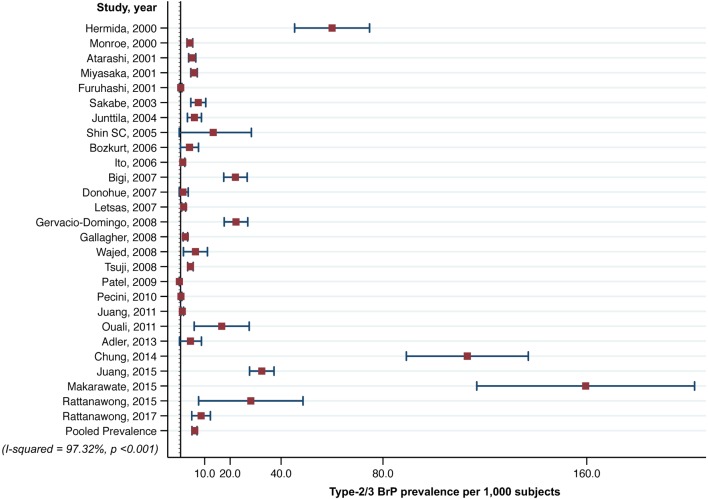
Prevalence of Type-2/3 Brugada ECG pattern
Of the 28 studies, 27 provided the prevalence of Type-2/3 BrP. The worldwide pooled prevalence of Type-2/3 BrP was 6.1 per 1,000 (95% CI: 5.0-7.1) (Figure 4). High heterogeneity was observed (I2 = 97.3%, p < 0.001). The highest prevalence of Type-2/3 BrP was reported in Thailand (60.1 per 1,000, 95% CI: 4.5-115.8), similar to the prevalence of BrS.15 The lowest prevalence was reported by Patel et al. in the United States (0.07 per 1,000, 95% CI: 0.0-0.1).16
Figure 4.
Forest plot of pooled prevalence of Type-2/3 Brugada electrocardiogram pattern (BrP) in adult population according to 27 cross-sectional and cohort studies.
We then analyzed the pooled prevalence of Type-2/3 BrP by ethnicity in Asian, Caucasian, and Hispanic populations. The prevalence of Type-2/3 BrP in Asian subjects was 8.3 per 1,000 (95% CI: 6.1-10.5), compared to 6.9 per 1,000 (95% CI: 4.7-9.2) in Caucasian, and 0.07 per 1,000 (95% CI: 0.0-0.1) in Hispanic subjects (Figure 5B). The heterogeneity of the prevalence among different ethnicities was high (I2 = 99.8%, p < 0.001).
Figure 5.
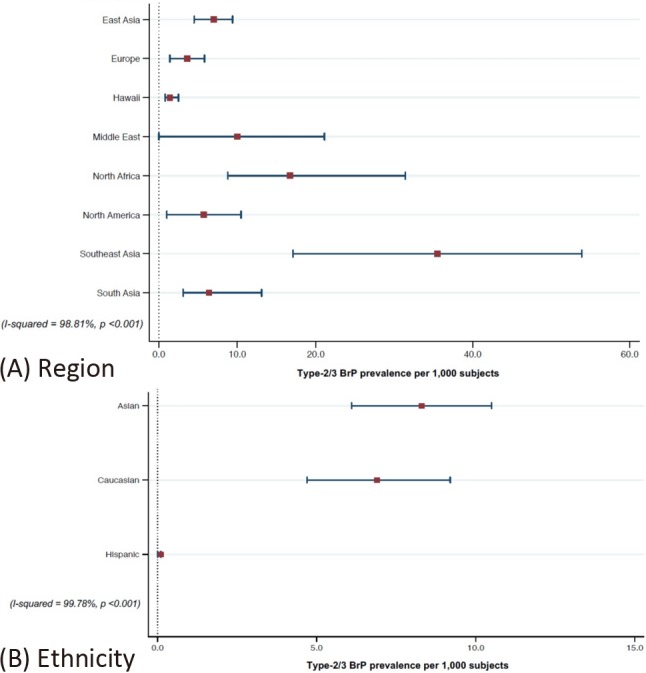
(A) Forest plot of pooled prevalence of Type-2/3 Brugada electrocardiogram pattern (BrP) by region and (B) Forest plot of pooled prevalence of Type-2/3 BrP by ethnicity.
Subgroup analysis of Type-2/3 BrP by geographical region was also performed. There were 16, 5, 4, 1, and 1 studies conducted in Asia, Europe, North America, Hawaii, and North Africa, respectively. In Asia, there were 4, 8, 1, and 3 studies conducted in Southeast Asia, East Asia, South Asia, and the Middle East, respectively. The pooled Type-2/3 BrP prevalence per 1000 was highest in Southeast Asia (35.5 per 1,000, 95% CI: 17.1-53.9) followed by North Africa (16.7 per 1,000, 95% CI: 8.8-31.4), the Middle East (10.0 per 1,000, 95% CI: 0.0-21.1), East Asia (7.0 per 1,000, 95% CI: 4.5-9.4), South Asia (6.4 per 1,000, 95% CI: 3.1-13.1), North America (5.7 per 1,000, 95% CI: 1.0-10.5), Europe (3.6 per 1,000, 95% CI: 1.4-5.8), and Hawaii (1.4 per 1,000, 95% CI: 0.8-2.5) (Figure 5A). Heterogeneity in the prevalence among different regions was high (I2 = 98.8%, p < 0.001).
Gender and prevalence of Brugada ECG pattern
On the 28 studies, 17 reported differences in the prevalence BrS and Type-2/3 BrP between genders. BrS was more common in males (0.6, 95% CI: 0.2-1.0) than in females (0.1, 95% CI: 0.0-0.2). Similar to BrS, Type-2/3 BrP was also more common in males (10.5, 95% CI: 7.5-13.5) than females (3.7, 95% CI: 2.1-5.3).
DISCUSSION
This study is the first systematic review and meta-analysis to assess the worldwide prevalence of BrS and Type-2/3 BrP among different regions, countries, and ethnicities. The worldwide prevalence of BrS was estimated at 0.5 per 1,000. BrS was highly prevalent in Southeast Asia as was Type-2/3 BrP. Thailand had the highest prevalence of BrS in the world with a prevalence of 6.8 per 1,000, which is approximately 14 times higher than the worldwide prevalence.
The coved type (BrS) ST segment elevation ≥ 2 mm in right precordial leads and saddle back type (Type-2/3 BrP) in the right precordial leads (V1-V3) are the main types of BrP.9 BrS is considered to be a cause of arrhythmia, syncope, VF, and SCD without structural heart disease. According to the recent consensus conference of J wave syndrome in 2016, finding only Type 1 BrP is the basis of the diagnosis of BrS. However, if the Type-1 BrP is unmasked by either fever or drug challenge test, the patients also need to have a clinical history, family history, or genetic test results, as proposed in the Shanghai Scoring System, to achieve a score of 3.5 score or greater for the definite diagnosis of BrS.9 Even though several studies have revealed distinctly larger right ventricular outflow tracts, changes in right ventricle volume and lower right ventricular ejection fraction in BrS from cardiovascular magnetic resonance imaging, there is currently no role for such imaging in diagnosing BrS.17,18 Furthermore, the proposed diagnostic scoring system for BrS, the Shanghai BrS score, includes ECG, clinical history, family history, and genetic test results, but not any kind of imaging.9
According to our results, the world prevalence map of BrS is shown in Figure 6. These results were obtained via meta-analysis which is the most accurate method to estimate pooled prevalence rates, unlike previous world prevalence maps which were estimated by simple summation and average.
Figure 6.
World prevalence map of Brugada syndrome.
Since Asia is large with diverse populations, the pooled prevalence analysis was conducted by difference regions of Asia, including Southeast Asia, East Asia, South Asia, and the Middle East. Similar to previous studies, we found that BrS was more common in Asian populations by approximately five times more than in Caucasian populations and 32 times more than in Hispanic populations, according to our pooled analyzed prevalence.
Our results revealed that gender, ethnicity, and geographic region affected the prevalence of BrS. The heterogeneity of the results may be secondary to gene distribution variance in different regions.19 We estimated that the prevalence of BrS in Thailand was over 146 times more common than in North America and 37 times more common than in Europe. BrS and Type-2/3 BrP were also more common in males than in females.
Limitations
Our inclusion criteria limited inaccurate methodology in prevalence studies by including only ECG screening studies to eliminate sampling bias. However, a limitation of this study is the heterogeneity in the overall and subgroup analyses. Heterogeneities in each analysis were high, likely due to differences in methodology, population, ethnicity, and geographic region. Moreover, we did not perform analysis of cardiovascular events among the subjects with BrP, due to inadequate information in the included studies. Our conclusion on the prevalence of BrS in North Africa may not reflect the true prevalence in this region. However, as only one study reported the prevalence in North Africa, this is the best conclusion we were able to make.
Lastly, all of our included studies were completed before the Shanghai Scoring System had been proposed. Most of the studies focused on only the Type-1 BrP ECG pattern and did not report any additional Type-2/3 BrP, family history or clinical history. Therefore, the prevalence of BrS in our study may underestimate the real prevalence, since some of the unmasked Type-1 BrP patients were excluded due to lack of adequate information that would fulfill the Shanghai Scoring System criteria for BrS.
CONCLUSIONS
This study is the first systematic review and meta-analysis to assess the worldwide prevalence of BrS among different regions, countries, and ethnicities. The worldwide prevalence of BrS was estimated at 0.5 per 1,000. BrS was highly prevalent in Southeast Asia along with Type 2/3 BrP. Thailand had the highest prevalence of BrS in the world, estimated at 15 times higher than the worldwide prevalence. Electrocardiogram screening in male subjects should be considered in Southeast Asia, especially Thailand.
ABBREVIATIONS
BrS, Brugada syndrome
BrP, Brugada electrocardiogram pattern
VF, ventricular fibrillation
SCD, sudden cardiac death
ECG, electrocardiogram
CI, confidence intervals
Acknowledgments
We would like to thank Dr. Dollawat Tantichariyangkul, MD for the figure illustrations.
We would like to thank Dr. Kenneth Nugent, MD for the critical reading.
Appendix
Supplement Data 1. Search term strategy.
CONFLICT OF INTEREST AND DISCLOSURE
Authors declare no conflict of interests for this article.
REFERENCES
- 1.Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391–1396. doi: 10.1016/0735-1097(92)90253-j. [DOI] [PubMed] [Google Scholar]
- 2.Probst V, Veltmann C, Eckardt L, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635–643. doi: 10.1161/CIRCULATIONAHA.109.887026. [DOI] [PubMed] [Google Scholar]
- 3.Rattanawong P, Ngarmukos T, Chung EH, et al. Prevalence of Brugada ECG pattern in Thailand from a population-based cohort study. J Am Coll Cardiol. 2017;69:1355–1356. doi: 10.1016/j.jacc.2016.12.028. [DOI] [PubMed] [Google Scholar]
- 4.Behr E, Wood DA, Wright M, et al. Cardiological assessment of first-degree relatives in sudden arrhythmic death syndrome. Lancet. 2003;362:1457–1459. doi: 10.1016/s0140-6736(03)14692-2. [DOI] [PubMed] [Google Scholar]
- 5.Postema PG. About Brugada syndrome and its prevalence. Europace. 2012;14:925–928. doi: 10.1093/europace/eus042. [DOI] [PubMed] [Google Scholar]
- 6.Priori SG, Blomstrom-Lundqvist C, Mazzanti A, et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015;36:2793–2867. doi: 10.1093/eurheartj/ehv316. [DOI] [PubMed] [Google Scholar]
- 7.Hedley PL, Jorgensen P, Schlamowitz S, et al. The genetic basis of Brugada syndrome: a mutation update. Hum Mutat. 2009;30:1256–1266. doi: 10.1002/humu.21066. [DOI] [PubMed] [Google Scholar]
- 8.Probst V, Wilde AA, Barc J, et al. SCN5A mutations and the role of genetic background in the pathophysiology of Brugada syndrome. Circ Cardiovasc Genet. 2009;2:552–557. doi: 10.1161/CIRCGENETICS.109.853374. [DOI] [PubMed] [Google Scholar]
- 9.Antzelevitch C, Yan GX, Ackerman MJ, et al. J-wave syndromes expert consensus conference report: emerging concepts and gaps in knowledge. Heart Rhythm. 2016;13:e295–e324. doi: 10.1016/j.hrthm.2016.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sakabe M, Fujiki A, Tani M, et al. Proportion and prognosis of healthy people with coved or saddle-back type ST segment elevation in the right precordial leads during 10 years follow-up. Eur Heart J. 2003;24:1488–1493. doi: 10.1016/s0195-668x(03)00323-3. [DOI] [PubMed] [Google Scholar]
- 11.Benito B, Brugada J, Brugada R, Brugada P. Brugada syndrome. Rev Esp Cardiol. 2009;62:1297–1315. doi: 10.1016/s1885-5857(09)73357-2. [DOI] [PubMed] [Google Scholar]
- 12.Quan XQ, Li S, Liu R, et al. A meta-analytic review of prevalence for Brugada ECG patterns and the risk for death. Medicine (Baltimore) 2016;95:e5643. doi: 10.1097/MD.0000000000005643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wells Ga SB oCD, Peterson J, Welch V, Tugwell P. The Newcastle-ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp] [Google Scholar]
- 14.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Makarawate P, Chaosuwannakit N, Ruamcharoen Y, et al. Prevalence and associated factors of early repolarization pattern in healthy young northeastern Thai men: a correlation study with Brugada electrocardiography. J Arrhythm. 2015;31:215–220. doi: 10.1016/j.joa.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel SS, Anees S, Ferrick KJ. Prevalence of a Brugada pattern electrocardiogram in an urban population in the United States. Pacing Clin Electrophysiol. 2009;32:704–708. doi: 10.1111/j.1540-8159.2009.02354.x. [DOI] [PubMed] [Google Scholar]
- 17.Rudic B, Schimpf R, Veltmann C, et al. Brugada syndrome: clinical presentation and genotype-correlation with magnetic resonance imaging parameters. Europace. 2016;18:1411–1419. doi: 10.1093/europace/euv300. [DOI] [PubMed] [Google Scholar]
- 18.Veltmann C, Papavassiliu T, Konrad T, et al. Insights into the location of type I ECG in patients with Brugada syndrome: correlation of ECG and cardiovascular magnetic resonance imaging. Heart Rhythm. 2012;9:414–421. doi: 10.1016/j.hrthm.2011.10.032. [DOI] [PubMed] [Google Scholar]
- 19.Juang JJ, Horie M. Genetics of Brugada syndrome. J Arrhythm. 2016;32:418–425. doi: 10.1016/j.joa.2016.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adler A, Topaz G, Heller K, et al. Fever-induced Brugada pattern: how common is it and what does it mean? Heart Rhythm. 2013;10:1375–1382. doi: 10.1016/j.hrthm.2013.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Atarashi H, Ogawa S, Harumi K, et al. Three-year follow-up of patients with right bundle branch block and ST segment elevation in the right precordial leads: Japanese Registry of Brugada Syndrome. Idiopathic Ventricular Fibrillation Investigators. J Am Coll Cardiol. 2001;37:1916–1920. doi: 10.1016/s0735-1097(01)01239-6. [DOI] [PubMed] [Google Scholar]
- 22.Bigi MA, Aslani A, Shahrzad S. Prevalence of Brugada sign in patients presenting with palpitation in southern Iran. Europace. 2007;9:252–255. doi: 10.1093/europace/eum023. [DOI] [PubMed] [Google Scholar]
- 23.Bozkurt A, Yas D, Seydaoglu G, et al. Frequency of Brugada-type ECG pattern (Brugada sign) in Southern Turkey. Int Heart J. 2006;47:541–547. doi: 10.1536/ihj.47.541. [DOI] [PubMed] [Google Scholar]
- 24.Chung EH, McNeely DE, 3rd, Gehi AK, et al. Brugada-type patterns are easily observed in high precordial lead ECGs in collegiate athletes. J Electrocardiol. 2014;47:1–6. doi: 10.1016/j.jelectrocard.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 25.Donohue D, Tehrani F, Jamehdor R, et al. The prevalence of Brugada ECG in adult patients in a large university hospital in the western United States. Am Heart Hosp J. 2008;6:48–50. doi: 10.1111/j.1751-7168.2008.06418.x. [DOI] [PubMed] [Google Scholar]
- 26.Furuhashi M, Uno K, Tsuchihashi K, et al. Prevalence of asymptomatic ST segment elevation in right precordial leads with right bundle branch block (Brugada-type ST shift) among the general Japanese population. Heart. 2001;86:161–166. doi: 10.1136/heart.86.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gallagher MM, Forleo GB, Behr ER, et al. Prevalence and significance of Brugada-type ECG in 12,012 apparently healthy European subjects. Int J Cardiol. 2008;130:44–48. doi: 10.1016/j.ijcard.2007.07.159. [DOI] [PubMed] [Google Scholar]
- 28.Gervacio-Domingo G, Isidro J, Tirona J, et al. The Brugada type 1 electrocardiographic pattern is common among Filipinos. J Clin Epidemiol. 2008;61:1067–1072. doi: 10.1016/j.jclinepi.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 29.Hermida JS, Lemoine JL, Aoun FB, et al. Prevalence of the Brugada syndrome in an apparently healthy population. Am J Cardiol. 2000;86:91–94. doi: 10.1016/s0002-9149(00)00835-3. [DOI] [PubMed] [Google Scholar]
- 30.Ito H, Yano K, Chen R, et al. The prevalence and prognosis of a Brugada-type electrocardiogram in a population of middle-aged Japanese-American men with follow-up of three decades. Am J Med Sci. 2006;331:25–29. doi: 10.1097/00000441-200601000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Juang JM, Phan WL, Chen PC, et al. Brugada-type electrocardiogram in the Taiwanese population--is it a risk factor for sudden death? J Formos Med Assoc. 2011;110:230–238. doi: 10.1016/S0929-6646(11)60035-1. [DOI] [PubMed] [Google Scholar]
- 32.Juang JM, Chen CY, Chen YH, et al. Prevalence and prognosis of Brugada electrocardiogram patterns in an elderly Han Chinese population: a nation-wide community-based study (HALST cohort). Europace. 2015;17 Suppl 2:ii54–ii62. doi: 10.1093/europace/euv141. [DOI] [PubMed] [Google Scholar]
- 33.Junttila MJ, Raatikainen MJ, Karjalainen J, et al. Prevalence and prognosis of subjects with Brugada-type ECG pattern in a young and middle-aged Finnish population. Eur Heart J. 2004;25:874–878. doi: 10.1016/j.ehj.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 34.Letsas KP, Gavrielatos G, Efremidis M, et al. Prevalence of Brugada sign in a Greek tertiary hospital population. Europace. 2007;9:1077–1080. doi: 10.1093/europace/eum221. [DOI] [PubMed] [Google Scholar]
- 35.Miyasaka Y, Tsuji H, Yamada K, et al. Prevalence and mortality of the Brugada-type electrocardiogram in one city in Japan. J Am Coll Cardiol. 2001;38:771–774. doi: 10.1016/s0735-1097(01)01419-x. [DOI] [PubMed] [Google Scholar]
- 36.Monroe MH, Littmann L. Two-year case collection of the Brugada syndrome electrocardiogram pattern at a large teaching hospital. Clin Cardiol. 2000;23:849–851. doi: 10.1002/clc.4960231112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ouali S, Ben Salem H, Hammas S, et al. Prevalence of Brugada-type ECG pattern and early ventricular repolarization pattern in Tunisian athletes. Open Access J Sports Med. 2011;2:33–40. doi: 10.2147/OAJSM.S19029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pecini R, Cedergreen P, Theilade S, et al. The prevalence and relevance of the Brugada-type electrocardiogram in the Danish general population: data from the Copenhagen City Heart Study. Europace. 2010;12:982–986. doi: 10.1093/europace/euq077. [DOI] [PubMed] [Google Scholar]
- 39.Rattanawong P, Vutthikraivit W, Charoensri A, et al. Fever-induced Brugada syndrome is more common than previously suspected: a cross-sectional study from an endemic area. Ann Noninvasive Electrocardiol. 2016;21:136–141. doi: 10.1111/anec.12288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sakabe M, Fujiki A, Tani M, et al. Proportion and prognosis of healthy people with coved or saddle-back type ST segment elevation in the right precordial leads during 10 years follow-up. Eur Heart J. 2003;24:1488–1493. doi: 10.1016/s0195-668x(03)00323-3. [DOI] [PubMed] [Google Scholar]
- 41.Schukro C, Berger T, Stix G, et al. Regional prevalence and clinical benefit of implantable cardioverter defibrillators in Brugada syndrome. Int J Cardiol. 2010;144:191–194. doi: 10.1016/j.ijcard.2009.03.136. [DOI] [PubMed] [Google Scholar]
- 42.Shin SC, Ryu HM, Lee JH, et al. Prevalence of the Brugada-type ECG recorded from higher intercostal spaces in healthy Korean males. Circ J. 2005;69:1064–1067. doi: 10.1253/circj.69.1064. [DOI] [PubMed] [Google Scholar]
- 43.Tsuji H, Sato T, Morisaki K, et al. Prognosis of subjects with Brugada-type electrocardiogram in a population of middle-aged Japanese diagnosed during a health examination. Am J Cardiol. 2008;102:584–587. doi: 10.1016/j.amjcard.2008.04.066. [DOI] [PubMed] [Google Scholar]
- 44.Wajed A, Aslam Z, Abbas SF, et al. Frequency of Brugada-type ECG pattern (Brugada sign) in an apparently healthy young population. J Ayub Med Coll Abbottabad. 2008;20:121–124. [PubMed] [Google Scholar]