Summary
Background
The End TB Strategy and the Sustainable Development Goals (SDGs) are intimately linked by their common targets and approaches. SDG 1 aims to end extreme poverty and expand social protection coverage by 2030. Achievement of SDG 1 is likely to affect the tuberculosis epidemic through a range of pathways. We estimate the reduction in global tuberculosis incidence that could be obtained by reaching SDG 1.
Methods
We developed a conceptual framework linking key indicators of SDG 1 progress to tuberculosis incidence via well described risk factor pathways and populated it with data from the SDG data repository and the WHO tuberculosis database for 192 countries. Correlations and mediation analyses informed the strength of the association between the SDG 1 subtargets and tuberculosis incidence, resulting in a simplified framework for modelling. The simplified framework linked key indicators for SDG 1 directly to tuberculosis incidence. We applied an exponential decay model based on linear associations between SDG 1 indicators and tuberculosis incidence to estimate tuberculosis incidence in 2035.
Findings
Ending extreme poverty resulted in a reduction in global incidence of tuberculosis of 33·4% (95% credible interval 15·5–44·5) by 2035 and expanding social protection coverage resulted in a reduction in incidence of 76·1% (45·2–89·9) by 2035; both pathways together resulted in a reduction in incidence of 84·3% (54·7–94·9).
Interpretation
Full achievement of SDG 1 could have a substantial effect on the global burden of tuberculosis. Cross-sectoral approaches that promote poverty reduction and social protection expansion will be crucial complements to health interventions, accelerating progress towards the End TB targets.
Funding
World Health Organization.
Introduction
The Sustainable Development Goals (SDGs) came into being in 2016 as a more detailed and globally focused successor to the Millennium Development Goals. Covering a broad range of environmental, economic, and social development initiatives, the SDG targets are regarded as being profoundly interlinked, integrated, and inseparable from one another.1 For example, progress in health (SDG 3) will depend on progress in poverty reduction efforts (SDG 1), highlighting the need for cross-sectoral thinking in their implementation. Tuberculosis, as a disease that features complex interactions with poverty and its associated social and structural factors, offers the opportunity to investigate closely how the SDGs align with disease control efforts.
The SDG targets share a conceptual and pragmatic vision with WHO's End TB Strategy.2 From the conceptual perspective, both the End TB Strategy and the SDG targets are concerned with the root determinants of human health.3 In line with this thinking, the social determinants of tuberculosis are increasingly recognised as a research and programmatic priority, and the overarching aims of the End TB and SDG agendas should be regarded as linked. The End TB Strategy aims to reduce tuberculosis incidence by 90%, related deaths by 95%, and catastrophic costs by 100% by 2035, and includes a milestone for 2030, reflected in SDG 3, of an 80% reduction in tuberculosis incidence.4
Specifically, the eventual elimination of tuberculosis will require progress on the SDG 1 subtargets, which include efforts towards the reduction of poverty and expansion of social protection coverage. The links between increased social protection and reduced tuberculosis burden are well known to be applicable at the ecological level.5, 6 Biosocial theories of disease provide a potential mechanism by which social protection and poverty reduction could reduce tuberculosis burden at the individual level.7, 8 Because biomedical innovation in the response to tuberculosis alone will not be able to accelerate the reduction in tuberculosis incidence required to meet the programmatic targets of the End TB Strategy,4 what impact a reduction in the socioeconomic drivers of tuberculosis might have is also important to investigate. The SDG 1 subtargets include several indicators designed to operationalise and measure progress towards poverty reduction and expansion of social protection programmes. In view of the ubiquity of SDGs in the development agenda, the SDG 1 indicators and timeline provide an appropriate framework.
Research in context.
Evidence before this study
Sustainable Development Goal 1 (SDG 1) commits to ending poverty and expanding social protection coverage. The link between poverty and tuberculosis has been well described and evidence from ecological studies supports an association between increased social protection and decreased tuberculosis burden. Both poverty reduction and social protection are codified as part of WHO's End TB Strategy to implement and strengthen bold policies and supportive systems. Two articles published in 2016 describe a shared conceptual and pragmatic alignment between the End TB Strategy and the broader SDGs, but no quantitative evidence or projections of effect exist to support this strategic link.
Added value of this study
Conceptually, our study is the first to adopt an SDG framework to quantify the interdependence between tuberculosis elimination and development. Methodologically, the use of a well defined conceptual framework and clear operationalisation of indicators and outcomes provides a robust approach to statistical modelling. The resulting estimate of a decrease in incidence of 84·3% (95% credible interval 54·7–94·9) from baseline by the target year for the SDGs reaffirms the role of poverty elimination and social protection in global tuberculosis control. Furthermore, because this methodological approach can be extended to SDGs other than SDG 1 and to diseases other than tuberculosis, our study provides a replicable analytical model suitable across a range of development and public health thematic areas.
Implications of all the available evidence
WHO's End TB Strategy arose in parallel with the SDGs with the precise intent of aligning indicators, targets, and strategic thinking. In the case of SDG 1, our study confirms this alignment is supported by quantitative evidence. Multisectoral approaches including the development sector are necessary if global health challenges, including tuberculosis, are to be addressed in an effective and sustainable way. The framing of our study within the broader development agenda should guide policy and practice across the development and health policy landscapes.
In this Article, reflecting a key target of the End TB Strategy, we estimate the reduction in global tuberculosis incidence that could be obtained by reaching SDG 1's targets of reducing poverty and expanding social protection.
Methods
Overview
To produce an estimate of the impact of attaining SDG 1 on tuberculosis incidence, we undertook three key steps: generation of a conceptual framework, reduction of that conceptual framework, and statistical modelling.
Conceptual framework generation
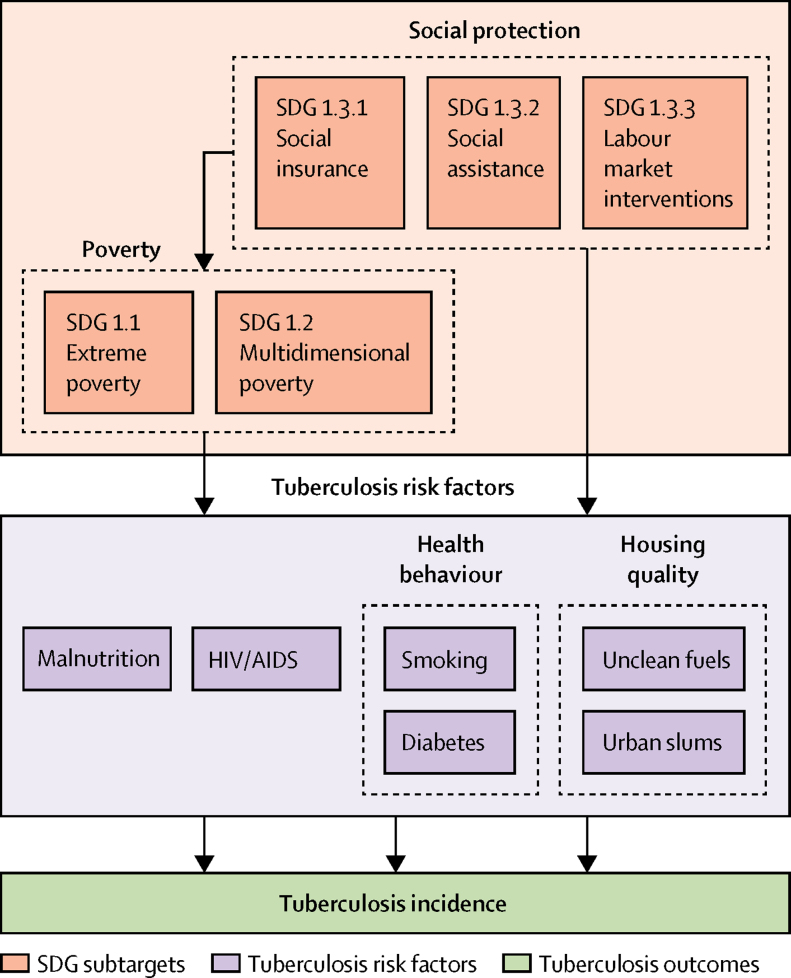
We sought to build a conceptual framework composed of theoretical pathways that link the relevant SDG 1 indicators, via several relevant risk factors, to an impact on tuberculosis incidence (figure 1). Furthermore, we sought to populate the framework with available data from a range of sources.
Figure 1.
Conceptual framework linking SDG 1 indicators to tuberculosis incidence
We assumed a hierarchical relation among subtargets, by which increasing social protection coverage affects extreme and multidimensional poverty. Each of the SDG subtargets is assumed to be linked to each of four tuberculosis-relevant risk factors (malnutrition, HIV, health behaviours, and housing quality), which in turn are linked to tuberculosis incidence. On the basis of this framework, simple epidemiological analyses were done to estimate the effect of meeting the three subtargets on tuberculosis incidence, both directly or as mediated by each of the four intermediate risk factors. SDG=Sustainable Development Goal.
As established by the UN, SDG 1 is composed of five subtargets. For this analysis, key subtargets of interest are SDG 1.1 (elimination of extreme poverty), SDG 1.2 (halving of multidimensional poverty), and SDG 1.3 (social protection for all). Extreme poverty is defined as living on less than US$1·90 per day, whereas multidimensional poverty is a composite measure of poor health, education, and living standards. Social protection refers to measures that are designed to reduce vulnerability to falling into poverty, including labour market interventions, contributory welfare programmes, and cash or resource transfers. We excluded subtargets SDG 1.4 (access to land rights and basic services for all) and SDG 1.5 (reduce mortality from climate-related disasters) from the overall analysis on the grounds of no evidence in the scientific literature for a relevant link to tuberculosis burden.9
The tuberculosis risk factors were selected on the basis of a review by Lönnroth and colleagues10 as proximal risk factors with the highest population attributable fraction. The risk factors include malnutrition, HIV infection, housing quality, and health behaviour. The health behaviour (smoking prevalence and diabetes prevalence) and housing quality (proportion exposed to indoor air pollution and proportion living in an urban slum) risk factors are composite factors informed by a principal components analysis done on the data. Care was taken to select only those risk factors that were thought to be more proximal to tuberculosis than the SDG 1 subtargets themselves.
Data were extracted to populate the framework for 192 countries from 2010 to 2015 corresponding to the indicators (measures) for the SDG subtargets and measures for the tuberculosis risk factors. The most recent value was carried forward. No data were more recent than 2015, so we consider 2015 the baseline year.
We populated the SDG subtargets with data taken from the SDG repository for their corresponding indicator.11 Indicators for SDG 1.1 and 1.2 are measures of poverty reduction. The primary indicator for SDG 1.1 is the proportion of individuals living under the extreme poverty line of $1·90 per day. The primary indicator for SDG 1.2 is the value of the multidimensional poverty index for that country. SDG 1.3 is composed of three primary indicators that are measures of social protection expansion: the proportion of people covered by labour market protections, the proportion of people covered by social assistance, and the proportion of people covered by social insurance.
We populated the risk factor measures with data obtained from the WHO databank for smoking, HIV, and diabetes prevalence, and data from the SDG repository for all other risk factors.11, 12 The measure for malnutrition was the proportion malnourished, for HIV infection was the proportion HIV positive, for housing quality was composed of the proportion burning unclean fuels in the home and the proportion living in urban slums, and for health behaviour was composed of the proportion of smokers and the proportion with diabetes. Although not proximal risk factors for tuberculosis, we also extracted information on gross domestic product and Gini coefficients from the SDG repository for sensitivity analyses.
After the most recent observed value was carried forward, all SDG indicators and risk factor measures had fairly large (>20%) amounts of missing data (appendix), with the exception of HIV prevalence, tuberculosis incidence, and malnutrition. A similar proportion of missing data were found across all different income levels and all different regions, suggesting that missingness was not associated with observed data and, as such, the data were unlikely to be missing not at random.13 In view of the large amounts of missing data, single imputation approaches were adopted for exploratory analyses and a multiple imputation approach using chained equations was used for analyses directly informing the statistical modelling (appendix).
Conceptual framework reduction
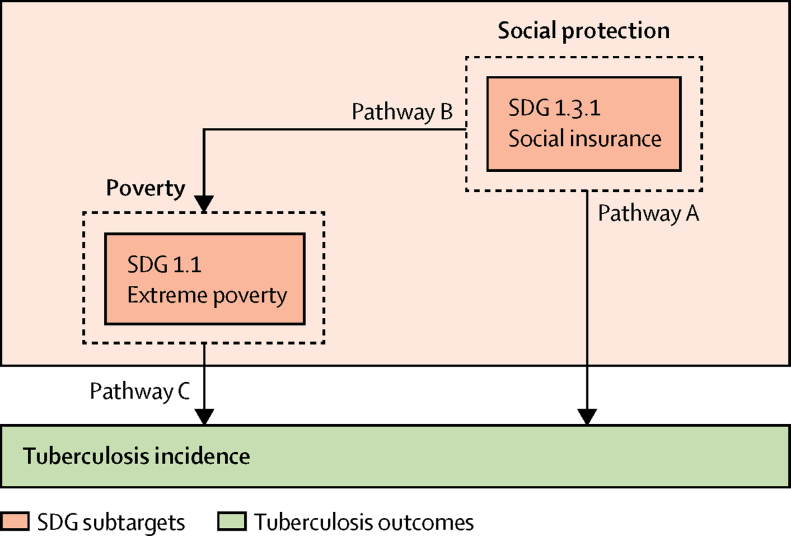
The conceptual framework (figure 1) is complex to model statistically because the multiple layers in the framework require hierarchical models and result in difficulties in propagating uncertainty. As such, we created a reduced version of the conceptual framework that was more amenable to quantitative analysis (figure 2). This reduced framework makes two key simplifying assumptions: that SDG 1.1 (extreme poverty) and SDG 1.2 (multidimensional poverty) measure a similar underlying construct, and that the intermediate layer composed of tuberculosis risk factors can be omitted.
Figure 2.
Reduced conceptual framework
A reduced framework amenable to statistical modelling, depicting five pathways to represent the direct effect of social protection for all on tuberculosis (Pathway A), the direct effect of poverty elimination on tuberculosis (Pathway C), the joint effect of the two simultaneous direct effects (Pathway A and Pathway C), the indirect effect of social protection on tuberculosis via poverty elimination (Pathways B + C), and the total effect of social protection on tuberculosis (Pathway A and Pathways B + C). SDG=Sustainable Development Goal.
We assessed the first assumption's validity by generating a correlogram between all measures in the complete framework and examining the resulting correlation coefficients, with particular focus on the SDG 1 subtargets. The correlogram would also inform which choice of metric (social insurance, social assistance, or labour market interventions) to use for SDG 1.3 (social protection) because the measure used must be associated directly with tuberculosis incidence. We created the correlogram after conducting a single imputation by region using the regression substitution method. We generated five imputations of the dataset and the data used to generate the correlogram come from a randomly selected imputed dataset.
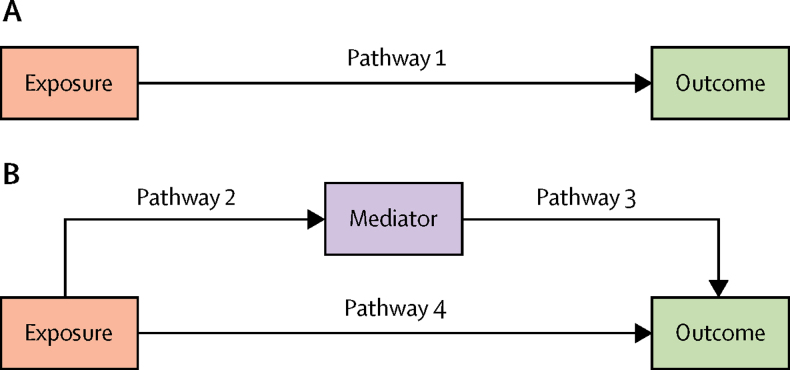
We did an assessment for mediation to confirm whether each tuberculosis risk factor is individually a mediator. We investigated whether adjusting for a single intermediary risk factor changed the association between tuberculosis incidence and a given SDG 1 subtarget. To omit the intermediate layer of tuberculosis risk factors from the framework for analysis, we assume that these proximal risk factors completely mediate the relation between the SDG indicators and tuberculosis incidence. For this assumption to hold, all risk factors should collectively be sufficient to account for the total effect of SDG 1 on tuberculosis incidence. For a risk factor to be a mediator, it must be associated with the outcome and exposure, and be on the causal pathway (figure 3).
Figure 3.
Examples of causal pathways
(A) Pathway 1 is the total effect of an exposure on an outcome. (B) The total effect of an exposure on an outcome can be decomposed into a direct effect of the exposure on the outcome (Pathway 4) and an indirect effect of the exposure on the outcome via a mediator (Pathways 2 + 3). Statistical adjustment for the mediator will show the amount of the total effect that is attributable to the indirect effect via the mediator. If a large amount of the total effect is accounted for by the indirect effect (Pathway 4 close to 0) and there is no residual confounding, modelling either the total effect (Pathway 1) or the indirect effect (Pathways 2 + 3) should result in similar effect estimates. This would justify the reduced modelling framework (structurally equivalent to Pathway 1) over the full framework (structurally equivalent to Pathways 2 + 3).
To assess whether the total effect of the SDG 1 subtargets was accounted for by the risk factors, we used linear models to estimate the total crude association of each SDG subtarget with tuberculosis incidence. We compared these associations with the adjusted associations between the SDG subtargets and tuberculosis incidence to determine the degree to which adjustment for the risk factor pathways changed the crude estimate from the linear models. We hypothesise that much of the total crude association is accounted for via adjustment for the risk factor pathways and expect a reduction of the estimated association towards 0 after adjustment. The total association would then be equivalent to the indirect association via the risk factor pathways and the risk factors can be omitted from the model, assuming that the set of variables adjusted for capture all major tuberculosis risk factors and that, consequently, there is minimal residual confounding (figure 3).
Statistical modelling
We used the reduced framework to statistically model five effects on tuberculosis incidence: the direct effect of increased social protection, the direct effect of reduced extreme poverty, the joint effect of increased social protection and reduced extreme poverty, the indirect effect of social protection via reduced poverty, and the total effect composed of the joint effect and indirect effect (figure 2).
We performed the statistical modelling in five steps. First, we estimated the association between the subtarget (or subtargets) of interest and tuberculosis incidence at baseline to provide the expected reduction in tuberculosis incidence per 1% change in subtarget measure (β). Second, we extracted the change per year (for t years) in absolute poverty (or increase in social protection) associated with an x% reaching of the SDG subtarget:
Third, we scaled the expected decrease in tuberculosis incidence by this change to get the expected incidence reduction from reaching the SDG subtarget:
Fourth, we obtained the annual proportional decrease in incidence by converting to a proportion of baseline incidence:
Fifth, we placed the annual proportional decrease into an exponential decay model:
or with multiple subtarget measures into the model:
This results in an expected tuberculosis incidence for 2035, the year by which both the SDG 1 and End TB targets are supposed to have been completed. We produced credible intervals (CrI) by applying the same modelling procedure to the 5% and 95% bounds of the initial estimate for β, capturing the uncertainty in the association and reflecting the bounds between which we expect 95% of incidence projections to fall.
Sensitivity analyses
We examined linear models that adjusted for income and income equality as a sensitivity analysis to determine if income effects accounted for any residual confounding and should thus have been included in the full framework in figure 1.
We also did sensitivity analyses to investigate some of the assumptions of the statistical modelling. We investigated the results in an analysis that included only countries with non-missing data for social protection outcomes and measures of extreme poverty. We further investigated how much the results would change under scenarios in which social protection coverage was expanded to 50% (instead of 100%) and in which extreme poverty was 90% eliminated (instead of 100%).
To determine whether the assumption of a linear trend for β was valid, we examined a model with a quadratic term for improved model fit. Restricted cubic spline methods and piecewise linear functions were also considered but would have resulted in substantial additional complexity in statistical modelling and eventual interpretation of projections, and thus, were not a valid alternative for the methodology presented in this study.
Role of the funding source
The funder of the study gave input on the general approach and provided some data on SDG and tuberculosis indicators. The funder had no role in collation of additional data, development of the analysis framework, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
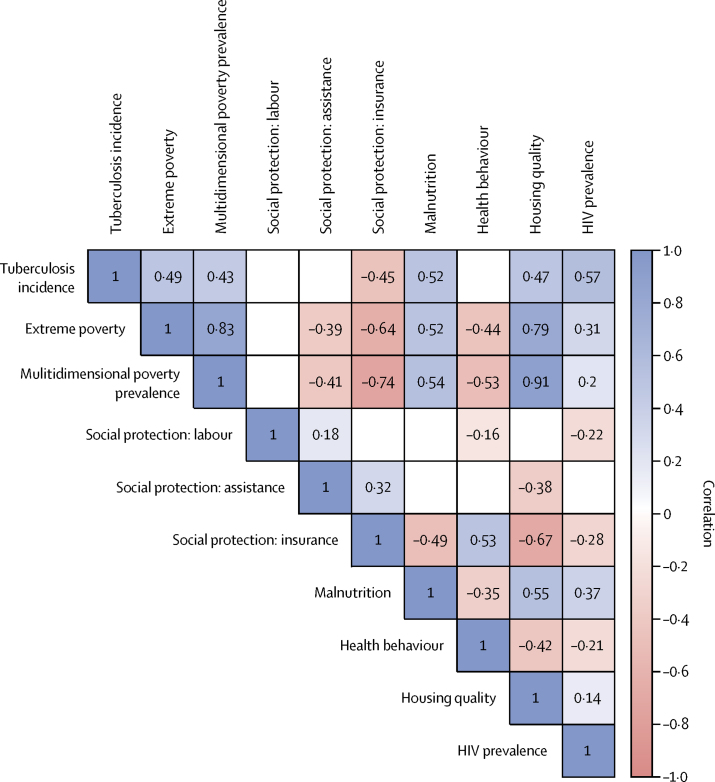
We created a correlogram that describes the structure of the data to validate the assumptions required for reducing the conceptual framework (figure 4). Extreme poverty and multidimensional poverty are strongly correlated (r=0·83), validating the assumption that they might be measuring the same underlying construct. Social insurance is the only form of social protection correlated with tuberculosis incidence (r=–0·45), and social insurance was therefore used as the measure of choice for statistical modelling of SDG 1.3.
Figure 4.
Correlogram of all indicators, measures, and tuberculosis incidence
Blue indicates positive correlation whereas red indicates negative correlation. The value inside each square of the grid is the correlation coefficient (r value). All correlation coefficients shown have an associated p value of less than 0·05 under a null hypothesis of pairwise independence. Malnutrition (r=0·52), extreme poverty (r=0·49), multidimensional poverty (r=0·43), HIV (r=0·57), and housing quality (r=0·47) are all moderately correlated with tuberculosis incidence. They are all strongly positively correlated with each other (dark blue values) and moderately negatively correlated with adverse health behaviours and social insurance (light red values).
We found evidence that all tuberculosis risk factors were potential mediators, but that social insurance was a particularly strong mediator, further suggesting its use in the statistical model (appendix).
There was no evidence that any of the SDG subtarget indicators were associated with tuberculosis after adjusting for more proximal factors or more and equally proximal factors (table 1). However, all four tuberculosis risk factors were associated with tuberculosis incidence after adjusting for other risk factors (table 1). These findings suggest that none of the set of four risk factors were solely responsible for the direct effect on tuberculosis incidence.
Table 1.
The association between each indicator or measure and tuberculosis incidence per 100 000 people per year
| Crude estimate (95% CI) | Adjusted estimate (95% CI)* | Adjusted estimate (95% CI)† | |
|---|---|---|---|
| Subtarget indicator | |||
| SDG 1.1: extreme poverty | 3·59 (2·54 to 4·65) | 0·22 (−1·22 to 1·66) | 0·62 (−1·08 to 2·33) |
| SDG 1.2: MPI prevalence | 2·52 (1·48 to 3·57) | −0·50 (−2·35 to 1·36) | −0·87 (−3·02 to 1·28) |
| SDG 1.3: labour protection | −0·19 (−5·38 to 5·01) | −1·04 (−3·97 to 1·89) | −0·92 (−4·09 to 2·26) |
| SDG 1.3: social assistance | −1·27 (−2·28 to −0·26) | −0·06 (−0·77 to 0·64) | 0·01 (−0·75 to 0·78) |
| SDG 1.3: social insurance | −3·52 (−4·44 to −2·60) | −0·94 (−2·36 to 0·48) | −1·04 (−2·55 to 0·48) |
| Risk factor measure | |||
| Malnourishment | 7·25 (5·54 to 8·95) | .. | 3·09 (1·19 to 4·98) |
| Health behaviour | −2·16 (−5·10 to 0·78) | .. | 4·13 (1·52 to 6·73) |
| Housing quality | 2·70 (1·89 to 3·51) | .. | 1·93 (1·19 to 2·68) |
| HIV prevalence | 26·85 (19·90 to 33·80) | .. | 23·62 (18·90 to 28·34) |
Equal hierarchy of risk factors was assumed, in line with figure 1. SDG=Sustainable Development Goal. MPI=Multidimensional Poverty Index.
The association between a single indicator or risk factor and tuberculosis, adjusted for all variables more proximal to tuberculosis incidence (tuberculosis risk factors).
The association between a single indicator or risk factor and tuberculosis, adjusted for all variables more and equally proximal to tuberculosis incidence (SDG subtargets and tuberculosis risk factors).
Taken together, these models suggest that the total effect of the SDG subtargets on tuberculosis incidence is representative of the indirect effect through the four tuberculosis risk factor pathways, validating the omission of the risk factor pathways in the reduced modelling framework. We do not suspect any residual confounding by gross domestic product or by Gini coefficient because these variables were not associated with tuberculosis incidence after adjustment for all other targets and risk factors (appendix).
Ending extreme poverty resulted in a reduction in global tuberculosis incidence of 33·4% (95% CrI 15·5–44·5) by 2035. Expanding social protection coverage resulted in a reduction in global tuberculosis incidence of 76·1% (95% CrI 45·2–89·9) by 2035. Both direct effects together resulted in a reduction in incidence of 84·3% (95% CrI 54·7–94·9).
The effect of eliminating poverty and increasing social protection coverage to 100% gives an estimated annual proportional decrease in tuberculosis incidence of approximately 9·1% (table 2). Increasing social protection coverage alone could result in an estimated annual proportional decrease of about 8·7%.
Table 2.
Projected tuberculosis incidence per 100 000 people per year associated with the achievement of selected SDG 1 subtargets
| β (95% CI) | Estimated 2035 incidence per 100 000 people (95% CrI) | Decrease from baseline*(95% CrI) | Expected annual proportional decrease | |
|---|---|---|---|---|
| Pathway A: social protection for all (100% coverage) | −2·13 (−3·36 to −0·90) | 28·5 (11·9 to 65·3) | 76·1% (45·2 to 89·9) | 8·7% |
| Pathway C: poverty elimination (100% eliminated) | −2·37 (−3·64 to −1·10) | 80·6 (66·2 to 100·7) | 33·4% (15·5 to 44·5) | 2·0% |
| Pathway A and Pathway C: social protection and poverty elimination | .. | 18·7 (6·0 to 54·0) | 84·3% (54·7 to 94·9) | 11·1% |
| Pathways B + C: social protection via poverty elimination | .. | 83·2 (65·7 to 103·2)†‡ | 30·2% (13·4 to 44·9) | 1·8% |
| Pathway A and Pathways B + C: total effect of social protection | .. | 21·6 (6·3 to 43·1)† | 81·9% (64·8 to 94·8) | 9·1% |
The value of β comes from linear associations generated from the pathways in figure 2 and represents the association of tuberculosis and social protection, independent of extreme poverty and vice versa. 95% CrIs represent the values between which 95% of model projections would be expected to fall on the basis of the distribution of β. 95% CrIs are not perfectly symmetrical because the exponential decay portion of the model creates an asymptote at y=0; as the expected incidence approaches 0, the 95% CrI will be closer to the estimate. Joint effects are calculated with the provided values of β. SDG=Sustainable Development Goal. CrI=credible interval.
Baseline: year 2015 with last year reported since 2010 carried forward.
Includes variance from Pathway C but not from B.
β for Pathway B alone is −0·57 (95% CI −0·72 to −0·42).
Adjustment for gross domestic product and the Gini coefficient resulted in a decrease in effect size for the health behaviour pathway and an increase in effect size for the social insurance pathway (appendix).
An analysis using complete cases for social insurance and extreme poverty was found to be broadly similar in terms of the size of the effect estimate produced by the statistical model, although with wider CrIs, which are likely to result from the insufficient power produced by restriction of the sample size. Under the scenario in which social protection was expanded to 50% (instead of 100%) and in which extreme poverty was 90% eliminated (instead of 100%), the point estimates for reduction from baseline were still substantial: 18·1% for absolute poverty elimination, 41·6% for social protection expansion, and 52·5% for the combination of these strategies (appendix).
The addition of a quadratic term in an additional sensitivity analysis did not substantially improve the fit of the model, suggesting no evidence of a non-linear trend in the association between extreme poverty and tuberculosis, and social protection and tuberculosis.
Discussion
The reduced framework linked SDG 1 subtargets directly to tuberculosis incidence, validated by correlational analyses and an assessment for mediation. Ending extreme poverty and expanding social protection coverage each resulted in a reduction in the global incidence of tuberculosis by 2035. Both direct effects together also resulted in a reduction in incidence, suggesting social protection expansion is key.
The scale of the reduction in tuberculosis incidence projected is particularly important in view of a 2017 study14 suggesting that fewer than 5% of countries will reach the goal for tuberculosis elimination outlined in SDG 3. The 11% annual proportional decrease in tuberculosis projected by this model is commensurate with the scale of the proportional annual decrease that the End TB Strategy suggests would be necessary to reach the 2035 targets and is likely to have an effect on transmission dynamics.4 Regardless of whether the SDG 1, SDG 3, or End TB targets are reached completely, our study shows that eliminating extreme poverty and especially increasing social protection coverage are key to reducing tuberculosis incidence.
A major strength of this study is the data-driven approach to generating and analysing the modelling framework. Validation of the modelling framework with an analytical approach means we are measuring the association of interest—namely, SDG 1 and tuberculosis incidence—while still accounting for major risk factor pathways. Our approach provides a reasonable balance between complexity and clarity. The statistical model extends beyond point associations and provides projections of future tuberculosis burden that are key for policy discussions. However, we avoid the escalating assumptions and uncertainties of using a mechanistic transmission model to capture these associations.
This study has some data-centric limitations. Not all countries yet collect routine prevalence estimates for social protection coverage or for extreme poverty. However, a robust protocol for the handling of missing data was implemented, and missing data on key exposure variables were not associated with tuberculosis risk factors or WHO region. Improved data availability and quality would have allowed for more refinements to the overall statistical model. Particularly, the production of regional estimates would have been preferable to the global model in view of the different effects of different types of social protection in different regions. The annual proportional decrease in tuberculosis incidence is probably lower than our estimate in high-income regions and higher than our estimate in regions with a greater proportion of low-income and middle-income countries, although in this global model, all regions are given equal weight.
Because the burden of tuberculosis and of poverty is concentrated in low-income and middle-income countries, the proportional annual decrease provided is probably a conservative estimate for the reduction in incidence expected were SDG 1 to be globally attained. With improved data quality, we could also assess whether the relation between poverty, social protection, and tuberculosis is non-linear in some regions, which could result in a more precise estimate than obtained by assuming linearity. Studies using similar analytical projection methodologies for tuberculosis have used regional models and non-linear associations to inform global estimates.15, 16 However, in this analysis, regional models resulted in wide confidence intervals for β due to sparsity of data. Although we acknowledge that, in a global model, countries will have heterogeneous profiles for risk factors, this heterogeneity must be considered in a trade off with statistical power. Sufficient statistical power to make robust conclusions is unlikely to be attained in subgroup analyses, particularly in view of the missing data in this study; this is evident in the sensitivity analysis done on complete cases.
The estimated annual proportional decrease in tuberculosis incidence projected assumes that the association between the SDG 1 subtargets remains constant as progress is made towards eliminating poverty. Because tuberculosis remains concentrated in the most vulnerable populations, elimination of the last 1% of extreme poverty might have a larger effect on incidence than elimination of the first 1%,17 and thus the value for β might increase over time, which is not captured by this model. This would imply the projections are conservative. However, the elimination of the last pockets of extreme poverty is likely to be more challenging than elimination at baseline, which is captured by the exponential decay component of the statistical model; the absolute decrease slows as progress is made towards reducing poverty. As such, the projections might overestimate the amount of poverty elimination (or social protection) that is feasible within the given timeframe. Both the changing value of β and the changing difficulty of eliminating poverty over time are likely to be heterogeneous between nations and regions, and it is not possible to tell from the collected data whether taken together these factors bias the global estimate upwards or downwards.
The sensitivity analysis investigating non-linearities in β suggest that the assumption of a constant β is not unreasonable. Although other shapes might be possible, little evidence is available to guide either selection of an appropriate non-linear term to replace our analysis or to estimate appropriate standard errors for the CrIs. Although we recognise that β can change over time, in practice incorporation of this change into the model while maintaining the present balance between complexity and interpretability is impossible. Similar concerns arise for changes in the scaling of poverty reduction or social protection expansion; what a reasonable value is for non-linearity with respect to Δx is unclear, as is how to propagate the uncertainty involved with a variable value of Δx.
The statistical model estimates use social insurance as the main measure of social protection, which tends to be more associated with higher-income countries relative to social assistance and labour protection measures (appendix). However, we found an association between social insurance and reduced tuberculosis incidence even after accounting for gross domestic product and the Gini coefficient, which suggests that social insurance is not simply acting as a proxy measure for being in a high-income country or for having low-income inequality (appendix). Social insurance might also be the only SDG 1 measure correlated with tuberculosis incidence because social insurance systems (eg, welfare and unemployment) have wide-ranging effects on society compared with social assistance schemes, which might be more directly targeted at groups that probably, but might not necessarily, overlap with patients with tuberculosis (eg, conditional cash transfers, disability grants, and child benefits). Social insurance is also likely to act more tangibly and more rapidly on tuberculosis trends than labour market reforms or social assistance programmes by enhancing access to tuberculosis care (eg, through health insurance) and by mitigating the effect of tuberculosis-related catastrophic costs and, more broadly, the financial consequences of tuberculosis (ie, unemployment programmes). Although an aggregate measure of social protection prevalence would be a useful metric for SDG 1.3, it is not provided by the SDG databank.
There are some limitations to the use of social insurance as a proxy measure of social protection coverage. We consider prevalence of social insurance to be a measure of a wider construct that includes the structural and social factors required to implement a social insurance system, which might bias our estimate higher. This is probably why social protection was found to be more efficacious than extreme poverty elimination alone; promotion of social insurance systems is likely to entail efforts to eradicate poverty. For a country to expand social insurance, its citizens need to be able to contribute in some way to a system of wealth redistribution, which in turn requires a degree of household financial stability that is unlikely to occur without the elimination of other factors associated with tuberculosis incidence, such as malnutrition, poor housing, and catastrophic costs. In this way, the floor of poverty is first raised by implementation of policy towards expanding social insurance, which might include forms of social protection that are comparatively easier to implement, such as social assistance and labour market interventions. As such, we might conceive of social insurance as a measure that indicates concomitant progress on the other SDG 1 targets.
Evidence is coalescing around a positive effect of social protection in tuberculosis control.5, 6, 18, 19 This is the first study to directly link policies that form part of the End TB Strategy to SDG 1 or to provide projections of potential future tuberculosis incidence reduction from SDG achievement. Through this alignment there are high level opportunities to enable common progress towards both sets of targets. In view of the strong potential of social protection in tuberculosis, even compared with extreme poverty elimination, further policy assessment and consideration should be given to the role that various social protection programmes might have in tuberculosis control efforts, including the added value of social protection to mitigate catastrophic costs.
In November, 2017, Russia hosted an unprecedented WHO Global Interministerial Conference on ending tuberculosis to stimulate action and commitments. The resulting Moscow resolution aimed for the development of a framework working towards improved integration between tuberculosis care and social protection services. This framework entails the development of cross-sectoral delivery models able to rapidly detect eligible patients on the basis of clinical and vulnerability criteria, rather than just income; identify the most suitable social protection scheme on the basis of the patient's profile; and facilitate access and enrolment by supporting the patients administratively and legally.
Because national social protection programmes are often under the jurisdiction of governmental development and welfare agencies or non-governmental organisations, the aforementioned cross-sectoral approaches are urgently needed if we are to capitalise on the opportunities to address the distal and proximal risk factors for tuberculosis. Political commitment is one of the key tenets of the End TB Strategy, and responsibility for work towards a sustainable solution to ending the tuberculosis epidemic rests in part with stakeholders outside the biomedical community capable of modifying its upstream drivers.
The scale of reduction in tuberculosis incidence seen by the attainment of SDG 1 would have a substantial effect on the progress towards tuberculosis elimination, accelerating the global downwards trend in tuberculosis incidence. Irrespective of whether the SDG 1, SDG 3, or End TB targets are reached completely, our research suggests that eliminating extreme poverty and especially increasing social protection coverage are key to reducing tuberculosis incidence. Cross-sectoral approaches that promote poverty reduction and social protection expansion will be crucial to the achievement of SDG 1 and provide the reduction in tuberculosis incidence that SDG 3 and the End TB Strategy are aiming to achieve. The approach of this study should be used to assess how other SDGs might affect the reduction of tuberculosis incidence to inform future advocacy and policy efforts.
Contributors
DJC, DB, and RMGJH conceptualised the Article. DJC, PG, KL, KF, MR, RMGJH, and DB agreed on the study protocol and analysis plan. DJC and PG were responsible for data procurement and storage. DJC did the data analysis and drafted the manuscript with input from RMGJH and DB. All authors discussed and agreed on the implications of the study findings and approved the final version to be published.
Declaration of interests
WHO provided financial assistance in the form of salary support during the study. We declare no competing interests.
Supplementary Material
References
- 1.Transforming our world: the 2030 Agenda for Sustainable Development: Sustainable Development Knowledge Platform. https://sustainabledevelopment.un.org/post2015/transformingourworld (accessed Aug 24, 2017).
- 2.Lönnroth K, Raviglione M. The WHO's new End TB Strategy in the post-2015 era of the Sustainable Development Goals. Trans R Soc Trop Med Hyg. 2016;110:148–150. doi: 10.1093/trstmh/trv108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fitchett JR, MacPherson P, Corbett EL. Implementing the End TB Strategy and the intersection with the Sustainable Development Goals, 2016–2030. Trans R Soc Trop Med Hyg. 2016;110:145–147. doi: 10.1093/trstmh/trw010. [DOI] [PubMed] [Google Scholar]
- 4.Uplekar M, Weil D, Lönnroth K. WHO's new End TB Strategy. Lancet. 2015;385:1799–1801. doi: 10.1016/S0140-6736(15)60570-0. [DOI] [PubMed] [Google Scholar]
- 5.Reeves A, Basu S, McKee M, Stuckler D, Sandgren A, Semenza J. Social protection and tuberculosis control in 21 European countries, 1995–2012: a cross-national statistical modelling analysis. Lancet Infect Dis. 2014;14:1105–1112. doi: 10.1016/S1473-3099(14)70927-2. [DOI] [PubMed] [Google Scholar]
- 6.Siroka A, Ponce NA, Lönnroth K. Association between spending on social protection and tuberculosis burden: a global analysis. Lancet Infect Dis. 2016;16:473–479. doi: 10.1016/S1473-3099(15)00401-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krieger N. Methods for the scientific study of discrimination and health: an ecosocial approach. Am J Public Health. 2012;102:936–944. doi: 10.2105/AJPH.2011.300544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ortblad KF, Salomon JA, Bärnighausen T, Atun R. Stopping tuberculosis: a biosocial model for sustainable development. Lancet. 2015;386:2354–2362. doi: 10.1016/S0140-6736(15)00324-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lönnroth K, Jaramillo E, Williams BG, Dye C, Raviglione M. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc Sci Med. 2009;68:2240–2246. doi: 10.1016/j.socscimed.2009.03.041. [DOI] [PubMed] [Google Scholar]
- 10.Lönnroth K, Castro KG, Chakaya JM. Tuberculosis control and elimination 2010–50: cure, care, and social development. Lancet Lond Engl. 2010;375:1814–1829. doi: 10.1016/S0140-6736(10)60483-7. [DOI] [PubMed] [Google Scholar]
- 11.UN SDG indicators. https://unstats.un.org/sdgs/metadata/ (accessed Aug 31, 2017).
- 12.WHO Tuberculosis data. http://www.who.int/tb/data/en/ (accessed Aug 31, 2017).
- 13.Rubin DB. Inference and missing data. Biometrika. 1976;63:581–592. [Google Scholar]
- 14.Abajobir AA, Abate KH, Abbafati C. Measuring progress and projecting attainment on the basis of past trends of the health-related Sustainable Development Goals in 188 countries: an analysis from the Global Burden of Disease Study 2016. Lancet. 2017;390:1423–1459. doi: 10.1016/S0140-6736(17)32336-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Odone A, Houben RMGJ, White RG, Lönnroth K. The effect of diabetes and undernutrition trends on reaching 2035 global tuberculosis targets. Lancet Diabetes Endocrinol. 2014;2:754–764. doi: 10.1016/S2213-8587(14)70164-0. [DOI] [PubMed] [Google Scholar]
- 16.Dye C, Trunz BB, Lönnroth K, Roglic G, Williams BG. Nutrition, diabetes and tuberculosis in the epidemiological transition. PLoS One. 2011;6:e21161. doi: 10.1371/journal.pone.0021161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ravallion M. How long will it take to lift one billion people out of poverty? World Bank Res Obs. 2013;28:139–158. [Google Scholar]
- 18.Boccia D, Hargreaves J, Lönnroth K. Cash transfer and microfinance interventions for tuberculosis control: review of the impact evidence and policy implications. Int J Tuberc Lung Dis. 2011;15(suppl 2):S37–S49. doi: 10.5588/ijtld.10.0438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nery JS, Rodrigues LC, Rasella D. Effect of Brazil's conditional cash transfer programme on tuberculosis incidence. Int J Tuberc Lung Dis. 2017;21:790–796. doi: 10.5588/ijtld.16.0599. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.