
Prof Dr Sanjay Kumar Singh
Epidemiology
Pterygium is a degenerative disorder of the conjunctiva. It is usually seen as a triangular fleshy fibrovascular proliferation from the bulbar conjunctiva onto the cornea, located mostly on the nasal side. Though it occurs worldwide, its prevalence is high in the “pterygium belt” between 30 degrees north and 30 degrees south of the equator.1 The prevalence of pterygium is reported to be 3% in Australians, 23% in blacks in United States, 15% in Tibetans in China, 18% in Mongolians in China, 30% in Japanese and 7% in Singaporean Chinese and Indians.2–7
In a population-based study from rural central India, prevalence of pterygium increased from 6.7±0.8% in the age group from 30–39 years to 25.3±2.1% in the age group of 70–79 years. Three population based studies have described the incidence of pterygium. Barbados eye study has described the nine year incidence of pterygium to be 11.6% (95% CI, 10.1–13.1), the Beijing Eye Study described the 10 year incidence of pterygium in the adult Chinese population to be 4.9%, and the five year cumulative incidence in Bai Chinese population in a rural community was 6.8% (95% CI, 5.2–8.4).8–10
Risk factors and pathogenesis
These population-based studies suggest that cumulative ultraviolet light exposure due to outdoor occupation is a major risk factor for the development of pterygium. Other factors associated with pterygium development are age, being male and having dry eyes.11–13 Genetic factors, tumor suppressor gene p53 and other genes may be involved in the pathogenesis of pterygium.14
A study indicated a two-stage hypothesis for pterygium pathogenesis: initial disruption of the limbal barrier and progressive active “conjunctivalisation” of the cornea.15 Identification of Fuchs Flecks at the head of pinguecula, primary pterygium, recurrent pterygium, and macroscopically normal nasal and temporal limbus may represent precursor lesions to UV associated ocular surface pathology.16
Prevention
Avoidance of environmental risk factors like sunlight, wind and dust by wearing UV rays protecting sunglasses and hat may prevent development of pterygium. These protective measures may help to prevent recurrence of pterygium after surgery. Similarly, wearing of eye safety equipment is recommended in environment exposed to chemical pollutants as a preventive measure for pterygium.
Indication for surgery
The main indication for pterygium surgery is visual disturbance secondary to encroachment over the pupillary area or induced astigmatism. Other indications which can be considered are, restriction in eye movements, chronic redness and foreign body sensation, and cosmetic concerns.17
Management
Surgery is the mainstay of treatment for pterygium causing visual disturbances. The primary complication of pterygium surgery is recurrence defined by regrowth of fibrovascular tissue across the limbus and onto the cornea. No uniformity of opinion exists regarding the ideal pterygium excision procedure associated with lowest recurrence rate. Bare sclera technique, which is widely used in the developing world for the ease and speed of surgery, is associated with high recurrence rates.18 Other adjunctive therapies combined with bare sclera technique have significantly reduced the recurrence rate (2% to 15%).19 Application of different agents like Strontium 90, Beta irradiation and cytotoxic drugs like Mitomycin-C and 5-Fluorouracil to the scleral bed have been tried but sight threatening complications like inflammatory scleritis, scleromalacia and loss of the eye have been occasionally reported.20 Amniotic membrane transplantation has been used after bare sclera technique with a reported recurrence rate of 4% to more than 60%.21,22 Currently, the most widely used procedure is pterygium excision with conjunctival autograft.23 Superior bulbar conjunctiva has been used widely since the early 1980s and is associated with recurrence rate of approximately 2% to 12% along with few complications.24–26 In the 1980s, Barraquer introduced the concept that removal of Tenon's layer may be important in reducing recurrence rate after pterygium removal as the tenon is the main source of fibroblasts.27 This was also emphasised by Solomon et al who combined this technique with Mitomycin-C application and amniotic membrane transplantation to achieve a low recurrence rate.28 A near zero recurrence rate with a good aesthetic result can be achieved by using Pterygium Extended Removal Followed by Extended Conjunctival Transplantation (P.E.R.F.E.C.T.).29–31 There is no ideal technique for conjunctival autografting which is safe, fast, easy and inexpensive. Various methods such as sutures, fibrin glue, autologous serum and electrocautery have been used for conjunctival autografting.32,33 Surgical steps for pterygium excision with conjunctival autograft that we have adopted at our hospitals under Eastern Regional Eye Care Programme in the eastern part of Nepal are as follows:
Anaesthesia: Peribulbar anaesthesia is preferable over the topical or subconjunctival to avoid pain during operation and to have smooth surgical procedure.
Figure 1.
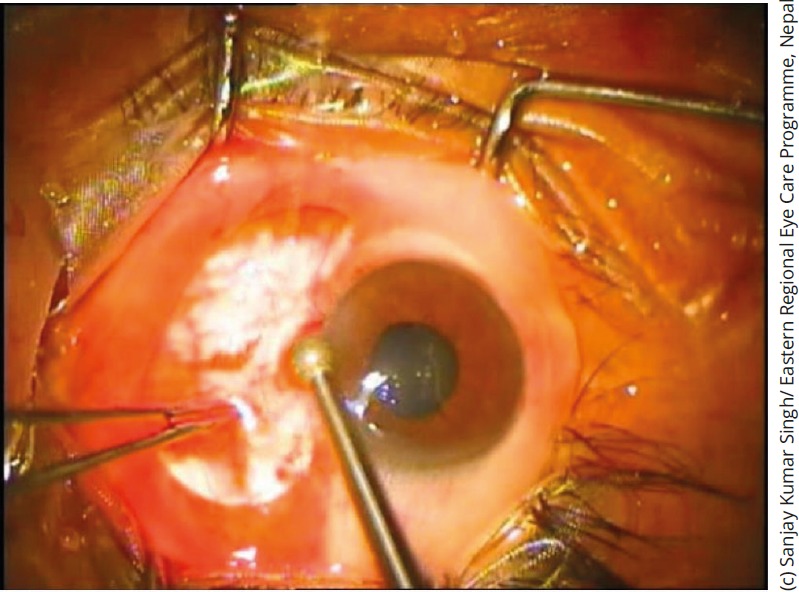
A diamond burr is used for smoothening of corneal surface
Pterygium excision: Pterygium body is excised carefully with conjunctival scissors and the head of pterygium can be removed from cornea by using a 15 degree Bard Parker blade. Tenons and subtenon tissue must be removed carefully as much as possible. Remaining pterygium tissues from over the corneal surface can be removed with a diamond burr.
Conjunctival autograft preparation: The conjunctival defect created by pterygium excision should be measured with a caliper and the superior bulbar conjunctiva should be marked by a marker. It is always preferable to use the marker to create exactly the same size of the graft. After marking, a subconjuctival injection of normal saline, around 2 ml, is injected on the superior bulbar conjunctiva to create the conjunctival balloon. A thin layer of conjunctival graft, devoid of tenons and subtenon tissue is prepared.
Conjunctival grafting: The thin conjunctival graft is placed with correct orientation on the area of the conjunctival defect created by pterygium excision. The marker helps to identify the correct orientation of the graft. The conjunctival graft can be sutured with the 8'0 Vicryl or 10'0 Nylon sutures or can be glued with fibrin glue.
Figure 2.
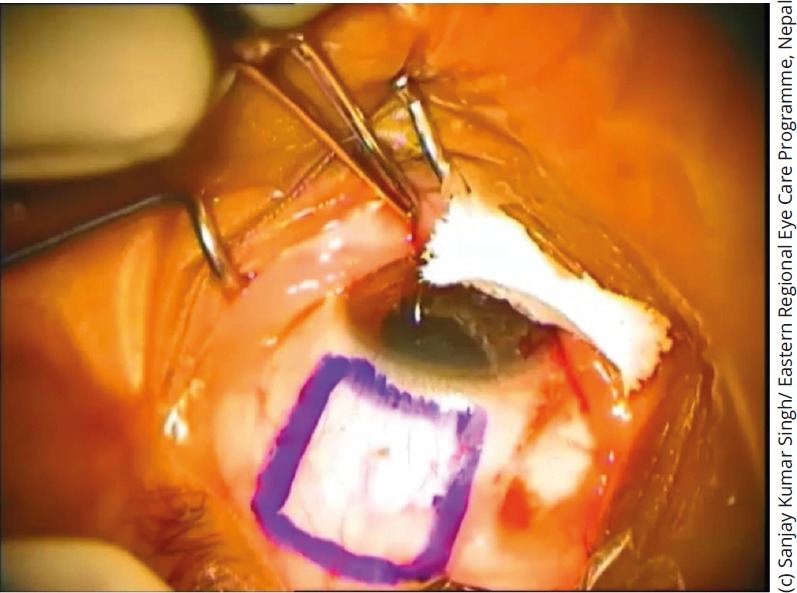
A conjunctival autograph marking
Conjunctival grafting with fibrin glue is a faster procedure and patients complain of less pain in the post-operative period.
Post-operative management: Antibiotic and steroid eye drops are given in tapering doses for one month.
Conclusion
Many ophthalmologists think that pterygium is a trivial condition for which not much time should be expended in surgery and for which the financial remuneration is low.34 But the patients want a cure, free of recurrence with good cosmesis after surgery. Pterygium excision with conjunctival autograft with fibrin glue offers a low recurrence rate, good cosmetic outcome with a reasonable speed of the pterygium surgery.
References
- 1.Detels R, Dhir SP, Pterygium: a geographical study. Arch Ophthalmol. 1967;78: 485–491. [DOI] [PubMed] [Google Scholar]
- 2.McCarty CA, Fu CL, Taylor HR. Epidemiology of Pterygium in Victoria, Australia. Br J Ophthalmology. 2000;84:289–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luthra R, Nemesure BB, Wu SY, et al. Frequency and Risk Factors for Pterygium in the Barbados Eye Study. Arch Ophthalmology. 2001;119:1827–1832. [DOI] [PubMed] [Google Scholar]
- 4.Lu P, Chen X, Kang Y, et al. Pterygium in Tibetans: a population-based study in China. Clin Experiment Ophthalmol. 2007;35:828–833. [DOI] [PubMed] [Google Scholar]
- 5.Lu J, Wang Z, Lu P, et al. Pterygium in an aged Mangolian Population: a population based study in China. Eye (Lond) 2009;23:421–427. [DOI] [PubMed] [Google Scholar]
- 6.Shirma H, Higa A, Sawaguchi S, et al. Prevalence and risk factors of Pterygium in southwestern island of Japan: the Kumejima Study. Am J Ophthalmolo. 2009;148:766–771.e761. [DOI] [PubMed] [Google Scholar]
- 7.Ang M, Li X, Wong W, eta al. Prevalence of and racial differences in pterygium a multiethnic population study in Asians. Ophthalmology. 2012;119:1509–1515. [DOI] [PubMed] [Google Scholar]
- 8.Nemesure B, Wu SY, Hennis A. et al. Nine-year incidence and risk factors for pterygium in the Barbados eye studies. Ophthalmology. 2008;115:2153–2158. [DOI] [PubMed] [Google Scholar]
- 9.Zhao L, You QS, Xu L, et al. 10 year incidence and association of Pterygium in adult Chinese: the Beijing Eye Study. Invest Ophthalmol Vis Science. 2013;54:1509–1514. [DOI] [PubMed] [Google Scholar]
- 10.Lan Li, Hua Zhong, Ermio Tian. et al. Five-Year Incidence and Predictors for Pterygium in a Rural Community in China: The Unnan Minority Eye Study. Cornea. 2015;34:1564–1568. [DOI] [PubMed] [Google Scholar]
- 11.Wong TY, Foster PJ, Johnson GJ, et al. The Prevalence and risk factors for pterygium in an adult Chinese population in Singapore: the Tanjong Pagar survey. Am J Ophthalmol. 2001;131:176–183. [DOI] [PubMed] [Google Scholar]
- 12.Saw SM, Banerjee K, Tan D. Risk factors for the development of pterygium in Singapore: a hospitalbased case control study. Acta Ophthalmol Scand. 2000;78:216–220. [DOI] [PubMed] [Google Scholar]
- 13.Ishioka M, Shimmura S, Yagi Y. et al. Pterygium and dry eye. Ophthalmologica. 2001:215:209–211. [DOI] [PubMed] [Google Scholar]
- 14.Liu T, Liu Y, Xie L, et al. Progress in the pathogenesis of pterygium. Current Eye Res. 2013;38:1191–1197. [DOI] [PubMed] [Google Scholar]
- 15.Coroneo M.T., Di Girolamo N, Wakeeld D. The pathogenesis of pterygia. Current Opinion in Ophthalmology. 1999;10:282–288. [DOI] [PubMed] [Google Scholar]
- 16.Ip Matthew H, Chui Jeanie J, Tat Lien, Coroneo Minas T. Significance of Fuchs Flecks in Patients With Pterygium/Pinguecula: Earliest Indicator of Ultraviolet Light Damage. Cornea. 2015;34:1560–1563. [DOI] [PubMed] [Google Scholar]
- 17.Hirst Lawrence W. The Treatment of Pterygium. Survey of Ophthalmology. 2003;48:2: 145–179. [DOI] [PubMed] [Google Scholar]
- 18.Hirst Lawrence W. Prospective Study of Primary Pterygium surgery using Pterygium Extended Removal Followed by Extended Conjunctival Transplantation. Ophthalmology. 2008;115:1663–1672. [DOI] [PubMed] [Google Scholar]
- 19.Simsek T, Gunlap I, Atilla H. Comparative efficacy of beta irradiation and mitomycin-C in primary and recurrent pterygium. Eur J Ophthalmol. 2001;11:126–132. [DOI] [PubMed] [Google Scholar]
- 20.Dougherty PJ, Hardten DR, Lindstrom RL. Corneoscleral melt after pterygium surgery using a single intraoperative application of mitomycin-C. Cornea. 1996;15:537–540. [PubMed] [Google Scholar]
- 21.Ma DH, See LC, Liau SB, Tsai RJ. Amniotic Membrane graft for primary pterygium: comparison with conjunctival autograft and topical mitomycin C treatment. Br J Ophthalmol. 2000;84:973–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Essex RW, Snibson GR, Daniell M, Tole DM. Amniotic membrane grafting in the surgical management of primary pterygium. Clin. Experiment Ophthalmol. 2004;32:501–504. [DOI] [PubMed] [Google Scholar]
- 23.Kenyon KR, Wagoner MD, Hettinger ME. Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology. 1985;92:1461–1470. [DOI] [PubMed] [Google Scholar]
- 24.Young AL, Leung GY, Wong AK. et al. A randomized trial comparing 0.02% mitomycin-C and limbal conjunctival autograft after excision of primary pterygium. Br J Ophthalmol. 2004;88:995–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mejia LF, Sanchez JG, Escobar H. Management of primary pterygia using free conjunctival and limbalconjunctival autografts without antimetabolites. Cornea. 2005;24:972–975. [DOI] [PubMed] [Google Scholar]
- 26.Fernandes M, Sangwan VS, Bansal AK. et al. Outcome of pterygium surgery: analysis over 14 years. Eye. 2005;19:1182–1190. [DOI] [PubMed] [Google Scholar]
- 27.Barraquer JI. Etiology, pathogenesis and treatment of the pterygium. Trans New Orleans Acad Ophthalmol. 1980;167–178. [Google Scholar]
- 28.Solomon A, Pires RT, Tseng SC. Amniotic membrane transplantation after extensive removal of primary and recurrent pterygia. Ophthalmology. 2001;108:449–460. [DOI] [PubMed] [Google Scholar]
- 29.Hirst LW. Prospective study of Primary Pterygium Surgery using Pterygium Extended Removal Followed by Extended Conjunctival Transplantation. Ophthalmology. 2008;115:1663–1672. [DOI] [PubMed] [Google Scholar]
- 30.Hirst LW. Cosmesis after Pterygium extended removal followed by extended conjunctival transplantation as assessed by a new, web-based grading system. Ophthalmology. 2011;118:1739–1746. [DOI] [PubMed] [Google Scholar]
- 31.Hirst LW. Pterygium Extended Removal Followed by Extended Conjunctival Transplantation: But on which eye? Cornea. 2013;32:799–802. [DOI] [PubMed] [Google Scholar]
- 32.Ratnalingam Vanitha, Keat Eu Andrew Lim, Leong Gem. et al. Fibrin Adhesive is Better Than Sutures in Pterygium Surgery. Cornea. 2010;29:485–489. [DOI] [PubMed] [Google Scholar]
- 33.Fan Xu, Min Li, Yumei Yan. et al. A Novel Technique of Sutureless and Glueless Conjunctival Autografting in Pterygium Surgery by Electrocautery Pen. Cornea. 2013;32:290–295. [DOI] [PubMed] [Google Scholar]
- 34.Essex RW, Snibson GR, Daniell M. et al. Amniotic Membrane grafting in the surgical management of primary pterygium. Clin Experiment Ophthalmol. 2004;32:501–504. [DOI] [PubMed] [Google Scholar]


