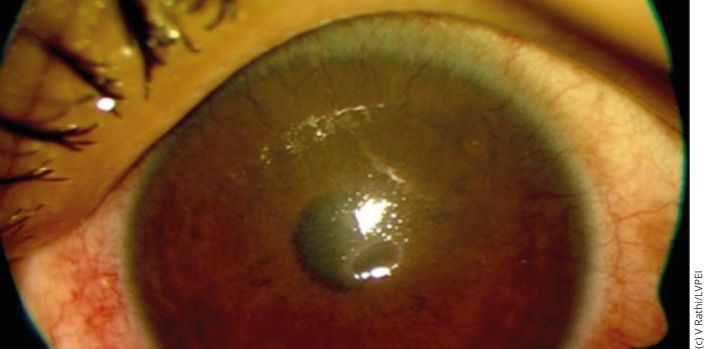
Roughness of epithelium as seen in shield ulcer

Varsha M Rathi

Somasheila I Murthy
The diagnosis of allergic diseases has increased in the last few decades and allergic conjunctivitis has emerged as a significant problem, which can cause severe ocular surface disease. Patients complain of itching, watering and redness. It can result in decreased quality of life, as patients with severe symptoms, if left untreated or treated poorly, may become school dropouts, unable to work outdoors and sometimes fail to sleep. The symptoms are aggravated by exposure to dry and windy climates.1,2 This article aims to provide a brief overview of the management of allergic conjunctivitis. The most important symptom of allergic conjunctivitis is itching. Table 1 lists spectrum of disorders of allergic conjunctivitis.3
Epidemiology
The diagnosis of allergic conjunctivitis is on the increase. SAC and PAC accounts for 15–20% of cases of allergic conjunctivitis.4 The disease is more common in hot, humid tropical climates.5 VKC has been reported from many Asian countries e.g. Nepal, Pakistan and India.2,6,7 VKC and AKC may cause corneal and ocular surface involvement leading to severe visual loss. Numerous factors such as changing climates, increasing pollution, genetics, cigarette pollutants and occurrence of allergy in early childhood have been proposed as causative agents or risk factors. Signfiicant correlations have been observed with mixed pollen, thresher dust and raw cotton with allergic rhinitis and allergic conjunctivitis.8 Seasonal peak is seen during April to August in patients having VKC.9
Classification
Seasonal allergic conjunctivitis
This condition is common, is seen among all ages and occurs seasonally when pollen is released in May and June. Itching followed by watering and a burning sensation is seen in these patients. Sometimes, it may be associated with a running nose (allergic rhinitis or rhinoconjunctivitis). Patients may complain of sinus pressure behind the eye.
Table 1.
Disorders of allergic conjunctivitis
| Mild allergic conjunctivitis | Severe allergic conjunctivitis | Chronic microtrauma related disorders |
|---|---|---|
| Seasonal conjunctivitis (SAC) | Vernal keratoconjunctivitis (VKC) | Contact lens induced papillaryconjunctivitis (CLPC) |
| Perennial conjunctivitis (PAC) | Atopic keratoconjunctivitis (AKC) | Giant papillary conjunctivitis (GPC) |
Perennial allergic conjunctivitis
PAC has similar signs and symptoms to SAC and as the name suggests it occurs throughout the year. PAC is due to allergy to animal dander, mites and feathers. The frequency of occurrence increases as the age increases.10 The patients have itching, redness and swelling of conjunctiva. Corneal involvement in SAC and PAC is rare.4
Vernal keratoconjunctivitis
VKC is a disease of warm climates and occurs predominantly in young males (8–12 years of age).2,11 Although VKC is more common in children, adults may also have VKC.12,13 It is a bilateral disease and may worsen with exposure to wind, dust and sunlight. These patients may have positive history of asthma or eczema. Patients present with severe itching (rubbing of eyes usually with a knuckle), redness, discharge, and photophobia. The mucus discharge is thread-like. School-going children may drop out from going to school because of severe itching and photophobia.
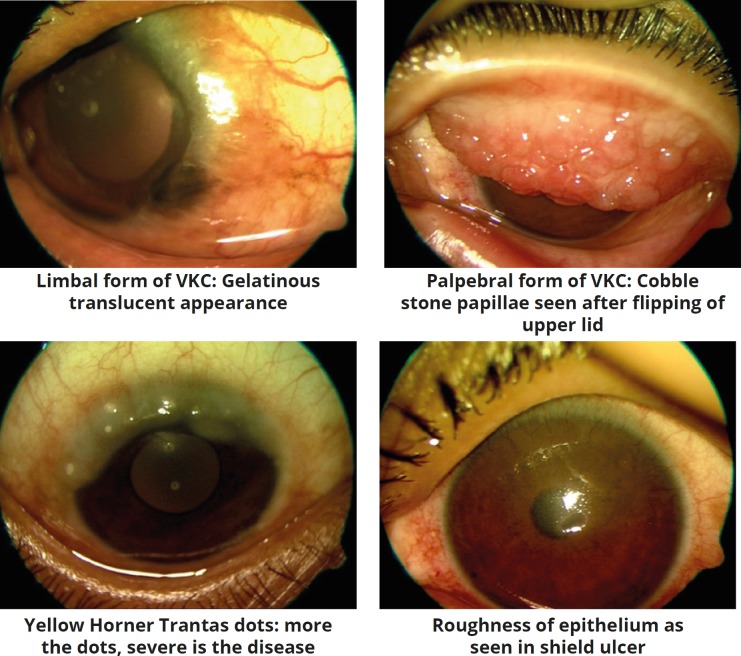
Three clinical forms of VKC are described: limbal or bulbar, palpebral and mixed (Figure 1). Limbal form is more common in dark skinned individuals. In Asia, the mixed form is more common compared to the limbal form, which is seen in Africans.7 However, studies from India and Nepal have reported that the bulbar form of the disease is common in some areas.2,9
Limbal or bulbar form may present as gelatinous thickening of the limbus, presence of papillae at the limbus and yellow Horner-Tranta's dots (Figure 1) usually at the superior limbus. These dots are seen when the disease is active and indicate severity of the disease.
The hallmark of the palpebral VKC is presence of giant papillae, which are seen on everting the upper lid – the giant papillae have a cobble stone appearance (Figure 1). This thickening of the upper lid may be associated with drooping of the lid (ptosis). Conjunctival pigmentation is common in patients having VKC.14
The mixed form of VKC has features of both palpebral and limbal VKC. Corneal involvement in VKC may occur as corneal epithelial punctuate keratitis, and where the epithelial erosions may coalesce and form a vernal or a shield ulcer. Presence of shield ulcer will worsen patients' symptoms and affect vision. These ulcers are oval and are usually present in the upper part of the cornea. The shield ulcers are classified based on the presence of white material at the base of the ulcer. Based on the grades of shield ulcer, the treatment options differ.15
Atopic keratoconjunctivitis
AKC is a bilateral disease of ocular surface and lids, which occurs throughout life. The patients will have eczematous skin lesions of the body. The conjunctiva may have papillae or Trantas dots. Cataract formation can occur in these patients. Table 2 shows the differentiating features of VKC and AKC.
Figure 1.
Clinical forms of VKC: Limbal or bulbar, palpebral and mixed
Table 2.
Differentiating features of vernal and atopic keratoconjunctivitis
| VKC | AKC | |
|---|---|---|
| VKC: vernal keratoconjunctivitis AKC: Allergic keratoconjunctivitis | ||
| Age | Young | Old |
| Sex | Males > Females | Equal ratio |
| Season | Spring | Perennial |
| Duration | Limited | Chronic |
| Skin involvement | No | Yes, extra lid fold, maceration of canthi |
| Punctal stenosis | No | Yes |
| Conjunctiva | Upper tarsal conjunctiva | Lower tarsal conjunctiva |
| Conjunctival scarring | Rare | Common |
| Cornea | Shield ulcer | Epithelial defects |
| Scarring | Peripheral | Central |
| Vascularisation | Rare | Common |
Giant papillary conjunctivitis
The presence of a contact lens, ocular prosthesis or sutures may sensitise and cause trauma to the upper tarsal conjunctiva with the formation of giant papillae. Removal of these external agents will reduce the papillae. Toxic allergic reactions may also be due to drugs such as neomycin, atropine, epinephrine or preservatives in medicines such as thiomersol.16
Contact hypersensitivity reactions
The pattern of involvement depends upon severity of the reaction and the site of contacts. Patients may have lid swelling, redness, chemosis, follicular reaction and later sometimes cicatrisation. The corneal involvement may be in the form of superficial punctate keratitis, pseudodendrites or grayish stromal infiltrates.17
Complications
Most often, the complications are because of poor compliance to treatment on the part of patient, or inadequate control of the disease when it presents in its severe form. Common complications include dry eye, infection and corneal scar. Chronicity of the untreated disease may lead to vision threatening problems like limbal stem cell deficiency (LSCD) and secondary keratoconus due to rubbing of the eyes.
As the treatment involves use of corticosteroids, steroid-induced raised intraocular pressure and cataract have been reported in these patients.7 Complications may lead to irreversible visual loss in some patients.7 Both the complications, keratoconus and LSCD need timely surgical treatment to prevent visual malfunction.
Diagnosis
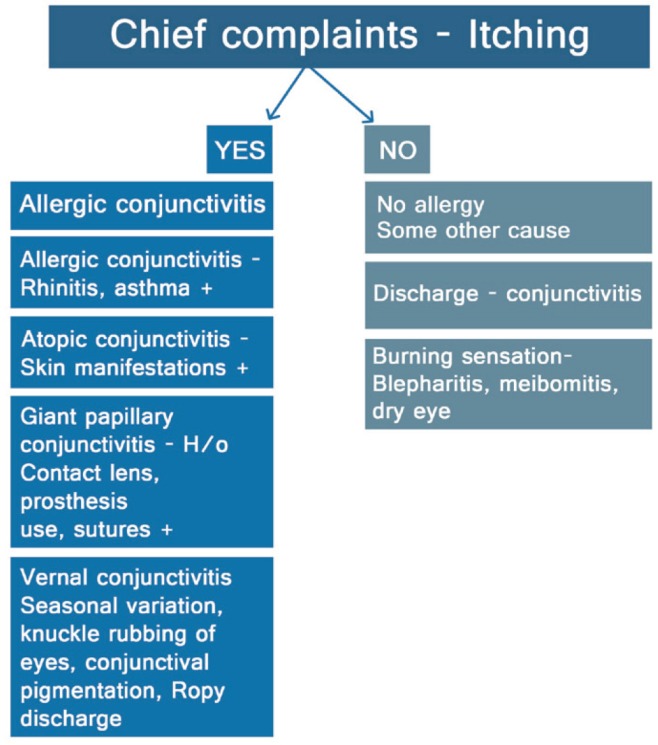
Appropriate management of allergic conjunctivitis needs a correct diagnosis. Figure 2 gives a guide for such diagnosis and ways to differentiate from other causes of red eyes. Presence of itching is a hallmark of ocular allergy.
Management
Though some authors have described management protocols, there are no universally accepted protocols of management for allergic eye diseases.11,12 Various drugs are available and the treatment options vary based on the severity of the disease. It is important to avoid any known allergen or reduce exposure to it by using wrap around glasses, by changing the environment, replacing allergen harbouring items such as pillows and carpets. However, such recommendations may be challenging for patients. In addition, cool compresses can be done to prevent rubbing of the eye. Ocular lubricating eye drops can be used to dilute the inflammatory agents in tears and wash away the allergen to reduce itching and to prevent further worsening of symptoms.19
The mainstay of treatment is the use of lubricants, anti-histamines and mast cell stabilisers.16,20 These are indicated in all forms of disease. Steroids are to be given under proper medical care when the cornea is involved or the disease is very severe with itching.
Overuse of corticosteroids may cause steroid induced cataracts and glaucoma and may result in blindness. The drugs that are used are:
Mast cell stabilisers: disodium cromoglyacate (not effective in acute stages), Nedocromil and Lodoxamide
Antihistamines: ketotifen, dual acting drugs such as olapatadine, azelastine, epinastine and bepostatine. Immediate symptomatic relief is possible with azelastine and epinastine, which are currently preferred.
Corticosteroids: such as prednisolone are given for a short duration during acute allergic disease; oral steroids or supratarsal injection of corticosteroids is required if the disease is severe.
Nonsteroidal anti-inflammatory agents (NSAIDS): ketorolac, diclofenac can be added to antihistamines. Steroid sparing agents such as Cyclosporine A, Tacrolimus are effective in severe AKC and VKC.
Conclusion
From a public health perspective, the number of patients being diagnosed with allergic conjunctivitis is increasing. However, not many studies are available from South East Asia, which give a complete picture of allergic eye disease. Severe conjunctivitis such as VKC, being a disease of the young may increase the number of school dropouts in these countries. Economic costs for patients are high, sometimes necessitating the need for medications to continue for years.21,22 Management of the disease is very challenging and a multipronged approach with well-trained primary and secondary care personnel to educate patients or parents about the disease, especially about good general hygiene; avoidance of allergens; cold compression; change of environment; and judicious use of corticosteroids may improve ocular health in patients by leaps and bounds.
Figure 2.
A guide to aid diagnosis of allergic conjunctivitis
Contributor Information
Varsha M Rathi, Faculty, Tej Kohli Cornea Institute, Gullapalli Pratibha Rao International Center for Advancement of Rural Eye Care, L V Prasad Eye Institute, Hyderabad, India.
Somasheila I Murthy, Faculty, Tej Kohli Cornea Institute, L.V. Prasad Eye Institute, Kallam Anji Reddy Campus, Hyderabad, India.
References
- 1.Bonini S, Bonini S, Lambiase A, Marchi S, Pasqualetti P, Zuccaro O, et al. Vernal keratoconjunctivitis revisited: a case series of 195 patients with long-term followup. Ophthalmology. 2000. Jun;107(6):1157–63. [DOI] [PubMed] [Google Scholar]
- 2.So RA, Mufti A. Vernal Keratoconjunctivitis in Kashmir: A temperate zone. International ophthalmology. 2016. Dec;36(6):875–879. Epub 2016 Mar 10. [DOI] [PubMed] [Google Scholar]
- 3.Ehlers WH, Donshik PC. Allergic ocular disorders: a spectrum of diseases. The CLAO journal: official publication of the Contact Lens Association of Ophthalmologists, Inc. 1992. Apr;18(2):117–24. [PubMed] [Google Scholar]
- 4.La Rosa M, Lionetti E, Reibaldi M, Russo A, Longo A, Leonardi S, et al. Allergic conjunctivitis: a comprehensive review of the literature. Italian journal of pediatrics. 2013;39:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buckley RJ. Vernal keratoconjunctivitis. International ophthalmology clinics. 1988. Winter;28(4):303–8. [DOI] [PubMed] [Google Scholar]
- 6.Pokharel N, Shah DN, Choudhary M. Vernal keratoconjunctivitis: modes of presentation in Nepalese population. Kathmandu University medical journal. 2007. Oct-Dec;5(4):526–30. [PubMed] [Google Scholar]
- 7.Saboo US, Jain M, Reddy JC, Sangwan VS. Demographic and clinical prole of vernal keratoconjunctivitis at a tertiary eye care center in India. Indian journal of ophthalmology. 2013. Sep;61(9):486–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed A, Minhas K, Micheal S, Ahmad F. Prevalence of skin test reactivity to aeroallergens in the Pakistani population. Public health. 2011. May;125(5):324–6. [DOI] [PubMed] [Google Scholar]
- 9.Kansakar I. Prole of vernal keratoconjunctivitis in Nepal: a hospital based study. Nepal Medical College journal: NMCJ. 2011. Jun;13(2):92–5. [PubMed] [Google Scholar]
- 10.Leonardi A, Piliego F, Castegnaro A, Lazzarini D, La Gloria Valerio A, Mattana P, et al. Allergic conjunctivitis: a cross-sectional study. Clinical and experimental allergy: journal of the British Society for Allergy and Clinical Immunology. 2015. Jun;45(6):1118–25. [DOI] [PubMed] [Google Scholar]
- 11.Katelaris CH. Ocular allergy in the Asia Pacic region. Asia Pacific allergy. 2011. Oct;1(3):108–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ukponmwan CU. Vernal keratoconjunctivitis in Nigerians: 109 consecutive cases. Tropical doctor. 2003. Oct;33(4):242–5. [DOI] [PubMed] [Google Scholar]
- 13.De Smedt S, Wildner G, Kestelyn P. Vernal keratoconjunctivitis: an update. The British journal of ophthalmology. 2013. Jan;97(1):9–14. [DOI] [PubMed] [Google Scholar]
- 14.Rao SK, Padmanabhan P. Perilimbal conjunctival pigmentation in vernal keratoconjunctivitis: a new sign. Cornea. 2002. May;21(4):432. [DOI] [PubMed] [Google Scholar]
- 15.Cameron JA. Shield ulcers and plaques of the cornea in vernal keratoconjunctivitis. Ophthalmology. 1995. Jun;102(6):985–93. [DOI] [PubMed] [Google Scholar]
- 16.Schmid KL, Schmid LM. Ocular allergy: causes and therapeutic options. Clinical & experimental optometry. 2000. Sep-Oct;83(5):257–70. [DOI] [PubMed] [Google Scholar]
- 17.Dart J. Corneal toxicity: the epithelium and stroma in iatrogenic and factitious disease. Eye. 2003;17(8):886–92. [DOI] [PubMed] [Google Scholar]
- 18.Kok YO, Tan GF, Loon SC. Review: keratoconus in Asia. Cornea. 2012. May;31(5):581–93. [DOI] [PubMed] [Google Scholar]
- 19.Hingorani M, Lightman S. Therapeutic options in ocular allergic disease. Drugs. 1995. Aug;50(2):208–21. [DOI] [PubMed] [Google Scholar]
- 20.Gokhale NS. Systematic approach to managing vernal keratoconjunctivitis in clinical practice: Severity grading system and a treatment algorithm. Indian journal of ophthalmology. 2016. Feb;64(2):145–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pitt AD, Smith AF, Lindsell L, Voon LW, Rose PW, Bron AJ. Economic and quality-of-life impact of seasonal allergic conjunctivitis in Oxfordshire. Ophthalmic epidemiology. 2004. Feb;11(1):17–33. [DOI] [PubMed] [Google Scholar]
- 22.Gupta R, Sheikh A, Strachan DP, Anderson HR. Burden of allergic disease in the UK: secondary analyses of national databases. Clinical and experimental allergy: journal of the British Society for Allergy and Clinical Immunology. 2004. Apr;34(4):520–6. [DOI] [PubMed] [Google Scholar]