Abstract
Background:
A substantial proportion of euthymic bipolar disorder patients have neuropsychological impairment which can have a significant impact on the overall functional recovery.
Materials and Methods:
A total of 60 bipolar disorder patients, currently in euthymic phase for the last 3 months with minimum duration of illness 2 years and current Young Mania Rating Scale <7 and Hamilton Depression Rating Scale <6, currently on medications were administrated various neuropsychological tests.
Results:
Approximately half of the patients have neuropsychological impairments in the areas of mental speed, sustained attention, verbal fluency, working memory, set shifting, verbal and visual memory, and visual-constructional ability.
Conclusion:
Findings of the current study provides evidence of neuropsychological impairment in euthymic bipolar disorder patients, and type of medications also has an impact on neuropsychological functions.
Key words: Bipolar, euthymic, functioning, neuropsychological
INTRODUCTION
Bipolar affective disorder (BPAD) is a chronic mood disorder characterized by repeated (i.e., at least two) episodes in which mood and activity levels are significantly disturbed.[1] Euthymic phase in BPAD is defined as normal range of mood, implying the absence of depressed or elevated mood. Symptoms in euthymic phase are not entirely absent but are subdued enough, so that mood and normal activity are not affected to a great extent.[2] Treatment of BPAD includes the conventional mood stabilizers (e.g., lithium, valproate, lamotrigine, and carbamazepine) and some of the atypical antipsychotics. Originally, it was thought that while in a euthymic mood state, a patient with BPAD had no impairment and experienced a return to normal functioning.[3] This may not hold true as patients with BPAD in a euthymic state experience difficulties in various domains of social and occupational functioning.[4] Neurocognitive deficits are impairments in cognitive ability that is closely linked to the functioning of specific brain areas, neural pathways, or cortical networks. Research in this area has found that neurocognitive deficits are characteristic of many psychiatric disorders and that they are present in addition to the more typical symptoms of a disorder.[5,6] Some of the deficits seem to be affected by the mood state the patient is experiencing, while others continue through periods where the patient is generally asymptomatic or euthymic.[5,7] During euthymic mood states, patients with BPAD continue to show deficits in executive functioning, verbal and visual memory, and sustained attention.[3,8] These deficits, which are present during asymptomatic states, may be trait-like characteristics of the disorder.
In fact, 40%–60% of euthymic patients present with neurocognitive disturbances[9] and which may affect the everyday activities, patients' ability to work and causes delay in reemployment. Therefore, neurocognition clearly has an important role in functional outcomes of BPAD patients.
In addition, lithium that constitutes the gold standard in long-term prophylactic treatment is involved in the determination of the cognitive dysfunction in BPAD patients, even if changes were relatively modest, reversible, and occur only in some areas of cognitive performance. Lithium can cause working memory deficits that may correlate with executive dysfunction in the frontal structures.[10] Valproate is associated with mild memory and attention impairments, reductions in verbal memory, and increased decision time.[10]
Hence, there is need to address this issue as most of the studies have focused on neuropsychological deficits in subjects during an episode, and very few studies have examined neuropsychological deficits in euthymic patients. Very limited numbers of studies are available to comment on neuropsychological functions in Indian patients, with BPAD during euthymic phase.
MATERIALS AND METHODS
Study design
The current study was an exploratory, single group, cross-sectional, and exploring the nature of neuropsychological functioning in euthymic phase of BPAD patients and further exploring the predictors of neuropsychological functioning in euthymic phase of BPAD. Patients in euthymic phase of BPAD for at least 3 months with minimum 2 years of illness duration in age group of 18–55 years of any gender, Hamilton Depression Rating Scale (HAM-D)[11]<6 and Young Mania Rating Scale (YMRS)[12]<7 and those who gave informed consent were inducted. Patients with cerebrovascular disease, neurodegenerative disorders, head injury with concussion, epilepsy, idiopathic Parkinsonism, systemic illness, any other organic disease, intellectual disability, received electroconvulsive therapy during the past 3 months, or change or addition of new psychotropics in the past 3 months, had a history of substance dependence except nicotine and caffeine were not included in the study.
Procedure
A total of 86 patients of BPAD were screened, and out of which, 60 patients met the study criteria and were enrolled in the study. The patients' samples vary with respect to the duration of illness, number of episodes, and types of medications. At the time of selection and assessment for study, all patients were on medication, and maximum numbers of patients were on lithium. Sociodemographic profile and history regarding clinical factors were recorded on a semi-structured pro forma used in the Department of Psychiatry, Government Medical College and Hospital, India. HAM-D,[11] YMRS,[12] and standardized neuropsychological tests from the National Institute of Mental Health and Neuro-Sciences (NIMHANS) Neuropsychological Battery-2004[13] were applied. Average functions defined as scores obtained are equal to and above 25 percentile as per age, gender, education norms of NIMHANS Neuropsychological Battery 2004.[13] Below average functions defined as scores obtained are within 15–25 percentile as per age, gender, and education norms of NIMHANS Neuropsychological Battery 2004.[13] Deficit functions defined as scores obtained are <15 percentile as per age, gender, and education norms of NIMHANS Neuropsychological Battery 2004.[13]
Statistical analysis
Descriptive and inferential statistical methods were used with the help of Statistical Package for Social Sciences (SPSS) version 22.0 (IBM Corp, Armonk, NY). Mean and standard deviation were used for demographic variables, frequency, and percent to explore the nature of neuropsychological functioning and Pearson's correlation was used to study the relationship of clinical factors with neuropsychological functioning. The trial was registered with Clinical Trial Registry-India and CTRI Reg. No. is CTRI/2017/03/008268.
The confidentiality of the information obtained was maintained, and the principles enunciated in the declaration of Helsinki were complied with. ICMR's ethical guidelines for biomedical research on human subjects were adhered to.
The study was approved by the local Institutional Ethics Committee.
RESULTS
Sociodemographic and clinical parameters showed that mean age of all 60 patients is 38.75 years. Mean education in years is 11.62. Out of total sample, majority of the patients were male (70%), married (75%), and employed (58.3%). Mean duration of illness was 10.77 years with minimum 2 and maximum 29 years. Mean no. of episodes was 4.10 with minimum 2 and maximum 10. Mean number of hospitalizations was 4.10 with minimum 0 and maximum 5. Mean no. of suicide attempts was 0.40 with minimum 0 and maximum 2. Mean HAM-D scores in study subjects are 0.45 with minimum 0 and maximum 4. Mean YMRS scores in study participants are 0.68 with minimum 0 and maximum 3.
All 60 patients were on medication, maximum number of patients was on lithium, 51.7%, followed by 30% who were on combination of lithium, valproate, and atypical antipsychotics, 11% were on lithium and atypical antipsychotic as shown in Table 1.
Table 1.
Clinical factor distribution in study group
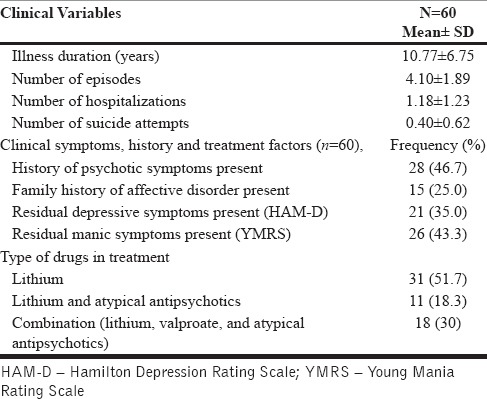
Out of 60 subjects, 28 (46.7%) have a positive history of psychotic symptoms, and 15 (25%) have a positive family history of affective disorder. A total of 21 (35%) have residual depressive symptoms, and 26 (43.3%) have residual manic symptoms.
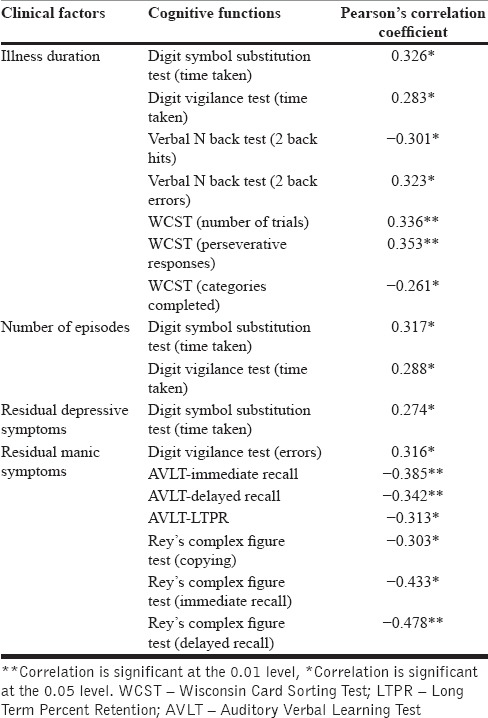
Table 2 shows that illness duration has a significant correlation with psychomotor performance, sustained attention, and set shifting. Number of episodes has significant correlation with psychomotor performance and sustained attention. Residual depressive symptoms have significant correlation with psychomotor performance. Residual manic symptoms have significant correlation with sustained attention, verbal learning and memory, visuospatial and construction ability, and visual learning and memory.
Table 2.
Relationship between clinical factors and cognitive functions
This study showed deficits in neuropsychological functioning in euthymic phase of BPAD in psychomotor performance, attention, executive function, verbal learning and memory, visuospatial and construction ability, and visual learning and memory. In addition, it showed the correlation of clinical factors (illness duration, number of episodes, and residual depressive and manic symptoms) with neuropsychological functioning.
DISCUSSION
In the present study, mental speed, sustained attention, verbal fluency, working memory, set shifting, verbal and visual memory, and visual-constructional ability were assessed and found to be affected in almost half of the patients as shown in Table 3 and Figure 1 and which is similar to other study[9] and suggests that this illness has a significant impact in the development of neuropsychological dysfunctions. On the other hand, response inhibition ability was less affected in these patients.
Table 3.
Neuropsychological functioning in euthymic bipolar affective disorder patients
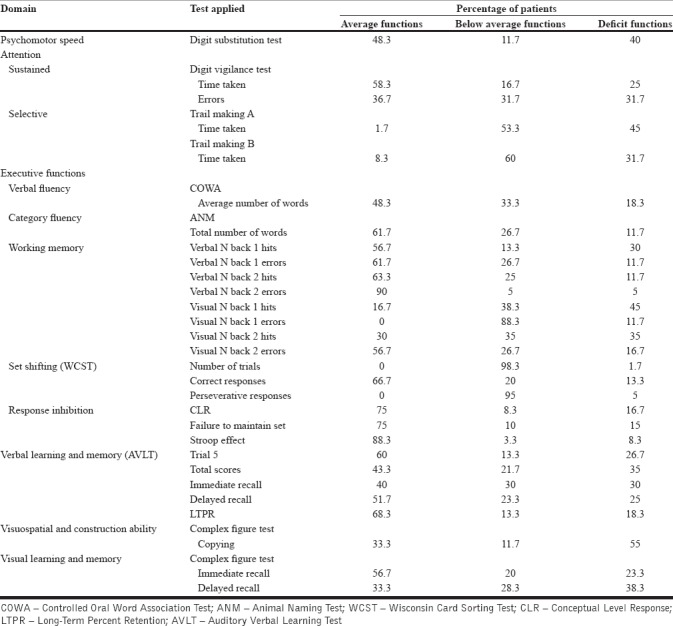
Figure 1.
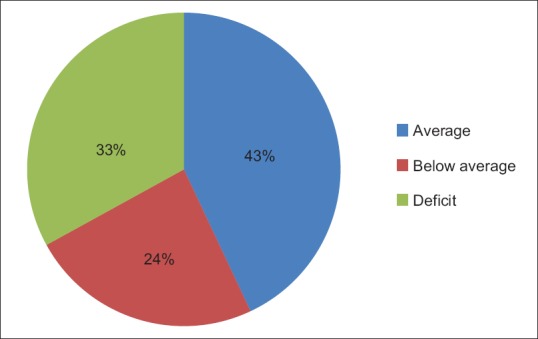
Overall neuropsychological functioning of euthymic patients in bipolar affective disorder
These impairments may have multifactorial causes; therefore, clinical factors such as illness duration, medication use, type and doses of medication, number of episodes, etc., may also contribute to the neuropsychological dysfunctions.
It is evident that illness duration was significantly associated with the mental speed, and set-shifting ability in these individuals whereas the number of episodes was significantly associated with mental speed and attention ability of these individuals.
Further, residual depressive symptoms were significantly associated with mental speed only whereas residual manic symptoms were significantly correlated with sustained attention, verbal learning and memory, and visual memory and visual-constructional ability in these patients in this study. These findings replicate those of some previous studies.[14,15] However, these findings do not match with other previous studies.[14,16,17,18,19,20] Difference in the present study as compared to the previous studies regarding these findings can be attributed to difference in the duration of illness, difference in euthymic phase duration, difference in cutoff for HAM-D and YMRS, difference in sample size, inclusion of comparison group in previous studies, and difference in age, gender, and occupation of subjects.
Further studying the impact of drugs on neuropsychological functioning; sample was divided into three groups, i.e., lithium alone, lithium plus atypical antipsychotic (Li + AAPD) and combination group consisting of lithium plus valproate plus atypical antipsychotic drug. Results are presented in Table 4, in which it was found that response inhibition dysfunctions were significantly higher in the lithium + atypical antipsychotic group in comparison to lithium alone and combination of valproate, lithium, and atypical antipsychotic group, suggestive of significant impact of the specific drugs on specifically on the response inhibition ability in these patients. These findings are consistent with the findings of a study done in 2016.[21]
Table 4.
Role of medication in the cognitive functioning of patients with bipolar affective disorder in euthymic phase
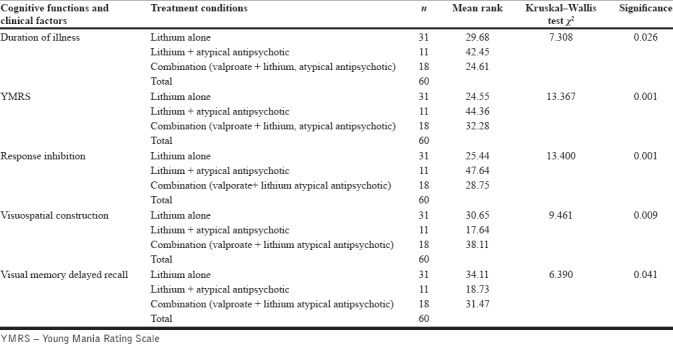
Further, visual-constructional ability is more affected in the combination group followed by lithium alone group and less affected in the Li + AAPD group, indicative of visual-motor coordination problems are much more in different combination of drugs. These findings are inconsistent with the previous study in which worsening of early visual processing was found to be associated with lithium.[22]
Visual memory was significantly more affected in the lithium alone group followed by combination group and was lesser in the Li + AAPD. This suggests that visual memory is highly sensitive to be affected by the lithium. These findings are inconsistent with the previous studies.[21,22]
Further to discuss that these dysfunctions were affected by illness-related factors also, as illness duration and YMRS scores were higher in the Li + AAPD group compare to the other groups. Hence, it indicates that those patients who had longer duration of illness and had more manic episodes and are on Li + AAPD have increased chances to develop response inhibition neuropsychological dysfunctions compare to others. Whereas visual construction dysfunction is more related with combinations of drugs and visual memory is related to lithium alone in this study.
CONCLUSION
The findings of the current study showed that the around half of euthymic bipolar disorder patients have some kind of neuropsychological impairments. Duration of illness, number of episodes, residual manic and depressive symptoms, and combination of medicines have a significant impact on neuropsychological functions. Hence, one should also focus on neuropsychological functioning while planning the pharmacological interventions for complete functional recovery in bipolar patients. The association of clinical factors with cognitive deficits showed in this study can help in predicting and segregating high-risk population for poor functional recovery and starts early initiation of cognitive remediation.
Since, this is a cross-sectional assessment and which was done on a single group only. In the future, longitudinal study with multiple assessments can be planned to study the effect of course of illness and to refine assessments further, and it can be coupled with neuroimaging to associate target area in the brain with deficits.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
- 2.Euthymia Definition in Bipolar Disorder. [Last accessed on 2014 Oct 30]. Available from: http://www.bipolar.about.com/od/glossaryef/g/gl_euthymia.htm .
- 3.Bello DT. Thesis (Philosophy) New York University; 2009. Neurocognitive Deficits and Functional outcome in Bipolar Disorder, Degree in Psychology. [Google Scholar]
- 4.Gitlin MJ, Swendsen J, Heller TL, Hammen C. Relapse and impairment in bipolar disorder. Am J Psychiatry. 1995;152:1635–40. doi: 10.1176/ajp.152.11.1635. [DOI] [PubMed] [Google Scholar]
- 5.Bearden CE, Hoffman KM, Cannon TD. The neuropsychology and neuroanatomy of bipolar affective disorder: A critical review. Bipolar Disord. 2001;3:106–50. doi: 10.1034/j.1399-5618.2001.030302.x. [DOI] [PubMed] [Google Scholar]
- 6.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–30. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 7.Murphy FC, Sahakian BJ. Neuropsychology of bipolar disorder. Br J Psychiatry Suppl. 2001;41:s120–7. [PubMed] [Google Scholar]
- 8.Lima FM, Czepielewski LS, Gama CS, Kapczinski F, Rosa AR. Cognitive and psychosocial impairment in remitted bipolar patients. Psicodebate. 2014;14:25–38. [Google Scholar]
- 9.Sole B, Bonnin CM, Torrent C, Martinez-Aran A, Popovic D, Tabarés-Seisdedos R, et al. Neurocognitive impairment across the bipolar spectrum. CNS Neurosci Ther. 2012;18:194–200. doi: 10.1111/j.1755-5949.2011.00262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quraishi S, Frangou S. Neuropsychology of bipolar disorder: A review. J Affect Disord. 2002;72:209–26. doi: 10.1016/s0165-0327(02)00091-5. [DOI] [PubMed] [Google Scholar]
- 11.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 13.Rao SL, Subbakrishnan DK, Gopulkumar K. National Institute of Mental Health and Neurosciences Neuropsychology Battery. Banglore: 2004. [Google Scholar]
- 14.Torrent C, Martinez-Arán A, del Mar Bonnin C, Reinares M, Daban C, Solé B, et al. Long-term outcome of cognitive impairment in bipolar disorder. J Clin Psychiatry. 2012;73:e899–905. doi: 10.4088/JCP.11m07471. [DOI] [PubMed] [Google Scholar]
- 15.Ferrier IN, Chowdhury R, Thompson JM, Watson S, Young AH. Neurocognitive function in unaffected first-degree relatives of patients with bipolar disorder: A preliminary report. Bipolar Disord. 2004;6:319–22. doi: 10.1111/j.1399-5618.2004.00122.x. [DOI] [PubMed] [Google Scholar]
- 16.Martínez-Arán A, Vieta E, Colom F, Torrent C, Sánchez-Moreno J, Reinares M, et al. Cognitive impairment in euthymic bipolar patients: Implications for clinical and functional outcome. Bipolar Disord. 2004;6:224–32. doi: 10.1111/j.1399-5618.2004.00111.x. [DOI] [PubMed] [Google Scholar]
- 17.Martínez-Arán A, Vieta E, Reinares M, Colom F, Torrent C, Sánchez-Moreno J, et al. Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am J Psychiatry. 2004;161:262–70. doi: 10.1176/appi.ajp.161.2.262. [DOI] [PubMed] [Google Scholar]
- 18.Thompson JM, Gallagher P, Hughes JH, Watson S, Gray JM, Ferrier IN, et al. Neurocognitive impairment in euthymic patients with bipolar affective disorder. Br J Psychiatry. 2005;186:32–40. doi: 10.1192/bjp.186.1.32. [DOI] [PubMed] [Google Scholar]
- 19.Rodríguez L, de la Vega I, Torrijos S, Barabash A, Ancín I, Peláez JC, et al. A study of verbal memory in a sample of euthymic patients with bipolar disorder. Actas Esp Psiquiatr. 2012;40:257–65. [PubMed] [Google Scholar]
- 20.Bourne C, Bilderbeck A, Drennan R, Atkinson L, Price J, Geddes JR, et al. Verbal learning impairment in euthymic bipolar disorder: BDI v BDII. J Affect Disord. 2015;182:95–100. doi: 10.1016/j.jad.2015.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sabater A, García-Blanco AC, Verdet HM, Sierra P, Ribes J, Villar I, et al. Comparative neurocognitive effects of lithium and anticonvulsants in long-term stable bipolar patients. J Affect Disord. 2016;190:34–40. doi: 10.1016/j.jad.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 22.Pfennig A, Alda M, Young T, MacQueen G, Rybakowski J, Suwalska A, et al. Prophylactic lithium treatment and cognitive performance in patients with a long history of bipolar illness: No simple answers in complex disease-treatment interplay. Int J Bipolar Disord. 2014;2:1. doi: 10.1186/s40345-014-0016-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


