Abstract
Background:
Polycystic ovarian syndrome (PCOS) is the most common endocrine disorder among women of reproductive age. Symptoms include amenorrhea, hirsutism, infertility, obesity, acne vulgaris, and androgenic alopecia. PCOS is a stigmatizing condition that affects a woman's identity, mental health and quality of life (QOL). This aspect has not received adequate attention in India.
Aims and Objectives:
(1) To study the prevalence of anxiety and depression among women suffering from PCOS (2) To determine if symptoms of PCOS were associated with psychiatric morbidity, and (3) To determine the impact of psychiatric morbidity on the QOL.
Materials and Methods:
Seventy females in the reproductive age group (18–45 years) diagnosed with PCOS as per Rotterdam criteria and without any preexisting psychiatric illness were clinically interviewed for anxiety and depressive disorders which were then rated according to the Hamilton scales. QOL was assessed using the World Health Organization-QOL-BREF. Binary logistic regression was performed to study the association of the symptoms with the psychiatric morbidity. QOL scores of patients with and without psychiatric morbidity were compared using Mann–Whitney U-test.
Results and Conclusions:
The prevalence of anxiety and depression in our sample was 38.6% and 25.7%, respectively. Infertility and alopecia were associated with anxiety, while acne was associated with depression. Hirsutism was associated with a lower psychological QOL. Patients with psychiatric morbidity had a significantly lower QOL than those without.
Key words: Anxiety, depression, polycystic ovarian syndrome, quality of life, symptomatology
INTRODUCTION
Polycystic ovarian syndrome (PCOS) is the most common endocrine disorder among women of reproductive age, affecting approximately 5%–10% of women in the Western world.[1] The Indian Fertility Society reported a prevalence of 3.7%–22.5% in India.[2] Women with PCOS exhibit a wide range of symptoms such as amenorrhea, oligomenorrhea, hirsutism, subfertility or infertility, anovulation, weight gain or obesity, acne vulgaris, and androgenic alopecia.[1]
They also experience higher rates of depression and anxiety than women in the general population.[3] Therefore, international[4] as well as Indian[2] guidelines suggest that psychological factors must be considered in all women with PCOS and they must be screened for anxiety and depression.[2] Yet, a literature search revealed only four published Indian studies on this subject.
Two of those studies had only assessed the prevalence of anxiety and depressive disorders among women with PCOS and had found a prevalence of 28% and 39% for anxiety and 11% and 25% for depression.[5,6] The study done by Sundararaman et al. in 2008[7] had determined psychological distress in these patients on the General Health Questionnaire and found it to be significantly related to obesity, infertility, acne, and hirsutism. On the other hand, a 2010 study by Bhattacharya and Jha[8] assessed the impact of four symptoms, namely, obesity, acne, hirsutism, and acanthosis, only on depression, and found no significant association between the variables. These findings are in stark contrast to each other.
No systematic study on anxiety has been conducted in India so far, although there is evidence that anxiety is a significant issue in PCOS.[3]
International research has shown that PCOS has an adverse effect on the patient's quality of life (QOL).[4] Globally, there has been an increasing focus on this aspect because it is a reflection of the true impact of the condition on the patients' lives.[4] The Indian perspective on the QOL in PCOS is completely unexplored.
The current understanding in the management of PCOS is that, it is paramount to understand the symptoms from the patient's perspective. We need to gain information as to which symptoms are likely to cause the maximum impact, so that novel therapies can be targeted toward improving the overall outcome in each patient.[4] The Indian literature on psychological aspects of PCOS is inconclusive and inconsistent. This gap in knowledge is of concern, given the high prevalence of PCOS and the physical and psychological burden the disease appears to place on women.
The need for this study is therefore obvious. To the best of our knowledge, this is one of the very few comprehensive Indian studies that focus on anxiety and depressive disorders among women with PCOS with emphasis on the symptomatology and QOL.
Aims and objectives
To study the prevalence of anxiety and depression among outpatients suffering from PCOS
To determine if any specific symptoms of PCOS are associated with psychiatric morbidity
To compare the QOL in the patients with and without psychiatric morbidity.
MATERIALS AND METHODS
Sample selection
Following approval from the Ethics Committee of the Hospital, the study was conducted for 1 year at Department of Psychiatry in coordination with the Department of Obstetrics and Gynaecology at a Government Hospital in Mumbai. The patients included government employees or their family members who are covered under a contributory health scheme. The design of the study was cross-sectional.
The prevalence of PCOS in India has varied from 3.7% to 22.5% across Indian studies,[2] so it was assumed at 23% for the purpose of this study. A confidence level of 95% and a 10% margin of error were finalized upon. The formula used to calculate sample size was n = z2 × p (1−p)/ε2, wherein Z-score for a confidence level of 95% is 1.96. The desired sample size was 68 which was rounded up to 70. Thus, consecutive patients with a diagnosis of PCOS as per Rotterdam criteria[9] were taken up for symptom evaluation as per the endocrine society guidelines at the Gynaecology outpatient department. They were then referred to the Psychiatry outpatient department where they were considered for any exclusion criteria. For the study, 70 consecutive patients aged 18–45 years were enrolled after due informed consent. Convenience sampling was used.
Inclusion criteria
-
Patients diagnosed with PCOS as per Rotterdam criteria
- Oligoovulation and/or anovulation
- Hyperandrogenism
- Polycystic ovaries
Adult female patients in the reproductive age group (18–45 years)
Patients willing to give informed consent.
Exclusion criteria
Patients who have consulted a psychiatrist or are already diagnosed as having a mental illness by self-report on history and perusal of past medical records
Patients having a concurrent, significant medical illness.
Instruments
The sociodemographic variables were collected using a specially designed semi-structured pro forma. The current mental health was assessed with a history and mental status examination. International classification of diseases-10[10] was used for diagnosis of psychiatric disorders
Hamilton Depression Rating Scale[11]
Hamilton Anxiety Rating Scale[12]
World Health Organization (WHO) QOL-BREF Scale.[13]
Statistical analysis
The data were pooled and statistically analyzed using IBM SPSS 20 Software. The sociodemographic profile and the prevalence of the different symptoms of PCOS, anxiety, and depression have been expressed in terms of frequency and percentages. Binary logistic regression analysis was performed to ascertain the effects of the symptoms of PCOS on the likelihood that the females suffered from anxiety and/or depression. The dependent variables were anxiety and depression that were dichotomous, that is, present and absent. All the symptoms of PCOS were entered as predictor variables. The scores on QOL have been expressed as mean, standard deviation, and median. Shapiro–Wilk test was performed, and they were not found to be normally distributed. Hence, the mean scores on these domains were compared using the nonparametric Mann–Whitney U-test.
RESULTS
Seventy-five consecutive patients diagnosed with PCOS at the Department of Gynaecology were referred for evaluation. Seventy patients consented to be enrolled in the study. Thus, a total of 70 females in the age group of 18–45 years were studied. The mean age of the sample was 27.65 ± 7.60 years.
Sociodemographic profile
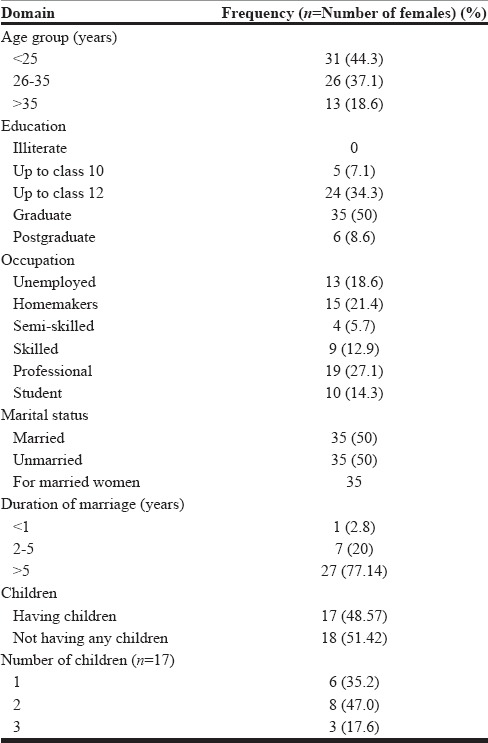
The sociodemographic profile of the sample is shown in Table 1.
Table 1.
Sociodemographic profile of the sample
Prevalence of anxiety and depression
Of the 70 females studied, 27 were found to be suffering from anxiety disorders, while 18 were found to be suffering from depressive disorders. Thus, the prevalence of anxiety disorders in our study sample was 38.6%, and the prevalence of depressive disorders was 25.7%.
The disorders noted were mixed anxiety depression (n = 10), other mixed anxiety disorders (n = 7), depressive episodes (n = 6), social phobia (n = 4), generalized anxiety disorder (n = 3), panic disorder (n = 3), and dysthymia (n = 2).
Ten females (14.3%) suffered from both anxiety and depressive disorders. A total of 35 patients, that is, 50%, had neither of the two.
The Hamilton rating scales for anxiety and depression were used to rate the severity of the respective conditions among those, in whom they were present. It was found that mild, moderate, and severe anxiety was present in 62.90%, 29.60%, and 7.40%, respectively. On the other hand, 50% had mild, 38.8% had moderate, and 11.10% had severe depressive symptoms.
Symptoms of polycystic ovarian syndrome
Menstrual abnormality was the most commonly noted symptom in the study population and was seen in 95.7% of the females.
The prevalence of the various symptoms is shown in Figure 1.
Figure 1.

The prevalence of the symptoms of polycystic ovarian syndrome in the study sample
Among the 35 married females, the symptom of infertility was seen in 18 females, thus indicating a prevalence of 51.4%.
Most of the study sample experienced more than one symptom. The symptom frequency is given in Figure 2.
Figure 2.
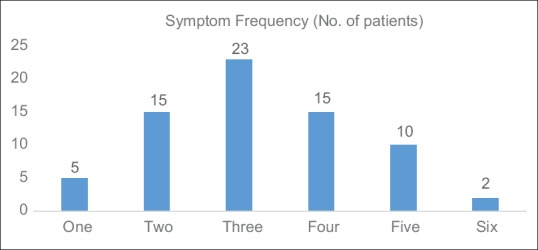
Number of symptoms experienced by the patients (n = 70)
Effects of the different symptoms of polycystic ovarian syndrome on anxiety and depression
Logistic regression was performed to ascertain the effects of the symptoms of PCOS on the likelihood that the females suffered from anxiety and/or depression. The variables entered were alopecia, hirsutism, acne, obesity, menstrual irregularities, acanthosis, and infertility. For the presence or absence of infertility, the data were entered only for married females.
The logistic regression model for the dependent variable anxiety is shown in Table 2
Table 2.
Logistic regression model for the dependent variable anxiety

A test of the full model against the constant only model was statistically significant (P = 0.010), indicating that the inclusion of the variables contributed significantly to the model. The Hosmer–Lemeshow test statistic was not significant (χ2 = 5.385; P = 4.95), indicating a well-fitting model. The logistic regression model was statistically significant (χ2 = 18.59, P < 0.05). The model explained 55.1% (Nagelkerke R2) of the variance in anxiety and correctly classified 74.3% of the cases. Symptom of alopecia and infertility were associated with an increased likelihood of anxiety.
Thus, in patients of PCOS, the odds of associated anxiety with and without alopecia are 3.06. The odds ratio for associated anxiety with and without infertility is 3.77.
The logistic regression model for the dependent variable depression is shown in Table 3.
Table 3.
Logistic regression model for the dependent variable depression

A test of the full model against the constant only model was statistically significant (P = 0.018), indicating that the inclusion of the variables contributed significantly to the model. The Hosmer–Lemeshow test statistic was not significant (χ2 = 1.428, P = 0.964) indicating a well-fitting model. The logistic regression model was statistically significant (χ2 Chi square = 16.86, P < 0.05). The model explained 53.7% (Nagelkerke R2) of the variance in depression and correctly classified 80% of the cases. Symptom of acne was associated with an increased likelihood of depression.
Thus, in patients of PCOS, the odds ratio of associated depression with and without acne is 3.78.
Impact of psychiatric morbidity on the quality of life
Among the four domains, the QOL in the domain of psychological health had the least mean and median scores. QOL in all the four domains was compared between patients with and without psychiatric morbidity using the Mann–Whitney U-test. This is shown in Table 4.
Table 4.
Group differences in the World Health Organization Quality of Life scores between those with and without psychiatric morbidity

Thus, patients with psychiatric morbidity had a significantly lower score on three domains of the QOL, namely, physical health, psychological health, and social and personal relationships. The domain of environmental and financial resources did not differ significantly between the two groups.
The mean scores of the QOL were compared for each symptom of PCOS. It was observed that patients with hirsutism had significantly lower scores on the psychological domain of QOL. (Mann–Whitney U = 407.000; Wilcoxon W = 758.000; Z = −2.065; Asymp Sig [2 tailed] = 0.039). None of the other symptoms, or the total number of symptoms, affected the QOL.
DISCUSSION
In our study, the overall prevalence of psychiatric morbidity was 50%, and that of anxiety disorders was 38.6%, and depressive disorders were 25.7%. Both the conditions were mild in majority of the cases. Comparisons across studies are difficult due to vast differences in methodology.
The Indian study from Kashmir[5] that also used a structured clinical interview found an overall prevalence of psychiatric morbidity to be 52.7%. The prevalence of anxiety and depressive disorders was 39% and 25%, respectively. A study from Iran,[14] in which patients were evaluated by a psychiatrist reported the prevalence of anxiety disorders to be 35.7% and depressive disorders to be 18.9%. This is similar to our findings which perhaps reflect the congruence in methodology.
A systematic review and meta-analysis on anxiety and depression in PCOS[15] concluded that women with PCOS tend to experience mildly elevated anxiety and depression, which concurs with the findings of the present study.
A recent German study[16] using a different design and the hospital anxiety and depression scale reported that 34% and 21% patients showed clinically relevant anxiety and depressive symptoms. Although these findings are in keeping with the ones in our research, studies using screening measures cannot be compared with those that have used clinical interview for obvious reasons. Cooney et al.[17] recently published their systemic review and meta-analysis of 30 cross-sectional studies that have used valid screening instruments to detect anxiety and depression in PCOS. They reported substantial heterogeneity among studies reporting anxiety symptoms but not so much for depressive symptoms. They also reported that these women had a higher prevalence of moderate-to-severe anxiety symptoms, which is different from our findings. Screening tests undoubtedly have their own utility and advantages. However, the diagnostic approach in the present study was interview-based and therefore more rigorous. The focus of the study was on anxiety and depression because they are well-defined constructs, amenable to intervention.
The reasons for the higher prevalence of anxiety and depression in PCOS are complex. In women diagnosed with PCOS, emotional distress could have psychosocial and/or pathophysiological causes.[18] Visible features of PCOS such as hirsutism, acne, and alopecia, as well as its potential consequences such as menstrual irregularity, infertility, and obesity, can be deeply stigmatizing to women.[18] In a qualitative study[19] on the subjective experience of PCOS, women described as feeling robbed of their self-concept, essence of being feminine, and attractive, thus making PCOS, the “thief of womanhood.” On the other hand, many researchers have postulated a biological mechanism between the symptoms of PCOS and anxiety and depression, proposing mechanisms such as hyperandrogenism and insulin resistance,[17] but the results have not been consistent.[20]
The present study found that infertility and alopecia were associated with anxiety, acne with depression, and hirsutism had an independent association with the psychological QOL. Clinical hyperandrogenism primarily includes hirsutism, acne, and male pattern alopecia.[21] Laboratory evaluation of hyperandrogenism was beyond the scope of this study, but this finding provides a direction for the future research.
The association of alopecia with anxiety was a new finding, not seen in previous research. One study was negative for alopecia and depression in PCOS,[22] but a clinical review by Hunt and McHale suggests that very little systematic research has examined the psychological effects of alopecia.[23] There is some evidence for acne and depression in PCOS[16,24] and studies done in dermatological settings have shown that female gender and acne are jointly and independently associated with a risk of major depression and suicide.[25] Studies on Asian populations[26,27,28] have emphasized the role of infertility in psychological distress and attributed it to the sociocultural milieu. Motherhood is a cherished experience and the fulfillment of a vital societal role. Childlessness is, therefore, a huge burden. Indian studies have also shown that infertility is associated with low self-esteem, marital discord, and significant social stigma.[29]
There is very robust evidence for the association of hirsutism with a poorer QOL.[7,28,30,31] Research shows that not only is hirsutism associated with low self-esteem and poor body image[32] but also the time and energy spent in concealing it aggravates the distress further.[33]
None of the other symptoms was associated with anxiety or depression or a poorer QOL in the present study. Obesity, which has shown a consistent association with these parameters in Western literature,[20,26] has not been replicated in studies in Eastern populations.[26,31] Researchers believe that while obesity is perceived as unattractive in Western countries, it may not be viewed so negatively in Asian countries. It may be in fact regarded as a sign of prosperity![31] However, some other studies did not replicate these results.[7,30]
While other studies have used disease-specific QOL measures,[30] we chose the WHOQOL-BREF,[13] keeping in mind that PCOS is a disorder that has multiple symptoms which can impact both physical and psychological health and have social ramifications as well. The scale has been validated in two PCOS studies from Asia.[31,34] We observed that the psychological domain of the QOL had the lowest score and psychiatric morbidity was significantly associated with a poorer QOL. This suggests that in PCOS, the presence of psychiatric morbidity can significantly undermine the QOL irrespective of the symptoms. Several international studies have reported that women with PCOS who suffer from anxiety and depression have a lower QOL.[14,20,35,36] Some authors suggest that psychological morbidity can impact on physical (e.g., eating and sleeping patterns), psychological (e.g., motivation and feelings of worthlessness), and social factors (e.g., relationships with others). Effective symptom management of PCOS is likely to be improved if existing anxiety and depression are effectively treated.[20]
CONCLUSIONS
The prevalence of anxiety disorders was 38.6% and that of depressive disorders was 25.7%. Symptom of alopecia and not having children were associated with an increased likelihood of exhibiting anxiety. The odds of associated anxiety with and without alopecia were 3.06:1 and for associated anxiety with and without infertility was 3.77:1. Symptom of acne was associated with an increased likelihood of exhibiting depression, and the odds ratio of associated depression with and without acne was 3.78:1. Patients with psychiatric morbidity had a significantly lower score on three domains of the QOL, namely, physical health, psychological health, and social and personal relationships. Patients with hirsutism had significantly lower scores on the psychological domain of the QOL.
Limitations
This study has certain limitations. It is a cross-sectional study carried out on the employees of a Central Government Health Scheme and their family members, hence their characteristics may not be shared by the general population. There was no control group for comparison with the study population. Hence, results had to be discussed with respect to the findings of previous studies.
Clinical implications and recommendations
Anxiety and depression are prevalent in patients with PCOS, and this study concurs with the guidelines recommending screening such patients for these disorders. The results of this study show that certain symptoms of PCOS are associated with anxiety and depression. The symptoms of PCOS may change throughout the course of the illness. Hence, it is vital that screening for psychiatric morbidity be incorporated as an ongoing process rather than a one-time assessment. The fact that psychiatric morbidity is associated with certain symptoms of PCOS and not with others makes it possible that there could be a biological link between the two. Further research on this subject could throw more light on these connections. Finally, the symptoms of PCOS are associated with anxiety and depression which in turn are associated with poorer QOL. The symptoms themselves did not appear to contribute to the poorer QOL. This could mean that perhaps the psychiatric morbidity is the mediator for a poorer QOL in patients with PCOS. There is, thus, a clear indication to treat these disorders whenever they are present.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Dr. Amrita Misri – Head Department of Obstetrics and Gynaecology for granting us permission to conduct the study on females with polycystic ovarian syndrome presenting to the Department of Obstetrics and Gynaecology.
REFERENCES
- 1.Malik-Aslam A, Reaney MD, Speight J. The suitability of polycystic ovary syndrome-specific questionnaires for measuring the impact of PCOS on quality of life in clinical trials. Value Health. 2010;13:440–6. doi: 10.1111/j.1524-4733.2010.00696.x. [DOI] [PubMed] [Google Scholar]
- 2.Malik S, Jain K, Talwar P, Prasad S, Dhorepatil B, Gouri Devi. Management of polycystic ovary syndrome in India. Fertil Sci Res. 2014;1:23–43. [Google Scholar]
- 3.Månsson M, Holte J, Landin-Wilhelmsen K, Dahlgren E, Johansson A, Landén M, et al. Women with polycystic ovary syndrome are often depressed or anxious – A case control study. Psychoneuroendocrinology. 2008;33:1132–8. doi: 10.1016/j.psyneuen.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Fauser BC. Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Consensus on women's health aspects of polycystic ovary syndrome (PCOS) Hum Reprod. 2012;27:14–24. doi: 10.1016/j.fertnstert.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 5.Hussain A, Chandel RK, Ganie MA, Dar MA, Rather YH, Wani ZA, et al. Prevalence of psychiatric disorders in patients with a diagnosis of polycystic ovary syndrome in Kashmir. Indian J Psychol Med. 2015;37:66–70. doi: 10.4103/0253-7176.150822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Upadhyaya SK, Sharma A, Agrawal A. Prevalence of anxiety and depression in polycystic ovarian syndrome. Int J Med Sci Public Health. 2016;5:681–3. [Google Scholar]
- 7.Sundararaman PG, Shweta, Sridhar GR. Psychosocial aspects of women with polycystic ovary syndrome from South India. J Assoc Physicians India. 2008;56:945–8. [PubMed] [Google Scholar]
- 8.Bhattacharya SM, Jha A. Prevalence and risk of depressive disorders in women with polycystic ovary syndrome (PCOS) Fertil Steril. 2010;94:357–9. doi: 10.1016/j.fertnstert.2009.09.025. [DOI] [PubMed] [Google Scholar]
- 9.Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19–25. doi: 10.1016/j.fertnstert.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 10.International Classification of Diseases. 10. (ICD-10) Chapter V: Mental and behavioural disorders. :F01–F99. [Google Scholar]
- 11.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 13.Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL group. Psychol Med. 1998;28:551–8. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 14.Sayyah-Melli M, Alizadeh M, Pourafkary N, Ouladsahebmadarek E, Jafari-Shobeiri M, Abbassi J, et al. Psychosocial factors associated with polycystic ovary syndrome: A Case control study. J Caring Sci. 2015;4:225–31. doi: 10.15171/jcs.2015.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barry JA, Kuczmierczyk AR, Hardiman PJ. Anxiety and depression in polycystic ovary syndrome: A systematic review and meta-analysis. Hum Reprod. 2011;26:2442–51. doi: 10.1093/humrep/der197. [DOI] [PubMed] [Google Scholar]
- 16.Benson S, Hahn S, Tan S, Mann K, Janssen OE, Schedlowski M, et al. Prevalence and implications of anxiety in polycystic ovary syndrome: Results of an internet-based survey in Germany. Hum Reprod. 2009;24:1446–51. doi: 10.1093/humrep/dep031. [DOI] [PubMed] [Google Scholar]
- 17.Cooney LG, Lee I, Sammel MD, Dokras A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: A systematic review and meta-analysis. Hum Reprod. 2017;32:1075–91. doi: 10.1093/humrep/dex044. [DOI] [PubMed] [Google Scholar]
- 18.Veltman-Verhulst SM, Boivin J, Eijkemans MJ, Fauser BJ. Emotional distress is a common risk in women with polycystic ovary syndrome: A systematic review and meta-analysis of 28 studies. Hum Reprod Update. 2012;18:638–51. doi: 10.1093/humupd/dms029. [DOI] [PubMed] [Google Scholar]
- 19.Kitzinger C, Willmott J. 'The thief of womanhood': Women's experience of polycystic ovarian syndrome. Soc Sci Med. 2002;54:349–61. doi: 10.1016/s0277-9536(01)00034-x. [DOI] [PubMed] [Google Scholar]
- 20.Deeks AA, Gibson-Helm ME, Paul E, Teede HJ. Is having polycystic ovary syndrome a predictor of poor psychological function including anxiety and depression? Hum Reprod. 2011;26:1399–407. doi: 10.1093/humrep/der071. [DOI] [PubMed] [Google Scholar]
- 21.Teede H, Deeks A, Moran L. Polycystic ovary syndrome: A complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010;8:41. doi: 10.1186/1741-7015-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quinn M, Shinkai K, Pasch L, Kuzmich L, Cedars M, Huddleston H, et al. Prevalence of androgenic alopecia in patients with polycystic ovary syndrome and characterization of associated clinical and biochemical features. Fertil Steril. 2014;101:1129–34. doi: 10.1016/j.fertnstert.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 23.Hunt N, McHale S. The psychological impact of alopecia. BMJ. 2005;331:951–3. doi: 10.1136/bmj.331.7522.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zangeneh FZ, Naghizadeh MM, Nasrin Abedinia N, Haghollahi F, Hezarehei D. Psychological signs in patients with polycystic ovary syndrome. J Fam Reprod Health. 2012;6:45–151. [Google Scholar]
- 25.Yang YC, Tu HP, Hong CH, Chang WC, Fu HC, Ho JC, et al. Female gender and acne disease are jointly and independently associated with the risk of major depression and suicide: A national population-based study. Biomed Res Int. 2014;2014:504279. doi: 10.1155/2014/504279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schmid J, Kirchengast S, Vytiska-Binstorfer E, Huber J. Infertility caused by PCOS – Health-related quality of life among Austrian and Moslem immigrant women in Austria. Hum Reprod. 2004;19:2251–7. doi: 10.1093/humrep/deh432. [DOI] [PubMed] [Google Scholar]
- 27.Guz H, Ozkan A, Sarisoy G, Yanik F, Yanik A. Psychiatric symptoms in Turkish infertile women. J Psychosom Obstet Gynaecol. 2003;24:267–71. doi: 10.3109/01674820309074691. [DOI] [PubMed] [Google Scholar]
- 28.Bazarganipour F, Ziaei S, Montazeri A, Foroozanfard F, Kazemnejad A, Faghihzadeh S, et al. Body image satisfaction and self-esteem status among the patients with polycystic ovary syndrome. Iran J Reprod Med. 2013;11:829–36. [PMC free article] [PubMed] [Google Scholar]
- 29.Deka PK, Sarma S. Psychological aspects of infertility. Br J Med Pract. 2010;3:a336. [Google Scholar]
- 30.Khomami MB, Tehrani FR, Hashemi S, Farahmand M, Azizi F. Of PCOS symptoms, hirsutism has the most significant impact on the quality of life of Iranian women. PLoS One. 2015;10:e0123608. doi: 10.1371/journal.pone.0123608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kumarapeli V, Seneviratne Rde A, Wijeyaratne C. Health-related quality of life and psychological distress in polycystic ovary syndrome: A hidden facet in South Asian women. BJOG. 2011;118:319–28. doi: 10.1111/j.1471-0528.2010.02799.x. [DOI] [PubMed] [Google Scholar]
- 32.Ekback M, Wijma K, Benzein E. “It is always on my mind”: Women's experiences of their bodies when living with hirsutism. Health Care Women Int. 2009;30:358–72. doi: 10.1080/07399330902785133. [DOI] [PubMed] [Google Scholar]
- 33.Brady C, Mousa SS, Mousa SA. Polycystic ovary syndrome and its impact on women's quality of life: More than just an endocrine disorder. Drug Healthc Patient Saf. 2009;1:9–15. doi: 10.2147/dhps.s4388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dilbaz B, Cınar M, Ozkaya E, Tonyalı NV, Dilbaz S. Health related quality of life among different PCOS phenotypes of infertile women. J Turk Ger Gynecol Assoc. 2012;13:247–52. doi: 10.5152/jtgga.2012.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Elsenbruch S, Benson S, Hahn S, Tan S, Mann K, Pleger K, et al. Determinants of emotional distress in women with polycystic ovary syndrome. Hum Reprod. 2006;21:1092–9. doi: 10.1093/humrep/dei409. [DOI] [PubMed] [Google Scholar]
- 36.Barnard L, Ferriday D, Guenther N, Strauss B, Balen AH, Dye L, et al. Quality of life and psychological well being in polycystic ovary syndrome. Hum Reprod. 2007;22:2279–86. doi: 10.1093/humrep/dem108. [DOI] [PubMed] [Google Scholar]


