Abstract
Aim:
To evaluate and compare the efficacy of “calcium sucrose phosphate” (CaSP) toothpaste (Enafix 5%) with ordinarily used calcium, phosphate-containing toothpaste in elevating the level of calcium, phosphate ions in saliva. Secondary aims were to evaluate substantivity and plaque-reducing ability of CaSP toothpaste.
Materials and Methods:
Thirty study participants of age group 6–13 years were divided into two groups: Group X (Control group) was made to continue brushing with their regularly used calcium, phosphate-containing toothpaste and Group Y (Test group) was allotted CaSP toothpaste. 1 ml of unstimulated saliva was periodically collected from both groups to determine any alteration in the salivary calcium, phosphate level. Parameters such as substantivity and plaque-reducing ability of CaSP toothpaste were also evaluated. Salivary mineral's intergroup comparison was evaluated by Student's t-test while its intragroup comparison along with the plaque amount variation in Group Y was evaluated by ANOVA and Tukey's post hoc test.
Results:
Group Y showed an increase in the salivary calcium level though not statistically significant. The increase was pronounced in samples collected on day 1. Group Y showed a consistent level of calcium, phosphate in samples collected immediately and 6 h postbrushing, indicating its substantivity. In addition, Group Y had an impact in reducing the plaque level when the 1st-month plaque score was compared with the 12th-month score.
Conclusion:
CaSP leads to an increase in the salivary calcium level though it was not statistically significant. Supervised brushing and dietary habits showed a positive effect on both the groups. CaSP toothpaste also showed substantivity and plaque-reducing ability.
Keywords: Calcium sucrose phosphate toothpaste, plaque, saliva, salivary calcium and phosphate
Introduction
Dental caries, despite various modern advancements, remains as one of the most widespread pandemic diseases worldwide. The new challenge now is to manage noncavitated lesions noninvasively, and thus, various methods and materials for remineralization of carious lesion have become the need of the hour. A combination of diet, pathogenic bacteria (plaque), and unfavorable salivary components together leads to production of organic acids which results in drop in pH, eventually leading to demineralization and cavitation. Conversely, remineralization is wherein the dissolution of minerals are prevented and by using oral fluids (plaque, saliva) as an intermediary, teeth are replenished back with the lost minerals like calcium and phosphate.[1]
Various remineralizing toothpastes containing agents such as fluoride, casein phosphopeptide, and novamin are in the market to yield daily remineralization and prevention against dental decay. Fluoride has been considered the cornerstone of remineralization.[2] Studies have shown that fluoride drives the process of remineralization only if there is adequate supply of calcium and phosphate.[3] Studies proving decrease in the incidence of caries postincorporation of calcium and phosphate into diet paved the way for these to be incorporated into toothpaste.[4] Further, along with calcium and phosphate, calcium sucrose phosphate (CaSP) addition was studied which also showed synergistic benefits.
Anticay, a CaSP–calcium orthophosphate complex, supplies both calcium and phosphate in a soluble form. It is a fine, white, nonhygroscopic powder with a neutral blend taste. It contains approximately 11.5% calcium on a dry weight basis. This complex helps reduce the acid solubility of enamel and increase the rate of remineralization by a common ion effect. Furthermore, it has shown to inhibit the formation and adherence of plaque to the enamel surface. This anticay technology has been incorporated into toothpastes such as Toothmin (Abbott Healthcare) and Enafix (Group Pharmaceuticals Ltd., India).[1] This study is on Anticay's (CaSP Enafix) ability to provide calcium and phosphate ions to saliva, to reduce the amount of plaque and to evaluate its substantivity potential in the oral cavity.
Materials and Methods
Two groups of study participants having 15 children each in the age group 6–13 years were selected for this study having a parallel design with 1:1 ratio. Each of the selected participant had nonrestored teeth and noncarious oral cavity. The institutional ethical committee approval was granted, and informed consent was attained from the secretary of both the orphanages and the study was commenced on December 2015 and continued for a year. After screening of a total of 70 children in the two orphanages located in the same area of Kerala, India, the eligible thirty participants were divided into two groups based on the orphanages they resided in. Fifteen males residing in one orphanage were allotted to control group (Group X) and were asked to continue using their regularly used calcium, phosphate-containing toothpaste which on verification was Colgate (Colgate Palmolive (India) Ltd.). Fifteen females residing in another orphanage were allotted to the test group (Group Y) and were given CaSP toothpaste (Enafix 5%). After intraoral examination and recording of diet chart, the study participants were demonstrated Bass brushing technique keeping time period of brushing (2 min), amount of paste (pea size), sugar exposure (3–5: solid and 5–7: liquid), and the frequency of brushing (twice daily) constant, which were regularly monitored by the warden of both the orphanages. These parameters are in accordance with literatures in the past.[5,6,7,8]
From each study participant of both groups, 1 ml of unstimulated saliva sample was collected before brushing (Sample A). Passive drooling method with minimal oral movements as described in previous studies was used to collect the unstimulated saliva.[9,10,11] Following that, study participants from their respective groups were asked to brush using the paste allotted to them. Half an hour and 6 h after brushing, saliva samples were again collected (Sample B and Sample C, respectively) from both the groups to evaluate the substantivity of the toothpaste in the oral cavity. Collected samples were immediately transported in an ice box maintaining a temperature of 4°C to the biochemistry laboratory for analysis of calcium and inorganic phosphate ions using Olympus AU2700 autoanalyzer (Beckman Coulter, Inc, Fullerton, CA, USA). It is a fully automated photometric analyzer which follows the colorimetric principle to analyze calcium, phosphate level of various body fluids.
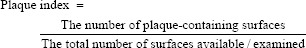
After collecting saliva 6 h postbrushing, a disclosing agent (2-tone dye: GC Tri Plaque ID Gel) was applied thoroughly on all the surfaces of teeth, and plaque index was recorded using O’Leary Plaque index given by Timothy J. O’Leary in 1972.[12] After rinsing, the presence of any colored stain on the dentogingival junction of buccal, lingual/palatal, mesial, and distal surfaces of all teeth present was examined, marked in the record form and summed up following which the given formula was applied:
In a similar manner, 6 h postbrushing evaluation of salivary calcium and phosphate ions was done every 3 months (Sample D), 6 months (Sample E), and 12 months (Sample F) in both the groups, while plaque index was recorded only for the test group (Enafix × 5%) in order to evaluate the efficacy of CaSP toothpaste in altering the amount of plaque [Figure 1]. In this way, the parameters recorded for each study participant were salivary calcium and phosphate level and plaque index. Constant reinforcement by regular calls, once in a week visit to the orphanages, getting attendance sheet marked by the warden indicative of the brushing protocol followed by the study participants, and constant look over the diet chart to note any variation was done to have an accurate result.
Figure 1.
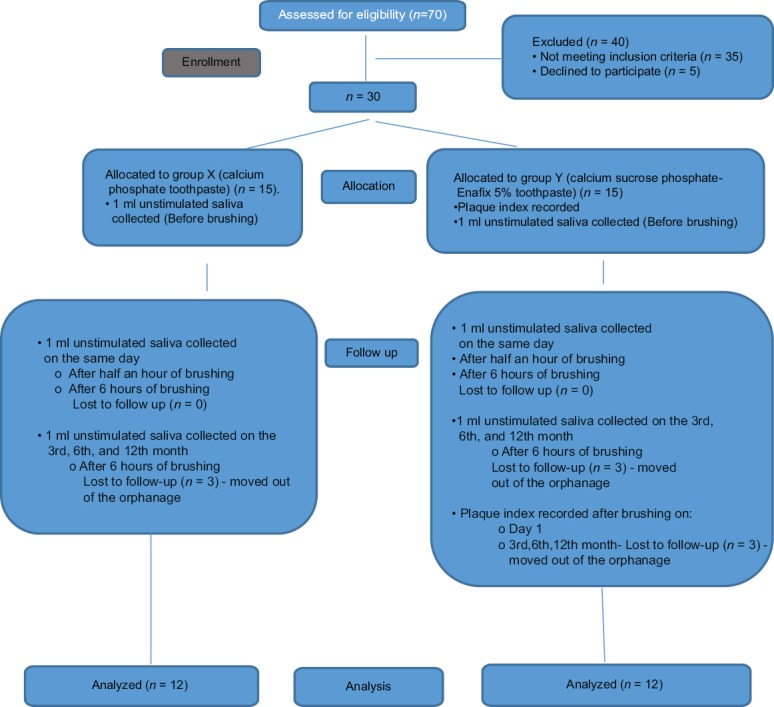
CONSORT flow diagram
Statistical analysis
Derivation of sample size was done using the following formula:
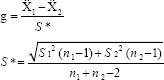
A sample size of five in each group was attained, following which 15 participants were chosen for each group keeping in mind the chances of dropouts in this 1-year study.
Student's t-test was applied to compare the calcium and phosphate values in control and test groups. ANOVA test was applied for an intragroup comparison of mean of calcium and phosphate level in samples collected at different time periods in both the groups. Once the values of ANOVA test gave a significant difference, it was subjected to Tukey's post hoc test. In addition, Group Y was subjected to ANOVA test to analyze the amount of difference in calcium and phosphate level between samples collected at different time intervals.
Results
Values were analyzed after removing the dropouts over a period of the 12-month study. Control group (X) and Test group (Y) had 3 dropouts each as the participants moved out of the orphanage and could not be followed up. Thus, the sample size was 12 in each group. Since both groups had equal number of participants after dropout, missing data analysis was not done. Results were considered statistically significant with P ≤ 0.005.
Abbreviations used are:
Control group (X), Test group (Y)
Saliva sample collected before brushing on day 1 (A)
Saliva sample collected ½ h after brushing on day 1 (B)
Saliva sample collected 6 h after brushing on day 1 (C)
Saliva sample collected after 3 months of intervention (D)
Saliva sample collected after 6 months of intervention (E)
Saliva sample collected after 12 months of intervention (F)
Plaque scored 6 h after brushing on day 1 (c)
Plaque scored after 3 months of intervention (d)
Plaque scored after 6 months of intervention (e)
Plaque scored after 12 months of intervention (f)
Salivary calcium and phosphate level
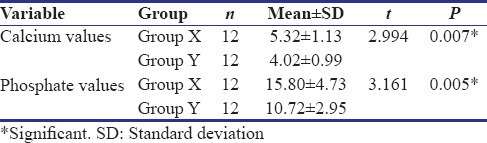
Intergroup comparison
Student's t-test was applied for each sample of both groups. A significant difference with P = 0.007 and 0.005 for calcium and phosphate level, respectively, was observed in Sample A [Table 1], while other samples did not give a significant difference. This indicated difference in baseline level of calcium and phosphate in the two groups with more calcium and phosphate levels in control group.
Table 1.
Sample A
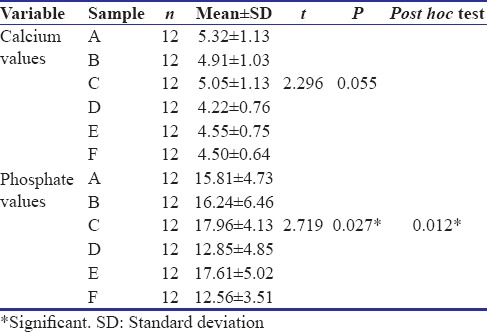
Intragroup comparison
Control group (Group X)
ANOVA test gave a significant difference with P = 0.055 for calcium level and 0.027 for phosphate level. Thus, there was a significant alteration in the phosphate level after intervention. Tukey's post hoc test showed that the samples collected at 6 h on day 1 showed maximum phosphate level [Table 2].
Table 2.
Group X
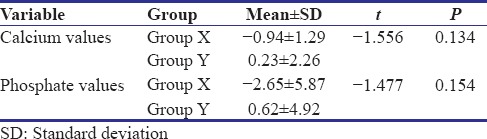
Test group (Group Y)
ANOVA test when applied to the difference in mean values of different samples gave a statistically significant difference of P = 0.008 in the calcium level [Table 3]. This suggests that there was a marked alteration in the calcium level between samples collected at different times with maximum alteration in the samples collected after ½ h and 6 h of brushing. Another noticeable result was the almost similar calcium and phosphate level in Sample B (½ h postbrushing) and Sample C (6 h postbrushing). This indicates that the test paste showed substantivity property in oral cavity.
Table 3.
Group Y
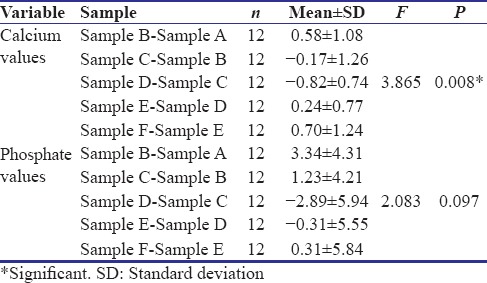
Since the baseline value of these parameters differed between the two groups, there was a need to find out which of the two groups showed more increase in calcium and phosphate level when the sample collected before intervention (Sample A) was compared with the 12th-month sample (Sample F). Followed by Student's t-test, the difference attained when subjected to an intergroup comparison showed a greater mean in the test group [Table 4], suggesting an increase in the salivary parameters in this group, though statistically not significant.
Table 4.
Intergroup comparison of difference between Sample F and Sample A
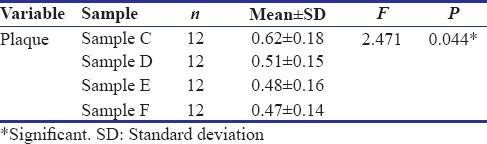
Plaque amount
The plaque amount in Group Y was subjected to ANOVA test which gave a statistically significant difference [Table 5 and Graph 1]. Difference in mean values between Sample C (sample collected 6 h after brushing on day 1) and Sample F (12th month of intervention) indicates a significant reduction in the plaque amount over a period of 12 months.
Table 5.
Plaque amount in Group Y
Graph 1.
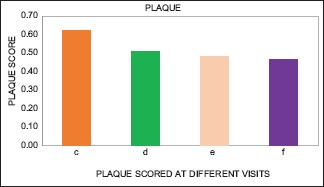
Difference in plaque level in Group Y
Discussion
Dental caries is a pathological process which leads to localized destruction of tooth tissue by microorganisms.[2] Once the tooth erupts into the oral cavity, it gets covered by a proteinaceous substance called acquired enamel pellicle (inner layer of plaque),[13] which houses the bacteria, providing it a favorable environment to grow and multiply, thereby contributing in dental caries.[14] Saliva, an oral fluid constantly bathing the teeth, has immense role in tooth repair as adequate amount of minerals are constantly supplied by healthy saliva.[14,15] However, this natural process of remineralization via oral fluids shows inability to withstand strong acidic challenge for a long period of time. During such occasions, there is a need for an exogenous supply of calcium and phosphate ions.[16] To prevent dissolution at low pH, 20–30 times of calcium that is naturally present in saliva is required.[17]
Due to the knowledge about all these factors that could possibly reverse demineralization, the concept of tooth demineralization has undergone a paradigm shift wherein the treatment now is aimed at reverting the tooth to nearby normalcy while simultaneously conserving the tooth structure.[18] Remineralization is defined as the process whereby calcium and phosphate ions (primarily from saliva) are supplied from a source external to the tooth to promote ion deposition into crystal voids in demineralized enamel.[1,19] Fluoride is considered to be the cornerstone of remineralizing agents.[2] Lately, studies proved that fluoride is not much of a remineralizing agent, but it decreases demineralization as minerals lost are not the minerals gained or redeposited.[20] However, it is seen how fluoride in the presence of calcium and phosphate can act as a potential remineralizing agent.[21]
Since 1990, numerous forms of amorphous calcium phosphate-based products as remineralizing agents are introduced.[1,14] Recently, CaSP, first prepared in 1910 by Neuberg and Pollak by phosphorylation of sucrose with phosphorus oxychloride in the presence of lime, was reintroduced as a promising remineralizing agent after once being clinically proven as a food additive that could decline the incidence of caries.[4,22,23,24,25] Anticay is a new technology which uses this CaSP–calcium orthophosphate complex to supply both calcium and phosphate which are the common ions of enamel in a highly soluble form and maintains an alkaline pH.[1] It is a mixture of calcium sucrose mono- and diphosphate, disucrose monophosphate, and inorganic calcium phosphate that contains 11% calcium, 9.5% organic phosphate, and 2.5% inorganic phosphate, respectively.[26] It soon breaks down into calcium ions, phosphate ions, and sucrose phosphate ions in saliva, thereby permitting creation of an aqueous solution consisting of very high concentration of calcium and phosphate while simultaneously preventing precipitation.[25,27]
One percent anticay provides 30 × 10−3 M Ca, 10 × 10−3 M PO4, and 20 × 10−3 M sucrose phosphate compared to saliva which contains 1.4 × 10−3 M Ca and 4 × 10−3 M P04, thereby serving an as ideal remineralizing agent.[17,28] It is shown to reduce the rate of acid solubility of enamel and increase its rate of remineralization by common ions effect,[17,18,26,28,29] inhibits the formation of plaque and its adherence to enamel,[26,28,30] and inhibits the formation of acid in plaque.[28,30,31] In this study, Enafix™ toothpaste (Group Pharmaceuticals Limited, India) was used to evaluate and compare the efficacy of CaSP toothpaste with ordinarily used calcium and phosphate-containing toothpaste in elevating the level of calcium, phosphate ions in saliva. Calcium and phosphate levels in saliva would serve as a biomarker in indicating the remineralization potential of that particular toothpaste. This is in accordance with the literature given by Raghu and Ananthakrishna in 2016,[32] Lindh et al. in 2014,[13] Hara and Zero in 2014,[16] and Buzalaf et al. in 2012.[33] Evaluation of the substantivity of Enafix (calcium sucrose phosphate toothpaste) in the oral cavity was done by analyzing the difference between salivary calcium and phosphate level after ½ h and after 6 h of brushing on day 1.
To the best of our knowledge, this is the first in vivo study evaluating the potential of CaSP in remineralizing the tooth via analysis of salivary calcium and phosphate level. Furthermore, no study so far has been conducted to test the substantivity of this toothpaste in the oral cavity. Although postulated before in several studies such as Awasthi et al. in 2015,[34] the ability of this agent in reducing the amount of plaque has not been much evaluated. Study participants were chosen from orphanages keeping in mind the uniform diet that they follow with minimal sugar exposure. This reasoning is supported by sequence of age old studies conducted by Harris et al. in 1967, 1968, and 1969.[23] Unstimulated saliva was collected as it leads to more accurate phosphate level as well as less bacterial contamination.[35]
Attempts to follow the standard protocol of study was done by constant calls, visits and demonstration of brushing technique, checking the attendance sheet given to the warden and evaluating any change in the diet. The 6h postbrushing saliva sample was selected for evaluation of parameters on 3rd, 6th, and 12th months as this is the time for maximum undersaturation of saliva due to the incorporation of in between meals, thereby creating a cariogenic environment. This is supported by the study done by Creanor et al. in 2011[36] and Sullivan et al. in 1997.[21] Difference in baseline salivary calcium and phosphate level could be possibly due to various factors, one of which is the gender difference in the two groups. This reasoning is supported by Mohammad and Sultan in 2007[37] and Dawes in 1970[38] who stated that there is a significant difference in the salivary inorganic components in males and females, with lower level seen in females due to their lesser flow rate compared to males. Gender difference between the groups can be considered as one of the limitations, while it cannot be ignored that this difference also gave an additional result to the study. Test group showed an overall improvement in salivary calcium and phosphate level, though statistically not significant.
ANOVA test revealed that test group's salivary calcium level showed marked increase in sample collected ½ h and 6 h after brushing on day 1 and also in the 12th month of intervention. In the control group, despite using the same calcium and phosphate-containing toothpaste even before intervention, a sudden rise on the 1st day followed by a drop to almost the preintervention values could be due to many reasons which primarily revolve around patient's compliance. The statistical analysis of the plaque level in test group revealed a decline on the 12th month when compared to the plaque level scored on day 1. This is parallel to the study conducted by Awasthi et al. in 2015[34] on autistic children.
The following summaries can be drawn from this 1-year study on Enafix (CaSP):
Enafix leads to an increase in the salivary minerals level, mostly calcium, which is pronounced in the samples taken ½ h and 6 h postbrushing on day 1, although its continuous effect all throughout 1 year is not significant
A consistent level of these minerals in ½ h and 6 h samples suggests its substantivity in the oral cavity
Enafix has a role to play in reducing the amount of plaque accumulation on tooth surfaces
Proper supervision and education on oral hygiene measures, dietary habits, and positive reinforcements inculcates good brushing habits, resulting in an increase in the potential of various dentifrices in guarding the tooth structure against dental decay and helping in remineralization
Gender could be considered as a factor in modifying the level of salivary calcium and phosphate.
Enafix seems to be a potent remineralizing agent considering all the properties described. Thus, components of this toothpaste could be used with other regularly used dentifrices to impart its beneficial effects and improve the quality of the toothpaste. However, Enafix's action in elevating the salivary calcium and phosphate level requires further research to be done.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to extend their sincere gratitude to Dr. Sajitha Krishnan, Professor, Department of Biochemistry, Amrita School of Medicine, for her willingness to support and guide us in the biochemical analysis and to Mr. Venugopal R, Supervisor, Biochemistry Lab, Amrita Institute of Medical Sciences and Research Centre, for sparing his valuable time in helping us use the laboratory facilities. We would also like to thank Dr. E. S. Jeevanand, Statistician, for the patience and dedication shown to do the necessary statistical analysis. Also, expressing our sincere acknowledgment to Dr. Kamala and the team of Group Pharmaceuticals Ltd., Bengaluru, for providing us with the toothpaste used in this study.
References
- 1.Raksha B, Mithra H. An overview on remineralizing agents. Indian J. Appl Res. 2015;6:331–6. [Google Scholar]
- 2.Reynolds EC. Calcium phosphate-based remineralization systems: Scientific evidence? Aust Dent J. 2008;53:268–73. doi: 10.1111/j.1834-7819.2008.00061.x. [DOI] [PubMed] [Google Scholar]
- 3.Reynolds EC, Cai F, Cochrane NJ, Shen P, Walker GD, Morgan MV, et al. Fluoride and casein phosphopeptide-amorphous calcium phosphate. J Dent Res. 2008;87:344–8. doi: 10.1177/154405910808700420. [DOI] [PubMed] [Google Scholar]
- 4.Harris R, Schamschula RG, Gregory G, Roots M, Beveridge J. Observations on the cariostatic effect of calcium sucrose phosphate in a group of children aged 5-17 years. Preliminary report. Aust Dent J. 1967;12:105–13. doi: 10.1111/j.1834-7819.1967.tb02184.x. [DOI] [PubMed] [Google Scholar]
- 5.Lehl G, Bansal K, Sekhon R. Relationship between cariogenic diet and dental caries as evaluated from a 5-day diet diary in 4-12 year-old children. J Indian Soc Pedod Prev Dent. 1999;17:119–21. [PubMed] [Google Scholar]
- 6.Bangash RY, Khan AU, Tariq KM, Rasheed D. Evaluation of tooth brushing technique and oral hygiene knowledge at Afid, Rawalpindi. Pak Oral Dent J. 2012;32:124–7. [Google Scholar]
- 7.Schlueter N, Klimek J, Saleschke G, Ganss C. Adoption of a toothbrushing technique: A controlled, randomised clinical trial. Clin Oral Investig. 2010;14:99–106. doi: 10.1007/s00784-009-0269-1. [DOI] [PubMed] [Google Scholar]
- 8.Bray KK. Using brief motivational interview to sustain tooth brushing behaviour change. Am Dent Hyg Assoc. 2010:1–4. [Google Scholar]
- 9.Chiappin S, Antonelli G, Gatti R, De Palo EF. Saliva specimen: A new laboratory tool for diagnostic and basic investigation. Clin Chim Acta. 2007;383:30–40. doi: 10.1016/j.cca.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 10.Menon MM, Balagopal RV, Sajitha K, Parvathy K, Sangeetha GB, Arun XM, et al. Evaluation of salivary interleukin-6 in children with early childhood caries after treatment. Contemp Clin Dent. 2016;7:198–202. doi: 10.4103/0976-237X.183059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Varma B, Fathima N. Importance of comprehensive dental treatment and health education for children with Down syndrome. Int J Paediatr Dent. 2015;25:36–7. [Google Scholar]
- 12.O’Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972;43:38. doi: 10.1902/jop.1972.43.1.38. [DOI] [PubMed] [Google Scholar]
- 13.Lindh L, Aroonsang W, Sotres J, Arnebrant T. Salivary pellicles. Monogr Oral Sci. 2014;24:30–9. doi: 10.1159/000358782. [DOI] [PubMed] [Google Scholar]
- 14.Wolff MS, Larson C. The cariogenic dental biofilm: Good, bad or just something to control? Braz Oral Res. 2009;23(Suppl 1):31–8. doi: 10.1590/s1806-83242009000500006. [DOI] [PubMed] [Google Scholar]
- 15.Vogel GL, Zhang Z, Carey CM, Ly A, Chow LC, Proskin HM, et al. Composition of plaque and saliva following a sucrose challenge and use of an alpha-tricalcium-phosphate-containing chewing gum. J Dent Res. 1998;77:518–24. doi: 10.1177/00220345980770031101. [DOI] [PubMed] [Google Scholar]
- 16.Hara AT, Zero DT. The potential of saliva in protecting against dental erosion. Monogr Oral Sci. 2014;25:197–205. doi: 10.1159/000360372. [DOI] [PubMed] [Google Scholar]
- 17.Rogerson MJ. The role of a calcium sucrose phosphate-calcium orthophosphate complex in the reduction of dental caries. Aust Dent J. 1973;18:160–6. doi: 10.1111/j.1834-7819.1973.tb03454.x. [DOI] [PubMed] [Google Scholar]
- 18.Sargod SS, Bhat SS, Hegde S, Karunakaran R. Remineralization potential using calcium sucrose phosphate (enafix) on artificial carious lesion – A polaroid microscopic study. Indian J Appl Res. 2015;5:421–3. [Google Scholar]
- 19.Featherstone JD. Caries prevention and reversal based on the caries balance. Pediatr Dent. 2006;28:128–32. [PubMed] [Google Scholar]
- 20.Cury JA, Tenuta LM. Enamel remineralization: Controlling the caries disease or treating early caries lesions? Braz Oral Res. 2009;23(Suppl 1):23–30. doi: 10.1590/s1806-83242009000500005. [DOI] [PubMed] [Google Scholar]
- 21.Sullivan RJ, Charig A, Blake-Haskins J, Zhang YP, Miller SM, Strannick M, et al. In vivo detection of calcium from dicalcium phosphate dihydrate dentifrices in demineralized human enamel and plaque. Adv Dent Res. 1997;11:380–7. doi: 10.1177/08959374970110040201. [DOI] [PubMed] [Google Scholar]
- 22.Harris R, Schamschula RG, Beveridge J, Gregory G. The cariostatic effect of calcium sucrose phosphate in a group of children aged 5-17 years. Aust Dent J. 1968;13:32–9. doi: 10.1111/j.1834-7819.1968.tb02230.x. [DOI] [PubMed] [Google Scholar]
- 23.Harris R, Roots M, Gregory G, Beveridge J. Calcium sucrose phosphate as a cariostatic agent in children aged 5-17 years 3. Aust Dent J. 1968;13:345–52. doi: 10.1111/j.1834-7819.1968.tb03842.x. [DOI] [PubMed] [Google Scholar]
- 24.Harris R, Schamschula RG, Beveridge J, Gregory G. The cariostatic effect of calcium sucrose phosphate in a group of children aged 5-17 years. IV. Aust Dent J. 1969;14:42–9. doi: 10.1111/j.1834-7819.1969.tb03331.x. [DOI] [PubMed] [Google Scholar]
- 25.Gangrade A, Gade V, Patil S, Gade J, Chandhok D, Thakur D, et al. In vitro evaluation of remineralization efficacy of different calcium- and fluoride-based delivery systems on artificially demineralized enamel surface. J Conserv Dent. 2016;19:328–31. doi: 10.4103/0972-0707.186449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thabitha Rani S, Manjula M, Reddy R, Kumar L. Evaluation of remineralizing potential of Calcium Sucrose Phosphate and CPPACP: An in vitro study. Pediatr Dent J. 2016;26:95–102. [Google Scholar]
- 27.Den Besten P, Giambro N. Treatment of fluorosed and white-spot human enamel with calcium sucrose phosphate in vitro . Pediatr Dent. 1995;17:340–5. [PubMed] [Google Scholar]
- 28.Craig GG. The use of a calcium sucrose phosphates-calcium orthophosphate complex as a cariostatic agent. Br Dent J. 1975;138:25–8. doi: 10.1038/sj.bdj.4803360. [DOI] [PubMed] [Google Scholar]
- 29.Kaur G, Sanap AU, Aggarwal SD, Kumar T. Comparative evaluation of two different remineralizing agents on the microhardness of bleached enamel surface: Results of an in vitro study. Indian J Dent Res. 2015;26:176–9. doi: 10.4103/0970-9290.159154. [DOI] [PubMed] [Google Scholar]
- 30.Clarke NG, Fanning EA. Plaque pH and calcium sucrose phosphate: A telemetric study. Aust Dent J. 1971;16:13–6. doi: 10.1111/j.1834-7819.1971.tb00974.x. [DOI] [PubMed] [Google Scholar]
- 31.Clarke NG, Fanning EA. Further consideration of the effects of calcium sucrose phosphate on dental plaque: A telemetric study. Aust Dent J. 1973;18:229–32. doi: 10.1111/j.1834-7819.1973.tb03472.x. [DOI] [PubMed] [Google Scholar]
- 32.Raghu TN, Ananthakrishna S. Remineralization potential of calcium sucrose phosphate on demineralized enamel: Results of an in vitro study. J Int Oral Health. 2016;8:704–8. [Google Scholar]
- 33.Buzalaf MA, Hannas AR, Kato MT. Saliva and dental erosion. J Appl Oral Sci. 2012;20:493–502. doi: 10.1590/S1678-77572012000500001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Awasthi P, Peshwani B, Tiwari S, Thakur R, Shashikiran ND, Singla S, et al. Evaluation and comparison of the efficacy of low fluoridated and calcium phosphate-based dentifrice formulations when used with powered and manual toothbrush in children with autism. Contemp Clin Dent. 2015;6:S188–91. doi: 10.4103/0976-237X.166811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edgar WM, Higham SM, Manning RH. Saliva stimulation and caries prevention. Adv Dent Res. 1994;8:239–45. doi: 10.1177/08959374940080021701. [DOI] [PubMed] [Google Scholar]
- 36.Creanor S, Creanor S, Alharthy N. A comparison of in vitro erosion-like mineral loss between continuous and intermittent acidic exposure with and without human saliva. Arch Oral Biol. 2011;56:703–8. doi: 10.1016/j.archoralbio.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 37.Mohammad S, Sultan A. The relationship between calcium, magnesium and inorganic phosphate of human mixed saliva and dental caries. Med Dig J. 2007;4:157–61. [Google Scholar]
- 38.Dawes C. Effects of diet on salivary secretion and composition. J Dent Res. 1970;49:1263–73. doi: 10.1177/00220345700490061501. [DOI] [PubMed] [Google Scholar]


