Abstract
Background:
Dental esthetics has become a great concern for both dental practitioners and patients in addition to maintaining oral health. The presence of interproximal papillae between the maxillary anterior teeth is a key esthetic component. Recession of interdental papilla leads to various functional problems such as food impaction, phonetics and esthetic problems such as the formation of black triangle which poses a great challenge.
Aim:
This study aims to evaluate the augmentation of interdental papilla with platelet-rich fibrin.
Materials and Methods:
A total of 25 sites from systemically healthy individuals with papillary recession (Nordland and Tarnow class 1 and 2) were recruited in the study. Han and Takei procedure was planned and augmentation was done with platelet-rich fibrin. Various parameters such as distance from the tip of the contact point to the gingival margin, width of the keratinized gingiva, and Jemt score were measured at baseline, 3 and 6 months postoperatively. Healing index was measured at the 1st, 2nd, and 3rd week postoperatively.
Results:
Data collected were statistically analyzed. Mean value of distance from the contact point to the gingival margin was 4.38 mm at baseline and at 6-month postoperatively, it reduced to 0.36 mm. There was an increase in width of the keratinized gingiva which was clinically and statistically significant. Other parameters such as healing index, Jemt score, and visual analog scale (aesthetics) were also statistically significant postoperatively.
Keywords: Esthetics, interdental papilla, magnification loupes, platelet-rich fibrin, regeneration
Introduction
Esthetics has become a great concern for both dental practitioners and patients. The presence of interproximal papillae between the maxillary anterior teeth is important for an esthetic smile. Problems associated with black triangles are food impaction, unesthetic smile, and phonetic problems.[1]
Various techniques were used to reconstruct the lost papilla. Nonsurgical techniques consist of restorative, orthodontic treatment, and repeated curettage of the interdental papilla. Several surgical procedures that rebuild lost papillae have also been elusive.[2,3]
In the present study, Han and Takei[4] procedure was used with platelet-rich fibrin (PRF)[5] to augment interdental papilla. The second surgical site is avoided by the use of PRF.
Materials and Methods
The present study was conducted in the Outpatient Department of Periodontology and Oral Implantology, Indira Gandhi Institute of Dental Sciences, Puducherry. Thirteen selected patients with 25 sites were explained the entire procedure and were requested to submit a duly signed written informed consent. The study was conducted with the clearance from the Institutional Ethical Committee.
Male and female patients who consented for treatment between the age groups of 18–55 years with papillary recession in the maxillary anterior teeth with intact contact point (Nordland and Tarnow class 1 and 2) were included in the study.[6] Patients with caries, restoration, or crowns present in the adjacent teeth, those with the habit of tobacco chewing, smoking, alcohol consumption, and patients with allergy/systemic disease/treatment that contraindicate or compromise results of surgical procedure were excluded from the study.
Patients fulfilling the inclusion criteria were selected and subjected to presurgical biochemical evaluation. Radiographs were taken preoperatively to assess the distance from the contact point to bone crest. To standardize radiographs, paralleling cone technique was used with Rinn holder in place.
The following clinical parameters were recorded at baseline (preoperative) and postoperatively at the 1st, 3rd, and 6th month intervals.
Distance from contact point to the tip of the interdental papilla
Width of keratinized gingiva[7]
Jemt index[8]
Healing index (1st, 2nd, and 3rd week postoperatively)[9]
Visual analog scale (esthetics) photograph was assessed comparing baseline and 6-month postoperative.[10]
Surgical procedure
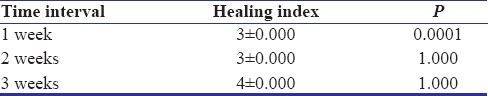
After the assessment of pretreatment records and clinical examination, patients who demonstrated a satisfactory response to Phase I therapy [Figure 1] were considered and subjected to surgical procedure. Ophthalmic tunnel blade (0.2 mm) and surgical compound loupes were used [Figure 2].
Figure 1.

Preoperative photograph
Figure 2.
Armamentarium used
The selected operative sites were anesthetized with 0.2% xylocaine with 2% adrenaline (1:200,000). A 3–5 mm semilunar incision was given with tunnel blade (0.2 mm) [Figure 3] at 2 mm coronal to the mucogingival junction, just over the papillary region followed by crevicular incision over the teeth neighboring the defect extending from the buccal aspect to the palatal aspect keeping the existing papilla preserved. Through the semilunar incision, the gingivopapillary unit was freed from the underlying bone using an orban knife extending toward the palate. Care was taken to avoid the perforation of the palatal tissue or damage to the interproximal papilla. The tissue was completely released from the root as well as bone, so that tissue becomes mobile, which allowed the coronal displacement of the gingivopapillary unit. A buccal/palatal void (dead space) was established between the soft tissue and the bone structure.
Figure 3.

Semilunar incision – Tunnel blade
Preparation of PRF was done according to Choukroun's protocol[5] [Figure 4].
Figure 4.

Platelet-rich fibrin
The PRF was trimmed to the desired size and placed under the recipient site using 5–0 vicryl sutures [Figure 5]. Periodontal dressing was given over the surgical area. Patients were prescribed with analgesics and antibiotics for 5 days. The patients were instructed to rinse with 0.2% chlorhexidine digluconate twice daily for 2 weeks and were given postsurgical instructions.
Figure 5.

Platelet-rich fibrin tucked and sutures placed
All the patients were recalled after 24 h to assess for postoperative complication such as bleeding, pain, swelling, and hematoma. After an interval of 1 week, patients were recalled for the removal of the periodontal dressing and to assess the extent of healing. The area was irrigated and healing index was evaluated postoperatively at 1, 2, and 3 weeks. Other clinical parameters were assessed at 3 and 6 months interval postoperatively [Figure 6].
Figure 6.

6-month postoperative photograph
Results
All the clinical parameters obtained at different intervals were entered in the standard proforma drawn for the study and were subjected to statistical analysis. The scores were statistically analyzed by calculating their mean values and standard deviation. Statistical analysis mean, standard deviation, and percentages were used as descriptive statistics. Nonparametric test was done as data did not follow normal distribution. The Friedman test which is the nonparametric alternative to the one-way ANOVA with repeated measures was applied.
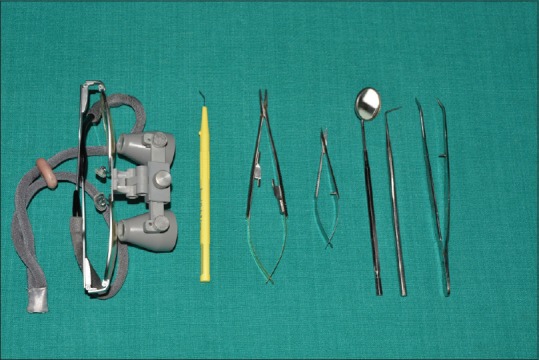
The mean value of the distance from the contact point to the tip of the papilla measured in millimeters at baseline was 4.38 ± 0.36. During 3-month follow-up, gradual papillary fill was noticed with a mean value of 2 ± 0.50. At 6-month postoperative evaluation, the distance further decreased indicating papillary fill with a mean value of 0.36 ± 0.638. The difference in papillary fill in 3 and 6 months postoperatively was statistically significant with P = 0.0001 [Table 1].
Table 1.
Clinical parameters recorded at baseline, 3 months, and 6 months
The width of the keratinized gingiva was measured at baseline, 3 and 6 months postoperatively. The mean value of the width of the keratinized gingiva measured in millimeters at baseline was 6.92 ± 1.579. There was an increase in width of keratinized gingiva at 3 months with a mean value of 7.84 ± 1.434. At 6 months evaluation, there was a further increase in the width of keratinized gingiva to 8.68 ± 1.345. The difference in width of the keratinized gingiva from baseline to 3 months and 6 months postoperatively was statistically significant with P = 0.0001 [Table 1].
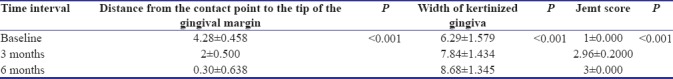
The healing index was recorded at 1 week, 2 weeks, and 3 weeks postoperatively. When healing was recorded postoperatively, the mean value was 3.00 and the mean value was 4.00 at the 2nd and 3rd week postoperatively. The difference in healing comparing the 1st and 2nd week was statistically significant with P = 0.0001 and comparing the 2nd and 3rd week was not statistically significant with P = 1.0 [Table 2].
Table 2.
Healing index recorded at the 1st, 2nd, and 3rd week postoperatively
The Jemt score was assessed at baseline and at 3 and 6 months postoperatively. The mean value at baseline was 1 at the 3rd month postoperatively a mean value of 2.96, and at the 6th month postoperatively, a mean value of 3 was noticed. When comparing Jemt score between baseline, 3 months and 6 months, it was clinically significant with P = 0.0001 [Table 1]. Visual analog scale scores (esthetics) were evaluated using two-independent examiners comparing pre- and postoperative photographs and an overall score of good was observed.
Discussion
Loss of interdental papilla leading to black triangle is one of the most troubling dilemmas in dentistry, thus predisposing the patient to phonetic, functional, and esthetic problems. Various surgical and nonsurgical approaches are proposed to help augment the lost interdental papilla.[11] Most of the surgical procedures fail to achieve long-term stability due to the minor blood supply in the limited area the interdental papilla occupies.[12] Surgical techniques aiming at correcting the problem of black triangle use mainly free epithelialized gingival grafts, repeated interproximal curettage, development of interproximal tissue in the buccal direction, and connective tissue graft.[13]
The Han and Takei procedure[4] used in this study offered predictable results as the technique allowed the formation of a pedicle using semilunar incision and coronal displacement of the entire gingivopapillary unit. This maintained the vascular supply in the augmentation site without creating tension, thereby preventing the rebounding of gingiva.
In the present study, augmentation of interdental papilla was done using PRF and various parameters were recorded. The distance from the contact point to the tip of the interdental papilla and width of the keratinized gingiva were measured at baseline and 3 and 6 months postoperatively, and results were clinically significant as there was complete papillary fill at 6 months postoperatively. Results were statistically significant with P value of 0.0001 similar to the study of Kaushik et al.[14]
The healing index was compared at 1, 2, and 3 weeks interval. Results were statistically significant comparing the 1st and 2nd week postoperatively, but no significance was seen between the 2nd and 3rd week postoperatively as reepithelialization of surgical site was completed by 2 weeks and our results were similar to the study conducted by Jankovic et al.[9]
Papillary fill was assessed using Jemt papilla index score.[8] Jemt score comparing baseline with immediate postoperative, 3 months and 6 months was statistically significant in accordance with a study Nemcovsky in 2001.
As the papilla augmentation procedure involved the improvement of esthetics, visual analog scale was performed using two-independent examiners, and the results were statistically analyzed which showed an overall result of a score good when comparing the preoperative and postoperative photographs which were statistically significant. Hence, this procedure basically improves the esthetic demands of the patient.
Various literatures quote the use of subepithelial connective tissue graft for the augmentation of interdental papilla. Although it gives predictable results, the need for the second surgical site cannot be avoided. Hence, in this study, connective tissue graft harvesting was avoided and PRF was used for papilla augmentation. PRF contains an intracellular storage of growth factors including transforming growth factor beta, platelet cytokines, platelet-derived growth factors, and insulin-like growth factor-1, which are gradually released from the fibrin matrix and aids in the process of healing.[15] The advantage of PRF over connective tissue graft is PRF is easy to procure, less expensive, better healing of surgical site, and no second surgical site required.[15]
There was complete fill of the papilla at 3 months and 6 months postoperatively and the results were similar to the study conducted by Arunachalam et al.[16] We were able to achieve stable results with this technique in our study.
The interdental papilla has a scalloped gingival unit which is usually delicate. Hence, gentle manipulation of the tissues and the use of ophthalmic tunnel blade and loupes can prevent the inadvertent severity of the tissues.[17] As there is limited access to the interdental papilla, surgical magnification and microsurgical instruments benefit the surgeon by increasing visibility, eliminating unnecessary releasing incisions, and facilitating access to the interdental papilla. Use of microscalpel allowed the surgeon to elevate the flap without injury, while avoiding vertical incisions, thus maintaining vascularity to the surgical area.[18,19]
Conclusion
The augmentation of the papilla using PRF in the new position was stable when reviewed at 3 and 6 months postoperatively
The use of PRF achieved successful and predictable results in the management of papillary recession
Loupes used in papilla augmentation resulted in improved outcomes and reduced tissue trauma and better operator's comfort.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chieh CM, Chan CP, Tu YT, Liao YF, Ku YC, Kwong KL, et al. Factors Influencing the length of the interproximal dental papilla between maxillary anterior teeth. J Dent Sci. 2009;4:103–9. [Google Scholar]
- 2.Nemcovsky CE. Interproximal papilla augmentation procedure: A novel surgical approach and clinical evaluation of 10 consecutive procedures. Int J Periodontics Restorative Dent. 2001;21:553–9. [PubMed] [Google Scholar]
- 3.Chu SJ, Tarnow DP, Tan JH, Stappert CF. Papilla proportions in the maxillary anterior dentition. Int J Periodontics Restorative Dent. 2009;29:385–93. [PubMed] [Google Scholar]
- 4.Han TJ, Takei HH. Progress in gingival papilla reconstruction. Periodontol 2000. 1996;11:65–8. doi: 10.1111/j.1600-0757.1996.tb00184.x. [DOI] [PubMed] [Google Scholar]
- 5.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e56–60. doi: 10.1016/j.tripleo.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 6.Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995–6. doi: 10.1902/jop.1992.63.12.995. [DOI] [PubMed] [Google Scholar]
- 7.Lang NP, Löe H. The relationship between the width of keratinized gingiva and gingival health. J Periodontol. 1972;43:623–7. doi: 10.1902/jop.1972.43.10.623. [DOI] [PubMed] [Google Scholar]
- 8.Carranza N, Zogbi C. Reconstruction of the interdental papilla with an underlying subepithelial connective tissue graft: Technical considerations and case reports. Int J Periodontics Restorative Dent. 2011;31:e45–50. [PubMed] [Google Scholar]
- 9.Jankovic SM, Zoran AM, Vojislav LM, Bozidar DS, Kenney BE. The use of platelet rich plasma in combination with connective tissue graft following treatment of gingival recessions. Periodontal Practice Today. 2007;4:63–71. [Google Scholar]
- 10.Shanmugam M, Sivakumar V, Anitha V, Sivakumar B. Clinical evaluation of alloderm for root coverage and colour match. J Indian Soc Periodontol. 2012;16:218–23. doi: 10.4103/0972-124X.99265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shapiro A. Regeneration of interdental papillae using periodic curettage. Int J Periodontics Restorative Dent. 1985;5:26–33. [PubMed] [Google Scholar]
- 12.Beagle JR. Surgical reconstruction of the interdental papilla: Case report. Int J Periodontics Restorative Dent. 1992;12:145–51. [PubMed] [Google Scholar]
- 13.Blatz MB, Hürzeler MB, Strub JR. Reconstruction of the lost interproximal papilla – Presentation of surgical and nonsurgical approaches. Int J Periodontics Restorative Dent. 1999;19:395–406. [PubMed] [Google Scholar]
- 14.Kaushik A, Pk P, Jhamb K, Chopra D, Chaurasia VR, Masamatti VS, et al. Clinical evaluation of papilla reconstruction using subepithelial connective tissue graft. J Clin Diagn Res. 2014;8:ZC77–81. doi: 10.7860/JCDR/2014/9458.4881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR, et al. Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:638–46. doi: 10.1016/s1079-2104(98)90029-4. [DOI] [PubMed] [Google Scholar]
- 16.Arunachalam LT, Merugu S, Sudhakar U. A novel surgical procedure for papilla reconstruction using platelet rich fibrin. Contemp Clin Dent. 2012;3:467–70. doi: 10.4103/0976-237X.107443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nordland P, Sandhu HS. Microsurgical technique for augmentation of the interdental papilla: Three case reports. Int J Periodontics Restorative Dent. 2008;28:543–9. [PubMed] [Google Scholar]
- 18.Tibbetts LS, Shanelac D. Principles and practice of periodontal micro surgery. Int J Microdent. 2009;1:13–24. [Google Scholar]
- 19.Burkhardt R, Hürzeler MB. Utilization of the surgical microscope for advanced plastic periodontal surgery. Pract Periodontics Aesthet Dent. 2000;12:171–80. [PubMed] [Google Scholar]


