Abstract
Introduction and Background:
Cleft lip and/or palate is the most common congenital craniofacial anomaly. Prenatal diagnosis of the craniofacial anomalies is possible with the advent of newer imaging modalities. The identification of the defect at an early stage in the pregnancy helps the parents to be well informed and counseled regarding the treatment possibilities and outcomes of cleft lip and palate (CLP) treatment.
Objectives:
To analyze the psychological effects of prenatal diagnosis of CLP on the parents.
Materials and Methods:
PubMed, Cochrane, and Google Scholar searches were made with search strings “prenatal diagnosis cleft lip palate,” “antenatal diagnosis,” “anomaly scan,” “psychological effect cleft lip palate,” and “prenatal counseling cleft lip palate.” Of the results obtained, studies which evaluated the psychological aspects of parents of cleft children were further included in the study.
Results:
Electronic search yielded 500 articles after duplication removal. Forty studies concentrated on the results of the scan and their implications predominantly in the diagnosis and management of cleft and other related abnormalities. Eight studies discussed the effects of prenatal diagnosis and counseling on the parents.
Conclusion:
Prenatal diagnosis enables appropriate and timely counseling of the parents by the cleft team and helps instill a sense of preparedness for the family which highly improves the quality of treatment received by the child enabling a near-to-normal quality and standard of life.
Keywords: Cleft lip and palate, prenatal diagnosis, psychological effect
Introduction
Rationale
Cleft lip with or without palate is the most common congenital birth defect occurring in the population. It has a varied prevalence of 1 in 500–1 in 2500 live births.[1] The prevalence of orofacial clefts varies by race and occurs more frequently among Asians and Native Americans, followed by europeans, Hispanics, and African-Americans. The critical period for cleft development ranges from the 4th to the 12th week of intrauterine life. Clefts of the primary palate develop between the 4th and 7th weeks of intrauterine life, while clefts of the secondary palate develop between the 8th and 12th embryonic weeks.
The relationship of a mother with her child begins during pregnancy in the early and grows over time during the period of pregnancy.[2] When a child is born with a cleft lip and palate (CLP), parents experience various emotional reactions such as shock, sadness, fear, grief, guilt, and anger that disrupt the equilibrium of the family.[3] Parents must be able to successfully handle their feelings, cope with this crisis, and reorganize to meet the needs of their affected child. Not only the facial appearance but also functions such as hearing, phonation, mastication, deglutition, and ventilation are altered by this malformation.[4]
An accurate prenatal diagnosis of the CLP anomaly is critical for establishing long-term treatment planning, prediction of prognosis, and proper counseling with the parent.[5] Although not a routine procedure according to the American Institute of Ultrasound in Medicine, accurate evaluation of craniofacial malformations is usually possible with the ultrasound scan performed during the pregnancy. The accuracy of ultrasonography for prenatal diagnosis of CLP is dependent on the experience of the sonologist, maternal body type, fetal position, the amount of amniotic fluid, and the type of cleft.[6] Three-dimensional (3D) ultrasonography and prenatal magnetic resonance imaging (MRI) improve the accuracy of prenatal diagnosis of orofacial clefts. 3D ultrasonography provides more precise image of the defect and it enhances 2D examination of fetus.[7]
The parents need to be informed and counseled regarding the severity of the cleft deformity and the predicted outcome and options of repair by a trained cleft palate team in association with the radiology team. Although there is no intrauterine treatment for CLP, both mother and child benefit from early diagnosis and counseling. The parents can spend time to adjust with the reality of the malformation as well as adequate time to educate themselves about the condition. Thus, the initial shock of the diagnosis usually can be overcome by a systematic and planned counseling.[8,9] A multidisciplinary team approach is now accepted as the standard of care in dealing with these complex patients.
Objectives
With improvements in the imaging technology and advent of prenatal diagnosis, several centers across the globe are conducting prenatal screening and counseling for the parents. Although many studies dealt the technological aspects of prenatal diagnosis and the counseling for the deformity postbirth, very few studies have discussed the psychological effect of prenatal diagnosis and prenatal counseling on expectant parents. Similarly, there are no systematic reviews that exclusively reviewed this particular aspect of CLP. This review is aimed to through light into the less known and discussed psychological aspect of prenatal diagnosis of CLP deformity and is the first systematic review of this kind.
Materials and Methods
Information sources
PubMed, Cochrane, and Google Scholar electronic searches were made with search strings “prenatal diagnosis cleft lip palate,” “antenatal diagnosis cleft lip palate,” “anomaly scan cleft lip palate,” “psychological effect cleft lip palate,” and “prenatal counselling cleft lip palate.” All the available articles were screened by the authors.
Search criteria
Search terms included (“prenatal diagnosis”[MeSH Terms] OR (“prenatal”[All Fields] AND “diagnosis”[All Fields]) OR “prenatal diagnosis”[All Fields]) AND (“cleft lip”[MeSH Terms] OR (“cleft”[All Fields] AND “lip”[All Fields]) OR “cleft lip”[All Fields]) AND (“palate”[MeSH Terms] OR “palate”[All Fields]) OR (“antenatal”[All Fields] AND “diagnosis”[All Fields]) OR “antenatal diagnosis”[All Fields]) AND (“cleft lip”[MeSH Terms] OR (“prenatal care”[MeSH Terms] OR (“prenatal”[All Fields] AND “care”[All Fields]) OR “prenatal care”[All Fields] OR “prenatal”[All Fields]) AND (“counselling”[All Fields] OR “counselling”[MeSH Terms] OR “counselling”[All Fields]) AND (“cleft lip”[MeSH Terms] OR (“cleft”[All Fields] AND “lip”[All Fields]) OR “cleft lip”[All Fields]) AND (“palate”[MeSH Terms] OR “palate”[All Fields])
Eligibility criteria
Of the results obtained, studies that evaluated the psychological aspects of parents of cleft children were selected and the studies that dealt with the technical aspects were excluded. The abstracts and full text of the selected studies were completely and individually reviewed and only those which dealt with how the prenatal or postnatal diagnosis of the cleft influenced the parents were selected.
Inclusion and exclusion criteria
The studies were selected if they described or made specific mention of prenatal counseling delivered to parents of a baby with a prenatal diagnosis of one or more congenital anomalies or assessed the psychological outcomes associated with prenatal counseling. The studies were excluded if only postnatal counseling was used and if there was no mention of prenatal diagnosis and its usefulness for the child.
Results
The search resulted in 1500 articles. Avoiding duplications, 500 articles were obtained. Most of them dealt the technical aspects of prenatal diagnosis such as the use of ultrasound and its modifications or the use of MRI. Eight studies concentrated on the prenatal diagnosis and its implications on the treatment of the cleft child and the psychological effects on parents and also on how well the parents were able to adjust with the diagnosis and how the diagnosis could be utilized for betterment of the child. Most of the studies were questionnaire based [Figure 1 and Table 1].
Figure 1.
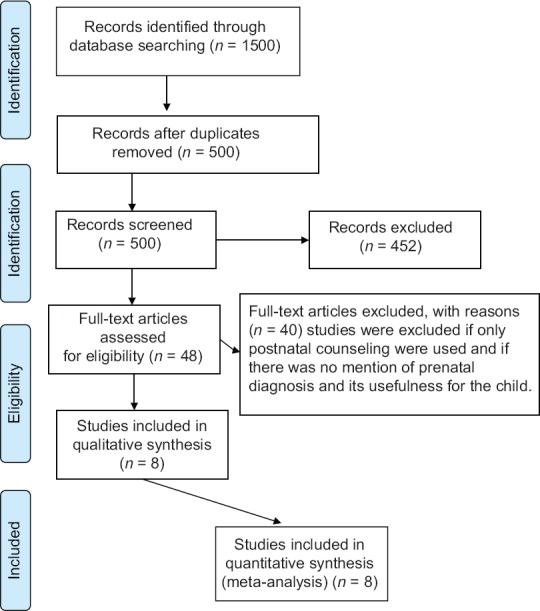
PRISMA checklist flow diagram
Table 1.
Summary of the studies included
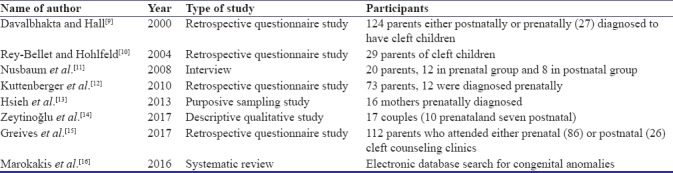
There were 4 retrospective questionnaire surveys, 1 systematic review, 1 interview-based survey, 1 descriptive qualitative study, and 1 purposive sampling study. In all the studies, parental outcomes were assessed after birth. Few of the parents included in the studies had children diagnosed with cleft lip prenatally and received a prenatal counseling by the cleft palate surgery team. Others had not received a prenatal diagnosis and hence attended only the postnatal clinics.
Davalbhakta and Hall[9] conducted a retrospective study of 124 primary cleft lip and/or palate repairs. In their study, 30% were diagnosed antenatally and received antenatal counseling. The rest received postnatal counseling. Of those who had received an antenatal diagnosis, 85% felt that the diagnosis prepared them psychologically for the birth of the child with deformity. Most of the parents who received the prenatal counseling were satisfied with the same and those who felt counseling to be confusing had only postnatal counseling. Most of the parents went ahead with the pregnancy, and since they were well aware of the options for management, they had never thought of terminating the pregnancy.
Rey-Bellet and Hohlfeld[10] evaluated 29 parents who were prenatally diagnosed to have cleft lip/palate babies. Parental reactions at the time of diagnosis varied among them, but most of them had severe psychological shock. Feelings of guilt, anxiety, fear, and sadness were also noticed among the parents. All the parents were explained in detail regarding the deformity and had full satisfaction about the prenatal counseling and diagnosis. Counseling during the antenatal period was considered essential by all the parents. Prenatal diagnosis gave the parents enough time to balance their feelings and accept the child at birth. They had time to warn and prepare family as well as friends.
Nusbaum et al.[11] conducted interviews with 20 parents of children with cleft lip with or without cleft palate to explore parental experiences of a diagnosis. The main discussions were regarding the advantages and disadvantages of prenatal diagnosis, preparedness for birth of child and most of the parents preferred receiving the diagnosis prenatally, and the awareness that the deformity is treatable brought about great satisfaction among the parents. The early diagnosis also helped the parents to have interactions with similar parents and have a better understanding of the condition.
Kuttenberger et al.[12] conducted a questionnaire survey to evaluate parents’ experiences of the first counseling at the cleft center concerning timing and content of the consultation and the quality of the information provided. To reduce anxiety, confusions, and uncertainty, clear and consistent information about the condition, its possible treatments, and prognosis has to be given during the initial counseling at the cleft center.[17]
Hsieh et al.[13] performed a purposive sampling study to identify the psychosocial factors that affect expecting mothers who continue their cleft lip/palate pregnancy to term. Most of the mothers initially experienced a sort of psychological stress and sorrow and had received blames from other relatives. This again concentrates on the necessity of a proper counseling which enables a better care of the child. Else if diagnosed after birth, the initial hiccups among the parents and relatives might lead to the neglect of child, resulting in a poor management.
Zeytinoǧlu et al. and Greives et al.[14,15] also conducted similar studies and were of the similar opinion that a prenatal diagnosis experience provided an opportunity to work as a team with the cleft surgeons and to be supportive of each other. Most of the parents had concerns regarding the well-being of the child and especially regarding the feeding techniques which can be adopted. A thorough prenatal counseling helped alleviate such concerns and led to a more successful parenting.
Discussion
The time period immediately after the diagnosis and the 1st year after the birth is most challenging for parents. Receiving a prenatal diagnosis of CLP is challenging for parents, and there are high levels of psychological distress after diagnosis. A systematically planned counseling will assist the parents to adjust during this difficult time. The primary goal of prenatal counseling is to educate parents about their child's congenital anomaly. The intense emotional waves experienced during counseling hinder parents’ ability to understand the information provided. Hence, repeated counseling by the cleft palate surgeons, gynecologists, maternal–fetal medicine specialists, and psychologists are mandatory.[18] The early diagnosis of the condition also helped the parents to undergo a genetic counseling to identify underlying genetic problems.[19] The counseling should be tailored to individual parents and expert psychologist opinion has to be taken for improving the effectiveness of the counseling.[20] Another important concern for the parents is the use of feeding devices specially manufactured for cleft babies. The initial exposure to these devices is bound to create confusion and apparent anxiety among the parents. With the prenatal diagnosis and the training in the use of these bottles, the problems usually faced after delivery can be minimized.[15] Another concern that could be addressed by a proper prenatal counseling is the parents’ apprehension about the appearance of child and the speech problems that the child may develop. With structured counseling, it is possible to give the parents an insight about these factors.[21] The early counseling of parents also enabled them to have a good backup of internet sources for child care, especially related to feeding of child.
Limitations
This study was performed by a literature review of PubMed, Google Scholar, and Cochrane databases only. Articles in English only were considered. Articles where an electronic edition was not there were not considered for the study. All the studies together evaluated 391 parents only, which is a small sample. Of them, only 50% attended the prenatal clinics. Hence, a broader study which involves a larger sample size is mandatory to evaluate the efficacy of prenatal counseling. Similarly, most studies used a retrospective questionnaire technique which again has limitations because only few questions were raised. The difference in pattern of questions also exists, and a proper standardization of results is not possible with the existing data.
Conclusion
Prenatal ultrasound imaging is an important diagnostic tool used in the evaluation and treatment of pregnant women. With advances in technology, the resolution and image quality have considerably improved, and newer modalities such as 3D/4D ultrasound and MRI of the child are gaining popularity in the field of prenatal diagnosis of congenital abnormalities. The presence of a congenital anomaly like cleft lip/palate has a severe effect on the general psychological well-being of the parents. If the condition can be identified early in the prenatal period itself, the parents can take help from the cleft surgeons and get a very good idea regarding the possible methods of treatment and be well prepared to have a child with the deformity. The aim of prenatal counseling is to educate and create awareness among parents about the child's congenital anomaly. The intense emotions experienced during counseling may hinder parents’ ability to understand the information provided, and parents may need and benefit from additional information, this helps in the overall betterment of the parents as well as the child, especially in a situation which demands early intervention for good results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.IPDTOC Working Group. Prevalence at birth of cleft lip with or without cleft palate: Data from the international perinatal database of typical oral clefts (IPDTOC) Cleft Palate Craniofac J. 2011;48:66–81. doi: 10.1597/09-217. [DOI] [PubMed] [Google Scholar]
- 2.Heidrich SM, Cranley MS. Effect of fetal movement, ultrasound scans, and amniocentesis on maternal-fetal attachment. Nurs Res. 1989;38:81–4. [PubMed] [Google Scholar]
- 3.Steinberg JP, Gosain AK. Thirty years of prenatal cleft diagnosis: What have we learned? Plast Reconstr Surg. 2015;136:550–7. doi: 10.1097/PRS.0000000000001533. [DOI] [PubMed] [Google Scholar]
- 4.Baker SR, Owens J, Stern M, Willmot D. Coping strategies and social support in the family impact of cleft lip and palate and parents’ adjustment and psychological distress. Cleft Palate Craniofac J. 2009;46:229–36. doi: 10.1597/08-075.1. [DOI] [PubMed] [Google Scholar]
- 5.Jones MC. Prenatal diagnosis of cleft lip and palate: Detection rates, accuracy of ultrasonography, associated anomalies, and strategies for counseling. Cleft Palate Craniofac J. 2002;39:169–73. doi: 10.1597/1545-1569_2002_039_0169_pdocla_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 6.Evans MI, Hume RF, Jr, Johnson MP, Treadwell MC, Krivchenia EL, Zador IE, et al. Integration of genetics and ultrasonography in prenatal diagnosis: Just looking is not enough. Am J Obstet Gynecol. 1996;174:1925–31. doi: 10.1016/s0002-9378(96)70230-2. [DOI] [PubMed] [Google Scholar]
- 7.Wang LM, Leung KY, Tang M. Prenatal evaluation of facial clefts by three-dimensional extended imaging. Prenat Diagn. 2007;27:722–9. doi: 10.1002/pd.1766. [DOI] [PubMed] [Google Scholar]
- 8.Matthews MS, Cohen M, Viglione M, Brown AS. Prenatal counseling for cleft lip and palate. Plast Reconstr Surg. 1998;101:1–5. doi: 10.1097/00006534-199801000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Davalbhakta A, Hall PN. The impact of antenatal diagnosis on the effectiveness and timing of counselling for cleft lip and palate. Br J Plast Surg. 2000;53:298–301. doi: 10.1054/bjps.2000.3330. [DOI] [PubMed] [Google Scholar]
- 10.Rey-Bellet C, Hohlfeld J. Prenatal diagnosis of facial clefts: Evaluation of a specialised counselling. Swiss Med Wkly. 2004;134:640–4. doi: 10.4414/smw.2004.10547. [DOI] [PubMed] [Google Scholar]
- 11.Nusbaum R, Grubs RE, Losee JE, Weidman C, Ford MD, Marazita ML, et al. A qualitative description of receiving a diagnosis of clefting in the prenatal or postnatal period. J Genet Couns. 2008;17:336–50. doi: 10.1007/s10897-008-9152-5. [DOI] [PubMed] [Google Scholar]
- 12.Kuttenberger J, Ohmer JN, Polska E. Initial counselling for cleft lip and palate: Parents’ evaluation, needs and expectations. Int J Oral Maxillofac Surg. 2010;39:214–20. doi: 10.1016/j.ijom.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 13.Hsieh YT, Chao YM, Shiao JS. A qualitative study of psychosocial factors affecting expecting mothers who choose to continue a cleft lip and/or palate pregnancy to term. J Nurs Res. 2013;21:1–9. doi: 10.1097/jnr.0b013e3182828dbd. [DOI] [PubMed] [Google Scholar]
- 14.Zeytinoǧlu S, Davey MP, Crerand C, Fisher K, Akyil Y. Experiences of couples caring for a child born with cleft lip and/or palate: Impact of the timing of diagnosis. J Marital Fam Ther. 2017;43:82–99. doi: 10.1111/jmft.12182. [DOI] [PubMed] [Google Scholar]
- 15.Greives MR, Anderson CL, Dean RA, Scerbo ML, Doringo IL, Bebbington MW, et al. Survey of parent experiences in prenatal visits for infants with cleft lip and palate. Cleft Palate Craniofac J. 2017;54:668–73. doi: 10.1597/16-036. [DOI] [PubMed] [Google Scholar]
- 16.Marokakis S, Kasparian NA, Kennedy SE. Prenatal counselling for congenital anomalies: A systematic review. Prenat Diagn. 2016;36:662–71. doi: 10.1002/pd.4836. [DOI] [PubMed] [Google Scholar]
- 17.Hunfeld JA, Tempels A, Passchier J, Hazebroek FW, Tibboel D. Brief report: Parental burden and grief one year after the birth of a child with a congenital anomaly. J Pediatr Psychol. 1999;24:515–20. doi: 10.1093/jpepsy/24.6.515. [DOI] [PubMed] [Google Scholar]
- 18.Aite L, Trucchi A, Nahom A, Casaccia G, Zaccara A, Giorlandino C, et al. Antenatal diagnosis of diaphragmatic hernia: Parents’ emotional and cognitive reactions. J Pediatr Surg. 2004;39:174–8. doi: 10.1016/j.jpedsurg.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 19.Petrucelli N, Walker M, Schorry E. Continuation of pregnancy following the diagnosis of a fetal sex chromosome abnormality: A Study of parents’ counseling needs and experiences. J Genet Couns. 1998;7:401–15. doi: 10.1023/A:1022828715158. [DOI] [PubMed] [Google Scholar]
- 20.Kolker A, Burke BM. Grieving the wanted child: Ramifications of abortion after prenatal diagnosis of abnormality. Health Care Women Int. 1993;14:513–26. doi: 10.1080/07399339309516081. [DOI] [PubMed] [Google Scholar]
- 21.Hasanzadeh N, Khoda MO, Jahanbin A, Vatankhah M. Coping strategies and psychological distress among mothers of patients with nonsyndromic cleft lip and palate and the family impact of this disorder. J Craniofac Surg. 2014;25:441–5. doi: 10.1097/SCS.0000000000000483. [DOI] [PubMed] [Google Scholar]


