Abstract
Eagle's syndrome (ES) refers to a group of various types and patterns of pain which spans over the head-and-neck region owing to an elongated styloid process or calcified stylohyoid ligament. These symptoms are often confused with those attributed to a wide variety of facial neuralgias. The diagnosis of ES is usually made through clinical exclusion which is then confirmed radiographically. Patients with ES are initially managed with nonsurgical therapy, but surgical resection seems to be the treatment of choice. The styloid process shortening can be achieved through an intraoral or extraoral approach. This clinical case report describes such a case of ES after sustaining neck trauma.
Keywords: Eagle's syndrome, elongated styloid process, neck trauma
Introduction
Eagle's syndrome (ES) refers to a rare constellation of symptoms caused by an abnormally long styloid process or stylohyoid chain ossification which is characterized by craniofacial or cervical pain. It was first described by an Italian surgeon, Piertro Marchetti in 1652; however, the clinical syndrome was definitively outlined by Eagle in the late early 1950s.[1] ES is an uncommon condition which comprises 4% of the population with an elongated styloid process.[2] It can be divided into two types; classic type and carotid type.[1,3] In the classic type of ES, compressive cranial neuropathy most commonly leads to the sensation of a foreign body in the throat, odynophagia, and dysphagia. In the carotid type, compression over the internal carotid artery can cause pain in the parietal region of the skull or in the superior periorbital region. Since the symptoms are variable and nonspecific, patients usually seek treatment from several different specialties such as otolaryngology, maxillofacial surgery, neurology, neurosurgery, and finally psychiatry.
Case Report
A 50-year-old Indian man was referred to the Hospital Universiti Sains Malaysia, Oral and Maxiilofacial Surgery Unit for persistent pain for almost 2 years over the right side of the neck which radiates ipsilaterally over to the face, temporal, and occipital area. He revealed later that he had sustained a fall preceding to the recurrent episodes of pain. The patient stated that he momentarily lost his balance at work which resulted in the right side of his neck hitting the staircase. He seeks treatment at a local hospital and was discharged on the same day after being diagnosed with a laceration wound over the right side of the neck without any hard tissue injury. The patient has no other associated medical illnesses.
He began experiencing short episodes of sharp pain over the right angle of mandible area 6 months after his fall. It was tolerable in the beginning, but, he started to be dependent on “over-the-counter” pain medication for symptomatic relief. These, however, only lasted him for another 6 months. The patient was given intramuscular diclofenac sodium injections at the local hospital as the nature, intensity, and distribution of pain has progressed over time. It had transformed to long episodes of severe “throbbing and stabbing” pain which radiates to the right side of the face. The oral medicine clinic initially excluded pain of dental origin by extracting an irrestorable nonvital lower right first molar and diagnosed him as a case of trigeminal neuralgia as other clinical examination of mandibular motion, both temporomandibular joints and masticatory musculature were unremarkable. He was embarked on various pharmacologic therapies for pain relief that eventually failed. The inability to rotate his head to contralateral side exacerbated his symptoms. Retrospective reviews of the orthopantomograph revealed an elongated right styloid process which was more apparent when compared to the contralateral side [Figure 1]. Subsequent 3D-cone beam computed tomography studies confirmed the previous finding of an elongated right styloid process measuring 48 mm [Figures 2 and 3]. The left styloid measured 37 mm. Diagnosis of ES was then assumed, and the patient underwent right partial styloidectomy under general anesthesia through an extraoral approach [Figures 4 and 5]. The resected segment was 26 mm in length [Figure 6]. The patient was reviewed postoperatively and was found be free from pain.
Figure 1.

Orthopantomograph revealed an elongated right styloid process
Figure 2.

3D cone-beam computed tomography showed an elongated right styloid process
Figure 3.
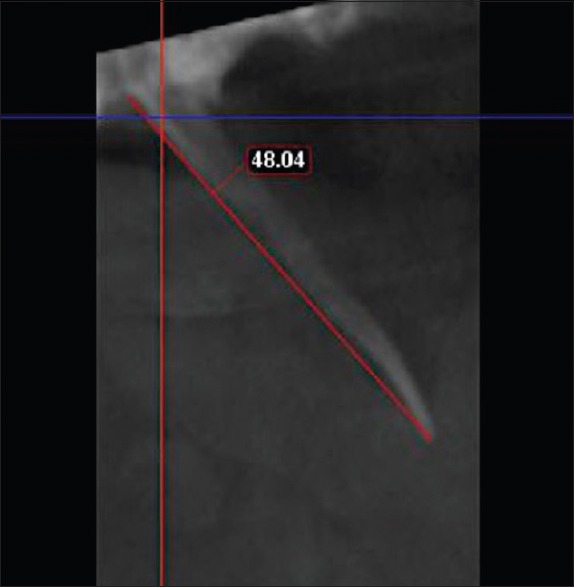
Styloid process measuring 48 mm in length
Figure 4.

Right partial styloidectomy through an extraoral approach
Figure 5.
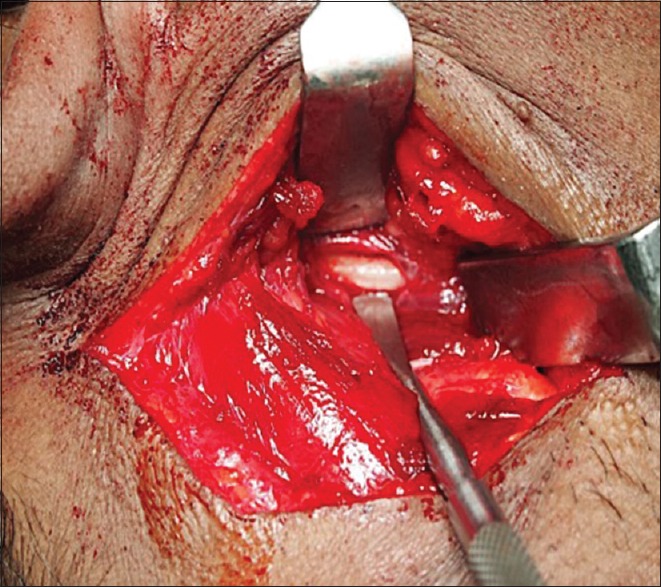
Right partial styloidectomy through an extraoral approach
Figure 6.

Resected styloid process of 26 mm in length
Discussion
The styloid process arises from the temporal bone just anteromedial to stylomastoid foramen. It is part of the stylohyoid complex consisting of the stylohyoid ligament and lesser horn of hyoid bone which derives from 2nd branchial arch of Reichert cartilage. The styloglossus, stylohyoid, and stylopharyngeus muscles are attached to the styloid process. Other attachments include the stylohoid and stylomandibular ligaments.
The tip of styloid process is usually situated between the internal and external carotid arteries. It also has a close relationship to other neurovascular structures in the neck i.e., V, VII, IX, X, XI, XII cranial nerves, and the internal jugular vein. The proximity of the aforementioned structures to the styloid process plays a crucial role in the pathophysiology of ES.[4] Eagle reported that the normal styloid process is approximately 2.5–3.0 cm in length. The length and direction of the styloid process and styloid chain are highly variable. By consensus, a styloid process longer than 30 mm confers an increased risk of ES.[5]
Eagle also noted that patients display severe symptoms of atypical facial pain when there is slight medial deviation of the elongated styloid process, stylohyoid ligament calcifications, or both.[6,7] He has described and categorized patients into two groups: Those who had classical symptoms of a palpable mass in the tonsillar region following tonsillectomy with “foreign body” sensation in the throat; and those with radiating pain in the neck and face following the carotid artery distribution (carotid artery syndrome). In the carotid type, pain in the parietal region of the skull or in the superior periorbital region is caused by the compression over the internal carotid artery[8] whereas pain in the ipsilateral face and neck is due to compression of external carotid artery branches.[9] Although these two types of ES have a common etiology, their symptomatology differs.[7] Our presented case represents “carotid artery syndrome” type of symptoms on the right side of his face and neck.
Although the classical descriptions of this condition were seen in patients with a history of tonsillectomy,[3] the pathophysiology of symptoms is not well understood. Factors believed as possible causes include previous trauma or an inflammatory process that produces a proliferation of granulation tissue and results in the calcification or ossification of the styloid process or the styloid chain itself.[10] Our patient has no history of tonsillectomy which could have manifest as trauma that initiated the calcification or ossification of the styloid process. However, as mentioned before, he did experience external trauma through a fall resulting in an injury over the right angle of mandible area. We postulated that this would have caused significant inflammatory and granulation tissue response in promoting the elongation or calcification of the right styloid process as compared to the contralateral side.[11] Mangano and Nylander reported a case of ES that occurred after an automobile accident and caused by cervicopharyngeal trauma.[12] Similar cases of traumatic ES have been reported by the previous studies.[13,14,15]
Given the variation in the clinical presentation of ES, the differential diagnosis is broad and includes atypical facial pain, trigeminal neuralgia, glossopharyngeal neuralgia,[16,17] occipital neuralgia,[18] sphenopalatine neuralgia, temporomandibular disorders,[19,20] dental infection,[21] tonsillitis,[22] mastoiditis,[23] and migraine.[18] Therefore, the role of trauma was misidentified initially as we had to exclude all other causes before diagnosing the patient with ES.
After establishing the final diagnosis, we opted to pursue with the option of surgical resection of the right styloid process as all noninvasive treatment of the neuropathic sequelae of the patient's condition have failed. These included various oral agents including gabapentin, amitriptyline, valproate, and carbamazepine.
An extraoral approach was preferred as the patient had not undergone tonsillectomy [Figures 4 and 5]. This approach provides better visualization and sterility as opposed to the risks of an intraoral route such as poor hemorrhage control, possible deep space neck infections, and airway edema which may compromise speech and swallowing.[24] We carried out a partial resection of the right styloid process measuring at 26 mm as we found it was not necessary to remove it at full length. This was done with reason that partial resection leaving 23 mm of the styloid was adequate to decompress the carotid vessels. We also did want to exert additional surgical morbidity by manipulating the carotid triangle area excessively to approach the proximal segment of the styloid process. The postsurgical recovery was uneventful, and the patient no longer exhibits unbearable episodes of pain as described previously.
Conclusion
ES can be diagnosed by thorough history and clinical examination which correlate with radiographical studies. It is often confused with other conditions which need be excluded prior achieving definitive diagnosis. Resection of the elongated styloid process has the most predictable outcome of success in reducing or eliminating the patient's symptoms.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Eagle WW. Elongated styloid process; Further observations and a new syndrome. Arch Otolaryngol. 1948;47:630–40. doi: 10.1001/archotol.1948.00690030654006. [DOI] [PubMed] [Google Scholar]
- 2.Murtagh RD, Caracciolo JT, Fernandez G. CT findings associated with eagle syndrome. AJNR Am J Neuroradiol. 2001;22:1401–2. [PMC free article] [PubMed] [Google Scholar]
- 3.Eagle WW. Elongated styloid process; Symptoms and treatment. AMA Arch Otolaryngol. 1958;67:172–6. doi: 10.1001/archotol.1958.00730010178007. [DOI] [PubMed] [Google Scholar]
- 4.Fusco DJ, Asteraki S, Spetzler RF. Eagle's syndrome: Embryology, anatomy, and clinical management. Acta Neurochir (Wien) 2012;154:1119–26. doi: 10.1007/s00701-012-1385-2. [DOI] [PubMed] [Google Scholar]
- 5.Kaufman SM, Elzay RP, Irish EF. Styloid process variation. Radiologic and clinical study. Arch Otolaryngol. 1970;91:460–3. doi: 10.1001/archotol.1970.00770040654013. [DOI] [PubMed] [Google Scholar]
- 6.Eagle WW. Symptomatic elongated styloid process report of two cases of styloid process–carotid artery syndrome with operation. Arch Otolaryngol. 1949;49:490–503. doi: 10.1001/archotol.1949.03760110046003. [DOI] [PubMed] [Google Scholar]
- 7.Breault MR. Eagle's syndrome: Review of the literature and implications in craniomandibular disorders. Cranio. 1986;4:323–37. doi: 10.1080/08869634.1986.11678161. [DOI] [PubMed] [Google Scholar]
- 8.Massey EW. Facial pain from an elongated styloid process (Eagle's syndrome) South Med J. 1978;71:1156–9. doi: 10.1097/00007611-197809000-00030. [DOI] [PubMed] [Google Scholar]
- 9.Petrović B, Radak Ð, Kostić V, Čovičković-Šternić N. Stylocarotid syndrome: A case report. Srp Arh Celok Lek. 2008;136:650–3. doi: 10.2298/sarh0812650p. [DOI] [PubMed] [Google Scholar]
- 10.Restrepo S, Palacios E, Rojas R. Eagle's syndrome. Ear Nose Throat J. 2002;81:700–1. [PubMed] [Google Scholar]
- 11.Oluseisi A. Traumatic eagle syndrome: Does neck trauma result in complete ossification in partially ossified stylohyoid ligament. Int J Otorhinolaryngol. 2006;4:2. [Google Scholar]
- 12.Piagkou M, Anagnostopoulou S, Kouladouros K, Piagkos G. Eagle's syndrome: A review of the literature. Clin Anat. 2009;22:545–58. doi: 10.1002/ca.20804. [DOI] [PubMed] [Google Scholar]
- 13.Smith RG, Cherry JE. Traumatic eagle's syndrome: Report of a case and review of the literature. J Oral Maxillofac Surg. 1988;46:606–9. doi: 10.1016/0278-2391(88)90153-x. [DOI] [PubMed] [Google Scholar]
- 14.Schroeder WA., Jr Traumatic eagle's syndrome. Otolaryngol Head Neck Surg. 1991;104:371–4. doi: 10.1177/019459989110400314. [DOI] [PubMed] [Google Scholar]
- 15.Boscainos PJ, Papagelopoulos PJ, Goudelis G, Partsinevelos A, Nikolopoulos K, Korres DS. Eagle's syndrome. Orthop N J. 2004;27:423–7. doi: 10.3928/0147-7447-20040401-23. [DOI] [PubMed] [Google Scholar]
- 16.Slavin KV. Eagle syndrome: Entrapment of the glossopharyngeal nerve? Case report and review of the literature. J Neurosurg. 2002;97:216–8. doi: 10.3171/jns.2002.97.1.0216. [DOI] [PubMed] [Google Scholar]
- 17.Shin JH, Herrera SR, Eboli P, Aydin S, Eskandar EH, Slavin KV, et al. Entrapment of the glossopharyngeal nerve in patients with eagle syndrome: Surgical technique and outcomes in a series of 5 patients. J Neurosurg. 2009;111:1226–30. doi: 10.3171/2009.1.JNS08485. [DOI] [PubMed] [Google Scholar]
- 18.Montalbetti L, Ferrandi D, Pergami P, Savoldi F. Elongated styloid process and eagle's syndrome. Cephalalgia. 1995;15:80–93. doi: 10.1046/j.1468-2982.1995.015002080.x. [DOI] [PubMed] [Google Scholar]
- 19.de Souza EA, Hotta TH, Bataglion C. Association of a temporomandibular disorder and eagle's syndrome: Case report. Braz Dent J. 1996;7:53–8. [PubMed] [Google Scholar]
- 20.Ferreira de Albuquerque R, Jr, Müller K, Hotta TH, Gonçalves M. Temporomandibular disorder or eagle's syndrome? A clinical report. J Prosthet Dent. 2003;90:317–20. doi: 10.1016/s0022-3913(03)00522-5. [DOI] [PubMed] [Google Scholar]
- 21.Aral IL, Karaca I, Güngör N. Eagle's syndrome masquerading as pain of dental origin. Case report. Aust Dent J. 1997;42:18–9. doi: 10.1111/j.1834-7819.1997.tb00090.x. [DOI] [PubMed] [Google Scholar]
- 22.Fritz M. Elongated styloid process: A cause of obscure throat symptoms. Arch Otolaryngol. 1940;31:911–8. [Google Scholar]
- 23.Douglas TE., Jr Facial pain from elongated styloid process. AMA Arch Otolaryngol. 1952;56:635–8. doi: 10.1001/archotol.1952.00710020660007. [DOI] [PubMed] [Google Scholar]
- 24.Chase DC, Zarmen A, Bigelow WC, McCoy JM. Eagle's syndrome: A comparison of intraoral versus extraoral surgical approaches. Oral Surg Oral Med Oral Pathol. 1986;62:625–9. doi: 10.1016/0030-4220(86)90253-7. [DOI] [PubMed] [Google Scholar]


