Abstract
Background and Objectives
Practicing clinical nephrologists are performing fewer diagnostic kidney biopsies. Requiring biopsy procedural competence for graduating nephrology fellows is controversial.
Design, Setting, Participants, & Measurements
An anonymous, on-line survey of all Walter Reed training program graduates (n=82; 1985–2017) and all United States nephrology program directors (n=149; August to October of 2017), regarding kidney biopsy practice and training, was undertaken.
Results
Walter Reed graduates’ response and completion rates were 71% and 98%, respectively. The majority felt adequately trained in native kidney biopsy (83%), transplant biopsy (82%), and tissue interpretation (78%), with no difference for ≤10 versus >10 practice years. Thirty-five percent continued to perform biopsies (13% did ≥10 native biopsies/year); 93% referred at least some biopsies. The most common barriers to performing biopsy were logistics (81%) and time (74%). Program director response and completion rates were 60% and 77%. Seventy-two percent cited ≥1 barrier to fellow competence. The most common barriers were logistics (45%), time (45%), and likelihood that biopsy would not be performed postgraduation (41%). Fifty-one percent indicated that fellows should not be required to demonstrate minimal procedural competence in biopsy, although 97% agreed that fellows should demonstrate competence in knowing/managing indications, contraindications, and complications. Program directors citing ≥1 barrier or whose fellows did <50 native biopsies/year in total were more likely to think that procedural competence should not be required versus those citing no barriers (P=0.02), or whose fellows performed ≥50 biopsies (P<0.01).
Conclusions
Almost two-thirds of graduate respondents from a single military training program no longer perform biopsy, and 51% of responding nephrology program directors indicated that biopsy procedural competence should not be required. These findings should inform discussion of kidney biopsy curriculum requirements.
Keywords: Biopsy, Contraindications, Curriculum, Fellowships and Scholarships, Interventional Radiology, kidney biopsy, Military Personnel, Nephrologists, nephrology, Nephrology Education, Nephrology Fellowship, Program Directors, Surveys and Questionnaires, Thinking, Transplants, United States
Introduction
Diagnostic kidney biopsy is performed increasingly by interventional radiology (IR). It is controversial whether biopsy should remain a “core” procedure for nephrology fellows (1–4). Surveys indicate that curriculum varies, up to 20% of graduating fellows do not feel prepared to perform biopsy, and many feel inadequately prepared to interpret tissue (2,4,5). In some programs, IR physicians exclusively supervise fellows, and nephrology faculty no longer attend the biopsy.
In the early 1990s, ultrasound visualization and automated spring-loaded needles were introduced for kidney biopsy at the Walter Reed fellowship program. By 1999, biopsy was done under real-time ultrasound in the nephrology infusion clinic, with IR handling the transducer, and nephrology fellows/faculty performing the biopsy. By the late 2000s, a pathologist attended, to ensure sufficient tissue was obtained.
In the late 1990s, we introduced a minimum requirement of five native/two transplant biopsies, and simulation training under real-time ultrasound (6,7). We have a long-standing, nephropathologist-led, monthly biopsy conference, and tissue interpretation is taught systematically. All native biopsies and some transplant biopsies are reviewed. Since 2010, all fellows attend a formal kidney biopsy histopathology interpretation course.
After 2012, it became increasingly complex and time-consuming to coordinate biopsies in the infusion clinic. IR workflow prevented radiologist flexibility. We began directly referring to IR, who performed the biopsy in the IR suite with a pathologist present. Referring fellows perform biopsies on their patients, with oversight by IR. Nephrology faculty may be present, but are not primarily responsible for the procedure. Biopsies referred by faculty are often done entirely by IR.
We retrospectively assessed biopsy safety, procedure number, and tissue adequacy for 2 years before and after this practice change, for all native biopsies referred/performed by nephrology for 2013–2014 (pre) versus 2015–2016 (post). Native biopsies increased (47 pre versus 80 post). Biopsies per fellow increased (4.3 to 10.1 per fellow per year). Complication rates were unchanged, with major complications (including gross hematuria) of 4% pre and 5% post. There were no deaths. Nondiagnostic biopsy frequency was not different: 8% versus 4%. These outcomes are similar to other reports (8,9).
Because of our recent curricular changes, and the perception that kidney biopsy was increasingly referred, rather than performed, by nephrologists, we conducted anonymous surveys of Walter Reed graduates’ training satisfaction and clinical practice and United States nephrology program directors’ educational practices to inform future biopsy training.
Materials and Methods
The protocol (#886423) was approved by the Walter Reed National Military Medical Center Department of Research Protections as “exempt” per 32 CFR 219.101(b) (2).
All 82 nephrologists who graduated from the Walter Reed nephrology training program from June 30, 1985 to June 30, 2017 were anonymously surveyed regarding kidney biopsy practice and whether training adequately prepared them for performing and interpreting native and transplant kidney biopsies. The 19-question survey (Supplemental Material) was performed using SurveyMonkey, with respondent internet protocol addresses blocked. The survey could be taken only once from the same device. The link was delivered by email (n=73) or fax (n=9), with delivery receipt. The survey was open from 10 July to September 10, 2017. Reminders were sent at 2-week intervals. The first question asked whether the respondent was “working as a nephrologist in clinical practice managing nephrology patients.” If “no,” respondents were directed away from the survey to a “Thank you for your participation” page. If “yes,” respondents were directed into the survey. Respondents were asked to indicate number of years in practice (including fellowship training), their present geographic area of practice (10), whether they practiced interventional nephrology, and if their practice was primarily rural, suburban, or urban.
All 149 nephrology program directors were anonymously surveyed (22 questions) regarding their kidney biopsy and tissue interpretation curriculum (Supplemental Material), using SurveyMonkey. Associate program directors and division chiefs were not surveyed. Respondent internet protocol addresses were blocked. The survey could be taken only once from the same device. Program directors were identified from the Public List of Nephrology Specialty programs from the Accreditation Council for Graduate Medical Education website (https://apps.acgme.org/ads/Public/Reports/ReportRun?ReportId=1&CurrentYear=2016&SpecialtyId=26&IncludePreAccreditation=false). The link was delivered by email (n=147) or fax (n=2), with delivery receipt. The survey was open from 10 August to October 10, 2017, and reminders were sent at 2-week intervals. The first question asked whether the respondent was the nephrology program director. If not, the respondent was directed away from the survey, and asked to forward the link to the program director. Program directors were then asked to indicate number of years in practice (including fellowship training), clinical fellow number, and numbers of institutional and fellow-performed biopsies. The remaining questions involved biopsy and tissue interpretation curriculum, barriers to fellow competency, and whether biopsy performance competence should be required for all fellows.
Statistical Analyses
Percentages, medians (range), and mean (SD) are reported as appropriate. Response frequencies were compared using Fisher’s exact test. P<0.05 (two-tailed) was considered significant.
Results
Graduate Survey
There was a 71% response rate (58 of 82). Median survey time was 4 minutes. Fifty-five respondents (67%) were in clinical practice. Completion rate was 98% (54 of 55; see the Supplemental Material for flow of respondents through the survey). Twenty-three (43%) had been in practice ≤10 years, 33 (61%) practiced in the southern United States, and 1 (2%) was an interventional nephrologist. Forty-six (85%) practiced in an urban (n=24) or suburban (n=22) setting. Response rate for those in practice ≤10 years was 96%, and 54% for practice >10 years.
The majority agreed/strongly agreed they were adequately prepared to perform native (83%) and transplant (82%) biopsies without direct supervision, and to interpret biopsy tissue (78%). There was no significant difference between those in practice ≤10 years versus >10 years (Table 1).
Table 1.
Graduate survey of kidney biopsy training adequacy
| Survey Question | Agree or Strongly Agree | Neither Agree nor Disagree | Disagree or Strongly Disagree | Other | P Value |
|---|---|---|---|---|---|
| Q6. I was adequately prepared to perform native kidney biopsies without direct supervision at the end of my nephrology fellowship. | 45 (83%) | 2 | 7 | ||
| Association of Q6 responses to time in clinical practice | |||||
| Clinical practice 10 yr or less | 19 (83%) | 4 | >0.99 | ||
| Clinical practice >10 yr | 26 (84%) | 5 | |||
| Q7. I was adequately prepared to perform transplant kidney biopsies without direct supervision at the end of my nephrology fellowship. | 44 (82%) | 4 | 6 | ||
| Association of Q7 responses to time in clinical practice | |||||
| Clinical practice 10 yr or less | 21 (91%) | 2 | 0.16 | ||
| Clinical practice >10 yr | 23 (74%) | 8 | |||
| Q8. I was adequately prepared to perform interpretation of kidney biopsy tissue at the end of my nephrology fellowship. | 41 (78%) | 5 | 7 | ||
| Association of Q8 response to time in clinical practice | |||||
| Clinical practice 10 yr or less | 17 (74%) | 6 | 0.74 | ||
| Clinical practice >10 yr | 25 (81%) | 6 |
Q, question number.
Thirty-five percent (n=19) performed native biopsies; 30% (n=16) did transplant biopsies. Of these, 37% (n=7) did ≥10 native biopsies/year; 13% (n=2) did ≥10 transplant biopsies/year. Median native biopsies/year was seven (range 2–42), and median transplant biopsies/year was two (0–10). Those in practice ≤10 years were no more likely to perform biopsies than those in practice >10 years (35% versus 36%). There was no significant difference on the basis of practice geography (southern 33% versus other 38%, P=0.76; rural 13% versus suburban/urban 39%, P=0.24). Thirteen percent (n=7) never performed a native biopsy after graduation, and 26% (n=14) never did a transplant biopsy. Of those in practice ≤10 years, 15 (65%) never performed biopsies or stopped within 5 years.
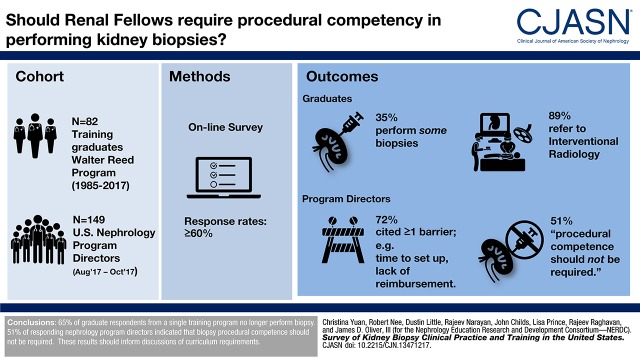
Of the 19 continuing to perform biopsies, four never refer to another practitioner. All use real-time ultrasound for visualization, but two also employ ultrasound or computed tomography localization. Fifteen (79%) of those continuing to perform biopsies refer some to IR. Eighty-nine percent of all graduates (48 of 54) refer some or all biopsies specifically to IR. Reasons for continuing to perform biopsies are shown in Figure 1A. The most frequently cited reasons were enjoyment of the procedure, and the opinion that all nephrologists should be willing/able to perform it.
Figure 1.
Walter Reed graduate opinions regarding kidney biopsy (1985–2017). (A) Reasons for continuing to perform kidney biopsy (n=19). (B) Barriers to performing kidney biopsy (n=54). Adeq, adequate; Post-Bx, post-biopsy; RVU, relative value units.
Barriers to performing biopsies are shown in Figure 1B. The most frequently cited barriers were logistics of setting up the biopsy (81%), time to do it (74%), complication risk (44%), and skill loss (due to low volume) (41%). Only four respondents (7%) perceived no barriers.
Program Director Survey
Response rate was 60% (90 of 149). Median survey time was 7 minutes. Completion rate was 77% (69 of 90; see the Supplemental Material for flow of respondents through the survey). In the 2016–2017 training year, median clinical fellow number (first+second year) was six (range 0–20), with 90 program directors reporting.
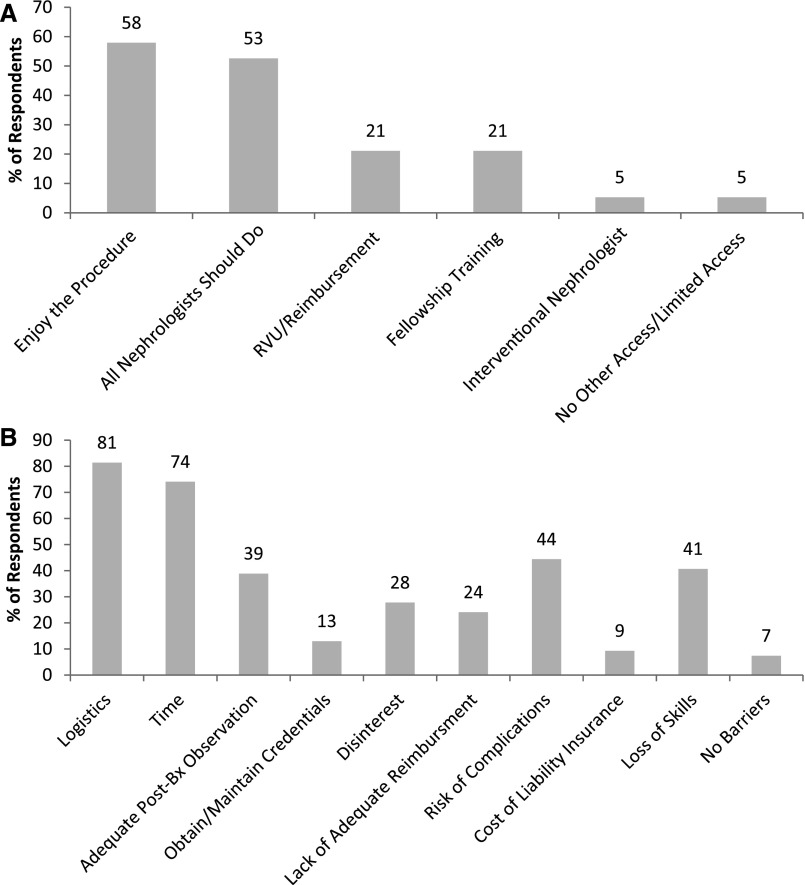
Figure 2 shows the number of native biopsies available to fellows and the number performed by fellows. “Available” biopsies are all those performed at the institution, whether by fellows or others. In the 2016–2017 training year, 37% reported <20 fellow-performed native biopsies/year, but only 4% reported <20 biopsies/year available. Among 52 programs with data, median number of native biopsies performed/fellow per year was 4 (range 0–25). However, 85% had ≥5 native biopsies available/fellow per year. The median available/fellow per year was 11 (range 1–100).
Figure 2.
Number of native kidney biopsies performed by fellows and available to institution (done institution-wide) in training year 2016–2017. Program director respondents n=70; median number of clinical fellows/program=6. TY, training year.
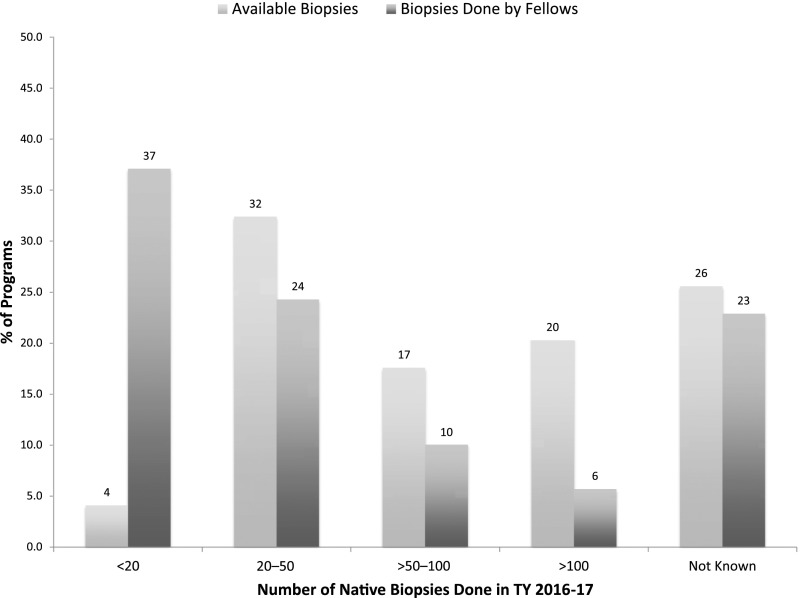
Sixty-two percent of program directors reported having a minimum biopsy number requirement to demonstrate readiness for unsupervised practice. The distribution for native biopsies is shown in Figure 3. The most common minimum was five native biopsies per fellow (33%). When asked what the minimum should be (if any), the number shifted upward, with 20% favoring a minimum of ten, and 19% favoring a minimum of five (Figure 3). Thirty-eight percent did not indicate a minimum, with many replying it should be individualized to observed competence.
Figure 3.
Required minimum number of native biopsies performed and desirable minimum number to demonstrate fellow competence (program director respondents n=69).
In the 2016–2017 training year (54 programs with data), median transplant biopsies performed/fellow per year was 2.5 (range 0–25). Median available/fellow was 10.8 (range 0–108). The most commonly reported minimum threshold was five (29%), with 33% having no minimum. When program directors were asked what the minimum should be, the number again shifted upward, with 3% favoring a minimum of five, 23% favoring a minimum of six, and 13% favoring a minimum of 15.
In 51% of programs, nephrology faculty supervise all native biopsies, whereas IR faculty supervise all native biopsies in 20%, and some in 45% of programs. The most common visualization method is real-time ultrasound (88%). In addition to directly performing patient biopsy, 43% offer simulation training, and 14% offer an interventional rotation.
Features of the tissue interpretation curriculum are shown in Table 2. An internal lecture series systematically reviewing biopsy interpretation is offered by 51%, and 19% send fellows to an external biopsy tissue interpretation course. Eighty-eight percent of programs have a nephropathologist at their institution, 81% have a formal biopsy coconference with pathology, and 81% hold the conference at least monthly.
Table 2.
Program training practices
| Kidney Biopsy Training (n=69) | 100% | >75%–99% | >50%–75% | >25%–50% | >0%–25% | % Programs |
|---|---|---|---|---|---|---|
| Q17. Faculty oversight (native biopsy), % | ||||||
| Nephrology | 51 | 9 | 0 | 6 | 13 | |
| Interventional nephrology | 1 | 1 | 1 | 3 | 1 | |
| Interventional radiology | 19 | 13 | 1 | 1 | 10 | |
| Other | 2a | 0 | 0 | 0 | 1 | |
| Q18. Kidney visualization (n=69) | ||||||
| Real-time ultrasound | 88 | |||||
| Ultrasound localization | 15 | |||||
| CT localization | 30 | |||||
| Fluoroscopy | 3 | |||||
| Physical landmarks | 0 | |||||
| Q22. Training other than clinical biopsy performance (n=69) | ||||||
| Biopsy simulation under real-time ultrasound at the training program | 36 | |||||
| Attending a biopsy simulation course at another site | 7 | |||||
| Internal lecture series at which tissue interpretation is systematically reviewed | 51 | |||||
| Attending an external kidney biopsy tissue interpretation training course | 19 | |||||
| Interventional nephrology rotation supervised by IR or interventional nephrology | 15 | |||||
| Otherb | 19 | |||||
| No other specific training | 15 | |||||
| Nephropathology training (n=69) | ||||||
| Q19. Nephropathologist at institution | 88 | |||||
| Q20. Review of tissue | ||||||
| Review of printed report only | 7 | |||||
| Review most with faculty only | 9 | |||||
| Review with pathology only if fellow performed the biopsy | 22 | |||||
| Review most biopsies performed by any fellow with pathology | 23 | |||||
| Review most biopsies done at institution with pathology | 38 | |||||
| Formal biopsy conference where some/all biopsies are reviewed with pathology | 81 | |||||
| Otherc | 19 | |||||
| Q21. Biopsy conference frequency (n=69) | ||||||
| Weekly | 15 | |||||
| Twice monthly | 15 | |||||
| Monthly | 52 | |||||
| Quarterly | 17 | |||||
| No formal conference | 0 |
Q, question number; US, ultrasound; CT, computed tomography; IR, interventional radiology.
One program reported all biopsies overseen by a urologist, and another by a ultrasound radiologist.
One program gave joint faculty appointments to IR, who is helping to develop a simulation lab, and will oversee fellows in the future.
Two programs offered a rotation with the nephropathologist. One program combined the tissue review conference with treatment plan development. Two programs access tissue images digitally, and interact with the nephropathologist on-line.
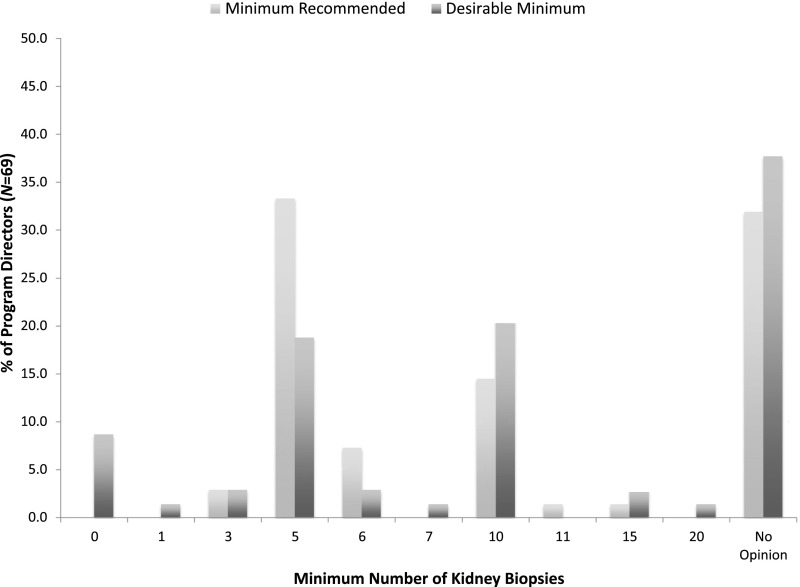
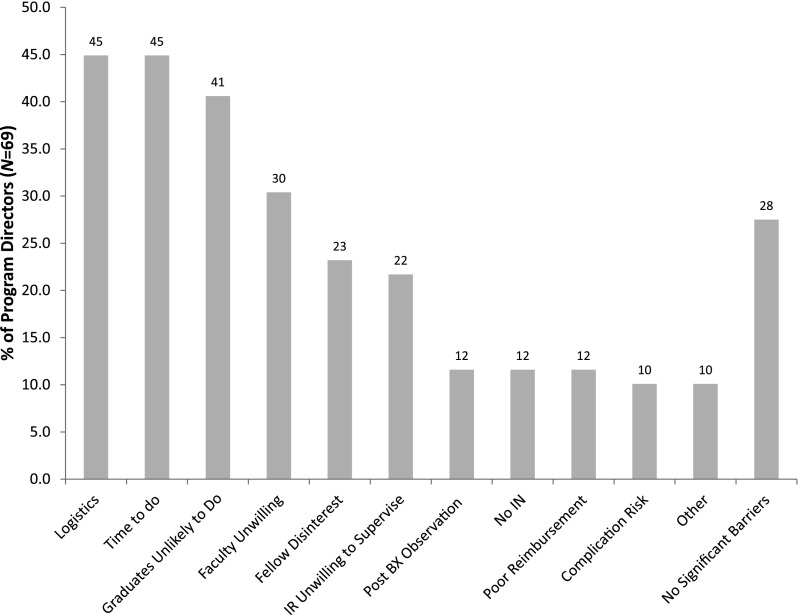
Barriers to achieving fellow competence are shown in Figure 4. The most commonly cited barriers were logistics (45%), time to do the biopsy (45%), perception that graduates were unlikely to perform biopsies (41%), and unwillingness/inability of nephrology faculty to supervise (30%). Twenty-eight percent cited no significant barriers.
Figure 4.
Barriers to achieving fellow competence in performing kidney biopsy (program director respondents n=69). BX, biopsy; IN, interventional nephrology; IR, interventional radiology.
To question 24, “Do you think attaining minimal competency in performing kidney biopsy should be required for nephrology fellowship completion for all nephrology fellows?,” 34 program directors (49%) said “yes” and 35 (51%) said “no.” Those in practice ≤20 years were as likely to answer “no” as those >20 years (50% versus 52%; P>0.99). Program directors who perceived no barriers to achieving fellow competence were significantly more likely to feel that performance competence should be required versus those who perceived ≥1 barrier (74% [14 of 19] versus 40% [20 of 50]; P=0.02). Those whose fellows performed <50 native biopsies/year were more likely to think that performance competence should not be required versus those whose fellows performed ≥50 (61% [25 of 41] versus 15% [2 of 13]; P<0.01). However, program directors at institutions with ≥100 native biopsies/year (regardless of whether fellows performed them) were no more likely to think that biopsy performance competence should be required than those with <100 (63% [12 of 19] versus 44% [14 of 32]; P=0.25).
Of the 35 who thought minimal performance competence should not be required, 97% thought all fellows should be required to demonstrate kidney biopsy knowledge competency (indications, contraindications, complications, appropriate referral, and tissue interpretation). Ninety-one percent thought some fellows should have the opportunity to achieve competency in an interventional/procedural track, even if fellowship length was increased.
Discussion
Graduate Survey
The graduate survey had an excellent response rate (71%), especially for those practicing ≤10 years, and included nephrologists with up to 30 years’ experience. Respondent practice locations varied geographically and with regard to population density. The sample size was small, and it is possible that significant geographic practice differences are not demonstrable, especially as few rural practitioners were surveyed. The clinical practice of graduates from a single military fellowship program may not be generalizable. However, the results are consistent with recent reports that the majority of nephrologists now refer some or all kidney biopsies, usually to IR (11–13).
Thirty-five percent of our graduates continue to perform kidney biopsies, which may be higher than among nonmilitary graduates. Military nephrologists serve at military academic medical centers for at least 2–4 years after graduation, and 21% (4 of 19) who continue to do biopsies indicated that they do so for fellowship training. We did not ask the respondents whether they were in academic practice. In 1990, 91% of United States nephrologists did their own biopsies (14,15). The advent of real-time ultrasound guidance was an impetus to refer to/collaborate with IR, who were more likely to acquire this new, expensive technology. By the mid-1990s, radiologists did 35% of biopsies (15).
Approximately 80% of graduates, independent of years in practice, agreed training was adequate for native biopsies, transplant biopsies, and histopathologic interpretation. Several commented that although they felt confident “firing the gun,” they were not confident in independent ultrasound localization. Because our program has always had a technologist or radiologist assist with localization, fellows were unlikely to achieve independent localization competence. In a survey of recently-graduated nephrologists, >80% felt well trained in biopsy, but only about 25% felt well trained in ultrasound localization (16). For ultrasound accreditation, the American Society of Diagnostic and Interventional Nephrology requires at least 50 hours of Continuing Medical Education (CME)-accredited training, or a 6-week experience in an accredited nephrology fellowship ultrasound training program (17). Such experience is unlikely, unless the program has an interventional nephrology track (5).
The most frequently cited barriers to performing biopsies for our graduates were systems-based: logistics (81%) and time (74%). One commented: “Doing only one would … wipe out 1/2 day of clinic … I can fill out and fax a request in 5 minutes …” Another: “The main reason (we) stopped was efficiency—(we) were at the mercy of the ultrasound suite.” Logistics require that the nephrologist coordinate access to an interventional suite with nursing support, conscious sedation, specialized equipment, and the necessary intra- and postprocedure monitoring. Most nephrologists are outpatient-based (18), and likely to perform biopsy less than monthly. They must compete for interventional suite time and efficiently integrate into a product line where kidney biopsy is likely seldom-performed. The facility may be distant from the nephrologist’s routine practice site. Moreover, the 2017 Medicare national average physician reimbursement for kidney biopsy (CPT code 50200) was only $135 (19). Efficiency of scale is against continuing, unless one is an interventional nephrologist, or a proceduralist in a group practice. Hospital systems may decide biopsies are best done by IR, and be overtly or tacitly unwilling to support product-line deviations.
Other concerns included skill loss when numbers dip under ten/year. Some rural nephrologists did not have resources available, although one continued to do biopsies because of limited IR access. Two nephrologists indicated that they recommended more biopsies after beginning IR referral. (Our own experience corroborates this—native biopsies increased 70% after beginning IR referral.) Three respondents specifically recommended that fellows continue to be trained so they can better select and counsel patients.
Program Director Survey
Fifty-one percent of program directors felt that biopsy performance competence should no longer be required. However, these 51% strongly favored offering an interventional track. Ten programs (15%) presently sponsor an interventional rotation.
The most common barriers to achieving fellow competence were the same faced by our graduates: time (45%) and logistics (45%). Other commonly cited barriers were that graduates were unlikely to perform biopsies (41%), and faculty unwillingness to supervise (30%). Fellowship programs are primarily hospital-based, and more likely to have access to IR suites and product lines, but the time and logistic systems barriers described seem difficult for programs to overcome. Some cited biopsy training time conflicts with other clinical procedures, prohibitive equipment costs, unwillingness of the ultrasound department or IR to share equipment or take time to involve nephrology in the biopsy, and product-line decisions by hospital administration that limit access to IR suites. High-volume programs (>100 biopsies/year, 15 of 74 programs) are likely to have dedicated facilities, equipment, and faculty—their systems allow logistic and time efficiency.
Identification of at least one barrier (73%) was significantly associated with the opinion that performance competence should not be required. Program directors whose fellows did <50 biopsies/year (76% who reported biopsy numbers) were also significantly more likely to believe that biopsy performance competence should not be required. The median number of theoretically available native kidney biopsies/fellow per year was 11, but fellows did a median of four, suggesting that barriers affect fellow procedure numbers. The existence of difficult-to-resolve systems barriers is suggested by the finding that recommended minimum numbers of biopsies shift upward when program directors were asked what the desirable minimum should be versus the achievable minimum, although there were very few exceeding ten (10–25 is the most common minimum for proficiency cited in an Australian survey) (13).
Several commented that the most important part of biopsy training is learning indications, contraindications, complications, and tissue processing (“what core goes where”), rather than physically obtaining tissue. These skills, and tissue interpretation, were endorsed as necessary by those who did not think biopsy performance competence should be required. In a survey of recent nephrology graduates, 54% did not feel well prepared to interpret tissue, although deemed it an important skill, and a recent educational needs assessment indicated that 32% of fellows would like more training in tissue interpretation (16,20). Improvements could include reviewing biopsies not done by fellows, attending a tissue interpretation course, or doing a nephropathology rotation.
The program director survey response rate (60%, with 77% completion rate) is similar to another recent survey, and robust for a web-based survey (21–23). We used several strategies to increase participation and limit stakeholder bias, including targeting only program directors, limiting response to one per device, and providing multiple reminders. The survey was relatively long, and required quantitative data—this may have decreased completion rate.
Kidney biopsy appears to be transitioning away from general nephrology practice, due to systems barriers. Fellows and recently-graduated nephrologists appear eager to become proficient in ultrasound interpretation and point-of-care diagnostic ultrasound, both well suited to outpatient practice and associated with fewer logistic barriers (5,20,21,24,25). Training might be better focused on ensuring fellows are fully competent to identify and refer patients for biopsy, robust training in histopathology interpretation, provision of an interventional nephrology track to selected trainees, and expanding point-of-care diagnostic ultrasound training.
Disclosures
D.J.L. is employed as a research physician at AstraZeneca. R.N. served as a councilor for the American Society of Diagnositic and Interventional Nephrology (ASDIN) from 2016 to 2017, and is Chair of the ASDIN communications committee.
Supplementary Material
Acknowledgments
The views expressed are those of the authors and do not necessarily reflect the official policy or position of the Department of the Army/Navy/Air Force, the Department of Defense, or the US Government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Does the Kidney Biopsy Portend the Future of Nephrology?,” on pages 681–682.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.13471217/-/DCSupplemental.
References
- 1.Clark E, Barsuk JH, Karpinski J, McQuillan R: Achieving procedural competence during nephrology fellowship training: Current requirements and educational research. Clin J Am Soc Nephrol 11: 2244–2249, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pivert K: ASN data brief: Nephrology procedures in GME (results of a FlashPoll). ASN data analytics, 2017. Available at https://www.researchgate.net/publication/315065568_ASN_Data_Brief_Nephrology_Procedures_in_GME. Accessed February 24, 2018
- 3.Basu A, Rope R: Mandating procedural competency in nephrology fellowship: Necessary or a loss of time? ASN kidney news, 2017. Available at https://www.kidneynews.org/kidneynews/9_3/16/16.pdf. Accessed February 24, 2018
- 4.Berns JS, O’Neill WC: Performance of procedures by nephrologists and nephrology fellows at U.S. nephrology training programs. Clin J Am Soc Nephrol 3: 941–947, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sachdeva M, Ross DW, Shah HH: Renal ultrasound, dialysis catheter placement, and kidney biopsy experience of US nephrology fellows. Am J Kidney Dis 68: 187–192, 2016 [DOI] [PubMed] [Google Scholar]
- 6.Mrug M, Bissler JJ: Simulation of real-time ultrasound-guided renal biopsy. Kidney Int 78: 705–707, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dawoud D, Lyndon W, Mrug S, Bissler JJ, Mrug M: Impact of ultrasound-guided kidney biopsy simulation on trainee confidence and biopsy outcomes. Am J Nephrol 36: 570–574, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Korbet SM, Volpini KC, Whittier WL: Percutaneous renal biopsy of native kidneys: A single-center experience of 1,055 biopsies. Am J Nephrol 39: 153–162, 2014 [DOI] [PubMed] [Google Scholar]
- 9.Chung S, Koh ES, Kim SJ, Yoon HE, Park CW, Chang YS, Shin SJ: Safety and tissue yield for percutaneous native kidney biopsy according to practitioner and ultrasound technique. BMC Nephrol 15: 96, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geography Division, United States Census Bureau: Census regions and divisions of the United States (17-April-2013). Available at: http://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed June 10, 2016
- 11.Lane C, Brown M: Alignment of nephrology training with workforce, patient, and educational needs: An evidence based proposal. Clin J Am Soc Nephrol 6: 2681–2687, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tøndel C, Vikse BE, Bostad L, Svarstad E: Safety and complications of percutaneous kidney biopsies in 715 children and 8573 adults in Norway 1988-2010. Clin J Am Soc Nephrol 7: 1591–1597, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ritchie AG, Saunders J, Baer R, May S; Australian and New Zealand Special Interest Group in Interventional Nephrology Research Collaboration : A survey of current procedural practices of Australian and New Zealand nephrologists. Semin Dial 26: E50–E53, 2013 [DOI] [PubMed] [Google Scholar]
- 14.Tape TG, Wigton RS, Blank LL, Nicolas JA: Procedural skills of practicing nephrologists. A national survey of 700 members of the American College of Physicians. Ann Intern Med 113: 392–397, 1990 [DOI] [PubMed] [Google Scholar]
- 15.Korbet SM: Nephrology and the percutaneous renal biopsy: A procedure in jeopardy of being lost along the way. Clin J Am Soc Nephrol 7: 1545–1547, 2012 [DOI] [PubMed] [Google Scholar]
- 16.Berns JS: A survey-based evaluation of self-perceived competency after nephrology fellowship training. Clin J Am Soc Nephrol 5: 490–496, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Society of Diagnostic and Interventional Nephrology (ASDIN): Requirements for certification in renal ultrasonography. Effective 07/01/2017; pp 3–4. Available at: http://c.ymcdn.com/sites/www.asdin.org/resource/resmgr/Updated_Cert_Recert_Apps/Renal_Ultrasound_Application.pdf. Accessed November 12, 2017
- 18.Salsberg E, Masselink L, Wu X: The US Nephrology Workforce: Developments and Trends, Washington, DC, American Society of Nephrology, 2014, pp 14–15, Available at: https://www.asn-online.org/education/training/workforce/Nephrology_Workforce_Study_Report_2014.pdf. Accessed November 12, 2017 [Google Scholar]
- 19.C.R. Bard, Inc.: 2017 reimbursement: Soft tissue biopsy. Available at: http://www.bardbiopsy.com/pdf/BPV-BBFA-0716-0021_2017_Biopsy_Reimbursement.pdf. Accessed January 9, 2018
- 20.Rope RW, Pivert KA, Parker MG, Sozio SM, Merell SB: Education in nephrology fellowship: A survey-based needs assessment. J Am Soc Nephrol 28: 1983–1990, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liebman SE, Moore CA, Monk RD, Rizvi MS: What are we doing? A survey of United States nephrology fellowship program directors. Clin J Am Soc Nephrol 12: 518–523, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martins Y, Lederman RI, Lowenstein CL, Joffe S, Neville BA, Hastings BT, Abel GA : Increasing response rates from physicians in oncology research: a structured literature review and data from a recent physician survey. Br J Cancer 106: 1021–1026, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, Samuel S, Ghali WA, Sykes LL, Jetté N: Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol 15: 32, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ross DW, Abbasi MM, Jhaveri KD, Sachdeva M, Miller I, Barnett R, Narasimhan M, Mayo P, Merzkani M, Mathew AT.Lung ultrasonography in end-stage renal disease: Moving from evidence to practice—a narrative review [published online ahead of print September 28, 2017]. Clin Kidney J. [DOI] [PMC free article] [PubMed]
- 25.Ross DW, Jhaveri KD, Narasimhan M: Point of care ultrasound: A new tool for the 21st century nephrologist. Nephrol News Issues 12: 2017. Available at: https://www.nephrologynews.com/point-care-ultrasound-new-tool-21st-century-nephrologist/. Accessed November 12, 2017 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.