Abstract
Acne vulgaris is a common disease among people in Asia. International guidelines and treatment recommendations emphasize the central role of topical retinoids in the management of acne. However, topical retinoids remain underutilized in clinical practise, which may be in part due to fear of retinoid‐associated dermatitis/lack of experience, particularly in Asian patients. There is a perception that Asian skin has a greater tendency toward sensitivity compared with Caucasian skin. In our clinical experience, topical retinoid therapy can be used with excellent effect to treat Asians with acne. This article discusses available published work regarding the use of topical retinoids in Asian populations, and presents tips for utilizing these important agents in daily practise. Optimizing use of topical retinoids may improve adherence and, in turn, therapeutic outcomes and patient satisfaction.
Keywords: acne vulgaris, irritation, racial skin, retinoids, tolerability
Introduction
Acne is a common problem among Asian adolescents and adults as reported in the published work and anecdotally by dermatologists from many countries. A 1992 survey of 74 589 Asian adults treated at the National Skin Center in Singapore found acne was the second most common disease.1Later, Han et al.2 reported that over a 10‐year study period (2004‐2013) there was a marked increase in the number of acne cases (from 5.8% to 8.1% of all new diagnoses) at the National Skin Center. In 2007, Wu et al.3 surveyed 3163 adolescent students (10–18 years) in China and reported a 53.5% prevalence of acne, which increased with age up to 70.4% in 16 year olds. Park et al.4 from Korea reported in 2015 that 36.2% of 693 elementary school children (7–12 years old) had acne and the prevalence increased with age, as was observed in the Chinese study. An older study (1998) of 866 adolescent students in Auckland, New Zealand, reported acne in 91% of males and 79% of females, which was predominantly mild to moderate in nature (>90%).5 An Indian study reported that the prevalence of acne was higher in an urban area versus rural (37.5% vs 21.4%).6
Data are somewhat sparse about differences among demographic groups in response to therapeutic interventions for acne; however, both histopathological and clinical features have been reported to vary among patient populations, with more inflammation reported in Asian and Fitzpatrick type VI individuals, a lower rate of nodulocystic acne in black type VI, and differing propensities to scarring and pigmentary problems among groups.7, 8, 9 There is also a clinical perception and some data showing that tolerability varies among populations, with some Asian subgroups more prone to sensitive skin than others.10, 11, 12 Generally, Asian skin tends to be more pigmented than that of white people of European descent and a high proportion of Asians have a predisposition to acne sequelae.13, 14 Abad‐Casintahan et al.13 reported that 58.2% of 342 acne patients consulting a dermatologist in seven Asian countries had postinflammatory hyperpigmentation (PIH). Hayashi et al.14 reported that 90.8% of Japanese patients with acne had some degree of acne scarring. Both PIH and scars are very concerning for Asian patients, and can have a large impact on quality of life in these patients.13, 14
It should be noted that the term “Asian” refers to a large group of peoples from various countries with a spectrum of climates and diverse skin types. For example, Northern Chinese and Japanese usually have lighter skin types (II–III), Malaysians and Filipinos have medium skin phototypes (III–IV), while other countries such as India have a wide range of phototypes from very light to very dark.15 Climates in Asian countries range from tropical to arid; these differences may have a bearing on treatment choices.
According to international treatment guidelines and recommendations, a topical retinoid plus antimicrobial is recommended as first‐line therapy for the majority of individuals with acne.16, 17, 18, 19, 20, 21 We discuss use of topical retinoids among Asians, with the goal of optimizing the management approach and patient satisfaction.
Differences in Skin Physiology and Other Factors
There are contradictory findings about differences in skin physiology among specific population groups, and these differences deserve more study because they may contribute to a variable therapeutic response. Corcuff et al.22 reported that there were no significant differences in corneocyte size between black, white and Asian subjects (911, 899 and 909 μm², respectively). However, there has been a suggestion that transepidermal water loss (TEWL) and barrier function may vary between groups. Of note, while one study found that Asians had the lowest TEWL, highest water content and highest stratum corneum lipid content, another study reported slightly higher TEWL and increased barrier permeability in Asian and black subjects compared with Caucasian.23, 24 Reed et al.25 reported that differences in barrier function were associated with skin phototype (II–III different from IV, with darker skin recovering faster after barrier damage) but not race (Caucasian vs Asian). According to Muizzuddin et al.,12 East Asian skin had the weakest skin barrier and lowest degree of cellular maturation, which they equated with the highest degree of skin sensitivity versus white or black skin. Asian skin is reported to be more sensitive to chemical stimuli, which has been hypothesized to be due to higher sweat gland density or possibly a thinner stratum corneum (required fewer tape strippings to break the barrier).24
Halder et al. found significant inflammation in all types of acne lesions on histopathology from 30 black females and theorized this may be the basis for PIH (Halder J Invest Dermatol 199626) Krutmann et al.8 reported that inflammatory acne is more common in Asian women than other population groups, suggesting that inflammation may play a role in this population's tendency to PIH as well.
The disease course of acne may also be affected by exposure to airborne pollutants, which can be high in some urban Asian settings.8 A survey conducted during the International Dermatology Conference in Beijing revealed that 67% of responding dermatologists agreed that acne is exacerbated by pollution.8 In addition, clinical studies in Shanghai and Mexico City (areas with high pollution levels) showed that skin quality worsened and sebum excretion was higher with chronic exposure to ambient pollution.27, 28 Analysis of retrospective data from acne patients in Beijing (n = 59 530) showed that high levels of ambient pollutants occurred contemporaneously with increased outpatient visits for acne.8 This was confirmed by a prospective study in 64 patients with acne that showed an association between high levels of airborne pollutants and increased sebum secretion and acne lesions. Krutmann et al.8 recommend to avoid medical therapy that disrupts skin barrier function and emphasize the importance of good skin care, particularly for Asians living in large cities with high pollution levels.8 Of interest, studies from Africa, Brazil and India showed that acne was more common in urban compared with rural populations.6, 29, 30
Central Role of Retinoids in Acne Management
Clinical guidelines and expert recommendations emphasize the central role of topical retinoids in acne management.16, 17, 18, 19, 20, 31 It is important to note that while antibiotics were once considered key for acne management, their role has changed over time due to understanding that acne is not a traditional bacterial infection, the steadily increasing public health concern about antimicrobial resistance and the introduction of topical retinoids.32, 33 Multiple clinical studies involving thousands of patients have consistently demonstrated significantly greater reductions in both inflammatory lesions and comedones with a regimen of topical retinoid plus antimicrobial therapy versus antimicrobial therapy alone.16, 17, 18, 19, 20, 31 Although some clinicians think the effect of topical retinoids is primarily on comedones, retinoids have been shown to have an excellent effect on inflammatory lesions when used as monotherapy.34 Topical retinoids target the microcomedone, the precursor to all acne lesions, as well as clinically visible acne lesions, and for this reason are well suited for both treating acne and maintaining acne clearance.35, 36, 37, 38, 39, 40, 41 Because of the unique action on microcomedones, patients should be instructed to apply the topical retinoid to the entire affected area as opposed to only on acne lesions (spot treatment).42
Using Topical Retinoids in Skin of Color
The first step in optimizing retinoid use in patients with skin of color is to assess the patient's skin‐care regimen and recommend a gentle cleanser and moisturizer.43 We find that being able to discuss skin care helps to impress upon the patient that the clinician has a strong professional interest in optimizing acne management.44 Callender43 recommends avoiding irritating products, particularly in individuals with a history of dry/sensitive skin, other dermatological diseases (eczema, atopic dermatitis, rosacea, xerosis) or reactions to previous therapy. Having a staff member available to educate the patient on what practises to avoid – frequent washing, overly aggressive washing with a buff‐puff or loofah scrub – is also useful.43
The need for early and efficacious intervention to minimize potential for acne‐associated PIH and other sequelae means that topical retinoids remain the top choice for first‐line therapy as well as for maintenance therapy.43, 45 Irritation is the most frequent adverse event associated with topical retinoids and this makes some clinicians hesitate to recommend these agents.43 However, the potential for irritation can be minimized with a few simple steps and the therapeutic rewards from retinoids can be great. Topical retinoids have an additional benefit for individuals with acne and skin of color because retinoids can improve the appearance of pigmented lesions. Bulengo‐Ransby et al.46 reported that tretinoin 0.1% lightened postinflammatory hyperpigmented lesions in black subjects (P < 0.001 vs vehicle). Further, application of tretinoin did not result in excessive hyperpigmentation or depigmentation of the normal skin in any subject.46 Jacyk et al.47 confirmed the action of retinoids on acne and PIH in a population of African patients treated with adapalene monotherapy. Grimes et al.48 reported that tazarotene 0.1% cream once daily was more effective than vehicle in improving acne (P = 0.01) and intensity of hyperpigmented lesions (P = 0.44) in subjects with skin types IV–VI and mild to moderate acne. According to Callender,43 educating patients about the dual benefits of retinoids on both acne and PIH can enhance compliance, resulting in even better treatment outcomes. There is evidence from Kang et al.49 that dermatologists prescribe retinoids for dyschromias in Asian patients and it is our anecdotal experience that retinoid therapy can result in improvements in overall skin tone and texture, including lightening of dark spots.
When prescribing topical retinoids, it is prudent to commence with a low concentration and select a tolerable formulation. Beginning therapy with alternate day dosing for the first 2 weeks can also help reduce risk of irritation and PIH.50 Notably, it has been shown that using a slower initiation of therapy by starting with a small area of application or application every other day is associated with the same excellent level of efficacy as daily application with adapalene 0.1% and benzoyl peroxide 2.5% (A‐BPO).51 Data from clinical studies shows that most adverse effects, including retinoid irritation, occur during the early phase of treatment (Fig. 1).52 Thus, strategies to minimize irritation – such as application every other day and/or use of a moisturizer prior to therapy – should be used at the initiation of therapy.51 In our experience, use of moisturizers can markedly improve the cutaneous tolerability of topical retinoids; we recommend application either 10 min prior to retinoid therapy or the retinoid and moisturizer can be mixed together for application.
Figure 1.
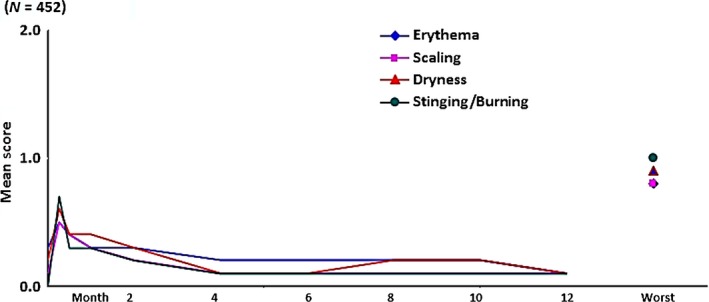
Retinoid‐associated skin tolerability problems are most frequently observed in the first few weeks of therapy and subside with continued use. (Reproduced from Pariser et al.,52 with permission.)
Kwon et al.53 hypothesized that adherence to treatment could be improved by a dermatological tutorial instructing patients on application techniques (to use a limited amount of product) and to apply moisturizer 10 min before the acne therapy. In a population of 85 Asian patients with acne, the use of a tutorial significantly improved tolerability with the fixed‐dose combination of A‐BPO versus no tutorial.53 Efficacy was significantly superior among patients who were treated with A‐BPO versus BPO (78.2% clear or almost clear vs 45.5% with BPO).53 In addition, the frequency and intensity of local irritation was significantly lower in the tutorial group, with 34.4% versus 80.7% experiencing one adverse event for tutorial versus non‐tutorial, respectively.53 All local irritation scores (erythema, dryness, stinging/burning) were significantly lower in the tutorial group at all time points (Fig. 2). Thus, use of the tutorial improved the ability of patients to tolerate highly effective A‐BPO therapy.53
Figure 2.
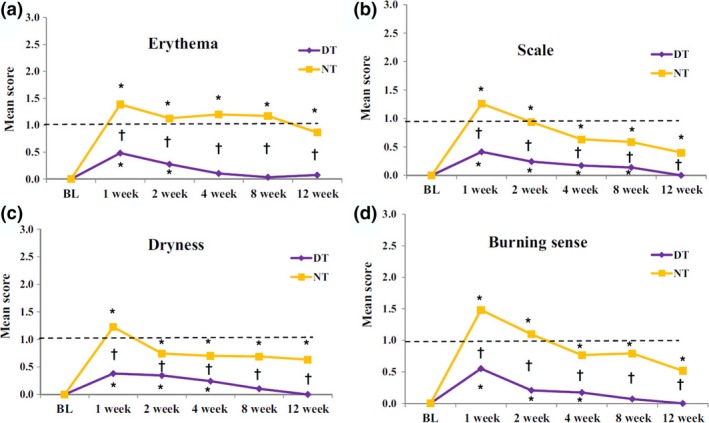
Local irritation scores reduced by use of educational tutorial and moisturizer. A‐BPO, adapalene 0.1%/benzoyl peroxide 2.5% gel; BL, baseline; DT, dermatological tutorial subgroup; NT, no tutorial subgroup. Irritation scored as none (0), mild (1), moderate (2) and severe (3). Graph shows mean scores for (a) erythema, (b) scaling, (c) dryness, and (d) burning sensation. Mean scores at each visit shown. (Reproduced from Kwon et al.,53 with permission.)
Similarly, Myhill et al.54 found that implementation of a supplementary patient education intervention improved both treatment adherence and satisfaction in acne patients. Subjects treated with A‐BPO gel were randomized to one of three treatment arms: (i) supplemental patient education including package inserts and oral instruction to set expectations for speed of results, potential side‐effects and how to apply therapy; (ii) standard of care education; or (iii) more frequent clinic visits (two more than the other groups). As shown in Figure 3, the supplemental patient education helped patients adhere to therapy, better use the product and manage skin irritation. Additionally, more subjects who received supplemental education reported not being bothered at all by side‐effects of treatment.54
Figure 3.
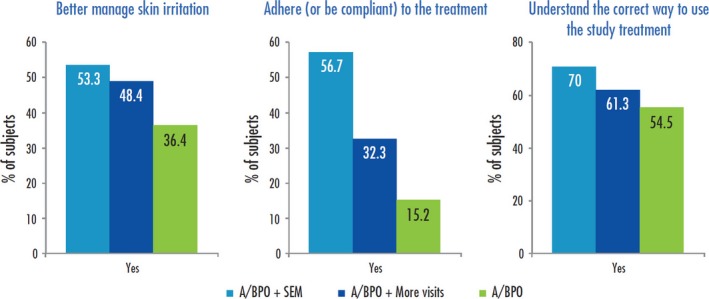
Impact of supplemental patient education on satisfaction with retinoid therapy. Percent of subjects in each treatment group answering “yes” to the survey prompt, “the information you have received in the study about the treatment helps you to (a) better manage skin irritation, (b) adhere (or be compliant) to the treatment, and (c) understand the correct way to use the study treatment”. Treatment groups: A/BPO + SEM, adapalene/benzoyl peroxide plus supplementary education materials; A/BPO + more visits, adapalene/benzoyl peroxide plus additional study visits; A/BPO, adapalene/benzoyl peroxide treatment with only standard of care patient education. (Reproduced from Myhill et al.,54 with permission.)
Retinoids in Asian skin
Because structural and biophysical distinctions among racial skin types may exist, potential differences in efficacy and tolerability may occur.24 However, a number of studies have shown efficacy and tolerability of topical retinoids in Asians, including the Kwon et al.53 study discussed above (Table 1). In South Korea, Ko et al.55 conducted a prospective, open‐label comparative study of clindamycin 0.1% benzoyl peroxide 5% (CLIN‐BPO) gel versus adapalene 0.1% gel in 69 Asian patients. Both treatments were efficacious and well tolerated in Asian patients with mild to moderate acne.55
Table 1.
Studies of retinoids in Asian populations
| Study | Population | Design | Efficacy | Tolerability |
|---|---|---|---|---|
| Kwon et al.53 | n = 85 Korean subjects, % skin phototypes II/IV/V = 28/48/23 | Split‐face 12‐week study comparing A/BPO 0.1%/2.5% vs BPO 2.5% and dermatological DT vs NT |
A/BPO > BPO for success rates and lesion count reduction as early as week 1 (success in 78.2% vs 45.5%, respectively) DT > NT |
BPO > A/BPO with NT; however, A/BPO tolerability markedly improved with DT DT > NT (local irritation 34.4% vs 80.7%, respectively) |
| Ko et al.55 | n = 69 Korean subjects, skin phototypes not reported | Open‐label 12‐week study of ADA 0.1% vs CLIN/BPO 1%/5% |
Both treatments improved acne (global improvement much or very much improved 68% CLIN/BPO and 61% ADA) CLIN/BPO > ADA for inflammatory lesions |
Both treatments were well tolerated with minimal adverse events |
| Tu et al.56 | n = 150 Chinese subjects, % skin phototypes I/II/III/IV = 1/6/64/30 | Randomized 8‐week study of ADA 0.1% vs tretinoin 0.025% | ADA = TRET (70% reduction in non‐inflammatory lesions from baseline for both, ADA 74.8% and TRET 72.2% reduction in inflammatory lesions) | ADA > TRET (P < 0.05 for erythema, burning) |
| Percy et al.57 | n = 571 Indian subjects | Open‐label 12‐week study of ADA 0.1% | Global improvement of acne in 96.3%, complete clearing in 18% | Excellent/good tolerability in 81% |
| Goswami et al.58 | n = 66 Indian subjects, skin phototypes not reported | Randomized 18‐week study of RBG 16% vs vehicle | RBG > vehicle (86.8% vs 40.1% reduction of total lesions) | Both well tolerated |
A/BPO, fixed combination of adapalene and benzoyl peroxide; ADA, adapalene; BPO, benzoyl peroxide; CLIN, clindamycin; DT, dermatological tutorial; NT, no tutorial; RBG, retinyl β‐glucuronide; TRET, tretinoin.
Tu et al.56 compared 8 weeks treatment with adapalene gel 0.1% versus tretinoin gel 0.025% in a Chinese patient population (n = 150) with mild to moderate acne vulgaris. Both retinoids significantly improved acne, with marked improvement or complete clearance in more than 70% of subjects in both groups. Irritation was mild in both groups, but was more frequent and more severe in the tretinoin group. The authors concluded that adapalene was a good treatment option for Chinese patients because “adapalene offers comparable efficacy to tretinoin but is less irritating”.56
A large‐scale postmarketing surveillance study in India involved 571 patients treated with adapalene 0.1% gel for 12 weeks.57 Virtually all subjects (96.3%) had improvement in acne from baseline, and 66% of patients had 75% or more improvement.57 Tolerability was rated as excellent/good in 81% of patients by the investigating physician.57 Another 18‐week double‐blind Indian study evaluated topical retinoyl β‐glucuronide (RBG) versus vehicle in patients with mild to moderate acne (n = 66). RBG was significantly superior (P < 0.001) to vehicle in reducing all lesion types (−86.8% total lesions, −80.2% inflammatory lesions, and −94.6% non‐inflammatory lesions vs 40.1%, 34.3% and 50%, respectively). RBG was well tolerated and had a rapid onset of action, and the authors recommended it as a good option for Asian–Indian acne patients.58
In Thai acne patients (n = 120), adapalene gel 0.1% was shown to be efficacious and tolerable in a double‐blind, randomized, vehicle‐controlled study.59 However, addition of a non‐comedogenic moisturizer (licochalcone A, L‐carnitine and 1.2‐decanediol) significantly improved tolerability by reducing skin irritation symptoms and TEWL.59 The efficacy of adapalene was improved by use of moisturizer, because there were fewer inflammatory flares and a more rapid onset of action in reducing acne lesions.59
Kim et al.60 compared the efficacy and tolerability of A‐BPO 0.1% versus adapalene gel 0.1% in treatment of Asian patients (n = 23) with acne in a 12‐week, split‐face, observer‐blinded study in Korea. A‐BPO 0.1% was significantly superior to adapalene gel monotherapy (P < 0.0001) and while more patients experienced irritation during the first 2 weeks of treatment with A‐BPO 0.1%, the authors noted that “all symptoms were tolerable and the prevalence of irritation did not differ between both sides (P > 0.05)”. Further, irritation decreased over time (as is consistent with topical retinoid therapy), resolving within 4–6 weeks.60
While the previous studies evaluated subjects with mild to moderate acne, a new fixed‐dose combination of adapalene 0.3%/BPO 2.5% (A‐BPO 0.3%) offers the ability to use topical therapy to effectively treat more severe cases.61, 62 To help determine if there may be differences in therapeutic response by race/phototype, Alexis et al.61 recently conducted a subgroup analysis of A‐BPO 0.3% phase III studies in patients with moderate to severe acne. The efficacy and safety of A‐BPO 0.3% in individuals with Fitzpatrick skin phototypes I–III (lighter skin) was compared with that of subjects with phototypes IV–VI (darker skin). A‐BPO 0.3% demonstrated good efficacy, achieving clear or almost clear in 32% of subjects with lighter skin and 28% of those with darker skin types. Tolerability was comparable among the two skin phototype groups, with tolerability scores similar to baseline by week 12.61
Goh et al.10 evaluated the tolerability of adapalene gel 0.1% versus tretinoin gel 0.025% in four racial groups (Chinese, Asian Indian, Malay and Caucasian) in a randomized split‐face study. Subjects (n = 73) applied each agent on one half of the face and on one of two test areas on the forearms, and tolerability was assessed by a tolerability score (sum of erythema, desquamation and dryness scores) and TEWL. As shown in Figure 4, adapalene was better tolerated than tretinoin in all racial groups. The difference in tolerability was apparent by study day 3 and sustained throughout the 21‐day study period. In addition, there was a small but significant difference in tolerability associated with the various racial groups (with Chinese patients demonstrating more irritation than the other groups); however, this was much smaller than the difference between adapalene and tretinoin overall.10
Figure 4.
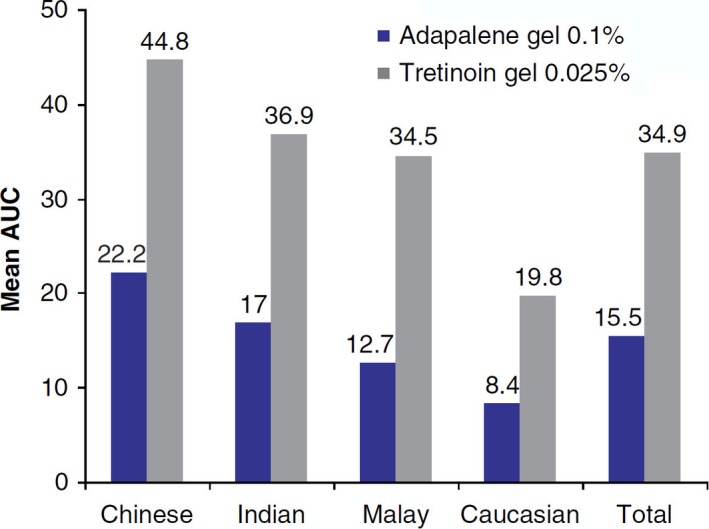
Tolerability of adapalene versus tretinoin by racial group. Local tolerability criteria are summarized in an area under the curve (AUC) analysis of a total sum score of facial irritation including erythema, desquamation and dryness from baseline to last measurement. Higher AUC value correlates with lower overall tolerability. (Reproduced from Goh et al.,10 with permission.)
Positive impact of moisturizers in Asian skin
There is additional evidence besides the Thai study discussed above supporting the use of moisturizers with topical retinoid therapy in Asian patients. In Japan, Munehiro et al.63 demonstrated that use of cosmetic moisturizers with adapalene and clindamycin gels significantly reduced the sensation of dryness and increased water content in the stratum corneum. Treatment efficacy was not diminished by use of moisturizers, and the authors recommended use of moisturizer plus topical treatment.63 In another Japanese study, Hayashi et al.64 reported that addition of a moisturizer to adapalene therapy improved tolerability and adherence, significantly lengthening the initial treatment period and reducing the number of treatment drop‐outs. This agrees with results reported by Matsunaga et al.,65 who evaluated tolerability of adapalene with and without a moisturizing lotion in 30 healthy volunteers of Chinese heritage. At all study visits, tolerability was better in skin treated with adapalene plus moisturizer compared with adapalene only; the difference was significant during the first 2 weeks of the study (P = 0.039 and 0.013, respectively), again emphasizing the importance of prudent initiation of retinoids. Global worst score (the average of worst scores for erythema, desquamation, dryness, stinging/burning and pruritus) was significantly lower in moisturizer‐treated skin than that treated with just adapalene gel (0.43 ± 0.34 vs 0.59 ± 0.44, P = 0.032). The authors noted that improved tolerability may contribute to better adherence.65
Conclusions
Acne is a common clinical problem in Asia, and there are increasing numbers of patients who are seeking treatment for this disease. Acne experts and clinical guidelines/recommendations agree that topical retinoids form the basis of acne treatment. Some controversies still exist regarding racial differences in skin sensitivity; however, increased susceptibility to irritation with topical retinoid therapy has been perceived as a challenge in this population. Studies consistently show that tolerability issues are most likely to occur in the first few weeks of treatment, but are generally mild and subside with continued use. Strategies such as slow initiation by application every other day can minimize the potential for irritation. Similarly, the use of moisturizers has been demonstrated to reduce the likelihood of irritation and can potentially improve patient satisfaction with the care provider by achieving faster results. Because many Asian acne patients are at risk for acne sequelae such as PIH and scarring, there is a therapeutic imperative to initiate effective treatment with retinoids as soon as possible. The best management for these problems is to avoid them occurring in the first place, as both PIH and scars are long lasting and distressing for patients once they occur. Patient and caregiver education are also valuable components of acne therapy, and may be streamlined by use of existing materials/strategies.
Conflict of Interest:
All authors have served as consultants for Galderma International (Advisory Board members).
Acknowledgments
Editorial services for this publication were provided by Galderma International. The authors wish to acknowledge Valerie Sanders, Sanders Medical Writing, for assistance with preparation of this publication.
References
- 1. Chua‐Ty G, Goh CL, Koh SL. Pattern of skin diseases at the National Skin Centre (Singapore) from 1989‐1990. Int J Dermatol 1992; 31: 555–559. [DOI] [PubMed] [Google Scholar]
- 2. Han XD, Oon HH, Goh CL. Epidemiology of post‐adolescence acne and adolescence acne in Singapore: a 10‐year retrospective and comparative study. J Eur Acad Dermatol Venereol 2016; 30: 1790–1793. [DOI] [PubMed] [Google Scholar]
- 3. Wu TQ, Mei SQ, Zhang JX et al Prevalence and risk factors of facial acne vulgaris among Chinese adolescents. Int J Adolesc Med Health 2007; 19: 407–412. [DOI] [PubMed] [Google Scholar]
- 4. Park SY, Kwon HH, Min S, Yoon JY, Suh DH. Epidemiology and risk factors of childhood acne in Korea: a cross‐sectional community based study. Clin Exp Dermatol 2015; 40: 844–850. [DOI] [PubMed] [Google Scholar]
- 5. Pearl A, Arroll B, Lello J, Birchall NM. The impact of acne: a study of adolescents’ attitudes, perception and knowledge. N Z Med J 1998; 111: 269–271. [PubMed] [Google Scholar]
- 6. Kubba R, Bajaj AK, Thappa DM et al Acne in India: guidelines for management ‐ IAA consensus document. Indian J Dermatol Venereol Leprol 2009; 75(Suppl 1): 1–62. [PubMed] [Google Scholar]
- 7. Shah SK, Alexis AF. Acne in skin of color: practical approaches to treatment. J Dermatolog Treat 2010; 21: 206–211. [DOI] [PubMed] [Google Scholar]
- 8. Krutmann J, Moyal D, Liu W et al Pollution and acne: is there a link? Clin Cosmet Investig Dermatol 2017; 10: 199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Taylor SC, Cook‐Bolden F, Rahman Z, Strachan D. Acne vulgaris in skin of color. J Am Acad Dermatol 2002; 46: S98–S106. [DOI] [PubMed] [Google Scholar]
- 10. Goh CL, Tang MB, Briantais P, Kaoukhov A, Soto P. Adapalene gel 0.1% is better tolerated than tretinoin gel 0.025% among healthy volunteers of various ethnic origins. J Dermatolog Treat 2009; 20: 282–288. [DOI] [PubMed] [Google Scholar]
- 11. Aramaki J, Kawana S, Effendy I, Happle R, Loffler H. Differences of skin irritation between Japanese and European women. Br J Dermatol 2002; 146: 1052–1056. [DOI] [PubMed] [Google Scholar]
- 12. Muizzuddin N, Hellemans L, Van Overloop L, Corstjens H, Declercq L, Maes D. Structural and functional differences in barrier properties of African American, Caucasian and East Asian skin. J Dermatol Sci 2010; 59: 123–128. [DOI] [PubMed] [Google Scholar]
- 13. Abad‐Casintahan F, Chow SK, Goh CL et al Frequency and characteristics of acne‐related post‐inflammatory hyperpigmentation. J Dermatol 2016; 43(7): 826–828. [DOI] [PubMed] [Google Scholar]
- 14. Hayashi N, Miyachi Y, Kawashima M. Prevalence of scars and “mini‐scars”, and their impact on quality of life in Japanese patients with acne. J Dermatol 2015; 42: 690–696. [DOI] [PubMed] [Google Scholar]
- 15. Taylor SC. Epidemiology of skin diseases in ethnic populations. Dermatol Clin 2003; 21: 601–607. [DOI] [PubMed] [Google Scholar]
- 16. Gollnick H, Cunliffe W, Berson D et al Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol 2003; 49: S1–S37. [DOI] [PubMed] [Google Scholar]
- 17. Nast A, Dreno B, Bettoli V et al European evidence‐based (S3) guideline for the treatment of acne ‐ update 2016 ‐ short version. J Eur Acad Dermatol Venereol 2016; 30: 1261–1268. [DOI] [PubMed] [Google Scholar]
- 18. Thiboutot D, Gollnick H, Bettoli V et al New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol 2009; 60: S1–S50. [DOI] [PubMed] [Google Scholar]
- 19. Gollnick HP, Bettoli V, Lambert J et al A consensus‐based practical and daily guide for the treatment of acne patients. J Eur Acad Dermatol Venereol 2016; 30(9): 1480–1490. [DOI] [PubMed] [Google Scholar]
- 20. Zaenglein AL, Pathy AL, Schlosser BJ et al Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol 2016; 74(945–73): e33. [DOI] [PubMed] [Google Scholar]
- 21. Goh CL, Abad‐Casintahan F, Aw DC et al South‐East Asia study alliance guidelines on the management of acne vulgaris in South‐East Asian patients. J Dermatol 2015; 42: 945–953. [DOI] [PubMed] [Google Scholar]
- 22. Corcuff P, Lotte C, Rougier A, Maibach HI. Racial differences in corneocytes. A comparison between black, white and oriental skin. Acta Derm Venereol 1991; 71: 146–148. [PubMed] [Google Scholar]
- 23. Kompaore F, Marty JP, Dupont C. In vivo evaluation of the stratum corneum barrier function in blacks, Caucasians and Asians with two noninvasive methods. Skin Pharmacol 1993; 6: 200–207. [DOI] [PubMed] [Google Scholar]
- 24. Rawlings AV. Ethnic skin types: are there differences in skin structure and function? Int J Cosmet Sci 2006; 28: 79–93. [DOI] [PubMed] [Google Scholar]
- 25. Reed JT, Ghadially R, Elias PM. Skin type, but neither race nor gender, influence epidermal permeability barrier function. Arch Dermatol 1995; 131: 1134–1138. [PubMed] [Google Scholar]
- 26. Halder RM. A clinicopathological study of acne vulgaris in black females. J Invest Dermatol 1996; 106: 888. [Google Scholar]
- 27. Lefebvre MA, Pham DM, Boussouira B, Bernard D, Camus C, Nguyen QL. Evaluation of the impact of urban pollution on the quality of skin: a multicentre study in Mexico. Int J Cosmet Sci 2015; 37: 329–338. [DOI] [PubMed] [Google Scholar]
- 28. Nouveau‐Richard S, Zhu W, Li YH et al Oily skin: specific features in Chinese women. Skin Res Technol 2007; 13: 43–48. [DOI] [PubMed] [Google Scholar]
- 29. Hogewoning AA, Koelemij I, Amoah AS et al Prevalence and risk factors of inflammatory acne vulgaris in rural and urban Ghanaian schoolchildren. Br J Dermatol 2009; 161: 475–477. [DOI] [PubMed] [Google Scholar]
- 30. Bechelli LM, Haddad N, Pimenta WP et al Epidemiological survey of skin diseases in schoolchildren living in the Purus Valley (Acre State, Amazonia, Brazil). Dermatologica 1981; 163: 78–93. [DOI] [PubMed] [Google Scholar]
- 31. Gollnick HP. From new findings in acne pathogenesis to new approaches in treatment. J Eur Acad Dermatol Venereol 2015; 29(Suppl 5): 1–7. [DOI] [PubMed] [Google Scholar]
- 32. Dreno B, Thiboutot D, Gollnick H et al Antibiotic stewardship in dermatology: limiting antibiotic use in acne. Eur J Dermatol 2014; 24: 330–334. [DOI] [PubMed] [Google Scholar]
- 33. Thiboutot D, Dreno B, Gollnick H et al A call to limit antibiotic use in acne. J Drugs Dermatol 2013; 12: 1331–1332. [PubMed] [Google Scholar]
- 34. Leyden JJ, Shalita A, Thiboutot D, Washenik K, Webster G. Topical retinoids in inflammatory acne: a retrospective, investigator‐blinded, vehicle‐controlled, photographic assessment. Clin Ther 2005; 27: 216–224. [DOI] [PubMed] [Google Scholar]
- 35. Thielitz A, Helmdach M, Ropke EM, Gollnick H. Lipid analysis of follicular casts from cyanoacrylate strips as a new method for studying therapeutic effects of antiacne agents. Br J Dermatol 2001; 145: 19–27. [DOI] [PubMed] [Google Scholar]
- 36. Thielitz A, Abdel‐Naser MB, Fluhr JW, Zouboulis CC, Gollnick H. Topical retinoids in acne–an evidence‐based overview. J Dtsch Dermatol Ges 2008; 6: 1023–1031. [DOI] [PubMed] [Google Scholar]
- 37. Thielitz A, Sidou F, Gollnick H. Control of microcomedone formation throughout a maintenance treatment with adapalene gel, 0.1%. J Eur Acad Dermatol Venereol 2007; 21: 747–753. [DOI] [PubMed] [Google Scholar]
- 38. Leyden J, Thiboutot DM, Shalita AR et al Comparison of tazarotene and minocycline maintenance therapies in acne vulgaris: a multicenter, double‐blind, randomized, parallel‐group study. Arch Dermatol 2006; 142: 605–612. [DOI] [PubMed] [Google Scholar]
- 39. Poulin Y, Sanchez NP, Bucko A et al A 6‐month maintenance therapy with adapalene‐benzoyl peroxide gel prevents relapse and continuously improves efficacy among patients with severe acne vulgaris: results of a randomized controlled trial. Br J Dermatol 2011; 164: 1376–1382. [DOI] [PubMed] [Google Scholar]
- 40. Thiboutot DM, Shalita AR, Yamauchi PS et al Adapalene gel, 0.1%, as maintenance therapy for acne vulgaris: a randomized, controlled, investigator‐blind follow‐up of a recent combination study. Arch Dermatol 2006; 142: 597–602. [DOI] [PubMed] [Google Scholar]
- 41. Zhang JZ, Li LF, Tu YT, Zheng J. A successful maintenance approach in inflammatory acne with adapalene gel 0.1% after an initial treatment in combination with clindamycin topical solution 1% or after monotherapy with clindamycin topical solution 1%. J Dermatolog Treat 2004; 15: 372–378. [DOI] [PubMed] [Google Scholar]
- 42. Thiboutot D, Dreno B, Layton A. Acne counseling to improve adherence. Cutis 2008; 81: 81–86. [PubMed] [Google Scholar]
- 43. Callender VD. Acne in ethnic skin: special considerations for therapy. Dermatol Ther 2004; 17: 184–195. [DOI] [PubMed] [Google Scholar]
- 44. Goh CL, Noppakun N, Micali G et al Meeting the Challenges of Acne Treatment in Asian Patients: a Review of the Role of Dermocosmetics as Adjunctive Therapy. J Cutan Aesthet Surg 2016; 9: 85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Halder RM, Nootheti PK. Ethnic skin disorders overview. J Am Acad Dermatol 2003; 48: S143–S148. [DOI] [PubMed] [Google Scholar]
- 46. Bulengo‐Ransby SM, Griffiths CE, Kimbrough‐Green CK et al Topical tretinoin (retinoic acid) therapy for hyperpigmented lesions caused by inflammation of the skin in black patients. N Engl J Med 1993; 328: 1438–1443. [DOI] [PubMed] [Google Scholar]
- 47. Jacyk WK. Adapalene gel 0.1% for topical treatment of acne vulgaris in African patients. Cutis 2001; 4(Suppl): 48–54. [PubMed] [Google Scholar]
- 48. Grimes P, Callender V. Tazarotene cream for postinflammatory hyperpigmentation and acne vulgaris in darker skin: a double‐blind, randomized, vehicle‐controlled study. Cutis 2006; 77: 45–50. [PubMed] [Google Scholar]
- 49. Kang SJ, Davis SA, Feldman SR, McMichael AJ. Dyschromia in skin of color. J Drugs Dermatol 2014; 13: 401–406. [PubMed] [Google Scholar]
- 50. Bershad S, Kranjac Singer G, Parente JE et al Successful treatment of acne vulgaris using a new method: results of a randomized vehicle‐controlled trial of short‐contact therapy with 0.1% tazarotene gel. Arch Dermatol 2002; 138: 481–489. [DOI] [PubMed] [Google Scholar]
- 51. Tan J. The safety and efficacy of four different fixed combination regimens of adapalene 0.1%/benzoyl peroxide 2.5% gel in the treatment of acne vulgaris: results from a randomized controlled trial. [DOI] [PubMed]
- 52. Pariser DM, Westmoreland P, Morris A, Gold MH, Liu Y, Graeber M. Long‐term safety and efficacy of a unique fixed‐dose combination gel of adapalene 0.1% and benzoyl peroxide 2.5% for the treatment of acne vulgaris. J Drugs Dermatol 2007; 6: 899–905. [PubMed] [Google Scholar]
- 53. Kwon HH, Park SY, Yoon JY, Min S, Suh DH. Do tutorials on application method enhance adapalene‐benzoyl peroxide combination gel tolerability in the treatment of acne? J Dermatol 2015; 42: 1058–1065. [DOI] [PubMed] [Google Scholar]
- 54. Myhill T, Coulson W, Nixon P et al Effect of supplementary patient educational material on treatment adherence and satisfaction among acne patients receiving adapalene 0.1%/benzoyl peroxide 2.5% gel. J Investig Dermatol 2016; 136: S164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ko HC, Song M, Seo SH, Oh CK, Kwon KS, Kim MB. Prospective, open‐label, comparative study of clindamycin 1%/benzoyl peroxide 5% gel with adapalene 0.1% gel in Asian acne patients: efficacy and tolerability. J Eur Acad Dermatol Venereol 2009; 23: 245–250. [DOI] [PubMed] [Google Scholar]
- 56. Tu P, Li GQ, Zhu XJ, Zheng J, Wong WZ. A comparison of adapalene gel 0.1% vs. tretinoin gel 0.025% in the treatment of acne vulgaris in China. J Eur Acad Dermatol Venereol 2001; 15(Suppl 3): 31–36. [DOI] [PubMed] [Google Scholar]
- 57. Percy SH. Safety and efficacy of adapalene gel 0.1% in acne vulgaris: results of a post‐marketing surveillance study. Indian J Dermatol Venereol Leprol 2003; 69: 277–280. [PubMed] [Google Scholar]
- 58. Goswami BC, Baishya B, Barua AB, Olson JA. Topical retinoyl beta‐glucuronide is an effective treatment of mild to moderate acne vulgaris in Asian‐Indian patients. Skin Pharmacol Appl Skin Physiol 1999; 12: 167–173. [DOI] [PubMed] [Google Scholar]
- 59. Chularojanamontri L, Tuchinda P, Kulthanan K, Varothai S, Winayanuwattikun W. A double‐blinded, randomized, vehicle‐controlled study to access skin tolerability and efficacy of an anti‐inflammatory moisturizer in treatment of acne with 0.1% adapalene gel. J Dermatolog Treat 2016; 27: 140–145. [DOI] [PubMed] [Google Scholar]
- 60. Kim WJ, Park JM, Ko HC, Kim BS, Kim MB, Song M. A split‐faced, observer‐blinded comparison study of topical adapalene/benzoyl peroxide and adapalene in the treatment of Asian acne patients. J Drugs Dermatol 2013; 12: 149–151. [PubMed] [Google Scholar]
- 61. Alexis AF, Cook‐Bolden FE, York JP. Adapalene/Benzoyl Peroxide Gel 0.3%/2.5%: a safe and effective acne therapy in all skin phototypes. J Drugs Dermatol 2017; 16: 574–581. [PubMed] [Google Scholar]
- 62. Weiss J, Stein Gold L, Leoni M, Rueda MJ, Liu H, Tanghetti E. Customized single‐agent therapy management of severe inflammatory acne: a randomized, double‐blind, parallel‐group, controlled study of a new treatment–Adapalene 0.3%‐Benzoyl Peroxide 2.5% Gel. J Drugs Dermatol 2015; 14: 1427–1435. [PubMed] [Google Scholar]
- 63. Munehiro A, Murakami Y, Shirahige Y et al Combination effects of cosmetic moisturisers in the topical treatment of acne vulgaris. J Dermatolog Treat 2012; 23: 172–176. [DOI] [PubMed] [Google Scholar]
- 64. Hayashi N, Kawashima M. Study of the usefulness of moisturizers on adherence of acne patients treated with adapalene. J Dermatol 2014; 41: 592–597. [DOI] [PubMed] [Google Scholar]
- 65. Matsunaga K, Leow YH, Chan R, Kerrouche N, Paliargues F. Adjunctive usage of a non‐comedogenic moisturizer with adapalene gel 0.1% improves local tolerance: a randomized, investigator‐blinded, split‐face study in healthy Asian subjects. J Dermatolog Treat 2013; 24: 278–282. [DOI] [PubMed] [Google Scholar]


