Abstract
Background and objectives
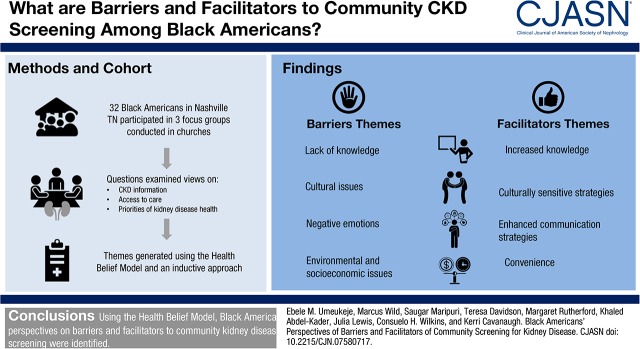
Incidence of ESKD is three times higher in black Americans than in whites, and CKD prevalence continues to rise among black Americans. Community-based kidney disease screening may increase early identification and awareness of black Americans at risk, but it is challenging to implement. This study aimed to identify participants’ perspectives of community kidney disease screening. The Health Belief Model provides a theoretic framework for conceptualization of these perspectives and optimization of community kidney disease screening activities.
Design, setting, participants, & measurements
Researchers in collaboration with the Tennessee Kidney Foundation conducted three focus groups of adults in black American churches in Nashville, Tennessee. Questions examined views on CKD information, access to care, and priorities of kidney disease health. Content analysis was used. Guided by the Health Belief Model, a priori themes were generated, and additional themes were derived from the data using an inductive approach.
Results
Thirty-two black Americans completed the study in 2014. Participants were mostly women (79%) with a mean age of 56 years old (range, 24–78). Two major categories of barriers to kidney disease screening were identified: (1) participant factors, including limited kidney disease knowledge, spiritual/religious beliefs, emotions, and culture of the individual; and (2) logistic factors, including lack of convenience and incentives and poor advertisement. Potential facilitators of CKD screening included provision of CKD education, convenience of screening activities, and use of culturally sensitive and enhanced communication strategies. Program recommendations included partnering with trusted community members, selecting convenient locations, tailored advertising, and provision of compensation.
Conclusions
Findings of this study suggest that provider-delivered culturally sensitive education and stakeholder engagement are critical to increase trust, decrease fear, and maximize participation and early identification of kidney disease among black Americans considering community screening.
Keywords: chronic kidney disease; clinical nephrology; ethnicity; Adult; United States; Female; Prevalence; Incidence; Focus Groups; Motivation; Research Personnel; Tennessee; African Americans; Kidney Diseases; Kidney Failure, Chronic; kidney; Fear; Emotions
Introduction
CKD is a public health concern affecting approximately 26 million United States adults, and another 20 million have risk factors for its development (1). Additionally, black Americans have a greater prevalence of macroalbuminuria compared with whites (2), a faster rate of progression to ESKD (3), and a persistently higher incidence of ESKD, which is estimated at three times that of whites (4). An analysis of recent trends in the United States revealed the stabilization of CKD prevalence in all racial subgroups, with the exception of black Americans (1). Explanatory factors for this continued rise in CKD prevalence in black Americans remain unknown and warrant aggressive examination. One cohort study has suggested that the disproportionate excess risk of CKD incidence in black Americans compared with whites may be explained in part by access to health care (5).
A common strategy to promote awareness of a health condition and identify individuals at risk is community-based health programs. Examples of this type of program specific to kidney disease include the National Kidney Foundation Kidney Early Evaluation Program (KEEP) (6,7) and the Kidney Disease Screening and Awareness Program, which focuses on underserved populations (8). The KEEP has been successful at identifying individuals at risk for kidney disease and advancing kidney disease knowledge to influence public health policies and practices (6). Despite the availability of community kidney disease screening, the participation rate is not optimal (6). People choose not to attend health-screening events for various reasons, such as lack of time and knowledge about the disease condition, fear of testing physicality, and potentially serious diagnoses (9,10). It has previously been suggested that black Americans are less likely to take advantage of screening programs (11) because of their limited knowledge of kidney disease (12) and low perceived susceptibility to CKD (13).
Previous research has identified barriers to seeking or accessing preventative care (14–16), and this is particularly true in black Americans (17). However, there is limited information specific to black Americans and their participation in kidney disease community screening. The Health Belief Model is a sociopsychologic theoretic framework that is widely and effectively used to explain health-seeking behavior influencing participation in screening tests (18–20). It posits that the motivation to undertake health behavior is informed by six critical elements of patients’ health beliefs: perceived seriousness, perceived susceptibility, perceived barriers versus benefits, perceived threat, self-efficacy, and cues to action. Informed by the Health Belief Model, the objective of this study was to assemble perspectives from black Americans who would be potential participants in a community screening for kidney disease program on the barriers and facilitators of successful engagement.
Materials and Methods
Participant Selection
In partnership with the Tennessee Kidney Foundation Kidney Awareness Risk Evaluation program (www.tennesseekidneyfoundation.org/programs-education/) and a network of black American churches in Nashville, Tennessee, fliers and verbal announcements were used to invite participants to focus groups. Participants were eligible if they were English-speaking black American adults at least 18 years old. They consisted of general community members and included those who had previously participated in kidney disease screening events as well as those who had not. The Vanderbilt University Medical Center Institutional Review Board approved this study, and all participants provided written informed consent.
Data Collection
During the focus group, participants completed a brief demographic survey. Focus group discussions lasted about 60 minutes each and were completed between August and December 2014. The discussions were led by a clinician researcher (E.M.U.) trained in moderating group discussions. A third party note taker was present to take detailed notes regarding the course of the focus group discussions, and all sessions were audio recorded and transcribed verbatim.
The focus group guide was developed by the research team through literature review (9,10,15,16,21) and uniformly used for all of the sessions (Supplemental Material). The Health Belief Model was used as a theoretic model to inform the generation of questions for the focus group guide and preset codes for qualitative content analysis. The focus group sessions were conducted until evidence of saturation of themes was noted.
Analyses
Transcriptions were analyzed using the HyperRESEARCH (version 3.5.2; ResearchWare Inc., Randolph, MA) qualitative data analysis software. Applying qualitative content analysis methodology (22–24) with combined deductive and inductive approach (23,25), open coding was performed. Guided by the Health Belief Model, a priori themes were deductively generated. Additional themes were inductively derived from the transcripts. The initial training included a partial coding of one of the focus group sessions to ensure that all definitions were set and clear among the coders. Three research team members (E.M.U., M.W., and M.R.) assigned theme and subtheme codes to each idea fragment. New codes were generated as needed. Any discrepancies in the coding were reconciled among the three coders, and a fourth member of the team (K.C.) provided input as needed for final reconciliation of the codes. Summary descriptive tables are reported.
Results
The numbers of participants in each focus group session were eight, ten, and 14 in the first, second, and third sessions, respectively (n=32). Participant characteristics are shown in Table 1. The mean age of the participants was 56 years old (SD=13), the majority was women (79%), and all were black American. Most had more than a high school education (82%) and health insurance (91%). Few self-reported a diagnosis of kidney disease (3%), but most reported having known risk factors, such as hypertension (70%), diabetes mellitus (24%), or a family history of kidney disease (27%). Participants also acknowledged family members receiving dialysis or having had a kidney transplant.
Table 1.
Characteristics of black American participants in focus groups that assessed barriers and facilitators of community screening for kidney disease
| Demographics | N |
|---|---|
| Age, yr, mean (SD) | 56 (13) |
| Age groups, yr | |
| 20–40 | 3 (9%) |
| 41–60 | 15 (47%) |
| >60 | 12 (38%) |
| Women | 24 (75%) |
| Income groups | |
| <$20,000 | 3 (9%) |
| Between $20,000 and $50,000 | 8 (25%) |
| >$50,000 to <$100,000 | 10 (31%) |
| >100,000 | 8 (25%) |
| Health insurance, yes | 28 (88%) |
| Education groups | |
| Some high school or less | 0 (0%) |
| High school diploma/GED | 6 (19%) |
| Some college | 8 (25%) |
| College degree | 18 (56%) |
| Self-report CKD | 1 (3%) |
| Self-report diabetes | 8 (25%) |
| Self-report hypertension | 22 (69%) |
| Family history of kidney disease | 9 (28%) |
| Family member(s) receiving dialysis | 5 (16%) |
| Family members with a kidney transplant | 1 (3%) |
| Family with diabetes | 14 (44%) |
| Family with hypertension | 17 (53%) |
GED, General Equivalency Diploma.
Barriers
Important individual and programmatic logistic factors influencing perceived barriers to CKD screening were discovered. These included four major themes: (1) knowledge of kidney disease and its associated risk factors; (2) cultural factors, such as limited trust; (3) emotions, including denial and fear; and (4) environmental and socioeconomic issues, including poor availability of health care and limited financial resources (Table 2).
Table 2.
Selected quotations to illustrate barriers by themes in focus groups that assessed barriers and facilitators of community screening for kidney disease
| Theme | Quotations |
|---|---|
| Knowledge themes | |
| Limited understanding of kidney disease | Kidney disease makes people lose weight (FG2 2) |
| Ignorance can be a huge factor; people just don’t know about the kidneys (FG3 1) | |
| Poor understanding of risk factors | I don’t understand what it means when my protein levels are high in the urine test. It threw me off—I had high levels of protein, but I’m not a red meat kind of person (FG3 2) |
| When my husband was diagnosed with high blood pressure, he initially wasn’t compliant with his medications. And I was the one to put the fear of God in him to make him understand why it’s important to make sure your blood pressure is managed… (FG3 5) | |
| Low health literacy | Most people are health illiterate, and so, they don’t know (FG3 5) |
| People don’t know that sodium is salt. You say lower your sodium, and they don’t know what you’re talking about (FG3 1) | |
| No belief that screening has benefits | We go to job fairs, we go to hair fairs, we do all those things, but there’s just something about going to health fairs that says to me that it is something [that we can give up]… (FG1 2) |
| The health fair is a necessity, but enough people don’t participate. A lot of times, we won’t come out unless there’s a gimmick or it’s not announced properly or if I don’t call Brother X to make sure he’s coming, I won’t go… (FG2 5) | |
| My relatives all lived long lives up to the high 90s and 100s. My grandfather was adamant about not going to the doctor, and he lived to be 98 yr old…you stop and think and start to believe that you don’t need to go to the doctor (FG2 6) | |
| Lack of CKD education and testing from clinicians | The failure here is the primary care providers. Unless you have an issue, they will not discuss it in general. Even routine physicals are so retracted now partly due to insurance companies, so unless you have a history of CKD or are more aware and bring it yourself, it won’t be discussed (FG1 1) |
| My primary care provider has told me nothing about kidney disease (FG3 2) | |
| And why don’t patients ask? Because they assume you know and they don’t want to look stupid, so they keep their mouths shut (FG3 10) | |
| A lot of times, doctors won’t say anything unless they see something. But because of our culture, I think it’s something we need to learn more about (FG3 1) | |
| I don’t think a lot of information is given to the community. I don’t specialize in kidney disease, but I will bet that black Americans get this disease more than anyone else, but yet a lot of the information is not out there in our health departments; our local health care centers… (FG2 1) | |
| “Ignorance is bliss” | People don’t ask [or go to the doctor], because they don’t want to know (FG3 11) |
| I think that the problem with the Y chromosome is that it has the denial gene inside of it (FG3 9) | |
| …[P]eople don’t want to make changes. They don’t want to get screened, because they want to keep doing the things that they’re doing (FG3 5) | |
| Cultural issues | |
| Low trust in health care activities | I think that some people, especially in the black American community, are not trusting of certain doctors, and they just don’t believe that they are getting what they need. They just don’t trust the community providers, and they just don’t go (FG2 7) |
| Some people are worried that the urine tests look for something other than protein—they just assume that you’re testing for drugs (FG3 1) | |
| Limited value for health | I would say not valuing your health would be a deterrent for health screening of any sort. This is because, from a health education standpoint, we don’t make changes until we value it (FG3 1) |
| I really wanted my sister to come to this focus group, because she is “antihealth.” She takes a pill when she chooses to (FG1 5) | |
| I’ve seen those illnesses in my family, and then, I say I wanna live…but a lot of people don’t know, and I see it all the time. I see it in people I’m around with. Hey, you need to get checked out. No, I’m cool; I’m good (FG3 12) | |
| Strong spirituality beliefs | Because it’s like God is going to heal it; God’s going to take care of my body. God also tells us that our body is the temple; it’s kind of up to us to take care of our body. We always think I can pray for it here and there, I can do this. God’s always said, if you destroy the temple (your body), He will destroy you. So you kind of have to always throw that out there too… (FG1 4) |
| In our community, a lot of times, we have great faith, and we believe that, when it comes to certain things, we can just give it to God and let him deal with it. When we say that we don’t claim it, what that means is that we’re not going to worry about it, because it’s not convenient right now… (FG3 4) | |
| Fear of side effects, ego, and machismo | This is caused by fear, ego, macho. A lot of men are afraid that if they go to the doctor, and they find out that they have high blood pressure, they will be given medications that will decrease their libido, sex drive (FG1 4) |
| Some of it has to do with the social paradigm that men have to be the strong ones; they have to be the ones who are supposed to be the helpers, and if they are the ones who get sick, then their manhood is challenged (FG3 3) | |
| Emotions | |
| Explicit kidney disease–related fear | My fear is that maybe I have a predisposition for kidney disease…my mother initially resisted dialysis; my sister is also on dialysis… (FG1 1) |
| Some people just do not want to know. We had this huge health fair, and you had to beg them to come get their blood pressure checked. Sometimes people just do not want to know, because they are more afraid of what the results will be, so they just say no, “I’ll just stick my head in the sand.” (FG2 4) | |
| I think it can be frightening…more so for older people (FG2 7) | |
| And young people are afraid of knowing, I believe (FG1 6) | |
| Young people feel like there’s no point in finding out diagnosis…we’re all going to die with something…they make excuses (FG1 6) | |
| Embarrassment and privacy | One of the things that I’ve found talking to different people is that, when you do a health fair at work, people are less prone to participate, because they’re really not sure if you have a health issue if it’s going to get back to your employer (FG1 6) |
| The location of the health fair matters…for instance, the corridor was not private enough for me (FG1 2) | |
| I noticed that, at the health care which we had, when you were told to go over to that table, then everyone knew that something was not right…people were kinda looking around (FG1 8) | |
| Environmental/socioeconomic issues | |
| Financial burden | The one thing that holds a lot of people back is health insurance and finances; even if you have health insurance, you still have to pay a certain amount, which people know, I can’t afford that, I just can’t afford to go with that. For instance, if I was to go into the hospital, my deductible will be $5000, and so well, I said that I’m not going. I can’t afford $5000; I’ll have to sell my house just to stay alive, so there are those kinds of factors (FG1 4) |
| I think finances really prevent a lot of people from checking up on themselves or trying (FG1 5) | |
| …[S]ome people can’t afford to go to the doctor and can’t afford insurance, so they don’t go get checked out until it’s too late or they have some type of disease, and then, they don’t have a choice but at health fairs; people come out to get a free screening and then maybe get checkups or try to get insurance and stuff… (FG1 4) | |
| Lack of convenience | Sometimes it depends on if you have other competing activities on that same day at the same time. You may not get as much turn out as you would otherwise (FG3 13) |
| …[I]f the health fair is conducted in the mall, those who don’t like the mall may not attend, while those who like the mall may prefer to spend their time shopping… (FG1 3) | |
| Poor/trivial advertisement | I’ve gone to a few health fairs at certain churches where a large portion of the membership didn’t know about the health fair (FG3 5) |
| I don’t always read emails or respond to texts [immediately] (FG1 6) | |
| You hear a lot about breast cancer, heart disease, etc., but you hardly ever hear about kidney disease (FG1 8) | |
| Lack of onsite incentives | If the health fair seems like it’s going to be really, really boring, then I don’t want to do it (FG3 4) |
| No one wants to show up at a health fair just to get stuck with a needle (FG3 3) |
FG, focus group.
Table 3.
Selected quotations to illustrate facilitators by themes in focus groups that assessed barriers and facilitators of community screening for kidney disease
| Theme | Quotations |
|---|---|
| Increased knowledge | |
| CKD education and testing from providers | A lot of times, doctors won’t say anything unless they see something. But because of our culture, I think it’s something we need to learn more about. Doctors should be saying, “because you have these risk factors and because of your background, we need to be paying close attention to…” (FG31) |
| I think a lot more education needs to be provided [in our health departments and local health centers], so people can have more awareness (FG2 1) | |
| [B]ut education is the key; we as a people, especially black Americans, take advantage of every opportunity for our lives, especially as we get older (FG1 5) | |
| Culturally sensitive strategies | |
| Influence of church leaders | If health fairs are marketed from the pulpit, it will help tremendously, because one person a lot of people do trust and believe in is the minister (FG2 2) |
| Positive peer pressure | If we ever do the job fair again, this is my thinking…we should form a group and call people and say, “look, we’re having a health fair, and this is something you may be interested in and you need to come and bring a friend with you” (FG1 3) |
| Integration of small group sessions | If we have a health fair, we should also have little seminars to discuss some certain areas which we need to address but more interactive type discussion, not just those boring ones (FG1 1) |
| When we had our health fair, our little sessions, that was a hit… (FG1 2) | |
| Increased participation from younger people | Have someone who is really good and animated in getting the point across, especially to the young ones, because they think they are invincible (FG1 1) |
| Enhanced communication strategies | |
| Critical role of physicians as communicators | Doctors really need to work…at enhancing their teams in their clinics and their hospitals…to reinforce and clarify with their patients and families (FG3 3) |
| The person that’s giving me my result, I would like for it to be a doctor or nurse practitioner (FG1 2) | |
| My experiences have been that, if you have an actual health professional, we tend to trust a little more, and to get that commitment from an agency is crucial to the success of your health fair (FG1 4) | |
| Tailored mode of communication | We have to use the form of advertisement that works…I’m old school, and I do believe that you need to call somebody up and talk to them and be more personal. I don’t always read emails or respond to texts in a timely manner (FG1 3) |
| We younger people like to text; we’re more text savvy, and I read my emails all day long, because they come through my phone (FG1 6) | |
| [Information at screening events is best communicated by] actual talk; a talk with a video or power point, because I’m a visual and audio learner…younger generations are more interactive. Older generations prefer brochures and pamphlets (FG3 2) | |
| Communication of relevant statistics and information | [P]ut out the statistics, because people are very visual. You see the numbers, oh there’s that many men, that many black Americans [affected] (FG1 8) |
| Sometimes you need people to be able to communicate to others and let them know what it is about these health disparities… (FG1 2) | |
| [W]hen you do urine tests, indicate exactly what is being tested and mention that it won’t be shared with their employers (FG3 4) | |
| Convenience | |
| Timing | Saturdays [preferably]. And if you did it during the week, it would have to be in the evenings after work hours…if it’s after work, you have that “I’ve gotta get there pressure” (FG1 2) |
| Location | The church or community center would be more convenient (FG1 3) |
| So doing it the way that we did it here at the church, no work involved, will encourage more people to participate (FG1 2) | |
| Onsite benefits | [O]ne [health fair] that I went to which I really enjoyed had a line dancing workshop with a lot of dances there (FG3 4) |
| We’re in a society now where people want to be entertained. So at our health fair, we had a bounce house for the kids. People want that as opposed to maybe finding out about their diagnosis or risk factors. It’s unfortunate, but that’s the way our culture is (FG3 10) |
FG, focus group.
Kidney Disease Knowledge
Limited Understanding of CKD.
Participants agreed that there was a lack of health knowledge in their community, including knowledge specific to CKD and its associated consequences. They felt that there was a paucity of information about CKD compared with the robust awareness about other diseases, such as heart disease and breast cancer. They also felt that this limitation in knowledge of CKD significantly contributed to a lack of adherence to prescribed medical therapy and self-care practices in addition to having a negative effect on the community’s degree of interest in screening for kidney disease.
Poor Understanding of Associated Risk Factors/Manifestations of CKD.
Participants expressed that their community did not know the risk factors for CKD. The participants also expressed uncertainty about the causes and significance of markers of kidney disease, such as proteinuria.
Low Health Literacy.
Participants noted that use of medical jargon and terms during screenings contributed to a low interest in participating. This was especially influential for people who have difficulty navigating the health care system.
Limited Appreciation of Long-Term Benefits of Screening.
The participants reflected on previous health screening events and reported that people prioritized attendance at job fairs or hair fairs over health fairs, because they disregarded the potential benefits of CKD screening, such as early diagnosis, establishing connections with health care, and early intervention to improve health outcomes. Participants also noted that some families experienced longevity even in the setting of CKD; therefore, the value of directly addressing it was questioned.
Lack of CKD Education and Testing from Providers.
Participants attributed the limited knowledge about CKD to a lack of counseling and testing by their current and previous clinical health care providers. Participants felt that often physicians did not routinely discuss health issues that could result from risk factors until people either became symptomatic or had abnormal laboratory results. They also admitted that they were reluctant to inquire about kidney health during their interactions with their primary care provider because of embarrassment and reluctance to display ignorance.
“Ignorance is Bliss.”
Ignorance was identified as a potential factor impeding participation in CKD screening. Participants attributed this ignorance to a lack of knowledge about kidney disease and its related risk factors as well as a lack of readiness to make health behavior changes. Participants suggested that community members may opt to be ignorant, because they prefer not to be aware of any existing diagnoses. This was felt to be more common in men.
Cultural
Low Trust.
The participants identified low trust in health care providers, the health care system, and community health screening events. Participants expressed that low trust in physicians was a primary reason that they do not engage with health evaluations. A specific concern was that urine tests were performed for drug screening rather than proteinuria.
Limited Value for Health.
Participants felt that there was a limited appreciation of health and resultant lack of motivation for health-promoting behavior by some people in their community.
Strong Spirituality Beliefs.
Participants expressed the belief that God was responsible for taking care of their bodies. They suggested that, sometimes, some people in their community stretched this belief to the extent that they give up their own responsibility for appropriate self-care practices and rather, focus on extensive prayers and faith-building practices.
Fear of Side Effects, Ego, and Machismo.
These were identified as factors that deterred men from participating in screening events. It was suggested that men worried about potential decrease in libido and sex drive from medications, such as antihypertensives. Participants also suggested that men resist the prospect of being labeled with a diagnosis that would force them to assume a “sick role,” which they felt would challenge their manhood.
Emotions
Explicit Kidney Disease–Related Fears.
Participants were specifically afraid of the possibility of being diagnosed with a disease that could lead to dialysis. There was controversy over whether this fear was more prevalent among older people in the community versus younger people, but there was agreement that this fear contributed significantly to nonparticipation in screening.
Fear of Embarrassment and Violation of Privacy.
Participants were concerned about health privacy at community events, because they are typically in a public venue. They reported that people would be even less likely to participate in screening events if conducted at their location of employment.
Environmental and Socioeconomic
Financial Burden of Disease if Diagnosed.
There was concern that the financial burden of disease if diagnosed deterred people from participating in community screening, including those who have health insurance but are unable to afford deductibles or medication payments. Conversely, participants also highlighted the fact that some people who had poor access to health care resources may default to health fairs for medical evaluation.
Lack of Convenience.
There was a unanimous agreement that optimal participation in screening events was affected by convenience. The timing and location of screening events were identified as highly important. They agreed that work places were not convenient for health screening fairs. There was no discussion about possible cost associated with attending screening health fairs, and participants did not express specific concerns about transportation costs related to health screening events.
Poor/Trivial Advertisement.
Participants expressed the notion that health fairs were not often optimally advertised, and they expressed concern over limited awareness of kidney disease compared with other disease conditions, such as cancer, heart disease, etc.
Lack of Onsite Incentives.
Participants felt that participation in health fairs is limited in the absence of onsite incentives. “No one wants to show up at a health fair just to get stuck with a needle and to get a urine test” (Focus Group 3: Participant 3).
Facilitators
Key facilitators to CKD screening events were identified and categorized into four major themes: (1) increased CKD knowledge, (2) culturally sensitive strategies, (3) enhanced communication strategies, and (4) convenience. There was unanimous consensus on the need for CKD education and testing from providers. Integration of culturally sensitive strategies was emphasized, and participants suggested that participation in health fairs was partly dependent on the assurance that people’s trusted friends, trusted religious leaders, or other respected members of the community would attend the screening events. They also suggested the need for incorporating specific strategies targeting increased participation from younger people.
Enhanced communication strategies were highlighted, including the critical role of physicians in communicating CKD information and results; use of tailored advertisement strategies; communication of relevant information, such as statistics about CKD; and full disclosure of use of biologic specimens in health fairs to dispel fears, build trust, and increase participation.
Many of the participants shared the view that the church or community center was often a preferred location and that weekends were more convenient. It was also suggested that the screening flow at health fairs should be structured in a standardized and consistent manner to avoid any sense of embarrassment, which participants may feel if they have the perception of having been singled out for additional diagnostic screening or additional counseling on the basis of the finding of an abnormal result. Participants highlighted that there was an existing notion in the community that people had to be incentivized to attend health fairs. These incentives ranged from the prospects of exciting “side attractions” at the health fairs, such as aerobics class, line dancing, and health walks, to even “bounce houses” for kids.
Discussion
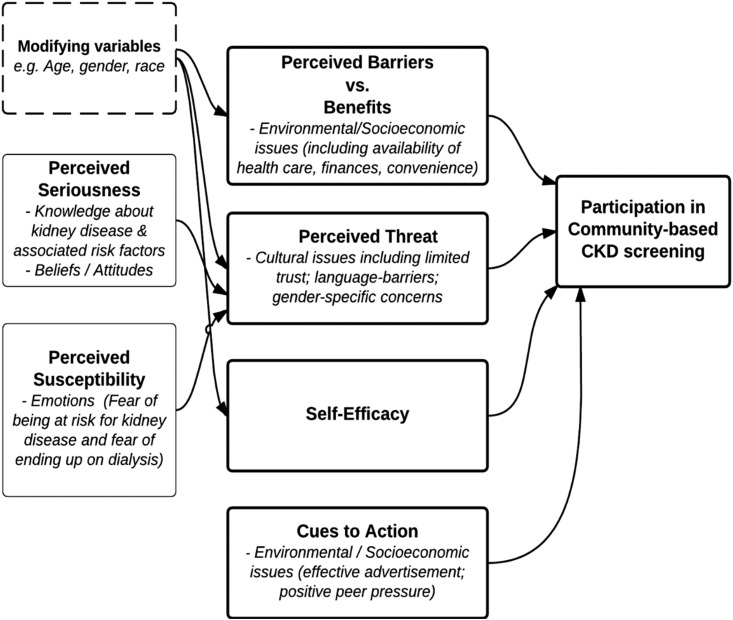
In this study, we applied the Health Belief Model to examine the knowledge and the psychologic factors influencing the uptake of community screening for kidney disease among black Americans. We also organized the themes of participants’ views into an architectural framework derived from this model to conceptualize preventive health behaviors (Figure 1) (26). The themes that are centered on knowledge, attitudes, and fears affect people’s perception of susceptibility to and severity of CKD. These both directly influence people’s perception of threat related to CKD diagnosis, which is also affected by underlying trust and communication factors. Tailored advertisement strategies and positive peer pressure are important examples of “cues to action.” The balance between the perceptions of barriers (including logistic factors) and benefits of participation in CKD screening in combination with the individual’s perception of threat of CKD and cues to action culminate in the decision to participate in community CKD screening.
Figure 1.
Application of the Health Belief Model to assess barriers and facilitators of community screening for kidney disease.
We broadly classified the key identified factors into person-centered factors and programmatic factors. The person-centered factors included trust; communication; emotions, such as fear and denial; kidney knowledge; and socioeconomic constraints. The program factors included convenience, privacy, and expectation of tangible benefits from participation in CKD screening.
Our findings confirmed those identified in previous research evaluating screening behavior in other chronic disease conditions (10,16,21,27) and CKD (15); however, we noted important novel barriers. We identified that, in black Americans, trust and effective communication from physicians about kidney disease were important in achieving optimal participation in community CKD screening.
Low trust among black Americans is associated with low participation in clinical research (28), including cancer (29) and cardiovascular disease prevention trials (30). Black Americans also report less trust in their physicians (31,32). Limited trust in the health care system by black Americans is associated with lower use of general preventative health services, such as dental and vision screening (33) and less use of women-specific preventative health screening, including pap smear and mammography (34). It even affects the uptake of prostate cancer screening resources (35–37). Our findings suggest that this extends beyond the health care setting to affect community efforts to improve health, such as kidney disease screening. More specifically, we discovered that participants were distrustful of urine collection during CKD screening, because they suspected that it would be used for purposes other than screening for proteinuria, such as drug testing. CKD screening programs need to make overt declarations of the purpose and use of any biologic specimens to build confidence and not deter participation.
Communication in addition to trust have been jointly identified as keys to promoting positive health behaviors, such as medication adherence and regular attendance at appointments for medical evaluation (10,38). Among black Americans, positive physician affect has been directly linked to patient trust (39), and “trustworthy” communication has been shown to enhance the effectiveness of outreach calls promoting colorectal cancer screening (40). These findings suggest that culturally sensitive health communication is also crucial in community screening for high-risk minority populations (21). This involves training program staff in communication skills that will facilitate rapport building, positive affect, and trust building.
Knowledge is a fundamental component of developing a true appreciation for one’s own health status, risk of future poor health, and risks or benefits of specific behaviors. Low levels of perceived CKD knowledge have been identified even among patients who have active follow-up in a CKD clinic, and they are associated with poor ratings of their physician’s communication (41). Methods to improve patient kidney knowledge in clinical encounters and more broadly, the community are important to increase awareness of susceptibility to CKD and encourage CKD screening. The National Kidney Disease Education Program (42), among others, offers tools that can be used by clinicians in either of these settings.
A key belief expressed was that people are absolved of the responsibility of self-care, because “God will take care of them.” Consideration for the spirituality of patients with CKD should be encouraged because of its direct correlation with health-related quality of life, mental health, and life expectancy (43). Collaboration with community spiritual leaders, especially to endorse rationale for screening participation, is also recommended in programs for black Americans.
Programmatic considerations were also identified as significant contributors to screening nonparticipation. In addition to convenience of screening locations, embarrassment associated with privacy was identified as a barrier to participation in screening. Participants suggested that there may be stigma related to the diagnosis of kidney disease. Chronic disease–specific stigma is emerging as a critical factor in diabetes diagnosis and self-care (44). Particular attention to the structure of the venue and ways to protect privacy with curtains or other visual barriers are required. Incentives, such as gift items, free food, and entertainment, were identified as major motivators for participation in CKD screening health fairs. This is similar to findings in other minority and economically disadvantaged populations (16,27) and can be addressed using the input of respected community leaders to shift people’s focus away from the expectation of tangible compensation toward the conviction of potential long-term benefits accrued from early diagnosis and early intervention.
A key strength of this study is the fact that it identifies both individual and programmatic factors important to black Americans, and it provides detailed examples that can be acted on to improve community CKD screening. Importantly, this study captures the views of people who are at risk for kidney disease. Our sample size was small and limited to black Americans in one geographic area of the United States, potentially limiting the generalizability of our findings to all black American patients or other racial or ethnic subgroups. We also acknowledge that a couple of the focus group sessions had a large sample size, which could lead to split conversations and also, limit participants’ opportunity to speak; however, deliberate steps were taken to minimize chances of these happening. Furthermore, although we reached theoretic saturation overall and captured a wide range of demographic characteristics of black American participants, this sample was composed of fairly highly educated black Americans, and there was a limited proportion of men. However, the beliefs discussed here are held by some black Americans in Tennessee; they may hold true for black Americans in other parts of the United States, and they may affect participation in kidney disease screening events.
This study identified key issues that may inform the future design of more effective, culturally sensitive community CKD screening programs targeting vulnerable minority population who are at high risk for kidney disease. Our findings emphasize the need for establishing strong collaborative partnerships with community leaders and stakeholders, with the aim of building trust among minority populations. These stakeholders will facilitate the dissemination of information and help optimize the logistics of upcoming health fairs. Our findings also emphasize the need to ensure that screening practices are standardized for all participants, regardless of results, to avoid any perception of breech of health privacy. The flow at screening events, use of biologic specimens, and details of screening practices should be fully disclosed. Programs and communities that address each of these pathways will effectively engage more black American participants in the goal to prevent kidney disease.
Disclosures
None.
Supplementary Material
Acknowledgments
We acknowledge support from the Tennessee Kidney Foundation (TKF) and Teresa Davidson (CEO of TKF from November 2004 to October 2015). This work was supported, in part, by National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases grants F32DK102366 (to E.M.U.), T32DK007569 (to E.M.U. and S.M.), and K23DK080952 (to K.C.). K.A.-K. was supported by NIH Career Development award K23DK090304. K.C. is further supported by NIH grant R01DK03935-01A1.
This work was presented as a poster at the 2015 Vanderbilt Master of Public Health Practicum Colloquium in Nashville, Tennessee, January 20, 2015. An abstract was presented at the 2016 National Kidney Foundation Spring Clinical Meeting in Boston, Massachusetts, April 27–May 1.
E.M.U. and K.C. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Community-Based CKD Screening in Black Americans,” on pages 521–523.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.07580717/-/DCSupplemental.
References
- 1.Murphy D, McCulloch CE, Lin F, Banerjee T, Bragg-Gresham JL, Eberhardt MS, Morgenstern H, Pavkov ME, Saran R, Powe NR, Hsu CY; Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance Team : Trends in prevalence of chronic kidney disease in the United States. Ann Intern Med 165: 473–481, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coresh J, Byrd-Holt D, Astor BC, Briggs JP, Eggers PW, Lacher DA, Hostetter TH: Chronic kidney disease awareness, prevalence, and trends among U.S. adults, 1999 to 2000. J Am Soc Nephrol 16: 180–188, 2005 [DOI] [PubMed] [Google Scholar]
- 3.Hunsicker LG, Adler S, Caggiula A, England BK, Greene T, Kusek JW, Rogers NL, Teschan PE: Predictors of the progression of renal disease in the Modification of Diet in Renal Disease Study. Kidney Int 51: 1908–1919, 1997 [DOI] [PubMed] [Google Scholar]
- 4.Lipworth L, Mumma MT, Cavanaugh KL, Edwards TL, Ikizler TA, Tarone RE, McLaughlin JK, Blot WJ: Incidence and predictors of end stage renal disease among low-income blacks and whites. PLoS One 7: e48407, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Evans K, Coresh J, Bash LD, Gary-Webb T, Köttgen A, Carson K, Boulware LE: Race differences in access to health care and disparities in incident chronic kidney disease in the US. Nephrol Dial Transplant 26: 899–908, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vassalotti JA, Li S, Chen SC, Collins AJ: Screening populations at increased risk of CKD: The Kidney Early Evaluation Program (KEEP) and the public health problem. Am J Kidney Dis 53[Suppl 3]: S107–S114, 2009 [DOI] [PubMed] [Google Scholar]
- 7.Whaley-Connell AT, Tamura MK, Jurkovitz CT, Kosiborod M, McCullough PA: Advances in CKD detection and determination of prognosis: Executive summary of the National Kidney Foundation-Kidney Early Evaluation Program (KEEP) 2012 annual data report. Am J Kidney Dis 61[Suppl 2]: S1–S3, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsiao LL, Wu J, Yeh AC, Shieh EC, Cui C, Li A, Polding LC, Ahmed R, Lim K, Lu TS, Rhee CM, Bonventre JV: The Kidney Disease Screening and Awareness Program (KDSAP): A novel translatable model for increasing interest in nephrology careers. J Am Soc Nephrol 25: 1909–1915, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eborall H, Stone M, Aujla N, Taub N, Davies M, Khunti K: Influences on the uptake of diabetes screening: A qualitative study in primary care. Br J Gen Pract 62: e204–e211, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Legido-Quigley H, Camacho Lopez PA, Balabanova D, Perel P, Lopez-Jaramillo P, Nieuwlaat R, Schwalm JD, McCready T, Yusuf S, McKee M: Patients’ knowledge, attitudes, behaviour and health care experiences on the prevention, detection, management and control of hypertension in Colombia: A qualitative study. PLoS One 10: e0122112, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Waterman AD, Browne T, Waterman BM, Gladstone EH, Hostetter T: Attitudes and behaviors of African Americans regarding early detection of kidney disease. Am J Kidney Dis 51: 554–562, 2008 [DOI] [PubMed] [Google Scholar]
- 12.Wright JA, Wallston KA, Elasy TA, Ikizler TA, Cavanaugh KL: Development and results of a kidney disease knowledge survey given to patients with CKD. Am J Kidney Dis 57: 387–395, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boulware LE, Carson KA, Troll MU, Powe NR, Cooper LA: Perceived susceptibility to chronic kidney disease among high-risk patients seen in primary care practices. J Gen Intern Med 24: 1123–1129, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deskins S, Harris CV, Bradlyn AS, Cottrell L, Coffman JW, Olexa J, Neal W: Preventive care in Appalachia: Use of the theory of planned behavior to identify barriers to participation in cholesterol screenings among West Virginians. J Rural Health 22: 367–374, 2006 [DOI] [PubMed] [Google Scholar]
- 15.Jennette CE, Vupputuri S, Hogan SL, Shoham DA, Falk RJ, Harward DH: Community perspectives on kidney disease and health promotion from at-risk populations in rural North Carolina, USA. Rural Remote Health 10: 1388, 2010 [PubMed] [Google Scholar]
- 16.Murimi MW, Harpel T: Practicing preventive health: The underlying culture among low-income rural populations. J Rural Health 26: 273–282, 2010 [DOI] [PubMed] [Google Scholar]
- 17.Goldade K, Sidhwani S, Patel S, Brendt L, Vigliaturo J, Kasiske B, Ahluwalia JS, Israni AK: Kidney transplant patients’ perceptions, beliefs, and barriers related to regular nephrology outpatient visits. Am J Kidney Dis 57: 11–20, 2011 [DOI] [PubMed] [Google Scholar]
- 18.Gillam SJ: Understanding the uptake of cervical cancer screening: The contribution of the health belief model. Br J Gen Pract 41: 510–513, 1991 [PMC free article] [PubMed] [Google Scholar]
- 19.Sung JJ, Choi SY, Chan FK, Ching JY, Lau JT, Griffiths S: Obstacles to colorectal cancer screening in Chinese: A study based on the health belief model. Am J Gastroenterol 103: 974–981, 2008 [DOI] [PubMed] [Google Scholar]
- 20.Taheri-Kharameh Z, Noorizadeh F, Sangy S, Zamanian H, Shouri-Bidgoli AR, Oveisi H: Factors associated with adherence to colorectal cancer screening among moderate risk individuals in Iran. Asian Pac J Cancer Prev 16: 8371–8375, 2015 [DOI] [PubMed] [Google Scholar]
- 21.Massaro E, Claiborne N: Effective strategies for reaching high-risk minorities with diabetes. Diabetes Educ 27: 820–828, 2001 [DOI] [PubMed] [Google Scholar]
- 22.Hsieh HF, Shannon SE: Three approaches to qualitative content analysis. Qual Health Res 15: 1277–1288, 2005 [DOI] [PubMed] [Google Scholar]
- 23.Elo S, Kyngäs H: The qualitative content analysis process. J Adv Nurs 62: 107–115, 2008 [DOI] [PubMed] [Google Scholar]
- 24.Berg BL: An introduction to content analysis. In: Qualitative Research Methods for the Social Sciences, 5th Ed, Boston, Pearson/Allyn & Bacon, 2004. pp 265–298 [Google Scholar]
- 25.Cho JY, Lee E: Reducing confusion about grounded theory and qualitative content analysis: Similarities and differences. Qual Rep 19: 1–20, 2014 [Google Scholar]
- 26.Orji R, Vassileva J, Mandryk R: Towards an effective health interventions design: An extension of the health belief model. Online J Public Health Inform 4: pii: ojphi.v4i3.4321, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shah VO, Ghahate DM, Bobelu J, Sandy P, Newman S, Helitzer DL, Faber T, Zager P: Identifying barriers to healthcare to reduce health disparity in Zuni Indians using focus group conducted by community health workers. Clin Transl Sci 7: 6–11, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Corbie-Smith G, Thomas SB, St George DM: Distrust, race, and research. Arch Intern Med 162: 2458–2463, 2002 [DOI] [PubMed] [Google Scholar]
- 29.Haynes-Maslow L, Godley P, Dimartino L, White B, Odom J, Richmond A, Carpenter W: African American women’s perceptions of cancer clinical trials. Cancer Med 3: 1430–1439, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Braunstein JB, Sherber NS, Schulman SP, Ding EL, Powe NR: Race, medical researcher distrust, perceived harm, and willingness to participate in cardiovascular prevention trials. Medicine (Baltimore) 87: 1–9, 2008 [DOI] [PubMed] [Google Scholar]
- 31.Peek ME, Gorawara-Bhat R, Quinn MT, Odoms-Young A, Wilson SC, Chin MH: Patient trust in physicians and shared decision-making among African-Americans with diabetes. Health Commun 28: 616–623, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR: Race and trust in the health care system. Public Health Rep 118: 358–365, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Strickland J, Strickland DL: Barriers to preventive health services for minority households in the rural south. J Rural Health 12: 206–217, 1996 [DOI] [PubMed] [Google Scholar]
- 34.O’Malley AS, Sheppard VB, Schwartz M, Mandelblatt J: The role of trust in use of preventive services among low-income African-American women. Prev Med 38: 777–785, 2004 [DOI] [PubMed] [Google Scholar]
- 35.Carpenter WR, Godley PA, Clark JA, Talcott JA, Finnegan T, Mishel M, Bensen J, Rayford W, Su LJ, Fontham ET, Mohler JL: Racial differences in trust and regular source of patient care and the implications for prostate cancer screening use. Cancer 115: 5048–5059, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jones RA, Steeves R, Williams I: How African American men decide whether or not to get prostate cancer screening. Cancer Nurs 32: 166–172, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jones RA, Steeves R, Williams I: Family and friend interactions among African-American men deciding whether or not to have a prostate cancer screening. Urol Nurs 30: 189–193, 2010 [PMC free article] [PubMed] [Google Scholar]
- 38.Khatib R, Schwalm JD, Yusuf S, Haynes RB, McKee M, Khan M, Nieuwlaat R: Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: A systematic review and meta-analysis of qualitative and quantitative studies. PLoS One 9: e84238, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martin KD, Roter DL, Beach MC, Carson KA, Cooper LA: Physician communication behaviors and trust among black and white patients with hypertension. Med Care 51: 151–157, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Albright K, Richardson T, Kempe KL, Wallace K: Toward a trustworthy voice: Increasing the effectiveness of automated outreach calls to promote colorectal cancer screening among African Americans. Perm J 18: 33–37, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wright Nunes JA, Wallston KA, Eden SK, Shintani AK, Ikizler TA, Cavanaugh KL: Associations among perceived and objective disease knowledge and satisfaction with physician communication in patients with chronic kidney disease. Kidney Int 80: 1344–1351, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang ES, Brown SE, Thakur N, Carlisle L, Foley E, Ewigman B, Meltzer DO: Racial/ethnic differences in concerns about current and future medications among patients with type 2 diabetes. Diabetes Care 32: 311–316, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fradelos EC, Tzavella F, Koukia E, Papathanasiou IV, Alikari V, Stathoulis J, Panoutsopoulos G, Zyga S: Integrating chronic kidney disease patient’s spirituality in their care: Health benefits and research perspectives. Mater Sociomed 27: 354–358, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Browne JL, Ventura AD, Mosely K, Speight J: Measuring the stigma surrounding type 2 diabetes: Development and validation of the Type 2 Diabetes Stigma Assessment Scale (DSAS-2). Diabetes Care 39: 2141–2148, 2016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.