Abstract
Background and objectives
Serious fall injuries in the setting of ESKD may be associated with poor access to kidney transplant. We explored the burden of serious fall injuries among patients on dialysis and patients on the deceased donor waitlist and the associations of these fall injuries with waitlisting and transplantation.
Design, setting, participants, & measurements
Our analytic cohorts for the outcomes of (1) waitlisting and (2) transplantation included United States adults ages 18–80 years old who (1) initiated dialysis (n=183,047) and (2) were waitlisted for the first time (n=37,752) in 2010–2013. Serious fall injuries were determined by diagnostic codes for falls plus injury (fracture, joint dislocation, or head trauma) in inpatient and emergency department claims; the first serious fall injury after cohort entry was included as a time-varying exposure. Follow-up ended at the specified outcome, death, or the last date of follow-up (September 30, 2014). We used multivariable Cox proportional hazards models to determine the independent associations between serious fall injury and waitlisting or transplantation.
Results
Overall, 2-year cumulative incidence of serious fall injury was 6% among patients on incident dialysis; with adjustment, patients who had serious fall injuries were 61% less likely to be waitlisted than patients who did not (hazard ratio, 0.39; 95% confidence interval, 0.35 to 0.44). Among incident waitlisted patients (4% 2-year cumulative incidence), those with serious fall injuries were 29% less likely than their counterparts to be subsequently transplanted (hazard ratio, 0.71; 95% confidence interval, 0.63 to 0.80).
Conclusions
Serious fall injuries among United States patients on dialysis are associated with substantially lower likelihood of waitlisting for and receipt of a kidney transplant.
Keywords: ESKD, geriatric nephrology, kidney transplantation, Adult, Humans, United States, Incidence, Accidental Falls, Proportional Hazards Models, Inpatients, Follow-Up Studies, Kidney Failure, Chronic, Waiting Lists, Tissue Donors, Fractures, Bone, Joint Dislocations, Emergency Service, Hospital, Craniocerebral Trauma, renal dialysis
Introduction
Among older adults, serious fall–related injuries are associated with poor outcomes, including mortality, institutionalization, and functional decline (1–3). Serious fall injuries are common among older persons with CKD (4), particularly as they approach ESKD (5); after dialysis initiation, nearly one half of older patients on hemodialysis report falls over 12 months (6). Approximately one in ten older patients on dialysis experience a serious fall injury in the first year (5), a burden approximately 40% higher than that in the general population age ≥65 years old (7). Such falls may provide prognostic information: we found that older patients on dialysis who experienced serious fall injuries in the year before dialysis initiation were more likely to have subsequent serious fall injuries, be hospitalized, use skilled nursing facilities, and die in the first year of dialysis (8). Furthermore, the multifactorial nature of falls and related injuries in this population means that serious fall injuries may be prognostic beyond traditional measures of frailty or lower extremity function.
However, little is known about serious fall injuries in the relatively younger patients who may seek kidney transplantation. Transplantation is associated with better outcomes than dialysis (9,10), but most (98%) patients with ESKD spend at least some time on dialysis (9), potentially putting them at risk for serious fall injuries that may adversely affect access to kidney transplantation. Patients on dialysis who have serious fall injuries may be evaluated negatively for potential placement on the deceased donor waitlist, and patients on the waitlist may lose their chance at transplantation because of perceived poor functioning associated with serious fall injuries. Furthermore, patients who experience serious fall injuries may be more likely to die before they can be waitlisted or transplanted. Here, we examine the burden of serious fall injuries and the associations between placement on the deceased kidney donor waitlist (waitlisting) and transplantation with serious fall injuries among United States patients initiating dialysis and being placed on the waitlist for the first time, respectively.
Materials and Methods
Study Population and Data Sources
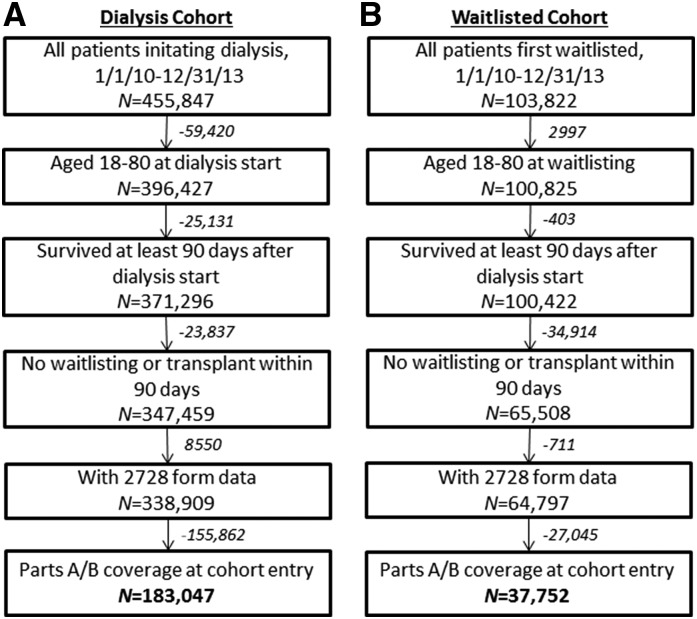
The study was approved by the Emory University Institutional Review Board. Data from Medicare ESKD eligibility (Centers for Medicare and Medicaid Services-2728 [CMS-2728]) forms and Part A (inpatient) and Part B (outpatient) claims were obtained from the US Renal Data System (USRDS) (9). Two retrospective cohorts were formed for the outcomes of waitlisting and transplantation. For both cohorts, patients ages 18–80 years old who initiated dialysis in 2010–2013 and survived ≥90 days after dialysis start were included (Figure 1). Patients with cohort entry (Figure 2) or outcomes in the first 90 days of ESKD treatment were excluded along with those lacking CMS-2728 forms. The cohorts were further limited to those with both Parts A and B coverage at cohort entry (Figure 1). Patients without Part B claims were excluded to avoid differential ascertainment of serious fall injuries treated in the emergency department. Overall, 183,047 patients on incident dialysis and 37,752 incident waitlisted patients were included in the cohorts to examine waitlisting and transplantation outcomes, respectively (Figure 1).
Figure 1.
Study exclusions leading to cohorts of 183,047 dialysis patients and 37,752 waitlisted patients. Flow of participants in incident 2010–2013 United States cohorts of (A) patients on dialysis and (B) waitlisted patients.
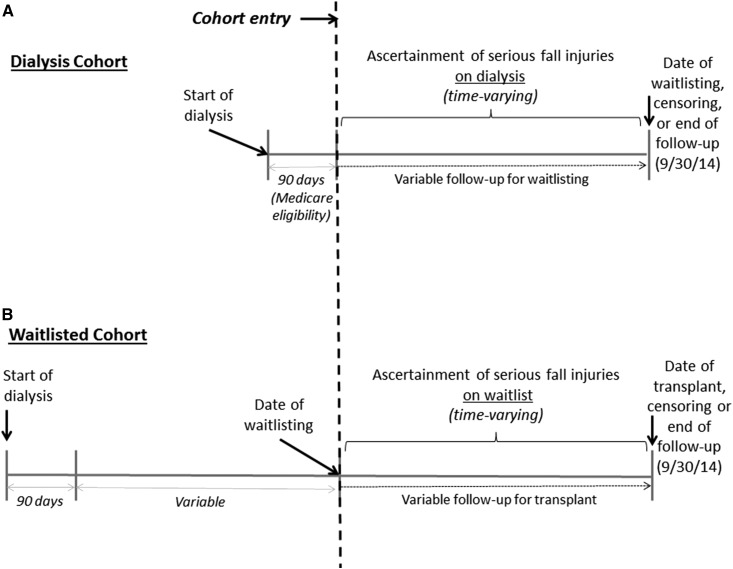
Figure 2.
The study timeline shows that cohort entry began at 90 days for dialysis patients and at the date of waitlisting for waitlisted patients, with patients followed until outcome or censoring. Cohort entry (dotted line), follow-up, and ascertainment of serious fall injuries for incident 2010–2013 United States cohorts of (A) patients on dialysis and (B) waitlisted patients.
Study Variables
Serious Fall Injuries.
Serious fall injuries were defined by International Classification of Diseases, Ninth Revision (ICD-9) codes in combined claims data from inpatient and emergency encounters using a claims-based algorithm (4,11,12). Emergency encounters were defined by place of service or the type of provider. Serious fall injuries were attributed to claims with a fall-related E code (8800–8889) and an injury code for nonpathologic skull, facial, cervical, clavicle, humeral, forearm, pelvic, hip, fibula, tibia, or ankle fractures (80000–80619, 8070–8072, 8080–8089, 81000–81419, 8180–8251, or 8270–8291), brain injury (85200–85239), or dislocation of the hip, knee, shoulder, or jaw (8300–83219, 83500–83513, or 83630–83660). For claims without a fall-related E code, claims for the serious injuries listed above were defined as a serious fall injury in the absence of a motor vehicle accident E code (8100–8199). Serious fall injuries were treated as time-varying exposures from the start of dialysis or waitlisting (Figure 2); after a patient experienced a serious fall injury, they remained exposed for the remainder of the study.
Outcomes.
Outcomes included time to waitlisting (90 days after dialysis start to date of waitlisting) and time to transplant (date of waitlisting to date of transplant). These time to event outcomes were censored for loss to follow-up (including uncertain dialysis modality, withdrawal from dialysis, and recovery of kidney function), death, end of Medicare Parts A and B coverage, or end of study follow-up (September 30, 2014).
Other Variables.
Incident age, sex, treatment modality history, and date of dialysis start were obtained from the USRDS standard analytic files. Age at waitlisting was estimated using the incident age, date of dialysis start, and date of waitlisting. Race/ethnicity and body mass index were provider reported on the Medicare ESKD eligibility form (CMS-2728). For the dialysis cohort, comorbid conditions were assigned if present on the CMS-2728. Because of the lag between dialysis initiation and time of waitlisting for the waitlisted cohort, comorbid conditions were assigned if present either on the CMS-2728 or in inpatient discharge codes from all hospital discharges in the year up to and including the cohort entry using the diagnostic codes outlined in the CMS Chronic Conditions Warehouse algorithms (13). Renal osteodystrophy and osteoporosis at the time of the serious injury fall were assessed by ICD-9 codes (588.0 and 733.X, respectively).
Statistical Analyses
Patient characteristics were summarized overall and by whether patients had at least one serious fall injury during follow-up. Continuous and categorical characteristics were compared by serious fall injury status by t tests and Fisher exact or chi-squared tests, respectively. Extended Cox proportional hazards models, allowing for changes in serious fall injury status over time, were used to obtain hazard ratios (HRs) for the association of serious fall injuries and time to event outcomes. Adjustment was performed for potential confounding demographic and clinical characteristics in the primary models. Sensitivity analyses included (1) additional adjustment for dialysis modality and additional comorbid conditions, (2) examination of the association with serious fall injuries defined only as those with an accompanying E code, and (3) examination of the association only among those without a fall on dialysis before waitlisting (waitlisted cohort only). We also examined (4) potential effect modification by age, sex, and race/ethnicity using stratified models and testing of interaction terms and (5) cumulative incidence of both mortality and transplant access outcomes and sub-HRs using flexible parametric and Fine and Gray (14) survival models incorporating the competing risk of mortality. Complete case analysis was used to handle missing covariate data; overall, 1%–2% of observations were excluded from the fully adjusted models because of missingness. All analyses were performed with Stata v 14.2 (College Station, TX).
Results
Characteristics of Patients on Incident Dialysis
Overall, 7% of patients on incident dialysis had at least one serious fall injury during follow-up (Table 1). Cumulative incidence rates of serious fall injury were 4% and 6% at 1 and 2 years, respectively. Those who had serious fall injuries were older (66 versus 61 years old), were more likely to be women (55% versus 42%), were white (64% versus 51%), had hemodialysis as their first modality (96% versus 93%), and had more comorbid conditions at dialysis start (Table 1) compared with those who did not have serious fall injuries. Patients excluded from this cohort because of lack of Part B coverage were slightly younger (59 years old) than the included patients (62 years old). Serious fall injuries in this cohort were primarily fractures, most commonly in the limbs (Table 2).
Table 1.
Characteristics of United States patients ages 18–80 years old initiating dialysis in 2010–2013 overall and by serious fall injury over follow-up
| Characteristic at Dialysis Start | Overall | At Least One Serious Fall Injury | |
|---|---|---|---|
| No | Yes | ||
| N (%) | 183,047 | 170,680 (93) | 12,367 (7) |
| Demographics | |||
| Mean (SD) age, yr | 62 (13) | 61 (13) | 66 (11) |
| Women, % | 43 | 42 | 55 |
| Race/ethnicity, % | |||
| Non-Hispanic white | 52 | 51 | 64 |
| Black | 29 | 30 | 19 |
| Hispanic white | 14 | 14 | 13 |
| Other | 5 | 5 | 4 |
| Clinical | |||
| Hemodialysis as first modality, % | 93 | 93 | 96 |
| Mean body mass index (SD), kg/m2 | 30.1 (8.3) | 30.2 (8.3) | 29.6 (8.2) |
| Comorbid conditions,a % | |||
| Diabetes | 61 | 61 | 66 |
| Ischemic heart disease | 19 | 19 | 24 |
| Cerebrovascular disease | 10 | 10 | 12 |
| Hypertension | 88 | 88 | 87 |
| Congestive heart failure | 32 | 31 | 38 |
| Cancer | 7 | 7 | 8 |
| Chronic obstructive pulmonary disease | 11 | 10 | 13 |
| Peripheral vascular disease | 13 | 13 | 16 |
| Amputation | 4 | 4 | 4 |
| Inability to walk | 7 | 7 | 8 |
| Inability to transfer | 4 | 4 | 4 |
| Institutionalized | 8 | 8 | 10 |
n=183,047 for all in the dialysis cohort, except body mass index (n=181,469), race/ethnicity (n=182,744), and perceived as ineligible (n=181,684).
As reported on the Centers for Medicare and Medicaid Services-2728 Medical Evidence form at dialysis start.
Table 2.
Type and location of serious fall injuries among United States patients ages 18–80 years old initiating dialysis in 2010–2013
| Type/Location of Serious Fall Injury | No. (%) of Injuriesa |
|---|---|
| Total no. of patients with at least one serious fall injury | 12,367 |
| Total no. of serious fall injuries | 15,641 |
| Type of injury | |
| Fracture | 14,350 (92) |
| Dislocation | 334 (2) |
| Subarachnoid and subdural hemorrhage after injury | 1034 (7) |
| Location of injury | |
| Head (skull, face, jaw) | 1216 (8) |
| Spine | 367 (2) |
| Chest (ribs, sternum, clavicle) | 2130 (14) |
| Pelvis/hip | 1283 (8) |
| Upper limb (shoulder to wrist) | 3412 (22) |
| Lower limb (femur to metatarsals) | 7903 (51) |
Total column percentages may exceed 100% because of multiple types and locations of injuries during a single fall event.
Association of Serious Fall Injuries with Waitlisting among Patients on Incident Dialysis
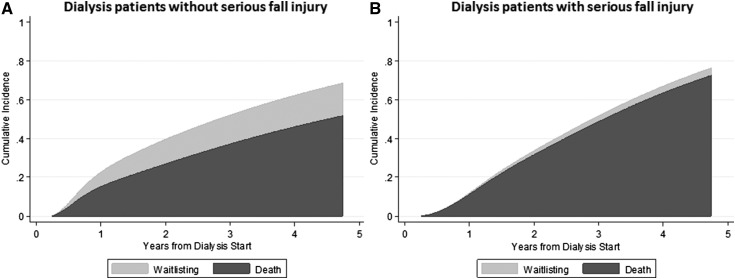
Crude waitlisting rates among those with versus without serious fall injuries on dialysis were 1.3 versus 7.6 per 100 patient-years (Table 3). With adjustment for demographic and clinical factors, patients who had serious fall injuries while on dialysis remained 61% less likely to be waitlisted than patients who did not (HR, 0.39; 95% confidence interval [95% CI], 0.35 to 0.44) (Table 3). Additional adjustment for dialysis modality, peripheral vascular disease, amputation, inability to walk or transfer, and institutionalization gave nearly identical results (Table 3). When only serious injury falls for which there was an accompanying E code were considered (23%), results were similar in magnitude (Table 3). Renal osteodystrophy and osteoporosis were coded in 1% and 6%, respectively, of serious fall injury events overall and 0.8% and 5%, respectively, of serious fall injury events lacking E codes. In subgroup analyses by age, sex, and race/ethnicity, the effect of serious fall injuries was strongest in the older and other race patients, but no interactions were statistically significant (Table 3). Cumulative incidence of mortality and waitlisting (Figure 3) indicates that mortality was more frequent than waitlisting in both groups but that this effect was disproportionately higher among patients on dialysis who had serious fall injuries while on dialysis; the sub-HR for waitlisting among those with serious fall injuries versus not, adjusting for the competing risk of mortality, was 0.19 (95% CI, 0.17 to 0.21).
Table 3.
Association between serious fall injuries and waitlisting among United States patients ages 18–80 years old initiating dialysis in 2010–2013
| Measure/Modela | Overall | Serious Fall Injurya | |
|---|---|---|---|
| No | Yes | ||
| No. of patients | 183,047 | 170,680 | 12,367 |
| No. of patients waitlisted | 18,811 | 18,470 | 341 |
| Total patient-yr | 269,965.1 | 243,425.9 | 26,539.2 |
| Waitlisting rate, per 100 patient-yr | 7.0 | 7.6 | 1.3 |
| Hazard ratios for waitlisting by serious fall injury (95% CI) | |||
| Primary analyses | |||
| Crude | 1.00 (Reference) | 0.31 (0.28 to 0.35) | |
| Adjusted, demographicsb | 1.00 (Reference) | 0.38 (0.34 to 0.43) | |
| Adjusted, demographics + clinicalb | 1.00 (Reference) | 0.39 (0.35 to 0.44) | |
| Sensitivity analysesc | |||
| Additional adjustment for | |||
| Dialysis modality | 1.00 (Reference) | 0.40 (0.36 to 0.45) | |
| Peripheral vascular disease | 1.00 (Reference) | 0.39 (0.35 to 0.44) | |
| Amputation | 1.00 (Reference) | 0.39 (0.35 to 0.44) | |
| Inability to walk | 1.00 (Reference) | 0.39 (0.35 to 0.44) | |
| Inability to transfer | 1.00 (Reference) | 0.39 (0.35 to 0.44) | |
| Institutionalization | 1.00 (Reference) | 0.39 (0.35 to 0.44) | |
| Fall injuries with E codes only | 1.00 (Reference) | 0.37 (0.30 to 0.47) | |
| Subgroup analysesc | |||
| Age, yr | |||
| 18–39 | 1.00 (Reference) | 0.43 (0.32 to 0.58) | |
| 40–64 (P40–64×18–39=0.70) | 1.00 (Reference) | 0.40 (0.35 to 0.46) | |
| ≥65 (P≥65×18–39=0.10) | 1.00 (Reference) | 0.35 (0.28 to 0.43) | |
| Sex | |||
| Men | 1.00 (Reference) | 0.38 (0.32 to 0.44) | |
| Women (Pwomen×men=0.56) | 1.00 (Reference) | 0.41 (0.35 to 0.48) | |
| Race/ethnicity | |||
| Non-Hispanic white | 1.00 (Reference) | 0.39 (0.33 to 0.45) | |
| Black (Pblack×white=0.59) | 1.00 (Reference) | 0.39 (0.31 to 0.50) | |
| Hispanic white (PHispanic×white=0.20) | 1.00 (Reference) | 0.45 (0.36 to 0.57) | |
| Other (Pother×white=0.10) | 1.00 (Reference) | 0.24 (0.14 to 0.42) | |
n=181,204 for models. 95% CI, 95% confidence interval.
From cohort entry to outcome or censoring.
Demographics: age, sex, and race/ethnicity. Clinical: demographics plus body mass index, comorbid diabetes, ischemic heart disease, hypertension, cerebrovascular disease, congestive heart failure, chronic obstructive pulmonary disease, and cancer.
Using the fully adjusted (demographics + clinical) model.
Figure 3.
Over 5 years of follow-up, dialysis patients were more likely to die than to be waitlisted, and this effect was more pronounced among those who experienced a serious fall injury over follow-up. (A) Cumulative incidence of death and waitlisting among patients on dialysis who did not experience a serious fall injury during follow-up. (B) Cumulative incidence of death and waitlisting among patients on dialysis who experienced a serious fall injury at any point during follow-up.
Incident Waitlisted Patient Characteristics
Among incident waitlisted patients, 5% had a serious fall injury during follow-up (Tables 4). Cumulative incidence rates of serious fall injury were 3% and 4% at 1 and 2 years, respectively. Those who had serious fall injuries were older (53 versus 50 years old), were more likely to be women (48% versus 37%), were white (48% versus 35%), were on hemodialysis at waitlisting (87% versus 85%), and had more comorbid conditions at waitlisting than those patients who did not. Those who experienced serious injury falls were more likely than those who did not to be removed from the waitlist because of deteriorating condition (11% versus 5%). Of those with serious fall injuries who were removed from the waitlist, 93% were removed after rather than before the fall event; of these, 4%, 10%, and 18% were removed within 30 days, 90 days, and 6 months, respectively, of the event. Patients who were excluded versus included from this waitlisted cohort because of lack of Part B coverage were of similarly ages (52 versus 52 years old). Fractures were the most common injury, and limbs were the most common site of injury (Table 5).
Table 4.
Characteristics of United States patients ages 18–80 years old placed on the deceased donor kidney transplant waitlist for the first time in 2010–2013 overall and by serious fall injury during follow-up
| Characteristic at Waitlisting | Overall | At Least One Serious Fall Injury | |
|---|---|---|---|
| No | Yes | ||
| N (%) | 37,752 | 35,808 (95) | 1944 (5) |
| Demographics | |||
| Mean (SD) age, yr | 50 (13) | 50 (13) | 53 (13) |
| Women, % | 38 | 37 | 48 |
| Race/ethnicity, % | |||
| Non-Hispanic white | 36 | 35 | 48 |
| Non-Hispanic black | 36 | 36 | 25 |
| Hispanic | 22 | 22 | 22 |
| Other | 7 | 7 | 5 |
| Clinical | |||
| Hemodialysis, % | 85 | 85 | 87 |
| Mean body mass index at dialysis start (SD), kg/m2 | 29.6 (7.3) | 29.6 (7.2) | 29.4 (7.5) |
| Mean dialysis vintage (SD), yr | 2.3 (2.4) | 2.3 (2.4) | 2.4 (2.4) |
| Comorbid conditions in year before cohort entry,a % | |||
| Diabetes | 51 | 50 | 61 |
| Ischemic heart disease | 13 | 13 | 16 |
| Cerebrovascular disease | 5 | 5 | 6 |
| Hypertension | 91 | 91 | 89 |
| Congestive heart failure | 19 | 19 | 23 |
| Cancer | 3 | 3 | 4 |
| Chronic obstructive pulmonary disease | 4 | 3 | 4 |
| Peripheral vascular disease | 6 | 6 | 9 |
| Amputation | 2 | 2 | 3 |
| Inability to walk | 1 | 1 | 1 |
| Inability to transfer | 0.4 | 0.4 | 0.5 |
| Institutionalized | 1 | 1 | 2 |
n=37,752 for all in waitlisted cohort, except body mass index (n=37,307), race/ethnicity (n=37,607), and perceived as ineligible (n=34,742).
As reported on the Centers for Medicare and Medicaid Services-2728 Medical Evidence form at dialysis start or in inpatient discharge codes from all hospital discharges in the year up to and including the date of waitlisting. Peripheral vascular disease, amputation, inability to walk and transfer, and institutionalization were obtained from the Centers for Medicare and Medicaid Services-2728 only.
Table 5.
Type and location of serious fall injuries among United States patients ages 18–80 years old placed on the deceased donor kidney transplant waitlist for the first time in 2010–2013
| Type/Location of Serious Fall Injury | No. (%) of Injuriesa |
|---|---|
| Total no. of patients with at least one serious fall injury | 1944 |
| Total no. of serious fall injuries | 2493 |
| Type of injury | |
| Fracture | 2334 (91) |
| Dislocation | 77 (3) |
| Subarachnoid and subdural hemorrhage after injury | 159 (6) |
| Location of injury | |
| Head (skull, face, jaw) | 191 (8) |
| Spine | 48 (2) |
| Chest (ribs, sternum, clavicle) | 302 (12) |
| Pelvis/hip | 144 (6) |
| Upper limb (shoulder to wrist) | 573 (23) |
| Lower limb (femur to metatarsals) | 1331 (53) |
Total column percentages may exceed 100% because of multiple types and locations of injuries during a single fall event.
Association of Serious Fall Injuries with Transplantation
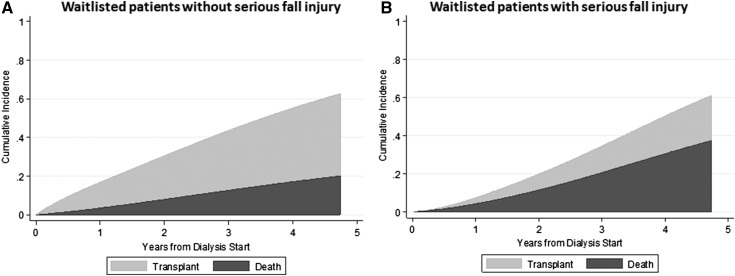
Crude transplantation rates among those with versus without serious fall injuries on the waitlist were 5.77 versus 13.71 per 100 patient-years (Table 6). With adjustment for demographic and clinical factors, patients who had serious fall injuries while on the waitlist remained 29% less likely to be transplanted than patients who did not (HR, 0.71; 95% CI, 0.63 to 0.80) (Table 6). Additional adjustment for dialysis modality at waitlisting and additional comorbid conditions at dialysis start gave nearly identical results. When only serious injury falls for which there was an accompanying E code were considered (21%), results were similar in magnitude (Table 6). Renal osteodystrophy and osteoporosis were coded in 0.9% and 5%, respectively, of serious fall injury events overall and 0.6% and 5%, respectively, of serious fall injury events lacking E codes. In the cohort excluding those with serious fall injuries on dialysis before waitlisting (n=760), results did not change (Table 6). Restricting the outcome to deceased donor transplant (100% and 71% of transplants among those with and without serious fall injuries, respectively) gave similar but attenuated results (HR, 0.82; 95% CI 0.72 to 0.93). In subgroup analyses by age, sex, and race/ethnicity, the effect of serious fall injuries on likelihood of transplantation was strongest in the youngest and white patients, but no interactions were statistically significant (Table 6). Cumulative incidence of mortality and transplantation (Figure 4) shows that mortality was more frequent than transplantation in patients who had serious fall injuries while on the waitlist; the sub-HR for transplantation among those with serious fall injuries versus not, adjusting for the competing risk of mortality, was 0.42 (95% CI, 0.38 to 0.47).
Table 6.
Association between serious fall injuries and kidney transplantation among United States patients ages 18–80 years old initially placed on the waitlist in 2010–2013
| Measure/Modela | Overall | Serious Fall Injurya | |
|---|---|---|---|
| No | Yes | ||
| No. of patients | 37,752 | 35,808 | 1944 |
| No. of patients transplanted | 8924 | 8638 | 286 |
| Total patient-yr | 67,978.9 | 63,020.6 | 4958.3 |
| Transplant rate per 100 patient-yr | 13.1 | 13.7 | 5.8 |
| Hazard ratios for waitlisting by serious fall injury (95% CI) | |||
| Primary analyses | |||
| Crude | 1.00 (Reference) | 0.77 (0.68 to 0.87) | |
| Adjusted, demographicsb | 1.00 (Reference) | 0.73 (0.65 to 0.82) | |
| Adjusted, demographics + clinicalb | 1.00 (Reference) | 0.71 (0.63 to 0.80) | |
| Sensitivity analysesc | |||
| Additional adjustment for | |||
| Dialysis modality | 1.00 (Reference) | 0.71 (0.63 to 0.80) | |
| Peripheral vascular disease | 1.00 (Reference) | 0.71 (0.63 to 0.80) | |
| Amputation | 1.00 (Reference) | 0.71 (0.63 to 0.80) | |
| Inability to walk | 1.00 (Reference) | 0.71 (0.63 to 0.80) | |
| Inability to transfer | 1.00 (Reference) | 0.71 (0.63 to 0.80) | |
| Institutionalization | 1.00 (Reference) | 0.71 (0.63 to 0.80) | |
| Fall injuries with E codes only | 1.00 (Reference) | 0.68 (0.54 to 0.87) | |
| Among those with no fall injuries before waitlisting | 1.00 (Reference) | 0.70 (0.62 to 0.79) | |
| Subgroup analysesc | |||
| Age, yr | |||
| 18–39 | 1.00 (Reference) | 0.62 (0.47 to 0.81) | |
| 40–64 (P40–64×18–39=0.47) | 1.00 (Reference) | 0.74 (0.64 to 0.86) | |
| ≥65 (P≥65×18–39=0.85) | 1.00 (Reference) | 0.68 (0.52 to 0.90) | |
| Sex | |||
| Men | 1.00 (Reference) | 0.68 (0.58 to 0.81) | |
| Women (Pwomen×men=0.61) | 1.00 (Reference) | 0.74 (0.62 to 0.87) | |
| Race/ethnicity | |||
| Non-Hispanic white | 1.00 (Reference) | 0.65 (0.56 to 0.77) | |
| Black (Pblack×white=0.11) | 1.00 (Reference) | 0.80 (0.63 to 1.02) | |
| Hispanic white (PHispanic×white=0.56) | 1.00 (Reference) | 0.78 (0.58 to 1.05) | |
| Other (Pother×white=0.35) | 1.00 (Reference) | 0.83 (0.49 to 1.38) | |
n=37,164 for models. 95% CI, 95% confidence interval.
From cohort entry to outcome or censoring.
Demographics: age, sex, and race/ethnicity. Clinical: body mass index, dialysis vintage, comorbid diabetes, ischemic heart disease, and hypertension.
Using the fully adjusted (demographics + clinical) model.
Figure 4.
Over 5 years of follow-up, waitlisted patients without a serious fall injury were more likely to be transplanted than to die, but the opposite was true for those with a serious fall injury. (A) Cumulative incidence of death and transplant among waitlisted patients who did not experience a serious fall injury during follow-up. (B) Cumulative incidence of death and transplant among waitlisted patients who experienced a serious fall injury at any point during follow-up.
Discussion
Among patients on incident dialysis and incident waitlisted patients, 6% and 4%, respectively, experienced serious fall injuries over 2 years. Although the waitlisted cohort, on average, was generally younger, was more likely to be men, and had fewer comorbid conditions than the dialysis cohort, serious fall injuries occurred more frequently among older patients, women, and sicker patients in each cohort. However, even with adjustment for these factors, patients on incident dialysis and incident waitlisted patients who experienced a serious fall injury remained approximately 60% and 30% less likely to be waitlisted and transplanted, respectively, than those who did not. The magnitude of the effects was even stronger when death was treated as a competing risk. Differences in observed associations by age, sex, and race/ethnicity were minimal and were not statistically significant.
Reduced rates of kidney transplantation among patients who experience serious fall injuries may be clinically appropriate if these serious fall injuries serve as proxies for vulnerable states that may lead to poor outcomes for the patient with a transplant. For example, frailty has been shown to be associated with falls and serious fall injuries among older adults (15) and patients on hemodialysis of all ages (16–18). Frailty is common even among the healthier transplant-eligible population of patients with ESKD, with as many as one in five kidney transplant recipients considered frail at the time of transplant (19). Importantly, frailty at transplant is associated with early hospital readmissions (20), graft loss (21), and mortality (22) among kidney transplant recipients. Poor overall physical functioning and specifically, lower extremity strength/mobility represent other important vulnerable conditions, separate from frailty, that could be indicated in serious fall injury events. Both have been shown to be strongly associated with higher risk of morbidity and mortality among transplant recipients (23–25).
For restricted access to transplantation on the basis of serious fall injuries to be clinically appropriate, providers must be aware of the injuries. This may be more likely among dialysis providers, who may strongly influence the likelihood of waitlisting via patient education, referral for evaluation, and assistance with completion evaluation requirements but who have little influence on likelihood of transplantation among the waitlisted. In contrast, transplant providers do not see patients as frequently, if at all, between waitlisting and transplant. The median waiting time in the United States is 3.5 years (9), a time period over which some patients may experience substantial deterioration in condition. Hospitalizations, including those for serious fall injuries, are not tracked by or considered in the national policy that determines deceased donor kidney allocation (26). Such events would likely have to be communicated by the dialysis provider to the transplant provider directly, which is difficult in our fragmented care system. Thus, transplant providers may not be aware of serious fall injuries among these patients during the waitlisted period, even when patients present for transplant. This discrepancy in provider awareness may partially explain the difference in magnitude of the effect of serious fall injuries on access to waitlisting among patients on dialysis versus access to transplant among waitlisted patients that we observed. However, underlying differences in the populations, including differences in competing risks of mortality, which we showed here to be far greater before waitlisting than on the waitlist, most likely contribute as well.
It is important to note that a one size fits all approach, in which access to transplantation is denied on the basis of suspected vulnerability to poor outcomes in the setting of a serious fall injury, is likely to unnecessarily restrict access to transplantation among patients with ESKD, because conditions, such as frailty, may be reversible after transplantation (19). Furthermore, frailty and poor functioning are not universal underlying causes of serious fall injuries in this population. Falls are multifactorial, with intrinsic factors (such as older age, being a woman, cognitive impairment, and underlying bone disease as well as frailty components, including weakness and gait problems), extrinsic factors (such as polypharmacy, substance abuse, hazards in the home, poor lighting, and inappropriate footwear), and risk exposure all contributing to falls. Thus, although serious fall injuries may provide useful prognostic information when they do occur, multifactorial interventions administered by dialysis providers, transplant providers, or both to prevent falls and related injuries should also be considered among patients on dialysis (18,27). Multifactorial interventions may include functional assessment, exercise, visual testing, home barrier assessment, and medication review. Many medications have delayed excretion in patients on dialysis, and drugs for pain, sleep, and anxiety (28,29) as well as drugs that are generally avoided in elderly patients (30) are commonly prescribed in dialysis and could lead to hypotension, dizziness, and/or altered mental status, potentially leading to falls. Additionally, dialysis-related factors, such as intradialytic hypotension (31) and underlying metabolic bone disease (32), may contribute to risk of falls and related injuries. Strategies to address these factors, such as the recent proposed quality measures to restrict ultrafiltration rates among United States patients on hemodialysis, may reduce hypotension related to large, rapid volume shifts (33); this may, in turn, decrease fall risk overall in this population. Particularly for patients who may be eligible for transplantation, such interventions may prevent further declines in functioning and the robustness necessary for good transplant outcomes.
Other limitations not noted above deserve mention. The exclusion of patients without Medicare Part B coverage may have led to lack of generalizability to the United States ESKD population as well as selection bias. However, we found that patients who were excluded versus included on the basis of Part B data availability were only slightly younger. Furthermore, this exclusion was necessary to include serious fall injuries treated on an outpatient basis only (which may be more likely among transplant-eligible patients). Misclassification of serious injuries as related to falls is possible, because E codes were missing in >70% of serious fall injury events; however, simultaneous coding of nontraumatic causes of fractures was infrequent, and similar results were obtained when serious fall injuries were limited to those with accompanying E codes. The algorithm for detecting serious fall injuries has not been validated, although it was first developed and used in the geriatric literature (12) on the basis of high correlations (κ=0.76) of these combinations of claims with self-report as fall as the cause of injury (34). There is also the potential for misclassification of the outcomes and comorbid conditions using claims data, although we attempted to maximize specificity by combining 2728 and claims data for the latter. As with all observational studies, residual confounding by unmeasured factors, such as history of falls (with or without injury), measures of physical performance, the use of assistive devices, and contraindications to transplant, is possible. However, this study also has several important strengths, including the capture of all treated United States patients with ESKD, limited loss to follow-up because of universal coverage of ESKD services by the CMS, completion of the Medicare eligibility form for all treated patients, and availability of claims data for all inpatient and outpatient services after the start of dialysis and when on the waitlist.
In conclusion, we found that, among United States patients with ESKD, serious fall injuries are associated with substantially lower likelihood of waitlisting for and receipt of a kidney transplant. Although primarily descriptive in nature, these data suggest that serious fall injuries may serve as a potential prognostic factor that could be tracked by dialysis and transplant providers to assess ongoing suitability for transplant. Future studies on the added value of serious fall injuries in prognostication among patients on dialysis could inform both the possibility of mandatory reporting of fall injuries to transplant centers and the new Kidney Allocation System, which matches recipient life expectancy to quality of the donor organ. Additionally, because serious fall injuries may result in risk for poor outcomes even among the previously robust, our results suggest that access to transplantation (and associated better outcomes) may be improved through the prevention of falls and related injuries among transplant-eligible patients with ESKD via design and testing of multicomponent fall prevention interventions tailored to this population.
Disclosures
None.
Acknowledgments
The data reported here have been supplied by the US Renal Data System.
Support was provided through an award (to L.C.P.) from the Extramural Grant Program by Satellite Healthcare, a not-for-profit renal care provider, and Career Development award IK2CX000856 (to C.B.B.) from the US Department of Veterans Affairs.
This work was presented in part at the American Geriatrics Society 2017 Annual Scientific Meeting held May 18–20, 2017, in San Antonio, Texas.
The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US Government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Gill TM, Murphy TE, Gahbauer EA, Allore HG: Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidemiol 178: 418–425, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gill TM, Murphy TE, Gahbauer EA, Allore HG: The course of disability before and after a serious fall injury. JAMA Intern Med 173: 1780–1786, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tinetti ME, Williams CS: Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med 337: 1279–1284, 1997 [DOI] [PubMed] [Google Scholar]
- 4.Bowling CB, Bromfield SG, Colantonio LD, Gutiérrez OM, Shimbo D, Reynolds K, Wright NC, Curtis JR, Judd SE, Franch H, Warnock DG, McClellan W, Muntner P: Association of reduced eGFR and albuminuria with serious fall injuries among older adults. Clin J Am Soc Nephrol 11: 1236–1243, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Plantinga LC, Patzer RE, Franch HA, Bowling CB: Serious fall injuries before and after initiation of hemodialysis among older ESRD patients in the United States: A retrospective cohort study. Am J Kidney Dis 70: 76–83, 2017 [DOI] [PubMed] [Google Scholar]
- 6.Cook WL, Tomlinson G, Donaldson M, Markowitz SN, Naglie G, Sobolev B, Jassal SV: Falls and fall-related injuries in older dialysis patients. Clin J Am Soc Nephrol 1: 1197–1204, 2006 [DOI] [PubMed] [Google Scholar]
- 7.Bergen G, Stevens MR, Burns ER: Falls and fall injuries among adults aged >=65 years: United States, 2014. MMWR Morb Mortal Wkly Rep 65: 993–998, 2016 [DOI] [PubMed] [Google Scholar]
- 8.Bowling CB, Hall R, Khakharia A, Franch HA, Plantinga LC: Serious fall injury history and adverse health outcomes after initiating hemodialysis among older U.S. adults. J Gerontol A Biol Sci Med Sci 2018, in press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.United States Renal Data System : USRDS 2016 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2016 [Google Scholar]
- 10.Tonelli M, Wiebe N, Knoll G, Bello A, Browne S, Jadhav D, Klarenbach S, Gill J: Systematic review: Kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant 11: 2093–2109, 2011 [DOI] [PubMed] [Google Scholar]
- 11.Shimbo D, Barrett Bowling C, Levitan EB, Deng L, Sim JJ, Huang L, Reynolds K, Muntner P: Short-term risk of serious fall injuries in older adults initiating and intensifying treatment with antihypertensive medication. Circ Cardiovasc Qual Outcomes 9: 222–229, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tinetti ME, Han L, Lee DS, McAvay GJ, Peduzzi P, Gross CP, Zhou B, Lin H: Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med 174: 588–595, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Medicare & Medicaid Services: Chronic Conditions Data Warehouse, 2018. Available at: https://www.ccwdata.org/web/guest/home. Accessed January 6, 2018
- 14.Fine JP, Gray RJ: A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94: 496–509, 1999 [Google Scholar]
- 15.Rothman MD, Leo-Summers L, Gill TM: Prognostic significance of potential frailty criteria. J Am Geriatr Soc 56: 2211–2216, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Delgado C, Shieh S, Grimes B, Chertow GM, Dalrymple LS, Kaysen GA, Kornak J, Johansen KL: Association of self-reported frailty with falls and fractures among patients new to dialysis. Am J Nephrol 42: 134–140, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McAdams-DeMarco MA, Suresh S, Law A, Salter ML, Gimenez LF, Jaar BG, Walston JD, Segev DL: Frailty and falls among adult patients undergoing chronic hemodialysis: A prospective cohort study. BMC Nephrol 14: 224, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kutner NG, Zhang R, Huang Y, Wasse H: Falls among hemodialysis patients: Potential opportunities for prevention? Clin Kidney J 7: 257–263, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McAdams-DeMarco MA, Isaacs K, Darko L, Salter ML, Gupta N, King EA, Walston J, Segev DL: Changes in frailty after kidney transplantation. J Am Geriatr Soc 63: 2152–2157, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McAdams-DeMarco MA, Law A, Salter ML, Chow E, Grams M, Walston J, Segev DL: Frailty and early hospital readmission after kidney transplantation. Am J Transplant 13: 2091–2095, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McAdams-DeMarco MA, Law A, Tan J, Delp C, King EA, Orandi B, Salter M, Alachkar N, Desai N, Grams M, Walston J, Segev DL: Frailty, mycophenolate reduction, and graft loss in kidney transplant recipients. Transplantation 99: 805–810, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McAdams-DeMarco MA, Ying H, Olorundare I, King EA, Haugen C, Buta B, Gross AL, Kalyani R, Desai NM, Dagher NN, Lonze BE, Montgomery RA, Bandeen-Roche K, Walston JD, Segev DL: Individual frailty components and mortality in kidney transplant recipients. Transplantation 101: 2126–2132, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reese PP, Shults J, Bloom RD, Mussell A, Harhay MN, Abt P, Levine M, Johansen KL, Karlawish JT, Feldman HI: Functional status, time to transplantation, and survival benefit of kidney transplantation among wait-listed candidates. Am J Kidney Dis 66: 837–845, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kutner NG, Zhang R, Bowles T, Painter P: Pretransplant physical functioning and kidney patients’ risk for posttransplantation hospitalization/death: Evidence from a national cohort. Clin J Am Soc Nephrol 1: 837–843, 2006 [DOI] [PubMed] [Google Scholar]
- 25.Nastasi AJ, McAdams-DeMarco MA, Schrack J, Ying H, Olorundare I, Warsame F, Mountford A, Haugen CE, González Fernández M, Norman SP, Segev DL: Pre-kidney transplant lower extremity impairment and post-kidney transplant mortality. Am J Transplant 18: 189–196, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lynch RJ, Zhang R, Patzer RE, Larsen CP, Adams AB: First-year waitlist hospitalization and subsequent waitlist and transplant outcome. Am J Transplant 17: 1031–1041, 2017 [DOI] [PubMed] [Google Scholar]
- 27.Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, Koch ML, Trainor K, Horwitz RI: A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med 331: 821–827, 1994 [DOI] [PubMed] [Google Scholar]
- 28.Koncicki HM, Brennan F, Vinen K, Davison SN: An approach to pain management in end stage renal disease: Considerations for general management and intradialytic symptoms. Semin Dial 28: 384–391, 2015 [DOI] [PubMed] [Google Scholar]
- 29.Winkelmayer WC, Mehta J, Wang PS: Benzodiazepine use and mortality of incident dialysis patients in the United States. Kidney Int 72: 1388–1393, 2007 [DOI] [PubMed] [Google Scholar]
- 30.Kondo N, Nakamura F, Yamazaki S, Yamamoto Y, Akizawa T, Akiba T, Saito A, Kurokawa K, Fukuhara S: Prescription of potentially inappropriate medications to elderly hemodialysis patients: Prevalence and predictors. Nephrol Dial Transplant 30: 498–505, 2015 [DOI] [PubMed] [Google Scholar]
- 31.Palmer BF, Henrich WL: Recent advances in the prevention and management of intradialytic hypotension. J Am Soc Nephrol 19: 8–11, 2008 [DOI] [PubMed] [Google Scholar]
- 32.Beaubrun AC, Kilpatrick RD, Freburger JK, Bradbury BD, Wang L, Brookhart MA: Temporal trends in fracture rates and postdischarge outcomes among hemodialysis patients. J Am Soc Nephrol 24: 1461–1469, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Flythe JE, Assimon MM, Wenger JB, Wang L: Ultrafiltration rates and the Quality Incentive Program: Proposed measure definitions and their potential dialysis facility implications. Clin J Am Soc Nephrol 11: 1422–1433, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tinetti ME, Doucette J, Claus E, Marottoli R: Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc 43: 1214–1221, 1995 [DOI] [PubMed] [Google Scholar]