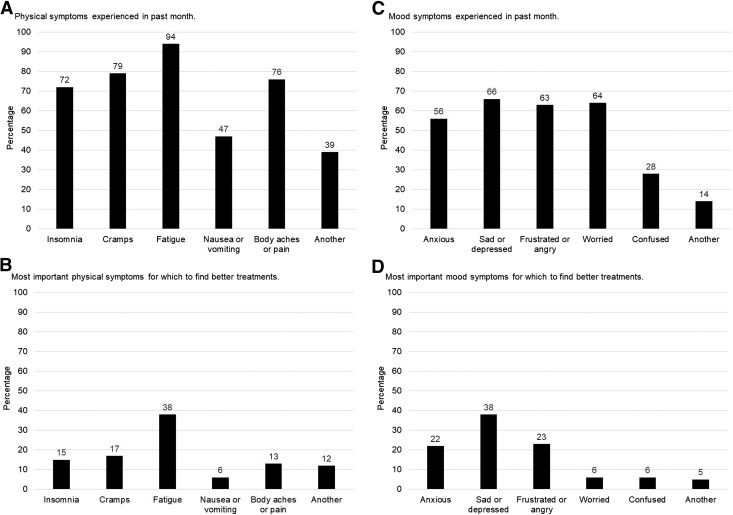
Abstract
Background and objectives
Individuals receiving in-center hemodialysis experience a high symptom burden that detrimentally affects their quality of life. There are few evidence-based interventions for symptom relief in this population. To stimulate innovation in symptom management, data on patient symptom prioritization and treatment preferences are needed. We undertook this study to (1) identify patient-prioritized symptoms for the development of symptom relief therapies and (2) elicit preferences for treatments among individuals receiving hemodialysis.
Design, setting, participants, & measurements
We conducted a mixed methods study that included focus groups in Carrboro, North Carolina; Tucson, Arizona; and Seattle, Washington and a nationally distributed online survey. Focus group transcripts were analyzed for patterns, and the highest priority symptoms were determined on the basis of frequency and report severity. We used focus group findings to inform survey items. Focus group and survey results were crossvalidated and synthesized for final symptom prioritization.
Results
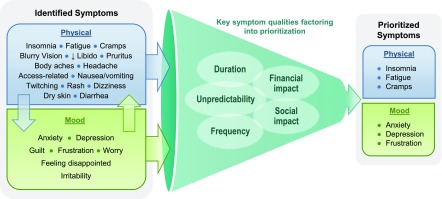
There were 32 participants across three focus groups and 87 survey respondents from 27 states in the United States. The physical symptoms of insomnia, fatigue, muscle cramping, and nausea/vomiting and the mood symptoms of anxiety and depressed mood were reported by participants in all focus groups. Among survey respondents, fatigue (94%), cramping (79%), and body aches (76%) were the most common physical symptoms, and feeling depressed (66%), worried (64%), and frustrated (63%) were the most common mood symptoms. The top-prioritized symptoms were consistent across focus group and survey participants and included the physical symptoms insomnia, fatigue, and cramping and the mood symptoms anxiety, depression, and frustration. Participants indicated that symptom frequency, duration, unpredictability, and social and financial effects factored most heavily into symptom prioritization.
Conclusions
Patients prioritized the physical symptoms of insomnia, fatigue, and cramping and the mood symptoms of anxiety, depression, and frustration as the top symptoms for which to find new therapies.
Keywords: chronic dialysis, dialysis, end-stage renal disease, ESRD, hemodialysis, Sleep Initiation and Maintenance Disorders, depression, Focus Groups, Frustration, quality of life, Anxiety, Emotions, Fatigue, Surveys and Questionnaires, Nausea, Vomiting, renal dialysis, Pain
Introduction
More than 400,000 people with ESKD receive in-center hemodialysis in the United States, and they experience exceptionally high rates of morbidity and poor quality of life relative to individuals with other chronic diseases (1–3). Existing data suggest that individuals on hemodialysis have, on average, 11 symptoms, and this high symptom burden contributes to poor outcomes (4). Patients on dialysis have identified symptom relief as a top research priority (5), and a recent international consensus-based prioritization initiative named fatigue, among other symptoms, as a high priority outcome for clinical trials (6). However, there have been few efforts to understand how and why patients prioritize symptoms. The first essential steps in fostering innovation in symptom relief are identifying the symptoms that patients feel are the most important to address and understanding which treatment strategies are most desired by patients.
Prior research has identified common symptoms among individuals on dialysis, including fatigue, sadness, difficulty falling or staying asleep, itching, muscle cramps, pain, and sexual dysfunction (4,7–9). There is a significant association between higher symptom burden and quality of life impairment (2,4). Thus, it is reasonable to posit that symptom amelioration may lead to meaningful improvement in patient-reported outcomes and/or quality of life. However, there are few drugs or devices that have been approved by the US Food and Drug Administration (FDA) that yield improvement in any patient-reported outcome among individuals on dialysis. Moreover, there has been little research on symptom prioritization and treatment preferences in this population.
Recognizing this knowledge gap, the Kidney Health Initiative (KHI), a public-private partnership between the American Society of Nephrology and the FDA, convened a multidisciplinary workgroup to design and execute a study aimed at prioritizing common hemodialysis symptoms to be targeted for innovation. The workgroup undertook this two-part, sequential, mixed methods study involving focus groups and an online survey. The study objectives were to (1) gain deeper understanding of symptom experiences among individuals on hemodialysis from diverse backgrounds, (2) prioritize the identified physical and mood symptoms for the development of new or improved therapies for symptom relief, and (3) elicit preferences for symptom treatment approaches among individuals receiving in-center maintenance hemodialysis.
Materials and Methods
Overview
We conducted a sequential exploratory mixed methods study that included three focus groups and an online survey (10). In this two-phase design, we performed qualitative data collection via focus groups first and collected quantitative data via a survey second. The qualitative phase was used to gain insight into factors considered by patients when prioritizing symptoms and generate a broad list of symptoms to consider for prioritization. Qualitative focus group findings informed the survey content. The quantitative survey phase was then used to investigate symptom prioritization in a broader patient sample.
We followed the Consolidated Criteria for Reporting Qualitative Health Research for focus group reporting (Supplemental Table 1) (11). All study phases were approved by the American Institutes for Research Institutional Review Board (project number 04222). Focus group participants provided written informed consent, and online survey participants provided electronic consent.
Focus Group Participant Selection, Setting, and Data Collection
Three in-person focus groups were conducted between February and April 2017 in Carrboro, North Carolina; Tucson, Arizona; and Seattle, Washington. Locations were selected to facilitate oversampling of southeastern United States black (Carrboro) and Hispanic (Tucson) individuals, populations with limited inclusion in prior studies (9,12). Participants were recruited from six dialysis facilities in the three geographic locations via posted flyers. Interested individuals contacted study staff via telephone for eligibility assessment. Iterative purposive sampling was used to capture a range of participant characteristics (age, sex, race, and education). The target size for each group was 10 to 12 participants. Individuals were eligible to participate if they (1) were English-speaking adults ages 18–85 years old, (2) had been on in-center hemodialysis for the previous 6 months, (3) had a history of physical and/or mood symptoms that they related to hemodialysis in the past month, and (4) reported no recent participation in a focus group study. Individuals with cognitive deficits were excluded. Participants were remunerated $65.
We drafted a focus group moderator guide on the basis of literature review and research team discussions. Moderator guide topics included symptom experiences (type, frequency, duration, and quality of life and social effects) and individual and group symptom prioritization for the development of new or improved symptom-targeted therapies (Figure 1, Supplemental Table 2). Oral and written exercises were used to spark discussion and ultimately, generate symptom priority lists among participants. All focus groups were led by the same experienced moderator who had no contact with participants before the study. The focus groups were semistructured, lasted 90 minutes each, and took place in private dialysis facility conference rooms with no dialysis facility staff present. Focus groups were audio recorded and professionally transcribed. Two research assistants took field notes. Participant characteristics were self-reported.
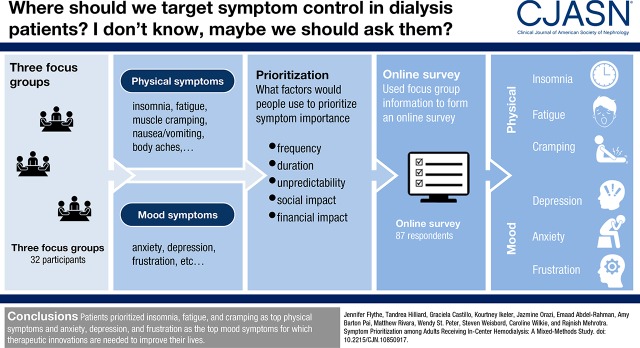
Figure 1.
Standardized exercises were used to elicit symptoms from and prioritize symptoms among focus group participants.
Survey Development, Recruitment, and Data Collection
We developed a draft online English language survey on the basis of focus group findings (top 10 focus group–identified symptoms were included) using Vovici survey software. We conducted virtual cognitive testing interviews using JoinMe online screen-sharing software in May 2017 with patients in Tucson, Arizona; Seattle, Washington; and Newark, Delaware to evaluate target population understanding and usability of the draft survey. Participants were recruited from four dialysis facilities via research team site liaisons. Focus group participants were not eligible for cognitive interview participation. Supplemental Table 3 provides cognitive testing details. Interviewees suggested consolidating the informed consent information; using alternate, more familiar terms (e.g., change “facility” to “clinic”); and adding clarifying words (e.g., add “other than cramps” to “body aches or pains”). We revised the survey on the basis of feedback from interviewees.
The final 28-question online survey was accessible on desktop and mobile applications, and it assessed patients’ experiences with physical (insomnia, muscle cramps, fatigue, nausea or vomiting, and body aches), mood (anxiety, depression, frustration, worry, and confusion), and other self-report symptoms as well as patients’ prioritization of symptoms for therapeutic intervention (Supplemental Table 4). The survey included an electronic consent and was open from May 30 to June 26, 2017.
Survey participants were recruited via informational flyers posted in 35 dialysis facilities located in diverse United States geographic regions, emails to members of the American Association of Kidney Patients (AAKP) and KHI Patient and Family Partnership Council mailing lists, and social media campaigns on Facebook (via the AAKP and patient affinity groups Dialysis Uncensored and I Hate Dialysis). Individuals were eligible to complete the survey if they (1) were at least 18 years of age and living in the United States, (2) currently received in-center hemodialysis, and (3) had experienced physical and/or mood symptoms from hemodialysis in the past month. Eligibility was assessed via questions at the survey start. Individuals not meeting eligibility criteria were not permitted to complete the survey (Supplemental Figure 1). Survey response rates could not be calculated due to the survey’s wide distribution. No incentive was provided.
Data Analyses
Focus group transcriptions were entered into NVivo software for qualitative analysis. The two-person analytic team first developed a list of potential thematic codes on the basis of the moderator guide. The team then reviewed the transcripts to identify early data patterns. They revised the initial code list and systematically coded the data on the basis of the refined coding scheme. The team drew conclusions by identifying and interpreting coding patterns, such as high-frequency codes and coding clusters. The highest priority symptoms were determined on the basis of the number of focus groups in which they were reported, the number of participants reporting them, and the strength of endorsement by participants. Focus group findings informed the symptoms and symptom characteristic and prioritization response options in the survey.
Qualitative data collected via open-ended survey responses were imported into a Microsoft Excel matrix and analyzed for key themes. Survey data were analyzed using descriptive statistics. Analyses were performed using STATA 13.0MP. Focus group and survey results were crossvalidated to identify areas of convergence. Findings were synthesized across methods within major topic areas.
Results
Participant Characteristics
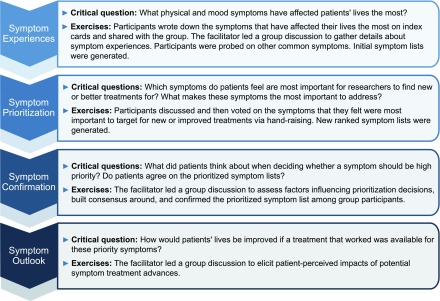
Table 1 displays focus group participant characteristics (three focus groups with a total of 32 participants). Among interested and qualifying individuals, the overall participation rate was 82% (77% for Carrboro, NC; 92% for Tucson, AZ; and 79% for Seattle, WA) (Figure 2). Participants ranged from 25 to 74 years of age (mean 52±14 years old); 14 (44%) were women, 14 (44%) were black, and eight (25%) were Hispanic. By design, Carrboro participants were all black (100%), Tucson participants were predominantly Hispanic (73%), and Seattle participants were predominantly white (64%).
Table 1.
Characteristics of focus group participants
| Characteristica | Participants, n=32, n (%) | ||
|---|---|---|---|
| Tucson, Arizona, n=11 | Carrboro, North Carolina, n=10 | Seattle, Washington, n=11 | |
| Age, yr | |||
| 20–29 | 3 (27) | 1 (10) | 0 (0) |
| 30–39 | 1 (9) | 0 (0) | 1 (9) |
| 40–49 | 1 (9) | 2 (20) | 2 (18) |
| 50–59 | 5 (46) | 3 (30) | 3 (27) |
| 60–69 | 1 (9) | 1 (10) | 4 (36) |
| 70–79 | 0 (0) | 3 (30) | 1 (9) |
| Sex | |||
| Men | 5 (46) | 6 (60) | 7 (64) |
| Women | 6 (55) | 4 (40) | 4 (36) |
| Education level | |||
| Less than high school | 3 (27) | 3 (30) | 3 (27) |
| High school graduate | 7 (64) | 3 (30) | 2 (18) |
| Associates degree or some college | 1 (9) | 3 (30) | 5 (46) |
| College graduate | 0 | 1 (10) | 1 (9) |
| Race/ethnicity | |||
| Black | 1 (9) | 10 (100) | 3 (27) |
| White | 0 (0) | 0 (0) | 7 (64) |
| Hispanic/Latino | 8 (73) | 0 (0) | 0 (0) |
| Asian/Pacific Islander | 1 (9) | 0 (0) | 0 (0) |
| American Indian or Alaska Native | 1 (9) | 0 (0) | 0 (0) |
| Other | 0 (0) | 0 (0) | 1 (9) |
| Time on dialysis | |||
| 6–11 mo | 0 (0) | 1 (10) | 0 (0) |
| 1–5 yr | 7 (64) | 5 (50) | 5 (46) |
| 6–10 yr | 3 (27) | 1 (10) | 3 (27) |
| >10 yr | 1 (9) | 3 (30) | 3 (27) |
| Comorbid conditionsb | |||
| Diabetes | 7 (64) | 6 (60) | 4 (36) |
| Hypertension | 9 (92) | 10 (100) | 6 (55) |
| Cardiovascular disease | 3 (27) | 2 (20) | 2 (18) |
| Congestive heart failure | 2 (18) | 1 (10) | 1 (9) |
| Peripheral vascular disease | 0 (0) | 1 (10) | 6 (55) |
| Neurologic | 0 (0) | 2 (20) | 9 (82) |
| Vision impairment | 0 (0) | 2 (20) | 1 (9) |
Values are presented as n (%). All characteristics were patient reported.
Comorbid conditions are not mutually exclusive.
Figure 2.
Flow chart displaying the selection of focus group participants.
Table 2 displays survey respondent characteristics. Respondents spanned 27 states in the Unites States, and overall, they were similar to the broader United States hemodialysis population in terms of age and sex (1). Of the 87 respondents, 43 (49%) were between 55 and 74 years of age, 47 (54%) were women, 58 (67%) were white, 19 (22%) were black, and five (6%) had less than a high school education. About one half of respondents (51%) rated their overall health as fair or poor.
Table 2.
Characteristics of survey respondents
| Characteristica | Respondents, n=87, n (%) |
|---|---|
| Age, yr | |
| 18–34 | 3 (4) |
| 35–54 | 36 (41) |
| 55–74 | 43 (49) |
| 75 or older | 5 (6) |
| Sex | |
| Men | 40 (46) |
| Women | 47 (54) |
| Education level | |
| Less than high school | 5 (6) |
| High school graduate or GED | 26 (30) |
| Associates degree or some college | 34 (39) |
| College graduate or higher | 22 (25) |
| Employmentb | |
| Employed full time | 8 (9) |
| Employed part time | 9 (10) |
| Unemployed | 13 (15) |
| Homemaker | 2 (2) |
| Full-time student | 1 (1) |
| Retired | 24 (28) |
| Disabled or cannot work because of health reasons | 44 (51) |
| Other | 1 (1) |
| Race/ethnicityb | |
| White | 58 (67) |
| Black | 19 (22) |
| Hispanic, Latino, or Spanish origin | 8 (9) |
| American Indian or Alaska Native | 6 (7) |
| Native Hawaiian or other Pacific Islander | 1 (1) |
| Asian | 1 (1) |
| Some other race, ethnicity, or origin | 2 (2) |
| United States region | |
| Northeast | 31 (36) |
| Midwest | 11 (13) |
| South | 21 (24) |
| West | 24 (28) |
| Length of time receiving in-center hemodialysis | |
| <6 mo | 8 (9) |
| 6–11 mo | 8 (9) |
| 1–5 yr | 39 (45) |
| 6–10 yr | 16 (18) |
| >10 yr | 16 (18) |
| History of kidney transplant | |
| Yes | 16 (18) |
| Overall health rating | |
| Excellent | 1 (1) |
| Very good | 16 (18) |
| Good | 26 (30) |
| Fair | 34 (39) |
| Poor | 10 (12) |
| Comorbid conditionsb | |
| Diabetes or “high sugar” | 29 (33) |
| High BP | 59 (68) |
| Heart problems | 31 (36) |
| Lung problems | 14 (16) |
| Problems with blood flow in legs | 8 (9) |
| Nerve pain from diabetes | 18 (21) |
| Vision problems | 32 (37) |
| Other | 21 (24) |
| Survey helper | |
| Yes | 7 (8) |
| Survey helper actionsb | |
| Read the questions to them | 3 (43) |
| Entered their answers into the online survey | 6 (86) |
| Translated the questions into their language | 0 (0) |
| Answered the questions for them, because I help take care of them, and they cannot answer the questions on their own | 1 (14) |
| Helped in some other way | 0 (0) |
GED, general equivalency diploma.
Values are presented as n (%). All characteristics were patient reported.
Responses are not mutually exclusive.
Focus Group Symptom Experiences
Focus group participants reported experiencing a range of physical and mood symptoms that they associated with hemodialysis (Table 3). Participants reported the physical symptoms of insomnia, fatigue, muscle cramps, and nausea/vomiting and the mood symptoms of anxiety and depression in all three focus groups. Less common but also reported physical symptoms included body aches and joint pain, vascular access–related problems and pain, and blurry vision. Other reported mood symptoms included worry, frustration, and feeling disappointed.
Table 3.
Illustrative quotations of patient perspectives on hemodialysis-related symptoms
| Symptom and Quotationsa |
|---|
| Top focus group–prioritized physical symptoms |
| Insomnia (22 of 32 participants; 67%) |
| “I may sleep for an hour, and then, when I am awake, I am awake. Like the night before last, I was up all night long. And then last night, I slept for about 2 h, and that was it, you know. And I don’t know if that is—because I didn’t do that before. So I don’t know if that is part of the dialysis or what it is, but it is there.” (Tucson participant) |
| Fatigue (20 of 32 participants; 63%) |
| “There’s days where I come in like two to three kilos heavier and sometimes where I go a little bit off track and come in like around four, four and a half … [Fatigue] is just like, imagine working 12 h and then having to go home and do all the house stuff.” (Tucson participant) |
| “I prefer to have showers more often than I do, but sometimes, I’m too fatigued to get up and go down there.” (Seattle participant) |
| Muscle cramping (18 of 32 participants; 56%) |
| “I used to get cramps, like what people call Charlie horses, every once in a blue moon. But like I said, on dialysis, I’m catching cramps where I never thought you could get cramps; in my eyelids and my throat. Say, in my ribs, right here. I can catch ’em anywhere and I never got ’em before, and I used to play sports.” (Seattle participant) |
| “Cramps, leg cramps. That is the most important to me, because I always cry when I get cramps.” (Tucson participant) |
| Nausea or vomiting (14 of 32 participants; 47%) |
| “I was walking to the buses, and I puked in the bushes. People think I’m a drunk.” (Seattle participant) |
| “The nausea thing for me; I have some stomach issues going on which kind of like, that is 24-7, but when I walk into those doors, the nausea kicks up. I think that has to do with my anxiety. So it’s like every run, I would say, so 4 d out of the week for me.” (Tucson participant) |
| Body aches (20 of 32 participants; 44%) |
| “[Body aches] hinder our day to day lifestyle, because we have to live with this pain or discomfort.” (Tucson participant) |
| “I have body aches … especially my arm.” (Tucson participant) |
| Vascular access–related discomfort (11 of 32 participants; 34%) |
| “Well, if you have steal syndrome, like sometimes, if I need to write and I got it, I can’t write. So that is how it affects my daily life.” (Tucson participant) |
| “Feel bad because of my fistula. After they poke you and then they say we got to move it again. Oh, shoot.” (Tucson participant) |
| “I have two fistulas in my hand, and certain movement that I do I feel like [a] cold shot through my arm. If I’m holding a bag or if I’m holding something, if I move my finger a certain way, I can dang near drop the bag if I don’t have this hand ready. And muscles, like the muscles in my arm, get sore after a while.” (Seattle participant) |
| Blurry vision (six of 32 participants; 19%) |
| “I know for me with the blurred vision, I go to a dark room … and just sit there, and I may sit there 2 h. And she comes in, and she’s like that’s depressing. No, it’s not. I’m trying to get my eyes focused, because when my eyes are blurry, I start to get headaches, and then, I just go down from there.” (Carrboro participant) |
| Top focus group–prioritized mood symptoms |
| Anxiety (16 of 32 participants; 50%) |
| “Anxiety—I am always anxious.” (Tucson participant) |
| “I have anxiety with the needle. I mean, I’m an 18-yr veteran, and every day is still a new day; it’s just like the first day with that needle. I can work all day long and not wear myself out, but I’ll wear myself out just when they put the needle … and it doesn’t even hurt. I mean, sometimes it does, but they numb it all up and stuff, but I still go through the changes as if I was going to get kicked upside the head.” (Seattle participant) |
| Depressed mood (14 of 32 participants; 44%) |
| “[Depression] happens all the time; I go home and start thinking about what I have to go through. You see the people [patients on dialysis] and then find out that they died, and it is just hard. It is depressing to be dependent on a machine and have to go through this over and over again. I move past it, but it happens all the time.” (Tucson participant) |
| “People get tired and worry; then they get depressed. They stop dialyzing and die. That needs to be looked at real hard.” (Seattle participant) |
| Frustration (nine of 32 participants; 28%) |
| “I mean the cramps, being tired, blurred vision—that happens because of the actual treatment. So that happens instantly. With me, it does. I mean the other stuff, like the frustration and what not, that comes after dialysis and having to deal with the technician. That’s something totally different.” (Carrboro participant) |
| Irritability (nine of 32 participants; 28%) |
| “Conversating [sic] with everybody, you really don’t want to. You don’t want to be around anybody. You just want to be by yourself.” (Carrboro participant) |
| “Sometimes you get in a bad mood—so you know—don’t talk to me.” (Tucson participant) |
| “Sometimes noise, loud noises is irritating. It irritates you real bad.” (Carrboro participant) |
| Worry (six of 32 participants; 19%) |
| “[Worry] all the time.” (Carrboro participant) |
| “Well, people get to worrying, and they get tired, and they get depressed, and then they quit dialyzing and die. I’ve seen a number of them do that. So that needs to be looked at real hard.” (Seattle participant) |
Quotations are from focus group participants.
Focus Group Symptom Prioritization
Physical and mood symptom prioritization exercises were performed separately. The most commonly experienced symptoms were also those that participants prioritized as most important to find new or improved treatments for (i.e., physical symptoms: insomnia, fatigue, and muscle cramps; mood symptoms: anxiety and depression). In prioritization exercises, participants indicated that symptom frequency, duration, unpredictability, social effect, and financial effect factored most heavily into symptom prioritization decisions (Table 4). Symptom prioritization rationale was similar across all three focus groups. Overall, participants felt that their symptoms were bothersome primarily because they interfered with daily activities and quality of life. One Carrboro participant described symptom-related social isolation, saying that “sometimes you can’t visit your family or people. You feel sick or tired.” Others reported frustration from not being able to work due to symptom burden. One Seattle participant said, “Sometimes I think I am a burden to my family because I cannot work [due to my symptoms] … Sometimes, I get real depressed.”
Table 4.
Illustrative quotations of patient perspectives on symptom prioritization reasoning
| Reason and Quotationsa |
|---|
| Frequency |
| “Because it’s something that happens on a regular basis.” (Carrboro participant) |
| “My doctor asked me all the time, when is it the time when you feel more light-headed than others? I don’t know, because it just comes. I can leave the room and all of a sudden feel light-headed. I get home, feel fine, and feel bad at the Kidney Center. It comes and goes. Like, you don’t throw up every day, but you do throw up. Just like I don’t feel light-headed every day, but it does come, you know what I’m saying? So like these symptoms come and they go.” (Seattle participant) |
| Duration |
| “[Symptoms last] until you come back to dialysis.” (Carrboro participant) |
| “Like I said, it varies, but it could last a couple of hours, or it can last the whole day, I have noticed. But that for me, it depends on how much they take off and how my run goes that day.” (Tucson participant) |
| Unpredictability |
| “I come to find I don’t make plans, because I don’t know how I’m gonna feel.” (participant in Seattle) |
| “I can’t keep plans with my mom, I can’t keep plans with nobody … That is true, I don’t want to be around anybody; I don’t want to be out.” (Tucson participant) |
| Social effect |
| “Isolation, I was always a very social person. And because of the weakness and all of the physical symptoms, I can’t get out, you know. And then I had to retire, so I am home. And I have very little contact with the outside world and so it is—it is depressing, that’s where my depression comes from.” (Tucson participant) |
| “I don’t want to do anything. I don’t want to eat. I don’t want to sleep. Just leave me alone.” (Carrboro participant) |
| Financial effect |
| “Were these symptoms not issues, I’d have an opportunity to make money to take care of myself.” (Seattle participant) |
| “I would go back to work. First thing I would do, back to school and work.” (Tucson participant) |
Quotations are from focus group participants.
Focus Group Perspectives on Symptom-Directed Therapies
Overall, participants indicated that their quality of life would improve significantly if they had meaningful improvement in their top physical and mood symptoms. Many participants recognized the interconnection between physical and mood symptoms. For example, one participant noted that his anxiety seemed to cause nausea. Several participants suggested that addressing physical symptoms might improve mood symptoms, such as depression and anxiety.
Participants discussed a variety of treatments used to address their symptoms. Treatments for physical symptoms included medications, light exercise, consuming certain foods, and smoking marijuana. However, participants noted that none of these strategies provided complete symptom relief. In two of the focus groups, participants expressed a desire for peer support programs, indicating that such programs would give them opportunities to share experiences and challenges with others facing similar issues. They indicated that such peer support might help with mood symptom management. Some participants expressed frustration with taking multiple medications and were skeptical that medication was the best strategy for symptom management. One Tucson participant said, “They only want to give you pills. And, yeah, sometimes that medicine makes you sicker.”
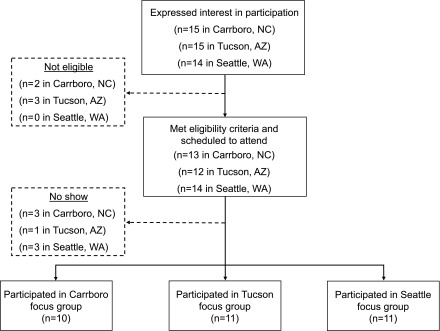
Survey Symptom Experiences and Prioritization
Figure 3 and Supplemental Table 5 display the survey results. Fatigue (94%), muscle cramps (79%), and body aches or pain (76%) were the most commonly experienced physical symptoms. Survey respondents also reported physical symptoms not identified in focus groups, such as diarrhea, dry skin, pruritus, twitching, dizziness, burning eyes, headache, rash, and decline in libido. Participants identified fatigue, muscle cramps, and insomnia as the most important physical symptoms for which to find better treatments. Feeling sad or depressed (66%), worried (64%), and frustrated or angry (63%) were the most commonly experienced mood symptoms. Participants identified feeling sad or depressed, frustrated or angry, and anxious or nervous as the most important mood symptoms for which to find better treatments. Symptom frequency, unpredictability, and life effects, such as the ability to do things that they want to do with friends or family, drove symptom prioritization decision making.
Figure 3.
Survey responses captured physical and mood symptoms experienced by patients and the most important physical and mood symptoms for which to find better treatments. (A) displays physical symptoms experienced in the past month. (B) displays the most important physical symptoms for which to find better treatments. (C) displays mood symptoms experienced in the past month. (D) displays the most important mood symptoms for which to find better treatments.
Overall Symptom Prioritization for Therapeutic Interventions
Considering both focus group and survey results, insomnia, fatigue, and muscle cramps were prioritized as the top physical symptoms, and anxiety, depression, and frustration were prioritized as the top mood symptoms (Figure 4). In general, participants were open to new medications for their physical symptoms but expressed some concern about pill burden. Many expressed interest in nonpharmaceutical interventions, such as meditation, massage, and dialysis facility–based strategies, including more flexible scheduling, better objective measures of dry weight and symptom monitoring, and improved patient-staff relations. The latter was felt to be important for fostering open communication about symptoms. In regards to scheduling and symptoms, one respondent noted, “Scheduling of dialysis in the late afternoon rather than early morning allows me to be more engaged.” Another respondent called for “better dialysis machines that are more in tune with the patients” to help prevent symptoms.
Figure 4.
Qualitative and quantitative data were synthesized to develop a final list of top-prioritized physical and mood symptoms. Focus group and survey participants identified a range of physical and mood symptoms, often recognizing a connection between physical and mood symptoms. After considering symptom duration, frequency, unpredictability, and social and financial effects, the participants prioritized the physical symptoms of insomnia, fatigue, and cramps and mood symptoms of anxiety, depression, and frustration as the most important symptoms to address when developing new or improved symptom management therapies.
Discussion
To our knowledge, this is the first published study evaluating symptom prioritization for the development of new or improved therapies for symptom relief among adults from diverse backgrounds receiving in-center hemodialysis. We found that patients prioritized the physical symptoms of insomnia, fatigue, and muscle cramps and the mood symptoms of anxiety, depression, and frustration. Symptom characteristics, including frequency, duration, unpredictability, social effect, and financial effect, drove prioritization decision making. Overall, participants felt that it was important to identify better therapies for both physical and mood symptoms rather than one symptom type over the other. However, many acknowledged a link between their physical and mood symptoms, suggesting that amelioration of the most troublesome body symptoms could lead to mood symptom improvements.
The nephrology community has shown increasing appreciation for the importance of studying outcomes that are meaningful and relevant to patients and other clinical stakeholders. The international Standardized Outcomes in Nephrology—Hemodialysis initiative recently reported a multistakeholder, consensus-based, prioritized list of outcome domains for research involving individuals on hemodialysis (6). Fatigue was one of the highest-prioritized outcomes, and other symptoms, such as pain, sleep, depression, and anxiety, ranked high, particularly among patients (6). Manns et al. (5) evaluated research uncertainties among Canadian patients, caregivers, and health professionals and reported that symptom management, specifically prevention of itching, fatigue, nausea, cramping, restless legs, and depression, was a top stakeholder-identified research uncertainty. Our findings build on these prior outcome prioritization studies as well as work showing substantial symptom burdens among individuals receiving maintenance hemodialysis. Prior studies have found that more than one half of individuals on dialysis report pain, cramps, fatigue, sexual dysfunction, and sleep disturbance (8,9,13). Increased symptom burdens are highly correlated with impaired quality of life and depression (2,4), and some symptom clusters associate with higher mortality risk (14). However, prior studies suggest that nephrology providers may not be aware of the symptoms that their patients on dialysis have, including symptoms that patients describe as severe (9). Consequently, many symptoms remain undertreated (15).
Given the documented associations between symptom burden and outcomes, there may be a substantial opportunity to improve quality of life and other outcomes through better symptom prevention and management among patients on hemodialysis. However, the existing evidence supporting symptom management strategies is poor. In fact, there have been no trials in which relief from any of the highly patient-prioritized symptoms of cramping, fatigue, or anxiety was the primary outcome measure. Similarly, there have been no pharmacotherapy trials and only two cognitive behavioral therapy trials focused on insomnia among individuals on dialysis (16,17). There has been somewhat greater attention paid to depression among patients on dialysis; however, a trial comparing sertraline with placebo suffered from poor recruitment, and results were not significantly different between groups (18). A trial comparing sertraline with cognitive behavioral therapy is ongoing (19). Given this paucity of data, it is not surprising that there have been so few drugs or devices approved by the FDA that improve patient-reported outcomes for patients on dialysis. Furthermore, there are no consensus clinical guideline recommendations on the optimal approach to symptom management in this population.
There is a critical need to foster innovation in symptom relief in the hemodialysis population and focus these innovations on therapeutic approaches that are appealing to patients. Our study findings highlight several potential paths forward in the effort to improve the symptom experience of patients on hemodialysis. Innovation in symptom-directed pharmacotherapy, including new drug development as well as testing of existing drugs approved for use in the general population in the dialysis population, should be undertaken. Additionally, innovation in bioengineering may improve symptom management through the development of new therapeutic devices and/or improvement on existing dialysis technologies. Examples of potential technical advances that may prevent or reduce symptoms include more accurate objective volume assessment tools, biofeedback-based ultrafiltration, dialyzers with improved middle molecule clearance, individualized dialysate profiling, and others. Additional evaluation of the roles of individual therapy and peer support in both physical symptom and mood symptom management is warranted. Many participants noted interest in peer support activities, such as symptom coping strategies. Finally, participants voiced desire for greater dialogue with their providers around symptoms, noting that such acknowledgment and engagement might improve the symptom experience. Given the substantial burden and quality of life effect of symptoms among individuals receiving hemodialysis, simultaneous pursuit of all potential paths to symptom relief is warranted.
Our findings must be considered in the context of study limitations. First, we evaluated symptom prioritization among patients on in-center hemodialysis. Findings should not be extrapolated to individuals receiving peritoneal dialysis or home hemodialysis. Study of symptom prioritization among these populations is needed. Second, there may be limits to the generalizability of our findings. Our sample size was moderate, and our findings may not generalize to all patients on hemodialysis. Our goal was to build on existing knowledge by selecting focus group locations that facilitated sampling from populations (blacks and Hispanics) and geographic areas (the South and the Northwest) under-represented in prior studies. Survey respondents resided in 27 states in the United States, suggesting reasonable geographic reach for the survey. However, over 85% of survey participants were white or black, potentially limiting generalizability of findings to other races or ethnic backgrounds. Cultural differences in symptom experiences have been reported among individuals on hemodialysis and in other populations (12,20,21). Exclusion of non–English-speaking individuals and individuals with cognitive deficits prevents generalizability to those excluded populations. Related to this point, online survey administration may have limited participation from individuals without internet access or those with mental or physical disabilities. Therefore, the generalizability of our findings must be interpreted with caution. Additional study of symptom prioritization in larger and more diverse populations is warranted. However, focus group and survey-elicited symptoms mirrored symptoms identified in other studies (4,8,22), providing some reassurance about validity. Third, our survey distribution approach prohibited calculation of a survey response rate. The estimated response rate was low as evidenced by the modest number of completed surveys, despite broad distribution. Symptom prioritization among survey responders versus nonresponders may differ, and we are unable to account for this potential bias. Fourth, our study was designed to elicit symptom perspectives from diverse individuals and was not designed to quantify differences across subpopulations.
In conclusion, our study provides a deeper understanding of the symptoms experienced by diverse individuals receiving hemodialysis therapy and insight into patient prioritization of physical and mood symptoms for the development of new or improved therapies for symptom relief. Participating patients prioritized the physical symptoms of insomnia, fatigue, and muscle cramping and the mood symptoms of depression, anxiety, and frustration as the most important symptoms on which to focus research efforts aimed at developing new symptom management strategies. These findings provide guidance and direction as we seek to foster innovation in symptom management among individuals on hemodialysis.
Disclosures
J.E.F. has received speaking honoraria from Dialysis Clinic, Incorporated; American Renal Associates; the American Society of Nephrology; the National Kidney Foundation; Baxter; and multiple universities. J.E.F. has received research funding for studies unrelated to this project from the Renal Research Institute, a subsidiary of Fresenius Medical Care, North America. A.B.P. has current funding from the Food and Drug Administration and the Renal Research Institute. A.B.P. has served as a consultant for Pfizer Inc., AMAG Pharmaceuticals, and Rockwell Medical. W.L.S.P. has received speaking honoraria from the American Society of Nephrology, the National Kidney Foundation, and the American Nephrology Nurses Association and has received research funding in the past 2 years for studies unrelated to this project from the University of Minnesota College and AstraZeneca.
Supplementary Material
Acknowledgments
The authors would like to thank all study participants for sharing their experiences and perspectives about symptoms related to in-center hemodialysis. The authors also thank the following research liaisons who assisted with focus group and survey coordination: Manisha Jhamb (University of Pittsburgh), Klemens Meyer (Tufts University), and Bijin Thajudeen (University of Arizona). The authors acknowledge Dialysis Clinic, Incorporated (Karen Majchrzak and Klemens Meyer) and the American Association for Kidney Patients (Paul Conway) for their support of the study survey.
This work was supported by the Kidney Health Initiative (KHI), a public-private partnership between the American Society of Nephrology, the US Food and Drug Administration, and >75 member organizations and companies to enhance patient safety and foster innovation in kidney disease. KHI funds were used to defray costs incurred during the conduct of the project, including project management support, which was expertly provided by American Society of Nephrology staff members, Melissa West, Ryan Murray, and Elle Silverman. There was no honorarium or other financial support provided to the KHI workgroup members. J.E.F. is supported by National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health grant K23 DK109401. M.B.R. is supported by grant KL2 TR000421 from the National Center for Advancing Translational Sciences.
The authors of this paper had final review authority and are fully responsible for its content. The KHI makes every effort to avoid actual, potential, or perceived conflicts of interest that may arise as a result of industry relationships or personal interests among the members of the workgroup. More information on the KHI, the workgroup, or the conflict of interest policy can be found at www.kidneyhealthinitiative.org.
Because Rajnish Mehrotra is the Editor-in-Chief (EIC) of the Clinical Journal of the American Society of Nephrology, he was not involved in the peer review process for this manuscript. Another editor oversaw the peer review and decision-making process for this manuscript. Ian de Boer, a Deputy Editor of CJASN, is at the same institution as some of the authors, including the EIC and therefore was also not involved in the peer review process for this manuscript.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.10850917/-/DCSupplemental.
References
- 1.Saran R, Robinson B, Abbott KC, Agodoa LY, Albertus P, Ayanian J, Balkrishnan R, Bragg-Gresham J, Cao J, Chen JL, Cope E, Dharmarajan S, Dietrich X, Eckard A, Eggers PW, Gaber C, Gillen D, Gipson D, Gu H, Hailpern SM, Hall YN, Han Y, He K, Hebert H, Helmuth M, Herman W, Heung M, Hutton D, Jacobsen SJ, Ji N, Jin Y, Kalantar-Zadeh K, Kapke A, Katz R, Kovesdy CP, Kurtz V, Lavalee D, Li Y, Lu Y, McCullough K, Molnar MZ, Montez-Rath M, Morgenstern H, Mu Q, Mukhopadhyay P, Nallamothu B, Nguyen DV, Norris KC, O'Hare AM, Obi Y, Pearson J, Pisoni R, Plattner B, Port FK, Potukuchi P, Rao P, Ratkowiak K, Ravel V, Ray D, Rhee CM, Schaubel DE, Selewski DT, Shaw S, Shi J, Shieu M, Sim JJ, Song P, Soohoo M, Steffick D, Streja E, Tamura MK, Tentori F, Tilea A, Tong L, Turf M, Wang D, Wang M, Woodside K, Wyncott A, Xin X, Zang W, Zepel L, Zhang S, Zho H, Hirth RA, Shahinian V: US renal data system 2016 annual data report: Epidemiology of kidney disease in the United States. Am J Kidney Dis 69[Suppl 1]: A7–A8, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merkus MP, Jager KJ, Dekker FW, de Haan RJ, Boeschoten EW, Krediet RT: Physical symptoms and quality of life in patients on chronic dialysis: Results of The Netherlands Cooperative Study on Adequacy of Dialysis (NECOSAD). Nephrol Dial Transplant 14: 1163–1170, 1999 [DOI] [PubMed] [Google Scholar]
- 3.Valderrábano F, Jofre R, López-Gómez JM: Quality of life in end-stage renal disease patients. Am J Kidney Dis 38: 443–464, 2001 [DOI] [PubMed] [Google Scholar]
- 4.Abdel-Kader K, Unruh ML, Weisbord SD: Symptom burden, depression, and quality of life in chronic and end-stage kidney disease. Clin J Am Soc Nephrol 4: 1057–1064, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manns B, Hemmelgarn B, Lillie E, Dip SC, Cyr A, Gladish M, Large C, Silverman H, Toth B, Wolfs W, Laupacis A: Setting research priorities for patients on or nearing dialysis. Clin J Am Soc Nephrol 9: 1813–1821, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Evangelidis N, Tong A, Manns B, Hemmelgarn B, Wheeler DC, Tugwell P, Crowe S, Harris T, Van Biesen W, Winkelmayer WC, Sautenet B, O'Donoghue D, Tam-Tham H, Youssouf S, Mandayam S, Ju A, Hawley C, Pollock C, Harris DC, Johnson DW, Rifkin DE, Tentori F, Agar J, Polkinghorne KR, Gallagher M, Kerr PG, McDonald SP, Howard K, Howell M, Craig JC; Standardized Outcomes in Nephrology–Hemodialysis (SONG-HD) Initiative : Developing a set of core outcomes for trials in hemodialysis: An International Delphi Survey. Am J Kidney Dis 70: 464–475, 2017 [DOI] [PubMed] [Google Scholar]
- 7.Weisbord SD, Fried LF, Arnold RM, Rotondi AJ, Fine MJ, Levenson DJ, Switzer GE: Development of a symptom assessment instrument for chronic hemodialysis patients: The Dialysis Symptom Index. J Pain Symptom Manage 27: 226–240, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Weisbord SD, Fried LF, Arnold RM, Fine MJ, Levenson DJ, Peterson RA, Switzer GE: Prevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patients. J Am Soc Nephrol 16: 2487–2494, 2005 [DOI] [PubMed] [Google Scholar]
- 9.Weisbord SD, Fried LF, Mor MK, Resnick AL, Unruh ML, Palevsky PM, Levenson DJ, Cooksey SH, Fine MJ, Kimmel PL, Arnold RM: Renal provider recognition of symptoms in patients on maintenance hemodialysis. Clin J Am Soc Nephrol 2: 960–967, 2007 [DOI] [PubMed] [Google Scholar]
- 10.Creswell JW: Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 4th Ed., Thousand Oaks, CA, Sage Publications, 2013 [Google Scholar]
- 11.Tong A, Sainsbury P, Craig J: Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care 19: 349–357, 2007 [DOI] [PubMed] [Google Scholar]
- 12.Weisbord SD, Bossola M, Fried LF, Giungi S, Tazza L, Palevsky PM, Arnold RM, Luciani G, Kimmel PL: Cultural comparison of symptoms in patients on maintenance hemodialysis. Hemodial Int 12: 434–440, 2008 [DOI] [PubMed] [Google Scholar]
- 13.Rosas SE, Joffe M, Franklin E, Strom BL, Kotzker W, Brensinger C, Grossman E, Glasser D, Feldman HI: Prevalence and determinants of erectile dysfunction in hemodialysis patients. Kidney Int 59: 2259–2266, 2001 [DOI] [PubMed] [Google Scholar]
- 14.Amro A, Waldum B, von der Lippe N, Brekke FB, Dammen T, Miaskowski C, Os I: Symptom clusters predict mortality among dialysis patients in Norway: A prospective observational cohort study. J Pain Symptom Manage 49: 27–35, 2015 [DOI] [PubMed] [Google Scholar]
- 15.Claxton RN, Blackhall L, Weisbord SD, Holley JL: Undertreatment of symptoms in patients on maintenance hemodialysis. J Pain Symptom Manage 39: 211–218, 2010 [DOI] [PubMed] [Google Scholar]
- 16.Hou Y, Hu P, Liang Y, Mo Z: Effects of cognitive behavioral therapy on insomnia of maintenance hemodialysis patients. Cell Biochem Biophys 69: 531–537, 2014 [DOI] [PubMed] [Google Scholar]
- 17.Chen HY, Chiang CK, Wang HH, Hung KY, Lee YJ, Peng YS, Wu KD, Tsai TJ: Cognitive-behavioral therapy for sleep disturbance in patients undergoing peritoneal dialysis: A pilot randomized controlled trial. Am J Kidney Dis 52: 314–323, 2008 [DOI] [PubMed] [Google Scholar]
- 18.Friedli K, Guirguis A, Almond M, Day C, Chilcot J, Da Silva-Gane M, Davenport A, Fineberg NA, Spencer B, Wellsted D, Farrington K: Sertraline versus placebo in patients with major depressive disorder undergoing hemodialysis: A randomized, controlled feasibility trial. Clin J Am Soc Nephrol 12: 280–286, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hedayati SS, Daniel DM, Cohen S, Comstock B, Cukor D, Diaz-Linhart Y, Dember LM, Dubovsky A, Greene T, Grote N, Heagerty P, Katon W, Kimmel PL, Kutner N, Linke L, Quinn D, Rue T, Trivedi MH, Unruh M, Weisbord S, Young BA, Mehrotra R: Rationale and design of A Trial of Sertraline vs. Cognitive Behavioral Therapy for End-stage Renal Disease Patients with Depression (ASCEND). Contemp Clin Trials 47: 1–11, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koffman J, Morgan M, Edmonds P, Speck P, Higginson I: Cultural meanings of pain: A qualitative study of Black Caribbean and White British patients with advanced cancer. Palliat Med 22: 350–359, 2008 [DOI] [PubMed] [Google Scholar]
- 21.Mesquita B, Walker R: Cultural differences in emotions: A context for interpreting emotional experiences. Behav Res Ther 41: 777–793, 2003 [DOI] [PubMed] [Google Scholar]
- 22.Cox KJ, Parshall MB, Hernandez SHA, Parvez SZ, Unruh ML: Symptoms among patients receiving in-center hemodialysis: A qualitative study. Hemodial Int 21: 524–533, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.