Abstract
Objectives
Anxiety is an increasingly recognised predictor of cognitive deterioration in older adults and in those with mild cognitive impairment. Often believed to be a prodromal feature of neurodegenerative disease, anxiety may also be an independent risk factor for dementia, operationally defined here as preceding dementia diagnosis by ≥10 years.
Design
A systematic review of the literature on anxiety diagnosis and long-term risk for dementia was performed following published guidelines.
Setting and participants
Medline, PsycINFO and Embase were searched for peer-reviewed journals until 8 March 2017. Publications reporting HR/OR for all-cause dementia based on clinical criteria from prospective cohort or case–control studies were selected. Included studies measured clinically significant anxiety in isolation or after controlling for symptoms of depression, and reported a mean interval between anxiety assessment and dementia diagnosis of at least 10 years. Methodological quality assessments were performed using the Newcastle-Ottawa Scale.
Outcome measure
HR/OR for all-cause dementia.
Results
Searches yielded 3510 articles, of which 4 (0.02%) were eligible. The studies had a combined sample size of 29 819, and all studies found a positive association between clinically significant anxiety and future dementia. Due to the heterogeneity between studies, a meta-analysis was not conducted.
Conclusions
Clinically significant anxiety in midlife was associated with an increased risk of dementia over an interval of at least 10 years. These findings indicate that anxiety may be a risk factor for late-life dementia, excluding anxiety that is related to prodromal cognitive decline. With increasing focus on identifying modifiable risk factors for dementia, more high-quality prospective studies are required to clarify whether clinical anxiety is a risk factor for dementia, separate from a prodromal symptom.
Keywords: dementia, anxiety disorders, epidemiology
Strengths and limitations of this study.
This systematic review used a rigorous methodology, with broad search terms and precisely predefined inclusion and exclusion criteria to investigate a life course association between a potentially modifiable risk factor, anxiety and dementia, while excluding anxiety related to preclinical dementia.
Strict exclusion criteria were used to remove studies that did not either discuss anxiety diagnosis alone or control for depression, to account for high levels of anxiety–depression comorbidity.
Study quality was formally investigated using the Newcastle-Ottawa Scale.
The review was limited by the lack of assessment of cognition at baseline in retrospective studies; however, the length of look back minimises the likelihood of cognitive impairment at baseline.
The small number and heterogeneity of study designs rendered a meta-analysis inappropriate; therefore, formal statistical analyses could not be performed.
Introduction
Dementia, and more specifically Alzheimer’s disease (AD), is a progressive neurocognitive disease. In the absence of any disease-modifying treatments, there is increasing focus on primary prevention to reduce the risk of its development and on early intervention to potentially slow progression. A better understanding of risk factors for dementia is therefore vital for improving therapeutic interventions. Alongside a number of well-described cardiovascular risk factors,1 increasing evidence has highlighted the association between psychiatric illnesses and the development of late-onset dementia.2 Further work is needed to understand whether these psychiatric symptoms and illnesses represent prodromal symptoms or act as independent risk factors.
Depression has been consistently related to the development of dementia.3 Three meta-analyses have reported that a diagnosis of depression is associated with up to a twofold increase in risk.3–5 Ownby and colleagues further report that a longer interval between diagnosis of depression and diagnosis of dementia is significantly associated with an increased OR of developing dementia.3 This substantiates interpretations of depression as a risk factor for developing dementia, whereas a stronger association over shorter intervals would have been more indicative of prodromal symptoms. Conversely, a recent study found no association between dementia and depressive symptoms experienced more than 22 years before dementia diagnosis; however, a positive association between dementia and depressive symptoms experienced on average 11 years prior to diagnosis of dementia was reported.6
Although anxiety is a prevalent psychiatric disorder7 and commonly co-occurs with depression, the impact of anxiety on risk for cognitive decline and dementia has been far less studied. Anxiety symptoms are commonly experienced in the years preceding a dementia diagnosis8 and have been associated with cognitive decline and the progression from mild cognitive impairment (MCI) to AD.9–11 A recent review reported that anxiety and neuropsychiatric symptoms not reaching clinically diagnostic levels were associated with increased risk of dementia.12 The authors indicated that anxiety was likely a prodromal symptom of dementia in these community samples. This may well have been the case, particularly given the relatively short intervals between assessment of anxiety symptoms and assessment of dementia; however, this does not preclude anxiety also being a risk factor.
The association between anxiety symptoms (independent of the dementia prodrome) and dementia in later life could more easily be investigated with longer intervals between anxiety assessment and dementia diagnosis, as the studies that have investigated this association within a 5-year to 10-year interval have reported variable results.13 14 The average length of prodromal preclinical cognitive decline has been proposed to be between 5 and 6 years,15 and individuals diagnosed with MCI may progress to AD within 5 years.16 Therefore, examining studies with at least a 10-year interval between anxiety assessment and dementia diagnosis would increase likelihood that anxiety is independent from the dementia prodrome.
It is possible that anxiety symptoms meeting diagnostic threshold will have a stronger association with dementia than general symptoms because this has been shown with depression.4 To date, there has been no systematic review to investigate the association between clinically significant anxiety and dementia. The aim of this study was therefore to review the literature examining the association between clinically significant levels of anxiety and dementia risk over a longer time scale (≥10 years).
Methods
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses and Centre for Reviews and Dissemination guidance for undertaking reviews in healthcare.17
Search strategy
A systematic literature search of Medline, PsycINFO and Embase databases was conducted in articles published from inception to 8 March 2017 to identify articles reporting analyses of the association between anxiety (as defined by clinical diagnosis or self-report scales with a clinically significant threshold) and dementia or MCI incidence. Search terms used consisted of: (dement* OR Alzheimer* OR “mild cognitive impairment” OR MCI) AND (anx* OR “generalised anxiety disorder” OR GAD) AND (risk* OR odds), as presented in online supplementary table ST1. We aimed to identify articles discussing (1) diagnosis of any type of dementia, (2) anxiety diagnosis and (3) risk of dementia. The search was restricted to human studies and those published in English. Reference lists were searched for additional relevant articles. Searches were conducted by a single reviewer (AG). An independent review of all screened articles was conducted by a second reviewer (MS). Any disagreement was resolved by consensus with a third reviewer (NM), which occurred in two cases.
bmjopen-2017-019399supp001.pdf (77.3KB, pdf)
Selection criteria and article screening
Inclusion criteria were (1) a diagnosis of anxiety or an assessment of anxiety symptoms meeting diagnostic criteria using a standardised assessment tool, excluding populations with post-traumatic stress disorder or obsessive–compulsive disorder; (2) population-based studies where anxiety is assessed at least—on average—10 years preceding final clinical assessment for dementia in line with previous meta-analyses on depression using intervals of at least 10 years3; (3) a diagnosis of dementia using validated criteria (eg, Diagnostic Statistical Manual III–IV (DSM III–IV), International Classification of Diseases, 10th Revision (ICD-10)) and (4) late-onset dementia diagnoses (aged ≥65 years). Eligible articles were identified by performing an initial screen of titles and abstracts, followed by a full article review of those that passed screening. All retrospective and prospective studies that met these criteria were selected.
Data extraction
Outcome measures related to anxiety and dementia diagnosis were independently extracted by two authors (AG, MS). Disagreements were resolved through discussion. Study design, sample characteristics (including educational level and age), follow-up length, dropout rate, anxiety (including measure and baseline score where appropriate), criteria for assessing dementia and measurements of depression as a confounder (including measure and baseline score) were recorded. In cases of insufficient data, authors were contacted by email.
Study quality
Two authors (AG, MS) independently assessed study quality and risk of bias using the Newcastle-Ottawa Scale, which contains separate quality assessment instruments for case–control and cohort studies.
Results
Literature search
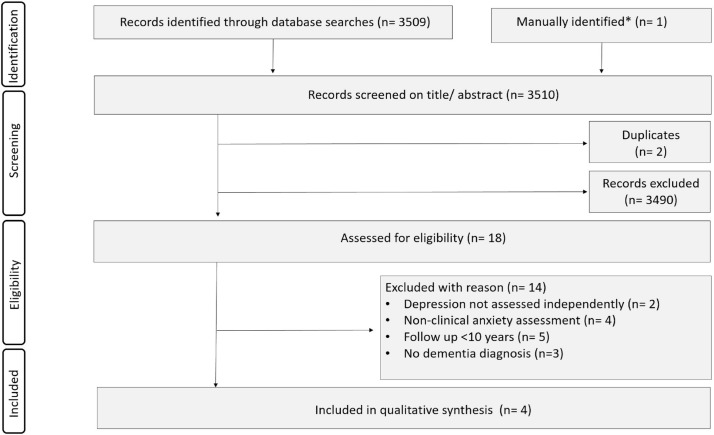
The literature search detected 3509 citations, of which two were duplicates. One further paper was identified manually during reference screening. After screening titles and abstracts, 18 full-text articles were assessed for eligibility. Fourteen articles were excluded based on criteria described earlier (figure 1), and four studies were included in the final review.18–21
Figure 1.
Flow chart of the search and study selection process. *Manually identified from Petkus et al.21
Study characteristics
Characteristics of the four selected studies are shown in table 1. Clinically significant anxiety was documented based on clinical diagnosis using ICD-10 criteria (n=2), the State Trait Anxiety Inventory (STAI, n=1) and a subscale of the State Trait Personality Inventory (STPI, n=1).
Table 1.
Study characteristics
| Study type and setting, location | Follow-up/look-back period, years (SD) | Mean age, years (SD) | Female, n (%) | Education level, n (%) | Dropout rate/response rate percentage | Baseline cognition measure | Anxiety measure; cut-off | Baseline anxiety, n (%) | Controls for depression; baseline depression measure | Dementia diagnosis; criteria (no of cases); OR/HR (95% CI) | |
| Boot et al19 (N=441) | Population-based matched case-controlled, Mayo Clinic Rochester, Minnesota, USA | Lifelong diagnoses documented by medical record | 72.5 (7.3) —DLB cases age at diagnosis | 103 (23.1) | >9 years education; (95) | NR | NR | Clinical diagnosis, present in medical history section of medical record | 23 (27) cases; 14 (5) controls |
Yes; clinical diagnosis from medical history record | DLB diagnosis by behavioural neurologist; published criteria by McKeith et al25 (n=147); OR 7.4 (3.5 to 16) |
| Gallacher et al20 (N=1160) |
Prospective, community-based cohort; Caerphilly, Wales, UK | Mean follow-up period; 17.3 (1.3) | 56.1 (4.4)—mean age at inclusion | 0 | No qualifications; 601 (55) | 20 | NR; dementia unlikely at inclusion (mean age <60 years) | STAI; score of ≥35 | 585 (50) | Yes; GHQ-30 | Dementia diagnosis; DSM-IV or medical records (n=90); OR 1.62 (0.59 to 4.41) |
| Petkus et al21 (N=1082) | Prospective, community based cohort; Swedish twins drawn from Swedish Twin Registry, Sweden | Follow-up period; 28 (0) | 60.86 (11.15)—mean age at inclusion | 612 (56.6) | Beyond elementary education; 423 (39) |
29.8 | MMSE | State anxiety subscale of STPI; STPI>1 SD Q1-Q4 (assessments over four time points) |
403 (37) | Yes; OARS Depression Subscale, CES-D | Dementia diagnosis; DSM-III or DMS-IV (n=172); HR 1.48 (1.01 to 2.18) |
| Zilkens et al18 (N=27 136) |
Population-based matched case-controlled, Western Australia | Mean look-back period; cases 20.4 (10.4), controls 20.0 (10.3) | 78.7 (4.7)—mean age at final time point | 15 359 (56.6) | NR | 6.17 (excluded individuals) |
NR | Clinical diagnosis using ICD-10 AM (Australian Modification) codes documented in health records; meeting diagnostic threshold | 379 (2.8) cases | Yes; clinical diagnosis by GP | Dementia diagnosis; ICD-10 (n=13 568); OR 1.61 (1.28 to 2.02) (>10 years look-back period) |
CES-D, Centre of Epidemiological Studies Depression Subscale; DLB, Dementia with Lewy bodies; DSM III/IV, Diagnostic and Statistical Manual of Mental Disorders III/IV; GHQ-30, 30-item General Health Questionnaire; GP, general practitioner; ICD-10, International Classification of Diseases, 10th Revision; MMSE, Mini-Mental State Examination; NR, not recorded; OARS, older American resources and services; STAI, State Trait Anxiety Inventory; STPI, State Trait Personality Inventory.
Gallacher et al20 measured anxiety using the STAI, which has a range from 20 to 8022 and is a validated measure for assessing anxiety symptoms. A clinically significant cut-off of 39–40 has been proposed.23 24 Gallacher et al20 categorised ‘high anxiety’ as having a STAI score between 35 and 72, compared with a ‘low anxiety’ group who had a STAI score between 20 and 34. Boot et al19 and Zilkens et al18 used ICD-10 criteria to diagnose an anxiety disorder. Petkus et al21 assessed anxiety using state anxiety subscale of the STPI, which contains a subset of items from the STAI. Participants scoring at least 1 SD above the population mean, equating to a score of ≥25 out of 40, were categorised having ‘high anxiety’. Although there is no established cut-off for clinically significant anxiety using this scale, scores >1 SD above the population mean are likely to represent a group with a high anxiety symptom burden. After discussion among the reviewers (AG, MS, NM), we reached a consensus judgement that the study was suitable for inclusion in this review.
Dementia diagnosis was in most cases assessed using DSM III–IV (n=2) or ICD-10 criteria (n=1), although the study by Boot et al19 assessed dementia with Lewy bodies by clinical diagnosis using published criteria.25
Sample sizes of the studies ranged from 441 to 27 136 participants, recruited from both or either community and hospital inpatient/outpatient populations. Gallacher et al20 and Petkus et al21 conducted prospective cohort studies using a community population that excluded dementia at baseline, the latter focused on twins. Zilkens et al,18 and Boot et al19 conducted matched case–control studies, which retrospectively analysed community and hospital records of individuals with dementia or case-matched controls for anxiety diagnosis and therefore did not include a cognitive assessment at baseline to exclude dementia. Zilkens et al18 drew controls from the electoral roll, whereas Boot et al19 drew them from the community-dwelling persons included in the Mayo Clinic Study of Aging. The proportion of women in each study ranged from 0% to 56.6%. Educational level was recorded for all but one study, and ranged from 55% with no qualifications to 95% with >9 years of education.
Anxiety diagnosis association with dementia
All studies included in this review found a significant increase in the number of dementia diagnoses in patients who had a clinical anxiety diagnosis or experienced clinically significant anxiety symptoms on average at least 10 years prior to their diagnosis of dementia; Zilkens et al18: OR=1.61 (95% CI 1.28 to 2.02), Boot et al19: OR=7.4 (95% CI 3.5 to 16), Gallacher et al20: OR=1.62 (95% CI 0.59 to 4.41) and Petkus et al21: OR=1.48 (95% CI 1.01 to 2.18), respectively.18–21 On the whole, retrospective studies that looked back for lifelong diagnoses of anxiety found a stronger association between midlife anxiety and later dementia diagnosis than prospective studies investigating an association over a shorter time period. Additionally, Petkus et al21 demonstrated that the association between high anxiety and dementia diagnosis remained when they excluded participants who developed dementia within 5 years of the baseline assessment. This subsample had an average interval between baseline and dementia diagnosis of 14.7 years (SD 6.7 years). Both lend support that the associations found were independent of prodromal dementia symptoms.
Each study controlled for a range of demographic factors, and all controlled for vascular and other psychiatric risk factors (tables 2 and 3). All studies assessed and controlled for depression symptoms in their analysis. Boot et al19 found a stronger association between anxiety diagnosis alone with future dementia than either depression diagnosis alone or mixed anxiety and depression diagnosis, although the number of individuals with anxiety was markedly larger than those in the other two categories (anxiety alone n=168; depression alone n=52; anxiety and depression n=56). Although Zilkens et al18 assessed a range of psychiatric diagnoses including anxiety and depression, they did not assess their interaction. Petkus et al21 and Gallacher et al,20 while controlling for depression, made no assessment of the comparative strength of relationship or their interaction.
Table 2.
Case-controlled studies: Newcastle-Ottawa Scale for the assessment of quality of included case-controlled studies
| Acceptable criteria | Zilkens et al 18 | Boot et al19 | |||
| Selection | |||||
| Case definition | With independent validation | Record linkage from Western Australian Data Linkage System and Death Registry, no independent validation | − | Assessment for DLB using behavioural neurologist | + |
| Representativeness of cases | Consecutive or representative series of cases | All dementia cases in period 2000–2009 identified via read code; lower limit index dementia age 65 years, upper limit 84 years; dementia in other diseases excluded | + | Recruited from longitudinal studies in period 1984–2013 (Alzheimer Disease Patient Registry, Alzheimer Disease Research Center Study and Mayo Clinic Study of Aging); community-dwelling persons aged 70–89 years; excluded structural brain lesions | + |
| Selection of controls | Community controls | Population controls; randomly selected from electoral role aged ≥65 years prior to extraction of health data for controls | + | Community controls from longitudinal study of ageing; individuals aged ≥65 years; selected if seen by physician in same month as clinical subject diagnosed; matched by age and sex | + |
| Definition of controls | No history of disease | Excluded if dementia read code in records; no independent screening | + | Excluded if diagnosed with DLB/AD during the study, previous stroke, head injury, neurological disease or movement disorder; extensive cognitive and medical examination | + |
| Comparability | |||||
| Comparability of cases and controls on basis of design and analysis | Study controls for the most important factor (+/−) and any additional factor (+/−) | Controls for age, sex, vascular risk factors (diabetes, IHD, AF, CVD, hypertension, hyperlipidaemia, heart failure and past or current smoking), head injury, alcohol dependence syndrome and depression | ++ | Controls for age, sex; multivariate analyses control for family history, depression, APOE ε4 alleles, education level, head injury, cancer and vascular risk factors (stroke, diabetes, alcohol, smoking) | ++ |
| Exposure | |||||
| Ascertainment of exposure | Secure record, structured interview by healthcare practitioner | Secure administrative health record, read codes for midlife factors documented between aged 30 and 65 years within years 1966–2009 | + | Anxiety history from medical history section of medical record | + |
| Same method of ascertainment for cases and controls | Yes | Yes; review of risk factor read codes | + | Yes; review of medical history | + |
| Non-response rate | Similar for both cases and controls | NR | − | NR | − |
| Total score | 7 | 8 | |||
+/− represents whether individual criterion within the subsection was fulfilled, two symbols indicate that two criteria were assessed within the subsection.
AD, Alzheimer’s disease; AF, atrial fibrillation; APOE, apolipoprotein E; CVD, cerebrovascular disease; DLB, dementia with Lewy bodies; IHD, ischemic heart disease; NR, not recorded.
Table 3.
Cohort studies: Newcastle-Ottawa Scale for assessment of quality of included cohort studies
| Acceptable criteria | Petkus et al21 | Gallacher et al20 | |||
| Selection | |||||
| Representativeness of exposed cohort | Representative of average adult in the community (age(s), BMI, BP, CAMDEX, CDR, DSM III/IV/V, FAB, GHQ-30, ICD-10, MMSE, NR, STAI) | Population-based Swedish twin registry, subsample of twins aged ≥50 years | + | Men only, representative of male inhabitants of Caerphilly region | − |
| Selection of non-exposed cohort | Drawn from same community as exposed cohort | Drawn from same community as exposed cohort | + | Drawn from same community as exposed cohort | + |
| Ascertainment of exposure | Secured records, clinical diagnosis using diagnostic tools (ICD-10/DSM-V) | State anxiety subscale of STPI, containing a subset of items from the STAI | + | Structured interview using STAI | + |
| Demonstration that outcome of interest was not present at start of study | Assessment for dementia at initial enrolment | No baseline screening, exclusion if previous dementia diagnosis, age at inclusion (mean age 60.86 years) makes cognitive impairment unlikely | − | Age at inclusion (mean age 56.1 years) makes cognitive impairment unlikely | − |
| Comparability | |||||
| Comparability of cohorts on basis of design or analysis | Study controls for the most important factor (+/-) and for any additional factor (+/-) | Multivariate models control for depression symptoms, baseline age, sex, education, physical illness | ++ | Study controls for age, social class, marital status, vascular risk factors (alcohol consumption, BP, BMI, total cholesterol, previous vascular disease), educational ability (National Adult Reading Test) and depression symptoms (GHQ-30) | ++ |
| Exposure | |||||
| Assessment of outcome | Independent blind assessment, record linkage | Screening for dementia using MMSE, cognitive in-person testing (assessing a range of cognitive domains), DSM-III or IV and record linkage using National Patient Registry and National Patient Cause of Death Registry | + | Cognitive function assessed using CAMDEX, FAB, CDR; diagnosis made using DSM-IV, screening of primary care and hospital records | + |
| Follow-up adequate for outcome to occur | Follow-up >10 years | 28 years | + | >20 years | + |
| Adequacy of follow-up of cohorts | Complete follow-up or subjects lost to follow-up unlikely to introduce bias | NR | − | 20% lost to follow-up | + |
| Total score | 7 | 7 | |||
+/− represents whether individual criterion within the subsection was fulfilled, two symbols indicate that two criteria were assessed within the subsection.
BMI, body mass index; BP, blood pressure; CAMDEX, Cambridge Mental Disorders of the Elderly Examination; CDR, Clinical Dementia Rating; DSM III/IV/V, Diagnostic and Statistical Manual of Mental Disorders III/IV/V; FAB, Frontal Assessment Battery; GHQ-30, 30-item General Health Questionnaire; ICD-10, International Classification of Diseases 10th Revision; MMSE, Mini-Mental State Examination; NR, not recorded; STAI, State Trait Anxiety Inventory; STPI, State Trait Personality Inventory.
Study quality rating
All studies included were rated highly on the Newcastle-Ottawa Scale.26 From a maximum score of 9, Boot et al19 was rated 8; and Zilkens et al,18 Petkus et al21 and Gallacher et al20 were each rated 7. These studies were of similar quality to those included in a recent meta-analysis examining dementia risk estimates associated with late-life depression.4
Three of the studies had representative samples of community populations; the fourth led by Gallacher et al20 included only men. All controlled for a range of both demographic, physical and psychological health factors. All outcomes were assessed either via secure health records or independent validation. Gallacher et al20 experienced 20% loss to follow-up, which compares favourably to the prementioned Cherbuin et al4 review, which considered studies with an attrition rate of between 4.3% and 55.46% and a review of MCI drug studies with attrition rates varying from 12% to 49%.27 Petkus et al21 did not clearly report lost to follow-up. For both case–control studies, the primary care records did not include a cognitive assessment at baseline. Therefore, pre-existing cognitive impairment before diagnosis cannot be ruled out, although long look-back periods make this less likely.
Discussion
This systematic review found four high-quality studies that all showed a positive association between clinically significant anxiety and risk of late-onset dementia over a mean interval of at least 10 years from anxiety assessment to dementia diagnosis, even after accounting for potential confounders. This important finding provides further evidence that a common mental health condition in midlife is associated with later life neurodegenerative disorders.
Anxiety symptomatology has previously been related to dementia risk and cognitive decline, although not conclusively.10 28 A recent systematic review reported a positive association between anxiety symptoms and dementia diagnosis over a short-time interval.12 In that review, the majority of studies reported follow-up periods between 2 and 3.8 years. A single study had a follow-up time of up to 11.8 years; however, the average interval between anxiety and dementia diagnosis may have been less than 10 years, therefore, it was not included in the current review.13 Gulpers et al found stronger associations with smaller intervals between assessment of anxiety and dementia diagnosis. As a result, the authors concluded that anxiety may result from a prodromal state of dementia, where an increase in anxiety may be due to an individual’s insight into their early subjective experience of cognitive decline.12 Given the short-time interval between assessments, Gulpers et al were unable to determine whether anxiety could also serve as an independent risk for dementia. This review reports solely articles that were not included Gulpers et al’s analyses and therefore furthers their work by providing an independent assessment of the anxiety–dementia association. Effect sizes of the studies included in this review (1.48–7.4) were comparable to the overall effect size found by Gulpers et al12 of 1.61, suggesting that the association between clinically significant midlife anxiety and later life dementia is as strong as that between late-life anxiety symptoms and dementia.
The prodromal phase of dementia can begin several years before objective dementia is manifest. In the present review, we sought to minimise the potential influence of preclinical cognitive decline by including only studies that assessed anxiety and dementia diagnoses over an extended period. Three studies18 20 21 demonstrated a mean interval of at least 10 years between the anxiety and dementia evaluations. Boot et al19 analysed participant’s lifelong medical record; however, the mean interval between anxiety and dementia diagnosis was not reported.
Findings from this review corroborate recent evidence that anxiety symptoms or diagnosis are associated with risk of MCI.29 30 These findings further complement the association between depression and dementia diagnosis,4 which is particularly relevant due to high levels of anxiety–depression comorbidity. Moreover, they lend support for the proposal that multiple psychiatric risk factors are implicated together as a latent risk factor for dementia.2
It has recently been suggested that a longer interval period between anxiety and dementia diagnosis may provide evidence for a common biological pathway linking anxiety, depression and dementia.20 An abnormal stress response, such as exhibited in anxiety disorders, may be associated with accelerated cellular ageing and neuroprogression (a pathological reorganisation of the central nervous system) resulting in increased neurodegeneration, neuronal apoptosis and lowered neuroplasticity.31 Although glucocorticoid, inflammatory mediator and vascular disease mechanisms are hypothesised,3 32 as yet, no convincing candidate biological mechanism linking anxiety and cognitive impairment exists.
The results of this review should be interpreted in the light of their limitations. Only studies that had been published and written in English were included, which may limit extrapolation across broader populations. Retrospective studies did not examine baseline cognition and therefore cannot exclude early cognitive decline at the time of anxiety assessment; however, the length of look back, ranging from over 10 years to the first entry of an individual’s medical record, minimises the likelihood of cognitive impairment at baseline. To account for high levels of anxiety–depression comorbidity, this review included only papers discussing anxiety diagnosis alone or those that controlled for depression symptomatology. However, Zilkens et al18 and Boot et al19 cannot completely exclude overlap of these two commonly comorbid illnesses because their occurrence was ascertained from lists of diagnoses in medical records. The use of read codes in retrospective studies may have resulted in lower identification of individuals with clinically significant anxiety as a result of inconsistent entry of read codes during evaluations or of absence of clinical record for non-help seekers.33 Publication bias may also have influenced the studies included, as positive findings may be more likely to have been published than studies finding no association. Furthermore, results must be interpreted in the light of proposals that the prodromal AD pathophysiological processes may develop beyond 10 years before the onset of clinical symptoms.34
Whether reducing anxiety in middle age would result in reduced risk of dementia remains an open question. The effect of treatment of anxiety using pharmacological and non-pharmacological therapies during midlife on later risk for dementia has not yet been investigated. Benzodiazepines, commonly used in the treatment of anxiety, have been shown to increase risk of mortality in some groups35 and therefore cannot be considered a measure to reduce dementia incidence in those with clinical anxiety. It is possible that diverse non-pharmacological therapies, including talking therapies36 and mindfulness-based interventions and meditation practices,37 that are known to reduce anxiety in midlife, could have a risk-reducing effect, although this is yet to be thoroughly researched.
Given the high prevalence of anxiety seen in primary care, we suggest that general practitioners could consider anxiety alongside depression as an indicator of risk for dementia. To improve the rate of earlier diagnosis of dementia, close monitoring of subtle cognitive decline in older adults with a history of anxiety, depression and cerebrovascular disease would be encouraged. This review expands our understanding of anxiety as a potentially modifiable risk for dementia. Given the limited number of studies investigating the anxiety–dementia relationship, further research is required to assess underlying mechanisms that link these disorders and to disambiguate anxiety’s potential role as a risk factor as separate from a prodromal symptom of dementia.
Supplementary Material
Acknowledgments
We thank Dr Bradley Boeve (Mayo Clinic College of Medicine, Rochester), Dr Claire Burton (Keele University) and Dr Andrew Petkus (University of Southern California) for providing clarification of articles screened for inclusion in support of this work.
Footnotes
Contributors: AG contributed to design of the study, data screening and extraction, drafting of the manuscript and submission. MS contributed to literature search, data screening and extraction and manuscript preparation. JDH contributed to the study design, provided methodological expertise and editing of the manuscript. NLM contributed to the conception and study design, data interpretation and editing of the manuscript.
Funding: This work was supported by a grant from the British Geriatrics Society. NLM was supported by University College London and Alzheimer’s Society (AS-SF-15b-002).
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Fillit H, Nash DT, Rundek T, et al. Cardiovascular risk factors and dementia. Am J Geriatr Pharmacother 2008;6:100–18. 10.1016/j.amjopharm.2008.06.004 [DOI] [PubMed] [Google Scholar]
- 2.Marchant NL, Howard RJ. Cognitive debt and Alzheimer’s disease. J Alzheimers Dis 2015;44:755–70. 10.3233/JAD-141515 [DOI] [PubMed] [Google Scholar]
- 3.Ownby RL, Crocco E, Acevedo A, et al. Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch Gen Psychiatry 2006;63:530 10.1001/archpsyc.63.5.530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cherbuin N, Kim S, Anstey KJ. Dementia risk estimates associated with measures of depression: a systematic review and meta-analysis. BMJ Open 2015;5:e008853 10.1136/bmjopen-2015-008853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diniz BS, Butters MA, Albert SM, et al. Late-life depression and risk of vascular dementia and Alzheimer’s disease: systematic review and meta-analysis of community-based cohort studies. Br J Psychiatry 2013;202:329–35. 10.1192/bjp.bp.112.118307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh-Manoux A, Dugravot A, Fournier A, et al. Trajectories of depressive symptoms before diagnosis of dementia. JAMA Psychiatry 2017;74:712 10.1001/jamapsychiatry.2017.0660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci 2015;17:327–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gallagher D, Coen R, Kilroy D, et al. Anxiety and behavioural disturbance as markers of prodromal Alzheimer’s disease in patients with mild cognitive impairment. Int J Geriatr Psychiatry 2011;26:166–72. 10.1002/gps.2509 [DOI] [PubMed] [Google Scholar]
- 9.Palmer K, Berger AK, Monastero R, et al. Predictors of progression from mild cognitive impairment to Alzheimer disease. Neurology 2007;68:1596–602. 10.1212/01.wnl.0000260968.92345.3f [DOI] [PubMed] [Google Scholar]
- 10.Yochim BP, Mueller AE, Segal DL. Late life anxiety is associated with decreased memory and executive functioning in community dwelling older adults. J Anxiety Disord 2013;27:567–75. 10.1016/j.janxdis.2012.10.010 [DOI] [PubMed] [Google Scholar]
- 11.Beaudreau SA, O’Hara R. Late-life anxiety and cognitive impairment: a review. Am J Geriatr Psychiatry 2008;16:790–803. 10.1097/JGP.0b013e31817945c3 [DOI] [PubMed] [Google Scholar]
- 12.Gulpers B, Ramakers I, Hamel R, et al. Anxiety as a predictor for cognitive decline and dementia: a systematic review and meta-analysis. Am J Geriatr Psychiatry 2016;24:823–42. 10.1016/j.jagp.2016.05.015 [DOI] [PubMed] [Google Scholar]
- 13.de Bruijn RF, Direk N, Mirza SS, et al. Anxiety is not associated with the risk of dementia or cognitive decline: the Rotterdam Study. Am J Geriatr Psychiatry 2014;22:1382–90. 10.1016/j.jagp.2014.03.001 [DOI] [PubMed] [Google Scholar]
- 14.Burton C, Campbell P, Jordan K, et al. The association of anxiety and depression with future dementia diagnosis: a case-control study in primary care. Fam Pract 2013;30:25–30. 10.1093/fampra/cms044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson RS, Leurgans SE, Boyle PA, et al. Cognitive decline in prodromal Alzheimer disease and mild cognitive impairment. Arch Neurol 2011;68:351–6. 10.1001/archneurol.2011.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gauthier S, Reisberg B, Zaudig M, et al. Mild cognitive impairment. Lancet 2006;367:1262–70. 10.1016/S0140-6736(06)68542-5 [DOI] [PubMed] [Google Scholar]
- 17.Centre for Reviews and Dissemination. CRD’s Guidance for undertaking reviews in health care, 2009. [Google Scholar]
- 18.Zilkens RR, Bruce DG, Duke J, et al. Severe psychiatric disorders in mid-life and risk of dementia in late- life (age 65-84 years): a population based case-control study. Curr Alzheimer Res 2014;11:681–93. 10.2174/1567205011666140812115004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boot BP, Orr CF, Ahlskog JE, et al. Risk factors for dementia with Lewy bodies: a case-control study. Neurology 2013;81:833–40. 10.1212/WNL.0b013e3182a2cbd1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gallacher J, Bayer A, Fish M, et al. Does anxiety affect risk of dementia? Findings from the Caerphilly Prospective Study. Psychosom Med 2009;71:659–66. 10.1097/PSY.0b013e3181a6177c [DOI] [PubMed] [Google Scholar]
- 21.Petkus AJ, Reynolds CA, Wetherell JL, et al. Anxiety is associated with increased risk of dementia in older Swedish twins. Alzheimers Dement 2016;12:399–406. 10.1016/j.jalz.2015.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spielberger C. Manual for the State-Trait Anxiety Inventory, 1983. [Google Scholar]
- 23.Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res 2011;63:S467–72. 10.1002/acr.20561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Knight RG, Waal-Manning HJ, Spears GF. Some norms and reliability data for the State-Trait Anxiety Inventory and the Zung Self-Rating Depression scale. Br J Clin Psychol 1983;22:245–9. 10.1111/j.2044-8260.1983.tb00610.x [DOI] [PubMed] [Google Scholar]
- 25.McKeith IG, Dickson DW, Lowe J, et al. Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology 2005;65:1863–72. 10.1212/01.wnl.0000187889.17253.b1 [DOI] [PubMed] [Google Scholar]
- 26.Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. 2012. http//www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 27.Jelic V, Kivipelto M, Winblad B. Clinical trials in mild cognitive impairment: lessons for the future. J Neurol Neurosurg Psychiatry 2006;77:429–38. 10.1136/jnnp.2005.072926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bierman EJ, Comijs HC, Rijmen F, et al. Anxiety symptoms and cognitive performance in later life: results from the longitudinal aging study Amsterdam. Aging Ment Health 2008;12:517–23. 10.1080/13607860802224276 [DOI] [PubMed] [Google Scholar]
- 29.Jacob L, Bohlken J, Kostev K. Risk factors for mild cognitive impairment in German primary care practices. J Alzheimers Dis 2017;56:379–84. 10.3233/JAD-160875 [DOI] [PubMed] [Google Scholar]
- 30.Kassem AM, Ganguli M, Yaffe K, et al. Anxiety symptoms and risk of dementia and mild cognitive impairment in the oldest old women. Aging Ment Health 2017:1–9. 10.1080/13607863.2016.1274370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perna G, Iannone G, Alciati A, et al. Are anxiety disorders associated with accelerated aging? A focus on neuroprogression. Neural Plast 2016;2016:1–19. 10.1155/2016/8457612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sapolsky RM. Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Arch Gen Psychiatry 2000;57:925–35. 10.1001/archpsyc.57.10.925 [DOI] [PubMed] [Google Scholar]
- 33.Davé S, Petersen I. Creating medical and drug code lists to identify cases in primary care databases. Pharmacoepidemiol Drug Saf 2009;18:704–7. 10.1002/pds.1770 [DOI] [PubMed] [Google Scholar]
- 34.Pietrzak RH, Lim YY, Neumeister A, et al. Amyloid-β, anxiety, and cognitive decline in preclinical Alzheimer disease: a multicenter, prospective cohort study. JAMA Psychiatry 2015;72:284–91. 10.1001/jamapsychiatry.2014.2476 [DOI] [PubMed] [Google Scholar]
- 35.Fontanella CA, Campo JV, Phillips GS, et al. Benzodiazepine use and risk of mortality among patients With schizophrenia. J Clin Psychiatry 2016;77:661–7. 10.4088/JCP.15m10271 [DOI] [PubMed] [Google Scholar]
- 36.Orgeta V, Qazi A, Spector AE, et al. Psychological treatments for depression and anxiety in dementia and mild cognitive impairment Orgeta V, Cochrane Database of Systematic Reviews. 23 Chichester, UK: John Wiley & Sons, Ltd, 2014. 10.1002/14651858.CD009125.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khoury B, Lecomte T, Fortin G, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev 2013;33:763–71. 10.1016/j.cpr.2013.05.005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-019399supp001.pdf (77.3KB, pdf)