Abstract
Objective:
Physicians’ knowledge of antibiotics, their attitudes, expectations, and practices regarding antibiotic prescription is fundamental for controlling the irrational antibiotic use. This study evaluates primary health care (PHC) physicians’ knowledge, expectation, and practices regarding antibiotics use in upper respiratory tract infections.
Methods:
A cross-sectional study conducted in the Qassim region where 32 PHC centers were selected randomly. A total of 294 PHC physicians were surveyed. A pre-tested questionnaire was used after an orientation of participating physicians.
Results:
Response rate was 80.3%. There is a significant belief among participants that the use of antibiotics leads to relief of symptoms in the case of viral disease and that taking antibiotics without rational indication increases the side effects. Participants identified that inadequate prescription, use without prescription, and non-compliance of patients are the most important factors contributing to the development of bacterial resistance. Participants often blamed the pharmacist for contributing mostly to the development of the problem of antibiotic resistance. Most physicians identified that they feel under pressure if patients expect an antibiotic prescription. In the absence of laboratory confirmation, most physicians selected high fever as the symptom that makes them prescribe antibiotics. Although having practice guidelines, participants demonstrated that these guidelines do not consider individual variations of patients’ need. They do not support a regulation to prohibit antibiotic prescription without laboratory confirmation.
Conclusions:
The distribution of PHC physicians’ knowledge, attitudes, and practices did not significantly vary between urban and rural centers. Therefore, whichever measures will be taken to improve the antibiotics practices can be applied to any PHC setting.
Keywords: Antibiotic prescription, physicians, primary health care, Saudi Arabia
Introduction
Bacterial resistance to antibiotics is one of the significant problems of health-care system. The World Health Organization has identified some factors in the physicians’ role related to bacterial resistance. These factors included - among others - patient pressure and demand for antibiotics that force a physician to prescribe them.[1]
Upper respiratory tract infection (URTI) patients make up the main part of the workload in primary health care (PHC) particularly during the winter months all over the world and in Saudi Arabia.[2,3] In most of the recorded cases, viral infections are the main etiological factor, and thus, prescribing of antibiotic treatment is not indicated.[4,5] However, several physicians prescribe antibiotics for URTI, while prescribing of antibiotics does not work against viral infection, but it may arise in the appearance and development of resistant viral strains.[6,7]
Many factors are suggested to influence physicians’ decision to prescribe antibiotics for URTI. These factors include expecting that a viral infection may lead to a secondary bacterial infection, suspected bacterial infection, and the belief that the prescribing antibiotics will satisfy the patient.[8-10]
Studies demonstrated that patients’ expectations for antibiotics are a significant influence of actual prescribing.[11-13] In addition, when physicians thought that the patient is expecting an antibiotic, they are also more likely to diagnose a bacterial infection.[14,15]
Physicians in PHC are dealing with a majority of patients with URTI. Improving our understanding of the physicians’ knowledge of antibiotics, their attitudes, expectations, and practices regarding antibiotic prescription is fundamental to controlling the irrational antibiotic use. This study aimed to evaluate PHC physicians’ knowledge, expectations, and practices regarding antibiotic use in URTI.
Methods
Design, setting, and population sampling
This study was conducted in Al-Qassim region of Saudi Arabia for 2 months.
Qassim region is located in the northern, central area of Saudi Arabia. In the Qassim region, there were 142 PHC Centers (PHCCs) distributed throughout the entire region. These centers provide comprehensive PHC services to the nearby general population. For administrative purposes, these centers were put under the supervision of 16 regional offices. Each of these offices supervises an average of 4–15 PHCCs. For this study, two centers from each regional supervising office were selected randomly which included 32 centers. This constituted about 22.5% of the PHCCs of Qassim region. The selected centers comprised of 20 rural with 139 PHC physicians, plus 12 urban PHCCs with 155 PHC physicians, and a total of 294 PHC physicians.
The instrument
A questionnaire that sought information related to knowledge, attitude, and practice of physicians toward URTI and prescribing antibiotics was developed. Review of relevant literature, opinions of experts, and a consensus among experts and authors were used to reach the final version of the questionnaire. The questionnaire was then tested on a subsample of physicians for understandability and reliability, and the necessary modification was done. The questionnaire has 7 parts. These parts are as follows: Personal data, beneficial effects of antibiotics, harmful effects of antibiotics, antibiotic resistance, and factors influencing antibiotic prescription, practice guidelines, efficacy of alternatives to antibiotics, and the advice that should be given to patients who are prescribed antibiotics.
Orientation of physicians
General practitioners in the selected PHC centers were recruited to participate in this study. They received an orientation session to illustrate the purpose of the study. All items of the questionnaire were explained to them to obtain standardized and valid responses.
All aspects of the study methodology were reviewed and approved by the Research and Ethical Committee of Qassim College of Medicine and by the PHC Directorate of the region.
Data analysis
Data were entered and analyzed using the Statistical Package for Social Sciences.[16] Frequency distributions of all variables were produced. All P values were based on the 2-sided test, and the cutoff value for statistical significance is set at 0.05. The Chi-squared analysis was used to test differences in proportions, and independent Student’s t-test was used for analysis of quantitative data.
Results
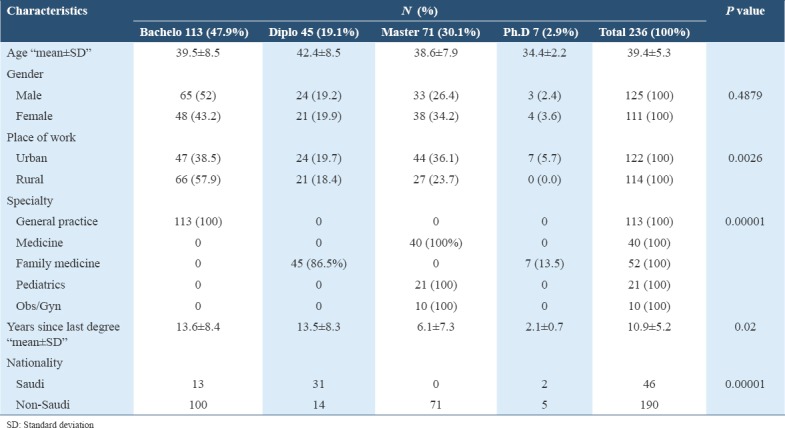
The questionnaire was distributed to 294 PHC physicians, 236 physicians returned their reply with a response rate 80.3%. Table 1 summarizes physicians’ personal and demographic characteristics. Physicians with an only bachelor degree constitute the majority (47.9%) of the sample and distributed similarly between rural and urban centers. Most physicians (113) are general practitioners, and only 7 physicians have Ph.D. in family medicine. The mean duration for the last degree for all physicians was 10.9 ± 5.2. The participants are mostly non-Saudis 80.5%. Male physicians constituted 52.9% of the study participants. Moreover, data were expressed mean, standard deviation, number, and percentage (%) wherever applicable.
Table 1.
Participants’ characteristics
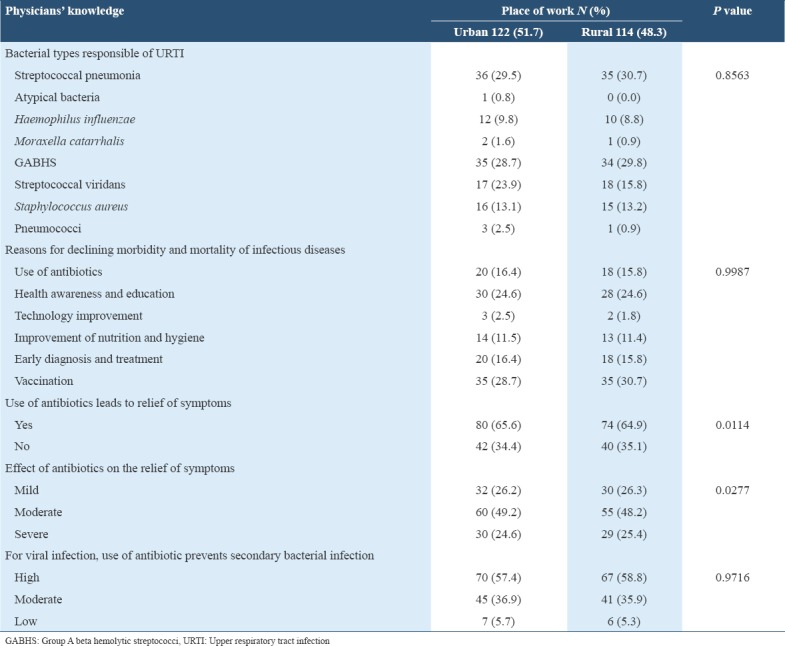
Beneficial effects
Table 2 summarizes physicians’ knowledge and expectations and shows the following results; participants identified correctly the bacterial types most responsible for URTI with no significant variation between urban and rural physicians. There is an apparent consensus among all physicians that the reasons for the current decline of morbidity and mortality due to infectious diseases are: Vaccination, health education and awareness, use of antibiotics, and early diagnosis and treatment. There is also a significant belief among physicians that the use of antibiotics leads to relief of symptoms and that this relief is mainly mild and moderate. Participants also agree that the use of antibiotics prevents secondary infections in the case of viral infections.
Table 2.
Participant’s knowledge and expectations of beneficial effects of antibiotics
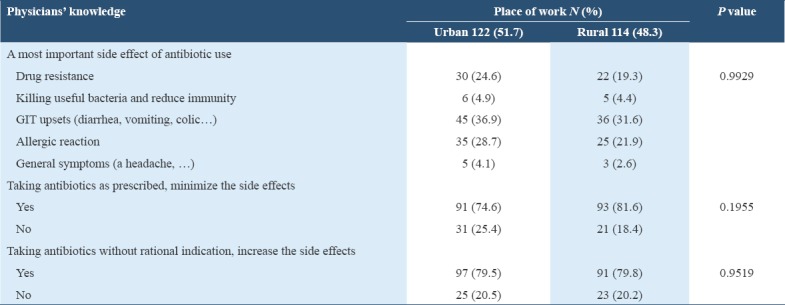
Harmful and side effects
On the other side, the most common harmful and side effects of antibiotics as identified by participants are gastrointestinal tract upsets, allergic reaction, and drug resistance. The statements that taking the antibiotics as prescribed minimizes the side effects and taking the antibiotics without rational indication increases the side effects were endorsed by the vast majority of both rural and urban physicians with no significant variations between them [Table 3].
Table 3.
Participant’s knowledge and expectations of harmful effects of antibiotics
Resistance to antibiotics
Knowledge of participants regarding resistance to antibiotics shows no significant difference between rural and urban physicians. Participants identified that inadequate prescription, use without prescription, and non-compliance of patients are the most important factors contributing to the development of bacterial resistance to antibiotics. When participants were asked “who is contributing the most to the development of the problem of antibiotic resistance,” they often put the responsibility on the pharmacist. The previous use of antibiotics increases the person’s risk of acquiring drug-resistant infection which was also endorsed by the majority of physicians.
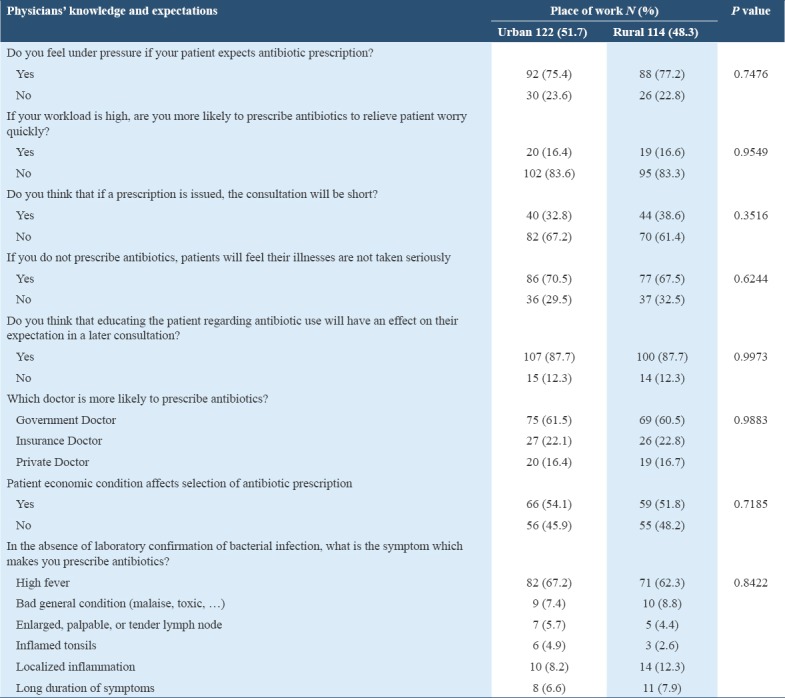
Factors affecting antibiotics prescription
Many factors influence physicals’ prescription of antibiotics as summarized in Table 4. Most physicians identified that they feel under pressure if patients expect an antibiotic prescription and if they feel their patient will believe their illnesses are not taken seriously. On the contrary, participants showed that high workload and patient economic condition do not affect significantly their choice whether or not to prescribe antibiotics. Educating the patient regarding antibiotic use was recognized by most physicians as an important factor that rationalizes patient expectation. In the absence of laboratory confirmation, most physicians selected high fever as the symptom that makes them prescribe antibiotics.
Table 4.
Participant’s knowledge and expectations of factors influencing antibiotic prescription
Practice guidelines
The presence of antibiotic practice guidelines affected physicians’ prescription of antibiotics. Almost two-third of physicians declared that their PHC centers have practice guidelines. The majority of physicians showed that these guidelines should affect their selection of the prescribed antibiotics; however, they demonstrated that practice guidelines do not consider individual variations of patients’ need. Although most physicians supported that the use of guidelines is needed for proper patient care, they do not support with the same degree the regulation to prohibit antibiotic prescription without laboratory confirmation.
Use of alternatives
Most physicians believed that drug groups other than antibiotics are not effective in the treatment of bacterial infection. Urban PHC physicians are significantly higher than rural PHC physicians in endorsing this belief. Most physicians also demonstrated that they will not try these alternatives as the first-line management in case of bacterial infection diagnosis
Physicians’ advice
Physicians’ advice to their patient regarding prescribed antibiotic use is multiple although variable. Advice to evade giving the left over to a family member if having a similar condition, to complete the full course of treatment, and to avoid repeating the treatment without consultation was recognized as always given to patients by more than 80% of participants. Some other advices such as proper use of antibiotics, do not stop, decrease or increase the treatment without consultation, and the side effects expected were recognized with less frequency by the physicians.
Other advice related to pregnancy status, missing a dose, having allergies to contain types of antibiotics, and how to deal with severe adverse side effects was identified correctly by the majority PHC participants.
In addition, most participants declared that the best person to provide information regarding proper use of antibiotics is the physician than the pharmacist. The majority of them also affirmed that they support a decision that stops providing antibiotics to patients without a prescription.
Discussion
Understanding the great importance of proper use of antibiotics, particularly in PHCCs, this work was done to examine this issue in detail from the perspectives of PHC physicians who are responsible for prescription and education of patients regarding antibiotics. Filling the gap in researches regarding this issue can offer proper research-derived recommendations.
In this study, comparisons are made between rural and urban physicians. Other factors such as gender, nationality, age, years since graduation, and background specialization do not seem to affect physicians’ knowledge and expectation since they all receive extensive and frequent orientation and training on PHC principles and practices. Unlike rural areas, urban settlements have superior public facilities, more opportunities for education, modern transportation, more developed business and social interaction, and in general, better living standards. People living in rural areas might be different socially and culturally from urban people. This difference can affect the doctor-patient interaction and consequently the doctor’s perception to antibiotic prescription.
The distribution of knowledge, attitudes, and practices of PHC physicians regarding the use of antibiotics did not significantly vary statistically, with very few exceptions, between urban and rural PHCCs. This observation might reflect agreement on the level of awareness among rural and urban physicians, rather than any specific financial, structural, or administrative factors, found in the different locations of the PHC system of the region. Therefore, any measures to improve the antibiotics practices will benefit the care of patients in any PHC setting.
The least consensus between rural and urban physicians is observed in their knowledge regarding the role of antibiotics to relieve symptoms of infections and how much is this relief whether mild, moderate, or severe. Our results indicate that the knowledge level of physicians, although appropriate, is not perfect and also varied between rural and urban physicians. Knowledge of physicians is important factors that influence prescribing of antibiotics.[17-19] Since knowledge and attitudes are potentially modifiable, this study suggests that plans specifically targeted at changing this knowledge and attitude of physicians could reduce irrational prescribing of antibiotics in primary care. The main strategy for improving deficient knowledge and attitude might lie in the training of PHC physicians and continuing medical education.
Many qualitative studies explored knowledge, attitude, and perceptions’ factors of physicians regarding antibiotic prescribing. These studies, however, did not determine which factors are associated with inappropriate prescription of antibiotics or the degree of association. One qualitative study stated that the attitudes most frequently referred to by physicians were satisfying the patient and fear to escape his expectation,[20] and this result is in line with the findings of our study. Patients’ expectations are often transformed as misprescription, due to the physician’s attempt to keep a good physician-patient relationship.[21]
This study demonstrated some shortage of knowledge in areas related to antibiotic prescriptions, such as organisms most responsible for URTI, use of antibiotics leads to relief of symptoms, and use of antibiotics for viral infection avoid bacterial infection. Since knowledge is a factor inversely associated with mis-prescription of antibiotics, it can be inferred that highest level of appropriate knowledge about antibiotic use among physicians must be associated with lowest level of mis-prescription. Other studies have confirmed that ongoing education is a successful intervention to raise doctors’ knowledge on antibiotic use and to improve their prescribing behavior.[22-24]
Trying to satisfy patients can be linked to patients’ attitude to antibiotics. In many worldwide countries, particularly in Saudi Arabia, patients are more likely to use antibiotics, even for treating viral illnesses.[25] In addition, trying to satisfy patients can be linked to average time doctor spent in consultation - the shorter the consultation time, the fewer possibilities of the patient involvement in decision-making.[26] For better management of average time per consultation, delayed prescribing is suggested to improve the influence of trying to satisfy patients. A recent study shows that most patients are satisfied with delayed prescribing.[27]
A recent retrospective cohort study demonstrated that physicians’ attitudes and knowledge determine the quality of prescription of antibiotics.[17] Therefore, understanding the physicians’ knowledge and attitude on antibiotic use is crucial to improve efforts to provide appropriate antibiotic prescribing. This study found that doctors have some shortage of knowledge and attitude about antibiotics regarding beneficial effects of antibiotics, harmful effects of antibiotics, antibiotic resistance, factors influencing antibiotic prescriptions, practice guidelines, the efficacy of alternatives to antibiotics, and the advice that should be given to patients who are prescribed antibiotics. Although ongoing education is partly successful in enhancing doctors’ knowledge and attitude on antibiotic use, the effect needs further improvement. Doctors of primary health-care institutions are in need for more targeted interventions such as the use of practice guidelines, improving patient awareness and education, and regulations for prescribing and dispensing antibiotics.
In this study, participants’ knowledge and expectations of antibiotic resistance are variable. They may be unaware of the specific antimicrobial resistance rates and their pattern in PHC settings. This may be the result of limited data sharing. A surveillance system for antimicrobial usage and resistance should include the well-timed distribution of information to all health-care workers.
Strengths of this study include the design of the questionnaire. The questionnaire was developed after a comprehensive review of the literature. The questionnaire was validated in terms of reproducibility, face, and content validity. Additional strength is the highest participation rate achieved by PHCCs physicians (80.3%) which reduced the risk of non-participation bias.
Conversely, the limitation of this study lay on the absence of standard indicators for knowledge and practices to compare them with the physicians’ antibiotic prescribing. Scoring of physicians knowledge and attitude was not performed in this study to assess how much lower, higher, or meeting the expectation. Furthermore, studying the influence of physicians’ knowledge and attitudes on the practice is lacking in this study. Comparing results of this study with international results were not done, and results from different countries may differ due to the doctors’ level of education, the standard level of care, and the setting whether primary or tertiary care.[18,19]
References
- 1.World Health Organization. Overcoming antimicrobial resist. J Am Med Assoc. 2000;117:245–50. [Google Scholar]
- 2.Bauman KA. The family physician's reasonable approach to upper respiratory tract infection care for this century. Arch Fam Med. 2000;9:596–7. doi: 10.1001/archfami.9.7.596. [DOI] [PubMed] [Google Scholar]
- 3.Annual Statistical Report. Ministry of Health, Primary Health Care. Saudi Arabia: 2003. [Google Scholar]
- 4.Orr PH, Scherer K, Macdonald A, Moffatt ME. Randomized placebo-controlled trials of antibiotics for acute bronchitis: A critical review of the literature. J Fam Pract. 1993;36:507–12. [PubMed] [Google Scholar]
- 5.Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the united states. Clin Infect Dis. 2001;33:757–62. doi: 10.1086/322627. [DOI] [PubMed] [Google Scholar]
- 6.Hamm RM, Hicks RJ, Bemben DA. Antibiotics and respiratory infections: Are patients more satisfied when expectations are met? J Fam Pract. 1996;43:56–62. [PubMed] [Google Scholar]
- 7.Braun BL, Fowles JB. Characteristics and experiences of parents and adults who want antibiotics for cold symptoms. Arch Fam Med. 2000;9:589–95. doi: 10.1001/archfami.9.7.589. [DOI] [PubMed] [Google Scholar]
- 8.Palmer DA, Bauchner H. Parents and physicians views on antibiotics. Pediatrics. 1997;99:E6. doi: 10.1542/peds.99.6.e6. [DOI] [PubMed] [Google Scholar]
- 9.Mangione-Smith R, McGlynn EA, Elliott MN, McDonald L, Franz CE, Kravitz RL, et al. Parent expectations for antibiotics, physician-parent communication, and satisfaction. Arch Pediatr Adolesc Med. 2001;155:800–6. doi: 10.1001/archpedi.155.7.800. [DOI] [PubMed] [Google Scholar]
- 10.Barden LS, Dowell SF, Schwartz B, Lackey C. Current attitudes regarding use of antimicrobial agents: Results from physician's and parents focus group discussions. Clin Pediatr. 1998;37:665–71. doi: 10.1177/000992289803701104. [DOI] [PubMed] [Google Scholar]
- 11.Cockburn J, Pit S. Prescribing behaviour in clinical practice: Patients expectations and doctors perceptions of patients expectations-a questionnaire study. BMJ. 1997;315:520–3. doi: 10.1136/bmj.315.7107.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwartz RH, Freij BJ, Ziai M, Sheridan MJ. Antimicrobial prescribing for acute purulent rhinitis in children: A survey of pediatricians and family practitioners. Pediatr Infect Dis J. 1997;16:185–90. doi: 10.1097/00006454-199702000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Stivers T, Mangione-Smith R, Elliott MN, McDonald L, Heritage J. Why do physicians think parents expect antibiotics? What parents report vs what physicians believe. J Fam Pract. 2003;52:140–8. [PubMed] [Google Scholar]
- 14.Cowan PF. Patient satisfaction with an office visit for the common cold. J Fam Pract. 1998;24:412–3. [PubMed] [Google Scholar]
- 15.Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. J Am Med Assoc. 1998;279:875–7. doi: 10.1001/jama.279.11.875. [DOI] [PubMed] [Google Scholar]
- 16.Norusis MJ. Statistical package for Social Sciences (SPSS) for Windows. Chicago, Ill: SPSS Inc; 1990. [Google Scholar]
- 17.Gonzalez-Gonzalez C, López-Vázquez P, Vázquez-Lago JM, Piñeiro-Lamas M, Herdeiro MT, Arzamendi PC, et al. Effect of physicians attitudes and knowledge on the quality of antibiotic prescription: A Cohort study. PLoS One. 2015;10:e0141820. doi: 10.1371/journal.pone.0141820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.García C, Llamocca LP, García K, Jiménez A, Samalvides F, Gotuzzo E, et al. Knowledge, attitudes and practice survey about antimicrobial resistance and prescribing among physicians in a hospital setting in lima, peru. BMC Clin Pharmacol. 2011;11:18. doi: 10.1186/1472-6904-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thriemer K, Katuala Y, Batoko B, Alworonga JP, Devlieger H, Van Geet C, et al. Antibiotic prescribing in DR congo: A knowledge, attitude and practice survey among medical doctors and students. PLoS One. 2013;8:e55495. doi: 10.1371/journal.pone.0055495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Teixeira Rodrigues A, Roque F, Falcão A, Figueiras A, Herdeiro MT. Understanding physician antibiotic prescribing behaviour: A systematic review of qualitative studies. Int J Antimicrob Agents. 2013;41:203–12. doi: 10.1016/j.ijantimicag.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Wartman SA, Morlock LL, Malitz FE, Palm E. Impact of divergent evaluations by physicians and patients of patients complaints. Public Health Rep. 1983;98:141–5. [PMC free article] [PubMed] [Google Scholar]
- 22.Kiang KM, Kieke BA, Como-Sabetti K, Lynfield R, Besser RE, Belongia EA. Clinician knowledge and beliefs after statewide program to promote appropriate antimicrobial drug use. Emerg Infect Dis. 2005;11:904–11. doi: 10.3201/eid1106.050144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Akter SF, Heller RD, Smith AJ, Milly AF. Impact of a training intervention on use of antimicrobials in teaching hospitals. J Infect Dev Ctries. 2009;3:447–51. doi: 10.3855/jidc.416. [DOI] [PubMed] [Google Scholar]
- 24.Roque F, Herdeiro MT, Soares S, Teixeira Rodrigues A, Breitenfeld L, Figueiras A, et al. Educational interventions to improve prescription and dispensing of antibiotics: A systematic review. BMC Public Health. 2014;14:1276. doi: 10.1186/1471-2458-14-1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.European Commission. Antimicrobial resistance. Eurobarometer 338/Wave 72.5-TNS Opinion and Social. Luxembourg: European Commission; 2010. Available from: http://www.ec.europa.eu/health/antimicrobial-resistance/docs/ebs-33-en.pdf . [Google Scholar]
- 26.Cadieux G, Tamblyn R, Dauphinee D, Libman M. Predictors of inappropriate antibiotic prescribing among primary care physicians. Can Med Assoc J. 2007;177:877–83. doi: 10.1503/cmaj.070151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Høye S, Frich JC, Lindbæk M. Use and feasibility of delayed prescribing for respiratory tract infections: A questionnaire survey. BMC Fam Pract. 2011;12:34. doi: 10.1186/1471-2296-12-34. [DOI] [PMC free article] [PubMed] [Google Scholar]


