Abstract
Objective
To examine the association between the amount, intensity, and pattern of steps·day−1 with weight loss.
Methods
Participants (N=260, age=42.8±8.9, BMI=32.8±3.5 kg/m2) completed an 18-month weight loss intervention that included a calorie-restricted diet and prescribed physical activity. Participants were categorized by 18- month weight loss as weight gain (GAIN), weight loss of 0 to <5% (WL<5%), 5 to <10% (WL<10%), ≥10% (WL≥10%). Steps·day−1 were measured at 0, 6, 12 and 18 months and defined as total steps·day−1, total steps·day−1 of moderate-to-vigorous physical activity (MVPA; ≥3 metabolic equivalents) in bouts of ≥10 minutes (BOUT-MVPA), MVPA in bouts of <10 minutes (NON-BOUT-MVPA), or non-MVPA steps·day−1 (NON-MVPA).
Results
There was a Weight Loss Category by Time interaction (p<0.0001) for total and BOUT-MVPA steps·day−1. Total steps·day−1 at 18 months was WL≥10%=9822 (95% CI: 9073, 10571), WL<10%=8612 (7613, 9610), WL<5%=7802 (6782, 8822), GAIN=7801 (6549, 9053). BOUT-MVPA steps·day−1 at 18 months was WL≥10%=3482 (2982, 3981), WL<10%=1949 (1269, 2629), WL<5%=1735 (1045, 2426), GAIN=1075 (210, 1941). Participant were also categorized based on achieving ≥10% weight loss at either 6 or 18 months and a similar pattern was observed.
Conclusions
10,000 steps·day−1, with approximately 3,500 steps·day−1 performed as BOUT-MVPA, is associated with enhanced weight loss in a behavioral intervention.
Keywords: physical activity, exercise, obesity
INTRODUCTION
Physical activity is an important component of weight management interventions.(1, 2, 3, 4, 5) Engagement in 200–300 minutes per week of moderate-to-vigorous physical activity (MVPA) is also predictive of improved longer-term weight loss.(6, 7, 8, 9, 10, 11, 12) Thus, promoting engagement in this level of MVPA may have public health implications for the effective treatment of overweight and obesity.
While current recommendations for physical activity for weight control are typically expressed in units of minutes per week, an alternative metric for physical activity is to prescribe a threshold of steps per day (steps·day−1). Tudor-Locke et al. reported that adults achieving the 30 minutes of daily MVPA accumulate about 8,000 steps·day−1, with 7,000 steps·day−1 every day of the week being the parallel to 150 minutes of weekly MVPA.(13) However, whether the number of steps, the intensity of these steps, or the pattern for how these steps are accumulate is associated with improved long-term weight loss within the context of a behavioral weight loss program has not been reported. Given the current widespread availability of consumer-based activity monitors that provide feedback on physical activity in units of steps·day−1,(14) clarifying the quantity of steps·day−1 that is associated with improved weight loss may have important clinical and public health implications.
Therefore, the purpose was to conduct a secondary data analysis from a clinical trial to examine whether the amount of steps, intensity of steps, or patterns of steps is associated with weight loss within the context of an 18-month behavioral weight loss intervention.
METHODS
Participants
Participants were recruited to participate in a behavioral weight loss intervention between May 2008 and February 2010. This study utilized two clinical sites (Pittsburgh, PA and Chapel Hill, NC), thus, study procedures were approved by the Institutional Review Boards at both institutions. Data collection was completed by September 2011. The primary outcomes of this study have been published previously.(15)
Participants were recruited through various types of advertisements and media outlets including television commercials, newspaper advertisements, and others. Prior to entry into the study, participants completed a telephone screening to determine initial eligibility. Once determined to be initially eligible, participants attended an orientation session where all study procedures were outlined and explained. After the orientation session and prior to entry into the study, interested participants provided written informed consent. Participants provided physician’s clearance, medical history, and completed a physical activity readiness questionnaire (PAR-Q) prior to engagement in baseline assessments and subsequent engagement into the weight loss intervention. Eligibility criteria included age 18 to 55 years old, BMI of 25.0 to <40.0 kg/m2, and other criteria that have been previously reported.(15)
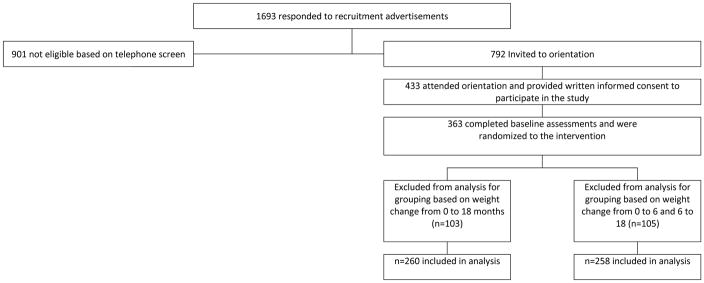
There were 363 individuals randomized in this study. Justification of sample size, randomization procedures, and the CONSORT diagram for the primary analysis have been published previously(15) along with the CONSORT diagram based on the categories of weight change patterns.(8) Thus, for the secondary data analyses that were conducted and presented in this reported, only those participants with weight data available at both 0 and 18 months (N=260) or 0, 6, and 18 months (N=258) were included (Figure 1). Participant demographic information is provided in Table 1, and is similar to what has previously been reported.(8)
Figure 1.
Consort Diagram
Table 1.
Descriptive characteristics of participants [N (%) for categorical variables and mean±SD for continuous variables]
| Subjects Randomized | Subjects with both Baseline and 18 Month Weight Measured | Subjects with both Baseline, 6, and 18 Month Weight Measured | |
|---|---|---|---|
| Number of Subjects [Number (% of total)] | 363 (100%) | 260 (100%) | 258 (100%) |
| Gender(Females) [Number (% of total)] | 300 (82.6%) | 206 (79.2%) | 206 (79.8%) |
| Age(years) | 42.2±9.0 | 42.8±8.9 | 42.9±8.9 |
| Body Mass Index(kg/m2) | 33.0±3.6 | 32.8±3.5 | 32.8±3.5 |
| Ethnicity [Number (% of total)] | |||
| Asian | N=2 (0.6%) | N=2 (0.8%) | N=2 (0.8%) |
| Black or African-American | N=103 (28.4%) | N=69 (26.5%) | N=68 (26.4%) |
| Hispanic, Latino, Portuguese, Cape Verdean | N=7 (1.9%) | N=5 (1.9%) | N=5 (1.9%) |
| White | N=243 (66.9%) | N=181 (69.6%) | N=180 (69.8%) |
| Other | N=8 (2.2%) | N=3 (1.2%) | N=3 (1.2%) |
Behavioral Weight Loss Intervention
Participants were randomized to either a standard behavioral weight loss intervention (SBWL) or a stepped-care weight loss intervention (STEP). Both interventions were 18-months long and included group meetings and phone call contacts. Both interventions received the same dietary recommendations and physical activity prescription. The details of each intervention and the main study outcomes have been reported previously, however, a brief description is provided below.(15)
Dietary Recommendations
SBWL and STEP were prescribed the same calorie-restricted diet consisting of 1,200–1,800 kcal/day based on initial body weight. In addition, both intervention groups were recommended to reduce fat intake to 20–30% of total energy intake. Participants were instructed to self-monitor dietary intake throughout the study using a weekly food diary; however, this self-monitoring was used as a weight loss strategy and these data were not intended to be used to quantify dietary intake for the purpose of data analysis.
Physical Activity
SBWL and STEP were prescribed identical physical activity programs. The physical activity prescription started at 100 min/week of moderate-to-vigorous intensity physical activity (MVPA) and increased by 50 minutes every 4 weeks until a prescription of 300 min/week was reached. Participants were encouraged to be physically active in bouts that were >10 min in duration and at a moderate-to-vigorous intensity. Physical activity was mainly prescribed in the form of a brisk walking program, however, other forms of aerobic physical activity (e.g., bicyling, swimming, running, etc.) were considered accepted alternatives to walking.
SBWL Intervention
SBWL was offered group-based intervention sessions regularly throughout the 18-month intervention. Group-based intervention sessions were conducted weekly during months 1–6, every other week during months 7–12, and monthly during months 13–18. Lessons focused on topics surrounding weight loss including dietary recommendations, physical activity, or behavioral strategies that would promote adherence to recommendations and ultimately success in the program. Participants were advised to attend all of the group sessions, however, participants who were unable to attend a group session were offered an individual make-up session. If an individual make-up session was not possible an attempt was made to conduct a brief session by telephone.
STEP Intervention
STEP was offered one group-based intervention session per month throughout the 18-month intervention. Investigators set a priori weight loss goals of 5% at 3 months, 7% at 6 months, and 10% at months 9, 12, and 15. If a participants did not achieve the pre-determined weight loss goal and any of the time points, additional intervention contact or other strategies were added in an attempt to improve weight loss as previously described.(15) Group-based intervention sessions had similar lessons to SBWL. Also, participants who were unable to attend a scheduled in-person intervention session were offered a make-up sessions similar to the process used for SBWL.
Assessment of Outcomes
Height, Weight, and BMI
Body weight was assessed at 0, 6, 12, and 18 months. Weight was assessed on a digital scale to the nearest 0.1 kg with the participant clothed in a hospital gown or light-weight clothing. Height was only measured at baseline to the nearest 0.1 cm using a wall-mounted stadiometer. BMI was computed as kilograms of body weight divided by height in meters squared (kg/m2).
Physical Activity
Physical activity was objectively measured SenseWear Pro Armband (BodyMedia, Inc.), which has been shown to provide a valid measure of energy expenditure.(16, 17) Participants were provided the device to wear for a period of one week at 0, 6, 12 and 18 months. Data were considered valid for each assessment period and used for analyses if the device was worn for ≥10 hours per day for ≥4 days, which is similar to other trials that have previously evaluated objectively measured physical activity patterns.(8, 18, 19, 20, 21)
The device provided steps data for each minute. Thus, data were available for total steps·day−1. Moreover, because energy expenditure at each minute was available from the device, steps across each minute were able to be categorized as meeting the criteria for moderate-to-vigorous physical activity (MVPA; ≥3METs) or not meeting this criteria (NON-MVPA; <3 METs). Moreover, steps meeting the criteria for MVPA were grouped as being performed in bouts of at least 10 consecutive minutes (BOUT-MVPA) or not meeting the criteria of at least 10 consecutive minutes (NON-BOUT-MVPA). These categories of steps·day−1 (total, NON-MVPA, NON-BOUT-MVPA, BOUT-MVPA) were used for data analysis.
Energy Intake
Energy intake, expressed as kilocalories per day, was assessed using a food frequency questionnaire that participants were asked to complete at 0, 6, 12, and 18 months.(22, 23) This questionnaire requires the participant to report the frequency and amount of consumption of common food items, and this information is used to estimate energy intake.
Statistical Analyses
Statistical analyses were performed using SAS (version 9.4). The type I error rate was fixed at 0.05 (two-tailed). Furthermore, we used the Bonferroni adjustment to account for multiple comparisons.
Two grouping variables were created: one based on weight change from 0 to 18-months and the other based on weight change patterns from 0 to both 6- and 18-months. For change in weight from baseline to 18 months, participants were categorize as gaining weight (GAIN), achieving weight loss of <5% (WL<5%), achieving weight loss of 5 to <10% (WL<10%), or achieving weight loss of ≥10% (WL≥10%). These categories were selected based upon previous literature which suggests that health benefits can be observed with at least 5% weight loss(4) and the general acceptance of 10% weight loss being an important clinical target that has also been shown to be associated with reduced cardiovascular disease in the Look AHEAD trial.(24) Participants were also grouped based on whether they lost ≥10% of their baseline weight at 6 and 18 months. Thus, participants were categorized as NON-LOSS (weight loss <10% at both 6 and 18 months), LATE-LOSS (weight loss <10% at 6 months and ≥10% at 18 months), NON-MAINTAIN (weight loss ≥10% at 6 months and <10% at 18 months), or MAINTAIN (weight loss ≥10% at both 6 and 18 months).
Only participants with objective physical activity measured for at least one time point (0, 6, 12, or 18 months) were included in the analysis. At each time point, participants were considered to provide valid data if they met the following criteria: minimum of 4 full days with ≥10 hours wear time per day. Separate mixed effects models with 4 time points were fitted to the steps·day−1 for each of the following activity bouts: total, NON-MVPA, NON-BOUT-MVPA, BOUT-MVPA. Pairwise comparisons were performed at a significance level that was adjusted using the Bonferroni method, resulting in a type I error rate of 0.008 for each of the 6 pairwise comparisons among the 4 groups. The models included covariate adjustment for clinic, gender, and race (white: yes/no), with inference focusing on the grouping variable, time, and their interaction. The main effect for randomization group assignment was also examined in these models.
Separate mixed effects models with weight change as outcome were also fitted. Change in steps·day−1 were included for each of the following activity bouts: total, NON-MVPA, NON-BOUT-MVPA, BOUT-MVPA, as time-varying covariate in these models. Other covariates included clinic, gender, race (white: yes/no), and baseline measure of the steps·day−1 variable for each activity bouts.
RESULTS
Comparison Based on Categores of Weight Change at 18 Months
Only participants who provided measured weight at both 0 and 18 months were categorized, which resulted in 260 individuals included in this analysis. Baseline characteristics of this sample (n=260) are shown in Table 1, which is similar to the characteristics of this sample that have been previously reported.(8) Percent weight change at 18 months and its standard error was consistent with the weight loss categories (3.1±0.7% in GAIN, −3.2 ± 0.6% in WL<5%, −7.8±0.6% in WL<10%, and −17.0±0.5% in WL≥10%).
Steps data, expressed as steps·day−1, are presented as LS Means (95% confidence interval) and are shown in Table 2. When the main effect of randomization group assignment (STEP vs. SBWL) was added to these models examining the pattern of change in steps·day−1 (total steps·day−1, BOUT-MVPA steps·day−1, NON-BOUT-MVPA steps·day−1, or NON-MVPA steps·day−1) and whether there was a significant difference among weight loss category, the main effect of randomization group assignment was not significant in all models (all p’s >0.05).
Table 2.
Differences in steps per day of physical activity by weight change categories at 18 months [LS Means (95% confidence interval)].
| Physical Activity Variable | Weight Change Category Based On 18-Month Weight Loss | Assessment Periods (Steps per Day) | P-Values** | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Baseline | 6 Months | 12 Months | 18 Months | Time | Weight Change Category | Weight Change Category X Time | ||
|
| ||||||||
| Total steps·day−1 | GAIN (N=36 ) | 8134(7212, 9056) | 8603(7490, 9716)a | 7965(6815, 9114) | 7801(6549, 9053)a | <0.0001 | 0.0588 | <0.0001 |
| WL<5% (N= 55 ) | 7233(6444, 8022) | 9613(8681, 10545) | 8187(7217, 9157) | 7802(6782,8822)b | ||||
| WL<10% (N= 57 ) | 7869(7096, 8641) | 9852(8933, 10771) | 8602(7676, 9528) | 8612(7613, 9610) | ||||
| WL≥10% (N= 106 ) | 7280(6680, 7880) | 10576(9882,11270)a | 9456(8749, 10164) | 9822(9073,10571)a,b | ||||
|
| ||||||||
| NON-MVPA steps·day−1 | GAIN | 4259(3805, 4713) | 4415(3894, 4937) | 4213(3661, 4765) | 4242(3674, 4809) | 0.9423 | 0.2032 | 0.9715 |
| WL<5% | 3919(3532, 4306) | 3952(3515, 4390) | 3994(3528, 4460) | 4018(3554, 4482) | ||||
| WL<10% | 4278(3898, 4657) | 4126(3696, 4557) | 4157(3712, 4602) | 4153(3707, 4599) | ||||
| WL≥10% | 3914(3620, 4208) | 3802(3475, 4128) | 3775(3435, 4115) | 3831(3493, 4169) | ||||
|
| ||||||||
| NON-BOUT-MVPA steps·day−1 | GAIN | 2491(2088, 2895) | 2646(2222, 3071) | 2576(2147, 3006) | 2500(2046, 2954) | 0.0002 | 0.6600 | 0.1839 |
| WL<5% | 2228(1886, 2571) | 2692(2338, 3046) | 2264(1903, 2625) | 2125(1754, 2496) | ||||
| WL<10% | 2539(2203, 2875) | 2675(2327, 3022) | 2421(2078, 2764) | 2525(2163, 2887) | ||||
| WL≥10% | 2230(1971, 2489) | 2585(2320, 2850) | 2377(2112, 2642) | 2520(2245, 2795) | ||||
|
| ||||||||
| BOUT-MVPA steps·day−1 | GAIN | 1404(918, 1890) | 1496(671, 2322)a,b,d | 1272(498, 2047)a | 1075(210, 1941)a | <0.0001 | <0.0001 | <0.0001 |
| WL<5% | 1097(684, 1511) | 2990(2299, 3681)a,c | 1941(1286, 2596)b | 1735(1045, 2426)b | ||||
| WL<10% | 1058(653, 1463) | 3059(2358, 3761)d | 2040(1423, 2658)c | 1949(1269, 2629)c | ||||
| WL≥10% | 1131(816, 1447) | 4145(3634,4656)b,c | 3301(2837,3764)a,b,c | 3482(2982,3981)a,b,c | ||||
|
| ||||||||
| Energy Intake kcal·day−1 | GAIN | 1981(1709, 2253) | 1580 (1374, 1786) | 1570 (1364, 1776) | 1587 (1367, 1806) | <0.0001 | 0.9773 | 0.2378 |
| WL<5% | 1986 (1756, 2217) | 1531 (1366, 1696) | 1681 (1510, 1853) | 1589 (1410, 1768) | ||||
| WL<10% | 2177 (1954, 2400) | 1567 (1406, 1728) | 1612 (1448, 1776) | 1561 (1384, 1738) | ||||
| WL≥10% | 2175 (2006, 2343) | 1546 (1421, 1671) | 1543 (1417, 1669) | 1546 (1411, 1681) | ||||
indicates no significant difference between randomized groups (data not presented)
Note: Groups with the same superscript at the same assessment point are significantly different at α<0.008 (p-value of 0.05 adjusted using Bonferroni adjustment for 6 group comparisons at that time point.)
Weight Change Category Based On 18-Month Weight Loss
GAIN: Weight gain ≥0% of baseline weight
WL<5%: weight loss <5% of baseline weight
WL<10%: weight loss of 5% to <10% of baseline weight
WL≥10%: weight loss ≥10% of baseline weight
There was a significant Weight Loss Category by Time interaction (p<0.0001) for total steps·day−1. Post hoc analysis with Bonferroni’s adjustment for multiple comparisons indicated that WL≥10% had significantly more total steps·day−1 [9822 (9151, 10531)] compared to GAIN [7801 (6549, 9053)] and WL<5% [7802(6782, 8822)] (p<0.008). Total steps·day−1 for WL≥10% and WL<10% [8612(7613, 9610)] were not significantly different at 18 months, and GAIN, WL<5%, and WL<10% did not differ at 18 months.
There was a significant Weight Loss Category by Time interaction (p<0.0001) for BOUT-MVPA steps·day−1 across the 18 months. Post-hoc analysis showed that WL≥10% had more BOUT-MVPA steps·day−1 [3482(2982, 3981)] compared to GAIN [1075(210, 1941)], WL<5% [1735(1045, 2426)], and WL<10% [1949(1269, 2629)] (p≤0.008). GAIN, WL<5%, and WL<10% did not differ significantly from each other in BOUT-MVPA steps·day−1 at 18 months.
There was a significant Time effect (p=0.0002) for NON-BOUT-MVPA steps·day−1; however, there were no differences between weight loss categories. NON-MVPA steps·day−1 did not change across the 18 months, and there were no differences between the weight loss categories.
Data for energy intake was compared between the weight loss categories (Table 2). There was no significant difference in total energy intake (kcal·day−1) between these weight loss categories.
Comparison Based on Categories of Weight Change at 6 and 18 Months
Only participants who provided measured weight at 0, 6, and 18 months were categorized, which resulted in 258 individuals included in this analysis. Baseline characteristics of this sample (n=258) are shown in Table 1, and reflect the characteristics as previously reported.(8) Percent weight change and its standard error at 18 months was consistent with the weight loss categories (−1.8±0.5% in NON-LOSS, −13.5±1.2% in LATE-LOSS, −6.8±0.8% in NON-MAINTAIN, and −17.9±0.6% in MAINTAIN).
Steps data, expressed as steps·day−1, are presented as LS Means (95% confidence interval) and are shown in Table 3. When the main effect of randomization group assignment (STEP vs. SBWL) was added to these models examining the pattern of change in steps·day−1 (total steps·day−1, BOUT-MVPA steps·day−1, NON-BOUT-MVPA steps·day−1, or NON-MVPA steps·day−1) and whether there was a significant difference among weight loss category, the main effect of randomization group assignment was not significant in all models (all p’s >0.05).
Table 3.
Differences in steps per day of physical activity by weight change categories at 6 and 18 months [LS Means (95% confidence interval)].
| Physical Activity Variable | Weight Change Category Based On 6 and 18-Month Weight Loss* | Assessment Periods (Steps per Day) | P-Values** | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Baseline | 6 Months | 12 Months | 18 Months | Time | Weight Change Category | Weight Change Category X Time | ||
|
| ||||||||
| Total steps·day−1 | NON-LOSS (N=103 ) | 7572(6954, 8190) | 9074(8353, 9795)a | 8205(7460, 8949) | 7981(7192, 8771)a | <0.0001 | 0.0501 | <0.0001 |
| LATE-LOSS (N= 19) | 8241(6959, 9524) | 10579(9060, 12099) | 9327(7770, 10885) | 9776(8056, 11495) | ||||
| NON-MAINTAIN (N=44) | 8092(7233, 8952) | 10404(9400, 11407) | 8659(7635, 9683) | 8520(7421, 9618) | ||||
| MAINTAIN (N= 86) | 7094(6433, 7755) | 10600(9839,11360)a | 9508(8730, 10287) | 9850(9032,10668)a | ||||
|
| ||||||||
| NON-MVPA steps·day−1 | NON-LOSS | 4094(3792, 4397) | 4109(3770, 4449) | 4163(3806, 4520) | 4173(3813, 4533) | 0.6764 | 0.1010 | 0.8698 |
| LATE-LOSS | 4367(3736, 4998) | 4455(3742, 5167) | 4279(3534, 5024) | 4094(3324, 4864) | ||||
| NON-MAINTAIN | 4328(3905, 4750) | 4251(3779, 4722) | 4080(3591, 4569) | 4132(3641, 4622) | ||||
| MAINTAIN | 3825(3501, 4149) | 3668(3310, 4026) | 3675(3302, 4048) | 3776(3407, 4144) | ||||
|
| ||||||||
| NON-BOUT-MVPA steps·day−1 | NON-LOSS | 2322(2057, 2587) | 2576(2301, 2852) | 2349(2069, 2629) | 2307(2018, 2596) | 0.0017 | 0.1850 | 0.5059 |
| LATE-LOSS | 2550(1991, 3110) | 2859(2288, 3431) | 2626(2052, 3201) | 3038(2420, 3655) | ||||
| NON-MAINTAIN | 2679(2305, 3052) | 2925(2545, 3305) | 2551(2173, 2930) | 2539(2143, 2934) | ||||
| MAINTAIN | 2164(1879, 2448) | 2528(2239, 2818) | 2326(2035, 2617) | 2421(2124, 2719) | ||||
|
| ||||||||
| BOUT-MVPA steps·day−1 | NON-LOSS | 1180(853, 1508) | 2368(1840, 2896)a | 1726(1235, 2218)a | 1543(1012, 2073)a | <0.0001 | <0.0001 | <0.0001 |
| LATE-LOSS | 1343(665, 2020) | 3277(2096, 4458) | 2447(1405, 3490) | 2701(1508, 3894) | ||||
| NON-MAINTAIN | 1092(637, 1546) | 3225(2466, 3983) | 2031(1353, 2710)b | 1869(1120, 2617)b | ||||
| MAINTAIN | 1093(743, 1443) | 4339(3774, 4904)a | 3496(2986, 4006)a,b | 3645(3098,4192)a,b | ||||
|
| ||||||||
| Energy Intake kcal·day−1 | NON-LOSS | 2064(1893, 2235) | 1594(1466, 1722) | 1651(1517, 1786) | 1581(1442, 1720) | <0.0001 | 0.1613 | 00935 |
| LATE-LOSS | 2322(1946, 2698) | 1594(1466, 1722) | 1734(1466, 2002) | 1725(1428, 2023) | ||||
| NON-MAINTAIN | 2094(1843, 2344) | 1484(1312, 1656) | 1573(1396, 1750) | 1570(1377, 1763) | ||||
| MAINTAIN | 2109(1924, 2293) | 1433(1300, 1565) | 1479(1342, 1616) | 1481(1335, 1626) | ||||
indicates no significant difference between randomized groups (data not presented)
Note: Groups with the same superscript at the same assessment point are significantly different at α<0.008 (p-value of 0.05 adjusted using Bonferroni adjustment for 6 group comparisons at that time point.)
Weight Change Category Based On 6 and 18-Month Weight Loss
NON-LOSS: <10% weight loss at both 6 and 18 months
NON-MAINTAIN: ≥10% weight loss at 6 months and <10% weight loss at 18 months
LATE-LOSS: 6 month weight loss <10% & 18 month weight loss ≥10%
MAINTAIN: ≥10% weight loss at both 6 and 18 months
There was a significant Weight Loss Category by Time interaction (p<0.0001) for total steps·day−1. Post hoc analysis with Bonferroni’s adjustment for multiple comparisons indicated that at 18 months MAINTAIN had significantly higher total steps·day−1 [9850 (9032, 10668)] than NON-LOSS [7981 (7192, 8771)], with neither LATE-LOSS [9776 (8056, 11495)] nor NON-MAINTAIN [8520 (7421, 9618)] differing from the other categories.
There was a significant Weight Loss Category by Time interaction (p<0.0001) for BOUT-MVPA steps·day−1 across the 18 months. Post-hoc analysis showed that at 18 months MAINTAIN had more BOUT_MVPA steps·day−1 [3645 (3098, 4192)] compared to the NON-LOSS [1543 (1012, 2073)] and NON-MAINTAIN [1869 (1120, 2617)], but not LATE-LOSS [2701 (1508, 3894)] (p≤0.008). No other weight loss category comparisons were significantly different from each other in BOUT-MVPA steps·day−1 at 18 months.
There was a significant Time effect (p=0.0017) for NON-BOUTMVPA steps·day−1; however, there were no differences between weight loss categories. NON-MVPA steps·day−1 did not change across the 18 months, and there were no differences between the weight loss categories.
Data for energy intake was compared between the weight loss categories (Table 3). There was no significant difference in total energy intake (kcal·day−1) between these weight loss categories.
Association Between Steps per Day and Weight Loss
Data were also analyzed to examine the association between steps·day−1 and weight loss, with separate analysis performed for total steps·day−1, BOUT-MVPA steps·day−1, NON-BOUT-MVPA steps·day−1, or NON-MVPA steps·day−1. Within these analyses steps·day−1 was consider a time varying covariate. After controlling for randomization group X time interaction, clinic (Pittsburgh vs. North Carolina), sex, ethnicity, and baseline steps steps·day−1 the analysis of total steps·day−1 showed a significant association with weight change (kg) across the 18-month intervention period (β= −0.00021, p=0.0003), suggesting that there was an additional 0.21 kg of weight loss with each additional 1,000 total steps·day−1. The analysis was repeated for BOUT-MVPA steps·day−1 and showed a significant association with weight change (kg) across the 18-month intervention period (β= −0.00033, p<0.0001), suggesting that there was an additional 0.33 kg of weight loss with each additional 1,000 BOUT-MVPA steps·day−1. Neither NON-BOUT-MVPA steps·day−1 (β= −0.00019, p=0.2153) or NON-MVPA steps·day−1 (β=0.00013, p=0.3009) were significantly associated with absolute weight change (kg) across the 18-month intervention period. These analyses were repeated replacing absolute weight change (kg) with percent weight change, and similar findings were observed (data not shown).
CONCLUSIONS
Physical activity has previously been shown to be associated with improved weight loss in comprehensive behavioral weight loss interventions, with the volume of physical activity typically expressed as time or energy expenditure.(1) This current report expands the scientific literature in this area and provides data on physical activity, expressed as steps, and their association with weight change across an 18-month behavioral weight loss intervention. The results show that those individuals achieving ≥10% weight loss at 18 months were engaging in approximately 10,000 total steps·day−1, which is consistent with a common public health recommendation for physical activity.
The results of this study are important because they provide additional insight into physical activity recommendations that may be important to facilitate weight loss success. Others have reported the association between physical activity expressed as energy expenditure from doubly-labeled water(25) and self-report.(6, 7, 10, 11, 12) Minutes of MVPA have also been shown to be associated with enhanced weight loss within a behavioral weight loss intervention.(6, 7, 9) Jakicic et al.(8) have reported that the pattern of minutes of MVPA may be important when determining the association with weight loss within a behavioral weight loss intervention. Thus, this study further contributes to this body of literature and suggests that the pattern of physical activity expressed as steps·day−1 is associated with enhanced weight loss within a behavioral weight loss intervention. These results suggest that the target physical activity expressed as steps·day−1 is approximately 10,000 with approximately 3,500 of these steps achieved at an intensity consistent with MVPA and in bouts of at least 10 minutes in duration. Assuming that 1 mile of walking is equivalent to 2,000 steps, and assuming a walking pace of 20 minutes per mile (3 miles per hour pace), this would suggest the need for approximately 35 minutes per day of MVPA performed in bouts of at least 10 minutes plus an additional 6,500 steps·day−1 of non-structured forms of physical activity. These data may have important public health implications when encouraging adults to engage in physical activity that is monitored as steps·day−1, and also implies the importance of intensity and duration when recommending the accumulation of steps of physical activity to impact body weight. These findings also have important translational implications for research, clinical and public health sectors which may further inform physical activity recommendations for long-term weight loss and weight management.
The public health recommendation for physical activity is to engage in at least 150 minutes per week of MVPA. Tudor-Locke et al. reported that individuals who attained 150 minutes per week of physical activity were taking an average of 7,000 steps·day−1.(13) The data from this study suggest that this amount of physical activity may not be sufficient to enhance long-term weight loss within the context of a behavioral weight loss intervention. In the current study, adults who successfully lost at least 10% of their baseline body weight by 18 months were engaging on average approximately 10,000 steps·day−1 at 6, 12, and 18 months (see Table 2). Moreover, adults who successfully lost at least 10% of their baseline weight at 6 months and were able to maintain at least this magnitude of weight loss at 18 months were also engaging in approximately 10,000 at 6, 12, and 18 months (see Table 3).
The finding of this study should be considered within the potential limitations. This is a secondary analysis of data from a randomized clinical trial that was not designed to empirically examine the magnitude, intensity, and duration of bouts of steps of physical activity that were associated with weight loss within the context of a behavioral weight loss intervention. Thus, we are unable to completely isolate the pattern of steps of physical activity from total physical activity or from the contribution of diet on weight loss. Thus, these results need confirmation in a properly designed and statistically powered randomized study. Moreover, while physical activity, including steps, was assessed objectively with a device shown to provide a valid measure of physical activity, it is possible that the data collected during one week periods at 0, 6, 12, and 18 months was not representative of all physical activity across the entire 18-month intervention. It is also possible that not all forms of physical activity were accurately measured with the device used in this study, resulting in the estimates of steps to be under- or over-estimated.
Within this study energy intake was assessed and no significant differences were observed between the weight loss categories (see Tables 2 and 3), despite these categories representing different magnitudes of weight loss. However, it is unlikely that the differences in steps·day−1 accounted for all of the weight loss difference across these categories, with the results suggesting that an increase of 1,000 total or BOUT-MVPA steps·day−1 accounted for an enhanced weight loss of 0.22 kg and 0.33 kg, respectively. Thus, there may have been limitations with the use of a food frequency questionnaire to assess energy intake, which may have result in self-reporting bias and an inaccurate quantification of energy intake. Thus, the lack of a difference in energy intake between the weight loss categories (Table 2 and 3) may be influenced by the limitations of using a food frequency questionnaire.
An additional limitation of this study is that there were participants who were initially randomized to this study who were not included within these secondary analyses (see Figure 1). These participants were excluded due to missing weight loss data that did not allow for them to be placed into one of the weight loss categories for analysis. It is unclear whether the results of this secondary analysis would have differed if these additional participants would have provided data and been able to be included in the analysis and results presented here.
Results support the recommendation of accumulating 10,000 steps·day−1, with approximately 3,500 of these steps·day−1 be performed at a moderate-to-vigorous intensity in bouts of at least 10 minutes, to enhance weight loss in response to a behavioral weight loss intervention. While these results have implications that inform public health recommendations for physical activity, confirmation of these findings is needed with properly designed clinical trials.
What is already known about this subject
Physical activity is a key contributor in weight loss interventions and contribute additional initial weight loss (within 6 months of treatment) and is associated with enhanced long-term weight loss maintenance and prevention of weight regain.
The dose of moderate-to-vigorous physical activity associated with enhanced weight loss has typically been described in units of minutes or energy expenditure.
What this study adds
Few studies have examined the number or pattern of physical activity steps that are associated with enhanced weight loss within the context of a behavioral intervention. This study shows that accumulating 10,000 steps per day, with approximately 3,500 of these steps performed at a moderate-to-vigorous intensity and in bouts of at least 10 continuous minutes, is associated with enhanced 18-month weight loss in response to a behavioral intervention in adults.
Acknowledgments
We recognize the contribution of the staff and students at the University of Pittsburgh and the University of North Carolina at Chapel Hill who received salary support or volunteered their effort on this project.
FUNDING: This study was supported by grant R01 HL084400 from the National Institutes of Health and the National Heart, Lung, and Blood Institute. The funding source (National Institutes of Health) was invited to have a representative present during Data and Safety Monitoring Board meetings, but otherwise did not have a role in the study design, conduct of the study, data analysis, or interpretation of the study findings.
Footnotes
CLINICAL TRIAL REGISTRATION: clinicaltrials.gov: NCT00714168
DISCLOSURES: Dr. Tate received an honorarium for serving on the Scientific Advisory Board for Weight Watchers International, and was the Principal Investigator on a grant awarded to the University of North Carolina at Chapel by Weight Watchers International. Dr. Jakicic received an honorarium for serving on the Scientific Advisory Board for Weight Watchers International and was a co-investigator on a grant award to the University of Pittsburgh by HumanScale and a grant awarded to the University of Pittsburgh by Weight Watchers International.
References
- 1.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. ACSM position stand on appropriate intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;42:459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 2.Haskell WL, Lee I-M, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 3.Jakicic JM, Clark K, Coleman E, Donnelly JE, Foreyt J, Melanson E, et al. American College of Sports Medicine Position Stand: Appropriate Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults. Med Sci Sports Exerc. 2001;33:2145–2156. doi: 10.1097/00005768-200112000-00026. [DOI] [PubMed] [Google Scholar]
- 4.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63:2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 5.National Institutes of Health National Heart Lung and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults - The Evidence Report. Obes Res. 1998;6(suppl 2) [PubMed] [Google Scholar]
- 6.Jakicic JM, Marcus BH, Gallagher KI, Napolitano M, Lang W. Effect of exercise duration and intensity on weight loss in overweight, sedentary women. A randomized trial. JAMA. 2003;290:1323–1330. doi: 10.1001/jama.290.10.1323. [DOI] [PubMed] [Google Scholar]
- 7.Jakicic JM, Marcus BH, Lang W, Janney C. Effect of exercise on 24-month weight loss in overweight women. Arch Int Med. 2008;168:1550–1559. doi: 10.1001/archinte.168.14.1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jakicic JM, Tate DF, Lang W, Davis KK, Polzien K, Neiberg R, et al. Objective physical activity and weight loss in adults: The Step-Up randomized clinical trial. Obesity. 2014;22:2284–2292. doi: 10.1002/oby.20830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jakicic JM, Winters C, Lang W, Wing RR. Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women: a randomized trial. JAMA. 1999;282:1554–1560. doi: 10.1001/jama.282.16.1554. [DOI] [PubMed] [Google Scholar]
- 10.Jeffery RW, Wing RR, Sherwood NE, Tate DF. Physical activity and weight loss: Does prescribing higher physical activity goals improve outcome? Am J Clin Nutr. 2003;78:684–689. doi: 10.1093/ajcn/78.4.684. [DOI] [PubMed] [Google Scholar]
- 11.Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. Am J Clin Nutr. 1997;66:239–246. doi: 10.1093/ajcn/66.2.239. [DOI] [PubMed] [Google Scholar]
- 12.Tate DF, Jeffery RW, Sherwood NE, Wing RR. Long-term weight losses associated with prescription of higher physical activity goals. Are higher levels of physical activity protective against weight regain? Am J Clin Nutr. 2007;85:954–959. doi: 10.1093/ajcn/85.4.954. [DOI] [PubMed] [Google Scholar]
- 13.Tudor-Locke C, Leonardi C, Johnson WD, Katzmarzyk PT, Church TS. Accelerometer steps/day translation of moderate-to-vigorous activity. Prev Med. 2011;2011:1. doi: 10.1016/j.ypmed.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 14.Piwek L, Ellis DA, Andrews S, Joinson A. The rise of consumer health wearable: promises and barriers. PLoS Med. 2016;13:e1001953. doi: 10.1371/journal.pmed.1001953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jakicic JM, Tate D, Davis KK, Polzien K, Rickman AD, Erickson K, et al. Effect of a stepped-care intervention approach on weight loss in adults: The Step-Up Study Randomized Trial. JAMA. 2012;307:2617–2626. doi: 10.1001/jama.2012.6866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jakicic JM, Marcus MD, Gallagher KI, Randall C, Thomas E, Goss FL, et al. Evaluation of the SenseWear Pro Armband ™ to assess energy expenditure during exercise. Med Sci Sports Exerc. 2004;36:897–904. doi: 10.1249/01.mss.0000126805.32659.43. [DOI] [PubMed] [Google Scholar]
- 17.St-Onge M, Mignault D, Allison DB, Rabasa-Lhoret R. Evaluation of a portable device to measure daily energy expenditure in free-living adults. Am J Clin Nutr. 2007;85:742–749. doi: 10.1093/ajcn/85.3.742. [DOI] [PubMed] [Google Scholar]
- 18.Jakicic JM, Davis KK, Rogers RJ, King WC, Marcus MD, Helsel D, et al. Effect of wearable technology combined with a lifestyle intervention on long-term weight loss in the IDEA Study: a randomized clinical trial. JAMA. 2016;316:1161–1171. doi: 10.1001/jama.2016.12858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jakicic JM, Gregg E, Knowler W, Kelley DE, Lang W, Miller GD, et al. Physical activity patterns of overweight and obese individuals with type 2 diabetes in the Look AHEAD Study. Med Sci Sports Exerc. 2010;42:1995–2005. doi: 10.1249/MSS.0b013e3181e054f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Masse LC, Fuemmeler BF, Anderson CB, Matthews CE, Trost SG, Catellier DJ, et al. Accelerometer data reduction: a comparison of four reduction algorithms on select outcome variables. Med Sci Sports Exerc. 2005;37:S544–S554. doi: 10.1249/01.mss.0000185674.09066.8a. [DOI] [PubMed] [Google Scholar]
- 21.Miller GD, Jakicic JM, Rejeski WJ, Whitt-Glover M, Lang W, Walkup MP, et al. Effect of varying accelerometry criteria on physical activity: the Look AHEAD Study. Obesity. 2013;21:32–44. doi: 10.1038/oby.2012.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Block G, Hartman AM, Dresser CM, Carol MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;108:161–175. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 23.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–1335. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 24.The Look AHEAD Research Group. Association of the magniture of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2016;4:913–921. doi: 10.1016/S2213-8587(16)30162-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schoeller DA, Shay K, Kushner RF. How much physical activity is needed to minimize weight gain in previously obese women. Am J Clin Nutr. 1997;66:551–556. doi: 10.1093/ajcn/66.3.551. [DOI] [PubMed] [Google Scholar]