Abstract
Background
Emerging data from animal and human studies suggest that traffic-related air pollution adversely affects early pregnancy outcomes; however evidence is limited.
Objective
We examined whether residential proximity to major roadways and traffic, as proxies for traffic-related air pollution, are associated with in vitro fertilization (IVF) outcomes.
Methods
This analysis included 423 women enrolled in the Environment and Reproductive Health (EARTH) Study, a prospective cohort study, who underwent 726 IVF cycles (2004–2017). Using geocoded residential addresses collected at study entry, we calculated the distance to nearest major roadway and the traffic density within a 100 m radius. IVF outcomes were abstracted from electronic medical records. We used multivariable generalized linear mixed models to evaluate the associations between residential proximity to major roadways and traffic density and IVF outcomes adjusting for maternal age, body mass index, race, education level, smoking status, and census tract median income.
Results
Closer residential proximity to major roadways was statistically significantly associated with lower probability of implantation and live birth following IVF. The adjusted percentage of IVF cycles resulting in live birth for women living ≥400 m from a major roadway was 46% (95% CI 36, 56%) compared to 33% (95% CI 26, 40%) for women living <50 m (p-for-comparison, 0.04). Of the intermediate outcomes, there were suggestive associations between living closer to major roadways and slightly higher estradiol trigger concentrations (p-trend=0.16) and lower endometrial thickness (p-trend=0.06). Near-residence traffic density was not associated with outcomes of IVF.
Conclusion
Closer residential proximity to major roadways was related to reduced likelihood of live birth following IVF.
Keywords: air pollution, assisted reproduction, fertility, in vitro fertilization, traffic
Introduction
Traffic emissions are a major source of local variability in air pollution levels (EEA 2016; Singh et al. 2014), with the highest concentrations and risk of exposure occurring near major roadways (Karner et al. 2010). Motor vehicle emissions represent a complex mixture of air pollutants, including carbon dioxide (CO2), carbon monoxide (CO), nitrogen oxides (NOx), hydrocarbons, volatile organic compounds (VOCs), and particulate matter (HEI 2010). Each of these components, along with their secondary by-products, such as ozone and secondary aerosols, can adversely affect health (HEI 2010). Of the motor vehicle generated air pollutants, diesel exhaust particles (DEPs) account for a high percentage of the particles emitted in many towns and cities (UNEP 1994) and are almost exclusively found in the submicrometer fraction. While DEPs represent a complex and variable mixture of components, their content of elemental and organic carbon, polycyclic aromatic hydrocarbons, and metals have received the most attention as the components responsible for DEPs negative health effects (Sydbom et al. 2001). Because the mixture of traffic-related air pollutants can be difficult to measure and model, many epidemiologic studies rely on measures of traffic (e.g., proximity to major roads and cumulative traffic density within a buffer) as surrogates of exposure.
Over the past decade, chronic exposure to traffic-related air pollution has become increasingly recognized as an important risk factor for adverse pregnancy outcomes (Stieb et al. 2016) including preterm birth (Yorifuji et al. 2011), gestational diabetes (Robledo et al. 2015), preeclampsia (Wu et al. 2009), restricted fetal growth (Fleisch et al. 2015), and low birth weight (Brauer et al. 2008). The proposed biological mechanisms mediating air pollution’s effect on these later pregnancy and birth outcomes such as increased oxidative stress (Moller et al. 2014), systemic inflammation (Panasevich et al. 2009), endothelial dysfunction (Wauters et al. 2013), and DNA damage (Risom et al. 2005) could also affect earlier pregnancy outcomes such as fertilization, early embryo development, and implantation. However, limited research has been conducted to this regard.
The objective of this study was to utilize data from an ongoing prospective cohort of couples undergoing in vitro fertilization (IVF) to explore the relationship between proxies of traffic-related air pollution and female reproductive outcomes using a unique model of human reproduction where clinically relevant, yet otherwise unobservable outcomes, such as fertilization and implantation, can be studied.
Methods
Study population
Study participants were recruited into the Environment and Reproductive Health (EARTH) Study between November 2004 and July 2016 from patients presenting for infertility evaluation and treatment at the Massachusetts General Hospital (MGH) Fertility Center. All women between 18 and 46 years of age at enrollment were eligible to participate. Approximately 60% of those contacted by the research nurses participated in the study. Upon enrollment into the study, all participants provided their residential address for reimbursement purposes. Women were then followed through each of their subsequent infertility treatment cycles until discontinuation of treatment or live birth.
Out of the total number of women enrolled in EARTH (n=867) only women who had completed at least 1 IVF cycle by March 2017 and were not undergoing controlled ovarian stimulation with the sole purpose of oocyte banking or egg donation were eligible (n=443). From the initial 443 eligible EARTH women we excluded 20 women whose primary residence was outside of Massachusetts leaving a final sample size of 423 women and 726 IVF cycles (see Figure S1). Twenty-two of the 423 women re-enrolled in the EARTH study after having a live birth. Of these, only 4 women had moved since their original enrollment. In these instances, the women’s new addresses were applied to all cycles initiated after re-enrollment. The EARTH study was approved by the Human Studies Institutional Review Boards of the MGH and the Harvard T.H. Chan School of Public Health. All study participants signed an informed consent after the study procedures were explained by a research nurse.
Traffic-related air pollution exposures
The residential address of each woman was geocoded using ArcGIS and linked to an official state-maintained street transportation dataset which was downloaded from the Massachusetts Department of Transportation through the Office of Geographic Information (MassGIS 2014). This dataset represents all the public and the majority of the private roadways in Massachusetts as of December 2013, including designations for interstates and highways and traffic count information. MassGIS classifies the following as major roadways: limited access highways, multi-lane highways (not limited access), other numbered routes, and major roads that are arterials and collectors. Using ArcGIS, we measured the Euclidian distance in meters from each geocoded residence to nearest major roadway. In the MassGIS data, annual average daily traffic (AADT) count information is reported by segment of road. Near-residence traffic density was defined as the length in kilometers of all roads within 100 m of a residence, multiplied by the annual average daily traffic counts for those roads (vehicles/day). Since not all segments of all roads in Massachusetts have traffic count information, it was possible for a woman to have no road segments within 100m of her residence with traffic count information.
Outcome Assessment
For fresh IVF cycles, patients underwent one of three stimulation protocols as clinically indicated: 1) luteal-phase GnRH agonist protocol; 2) follicular-phase GnRH-agonist/Flare protocol; or 3) GnRH-antagonist protocol. Patients were monitored during gonadotropin stimulation for serum estradiol, follicle size measurements and counts, and endometrial thickness. Human chorionic gonadotropin (hCG) was administered approximately 36 hours before the scheduled oocyte-retrieval procedure to induce oocyte maturation. Couples underwent IVF with conventional insemination or intra-cytoplasmic sperm injection (ICSI) as clinically indicated. The nuclear maturity of oocytes was determined before ICSI but not before conventional insemination/IVF. Embryologists classified oocytes as germinal vesicle, metaphase I, metaphase II (MII) or degenerated. Embryologists determined fertilization 17–20 hours after insemination as the number of oocytes with two pronuclei (2PN). The procedures regarding the timing and grading of embryo quality have varied during the follow-up of EARTH patients and thus are not included as an outcome for analysis.
For cryo-thaw cycles or donor egg recipient cycles, patients underwent either the standard endometrial preparation protocol or the resistant endometrium protocol that involves a longer low-dose estradiol period. In cryo-thaw cycles, on day 18 of the standard protocol, patients underwent an ultrasound to determine sufficient endometrial development. If the lining was ≥6 mm then intramuscular progesterone injections (or in very rare instances progesterone vaginal suppositories) began and embryo transfer was scheduled for day 24. In donor egg recipient cycles, patients were assessed for sufficient endometrial development around day 18, progesterone began on the day of donor egg retrieval, and embryo transfer occurred 6 days later (on day 5 of embryonic life).
Following embryo transfer, all clinical outcomes were assessed identically across fresh, cryo-thaw, and donor-egg recipient cycles. Specifically, successful implantation was defined as a serum β-hCG level >6 mIU/mL typically measured 17 days (range 15–20 days) after egg retrieval, clinical pregnancy as the presence of an intrauterine pregnancy confirmed by ultrasound at 6 weeks gestation, and live birth as the birth of a neonate on or after 24 weeks gestation.
Covariate Assessment
At enrollment, height and weight were measured by a trained research nurse to calculate body mass index (BMI) (kg/m2) and data on demographics, medical history, and lifestyle characteristics was collected on a brief, nurse-administered questionnaire. Participants also completed a detailed take-home questionnaire with additional questions on lifestyle factors, reproductive health, and medical history. Census tract level median family income in the past 12 months (in 2011 inflation-adjusted dollars) from the American Community Survey 2007–2010 was used as a proxy for socioeconomic status. Clinical information including infertility diagnosis and protocol type was abstracted from electronic medical records.
Statistical Analysis
Women were classified into categories of residential proximity to major roadways based on cut points drawn to reflect the exponential-type pattern of spatial decay observed for some components of traffic-related air pollution (Zhou and Levy 2007) and the distribution of this exposure in our cohort (e.g. <50, 50–99, 100–199, 200–399, ≥400m). A sizable proportion of women had no traffic count data recorded for the road segments within 100m of their home and as such their near distance traffic density was missing. Therefore, we classified women into a zero or “missing” traffic density group and then quartiles for the remaining women with available near-residence traffic density information. Descriptive statistics were calculated across categories of distance to major roadway for demographic and initial cycle characteristics. To test for differences across categories, Kruskal-Wallis tests were used for continuous variables and chi-squared tests (or Fisher’s exact tests when cell counts were <5) were used for categorical variables.
Multivariate generalized linear mixed models with random intercepts were used to evaluate the association between distance to major roadways and traffic density and IVF outcomes while accounting for within-person correlations in outcomes. These models generate unbiased estimates in the presence of an unbalanced design (e.g. different number of cycles per woman) when data is missing at random and the model is correctly specified (Fitzmaurice et al. 2004). A normal distribution and an identity link function were specified for peak estradiol and endometrial thickness (both normally distributed), a Poisson distribution and a log link function were specified for oocyte counts, and binomial distribution and logit link function were specified for the clinical outcomes. Tests for trend across categories were conducted using a variable with the median exposure level in each group. All results are presented as population marginal means, at the average value of all the covariates (Searle et al. 1980).
As a secondary analysis, we examined the possible non-linear relation between distance to major roadways and residential traffic density to the odds of live birth non-parametrically with the restricted cubic splines (Durrleman and Simon 1989). All models were specified with a binomial distribution and logit link function and adjusted for age, BMI, race, and smoking status, education level and census tract median income. The reference point for the spline was set to the mean value in the population and the macro was allowed to choose up to 3 knots. The maximum value for the x-axis was set at the 95th percent of the distribution. For the analysis of residential traffic density, models were run with and without inclusion of women who had no traffic count data recorded for the road segments within 100m of their home.
Confounding was evaluated using prior knowledge and descriptive statistics from our cohort through the use of directed acyclic graphs (Weng et al. 2009). Variables retained in the final multivariable models were maternal age, race, BMI, education level, smoking status, and census tract median income. Fully-adjusted models were run both with and without adjusting for nulliparity and nulligravity since adjusting for reproductive history might lead to overadjustment if residential distance to roadways is related to the inability to carry a pregnancy to term which could manifest as nulliparity (Howards et al. 2007; Weinberg 1993). Sensitivity analyses were conducted using other buffer sizes for the residential traffic density exposure (50m and 200m). Effect modification by specific characteristics such as age, smoking status, race, infertility diagnosis, cycle type (e.g. fresh, cryo-thaw, donor), season the IVF cycle began (April-September vs. October-March), and insemination method were tested using cross-product terms in the final multivariate models. A p-value for interaction of <0.1 was considered suggestive; however for all other analyses a p-value<0.05 was considered statistically significant. Several sensitivity analyses were conducted to evaluate the robustness of our results including restricting our analyses to 1) only the first IVF cycle per woman, 2) only non-current smokers, 3) only autologous fresh IVF cycles, and 4) only cycles with embryo transfer. SAS version 9.4 (SAS Institute, Cary, NC, USA) was used for all statistical analyses.
Results
Women in the EARTH cohort were, on average, 35.3 years of age (range: 21 to 47 years) at the start of their first in-study IVF cycle and had a BMI of 24.2 kg/m2 (range: 16.1 to 45.8 kg/m2) at enrollment. The majority of women were white (83%), never smokers (73%), with a college education or higher (93%). Of the 726 IVF cycles included in the study, 601 (83%) were fresh IVF cycles, 97 (13%) were autologous cryo-thaw cycles, and 28 (4%) were donor egg-recipient cycles. A total of 650 (90%) of the initiated cycles had at least one embryo transferred with 401 (55%) resulting in implantation, 349 (48%) in clinical pregnancy, and 284 (39%) in live birth (see Figure S2). Women were followed for a total of 1 (55%), 2 (26%), 3 (14%), or 4+ (5%) IVF cycles (with a maximum of 7 cycles).
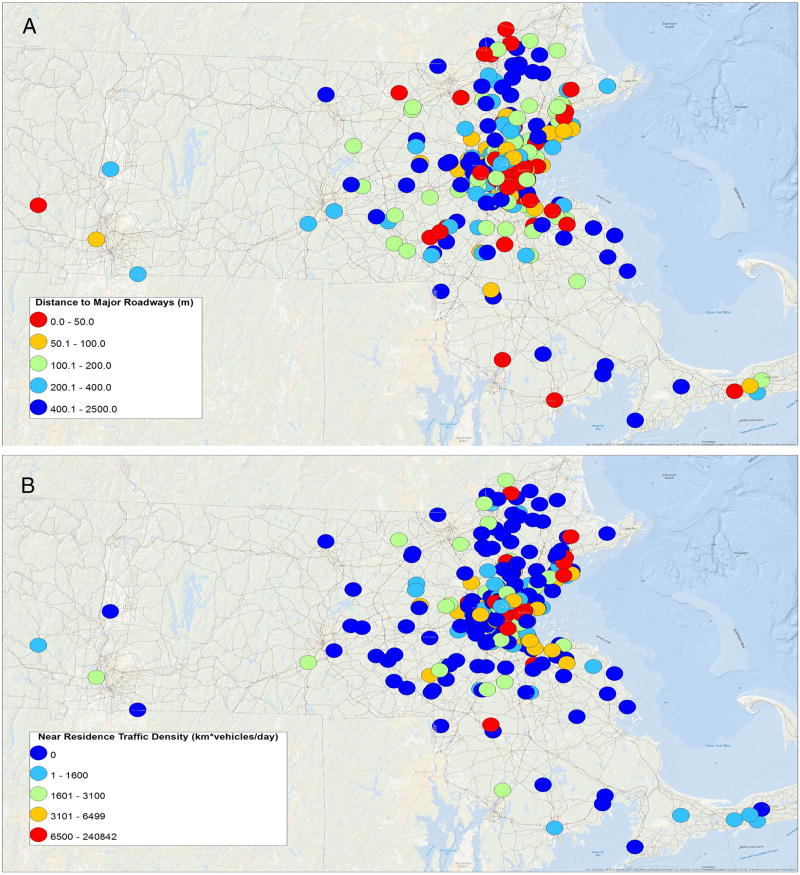
Both residential distance to major roadway and near-residence traffic density were highly skewed having a median (range) of 105 m (1 to 2410 m) and 1281 km*vehicles per day (range 0 to 240,842 km*vehicles per day), respectively. The geographic distribution of residential proximity to major roadways and traffic are shown in Figure 1 A & B. Women who lived closer to major roadways were slightly less likely to be white (p-value=0.20), have a college education or higher (p-value=0.05), and reside in a census tract with slightly lower median income (p-value=0.02) (Table 1); however differences across categories were small and most were only marginally statistically significant. All other demographic and initial cycle-level characteristics were similar across categories of distance to major roadways.
Figure 1.
Geographical distribution of residential distance to (A) nearest major roadway and (B) traffic density within 100m of residence among 423 women (427 unique addresses) enrolled in the Environmental and Reproductive Health Study (2004–2017).
Table 1.
Baseline characteristics of 423 women in Environment and Reproductive Health (EARTH) Study (2004–2017) by category of distance from residential address to nearest major roadway.
| Categories of Residential Distance to Major Roadway
|
||||||
|---|---|---|---|---|---|---|
| Range, m | <50 | 50–99 | 100–199 | 200–399 | ≥400 | |
| Number of women | 105 | 99 | 84 | 70 | 65 | p-valuea |
| Personal Characteristics | ||||||
| Age, years | 35.4 ± 4.3 | 35.2 ± 4.0 | 35.3 ± 3.8 | 35.0 ± 3.5 | 35.5 ± 4.6 | 0.89 |
| BMI, kg/m2 | 24.4 ± 4.6 | 24.1 ± 4.3 | 24.0 ± 4.7 | 24.0 ± 4.1 | 24.8 ± 4.2 | 0.45 |
| Ever smoker, n (%) | 29 (27.6) | 27 (27.3) | 24 (28.6) | 17 (24.3) | 16 (24.6) | 0.97 |
| White/Caucasian, n (%) | 90 (85.7) | 79 (79.8) | 65 (77.4) | 57 (81.4) | 59 (90.8) | 0.20 |
| Education Level, n (%) | <0.001 | |||||
| Less than college | 12 (11.4) | 10 (10.1) | 0 (0.0) | 3 (4.3) | 5 (7.7) | |
| College degree | 41 (39.1) | 32 (32.3) | 41 (48.8) | 25 (35.7) | 26 (40.0) | |
| Graduate degree | 52 (49.5) | 57 (57.6) | 43 (51.2) | 42 (60.0) | 34 (52.3) | |
| Census Tract Median Incomeb, $ | 105,232 ± 52,200 | 105,239 ± 47,378 | 101,721 ± 35,597 | 105,856 ± 37,192 | 118,366 ± 35,818 | 0.02 |
| Currently working, n (%) | 85 (94.4) | 84 (94.4) | 74 (96.1) | 60 (98.4) | 55 (93.2) | 0.69 |
| Residential Traffic Density, Km*vehicles/day | 19449 ± 40520 | 7613 ± 19931 | 221 ± 504 | 418 ± 701 | 357 ± 655 | <0.001 |
| Initial IVF Cycle Characteristics | ||||||
| Nulligravid, n (%) | 62 (59.1) | 61 (61.6) | 56 (66.7) | 40 (57.1) | 35 (53.9) | 0.56 |
| Nulliparous, n (%) | 92 (87.6) | 92 (92.9) | 74 (88.1) | 55 (78.6) | 54 (83.1) | 0.08 |
| Infertility diagnosis, n (%) | 0.68 | |||||
| Female factor | 38 (36.2) | 29 (29.3) | 31 (36.9) | 24 (34.3) | 18 (27.7) | |
| Male factor | 27 (25.7) | 35 (35.4) | 23 (27.4) | 21 (30.0) | 26 (40.0) | |
| Unexplained | 40 (38.1) | 35 (35.4) | 30 (35.7) | 25 (35.7) | 21 (32.3) | |
| Treatment Protocol, n (%) | 0.90 | |||||
| Antagonist or Flare | 22 (21.0) | 21 (21.2) | 22 (26.2) | 16 (22.9) | 16 (24.6) | |
| Luteal Phase Agonist | 78 (74.3) | 71 (71.7) | 55 (65.5) | 47 (67.1) | 43 (66.2) | |
| Egg Donor or Cryo Cycle | 5 (4.8) | 7 (7.1) | 7 (8.4) | 7 (10.0) | 6 (9.2) | |
| Method of Inseminationc, n (%) | 0.81 | |||||
| Conventional | 45 (48.9) | 41 (48.2) | 41 (56.2) | 32 (53.3) | 26 (47.3) | |
| ICSI | 47 (51.1) | 44 (51.8) | 32 (43.8) | 28 (46.7) | 26 (52.7) | |
| Embryo Transfer Day, n (%) | 0.60 | |||||
| No embryos transferred | 14 (13.5) | 10 (10.1) | 7 (8.4) | 9 (12.9) | 5 (7.7) | |
| Day 2 | 3 (2.9) | 2 (3.0) | 5 (6.0) | 4 (5.7) | 6 (9.2) | |
| Day 3 | 41 (39.4) | 40 (40.4) | 38 (45.8) | 34 (48.6) | 27 (41.5) | |
| Day 5 | 41 (39.4) | 39 (39.4) | 26 (31.3) | 16 (22.9) | 21 (32.3) | |
| Egg Donor or Cryo Cycle | 5 (4.8) | 7 (7.1) | 7 (8.4) | 7 (10.0) | 6 (9.2) | |
| Embryos Transferred, n (%) | 0.74 | |||||
| No embryos transferred | 14 (13.5) | 10 (10.1) | 7 (8.4) | 9 (12.9) | 5 (7.7) | |
| 1 embryo | 25 (24.3) | 16 (16.2) | 16 (19.3) | 12 (17.1) | 9 (13.9) | |
| 2 embryos | 41 (39.8) | 49 (49.5) | 43 (51.8) | 35 (50.0) | 32 (49.6) | |
| 3+ embryos | 18 (17.5) | 17 (17.2) | 10 (12.1) | 7 (10.0) | 6 (9.2) | |
| Egg Donor or Cryo Cycle | 5 (4.8) | 7 (7.1) | 7 (8.4) | 7 (10.0) | 6 (9.2) | |
Abbreviations: BMI, body mass index; DOR, diminished ovarian reserve; IVF, in vitro fertilization.
For continuous variables, Kruskal Wallis tests were used to test for associations across categories of distance to nearest roadway. For categorical variables, chi-squared tests (or Fisher’s exact tests if cell counts were <5) were used to test the associations across categories of distance to nearest roadway.
Median family income in the past 12 months (in 2011 inflation-adjusted dollars) by tract from the American Community Survey 2007–2010 estimates.
Only available for fresh autologous cycles with oocytes successfully retrieved.
In multivariable models after adjusting for age, BMI, race, smoking status, education level, and census tract median income, women who lived within close proximity of a major roadway had lower probabilities of implantation and live birth following IVF (Table 2). Compared to women who lived ≥400 m from a major roadway, women who lived within 50 m of a major roadway had an adjusted difference in the probability of implantation and live birth of 13% (62% vs. 49%, p-for-difference= 0.05) and 13% (46% vs. 33%, p-for-difference=0.04), respectively. Traffic density within 100 m of a woman’s residence was not associated with probability of implantation, clinical pregnancy, or live birth. The continuous association between residential distance to major roadway and odds of live birth as modelled using restricted cublic splines was similar to the association observed across categories (see Figure S3). The same was true for the association between traffic density and odds of live birth (see Figure S4A). However, when we excluded women with no traffic information within 100m of their residence, there was a suggestive inverse association between residential traffic density and live birth (see Figure S4B), consistent with an adverse effect of higher exposure to traffic.
Table 2.
Associations between distance from residential address to nearest major roadway and near-residence traffic density and clinical outcomes in 423 women (726 initiated cycles) from the Environment and Reproductive Health (EARTH) Study (2004–2017).
| Adjusted Proportions (95% Cl)a
|
||||
|---|---|---|---|---|
| Women/Cycles | Implantation | Clinical Pregnancy | Live Birth | |
|
|
||||
| Distance to Nearest Major Roadway (m) | ||||
| <50 | 105/174 | 0.49 (0.42, 0.57) | 0.43 (0.35, 0.50) | 0.33 (0.26, 0.41)* |
| 50–99 | 99/168 | 0.59 (0.51, 0.67) | 0.53 (0.45,0.61) | 0.43 (0.35, 0.51) |
| 100–199 | 84/152 | 0.55 (0.46, 0.63) | 0.46 (0.38, 0.54) | 0.37 (0.30, 0.46) |
| 200–399 | 70/127 | 0.56 (0.47, 0.65) | 0.47 (0.38, 0.56) | 0.39 (0.30, 0.48) |
| ≥400 | 65/105 | 0.62 (0.52, 0.71) | 0.54 (0.44, 0.64) | 0.46 (0.36, 0.56) |
| P for trend | 0.13 | 0.19 | 0.11 | |
| Near-Residence Traffic Density (km*vehicles/day) | ||||
| 0 | 157/283 | 0.54 (0.47, 0.60) | 0.45 (0.40, 0.51) | 0.37 (0.31, 0.43) |
| 1–1599 | 66/105 | 0.68 (0.58, 0.77) | 0.58 (0.48, 0.67) | 0.48 (0.38, 0.58) |
| 1600–3099 | 71/124 | 0.52 (0.43, 0.62) | 0.45 (0.36, 0.54) | 0.38 (0.29, 0.47) |
| 3100–6499 | 62/104 | 0.51 (0.41, 0.61) | 0.45 (0.36, 0.55) | 0.38 (0.29, 0.48) |
| ≥6500 | 67/110 | 0.58 (0.48, 0.67) | 0.52 (0.43, 0.62) | 0.37 (0.28, 0.47) |
| P for trend | 0.81 | 0.38 | 0.71 | |
All analyses were run using generalized linear mixed models with random intercepts, binomial distribution, and logit link function. Data are presented as predicted marginal proportions (95% CI) adjusted for age, BMI, race, and smoking status, education level and census tract median income.
p-value < 0.05 for comparison with reference category (≥400 m and 0 km*vehicles/day).
In regards to intermediate endpoints of IVF, residential proximity to a major roadway was not associated with the number of total, mature, or fertilized oocytes (Table 3); however, there were marginally statistically significant associations with estradiol levels (p-trend=0.16) and endometrial thickness (p-trend=0.06). Specifically, women who lived within 50 m of a major roadway had slightly higher estradiol levels (adjusted difference=152 pmol/L) and lower endometrial thickness (adjusted difference= −0.8 mm) compared with women who lived ≥400 m from a major roadway. Near-residence traffic density was not associated with any of the intermediate outcomes.
Table 3.
Associations between distance from residential address to nearest major roadway and near-residence traffic density and intermediate outcomes in 382 women (563 fresh cycles with egg retrieval) from the Environment and Reproductive Health (EARTH) Study (2004–2017).
| Adjusted Means (95% Cl)a
|
|||||
|---|---|---|---|---|---|
| Estradiol Trigger Levels,b pmol/L |
Endometrial Thickness,15 mm |
Total Oocyte Yield, N |
Mature Oocyte Yield, N |
Normally Fertilized Oocytes, N |
|
|
|
|||||
| Distance to Nearest Major Roadway (m) | |||||
| <50 | 2137 (1986, 2287) | 10.1 (9.7, 10.6)* | 11.1 (10.1, 12.1) | 8.9 (8.1, 9.7) | 6.2 (5.5, 6.9) |
| 50–99 | 2114 (1956, 2268) | 10.3 (9.9, 10.8) | 11.4 (10.3, 12.5) | 9.7 (8.8, 10.7) | 6.8 (6.1, 7.6) |
| 100–199 | 2117 (1950, 2284) | 10.3 (9.8, 10.8) | 10.8 (9.7, 11.9) | 8.9 (8.0, 9.9) | 6.4 (5.7, 7.2) |
| 200–399 | 1991 (1811, 2172) | 10.2 (9.6, 10.7) | 10.4 (9.3, 11.7) | 8.8 (7.8, 9.8) | 6.2 (5.4, 7.0) |
| ≥400 | 1985 (1786, 2185) | 10.9 (10.3, 11.5) | 10.8 (9.5, 12.2) | 9.3 (8.2, 10.5) | 6.1 (5.3, 7.0) |
| P for trend | 0.16 | 0.06 | 0.54 | 0.93 | 0.51 |
| Near-Residence Traffic Density (km*vehicles/day) | |||||
| 0 | 2013 (1890, 2135) | 10.3 (10.0, 10.7) | 10.6 (9.8, 11.4) | 8.8 (8.1, 9.5) | 6.0 (5.5, 6.5) |
| 1–1599 | 2223 (2027, 2419) | 10.4 (9.9, 11.0) | 11.8 (10.4, 13.2) | 9.9 (8.8, 11.1) | 7.1 (6.2, 8.1) |
| 1600–3099 | 2101 (1915, 2287) | 10.2 (9.6, 10.7) | 9.8 (8.8, 11.0) | 8.1 (7.2, 9.1) | 5.9 (5.2, 6.7) |
| 3100–6499 | 2060 (1871, 2249) | 10.2 (9.7, 10.7) | 12.1 (10.8, 13.5) | 10.2 (9.1, 11.4) | 7.3 (6.4, 8.4) |
| ≥6500 | 2105 (1912, 2297) | 10.5 (9.9, 11.0) | 11.0 (9.8, 12.4) | 9.3 (8.2, 10.4) | 6.2 (5.4, 7.1) |
| P for trend | 0.72 | 0.67 | 0.67 | 0.48 | 0.92 |
All analyses were conducted using generalized linear mixed models with random intercepts, normal (for estradiol levels and endometrial thickness) or Poisson (for oocyte counts) distribution and identity (for estradiol levels and endometrial thickness) or log (for oocyte counts). Data are presented as predicted marginal means or percentages adjusted for age, BMI, race, and smoking status, education level, and census tract median income.
One woman is missing all intermediate outcomes because her egg retrieval was done at a different hospital. An additional woman is missing endometrial thickness because the endometrium was unable to be visualized.
p-value < 0.05 for comparison with reference category (≥400 m and 0 km*vehicles/day).
Effect estimates were slightly stronger when analyses were restricted to the first cycle per woman and non-current smokers (see Table S1). Results were similar when donor egg recipient cycles, cryo-thaw cycles, and cycles not making it to embryo transfer were excluded. The null association between residential traffic density and clinical outcomes of IVF was consistent whether the buffer size was a 50m, 100m, or 200m radius from the woman’s residential address (see Table S2). There was no evidence of effect modification of the association between residential proximity to major roadways and live birth by race (p-interaction=0.27), smoking status (p-interaction=0.16), maternal age (p-interaction=0.35), infertility diagnosis (p-interaction=0.47), cycle type (p-interaction=0.58), season the IVF cycle began (p-interaction=0.31), or insemination method (p-interaction=0.76) (data not shown). Results were also similar after further adjustment for nulliparity and nulligravidity.
Discussion
In a prospective cohort study of women in Massachusetts we found that closer residential proximity to a major roadway was associated with lower probability of implantation and live birth following IVF. The magnitude of this reduction was clinically relevant as the adjusted difference in the percentage of cycles resulting in live birth comparing women living <50 m vs. ≥400 m from a major roadway was 13% which roughly corresponds to the difference in live birth expected when comparing a woman who is 30 years to one that is 37 years (McLernon et al. 2016). While residential distance to major roadways had a marginal inverse association with estradiol and positive association with endometrial thickness, none of our traffic-related exposures were associated with oocyte parameters or fertilization.
To our knowledge, our study is the first to evaluate the relationship between residential proximity to major roadways and traffic density (as proxies for traffic-related air pollution) and in vitro fertilization outcomes; however, the existing literature on traffic-related air pollution and infertility as well as specific air pollutants and IVF outcomes supports our findings (Carre et al. 2017; Checa Vizcaino et al. 2016). Among women in the Nurses’ Health Study II, those who lived within 200 m of a major roadway had 1.11 (95% CI 1.02–1.20) times the risk of self-reported infertility compared to women living ≥200 m away (Mahalingaiah et al. 2016). Among couples in the Longitudinal Investigation of Fertility and the Environment (LIFE) Study, the likelihood of pregnancy was increased 3% for every 200 m further away the couples’ residence was from a major roadway (Mendola et al. 2017). Regarding specific air pollutants and spontaneous fertility, a cross-sectional study found that the number of live births per 1000 women between the ages of 15 and 44 years was significantly lower in census tracts with higher exposure to NOx, nitrogen dioxide (NO2), fine particular matter (PM2.5), and course particulate matter (PM10) (Nieuwenhuijsen et al. 2014). Moreover, a retrospective time to pregnancy cohort showed that higher levels of PM2.5 and NO2 in the 2 months before the end of the first month of unprotected intercourse were associated with decreases in fecundability (Slama et al. 2013). While researchers from the LIFE Study found no association between time-varying, cycle-averaged exposure to various air pollutants and fecundability, they did find that acute exposure to ozone prior to ovulation and nitrogen oxides around implantation was associated with a decrement in fecundability and higher exposure to sulfate prior to ovulation and PM10 around implantation were associated with slightly greater fecundability (Nobles et al. 2018). Further work in this cohort also showed that chronic rather than acute exposure to ozone and PM2.5 throughout pregnancy was associated with pregnancy loss (Ha et al. 2018). Taken together, these results support our findings that traffic-related air pollution may be associated with lower fertility, specifically implantation failure that could manifest as infertility or lower fecundability in spontaneous pregnancies and higher risk of pregnancy loss. Moreover, acute exposure to air pollution during sensitive windows of the menstrual cycle and potentially during the early stages of IVF may be particularly important for fecundity whereas chronic exposure to air pollution may be a more relevant time window of susceptibility for pregnancy loss.
Similar findings have been observed in studies of specific air pollutants and outcomes of IVF. Legro and colleagues found that among women undergoing IVF at three centers across the northeastern US, higher estimated mean NO2 concentrations at the woman’s address throughout the IVF cycle was associated with a lower probability of live birth (Legro et al. 2010); however, none of the other criteria air pollutants (PM2.5, PM10, SO2, or O3) showed consistent associations. While this study did not specifically evaluate residential distance to roadways or traffic density on outcomes of IVF, spatial-temporal models of residence-level NO2 concentrations consistently show that local traffic, particularly traffic within 50 m of the residence, is a strong predictor of NO2 concentrations (Clougherty et al. 2008; Hochadel et al. 2006). On the other hand, among women who achieved clinical pregnancy following IVF in Sao Paulo, Brazil, the risk of early pregnancy loss increased 5% per unit increase in follicular-phase city-wide average PM10 concentrations. No effects, however, were observed for earlier end points or for live birth rates (Perin et al. 2010a). In a separate study, these same authors also found that higher follicular-phase city-wide concentrations of PM10 were associated with a 2.6-fold increase in the risk of early pregnancy loss, regardless of the method of conception (Perin et al. 2010b).
In our study we found no associations between our proxies for traffic-related air pollution and oocyte yield and fertilization but possible effects on peak estradiol and endometrial thickness levels suggesting that the adverse effects we observed of distance to roadways on implantation could be potentially mediated by hormonal changes affecting the endometrium. A handful of animal and laboratory studies further suggest that impaired embryo development, altered placental function, and abnormal gene expression (all parameters we were unable to assess) could also be plausible mechanisms linking traffic-related air pollution to lower probability of implantation and live birth. When zygotes obtained from supraovulated mice after IVF were cultured in different concentrations of diesel exhaust particles (DEP) (0, 0.2, 2, and 20 µg/cm2) for 5 days, a negative dose-response relationship was observed for inner cell mass (ICM) cell number and ICM/trophectoderm ratio, pointing to a shift of cell specification to the placental lineage and signifying altered early embryo development (Januario et al. 2010). Moreover, while neither the adhesion nor the peri-implantation development of mouse blastocysts on a fibronectin matrix was compromised by the exposure to DEP, a significant impairment of ICM morphological integrity was seen, suggesting that DEP could play an important role in disrupting the growth and viability of the blastocyst even after successful implantation (Januario et al. 2010).
In animal models, pre-pregnancy and pregnancy exposure to nonfiltered ambient air sampled close to a busy street of traffic resulted in morphological changes in the placenta, including reductions in the volume of the maternal blood space and the maternal:fetal surface ratio among mice (Veras et al. 2008) and reductions in placental efficiency, placental blood flow, and fetal vessel volume among rabbits (Valentino et al. 2016) suggesting that maternal vascular changes as a result of exposure to polluted air could result in a compromised uterine environment. Finally, exposure to traffic-related air pollution has been linked to increased inflammation, oxidative stress, DNA damage, and altered DNA methylation which could all be possible biological mechanisms linking traffic-related air pollution to impaired reproduction and more specifically impaired implantation or early embryo development (Barth et al. 2017; Pacchierotti and Spano 2015).
There are some limitations to the present analysis. First, the availability of traffic volume data, the coverage of roads in the traffic count station network, the spacing between stations, and the frequency with which counts are taken are not uniformly collected across Massachusetts and are all factors that influence the validity of our traffic density exposure assessment. We also relied on the most recent version of MassGIS data (2013) for all the women in our cohort despite the fact that some women began their IVF cycle as early as 2004. While a woman’s residential distance to a major road was unlikely to substantially change based on the 2004 or 2014 road network, the traffic counts on these roads might have changed. Taken together, these limitations of the MassGIS traffic data likely resulted in substantial measurement error including having many women who lacked information on traffic in road segments near their residence. These women represent a combination of women who truly have very little traffic near their residence and those who do, but the information is missing in the MassGIS database. While we saw null results overall for near residence traffic density and probability of live birth in the categorical analysis, in the continuous analysis, when we restricted to women with available traffic information, there was a suggestion of an inverse association. Thus, it is hard to determine whether our null results for near-residence traffic density and IVF outcomes are due to these combined, substantial sources of measurement error or truly due to lack of biological effect. Women who moved after enrollment into the EARTH study could also be an additional source of measurement error for both exposure metrics, as the exact date of their address change is not known.
Additionally, distance to major roadways and traffic metrics do not capture the dispersion and degradation profiles of the actual pollutant mix that originates from roadways and is likely the ultimate source of adverse health effects (Jerrett et al. 2005). However, future research in this cohort is planned to better ascertain which specific traffic-related pollutants might be driving these associations. As with most other studies of roadway proximity, we lacked information on greenspace, air purification systems, commuting patterns, and work location which likely introduced error into our exposure assessment. However, many studies suggest that metrics such as distance to roadways are reasonable surrogates for personal monitoring of exposure to air pollutants (Gilbert et al. 2003; van Roosbroeck et al. 2006). As this was an observational study, residual or unmeasured confounding may explain our associations despite our ability to control for many important confounders such as age, body weight, smoking status, education, and census tract median income. It is also possible distance to roadways represents other harmful exposure besides air pollution such as noise or neighborhood socioeconomic status. We did not adjust our p-values for multiple comparisons given our low power, which could have resulted in chance findings. Most of the women in our study also resided at the same address as their male partner, and while preliminary work suggests no association between distance to roadways and semen quality parameters in our cohort (Nassan et al. 2017), we cannot decisively link the detrimental effect we observed solely to the female partner. Finally, our analysis only included women residing in Massachusetts who were primarily living in an urban setting and undergoing IVF at a single academic medical center. While this benefitted our analysis in terms of limiting confounding across regions and IVF centers, it is unclear how generalizable our results will be to all women undergoing IVF across the US, Europe, or other regions of the world where air pollution from traffic may be different (for example, due to more or less diesel vehicles on the roadways).
Despite these limitations, our study had many strengths including its prospective design and the standardized assessment of a wide variety of participant characteristics including smoking (which many other studies lacked). By studying a fertility clinic population we were also able to utilize an efficient study design to investigate how traffic-related air pollution influences clinically relevant, yet previously unobservable, outcomes in a potentially vulnerable sub-population.
In conclusion, residing within 50 m of a major roadway had a negative impact on the likelihood of implantation and live birth following IVF in this cohort. As the number of couples seeking medical treatment for infertility continues to rise (Kushnir et al. 2017), a better understanding of how environmental factors impact outcomes of IVF remains an important health issue particularly given the high costs and psychological toll of having to undergo multiple IVF treatments (Brandes et al. 2009; Katz et al. 2011). Our research not only corroborates evidence from studies among women attempting to conceive naturally (Mahalingaiah et al. 2016; Mendola et al. 2017) and through assisted reproduction (Legro et al. 2010), it further highlights that exposure to traffic-related air pollution may have an effect on early implantation failure. More research is needed to evaluate which specific traffic-related air pollutant(s) may be responsible for this association and whether there is a specific window of heightened susceptibility to its adverse effects.
Supplementary Material
Highlights.
We examined whether residential proximity to major roadways and traffic, as proxies for traffic-related air pollution, are associated with in vitro fertilization (IVF) outcomes.
Closer residential proximity to major roadways was significantly associated with lower probability of implantation and live birth following IVF.
Of the intermediate outcomes, there were suggestive associations between living closer to major roadways and slightly higher estradiol trigger concentrations and lower endometrial thickness.
Near-residence traffic density was not associated with outcomes of IVF.
Acknowledgments
The authors gratefully acknowledge all members of the EARTH study team, specifically Myra G. Keller, Ramace Dadd, the physicians and staff at Massachusetts General Hospital fertility center, and the study participants.
Funding: Supported by grants ES009718, ES022955, ES000002, and K99ES026648 from the National Institute of Environmental Health Sciences (NIEHS) and grant L50HD085359 from the National Institute of Child Health and Human Development (NICHD).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing Financial Interests: The authors declare they have no actual or potential competing financial interests.
References
- Barth A, Brucker N, Moro AM, Nascimento S, Goethel G, Souto C, et al. Association between inflammation processes, DNA damage, and exposure to environmental pollutants. Environ Sci Pollut Res Int. 2017;24:353–362. doi: 10.1007/s11356-016-7772-0. [DOI] [PubMed] [Google Scholar]
- Brandes M, van der Steen JO, Bokdam SB, Hamilton CJ, de Bruin JP, Nelen WL, et al. When and why do subfertile couples discontinue their fertility care? A longitudinal cohort study in a secondary care subfertility population. Hum Reprod. 2009;24:3127–3135. doi: 10.1093/humrep/dep340. [DOI] [PubMed] [Google Scholar]
- Brauer M, Lencar C, Tamburic L, Koehoorn M, Demers P, Karr C. A cohort study of traffic-related air pollution impacts on birth outcomes. Environ Health Perspect. 2008;116:680–686. doi: 10.1289/ehp.10952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carre J, Gatimel N, Moreau J, Parinaud J, Leandri R. Does air pollution play a role in infertility?: A systematic review. Environ Health. 2017;16:82. doi: 10.1186/s12940-017-0291-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Checa Vizcaino MA, Gonzalez-Comadran M, Jacquemin B. Outdoor air pollution and human infertility: A systematic review. Fertil Steril. 2016;106:897–904. e891. doi: 10.1016/j.fertnstert.2016.07.1110. [DOI] [PubMed] [Google Scholar]
- Clougherty JE, Wright RJ, Baxter LK, Levy JI. Land use regression modeling of intraurban residential variability in multiple traffic-related air pollutants. Environ Health. 2008;7:17. doi: 10.1186/1476-069X-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–561. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- European Environment Agency (EEA) [accessed July 28 2017];Contribution of the transport sector to total emissions of the main air pollutants. 2016 Available: https://www.eea.europa.eu/data-and-maps/daviz/contribution-of-the-transport-sector-3.
- Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. Hoboken, New Jersey: John Wiley and Sons, Inc; 2004. Chapter 14: Missing data and dropout. [Google Scholar]
- Fleisch AF, Rifas-Shiman SL, Koutrakis P, Schwartz JD, Kloog I, Melly S, et al. Prenatal exposure to traffic pollution: Associations with reduced fetal growth and rapid infant weight gain. Epidemiology. 2015;26:43–50. doi: 10.1097/EDE.0000000000000203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert NL, Woodhouse S, Stieb DM, Brook JR. Ambient nitrogen dioxide and distance from a major highway. Sci Total Environ. 2003;312:43–46. doi: 10.1016/S0048-9697(03)00228-6. [DOI] [PubMed] [Google Scholar]
- Ha S, Sundaram R, Buck Louis GM, Nobles C, Seeni I, Sherman S, et al. Ambient air pollution and the risk of pregnancy loss: A prospective cohort study. Fertil Steril. 2018;109:148–153. doi: 10.1016/j.fertnstert.2017.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Effects Institute (HEI) Traffic-related air pollution: A critical review of the literature on emissions, exposure, and health effects. (HEI Special Report 17) Boston, MA: 2010. [Google Scholar]
- Hochadel M, Heinrich J, Gehring U, Morgenstern V, Kuhlbusch T, Link E, et al. Predicting long-term average concentrations of traffic-related air pollutants using gis-based information. Atmos Environ. 2006;40:542–553. [Google Scholar]
- Howards PP, Schisterman EF, Heagerty PJ. Potential confounding by exposure history and prior outcomes: An example from perinatal epidemiology. Epidemiology. 2007;18:544–551. doi: 10.1097/ede.0b013e31812001e6. [DOI] [PubMed] [Google Scholar]
- Januario DA, Perin PM, Maluf M, Lichtenfels AJ, Nascimento Saldiva PH. Biological effects and dose-response assessment of diesel exhaust particles on in vitro early embryo development in mice. Toxicol Sci. 2010;117:200–208. doi: 10.1093/toxsci/kfq165. [DOI] [PubMed] [Google Scholar]
- Jerrett M, Arain A, Kanaroglou P, Beckerman B, Potoglou D, Sahsuvaroglu T, et al. A review and evaluation of intraurban air pollution exposure models. J Expo Anal Environ Epidemiol. 2005;15:185–204. doi: 10.1038/sj.jea.7500388. [DOI] [PubMed] [Google Scholar]
- Karner AA, Eisinger DS, Niemeier DA. Near-roadway air quality: Synthesizing the findings from real-world data. Environ Sci Technol. 2010;44:5334–5344. doi: 10.1021/es100008x. [DOI] [PubMed] [Google Scholar]
- Katz P, Showstack J, Smith JF, Nachtigall RD, Millstein SG, Wing H, et al. Costs of infertility treatment: Results from an 18-month prospective cohort study. Fertil Steril. 2011;95:915–921. doi: 10.1016/j.fertnstert.2010.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushnir VA, Barad DH, Albertini DF, Darmon SK, Gleicher N. Systematic review of worldwide trends in assisted reproductive technology 2004–2013. Reprod Biol Endocrinol. 2017;15:6. doi: 10.1186/s12958-016-0225-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legro RS, Sauer MV, Mottla GL, Richter KS, Li X, Dodson WC, et al. Effect of air quality on assisted human reproduction. Hum Reprod. 2010;25:1317–1324. doi: 10.1093/humrep/deq021. [DOI] [PubMed] [Google Scholar]
- Mahalingaiah S, Hart JE, Laden F, Farland LV, Hewlett MM, Chavarro J, et al. Adult air pollution exposure and risk of infertility in the nurses’ health study ii. Hum Reprod. 2016 doi: 10.1093/humrep/dev330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massachusetts Office of Geographic Information (MassGIS) [accessed June 2 2017];MassGIS data -Massachusetts Department of Transportation (MassDOT) roads. 2014 Available: http://www.mass.gov/anf/research-and-tech/it-serv-and-support/application-serv/office-of-geographic-information-massgis/datalayers/eotroads.html.
- McLernon DJ, Steyerberg EW, Te Velde ER, Lee AJ, Bhattacharya S. Predicting the chances of a live birth after one or more complete cycles of in vitro fertilisation: Population based study of linked cycle data from 113 873 women. BMJ. 2016;355:i5735. doi: 10.1136/bmj.i5735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendola P, Sundaram R, Louis GMB, Sun L, Wallace ME, Smarr MM, et al. Proximity to major roadways and prospectively-measured time-to-pregnancy and infertility. Sci Total Environ. 2017;576:172–177. doi: 10.1016/j.scitotenv.2016.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moller P, Danielsen PH, Karottki DG, Jantzen K, Roursgaard M, Klingberg H, et al. Oxidative stress and inflammation generated DNA damage by exposure to air pollution particles. Mutat Res Rev Mutat Res. 2014;762:133–166. doi: 10.1016/j.mrrev.2014.09.001. [DOI] [PubMed] [Google Scholar]
- Nassan F, Gaskins AJ, Tanrikut C, Hauser R, Chavarro JE. Residential distance to major roadways and semen quality among men attending a fertility clinic. Fertil Steril. 2017;108:e4–e5. [Google Scholar]
- Nieuwenhuijsen MJ, Basagana X, Dadvand P, Martinez D, Cirach M, Beelen R, et al. Air pollution and human fertility rates. Environ Int. 2014;70:9–14. doi: 10.1016/j.envint.2014.05.005. [DOI] [PubMed] [Google Scholar]
- Nobles CJ, Schisterman EF, Ha S, Buck Louis GM, Sherman S, Mendola P. Time-varying cycle average and daily variation in ambient air pollution and fecundability. Hum Reprod. 2018;33:166–176. doi: 10.1093/humrep/dex341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacchierotti F, Spano M. Environmental impact on DNA methylation in the germline: State of the art and gaps of knowledge. Biomed Res Int. 2015;2015:123484. doi: 10.1155/2015/123484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panasevich S, Leander K, Rosenlund M, Ljungman P, Bellander T, de Faire U, et al. Associations of long- and short-term air pollution exposure with markers of inflammation and coagulation in a population sample. Occup Environ Med. 2009;66:747–753. doi: 10.1136/oem.2008.043471. [DOI] [PubMed] [Google Scholar]
- Perin PM, Maluf M, Czeresnia CE, Januario DA, Saldiva PH. Impact of short-term preconceptional exposure to particulate air pollution on treatment outcome in couples undergoing in vitro fertilization and embryo transfer (ivf/et) J Assist Reprod Genet. 2010a;27:371–382. doi: 10.1007/s10815-010-9419-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perin PM, Maluf M, Czeresnia CE, Nicolosi Foltran Januario DA, Nascimento Saldiva PH. Effects of exposure to high levels of particulate air pollution during the follicular phase of the conception cycle on pregnancy outcome in couples undergoing in vitro fertilization and embryo transfer. Fertil Steril. 2010b;93:301–303. doi: 10.1016/j.fertnstert.2009.06.031. [DOI] [PubMed] [Google Scholar]
- Risom L, Moller P, Loft S. Oxidative stress-induced DNA damage by particulate air pollution. Mutat Res. 2005;592:119–137. doi: 10.1016/j.mrfmmm.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Robledo CA, Mendola P, Yeung E, Mannisto T, Sundaram R, Liu D, et al. Preconception and early pregnancy air pollution exposures and risk of gestational diabetes mellitus. Environ Res. 2015;137:316–322. doi: 10.1016/j.envres.2014.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Searle SR, Speed FM, Milliken GA. Population marginal means in the linear model: An alternative to least square means. The American Statistician. 1980;34:216–221. [Google Scholar]
- Singh V, Sokhi RS, Kukkonen J. Pm2.5 concentrations in london for 2008--a modeling analysis of contributions from road traffic. J Air Waste Manag Assoc. 2014;64:509–518. doi: 10.1080/10962247.2013.848244. [DOI] [PubMed] [Google Scholar]
- Slama R, Bottagisi S, Solansky I, Lepeule J, Giorgis-Allemand L, Sram R. Short-term impact of atmospheric pollution on fecundability. Epidemiology. 2013;24:871–879. doi: 10.1097/EDE.0b013e3182a702c5. [DOI] [PubMed] [Google Scholar]
- Stieb DM, Chen L, Hystad P, Beckerman BS, Jerrett M, Tjepkema M, et al. A national study of the association between traffic-related air pollution and adverse pregnancy outcomes in canada, 1999–2008. Environ Res. 2016;148:513–526. doi: 10.1016/j.envres.2016.04.025. [DOI] [PubMed] [Google Scholar]
- Sydbom A, Blomberg A, Parnia S, Stenfors N, Sandstrom T, Dahlen SE. Health effects of diesel exhaust emissions. Eur Respir J. 2001;17:733–746. doi: 10.1183/09031936.01.17407330. [DOI] [PubMed] [Google Scholar]
- United Nations Environment Program (UNEP) Air pollution in the worlds megacities. Environment. 1994;36:5–37. [Google Scholar]
- Valentino SA, Tarrade A, Aioun J, Mourier E, Richard C, Dahirel M, et al. Maternal exposure to diluted diesel engine exhaust alters placental function and induces intergenerational effects in rabbits. Part Fibre Toxicol. 2016;13:39. doi: 10.1186/s12989-016-0151-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Roosbroeck S, Wichmann J, Janssen NA, Hoek G, van Wijnen JH, Lebret E, et al. Long-term personal exposure to traffic-related air pollution among school children, a validation study. Sci Total Environ. 2006;368:565–573. doi: 10.1016/j.scitotenv.2006.03.034. [DOI] [PubMed] [Google Scholar]
- Veras MM, Damaceno-Rodrigues NR, Caldini EG, Maciel Ribeiro AA, Mayhew TM, Saldiva PH, et al. Particulate urban air pollution affects the functional morphology of mouse placenta. Biol Reprod. 2008;79:578–584. doi: 10.1095/biolreprod.108.069591. [DOI] [PubMed] [Google Scholar]
- Wauters A, Dreyfuss C, Pochet S, Hendrick P, Berkenboom G, van de Borne P, et al. Acute exposure to diesel exhaust impairs nitric oxide-mediated endothelial vasomotor function by increasing endothelial oxidative stress. Hypertension. 2013;62:352–358. doi: 10.1161/HYPERTENSIONAHA.111.00991. [DOI] [PubMed] [Google Scholar]
- Weinberg CR. Toward a clearer definition of confounding. American journal of epidemiology. 1993;137:1–8. doi: 10.1093/oxfordjournals.aje.a116591. [DOI] [PubMed] [Google Scholar]
- Weng HY, Hsueh YH, Messam LL, Hertz-Picciotto I. Methods of covariate selection: Directed acyclic graphs and the change-in-estimate procedure. Am J Epidemiol. 2009;169:1182–1190. doi: 10.1093/aje/kwp035. [DOI] [PubMed] [Google Scholar]
- Wu J, Ren C, Delfino RJ, Chung J, Wilhelm M, Ritz B. Association between local traffic-generated air pollution and preeclampsia and preterm delivery in the south coast air basin of california. Environ Health Perspect. 2009;117:1773–1779. doi: 10.1289/ehp.0800334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yorifuji T, Naruse H, Kashima S, Ohki S, Murakoshi T, Takao S, et al. Residential proximity to major roads and preterm births. Epidemiology. 2011;22:74–80. doi: 10.1097/EDE.0b013e3181fe759f. [DOI] [PubMed] [Google Scholar]
- Zhou Y, Levy JI. Factors influencing the spatial extent of mobile source air pollution impacts: A meta-analysis. BMC Public Health. 2007;7:89. doi: 10.1186/1471-2458-7-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.