Abstract
Although there is much discussion about population health in academic medical centers, managed care organizations, and a variety of disciplines, it is not always clear what this term means. Population health describes the health outcomes of a group of individuals including health disparities, social determinants of health, and policies and interventions that link health outcomes with and patterns of health determinants. We describe some of the successes and challenges to addressing reproductive health issues in Georgia from a population health perspective, focusing on efforts to reduce teenage pregnancy and improve maternal health.
Introduction
Although there is much discussion about Population Health in academic medical centers, managed care organizations, and a variety of disciplines, it is not always clear what this term means. Further, the distinction between public health and population health is often not clear. Yet as this field gains center stage, it is critical that obstetrician–gynecologists (ob-gyns) understand how this term is used and how this field is developing so that we can be part of the conversation and take on leadership roles to shape this discussion. Substantial resources are being directed towards improving population health, thus these discussions will be shaping how health care, disease prevention, and research dollars are being spent.
What is population health? One commonly used definition was first proposed in 2003 by Drs. Kindig and Soddart, pioneers and leaders in the field of population health. They defined population health as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group”(1). In addition to measuring overall health outcomes, this definition accounts for health disparities, since the distribution of health outcomes is also measured. A population health perspective recognizes that in addition to genetic predisposition and medical care, a broad variety of factors influence health, including social, educational, and economic conditions(2). Since social circumstances, environmental exposures, and behavior account for an estimated 60% of early deaths in the United States(2), it is critical to include determinants of health beyond those ordinarily addressed in the traditional medical care system. A population health framework also includes policies and interventions that link health outcomes and patterns of health determinants (1).
How the term “population” within population health is defined depends upon whether a broad public health or a narrower clinical perspective is taken. Public health’s focus is protecting and improving the health of populations with these populations tending to be large and inclusive. From a public health perspective, a population-based surveillance system for influenza in pregnancy might be a nationwide surveillance system including all pregnant women in the United States who are hospitalized for influenza. From a clinical or health care systems perspective, populations may be smaller and include only those served by a specific health care facility; for example, a system for monitoring influenza in pregnancy might include a system for tracking what proportion of patients delivering at hospital X received the influenza vaccine during pregnancy and the number and length of hospitalizations among pregnant women with laboratory-confirmed influenza during the year. From a population health-management perspective, the cost effectiveness of providing a vaccine program in prenatal clinics may be evaluated in terms of its ability to save money on inpatient hospitalizations.
Regardless of the size or representativeness of the population, the underlying principles of population health are the same — prevent disease and promote health. While clearly the approach should include effective health care delivery, this is only a small part of the population health paradigm. The paradigm requires a close partnership between clinical medicine and public health, and is laid out nicely by Dr. Thomas Frieden, former director of the U.S. Centers for Disease Control and Prevention (CDC) from 2009 to 2017, in series of publications. Dr. Frieden describes a “health impact pyramid” consisting of a series of interventions to provide a framework for improving health, with socioeconomic factors, or social determinants of health, at the base(3) (Figure 1). Ascending from the base to the top of the pyramid, the next level includes interventions that change the environmental context (eg, fluoridated water, elimination of asbestos) and long-lasting protective interventions (eg, immunization, colonoscopy). Clinical interventions, counseling, and education are at the top and require more individualized focus and effort. Public health efforts generally focus more on the lower tiers of the pyramid and clinical medicine focuses more on the higher tiers. At the bottom of the pyramid the population affected is very large, but with ascent of the pyramid the population that is reached becomes smaller as increasingly individualized approaches are required. Figure 1 provides examples of how this health impact pyramid can be applied to health outcomes: improving neonatal outcomes and reducing sexually transmitted infections.
Figure 1.
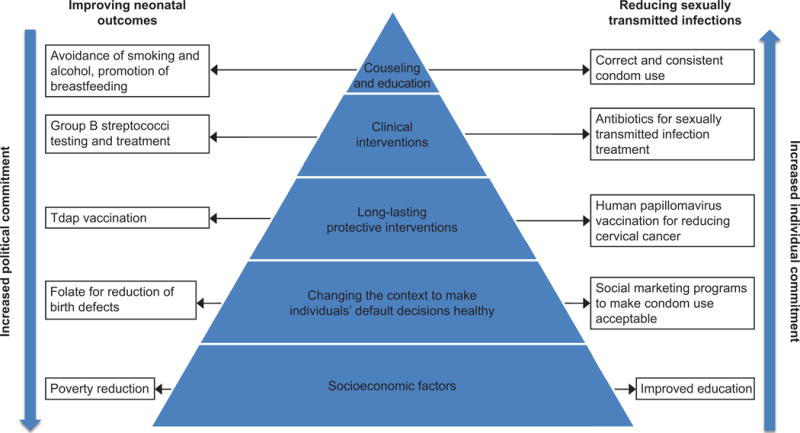
The health impact pyramid for reproductive health outcomes (based on Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health 2010;100(4):590–95); published by Sheridan. The American Public Health Association is not responsible for the translation of this figure. Tdap, tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis.
This broad framework has been used to combat a number of serious and complex health threats. In 2010, the CDC defined 6 “Winnable Battles”, including teenage pregnancy(4, 5). These were focus areas in which it was believed that measurable improvement could be achieved through the use of broad-based strategies including developing policies, establishing clinical guidelines, and working with a variety of partners including clinicians, local, state, and federal governments, private industry, and the media. Although improvements in teenage pregnancy rates were occurring prior to the identification of the Winnable Battles, teenage pregnancy rates declined substantially during this 5-year period of sustained focus(4). The measurable success achieved during this period in a number of areas may serve as a call to action for closer partnerships between clinical medicine and public health(6); reproductive health challenges addressed in an OB/GYN setting can be complex and beyond the scope of routine delivery of clinical care, and would likely benefit from the inclusion of a broader population health perspective, in effect addressing the lower tiers of the health outcome pyramid. Since we both currently practice obstetrics and gynecology at Grady Hospital in Atlanta, Georgia, we will describe here some of the successes and challenges to addressing reproductive health through a population health lens here in Georgia.
Population Heath in Georgia and at Grady Hospital
Grady Hospital, founded in 1892, is one of the largest hospitals in the Southeast and operates as a safety-net hospital providing care for medically underserved patients. It is the only level-one trauma center within a 100-mile radius of downtown Atlanta. The Grady health system operates with the collaborative support of Emory and Morehouse Schools of Medicine. Grady’s mission is to “improve the health of the community by providing quality, comprehensive healthcare in a compassionate, culturally competent, ethical and fiscally responsible manner”. For many years, 2 major metropolitan counties (Fulton and DeKalb) have provided substantial financial support to Grady. While a majority of Grady’s revenue is generated through Medicare and Medicaid reimbursement, Grady provides substantial indigent and charity care (7) with over $220 million in indigent and charity care provided in 2010. Beyond direct patient care, Grady’s commitment to the community is demonstrated through its community wellness and education outreach, free health screenings, seminars, community fairs, educational conferences, support groups, and personal resource assistance programs.
Several of the poor health outcomes that seem to disproportionately plague many of the patients served at Grady, such as unintended pregnancy, teenage pregnancy, and adverse maternal health outcomes such as preterm birth, are largely influenced by factors that are distinct from direct patient care and service delivery. Given this, within the Grady health system, there are opportunities to address and improve not only clinical care and service delivery, but also the larger social determinants of health by leveraging a population health framework to guide efforts towards improving health outcomes. Examples we highlight include programs aimed at reducing teenage pregnancy and strategies to improve maternal health outcomes, two issues that are not only critical for our Grady patient population but have regional importance. We have created a population health driver diagram (8) to illustrate how the primary drivers can help align interventions and policies to influence change (figure 2). In addition to these current examples, we also need to know how to prepare for emerging health threats using a population health approach. For example, because Atlanta is a key travel hub and Grady has a large immigrant and foreign-born population(9), emerging infections have the potential to surface early in our community(10).
Figure 2.
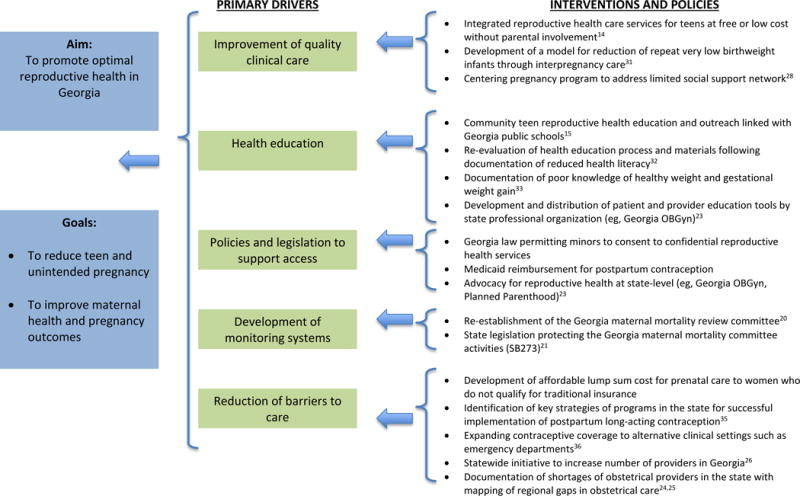
Diagram depicting population health drivers for improvement of reproductive health in Georgia. GeorgiaOBGyn, Georgia Obstetrical and Gynecological Society.
Reducing Teenage Pregnancy
For years, Georgia has had one of the highest rates of teenage pregnancy in the nation(11). Teen pregnancy is associated with poorer birth outcomes including higher rates of low birth weight and preterm birth as well as decreased educational and economic attainment for the mother. Between 1998 and 2012, there was a 50% reduction in teenage pregnancy rates in Georgia, with a greater than 12% drop between 2011 and 2012. This decline has led to an estimated $400-500 million dollars per year in savings(12).
Increases in contraceptive use, particularly the more effective contraceptive methods, are a primary driver in the national decline in teenage births(13). Georgia law specifically permits minors under the age of 18 to consent to confidential health services to prevent pregnancy including contraception, and for HIV and STI testing and treatment. Recognizing the high incidence and effects of teenage pregnancy on our population, for decades Grady has provided family planning services to teenagers, with the encouragement, but not requirement of parental involvement. Title X funding removed cost barriers and allowed for comprehensive reproductive healthcare services, STI screening and treatment, and contraceptive delivery regardless of insurance status. The teenage-friendly adolescent reproductive health center provides services primarily aimed at the top and middle tiers of the health impact pyramid. The teenage center integrates health educators into all aspects of service delivery with protocols and policies supporting evidence-based and teenage-friendly care, such as walk-in and weekend appointments, same day contraceptive initiation, and long lasting protective interventions, such as HPV vaccination and use of IUDs and implants for contraception. These clinical efforts were augmented by the Jane Fonda Center, established in 2000 through a gift from Jane Fonda to Emory University School of Medicine aimed at advancing the science around adolescent reproductive healthcare and enhancing service delivery. The Center conducts research to both determine and help implement best practices for reproductive health for teenagers (14).
External partnerships have been an essential part of addressing some of the lower tiers of the health impact pyramid in relation to teenage pregnancy prevention. The Georgia Campaign for Adolescent Pregnancy and Prevention, recently renamed Georgia Campaign for Adolescent Power and Potential (GCAPP), has been a key partner in these efforts. GCAPP is a non-profit, also founded by Jane Fonda to reduce adolescent pregnancy in Georgia(15). The organization operates on a community-based level across the state with efforts focused on the lower tiers of the health impact pyramid, addressing a broader scope of factors, such as education and empowerment, which are key determinants of teenage reproductive health. With GCAPP as a backbone agency, the Georgia Public-Private Partnership (P3) uses a collective impact model to bring together public agencies, non-profits, clinicians, educators, community-based organizations, and foundations. P3 collectively addresses several levels of the health-impact pyramid with a goal to reduce teenage pregnancy in Georgia. OB/GYN physician members are critical to entities like this; their clinical observations from providing care to young people can contribute to organizational direction, priority and activity development.
Although the teenage birth rate in Georgia has declined substantially, it remains unacceptably high, with Georgia ranking 15th highest among the 50 states for teen pregnancy(16). With potential changes to the contraceptive mandate under the Affordable Care Act, and changes in funding support for Title X, it is unclear how many women and teenagers in Georgia, and nationally, may lose access to contraception due to financial barriers(17). As these policy and funding changes translate into changes in health, ob-gyns will have an important role in maintaining teenage pregnancy prevention as a priority, advocating for ongoing public attention and research dollars and working with partners to continue to address efforts as new challenges arise.
Improving Maternal Health Outcomes
Georgia has consistently ranked among the 10 states with the highest maternal mortality rate as well as feto-infant mortality rate(18). Marked racial disparities exist with African American women having significantly greater incidence of these outcomes(19). For example, the maternal mortality ratio (MMR) for Black and African American women in Georgia in 2016 was greater than twice the MMR for white women(19). To address these poor outcomes, several important partnerships between clinical care, public health, and policy organizations have developed at Grady and at the state level to address some of the underlying contributors to adverse maternal and fetal outcomes.
Maternal, perinatal and infant mortality review committees are partnerships between public health and academic communities that have been proposed as strategies to reduce these poor outcomes(20). In recognition of the high pregnancy-related mortality rate in the state, the Georgia maternal mortality review committee was reestablished in 2012(20). This multidisciplinary committee is led by the Georgia Obstetrical and Gynecologic Society and includes public health professionals from the Georgia Department of Health, epidemiologists from the Centers for Disease Control and Prevention (CDC), and Emory obstetrician-gynecologists who practice at Grady. The support of the Georgia General Assembly and Governor with the passage of Senate Bill 273 provided legal protection for the committee members and the review process, ensured confidentiality of the review and authority to the committee for the collection of data for effective case review(21). A recent evaluation by this group determined that the five most common causes of pregnancy-related mortality were hemorrhage, hypertension, cardiac disease, embolism and seizures. Current recommendations from this review have highlighted several avenues where improvement is essential – including improving effective contraceptive and preconception counseling for women with medical comorbidities and increasing consultation with maternal-fetal medicine specialists during pregnancy for these women with medical comorbidities. At a national level, the Council on Patient Safety in Women’s Health Care, a broad consortium of women’s health organization and the Alliance for Innovation on Maternal Health (AIM) Program(22) are supporting patient safety bundles that can be implemented at the local, regional and state-level. The Georgia Obstetrical and Gynecologic Society and its physician members have been leading the effort to address these issues through development of provider education resources as well as statewide advocacy through their political action committee (PAC)(23).
Access to care is particularly challenging in Georgia given shortages in obstetric providers throughout the state(24, 25). Statewide initiatives to reduce the physician shortage in Georgia have led to increases in medical school enrollment by 600 students from 2000 to 2010 and the establishment of new graduate medical education (GME) programs at new teaching hospitals in the state. (26). Other programs aimed at reducing the effects of the obstetric shortage include the Georgia Center for Obstetrics Re-Entry Program(27) and expansion of consultative services and transport teams through the regional perinatal centers. Despite these efforts, ongoing challenges continue in Georgia that affect clinical care provision.
Grady has a number of initiatives to improve the quality of and reduce barriers to prenatal care (figure 2). Recognizing that many women attending Grady have no health insurance or Medicaid coverage, Grady aimed to develop programs to provide quality care for this population by reducing financial barriers to care. Grady Healthy Baby (GHB) was developed in 2010 to provide an affordable lump sum cost for prenatal care to women who do not qualify for traditional insurance. And while some of these factors may not directly affect the underlying issues such as education and socioeconomic barriers within the health impact pyramid, they aim to help reduce the effects of these factors and eliminate these barriers to improve care.
Other examples of Grady initiatives aimed at reducing barriers to care include the centering pregnancy program and the interpregnancy care program (ICP). The centering pregnancy program has been developed in an effort to address the limited social support network for many of our pregnant patients. Centering pregnancy programs have developed nationally as a model of group prenatal care that provides individual health assessments along with patient education and group support(28). The Centering model of prenatal care, compared to a traditional prenatal care model, has been demonstrated in some but not all studies to improve a number of perinatal outcomes, including reduced rates of preterm birth and improved birth weight(29, 30). Grady’s program provides group pregnancy care through our midwives, helps individuals to develop social support networks and is linked with education modules to improve health care outcomes. Grady also had a pilot program which provided comprehensive interpregnancy care for women at risk for recurrent very low birthweight births. The Grady Memorial Hospital IPC Program, developed out of the 1998 Georgia task force on perinatal care recommendations, provided 24-months of integrated primary care and dental services through enhanced nurse care management and community outreach through a resource mother, a layperson trained to facilitate life skills and health education acquisition(31). While the initial program had some modest success, some of the barriers recognized included lack of financial coverage for health care services for IPC, participant’s poor understanding of the consequences of substance abuse on pregnancy outcomes, and individuals prioritizing securing employment over health care, and lack of employment, childcare services, and housing.
Several other research efforts and programs have been developed within the Grady obstetric program to help identify key predictors of poor health as well as address some of these factors. For example, we recently documented a high prevalence of reduced health literacy (54% had impaired health literacy) among our postpartum patients and demonstrated that impaired health literacy was associated with reduced contraceptive uptake and breastfeeding postpartum(32). In response, we reevaluated our health education process and materials with the aim of developing approaches necessary to address this health literacy barrier. Similarly, despite the high prevalence of obesity and other medical comorbidities such as hypertension and diabetes among our obstetric patients, a recent evaluation demonstrated that over 50% of patients inappropriately identify their own weight category and over 70% of the pregnant women incorrectly identified their gestational weight gain goals(33). Efforts to overcome patient misconceptions and adjust health expectations within a culturally sensitive context are critical to women’s health through pregnancy and postpartum in our community. Furthermore, an important part of population health is direct improvement of healthcare capacity to respond to adverse and emerging health outcomes. For example, the increasing obesity epidemic has required the development of different approaches and protocols at Grady for the care of morbidly obese obstetric patients(34).
Contraception has been recognized as an important cost-effective measure to reduce maternal mortality and poor maternal health outcomes that stem from unintended pregnancy. Multiple factors within the population health framework contribute to challenges for the receipt of contraception among women desiring to delay or cease childbearing. While many women have reduced access to care outside of the peripartum period, addressing contraceptive needs within the immediate post-partum period can help overcome some of those barriers. Georgia was one of the first states to provide Medicaid reimbursement for immediate postpartum contraception. This is particularly important for the long-acting reversible contraceptives (LARC), intrauterine devices and implants, which are the most effective user-independent methods. Efforts to increase postpartum LARC throughout the state have been varied, with several systemic barriers limiting some healthcare systems from effectively integrating immediate post-partum contraceptive services. However, several hospitals, including Grady, have successfully implemented immediate post-partum LARC and have identified several key strategies that facilitated successful implementation(35). Another opportunity to reach women with poor access to healthcare may be through nontraditional settings such as emergency departments. Women who receive care in emergency departments often have limited access to preventive health care and are at increased risk for unintended pregnancy. A recent evaluation of providers in the state highlighted opportunities to improve access to contraceptive provision and referral within the emergency department setting(36). Similarly, in recognizing gaps in contraceptive provision for women with medical comorbidities, we have aimed to simplify referral systems to contraceptive care and in some cases, such as in the HIV care setting, have aimed to integrate contraceptive care into that specific clinic setting. These efforts to expand contraceptive access recognize the current barriers to care and utilize existing clinical settings to increase contraceptive care.
Next Steps – Clarifying a Role for Ob-Gyn Providers Within a Population Health Framework
Many efforts have been taken among providers at our institution, similar to other academic centers, to consider health through a broader “population health” lens. However, the approach is often not comprehensive, integrated, and sustainable. Our efforts in improving maternal health at Grady, for example, can be strengthened with unified population health approach. Recognizing these limitations, we are now attempting to develop an integrated strategy. It is essential for ob-gyns to work with other public health experts in the community to integrate in programs with clear measurements and strategies to address underlying health determinants.
Discussion
The Healthy People 2020 initiative (https://www.healthypeople.gov/), sponsored by the U.S. Department of Health and Human Services, has identified key topic areas and objectives to improve population health. Among these, several are within the domain of reproductive health including adolescent health, family planning, maternal, infant and child health, and sexually transmitted diseases. Additionally, addressing the social determinants of health is an independent objective with the goal of creating social and physical environments that promote good health for all. How these reproductive health challenges are operationalized in an ob-gyn setting can be complex and beyond the scope of the delivery of clinical care. It is important to recognize that there are often population health efforts that may have overlooked the important involvement and critical insight of the ob-gyn provider. For example, the initial strategy for Ebola response in many international settings failed to accommodate specific plans for pregnant women and obstetric care. (10) As a result, there is indirect evidence that labor and delivery units became a site for amplification of the virus(37, 38). It is not uncommon that in addressing health issues, specific issues related to women and pregnancy get overlooked. Thus, we ob-gyns, as comprehensive women’s health providers, need to be aware of and involved with these discussions.
As pointed out by Dr. Frieden, it is critical that public health and clinical medicine work together to tackle disease and to improve health according to a new paradigm. As leaders in women’s health, it is critical that we understand the underlying principles of Population Health, have a framework for how to address reproductive health issues in a larger context, and help to lead the discussions with public health colleagues about how to tackle complex reproductive health issues. As ob-gyns, we can help frame the discussion to center on key reproductive health outcomes and to clearly delineate measurable goals including defining all terms. This may require involvement beyond health care delivery and will include advocating for patients, garnering resources from public and private sources, providing input into policy decisions, and partnering with local and national public health agencies as well as the private sector (Box 1). At an individual practice level, ob-gyn providers may be able to reduce some barriers to care. For example, adjusting clinic hours, locations, or both, and adding child-care capacity in the clinic or partnering with groups to help provide ancillary services, may be helpful in some populations. This collaborative paradigm and opportunities for the clinical provider to be relevant and essential to improving population health is highlighted by Dr. Frieden: “Working together, clinical medicine and public health can ensure that people live active and productive lives far longer than was ever thought possible.(39)” The role of the obstetrician–gynecologist in this call to action for a closer partnership between public health and clinical medicine in order to improve reproductive health requires that we understand and embrace a population health paradigm.
Box 1. What Obstetrician–Gynecologists Can Do to Affect Population Health.
Learn about the specific reproductive health determinants in your community
Recognize the specific reproductive health outcomes that are important to address in your population
Develop partnerships with community-based organizations, department of public health and schools of public health with shared missions of improving reproductive health
Develop and collaborate on comprehensive clinical or research programs that can quantify key reproductive health outcomes and determinants
Get involved locally including at school boards, state professional organizations, local public and private organizations, hospital boards
Advocate for policies and programs that can positively impact care locally, regionally and nationally
Educate on strategies to improve health outcomes locally, e.g. community health fairs, churches, synagogues, mosques, rotary club, schools
Identify strategies within your clinic to help reduce the burden of socio-economic and environmental barriers to care
Work within your healthcare system to identify quality improvement projects
Stay aware of health interventions, research, programs and policies to ensure reproductive health specific issues are incorporated
Join or create multidisciplinary working groups focused on population health
Supplementary Material
Acknowledgments
The authors thank Drs. Michael Lindsay, Eva Lathrop, and Melissa Kottke for their thoughtful feedback in the development of the manuscript.
Dr. Haddad is supported by the NICHD (1K23HD078153-01A1).
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Each author has indicated that she has met the journal’s requirements for authorship.
References
- 1.Kindig D, Stoddart G. What is population health? Am J Public Health. 2003 Mar;93(3):380–3. doi: 10.2105/ajph.93.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood) 2002 Mar-Apr;21(2):78–93. doi: 10.1377/hlthaff.21.2.78. [DOI] [PubMed] [Google Scholar]
- 3.Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010 Apr;100(4):590–5. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frieden TR, Ethier K, Schuchat A. Improving the Health of the United States With a “Winnable Battles” Initiative. JAMA. 2017 Mar 07;317(9):903–4. doi: 10.1001/jama.2017.0436. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Winnable Battles. [cited Dec 1, 2017]; Available from: https://www.cdc.gov/winnablebattles/index.html.
- 6.Frieden TR. A Safer, Healthier U.S.: The Centers for Disease Control and Prevention, 2009–2016. Am J Prev Med. 2017 Mar;52(3):263–75. doi: 10.1016/j.amepre.2016.12.024. [DOI] [PubMed] [Google Scholar]
- 7.[cited Dec 1, 2017; Available from: https://www.gradyhealth.org/learn-about-us/
- 8.Public Health Foundation (PHF) [cited Dec 1, 2017; Available from: http://www.phf.org/programs/driverdiagram/Pages/Using_Driver_Diagrams_to_Improve_Population_Health.aspx.
- 9.Forna F, Jamieson DJ, Sanders D, Lindsay MK. Pregnancy outcomes in foreign-born and US-born women. Int J Gynaecol Obstet. 2003 Dec;83(3):257–65. doi: 10.1016/s0020-7292(03)00307-2. [DOI] [PubMed] [Google Scholar]
- 10.Haddad L, Horton J, Ribner B, Jamieson D. Ebola Infection in Pregnancy: A Global Perspective and Lessons Learned. Clinical Obstetrics and Gynecology. doi: 10.1097/GRF.0000000000000332. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kost K, Maddow-Zimet I. A A Pregnancies, Births and Abortions Among Adolescents and Young Women in the United States, 2013: National and State Trends by Age, Race and Ethnicity. 2017 [cited December 1, 2017]; Available from: https://www.guttmacher.org/report/us-adolescent-pregnancy-trends-2013.
- 12.Georgia Department of Public Health. Teen Pregnancy Prevention. [cited September 24th, 2017]; Available from: https://dph.georgia.gov/teen-pregnancy-prevention.
- 13.Lindberg L, Santelli J, Desai S. Understanding the Decline in Adolescent Fertility in the United States, 2007-2012. J Adolesc Health. 2016 Nov;59(5):577–83. doi: 10.1016/j.jadohealth.2016.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jane Fonda Center. [cited December 1, 2017]; Available from: http://janefondacenter.emory.edu.
- 15.Georgia Campaign for Adolescent Power and Potential (GCAPP) [cited December 1, 2017]; Available from: https://www.gcapp.org.
- 16.The National Campaign to Prevent Teen and Unplanned Pregnancy. [cited December 1, 2017]; Available from: https://thenationalcampaign.org/data/state/georgia.
- 17.Pear R, Ruiz R, Goodstein L. Trump Administration Rolls Back Birth Control Mandate. The New York Times. 2017 2017 October 6. [Google Scholar]
- 18.MacDorman MF, Gregory EC. Fetal and Perinatal Mortality: United States, 2013. Natl Vital Stat Rep. 2015 Jul 23;64(8):1–24. [PubMed] [Google Scholar]
- 19.Georgia Department of Public Health. OASIS Online analytical statistical information system. [cited Sept 16, 2017]; Available from: https://oasis.state.ga.us/oasis/webquery/qryMaternalDeath.aspx.
- 20.Lindsay MK, Goodman D, Csukas S, Cota P, Loucks TL, Ellis JE, et al. Partnering of Public, Academic, and Private Entities to Reestablish Maternal Mortality Review in Georgia. Obstet Gynecol. 2017 Sep;130(3):636–40. doi: 10.1097/AOG.0000000000002204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Georgia Senate Bill 273: 213-2014 regular session. [cited Dec 1, 2017]; Available from: https:/dph.georgia.gov/maternal-mortality.
- 22.Council on Patient Safety in Women’s Health Care. [cited Dec 1, 2017]; Available from: http://safehealthcareforeverywoman.org.
- 23.Georgia Obstetrical and Gynecological Society. [cited Dec 1, 2017]; Available from: http://gaobgyn.org.
- 24.Spelke B, Zertuche AD, Rochat R. Obstetric Provider Maldistribution: Georgia, USA, 2011. Matern Child Health J. 2016 Jul;20(7):1333–40. doi: 10.1007/s10995-016-1999-8. [DOI] [PubMed] [Google Scholar]
- 25.Meyer E, Hennink M, Rochat R, Julian Z, Pinto M, Zertuche AD, et al. Working Towards Safe Motherhood: Delays and Barriers to Prenatal Care for Women in Rural and Peri-Urban Areas of Georgia. Matern Child Health J. 2016 Jul;20(7):1358–65. doi: 10.1007/s10995-016-1997-x. [DOI] [PubMed] [Google Scholar]
- 26.Nuss MA, Robinson B, Buckley PF. A Statewide Strategy for Expanding Graduate Medical Education by Establishing New Teaching Hospitals and Residency Programs. Acad Med. 2015 Sep;90(9):1264–8. doi: 10.1097/ACM.0000000000000803. [DOI] [PubMed] [Google Scholar]
- 27.Georgia Center for Obstetrics Re-Entry Program, Augusta Univeristy. [cited Dec 1, 2017]; Available from: https://www.augusta.edu/mcg/obgyn/documents/georgiacorp.pdf.
- 28.Centering Pregnancy Georgia. [cited Dec 1, 2017]; Available from: http://www.centeringgeorgia.org/aboutus.html.
- 29.Ickovics JR, Kershaw TS, Westdahl C, Magriples U, Massey Z, Reynolds H, et al. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstet Gynecol. 2007 Aug;110(2 Pt 1):330–9. doi: 10.1097/01.AOG.0000275284.24298.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tanner-Smith EE, Steinka-Fry KT, Lipsey MW. Effects of CenteringPregnancy group prenatal care on breastfeeding outcomes. J Midwifery Womens Health. 2013 Jul-Aug;58(4):389–95. doi: 10.1111/jmwh.12008. [DOI] [PubMed] [Google Scholar]
- 31.Biermann J, Dunlop AL, Brady C, Dubin C, Brann A., Jr Promising practices in preconception care for women at risk for poor health and pregnancy outcomes. Matern Child Health J. 2006 Sep;10(5 Suppl):S21–8. doi: 10.1007/s10995-006-0097-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stafford J, Lathrop E, Haddad L. Health literacy and associated outcomes in post partum period at Grady Memorial Hospital. American College of Obstetricians and Gynecologists 2016 Annual Clinical and Scientific Meeting Washington DC: Obstet Gynecol; 2016; pp. 66S–7S. [Google Scholar]
- 33.Shulman R, Kottke M. Impact of maternal knowledge of recommended weight gain in pregnancy on gestational weight gain. Am J Obstet Gynecol. 2016 Jun;214(6):754 e1–7. doi: 10.1016/j.ajog.2016.03.021. [DOI] [PubMed] [Google Scholar]
- 34.Martin A, Krishna I, Ellis J, Paccione R, Badell M. Super obesity in pregnancy: difficulties in clinical management. J Perinatol. 2014 Jul;34(7):495–502. doi: 10.1038/jp.2014.4. [DOI] [PubMed] [Google Scholar]
- 35.Hofler LG, Cordes S, Cwiak CA, Goedken P, Jamieson DJ, Kottke M. Implementing Immediate Postpartum Long-Acting Reversible Contraception Programs. Obstet Gynecol. 2017 Jan;129(1):3–9. doi: 10.1097/AOG.0000000000001798. [DOI] [PubMed] [Google Scholar]
- 36.Liles I, Haddad LB, Lathrop E, Hankin A. Contraception Initiation in the Emergency Department: A Pilot Study on Providers’ Knowledge, Attitudes, and Practices. South Med J. 2016 May;109(5):300–4. doi: 10.14423/SMJ.0000000000000457. [DOI] [PubMed] [Google Scholar]
- 37.Gostin LO, Lucey D, Phelan A. The Ebola epidemic: a global health emergency. JAMA. 2014 Sep 17;312(11):1095–6. doi: 10.1001/jama.2014.11176. [DOI] [PubMed] [Google Scholar]
- 38.Jamieson DJ, Uyeki TM, Callaghan WM, Meaney-Delman D, Rasmussen SA. What obstetrician-gynecologists should know about Ebola: a perspective from the Centers for Disease Control and Prevention. Obstet Gynecol. 2014 Nov;124(5):1005–10. doi: 10.1097/AOG.0000000000000533. [DOI] [PubMed] [Google Scholar]
- 39.Frieden TR. SHATTUCK LECTURE: The Future of Public Health. N Engl J Med. 2015 Oct 29;373(18):1748–54. doi: 10.1056/NEJMsa1511248. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


