Abstract
Purpose of Review
This review will focus on the evaluation and management of patellar instability in the developing patient.
Recent Findings
A large number of surgical techniques have been described to prevent recurrent patellofemoral instability in the pediatric population, including both proximal and distal realignment procedures. The wide variety of treatment options highlights the lack of agreement as to the best surgical approach. However, when a comprehensive exam and workup are paired with a surgical plan to address each of the identified abnormalities, outcomes are predictably good.
Summary
Patellar instability is a common knee disorder in the skeletally immature patient that presents a unique set of challenges. Rates of re-dislocation in pediatric and adolescent patients are higher than in their adult counterparts. Careful consideration of the physeal and apophyseal anatomy is essential in these patients. While the majority of primary patellar instability events can be treated conservatively, multiple events often require surgical intervention.
Keywords: Pediatric patellar instability, MPFL, Growth plate, Guided growth, Modified Grammont
Introduction
An acute patellofemoral dislocation is the most common acute knee injury in children [1, 2]. Recent studies suggest up to 40% of immature patients may develop recurrent instability [3]. Furthermore, recent studies also highlight that up to 10% of these patients may develop contralateral knee patellar instability and 20% may develop arthritis within 20 years following the initial dislocation [4•].
Classification
Historically, multiple classification systems have been proposed to describe lateral patellar instability, based primarily on symptoms or etiology. Chotel et al. expanded on these systems to describe five patterns of patellar instability [5]:
Congenital dislocation is driven by a short, externally rotated quadriceps muscle manifesting with genu valgum, fixed knee flexion, and an irreducible patella. Abnormal development of the patellofemoral articulation leads to a flat trochlea and hypoplastic patella.
Permanent dislocation occurs after walking age. It is distinguished morphologically by normal patellar height and an intact, rounded lateral trochlea and single-facet patella. Antalgic gait is quite common.
Habitual dislocation in knee flexion is driven by a short vastus lateralis and evident at variable angles of flexion. The patella reduces in extension, and children may experience difficulty with activities that involve running or jumping.
Habitual dislocation in knee extension manifests with preserved patellofemoral articulation through most of the motion arc until the knee is near full extension. The patella slides over the lateral trochlea into a dislocated position.
Episodic/recurrent instability presents near adolescence, more commonly in females, and is typically associated with a specific sports-related event. Patellar apprehension is more prevalent than pain. This is the most common type of patellar instability.
Parikh and Lykissas proposed a classification system seeking to incorporate the patient’s history of dislocations, the morphology of the patellofemoral articulation, and examination findings [6]. Type I represents a first patellofemoral dislocation, with (A) or without (B) osteochondral fracture. Type II represents recurrent subluxation (A) or dislocation (B). Type III represents a dislocatable patella by the examiner or patient which is either passive (A) or habitual in flexion/extension (B). Type IV is a dislocated patella that is either reducible (A) or irreducible (B).
To augment the above classification systems, it may be important to consider other etiologies of patellar instability. Syndromic instability refers to that occurring in the setting of neuromuscular, connective tissue, or other disorders. Disorders commonly associated with patellar instability include the following: cerebral palsy, Ehlers-Danlos syndrome, Marfan Syndome, Down syndrome, Ellis-van Creveld syndrome, nail-patella syndrome, Rubenstein-Taybi syndrome, Kabuki syndrome, and hypoplastic patella syndromes [5, 7, 8].
Risk Factors for Instability
Dejour et al. described four main morphologic risk factors contributing to patellar instability including trochlear dysplasia, patella alta, patellar tilt and a laterally placed tibial tubercle with resultant increased Q angle [9] (Table 1). Trochlear dysplasia and associated lateral femoral condyle hypoplasia both increase the sulcus angle and therefore decrease the bony constraint of the trochlea. Patella alta decreases the effective constraint of the trochlear sulcus by delaying patellofemoral engagement with knee flexion. A lateralized tibial tubercle also creates a net resultant lateral force vector predisposing the patella to lateral instability. Altered force vectors can also be the result of vastus medialis obliquus (VMO) dysplasia or over-pull of lateral structures such as the vastus lateralis and iliotibial band.
Table 1.
DeJour factors contributing to patellar instability [9]
| DeJour four main factors driving instability | Features |
|---|---|
| TT:TG | > 20 mm abnormal, 15–20 equivocal but in pediatric patients with instability average 12.1 mm21 |
| Patellar Tilt | > 20° |
| Caton-Deschamps | > 1.3 |
| Trochlear Dysplasia | 4 Types described by DeJour A = shallow, crossover B = flat with supratrochlear spur C = hypoplasia media, convex, double contour D = Cliff, crossover and supratrochlear spur |
The contribution of these factors in recurrent patellar instability was reported by Christensen et al. in a retrospective review noting an increased odds ratio (OR) with trochlear dysplasia (OR, 18.1), patella alta (OR, 10.4), and elevated TT-TG distance (OR, 2.1) [10•]. Additional contributing general factors included age < 18 at time of first dislocation (OR, 2.4) and female sex (OR, 2.1).
Recent literature continues to highlight the importance of trochlear dysplasia as a risk factor for recurrent instability [3, 11]. First-time pediatric dislocators had a 38% recurrence rate, but if trochlear dysplasia was present, this number jumped to 69% [3]. Furthermore, a study looking at the anatomic patellar instability risk factors identified that 74% of patients in the dislocation group had trochlear dysplasia whereas only 4% of patients in the control group met criteria for trochlear dysplasia.
Additional risk factors include ligamentous laxity and connective tissue disorders. Marfan syndrome and Ehlers-Danlos, for instance, affect the strength of medial peripatellar retinacular structures such as the MPFL.
Physical Exam
Physical examination of the patient should begin with evaluation of overall limb alignment including genu valgum or varum, patellar height, quadriceps’ girth, and tone. Mobility of the patella is assessed with the knee in full extension and considered abnormal when there is greater than 2 quadrants of translation. Ahmad et al. describe the Moving Patellar Apprehension Test that has 100% sensitivity and 88.4% specificity [12]. The test is performed by taking the knee from full extension into flexion with a laterally directed force on the patella. This causes apprehension and involuntary quad activation by the patient to prevent further knee flexion. In the second part of the test, the knee is again taken from extension to flexion, this time with a medially directed force on the patella. A positive test shows no apprehension in this phase and the patient allows the knee to be fully flexed. The patient is then checked for generalized ligamentous laxity with the Beighton score (Table 2). Six or more points qualify a patient as being ligamentously lax, with further discussion in the “Special Considerations” section.
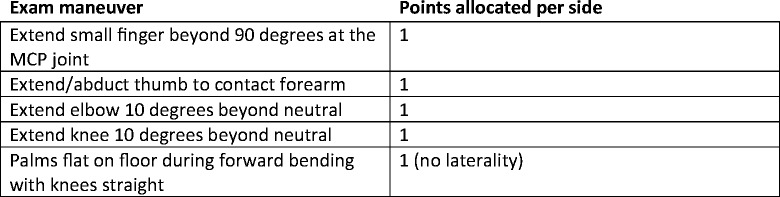
Table 2.
Joint hypermobility assessment with the Beighton score. A total of 9 points is possible based on bilateral findings. In children and adolescents, a positive score is considered greater than 6 points. A score greater than 8 points may influence surgical techniques
Patellar tracking is best assessed with active knee range of motion in a seated position. The presence of a J sign is noted with excessive lateral translation of the patella as it disengages from the trochlear groove in extension and is often associated with patella alta and trochlear dysplasia. The presence of crepitus can indicate concomitant osteochondral injury.
In the acutely dislocated patella, there may be a large hemarthrosis, with medial knee pain indicating injury to the MPFL, and lateral knee pain due to contusion of the patella against the lateral femoral condyle. Focal tenderness over the MPFL femoral insertion site is called “Bassett’s sign” [13]. The absence of these findings should raise concern regarding chronic, congenital, or habitual patellar instability warranting additional evaluation. Lastly, dysmorphic features, size of the patella, and location of the patella at rest should also be noted as patellar instability can be an isolated feature in a larger constellation of abnormalities as seen in Nail-patella Syndrome, Ehlers-Danlos, or Down Syndrome.
Imaging
Plain radiographs are a key component of the static diagnostic evaluation of older children and adolescents and should include four views: anteroposterior (AP), weightbearing Rosenberg (bent knee PA), lateral, and sunrise (bent knee axial). Dejour et al. provide the seminal description of radiographic parameters in patellar instability [9]. On the sunrise view, one can quantify patellar tilt (Laurin’s angle) and subluxation (Merchant’s congruence angle). The lateral view can be used to assess for trochlear dysplasia, which can be graded as type I (minor dysplasia), type II, or type III (major dysplasia).
The lateral view has received particular attention for the multiple methods reported to assess patellar height, amongst them the Blackburne-Peel ratio [14], Koshino ratio [15], Insall-Salvati Ratio [16], and Caton-Deschamps index (CDI) [17, 18]. The CDI is now commonly regarded as having the highest fidelity in skeletally immature patients. Aparicio et al. evaluated three parameters in 36 lateral knee radiographs of unaffected patients and found the Caton-Deschamps to have the lowest interobserver variability and was the least affected by the patient’s skeletal maturity [19]. Thévenin-Lemoine et al. reviewed 300 lateral knee radiographs in unaffected children and established an index of Caton-Deschamps ratios across age groups [17].
The study of choice in assessing patients with patellar instability has become the MRI (Fig. 1a, b). In addition to demonstrating any osteochondral injuries and the status of the physes, MRI provides further morphologic information to stratify patients at risk and to guide treatment planning. One parameter to consider is the tibial tubercle-trochlear groove (TT-TG) distance, which quantifies how lateralized the patellar tendon insertion is on the tibia. Two recent studies demonstrate high intra- and interobserver reliability of TT-TG measurements across interdisciplinary providers [20] and in children [21]. Historically, adult references for abnormal TT-TG distances have been used to guide pediatric treatment planning [22]. Dickens et al. showed that normal TT-TG distances in children increase with chronologic age. They found that a TT:TG of 8.6 mm correctly predicted no patellar instability in 95% of their patients and patients with instability had a TT:TG mean of 12.1 [21]. They developed a percentile-based growth chart in order to help depict normal TT-TG in the developing patient population.
Fig. 1.
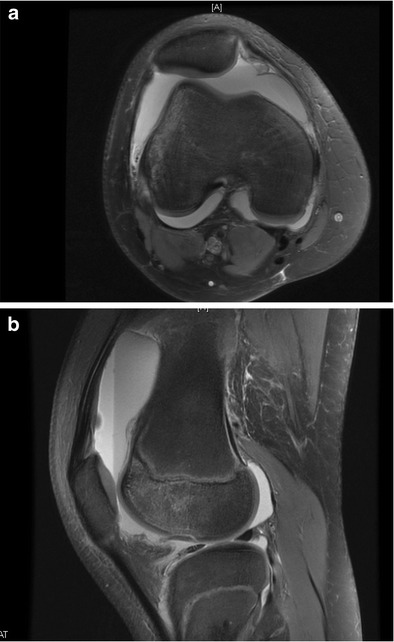
a, b Axial and sagittal image of recent patellar dislocation MRI in a 12-year-old girl. Note the lipohemarthrosis and the osteochondral injury involving the lateral femoral condyle (sagittal view)
The natural progression of this growing body of morphologic data is to develop a predictive or prognostic tool to determine which patients are at greater risk of recurrent patellar instability following an index dislocation. Lewallen et al. reviewed 222 knee radiographs in patients of varying skeletal maturity and found that trochlear dysplasia and open physes conferred an odds ratio (OR) of 3.3 for a second instability episode at mean follow-up of 3.1 years [3].
Jaquith and Parikh reviewed demographic and radiographic data in 266 patients and proposed the following four binary items as risk factors for recurrent instability: any trochlear dysplasia (OR 3.6), history of contralateral patellar dislocation (OR 3.1), skeletal immaturity (OR 2.2), and Caton-Deschamps ratio > 1.45 (OR 2.1) [23•]. The recurrence risk increases from 14% in a first-time dislocator with none of the above risk factors to 88% in a patient with all four factors (Table 3). Currently, the JUPITER Group (Justifying Pediatric Instability Treatment by Early Reporting) is expanding on the work of Parikh by adding MRI and Beighton scores in generating a new prognostic tool for predicting patellar instability.
Table 3.
Increase in recurrence risk of patellar dislocation after a first-time dislocation event as demonstrated by Jaquith and Parikh [23•] (reprinted with permission from publisher). The four risk factors comprise of any trochlear dysplasia, history of contralateral patellar dislocation, skeletal immaturity, and Caton-Deschamps ratio > 1.45
| Number of risk factors | Recurrence risk (%) |
|---|---|
| 0 | 14 |
| 1 | 30 |
| 2 | 54 |
| 3 | 75 |
| 4 | 88 |
Non-operative Management
Non-operative management of first-time patellar instability is the current standard of care unless there is an associated osteochondral fragment (≥ 5 mm), osseous avulsion of the MPFL or an associated meniscus tear [13, 24, 25]. This was agreed upon during a consensus statement from the International Patellofemoral Group [26]. There is no evidence at this time of the superiority of one treatment protocol versus another after first-time dislocation, but full recovery time traditionally takes 3 months. The initial aim after the acute dislocation is to decrease swelling and pain, strengthen the vastus medialis and gluteal muscles, and regain motion to the knee. Recommendations vary significantly on duration of and need for immobilization after a first-time dislocation. Some authors recommend immediate mobilization whereas others recommend up to 6 weeks of cast or splint immobilization [27]. In a study of 100 patients in Finland with primary acute patella dislocation were treated with either a cast, posterior splint, or a patella brace/bandage, at 13 year average follow up, the posterior splint group had the lowest re-dislocation rate. There was a three-fold increase in patella instability in patients treated with the patella brace [28]. However, Buchner et al. found that short periods of immobilization can significantly increase muscle atrophy [29]. Currently, our rehab protocol immobilizes the patient for 3 weeks in a lateral J type brace and then focuses on increasing mobility (regressive immobilization) 29. Physical therapy emphasizes isometric quadriceps strengthening, specific VMO strengthening, and progression to more dynamic exercises involving the core and gluteal muscles [30]. Return to sport and activity is only allowed after full recovery of knee motion, strength, absence of a knee effusion and pain, and demonstration of competence with sport specific exercises. We recommend the developing athlete wear a lateral stabilizing brace with sport and activity for 1 year after the initial injury. The brace can heighten the patient’s sense of patellar stability. Adjunctive taping with kinesio-tape can also be utilized during the return to sport phase.
Operative Management
Proximal Realignment
Medial Repair
Medial repair either through imbrication or reefing has been described for treatment of patellar instability with variable results. Palmu et al. reported recurrence rates of 71% with direct repair with no significant difference compared to non-operative treatment [31]. Others have reported lower recurrence rates ranging from 12 to 30% in the adolescent population [32, 33]. Ahmad et al. reported no re-dislocations in a series of 8 patients treated with direct repair of the MPFL and the VMO [24]. However, because imbrication and reefing are non-anatomic procedures, some have raised concern over the altered joint reactive forces [34] and kinematics [35] with such procedures.
Medial Patellofemoral Reconstruction
Advances in the understanding of MPFL anatomy and the role it plays in lateral patellar dislocation as the “essential lesion” have redirected soft tissues treatment strategies to focus on its reconstruction (Fig. 2a). Multiple techniques have been described including the utilization of hamstring autograft, various allografts (gracilis, semitendinosus, tibialis anterior, tibialis posterior) in both anatomic and non-anatomic fashions (quadriceps turn down, adductor sling) with various forms of fixation (suspensory, interference screw, suture anchor). Outcomes are generally reported to be good with low rates of re-dislocation; however, there is a paucity of literature to establish a direct advantage of a certain graft, fixation, or technique choice.
Fig. 2.
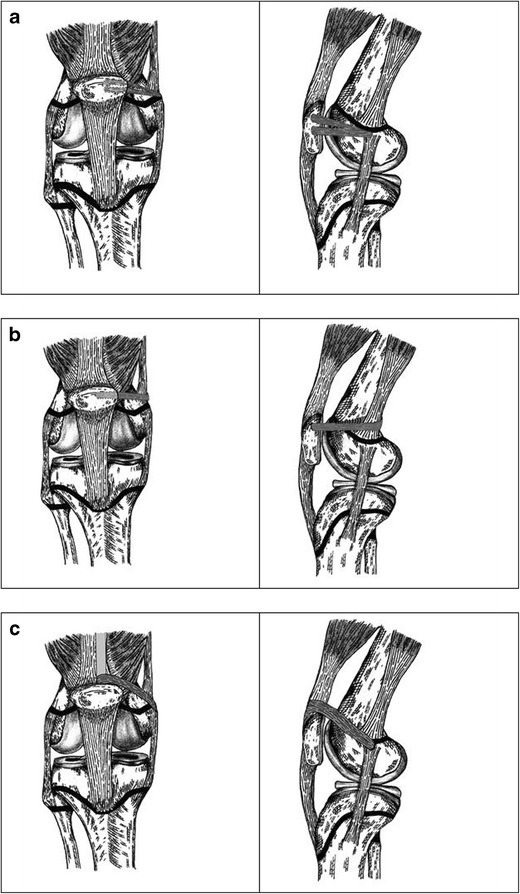
Proximal reconstructions (all artwork original and drawn by Evan Trupia, MD). a MPFL. b Adductor sling. c Quadriceps turndown/HemiQuad
Much attention has been directed towards the femoral origin of the MPFL as non-isometric attachment sites have been related to poor outcomes. The MPFL femoral origin is at the midpoint between the adductor tubercle and medial epicondyle in the skeletally mature [36–39] and radiographically represented as Schöttle’s point [40]. Rather than a single point, this insertion should be referred to as Schöttle’s cloud. The anatomic location is of concern in the skeletally immature knee as this site is almost always in close proximity to the distal femoral physis. Radiographic and cadaveric studies have reported the femoral origin site to be just proximal to the physis [41], variably around the physis [42], with the majority reporting the location to be just distal to the physis [43–45].
To avoid the distal femoral physis, the adductor sling has been described in which a graft is looped around the tendon of the adductor magnus at its femoral insertion and secured on the medial aspect of the patella (Fig. 2b) [46]. Some have advocated for the quadriceps tendon turn down to avoid the potential complication of patella fractures during patellar drilling (Fig. 2c) [47]. This technique takes advantage of the natural quadriceps tendons’ attachment to the patella but results in a non-anatomic MPFL reconstruction which is currently of unknown significance.
Distal Realignment
Patients with patella alta or increased TT-TG distances may benefit from functional or explicit realignment of the patellar tendon insertion distally. In the setting of open apophyses and concern for growth injury, multiple techniques have been developed.
The Roux-Goldthwait procedure was originally described in the late 1800s and has been evaluated in several modern series with satisfactory outcomes [48, 49]. The lateral one-half of the patellar tendon is split, detached from the tibial tuberosity, and transferred deep to the medial tendon before securing it to the periosteum and soft tissues of the medial tibia.
Galeazzi originally described a tenodesis technique in 1922 in which the semitendinosus tendon is harvested from its distal insertion and secured to the medial patella in an oblique manner (Fig. 3) [50]. Performed in isolation with minor modifications, outcomes of this tenodesis have varied with respect to recurrent instability and knee function. The original series and subsequent studies showed 80–88% good to excellent results with re-dislocation rates lower than 10% in most series [51, 52]. However, a recent long-term follow-up study by Grannatt et al. demonstrated 28 of 34 patients reported recurrent instability (82%) with 41% of those patients requiring subsequent surgical stabilization [53].
Fig. 3.
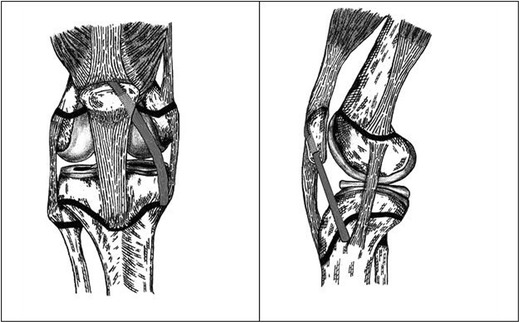
Distal reconstructions. Galeazzi Procedure
Kraus et al. report favorable outcomes in 65 knees of a modification of a technique originally described by Grammont [54]. Following a lateral retinacular release, the distal patellar tendon is dissected sharply from the apophysis while preserving a periosteal attachment and elevating a portion of the periosteum distally. The technique allows the tendon to glide medially in a more centralized position. The original technique by Grammont et al. was published in German and included fixation of the medial patella to the tibia [55] The modified Grammont procedure is slowly gaining traction in the USA for patients with elevated TT-TG distances, patella alta, and hyperlaxity in whom there is a high concern that an MPFL reconstruction or adductor sling alone may have a high failure rate.
Guided Growth
Genu valgum can be a contributor to patellar instability and warrants consideration in the developing child [1, 56•]. Clinically, pathologic genu valgum is defined as a patient with an intermalleolar distance greater than 8 cm and a tibiofemoral angle > 15° [57]. Radiographically, to meet criteria, the anatomic lateral distal femoral angle (aLDFA) < 79°, the anatomic medial proximal tibial angle can be aMPTA > 90° with the mechanical axis falling in the lateral compartment of the knee. The principle of guided growth in these patients is to improve patellar stability by restoring the normal anatomic relationship between the knee joint and the extensor mechanism by correcting the patient’s mechanical axis to the center of the knee [56•].
For these patients, it is recommended to use guided growth to slowly correct the valgus deformity. The patients should be followed with interval 3 joint standing radiographs, and the implants should be removed when the mechanical axis is restored to normal.
Kearney and Mosca reported their series of hemiepiphysiodesis in 26 knees utilizing both staples and 8 plates [56•]. All of these involved hemiephysiodsesis of the medial distal femurs and 4 knees required medial tibial plates as well for aMPTA > 90°. The authors reported 69% had complete symptom resolution and all 6 of their competitive athletes in the series returned to sport. They removed the hardware at an average of 9.6 months from the procedure to prevent overcorrection. One patient required reoperation for a staple that backed out of place. The authors did not include clinical and radiographic pre and post op alignment measures, and this study is only relevant for patients with genu valgum contributing to their instability.
Special Considerations
Chondral Shear Injuries
In the setting of patellar instability, one reason to operate on a pediatric patient is an osteochondral injury [26]. However, it is not uncommon when closely examining the injured piece to find that there is no attached bone. Traditional teaching is that cartilage only injuries cannot be reaffixed and are doomed to fail. Chondral only in this study was defined as inability to see the fragment on radiographs and the inability to see any bone on the fragment intraoperatively [58•]. Recent experience and literature is suggesting that this may not be the case in pediatric and adolescent patients. Fabricant et al. reported their findings of chondral-only shear fractures of the knee in ten patients [58•]. Fragments were fixed an average of 1.3 weeks from injury, and the average age at time of surgery for the patients was 12.5 years. One patient had re-injury at 8 weeks and required fragment excision. The authors were able to obtain 6 MRIs postoperatively and found resolution of edema and incorporation in 3 of the 6 MRIs (50%). One patient showed thinning of the cartilage, one had thickening of the cartilage, and one MRI signs consistent with the lesion not healing (edema, cysts, and fissures). The overall return to activity in these patients took almost 6 months. Fixation of these chondral only injuries can be done with bioabsorbable tacks or screws. The patients need to be followed closely with physical exam with special attention paid to any mechanical symptoms or effusion.
Technical Challenges for MPFL After Guided Growth
Guided growth with a temporary hemiephiphysiodesis (TH) has a role in the developing patient with significant genu valgum. There are some important technical considerations to consider when planning a MPFL reconstruction with a tension-band plate. If the plate is placed first and the MPFL reconstruction over the top, this can cause fraying and graft failure. If the MPFL is reconstructed and then the TH is performed, there can be a functional shortening of the graft which can cause early failure of the MPFL. In a cadaveric study, the authors demonstrated that during placement of the tension band plate for the TH in 8 knees, there were 2 cases of the MPFL being transected and 4 others with significant damage, a 75% injury rate (6/8) [59•].
There are options to circumvent these potential technical issues that arise with patients who would benefit from the guided growth and MPFL. The first is to utilize a type of TH technique described by Métaizeau et al. for percutaneous epiphysiodesis transphyseal screw placement (PETS) [60]. The course of the screw is from proximal-lateral to distal medial and comes anterior to the placement of the MPFL graft. Early work by Parikh out of the Patellofemoral Study group have demonstrated that this can be done safely without injury to the MPFL reconstruction with the benefit of doing both procedures in the same setting [61]. This is an ideal choice for the patient with 2–3 years of growth remaining.
Another option is to do the TH as the initial procedure and then perform the MPFL reconstruction when the surgeon goes back to remove the hardware. This is the preferred option for very young children (< 10 years of age) with many years of growth remaining. There are couple additional pearls with this approach that warrant further discussion. The screw holes from the tension band plate are often close to the anatomic insertion of the MPFL on the femur in the saddle area. For this type of MPFL, it is recommended to use suture anchors instead of a larger interference screw for fixation of the graft on the femur. This modification minimizes the chance of the femoral socket breaking into a previous hole from the tension band plate [60].
Role of Generalized Laxity in Decision Making
The use of the Beighton score helps to identify patients with hypermobility. This is a 9-point scale that requires the use of 5 maneuvers, 4 passive and one active to assess mobility (see Table 2). According to Beighton and Horan original criteria, generalized laxity is present with a score of 6 or greater [62].
For adolescent and pediatric patients, we use a Beighton score of 6 to help our decision making. In patients with a Beighton score of 6 and higher, if an MPFL reconstruction is part of the surgical plan, we recommend using allograft as opposed to autograft hamstring. Additionally, any patient presenting with a perfect 9/9 is referred to genetics for Ehlers-Danlos/connective tissue disorder testing.
A very elevated Beighton score can also factor into the surgical decision in a patient with mild patella alta (CD 1.35), borderline TT-TG of 19 and a Beighton score of 8. In such a patient, it may be the more prudent to perform a Modified Grammont tibial tubercle periosteum transfer if the growth plates are open in addition to the MPFL.
Return to Play Considerations in the Pediatric and Adolescent Patient
The current literature on return to play and activity after patellar instability surgery is limited and poorly described [63•, 64]. A recent systematic review by Zaman et al. identified a lack of objective guidelines for return to play after patellar instability. There was a wide range of time lines and criteria in the 53 studies reviewed. With the lack of agreement, we recommend using the criteria set forward by Menetrey et al. [65] when deciding to allow an athlete to return after patellar instability: no pain, full motion, no effusion, no objective patellofemoral instability on exam, near symmetric strength (85% limb symmetry), and excellent dynamic stability (therapist feels patient doing sport-specific drills with no hesitation). Time guidelines in the literature range from anywhere from 3 to 8 months and depend on concomitant procedures performed [63•, 64].
Complications
There are potential complications which can arise from the management of pediatric and adolescent patellar instability. The first is injury to the growth plate causing a physeal arrest. This can occur in the patients with open growth plates undergoing MPFL reconstruction or can result from an arrest with the Modified Grammont technique involving the tibial tubercle. Management of a partial physeal arrest can include additional surgery to correct the arrest either by completion, excision, or hemiepiphysiodesis. The index surgery, particularly for the MPFL reconstruction with open growth plates, should be performed with the aid of fluoroscopy to confirm that the tunnel or implant will not violate the growth plate. Knee arthrofibrosis is also a potential complication and can occur from improperly placed MPFL grafts, combined surgeries (cartilage injury), and prolonged immobilization [66]. Current MPFL reconstruction technique use bone tunnels for anchors or transosseous drilling for docking which can cause patellar fracture [67]. There are reports of patella fracture occurring after MPFL reconstruction [68, 69]. Fulkerson’s MQTFL reconstruction has been a proposed solution to the patella fracture issue by avoiding drilling in the patella all together [67]. Recurrent instability, failure of the procedure, inability to return to sport, wound infection, quadriceps weakness, and neuroma formation are all possible complications in the pediatric and adolescent patient being treated surgically for patellar instability.
Conclusion
Patellar instability is a common condition seen in pediatric and adolescent patients. The treatment course for developing patients is a challenge as there are many factors at play causing the instability as these individuals mature. A comprehensive workup and understanding of the anatomy, biomechanics, and ligamentous laxity are essential in formulating a treatment plan to prevent re-dislocation and allow return to activity.
Compliance with Ethical Standards
Conflict of Interest
All authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Advances in Patellofemoral Surgery
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Hennrikus W, Pylawka T. Patellofemoral instability in skeletally immature athletes. J Bone Joint Surg Am. 2013;95(2):176–183. [PubMed] [Google Scholar]
- 2.Weeks KD, 3rd, Fabricant PD, Ladenhauf HN, Green DW. Surgical options for patellar stabilization in the skeletally immature patient. Sports Med Arthrosc. 2012;20(3):194–202. [PubMed] [Google Scholar]
- 3.Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med. 2013;41(3):575–581. doi: 10.1177/0363546512472873. [DOI] [PubMed] [Google Scholar]
- 4.• Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ. High rate of recurrent patellar dislocation in skeletally immature patients: a long-term population-based study. Knee Surg Sports Traumatol Arthrosc. 2017. Skeletally immature patients had a high rate of recurrent instability , 10% of patients in this long term study developed contralateral dislocation and 20% of patients had arthritis at 20 year follow up. [DOI] [PubMed]
- 5.Chotel F, Berard J, Raux S. Patellar instability in children and adolescents. Orthop Traumatol Surg Res. 2014;100(1 Suppl):S125–S137. doi: 10.1016/j.otsr.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 6.Parikh SN, Lykissas MG. Classification of lateral patellar instability in children and adolescents. Orthop Clin North Am. 2016;47(1):145–152. doi: 10.1016/j.ocl.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 7.Gong Y, Yang C, Liu Y, Liu J, Qi X. Treatment of patellar instability in a case of hereditary onycho-osteodysplasia (nail-patella syndrome) with medial patellofemoral ligament reconstruction: A case report. Exp Ther Med. 2016;11(6):2361–2364. doi: 10.3892/etm.2016.3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rouffiange L, Dusabe JP, Docquier PL. Recurrent dislocation of the patella in kabuki make-up syndrome. Case Rep Orthop. 2012;2012:501453. doi: 10.1155/2012/501453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 10.Christensen TC, Sanders TL, Pareek A, Mohan R, Dahm DL, Krych AJ. Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am J Sports Med. 2017;45(9):2105–2110. doi: 10.1177/0363546517704178. [DOI] [PubMed] [Google Scholar]
- 11.Askenberger M, Janarv PM, Finnbogason T, Arendt EA. Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations: a prospective magnetic resonance imaging study in skeletally immature children. Am J Sports Med. 2017;45(1):50–58. doi: 10.1177/0363546516663498. [DOI] [PubMed] [Google Scholar]
- 12.Ahmad CS, McCarthy M, Gomez JA, Shubin Stein BE. The moving patellar apprehension test for lateral patellar instability. Am J Sports Med. 2009;37(4):791–796. doi: 10.1177/0363546508328113. [DOI] [PubMed] [Google Scholar]
- 13.Khormaee S, Kramer DE, Yen YM, Heyworth BE. Evaluation and management of patellar instability in pediatric and adolescent athletes. Sports Health. 2015;7(2):115–123. doi: 10.1177/1941738114543073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59(2):241–242. doi: 10.1302/0301-620X.59B2.873986. [DOI] [PubMed] [Google Scholar]
- 15.Koshino T, Sugimoto K. New measurement of patellar height in the knees of children using the epiphyseal line midpoint. J Pediatr Orthop. 1989;9(2):216–218. [PubMed] [Google Scholar]
- 16.Grelsamer RP, Meadows S. The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop Relat Res. 1992;282:170–176. [PubMed] [Google Scholar]
- 17.Thevenin-Lemoine C, Ferrand M, Courvoisier A, Damsin JP, Ducou le Pointe H, Vialle R. Is the Caton-Deschamps index a valuable ratio to investigate patellar height in children? J Bone Joint Surg Am. 2011;93(8):e35. doi: 10.2106/JBJS.J.00759. [DOI] [PubMed] [Google Scholar]
- 18.Caton J, Deschamps G, Chambat P, Lerat J, Dejour H. Les rotules basses:a propos de 128 observations. Rev Chir Orthop Reparatrice Appar Mot. 1982;68:317–325. [PubMed] [Google Scholar]
- 19.Aparicio G, Abril JC, Albinana J, Rodriguez-Salvanes F. Patellar height ratios in children: an interobserver study of three methods. J Pediatr Orthop B. 1999;8(1):29–32. [PubMed] [Google Scholar]
- 20.Skelley N, Friedman M, McGinnis M, Smith C, Hillen T, Matava M. Inter- and intraobserver reliability in the MRI measurement of the tibial tubercle-trochlear groove distance and trochlea dysplasia. Am J Sports Med. 2015;43(4):873–878. doi: 10.1177/0363546514565768. [DOI] [PubMed] [Google Scholar]
- 21.Dickens AJ, Morrell NT, Doering A, Tandberg D, Treme G. Tibial tubercle-trochlear groove distance: defining normal in a pediatric population. J Bone Joint Surg Am. 2014;96(4):318–324. doi: 10.2106/JBJS.M.00688. [DOI] [PubMed] [Google Scholar]
- 22.Balcarek P, Jung K, Frosch KH, Sturmer KM. Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med. 2011;39(8):1756–1761. doi: 10.1177/0363546511404883. [DOI] [PubMed] [Google Scholar]
- 23.Jaquith BP, Parikh SN. Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. J Pediatr Orthop. 2017;37(7):484–490. doi: 10.1097/BPO.0000000000000674. [DOI] [PubMed] [Google Scholar]
- 24.Ahmad CS, Stein BE, Matuz D, Henry JH. Immediate surgical repair of the medial patellar stabilizers for acute patellar dislocation. A review of eight cases. Am J Sports Med. 2000;28(6):804–810. doi: 10.1177/03635465000280060701. [DOI] [PubMed] [Google Scholar]
- 25.Christiansen SE, Jakobsen BW, Lund B, Lind M. Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy. 2008;24(8):881–887. doi: 10.1016/j.arthro.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 26.Liu JN, Steinhaus ME, Kalbian IL, et al. Patellar instability management: a survey of the International Patellofemoral Study Group. Am J Sports Med. 2017:363546517732045. [DOI] [PubMed]
- 27.Dixit S, Deu RS. Nonoperative treatment of patellar instability. Sports Med Arthrosc. 2017;25(2):72–77. doi: 10.1097/JSA.0000000000000149. [DOI] [PubMed] [Google Scholar]
- 28.Maenpaa H, Lehto MU. Patellar dislocation. The long-term results of nonoperative management in 100 patients. Am J Sports Med. 1997;25(2):213–217. doi: 10.1177/036354659702500213. [DOI] [PubMed] [Google Scholar]
- 29.Buchner M, Baudendistel B, Sabo D, Schmitt H. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med. 2005;15(2):62–66. doi: 10.1097/01.jsm.0000157315.10756.14. [DOI] [PubMed] [Google Scholar]
- 30.Hasler CC, Studer D. Patella instability in children and adolescents. EFORT Open Rev. 2016;1(5):160–166. doi: 10.1302/2058-5241.1.000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(3):463–470. doi: 10.2106/JBJS.G.00072. [DOI] [PubMed] [Google Scholar]
- 32.Hartmann F, Dietz SO, Rommens PM, Gercek E. Long-term outcome after operative treatment of traumatic patellar dislocation in adolescents. J Orthop Trauma. 2014;28(3):173–180. doi: 10.1097/BOT.0b013e318299cb50. [DOI] [PubMed] [Google Scholar]
- 33.Ma LF, Wang CH, Chen BC, et al. Medial patellar retinaculum plasty versus medial capsule reefing for patellar dislocation in children and adolescents. Arch Orthop Trauma Surg. 2012;132(12):1773–1780. doi: 10.1007/s00402-012-1598-0. [DOI] [PubMed] [Google Scholar]
- 34.Edmonds EW, Glaser DA. Adolescent patella instability extensor mechanics: Insall extensor realignment versus medial patellofemoral ligament reconstruction. J Pediatr Orthop. 2016;36(3):262–267. doi: 10.1097/BPO.0000000000000430. [DOI] [PubMed] [Google Scholar]
- 35.Ostermeier S, Holst M, Hurschler C, Windhagen H, Stukenborg-Colsman C. Dynamic measurement of patellofemoral kinematics and contact pressure after lateral retinacular release: an in vitro study. Knee Surg Sports Traumatol Arthrosc. 2007;15(5):547–554. doi: 10.1007/s00167-006-0261-0. [DOI] [PubMed] [Google Scholar]
- 36.Kang HJ, Wang F, Chen BC, Su YL, Zhang ZC, Yan CB. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1511–1516. doi: 10.1007/s00167-010-1090-8. [DOI] [PubMed] [Google Scholar]
- 37.Nomura E, Inoue M, Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):510–515. doi: 10.1007/s00167-004-0607-4. [DOI] [PubMed] [Google Scholar]
- 38.Conlan T, Garth WP, Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682–693. doi: 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Tuxoe JI, Teir M, Winge S, Nielsen PL. The medial patellofemoral ligament: a dissection study. Knee Surg Sports Traumatol Arthrosc. 2002;10(3):138–140. doi: 10.1007/s00167-001-0261-z. [DOI] [PubMed] [Google Scholar]
- 40.Schottle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 41.Shea KG, Grimm NL, Belzer J, Burks RT, Pfeiffer R. The relation of the femoral physis and the medial patellofemoral ligament. Arthroscopy. 2010;26(8):1083–1087. doi: 10.1016/j.arthro.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 42.Shea KG, Styhl AC, Jacobs JC, Jr, et al. The relationship of the femoral physis and the medial patellofemoral ligament in children: A Cadaveric Study. Am J Sports Med. 2016;44(11):2833–2837. doi: 10.1177/0363546516656366. [DOI] [PubMed] [Google Scholar]
- 43.Nelitz M, Dornacher D, Dreyhaupt J, Reichel H, Lippacher S. The relation of the distal femoral physis and the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2067–2071. doi: 10.1007/s00167-011-1548-3. [DOI] [PubMed] [Google Scholar]
- 44.Farrow LD, Alentado VJ, Abdulnabi Z, Gilmore A, Liu RW. The relationship of the medial patellofemoral ligament attachment to the distal femoral physis. Am J Sports Med. 2014;42(9):2214–2218. doi: 10.1177/0363546514539917. [DOI] [PubMed] [Google Scholar]
- 45.Shea KG, Polousky JD, Jacobs JC, Jr, et al. The relationship of the femoral physis and the medial patellofemoral ligament in children: a cadaveric study. J Pediatr Orthop. 2014;34(8):808–813. doi: 10.1097/BPO.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 46.Gomes JE. Comparison between a static and a dynamic technique for medial patellofemoral ligament reconstruction. Arthroscopy. 2008;24(4):430–435. doi: 10.1016/j.arthro.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 47.Noyes FR, Albright JC. Reconstruction of the medial patellofemoral ligament with autologous quadriceps tendon. Arthroscopy. 2006;22(8):904 e901–904 e907. doi: 10.1016/j.arthro.2005.12.058. [DOI] [PubMed] [Google Scholar]
- 48.Marsh JS, Daigneault JP, Sethi P, Polzhofer GK. Treatment of recurrent patellar instability with a modification of the Roux-Goldthwait technique. J Pediatr Orthop. 2006;26(4):461–465. doi: 10.1097/01.bpo.0000217711.34492.48. [DOI] [PubMed] [Google Scholar]
- 49.Vahasarja V, Kinnunen P, Lanning P, Serlo W. Operative realignment of patellar malalignment in children. J Pediatr Orthop. 1995;15(3):281–285. doi: 10.1097/01241398-199505000-00002. [DOI] [PubMed] [Google Scholar]
- 50.Galeazzi R. Nuove appliccazioni del trapianto musculare e tendineo [in Italian] Ard Di Orthop Milano. 1922;38:315–323. [Google Scholar]
- 51.Letts RM, Davidson D, Beaule P. Semitendinosus tenodesis for repair of recurrent dislocation of the patella in children. J Pediatr Orthop. 1999;19(6):742–747. [PubMed] [Google Scholar]
- 52.Hall JE, Micheli LJ, McManama GB., Jr Semitendinosus tenodesis for recurrent subluxation or dislocation of the patella. Clin Orthop Relat Res. 1979;144:31–35. [PubMed] [Google Scholar]
- 53.Grannatt K, Heyworth BE, Ogunwole O, Micheli LJ, Kocher MS. Galeazzi semitendinosus tenodesis for patellofemoral instability in skeletally immature patients. J Pediatr Orthop. 2012;32(6):621–625. doi: 10.1097/BPO.0b013e318263a230. [DOI] [PubMed] [Google Scholar]
- 54.Kraus T, Lidder S, Svehlik M, et al. Patella re-alignment in children with a modified Grammont technique. Acta Orthop. 2012;83(5):504–510. doi: 10.3109/17453674.2012.736168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grammont PM, Latune D, Lammaire IP. Treatment of subluxation and dislocation of the patella in the child. Elmslie technic with movable soft tissue pedicle (8 year review) Orthopade. 1985;14(4):229–238. [PubMed] [Google Scholar]
- 56.Kearney SP, Mosca VS. Selective hemiepiphyseodesis for patellar instability with associated genu valgum. J Orthop. 2015;12(1):17–22. doi: 10.1016/j.jor.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Heath CH, Staheli LT. Normal limits of knee angle in white children—genu varum and genu valgum. J Pediatr Orthop. 1993;13(2):259–262. [PubMed] [Google Scholar]
- 58.Fabricant PD, Yen YM, Kramer DE, Kocher MS, Micheli LJ, Heyworth BE. Fixation of chondral-only shear fractures of the knee in pediatric and adolescent athletes. J Pediatr Orthop. 2017;37(2):156. doi: 10.1097/BPO.0000000000000955. [DOI] [PubMed] [Google Scholar]
- 59.Bachmann M, Rutz E, Brunner R, Gaston MS, Hirschmann MT, Camathias C. Temporary hemiepiphysiodesis of the distal medial femur: MPFL in danger. Arch Orthop Trauma Surg. 2014;134(8):1059–1064. doi: 10.1007/s00402-014-2032-6. [DOI] [PubMed] [Google Scholar]
- 60.Metaizeau JP, Wong-Chung J, Bertrand H, Pasquier P. Percutaneous epiphysiodesis using transphyseal screws (PETS) J Pediatr Orthop. 1998;18(3):363–369. [PubMed] [Google Scholar]
- 61.Parikh SN. Surgical correction for patellar instability and genu valgum in skeletally immature patients. Patellofemoral foundation. Update. 2017;
- 62.Beighton P, Horan FT. Surgical aspects of the Ehlers-Danlos syndrome. A survey of 100 cases. Br J Surg. 1969;56(4):255–259. doi: 10.1002/bjs.1800560404. [DOI] [PubMed] [Google Scholar]
- 63.• Zaman S, White A, Shi WJ, Freedman KB, Dodson CC. Return-to-play guidelines after medial patellofemoral ligament surgery for recurrent patellar instability: a systematic review. Am J Sports Med. 2017:363546517713663. Systematic review that emphasizes that more research and work needs to be done to determine safe and effective guidelines for return to play after MPFL. [DOI] [PubMed]
- 64.Krych AJ, O'Malley MP, Johnson NR, et al. Functional testing and return to sport following stabilization surgery for recurrent lateral patellar instability in competitive athletes. Knee Surg Sports Traumatol Arthrosc. 2016. [DOI] [PubMed]
- 65.Menetrey J, Putman S, Gard S. Return to sport after patellar dislocation or following surgery for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2320–2326. doi: 10.1007/s00167-014-3172-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Parikh SN, Nathan ST, Wall EJ, Eismann EA. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41(5):1030–1038. doi: 10.1177/0363546513482085. [DOI] [PubMed] [Google Scholar]
- 67.Fulkerson JP, Edgar C. Medial quadriceps tendon-femoral ligament: surgical anatomy and reconstruction technique to prevent patella instability. Arthrosc Tech. 2013;2(2):e125–e128. doi: 10.1016/j.eats.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Parikh SN, Wall EJ. Patellar fracture after medial patellofemoral ligament surgery: a report of five cases. J Bone Joint Surg Am. 2011;93(17):e97 91–e97 98. doi: 10.2106/JBJS.J.01558. [DOI] [PubMed] [Google Scholar]
- 69.Dhinsa BS, Bhamra JS, James C, Dunnet W, Zahn H. Patella fracture after medial patellofemoral ligament reconstruction using suture anchors. Knee. 2013;20(6):605–608. doi: 10.1016/j.knee.2013.05.013. [DOI] [PubMed] [Google Scholar]


