Abstract
Purpose of review
The purpose of this review is to describe the current understanding of the medial patellofemoral complex, including recent anatomic advances, evaluation of indications for reconstruction with concomitant pathology, and surgical reconstruction techniques.
Recent findings
Recent advances in our understanding of MPFC anatomy have found that there are fibers that insert onto the deep quadriceps tendon as well as the patella, thus earning the name “medial patellofemoral complex” to allow for the variability in its anatomy. In MPFC reconstruction, anatomic origin and insertion points and appropriate graft length are critical to prevent overconstraint of the patellofemoral joint.
Summary
The MPFC is a crucial soft tissue checkrein to lateral patellar translation, and its repair or reconstruction results in good restoration of patellofemoral stability. As our understanding of MPFC anatomy evolves, further studies are needed to apply its relevance in kinematics and surgical applications to its role in maintaining patellar stability.
Keywords: Medial patellofemoral complex, Medial patellofemoral ligament, Patellar instability, MPFC, MPFL
Introduction
Patellar instability is a common cause of knee dysfunction in adolescents and young adults [1]. Treatments and techniques for restoring stability have continued to evolve in recent years. A tear of the medial patellofemoral ligament (MPFL) has been considered the essential lesion of lateral patellar instability [2]. Newer anatomic studies have defined a broader medial structure that attaches to the quadriceps tendon in addition to the patella, which has led to some authors referring to this as the medial patellofemoral complex (MPFC), to allow for its variability in attachment sites [3•, 4]. In recurrent patellar instability, a tear in this critical soft tissue complex may not be the only pathology, as these patients can present with concomitant lateralized tibial tuberosities, patella alta, and/or trochlear dysplasia [1]. We aim to review the current understanding of the MPFC as it relates to patellofemoral anatomy and function, as well as surgical indications, techniques, and outcomes in the treatment of patellar instability.
Anatomy and function
The anatomic and biomechanical definitions of the MPFC have evolved over time. Earlier defined as a pure ligament spanning from femur to patella, the MPFC has been more recently identified as a broad, fan-shaped structure with both bony and soft tissue insertions (Fig. 1) [3•, 4]. The MPFC is located in layer 2, runs deep to the vastus medialis obliquus, and is distinct from the medial retinaculum [3•]. The MPFC origin is generally accepted to originate within a triangular saddle of bony landmarks on the medial femur formed by the medial gastrocnemius tubercle, the medial epicondyle, and the adductor tubercle [2, 3•, 4]. The MPFC insertion is more variable, and averages 57.3% of its fibers attaching to the patella, with the remaining 42.7% attaching to the deep quadriceps tendon [5]. Fulkerson has described this quadriceps portion of the MPFC as the medial quadriceps tendon-femoral ligament (MQTFL) [6•]. The midpoint of the 30.4-mm-wide insertion of the MPFC has been reproducibly found at the junction of the medial quadriceps tendon border with the articular surface of the patella (Fig. 1) [3•, 5].
Fig. 1.
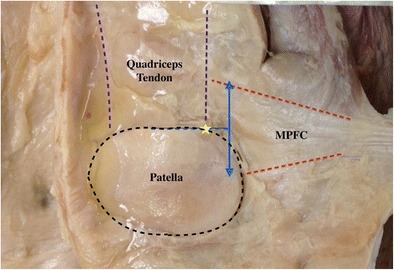
The anatomy of the MPFC (dashed red line) is shown from the articular surface, with fibers inserting on the patella and the quadriceps tendon (dashed purple line). The midpoint (dashed blue line) is shown at the junction of the medial border of the quadriceps tendon with the patella (yellow star)
For pediatric patients, there has been a great deal of investigation into the relationship of the MPFC to the distal femoral physis. There has been wide variability in findings, with the average origin of the MPFC occurring 4.7–10 mm distal to the physis [7, 8]. The superior-most fibers of the MPFC origin commonly overlie the physis [7, 8]. The origin may migrate closer to the physis in adolescence [8].
The MPFL has been described as the primary static restraint to lateral patellar translation, providing approximately 208 N of mean tensile strength before rupture [9, 10]. Interestingly, this data concerns only the bony attachment of the MPFC, as the proximal MQTFL fibers were seemingly dissected away before analysis. Rupture of the MPFL occurs at an average 26 mm elongation, representing a supple 49% strain [9]. In looking at the MPFC’s functionality in the dynamic knee, patterns of ligament strain and contact pressures have emerged. The largest change in MPFC strain occurs at 25°–30° of flexion as the patella engages with the trochlea [11]. As such, transection of the MPFC results in maltracking with lateral translation and increased lateral trochlea contact pressures [12]. Past 60° of knee flexion, lateral patellar translation is prevented by trochlear engagement, and the force required to displace the patella is independent of damage or reconstruction of the MPFC [13]. Both lateralization and proximalization of the tibial tubercle, representing increased TT-TG distance and patella alta, result in anisometry and significantly increased strain of the MPFC [14]. Looking at individual fibers of the MPFC with 4D CT, it seems that the superior-most fibers resist dislocation at low flexion angles, while the inferior-most fibers maintain tilt in midflexion [15].
In addition to the MPFC, a medial patellotibial ligament and a medial patellomeniscal ligament have been identified as structures with possible independent contribution to patellar stability, though their significance is uncertain [16]. It is postulated that these structures resist lateral translation in deep flexion [17].
Surgical indications
Initial patellar dislocations are typically managed non-operatively with functional bracing, quadriceps strengthening, and progressive return to activity [1, 18]. Diagnosis relies primarily on history and physical examination, with the glide test (Fig. 2) allowing for quantification of patellar translation based on patellar quadrants. MRI can be useful in the assessment of patellar dislocation, to identify chondral fractures, as well as localize the injury to the MPFC (Fig. 3).
Fig. 2.

The glide test is used to quantify medial and lateral patellar translation based on patellar quadrants, with two quadrants in each direction typically representing normal motion
Fig. 3.
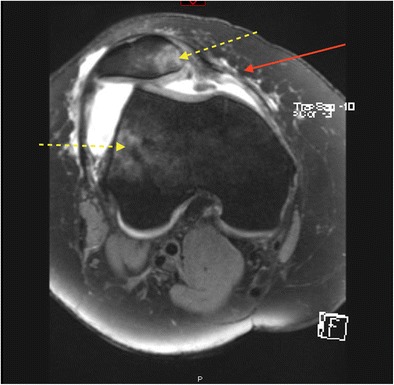
Axial view of the right knee on T2 fat-suppressed MR imaging demonstrates and effusion and increased lateral translation and tilt after patellar dislocation. A typically bony edema pattern is demonstrated on the medial patella and lateral femoral condyle (dotted yellow arrows). Additionally, injury to the MPFC at the midsubstance is noted (red arrow)
Ultrasound has also been shown to demonstrate excellent specificity, sensitivity, and localization of MPFL lesions; its future role may be expanded in the case of acute primary patellar dislocation [19, 20].
Recurrent lateral patellar instability that has failed conservative management is the primary indication for MPFC reconstruction. In this clinical setting, a thorough investigation into the multifactorial nature of the instability is warranted, which includes lateralization of the tibial tuberosity, as well as patella alta and trochlear dysplasia. Often, a combination of the above associated pathologies can be identified, and is usually the circumstance in pediatric cases. For skeletally immature patients treated nonoperatively, the risk of recurrent patellar dislocation is reported to be 31% [21]. High-grade trochlear dysplasia and younger age contribute to the greatest risk [21].
Understanding the influence of other factors that involve bony malalignment is critical in determining the need for concurrent surgical procedures at the time of MPFC reconstruction. Increased tibial tubercle-trochlear groove (TT-TG) distances may indicate a lateralized extensor mechanism relative to the trochlear groove, which may occur in the setting of external tibial torsion, femoral anteversion, or genu valgum. In these cases, medializing tibial tuberosity osteotomy (TTO) may be performed to correct alignment. A cadaveric study by Stephen et al. demonstrated that MPFC reconstruction alone restored normal patellar kinematics in the setting of TT-TG distance of approximately 15 mm, but that abnormal patellar tilt could not be corrected with MPFC reconstruction alone for TT-TG distances of 20 and 25 mm [22]. While the indications to add TTO to a procedure can vary, studies suggest that TT-TG distance should be used to consider TTO in addition MPFC in the setting of excessive bony malalignment [23].
Patellar dislocation is often associated with other conditions and injuries about the knee. In a multiligament knee injury study by Allen et al., 59% of cases also had injury to the MPFC. Concomitant superficial medial collateral ligament injury was noted in all of these cases, likely indicating the valgus moment contributing to both the MPFC and medial collateral ligament injuries [24]. These cases were treated nonoperatively with respect to the MPFC and did not demonstrate recurrent instability or lower outcome scores [24]. Combination anterior cruciate ligament and MPFC injuries, more commonly seen in hyperlax patients, may be addressed with simultaneous reconstruction with good outcomes [25]. However, Howells et al. noted that outcome scores for hyperlax patients with Beighton scores greater than or equal to 6 were significantly worse at 6-month follow-up (Kujala scores of 82.56 vs. 64.28) [26].
Surgical reconstruction techniques
A multitude of techniques in repair and reconstruction of the MPFC exist. Key considerations in MPFC reconstruction include appropriate graft length and anatomic placement of graft insertion and origin, while choice of fixation and use of double or single bundle grafts (Fig. 4) can vary by surgeon preference. Overconstraint of the patellofemoral joint due to an overly tight graft is a serious concern in MPFC reconstruction, as the increased pressures can lead to patellofemoral pain and accelerated degeneration of the joint [27]. A study by Stephen et al. of patellofemoral contact pressures in cadavers has demonstrated that fixation of the MPFC graft at full extension or with too much force causes increased medial pressures and medial tilt of the patella [28]. The authors reported that the safest place to tension the graft was with 2 N of force in 30° to 60° of flexion [28]. McCulloch et al. demonstrated that fixation in 45° of flexion replicates the strain patterns of the native MPFC [11]. In a cadaveric study, Burrus et al. described graft length changes that occurred throughout knee flexion that varied with femoral tunnel position [29]. The authors demonstrated that graft length variability stemming from errant femoral tunnel position was minimized when the graft was fixed at low flexion angles [29]. Elias et al. studied a clinically pragmatic technique of graft tensioning with computational modeling. They demonstrated that allowing 0.5 to 1 quadrant of lateral patellar translation at 30° flexion successfully prevents maltracking and overconstraint of the medial facet [30]. Direct visualization of the patellofemoral joint with arthroscopy at the time of graft tensioning and fixation was shown by Kang et al. to not change outcomes, patellar tilt, or congruence angle [31].
Fig. 4.

Both single-bundle and double-bundled reconstruction of the MPFC have been described. The figure demonstrates an intraoperative example of single-bundle MPFC reconstruction utilizing the docking technique
Recreating the anatomy of the MPFC during reconstruction is critical for the function of the graft. Several authors have demonstrated that small errors in femoral tunnel position can lead to changes in patellofemoral contact pressures [32•]. Radiographic landmarks corresponding to the anatomic origin and insertion of the MPFC have been described in multiple studies. Schöttle originally described the femoral origin as a radiographic point 1.3 mm anterior to the posterior cortical line and 2.5 mm distal to the posterior origin of the medial femoral condyle (Fig. 5) [33]. It is important to note that a perfect lateral radiograph is mandatory when establishing the femoral start point. Ziegler et al. discovered that a radiograph taken with 5° of obliquity results in a reference point that is 7.5–9.2 mm off target, depending on the plane of error [34]. Radiographic reference points should be used in conjunction with direct visual and tactile assessment of the anatomic saddle when establishing the femoral start point.
Fig. 5.

Schottle’s point is demonstrated on a lateral radiograph of a left knee, approximating the femoral origin of the MPFC. This is found anterior to the posterior cortical line, and distal to the posterior medial femoral condyle, and can be utilized intraoperatively to guide femoral tunnel placement during MPFC reconstruction
The patellar insertion of the MPFC has been described as the radiographic junction of the proximal and middle thirds of the patella [35], though this is brought into question given recent work demonstrating a more proximal midpoint as discussed previously [3•]. Fulkerson et al. have demonstrated that isolated MQTFL reconstruction with graft running deep to the vastus medialis obliquus and sutured directly to the distal medial quadriceps tendon at its junction with the patella is a viable alternative to bony patellar fixation [6•]. This technique eliminates the risk of patellar fracture and may be more precise, as it uses direct visualization rather than radiographic landmarks [6•]. A similar reconstruction technique has been described by Fink, in which a 10–12-mm-wide and 3-mm-deep sleeve of superficial quadriceps tendon is elevated, left attached to the patella, reflected medially, and fixed with an interference screw at the femoral isometric point [36]. Both of these techniques use a patellar fixation point that is closer to the previously described anatomic midpoint. Autologous gracilis or semitendinosus grafts provide adequate length, and are considerably stronger than the native MPFC [9, 37]. Kujala scores between the two options have been reported to demonstrate a 32.2 point improvement with autografts compared to 22.5 with allografts [38], yet reported failure rates between autografts and allografts are similar, at 5.7 versus 6.7%, respectively [38].
While many authors describe single-bundle reconstruction techniques, double-bundle grafts have demonstrated significantly lower rates of failure and recurrent instability compared to single-bundle grafts in some studies. Though single-stranded grafts, as used in most reconstruction techniques, may slacken at some flexion angles due to not being fan-shaped, they remain a stable construct [39]. The heterogeneity of single-bundle reconstruction techniques should be taken into account when reviewing this data. Weinberger et al. found the failure rate of double-bundle grafts to be 5.5% compared to 10.6% with single-bundle grafts [38]. Wang et al. quotes the rate of recurrent instability with double-bundle grafts to be 4.54% compared to 26.9% with single-bundle grafts [40]. In the same study, Kujala scores were noted to be better with double-bundle grafts compared to single-bundle (92.86 vs. 80.46) [40], yet further studies are needed to identify optimal reconstruction techniques.
Fixation choice continues to be a source of debate. Methods of fixation include interference screws, suspensory cortical fixation, suture anchors, and suture over bone bridge. In some biomechanical studies, suture anchor fixation displays a lower load to failure than interference screws, and a lower load to failure than the native intact MPFC if anchors are used in the patella [41, 42]. Various fixation options have advantages and disadvantages, however, location of graft fixation and graft length are considered to be more critical than fixation choice in MPFC reconstruction.
Outcomes and complications
Enderlein et al. demonstrated that MPFL reconstruction consistently improves knee function, the average Kujala score increasing from 62.5 to 80.4 in 1 year [43]. Age greater than 30 years, female gender, high-grade cartilage injury, and obesity were predictors for a poorer outcome score [43]. Redislocation was uncommon at 4.5%, but a sensation of subluxation occurring more than a month after surgery was more common at 11% [43]. Other complications besides recurrent lateral instability include restricted knee range of motion, arthrofibrosis, medial instability, patellofemoral arthrosis and pain, patellar fracture, graft failure, wound complications, and implant pain [27, 44]. Many of these complications are preventable and have been reported to be the result of technical error [27]. In a systematic review, Shah et al. found a complication rate of 26.1%, with nearly a third of these complications attributed to recurrent apprehension [45]. More complications were seen in reconstruction using bone tunnels, but suture fixation in this study had a higher reported rate of recurrent instability [45]. Graft fixation at 60° or greater of knee flexion resulted in less complications and recurrent instability compared to fixation in less flexion [45]. Patella fractures were seen only in transverse or anterior patellar bone tunnels [45]. In pediatric patients averaging 14.9 years old, Parikh et al. showed a complication rate of 16.2%, with 4.5% redislocation, 4.5% stiffness, 3.4% patella fracture, and 2.8% patellofemoral pain/arthrosis [44].
Identifying and addressing concomitant pathology at the time of MPFC reconstruction can prevent recurrent instability and address other factors contributing to symptoms. Steiner et al. demonstrated no difference in outcomes after MPFC reconstruction among different grades of trochlear dysplasia, with a mean Kujala score improvement from 53.3 to 90.7 [46]. However, in a study by Hiemstra et al., associated high-grade trochlear dysplasia (Dejour types B-D) was associated with worse Banff instrument scores compared to low grade dysplasia for patients treated with isolated MPFL reconstruction or MPFL imbrication (69.91 vs. 60.02) [47]. Trochlear bumps greater than 5 mm in size especially were associated with worse outcomes (69.28 vs. 59.67) [47]. Recurrent instability for isolated MPFC reconstruction in Dejour types C and D has been quoted as high as 100%, compared to 7.4% in types A and B [48].
Nonrandom prospective cohort studies have demonstrated that isolated MPFC reconstruction may be equivalent to MPFC reconstruction with concomitant TTO for select patients, while others have shown a benefit with concurrent TTO [49, 50]. A recent randomized study by Damasena et al. demonstrated significantly improved patellar tilt and congruence angle measurements for patients treated with MPFC reconstruction and TTO versus TTO alone [51].
Rehabilitation after MPFC reconstruction has not been standardized, but typically includes progressive weightbearing and range of motion, with graduated and progressive return to full activity within 6–9 months [52]. With dynamometer testing, Krych et al. demonstrated that athletes exhibit a 21.4% extension strength deficit and 15.8% flexion strength deficit at 6 months after MPFC reconstruction [53]. Strength was noted to be significantly worse in males and patients with patella alta [53]. Patients who received concomitant TTO saw significantly slower return to sport and decreased strength metrics [53]. Closed chain exercises are superior to open chain exercises in the short term for thigh circumference and pain scores [54]. Biomechanically normal gait, specifically knee flexion angle and internal knee extension moment as assessed by 3D motion analysis, returns to normal at 1-year follow-up after reconstruction [55]. In isolated MPFC reconstructions studied by Lippacher et al., 53% of athletes return to an equal or higher level of play [56].
Conclusions
The medial patellofemoral complex is an important soft tissue restraint in lateral patellar translation that includes the insertions on both the patella and the quadriceps tendon. MPFC reconstruction can reestablish the patellar checkrein and limit recurrent instability in patients with medial soft tissue deficiency. Techniques which include quadriceps fixation look to better reconstruct the anatomy of the MPFC and may be the subject of future studies. Patients with recurrent patellar instability should be evaluated for associated contributing factors such as lateralized tibial tuberosity, patella alta, and trochlear dysplasia, and the appropriate concurrent surgeries should be performed to address these. Graft origin and insertion should be anatomic optimize function and minimize complications, and graft length should be appropriately set so as to not overconstrain the patellofemoral joint. MPFC reconstruction has been shown to have good to excellent results with proper indications, and complications can often be avoided due to minimizing technical error.
Compliance with ethical standards
Conflict of interest
Both authors declare that they have no conflict of interest.
Human and animal rights and informed consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Footnotes
This article is part of the Topical Collection on Advances in Patellofemoral Surgery
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Weber AE, Nathani A, Dines JS, Allen AA, Shubin-Stein BE, Arendt EA, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Jt Surg. 2016;98(5):417–27. 10.2106/JBJS.O.00354. [DOI] [PubMed]
- 2.Aframian A, Smith TO, Tennent TD, Cobb JP, Hing CB. Origin and insertion of the medial patellofemoral ligament: a systematic review of anatomy. Knee Surgery, Sport Traumatol Arthrosc. 2016;25:1–18. doi: 10.1007/s00167-016-4272-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanaka MJ, Voss A, Fulkerson JP. The anatomic midpoint of the attachment of the medial patellofemoral complex. J Bone Joint Surg Am. 2016;98(14):1199–1205. doi: 10.2106/JBJS.15.01182. [DOI] [PubMed] [Google Scholar]
- 4.Tanaka MJ. The anatomy of the medial patellofemoral ligament. Sports Med Arthrosc. 2017;25(2):8–11. doi: 10.1097/JSA.0000000000000143. [DOI] [PubMed] [Google Scholar]
- 5.Tanaka MJ. Variability in the patellar attachment of the medial patellofemoral ligament. Arthrosc - J Arthrosc Relat Surg. 2016;32(8):1667–1670. doi: 10.1016/j.arthro.2016.01.046. [DOI] [PubMed] [Google Scholar]
- 6.Fulkerson JP, Edgar C. Medial quadriceps tendon-femoral ligament: surgical anatomy and reconstruction technique to prevent patella instability. Arthrosc Tech. 2013;2(2):e125–e128. doi: 10.1016/j.eats.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greenrod W, Cox J, Astori I, Baulch J, Williams J. A magnetic resonance imaging study of the significance of the distal femoral physis during medial patellofemoral ligament reconstruction. Orthop J Sport Med. 2013;1(4):232596711350263. doi: 10.1177/2325967113502638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shea KG, Martinson WD, Cannamela PC, Richmond CG, Fabricant PD, Anderson AF, et al. Variation in the medial patellofemoral ligament origin in the skeletally immature knee: an anatomic study. Am J Sports Med. 2017;46:1–7. 10.1177/0363546517738002. [DOI] [PubMed]
- 9.Mountney J, Senavongse W, Amis AA, Thomas NP. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87(1):36–40. doi: 10.1302/0301-620X.87B1.14924. [DOI] [PubMed] [Google Scholar]
- 10.Conlan T, Garth WP, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682–693. doi: 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 11.McCulloch PC, Bott A, Ramkumar PN, Suarez A, Isamaily S, Daylamani D, et al. Strain within the native and reconstructed MPFL during knee flexion. J Knee Surg. 2014;27(2):125–31. 10.1055/s-0033-1357496. [DOI] [PubMed]
- 12.Stephen JM, Kader D, Lumpaopong P, Deehan DJ, Amis AA. Sectioning the medial patellofemoral ligament alters patellofemoral joint kinematics and contact mechanics. J Orthop Res. 2013;31(9):1423–1429. doi: 10.1002/jor.22371. [DOI] [PubMed] [Google Scholar]
- 13.Wang Q, Huang W, Cai D, Huang H. Biomechanical comparison of single- and double-bundle medial patellofemoral ligament reconstruction. J Orthop Surg Res. 2017;12(1):29. doi: 10.1186/s13018-017-0530-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Redler L, Meyers K, Munch J, Dennis E, Nguyen J, Stein BS. Anisometry of medial patellofemoral ligament reconstruction in the setting of Patella Alta and increased Tibial tubercle-trochlear groove (TT-TG) distance. Arthrosc J Arthrosc Relat Surg. 2016;32((6):e10. doi: 10.1016/j.arthro.2016.03.054. [DOI] [PubMed] [Google Scholar]
- 15.Song SY, Pang C-H, Kim CH, Kim J, Choi ML, Seo Y-J. Length change behavior of virtual medial patellofemoral ligament fibers during in vivo knee flexion. Am J Sports Med. 2015;43(5):1165–1171. doi: 10.1177/0363546514567061. [DOI] [PubMed] [Google Scholar]
- 16.Kruckeberg BM, Chahla J, Moatshe G, Cinque ME, Muckenhirn KJ, Godin JA, et al. Quantitative and qualitative analysis of the medial patellar ligaments: an anatomic and radiographic study. Am J Sports Med. 2017;46:153–62. 10.1177/0363546517729818. [DOI] [PubMed]
- 17.Hinckel BB, Gobbi RG, Kaleka CC, Camanho GL, Arendt EA. Medial patellotibial ligament and medial patellomeniscal ligament: anatomy, imaging, biomechanics, and clinical review. Knee Surg Sports Traumatol Arthrosc. 2018 Mar;26(3):685-696. [DOI] [PubMed]
- 18.Vavken P, Wimmer MD, Camathias C, Quidde J, Valderrabano V, Pagenstert G. Treating patella instability in skeletally immature patients. Arthrosc - J Arthrosc Relat Surg. 2013;29(8):1410–1422. doi: 10.1016/j.arthro.2013.03.075. [DOI] [PubMed] [Google Scholar]
- 19.Zhang GY, Zheng L, Ding HY, Li EM, Sun BS, Shi H. Evaluation of medial patellofemoral ligament tears after acute lateral patellar dislocation: comparison of high-frequency ultrasound and MR. Eur Radiol. 2015;25(1):274–281. doi: 10.1007/s00330-014-3407-3. [DOI] [PubMed] [Google Scholar]
- 20.Zhang GY, Zheng L, Shi H, Qu SH, Ding HY. Sonography on injury of the medial patellofemoral ligament after acute traumatic lateral patellar dislocation: injury patterns and correlation analysis with injury of articular cartilage of the inferomedial patella. Injury. 2013;44(12):1892–1898. doi: 10.1016/j.injury.2013.08.027. [DOI] [PubMed] [Google Scholar]
- 21.Nwachukwu BU, So C, Schairer WW, Green DW, Dodwell ER. Surgical versus conservative management of acute patellar dislocation in children and adolescents: a systematic review. Knee Surgery, Sport Traumatol Arthrosc. 2016;24(3):760–767. doi: 10.1007/s00167-015-3948-2. [DOI] [PubMed] [Google Scholar]
- 22.Stephen JM, Dodds AL, Lumpaopong P, Kader D, Williams A, Amis AA. The ability of medial patellofemoral ligament reconstruction to correct patellar kinematics and contact mechanics in the presence of a lateralized tibial tubercle. Am J Sports Med. 2015;43(9):2198–2207. doi: 10.1177/0363546515597906. [DOI] [PubMed] [Google Scholar]
- 23.D’Amore T, Tanaka MJ, Cosgarea AJ. When and how far to move the tibial tuberosity in patients with patellar instability. Sports Med Arthrosc. 2017;25(2):78–84. doi: 10.1097/JSA.0000000000000146. [DOI] [PubMed] [Google Scholar]
- 24.Allen BJ, Krych AJ, Engasser W, Levy BA, Stuart MJ, Collins MS, et al. Medial patellofemoral ligament tears in the setting of multiligament knee injuries rarely cause patellar instability. Am J Sports Med. 2015;43(6):1386–90. 10.1177/0363546515576902. [DOI] [PubMed]
- 25.Hiemstra LA, Kerslake S, Heard M, Buchko G, Lafave M. Outcomes of surgical stabilization in patients with combined ACL deficiency and patellofemoral instability—a case series. Knee. 2016;23(6):1106–1111. doi: 10.1016/j.knee.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 26.Howells NR, Eldridge JD. Medial patellofemoral ligament reconstruction for patellar instability in patients with hypermobility: a case control study. Bone Joint J. 2012;94-B(12):1655–1659. doi: 10.1302/0301-620X.94B12.29562. [DOI] [PubMed] [Google Scholar]
- 27.Tanaka MJ, Bollier MJ, Andrish JT, Fulkerson JP, Cosgarea AJ. Complications of medial patellofemoral ligament reconstruction: common technical errors and factors for success: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94(12):1–8. doi: 10.2106/JBJS.K.01449. [DOI] [PubMed] [Google Scholar]
- 28.Stephen JM, Kaider D, Lumpaopong P, Deehan DJ, Amis AA. The effect of femoral tunnel position and graft tension on patellar contact mechanics and kinematics after medial patellofemoral ligament reconstruction. Am J Sports Med. 2014;42(2):364–372. doi: 10.1177/0363546513509230. [DOI] [PubMed] [Google Scholar]
- 29.Burrus MT, Werner BC, Cancienne JM, Gwathmey FW, Diduch DR. MPFL graft fixation in low degrees of knee flexion minimizes errors made in the femoral location. Knee Surgery, Sport Traumatol Arthrosc. 2017;25(10):3092–3098. doi: 10.1007/s00167-016-4111-4. [DOI] [PubMed] [Google Scholar]
- 30.Elias JJ, Jones KC, Lalonde MK, Gabra JN, Rezvanifar SC, Cosgarea AJ. Allowing one quadrant of patellar lateral translation during medial patellofemoral ligament reconstruction successfully limits maltracking without overconstraining the patella. Knee Surgery, Sport Traumatol Arthrosc. 2017;0(0):1–8. doi: 10.1007/s00167-017-4799-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kang H, Wang F, Cao J, Liu X, Ji G. A prospective randomized trial evaluating two different tensioning techniques for medial patellofemoral ligament reconstruction. Knee. 2016;23(5):826–829. doi: 10.1016/j.knee.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 32.Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage. Am J Sports Med. 2006;34(9):1478–1485. doi: 10.1177/0363546506287486. [DOI] [PubMed] [Google Scholar]
- 33.Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 34.Ziegler CG, Fulkerson JP, Edgar C. Radiographic reference points are inaccurate with and without a true lateral radiograph. Am J Sports Med. 2016;44(1):133–142. doi: 10.1177/0363546515611652. [DOI] [PubMed] [Google Scholar]
- 35.Barnett AJ, Howells NR, Burston BJ, Ansari A, Clark D, Eldridge JD. Radiographic landmarks for tunnel placement in reconstruction of the medial patellofemoral ligament. Knee Surgery, Sport Traumatol Arthrosc. 2012;20(12):2380–2384. doi: 10.1007/s00167-011-1871-8. [DOI] [PubMed] [Google Scholar]
- 36.Fink C, Veselko M, Herbort M, Hoser CMPFL. Reconstruction using a quadriceps tendon graft part 2: operative technique and short term clinical results. Knee. 2014;21(6):1175–1179. doi: 10.1016/j.knee.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 37.Hamner D, Brown C, Steiner M, Hecker A, Hayes W. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Jt Surg Am. 1999;81(4):549–557. doi: 10.2106/00004623-199904000-00013. [DOI] [PubMed] [Google Scholar]
- 38.Weinberger JM, Fabricant PD, Taylor SA, Mei JY, Jones KJ. Influence of graft source and configuration on revision rate and patient-reported outcomes after MPFL reconstruction: a systematic review and meta-analysis. Knee Surgery, Sport Traumatol Arthrosc. 2017;25(8):2511–2519. doi: 10.1007/s00167-016-4006-4. [DOI] [PubMed] [Google Scholar]
- 39.Ntagiopoulos PG, Sharma B, Bignozzi S, Lopomo N, Colle F, Zaffagnini S, et al. Are the tubular grafts in the femoral tunnel in an anatomical or isometric position in the reconstruction of medial patellofemoral ligament? Int Orthop. 2013;37(10):1933–41. 10.1007/s00264-013-1938-x. [DOI] [PMC free article] [PubMed]
- 40.Wang CH, Ma LF, Zhou JW, Ji G, Wang HY, Wang F, et al. Double-bundle anatomical versus single-bundle isometric medial patellofemoral ligament reconstruction for patellar dislocation. Int Orthop. 2013;37(4):617–24. 10.1007/s00264-013-1788-6. [DOI] [PMC free article] [PubMed]
- 41.Joyner PW, Bruce J, Roth TS, Mills FB IV, Winnier S, Hess R, et al. Biomechanical tensile strength analysis for medial patellofemoral ligament reconstruction. Knee. 2017;24(5):965–76. 10.1016/j.knee.2017.04.013. [DOI] [PubMed]
- 42.Russ SD, Tompkins M, Nuckley D, Macalena J. Biomechanical comparison of patellar fixation techniques in medial patellofemoral ligament reconstruction. Am J Sports Med. 2015;43(1):195–199. doi: 10.1177/0363546514550992. [DOI] [PubMed] [Google Scholar]
- 43.Enderlein D, Nielsen T, Christiansen SE, Faunø P, Lind M. Clinical outcome after reconstruction of the medial patellofemoral ligament in patients with recurrent patella instability. Knee Surgery, Sport Traumatol Arthrosc. 2014;22(10):2458–2464. doi: 10.1007/s00167-014-3164-5. [DOI] [PubMed] [Google Scholar]
- 44.Parikh SN, Nathan ST, Wall EJ, Eismann EA. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41(5):1030–1038. doi: 10.1177/0363546513482085. [DOI] [PubMed] [Google Scholar]
- 45.Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40(8):1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Steiner TM, Torga-Spak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34(8):1254–1261. doi: 10.1177/0363546505285584. [DOI] [PubMed] [Google Scholar]
- 47.Hiemstra LA, Kerslake S, Loewen M, Lafave M. Effect of trochlear dysplasia on outcomes after isolated soft tissue stabilization for patellar instability. Am J Sports Med. 2016;44(6):1515–1523. doi: 10.1177/0363546516635626. [DOI] [PubMed] [Google Scholar]
- 48.Hopper GP, Leach WJ, Rooney BP, Walker CR, Blyth MJ. Does degree of trochlear dysplasia and position of femoral tunnel influence outcome after medial patellofemoral ligament reconstruction? Am J Sports Med. 2014;42(3):716–722. doi: 10.1177/0363546513518413. [DOI] [PubMed] [Google Scholar]
- 49.Mulliez A, Lambrecht D, Verbruggen D, Van Der Straeten C, Verdonk P, Victor J. Clinical outcome in MPFL reconstruction with and without tuberositas transposition. Knee Surgery, Sport Traumatol Arthrosc. 2017;25(9):2708–2714. doi: 10.1007/s00167-015-3654-0. [DOI] [PubMed] [Google Scholar]
- 50.Kohn LM, Meidinger G, Beitzel K, Banke IJ, Hensler D, Imhoff AB, et al. Isolated and combined medial patellofemoral ligament reconstruction in revision surgery for patellofemoral instability. Am J Sports Med. 2013;41(9):2128–35. 10.1177/0363546513498572. [DOI] [PubMed]
- 51.Damasena I, Blythe M, Wysocki D, Kelly D, Annear P. Medial patellofemoral ligament reconstruction combined with distal realignment for recurrent dislocations of the patella: 5-year results of a randomized controlled trial. Am J Sports Med. 2017;45(2):369–376. doi: 10.1177/0363546516666352. [DOI] [PubMed] [Google Scholar]
- 52.Zaman S, White A, Shi WJ, Freedman KB, Dodson CC. Return-to-play guidelines after medial patellofemoral ligament surgery for recurrent patellar instability: a systematic review. Am J Sports Med. 2017;36354651771366:036354651771366. doi: 10.1177/0363546517713663. [DOI] [PubMed] [Google Scholar]
- 53.Krych AJ, O’Malley MP, Johnson NR, Mohan R, Hewett TE, Stuart MJ, et al. Functional testing and return to sport following stabilization surgery for recurrent lateral patellar instability in competitive athletes. Knee Surgery, Sport Traumatol Arthrosc. 2016;26:1–8. 10.1007/s00167-016-4409-2. [DOI] [PubMed]
- 54.Zhang F, Wang J, Wang F. Comparison of the clinical effects of open and closed chain exercises after medial patellofemoral ligament reconstruction. J Phys Ther Sci. 2014;26(10):1557–1560. doi: 10.1589/jpts.26.1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Asaeda M, Deie M, Fujita N, Shimada N, Orita N, Iwaki D, et al. Knee biomechanics during walking in recurrent lateral patellar dislocation are normalized by 1 year after medial patellofemoral ligament reconstruction. Knee Surgery, Sport Traumatol Arthrosc. 2016;24(10):3254–61. 10.1007/s00167-016-4040-2. [DOI] [PubMed]
- 56.Lippacher S, Dreyhaupt J, Williams SRM, Reichel H, Nelitz M. Reconstruction of the medial patellofemoral ligament. Am J Sports Med. 2014;42(7):1661–1668. doi: 10.1177/0363546514529640. [DOI] [PubMed] [Google Scholar]


