Abstract
Background
Police officers experience a high degree of chronic stress. Policing ranks among the highest professions in terms of disease and accident rates. Mental health is particularly impacted, evidenced by elevated rates of burnout, anxiety and depression, and poorer quality of life than the general public. Mindfulness training has been shown to reduce stress, anxiety, burnout and promote quality of life in a variety of settings, although its efficacy in this context has yet to be systematically evaluated. Therefore, this trial will investigate the efficacy of a mindfulness-based intervention versus a waitlist control in improving quality of life and reducing negative mental health symptoms in police officers.
Methods
This multicenter randomized controlled trial has three assessment points: baseline, post-intervention, and six-month follow-up. Active police officers (n = 160) will be randomized to Mindfulness-Based Health Promotion (MBHP) or waitlist control group at two Brazilian major cities: Porto Alegre and São Paulo. The primary outcomes are burnout symptoms and quality of life. Consistent with the MBHP conceptual model, assessed secondary outcomes include perceived stress, anxiety and depression symptoms, and the potential mechanisms of resilience, mindfulness, decentering, self-compassion, spirituality, and religiosity.
Discussion
Findings from this study will inform and guide future research, practice, and policy regarding police offer health and quality of life in Brazil and globally.
Trial registration
ClinicalTrials.gov NCT03114605. Retrospectively registered on March 21, 2017.
Keywords: Mindfulness, Police, Quality of life, Burnout, Stress
Background
Police officers are routinely exposed to dangerous and unpredictable situations [1]. Exposure to acute and chronic stress is reflected in elevated officer rates of burnout [2, 3], depression [4], suicide [5–7], and anxiety [8]. In addition to higher rates of mental health concerns, police officers have an increased risk of sudden cardiac death, diabetes, obesity and metabolic syndrome [9, 10]. It is no surprise to find that this occupation ranks highest on diseases and accidents rates among all professions [11, 12]. Police quality of life is generally poor [13], including among Brazilian military police [14, 15] and recruits [16]. Brazil has the 7th highest crime index in the world, and Porto Alegre and São Paulo—where participants will be recruited for this study—have the 11th and 14th highest crime index of cities in the world, respectively [17, 18].
Police stress and related mental and physical health consequences can negatively impact work and personal life. Stress-impaired officers are more likely to make serious errors, and exhibit other adverse work outcomes including uncontrolled anger toward suspects, excessive use of force, and absenteeism [19, 20]. The effects of work-related stress also extends to personal life, contributing to disruptive family relationships [21]. It is estimated that approximately one third of police officers meet criteria for burnout syndrome (emotional exhaustion, despersonalization, and low personal accomplishment) [22]. The emotional, physical, economic and social damage of stress in police indicates an urgent call for effective preventive programs to reduce the negative impact of stress and burnout, and to enhance quality of life and well-being.
Mindfulness is an innate meta-awareness capacity to attend to present-moment experience while avoiding entanglement in cognitive biases. It can be enhanced by simple meditative attentional practices, as well as through structured training programs such as mindfulness-based interventions (MBIs). MBIs are generally group-based weekly classes consisting primarily of meditation practices, such as the body scan, mindful movement, sitting and walking meditation. By repeatedly bringing attention back to the current experience, participants gradually learn to disengage from “automatic pilot”, and directly experience emotions and bodily sensations in the present moment. In MBIs, participants learn the ability to step back from ruminating about the past or worrying about the future and simply allow experiences to unfold [23, 24].
Mindfulness training may regulate how the individual appraises stress, and increase secondary appraisals of approach-oriented coping resources, thus reducing stress reactivity. Recent meta-analyses support this theory, indicating MBIs improve common health and risk factors, including stress [25, 26], depression and suicidal ideation [26, 27], anxiety and burnout [28, 29], and increases psychological resilience [30, 31]. MBIs have been shown to be feasible and to lead to improved health outcomes among several high-stress populations, such as military personnel [32, 33], physicians [34, 35], firefighters [36], and inner-city teachers [37].
MBI studies among police officers are limited; however, a pre-post study suggests that mindfulness training can reduce stress and burnout symptoms [38], and findings from a recent RCT indicate that relative to waitlist control, MBI participants experienced greater reductions in salivary cortisol (AUCi), self-reported aggression, burnout, alcohol use, sleep disturbance, and increases in psychological flexibility and non-reactivity at post-training [39]. Despite these promising findings and a global increase among law enforcement agencies integrating mindfulness into trainings, the impact and benefits of MBIs have yet to be systematically evaluated in this context.
Aims
The aim of the POLICE (imPact Of a mindfuLness-based Intervention on burnout and quality of life in poliCE officers) study is to evaluate the efficacy of a MBI, compared to a waitlist control group, in promoting quality of life and mental health in police officers. We also aim to investigate the feasibility and acceptability of an 8-week, 2-h long MBI on this particular setting.
Our main hypothesis is that mindfulness training will reduce burnout symptoms and improve quality of life. We expect individuals allocated to the MBI group will endorse improved quality of life and reduced burnout (primary outcomes), as well as reduced stress, anxiety, and depression symptoms (secondary outcomes). Potential mechanisms of change include mindfulness, self-compassion, spirituality, decentering, and resilience skills.
Methods
Study design
The POLICE study is a multicenter, parallel, two-armed, RCT with 3 assessment points (baseline, post-intervention, and six-month follow-up). Participants will be randomized to MBI or a waiting list control group. This protocol was prepared in accordance with SPIRIT 2013 statement [40] and was approved by the centers ethical committees. The study was registered under ClinicalTrials.gov NCT03114605 on 03/21/17 and will be conducted following the CONSORT guidelines [41]. Figure 1 shows the participant flow through the trial.
Fig. 1.
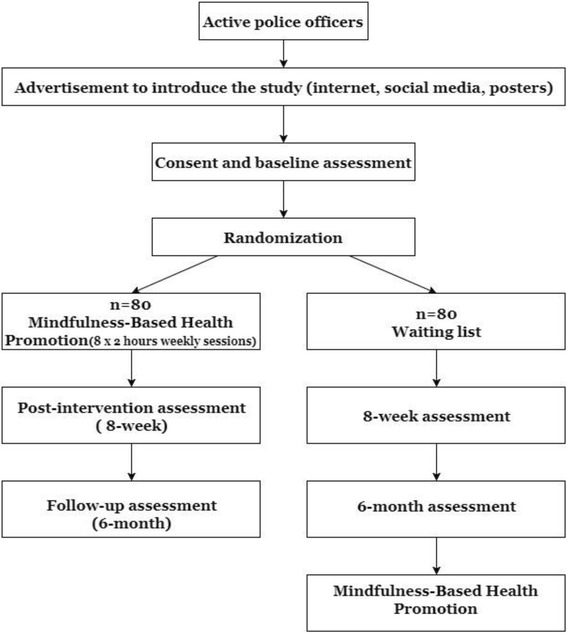
Study design
Sample size and power calculations
Power calculations were conducted to determinate the required sample size for the primary outcomes using the statistical software G * Power 3.1.9.2. The minimum sample for each group was identified as 64 to detect a moderate effect size of 0.5 (Cohen’s d) with a power of .80 and an alpha of 0.05, based on a previous study [42]. Therefore, the RCT will enroll 160 participants (80 each group) and allow for up to 20% loss to follow-up, expecting a minimum effective sample size of 128 individuals.
Participants and settings
Two types of police officers will be recruited for the POLICE study in two Brazilian metropolitan areas:
Civil Police. The study center in Porto Alegre will be located in the Police Hall of the State of Rio Grande do Sul. Civil Police main duties are to oversee public order and security, adopt measures necessary to avoid danger or injury to persons and public or private property, ensure the administration of criminal offenses, including execution of arrest warrants and requisitions requested by the judicial branch.
Civil Guard. The study center in São Paulo will be located in the headquarters of Unifesp Santo Amaro Campus. Civil Guard fundamental duties include the protection of goods, services and municipal facilities, as well as patrolling areas and preventive policing.
Eligibility
To be admitted in the study, participants will meet the following inclusion criteria: (a) be active police officers; (b) 21 to 65 years old; (c) available to attend 8 sessions; (d) willing to voluntarily participate. Exclusion criteria include: (a) previous involvement in any mindfulness-based intervention or being practicing mindfulness regularly in the last 3 months, or one of the following diagnosis, as evaluated by a trained psychologist using the Mini International Neuropsychiatric Interview (MINI) [43]: (b) major depressive episode (current); (c) manic or hypomaniac episode (current); (d) psychotic syndrome (current or past); (e) substance use disorder (past 12 months, except tobacco); (f) risk of suicide.
Recruitment, procedures and randomization
We will recruit 160 police officers from 2016 to 2018. Recruitment will be conducted using advertisements within the participating police organizations (Internet, social media, posters). Interested officers will contact the research team. After the first screening by phone or e-mail, potential participants will be scheduled for a face-to face interview, where they will be provided with detailed information about the study, fill the informed consent form and inclusion/exclusion criteria will be evaluated. Successful volunteers will be randomly assigned to the MBI or waitlist. Randomization will be implemented using sealed envelopes by an independent researcher who will be unaware of the characteristics of the study and will have no involvement in the trial or access to the study data. Participants allocated to the waitlist will not participate in any active intervention during this study period; however, they offered the MBI program after the 6-month follow-up. Each intervention and waitlist control group will be composed of around 20 participants. Due to the nature of the intervention, this will be a single-blind study, in which the outcomes assessment will be blind, but participants will be aware of their group assignment.
Interventionists
Two interventionists will lead the MBI groups - one in Porto Alegre and one in São Paulo. Both have been certified by Mente Aberta - Brazilian Center for Mindfulness and Health Promotion to teach mindfulness courses. This rigorous training follows the British and Brazilian guidelines for good practices of mindfulness [44, 45]. An independent experienced mindfulness teacher will assess intervention fidelity using video recordings of the sessions.
Intervention
The intervention in the POLICE study will be the Mindfulness-Based Health Promotion (MBHP) program [46]. MBHP is an 8-week MBI developed by our research group (see Table 1), based on the Mindfulness-Based Stress Reduction (MBSR) model created by Jon Kabat-Zinn and colleagues [47]. We adapted the MBSR model in order to suit the context and needs of primary health care and national and local health systems, developing a framework that supports the learning process to individuals from distinctive cultural and educational backgrounds. MBHP was designed to address human universal vulnerabilities, not focusing in any specific health condition. It has been applied over the last years by Mente Aberta - Brazilian Center for Mindfulness and Health Promotion [48], and by the University of Zaragoza, in Spain [49]. There is a strong emphasis on informal mindfulness practices, such as walking, eating, exercising, talking and doing housework. Concepts of radical acceptance [50], values clarification [51] and positive psychology [52] are also heavily emphasized. Compassion training techniques are also included in the program (equanimity in the condition of human suffering, receiving affection and showing affection to oneself), which can be particularly useful for persons high on guilt or self-criticism like police officers.
Table 1.
Mindfulness-Based Health Promotion content
| Session | Didactive teaching | Practices | Homework |
|---|---|---|---|
| 1. What is mindfulness | -Presentation and aims-Stress and dispersion-What is and what isn’t mindfulness-Characteristics, attitudes and motivation-Introduction to practice diaries | -Eating a raisin-Simple mindfulness exercises (listening to sounds, areas of contact with your body, the feel of your feet touching the floor)-Body scan-9-dots exercise | -Body scan-Attention for routine activity-Eating one meal mindfully-Mindfulness diary |
| 2. Mindfulness in breathing | -What to do with the body-What to do with the mind-Breathing-Information on posture-Preconceptions/fears/challenges in meditation | -Mindfulness in breathing-Body scan-Primary and secondary suffering | -Body scan-Mindfulness in breathing-Awareness of pleasant events (diary)-Attention for routine activity-Habit changing |
| 3. Mindfulness in the body (part I) | -Importance of the body-How mindfulness works-Cognitive defusion | -Mindful walking-Mindfulness in breathing-Hello, thank you and goodbye | -Body scan-Mindfulness in breathing-Mindful walking-Awareness of unpleasant events (diary)-Attention for routine walking |
| 4. Mindfulness in the body (part II) | -Doing mode/being mode-Reinforcing daily practice-Obstacles to the practice-Self -compassion | -Mindful movements -Mindfulness in breathing, sensations, sounds and thoughts-3-min breathing space-Mindful walking | -Body scan-Mindfulness in breathing-Mindful walking-3-min breathing space-Awareness of communication difficulties (diary) |
| 5. Mindfulness, acceptance and values | -Importance of acceptance-Values and committed action-Meaning of life-Hedonic and eudaimonic well-being | -Mindful movements-Mindfulness of thoughts-3-min breathing space in doubles | -Practice of choice-3-min breathing space during stress |
| 6. Silence | -Mindful movements-Body scan-Sitting meditation-Mindful walking | -Practice of choice-Mindfulness conversation | |
| 7. Compassion | -What is and what isn’t compassion-Biological basis-Ways of training compassion-Fear of compassion in western society | -Loving-kindness (for oneself and others)-Sitting meditation-Mindful movements | -Practice of choice- Loving-kindness (for oneself and others)-Attention for self-compassion in routine activity |
| 8. Mindfulness for life | -Mindfulness in daily life-Recommendation for long-term practice | -Loving-kindness (for oneself and others)-Mindfulness poetry | -Daily life mindfulness incorporation |
Assessments and outcomes
The three assessment points—baseline, post-intervention and follow-up—will occur over the two weeks preceding the intervention, the two weeks after the intervention, and six months after the intervention, respectively (see Table 2). The baseline assessment also will include sociodemographic and clinical characteristics. Survey Monkey Software [53] will be used for data collection. During research visits the participants will enter responses directly into the electronic system. Whenever this may not be possible, the research team will provide sheets of paper and the answers will be uploaded by the team. All instruments have been translated to Portuguese with reliable psychometric properties [54–64].
Table 2.
Assessments as a function of time points (according to 2013 SPIRIT figure guidelines)
| Measure | Target | T0 | T1 | T2 |
|---|---|---|---|---|
| Baseline | Post-intervention (8 weeks) | Follow-up (6 months) | ||
| MINI | Psychiatry disorders | x | ||
| WHOQOL-BREF | Quality of life | x | x | X |
| MBI-GS | Burnout symptoms | x | x | X |
| PSQ | Stress | x | x | X |
| HADS | Anxiety and depression symptoms | x | x | X |
| CD-RISC-25 | Resilience | x | x | X |
| MAAS | Mindfulness trait | x | x | X |
| EQ | Decentering | x | x | X |
| SCS | Self-compassion | x | x | X |
| GHQ-12 | Mental well-being | x | x | X |
| BCSQ-12 | Burnout subtypes | x | x | X |
| WHOQOL-SRPB-BREF | Spirituality, religiosity and personal beliefs | x | x | X |
| DUREL | Religiosity | x | x | X |
MINI Mini International Neuropsychiatric Interview, WHOQOL-BREF World Health Organization Quality of Life bref, MBI-GS Maslach Burnout Inventory - General Survey, PSQ Police Stress Questionnaire, HADS Hospital Anxiety and Depression Scale, CD-RISC-25 Connor-Davidson-25 Scale of Resilience, MAAS Mindful Attention Awareness Scale, EQ Experience Questionnaire, SCS Self Compassion Scale, GHQ-12 The 12-Item General Health Questionnaire, BCSQ-12 Burnout Clinical Subtype Questionnaire, WHOQOL-SRPB-BREF World Health Organization Quality of Life Bref -Spirituality, Religiousness and Personal Beliefs, DUREL Duke University Religion Index
Diagnostic interview
The Mini International Neuropsychiatric Interview (MINI) is a short, structured diagnostic interview that is used for the diagnosis of DSM-IV and ICD-10 psychiatric disorders. With an administration time of approximately 15 min, the MINI was designed to provide a short but accurate structured psychiatric interview for multicentric clinical trials and epidemiology studies [43].
Primary outcomes measures
World Health Organization Quality of Life- BREF (WHOQOL-BREF): the World Health Organization has developed a quality of life instrument, the WHOQOL, which captures many subjective aspects of quality of life. The WHOQOL-BREF is a WHOQOL shorter version, comprises 26 items that produces scores for four domains related to quality of life: physical health, psychological, social relationships and environment. It also includes one facet on overall quality of life and general health. Is one of the best known instruments that has been developed for cross-cultural comparisons of quality of life and is available in more than 40 languages [65]. Evidence consistently shows that officers exhibit low quality of life and its correlation with adverse mental health outcomes [4, 66, 67].
Maslach Burnout Inventory - General Survey (MBI-GS): is considered one of the leading measures of burnout. Validated by extensive research, MBI-GS Surveys address three dimensions: Emotional Exhaustion measures feelings of being emotionally overextended and exhausted by one’s work; Depersonalization measures an unfeeling and impersonal response toward recipients of one’s service, care treatment, or instruction; Personal Accomplishment measures feelings of competence and successful achievement in one’s work. The MBI-GS is designed for use with occupational groups. The 3 dimensions are distributed in 16 items, whose answers are given on a 7-point Likert scale that varies from “never” to “every day” [68]. Nature and environment of police work contributes to high burnout rates which are associated with escalating symptoms of diminished health [22].
Secondary outcomes measures
Police Stress Questionnaire (PSQ) - stress will be measured using the PSQ, a 40-item psychometric questionnaire consisting of two subscales that measure organizational and operational stressors in the context of police work, using 7-point scales (Likert type) ranging from 1 (absence of stress) to 7 extreme stress). The PSQ was developed as an alternative to the general scales of stress at work in order to reflect the specifics stressors of police occupation [69].
Hospital Anxiety and Depression Scale (HADS) - is a 14-item questionnaire with seven items measuring anxiety (HAD-A) and seven measuring depression (HAD-D). The ratings are totaled to obtain a score ranging from 0 to 21 for anxiety and depression, with higher scores indicating greater depression or anxiety. Scores between 8 and 10 represent possible cases of anxiety or depression, and scores that are ≥11 correspond to probable cases [70].
Connor-Davidson-25 Scale of Resilience (CD-RISC-25): it assesses the ability of individuals to cope and adapt physically, mentally, and spiritually to the circumstances imposed by life. CD-RISC-25 is composed of 25 items on a Likert scale (0–4), with larger scores reflecting greater resilience. Resilience may be viewed as a measure of stress coping ability and, as such, could be an important target of treatment in anxiety, depression, and stress reactions [71].
Mindful Attention Awareness Scale (MAAS): is a 15-item scale designed to assess a core characteristic of dispositional mindfulness, namely, open or receptive awareness of and attention to what is occurring in the present. The scale has strong psychometric properties and has been validated with college, community, and cancer patient samples [72].
Experience Questionnaire (EQ): this instrument was designed to measure the capacity to observe one’s thoughts and feelings as temporary and objective events of the mind, also known as “decentering”. Items from the scale are rated on a Likert scale ranging between 1 (never or very rarely true) and 5 (very often or always true), with higher scores indicating greater decentering [73].
Self Compassion Scale (SCS): is composed by 26 items measuring six components of self-compassion: self-kindness, self-judgment, common humanity, isolation, mindfulness and over-identification.The items are rated on a five-point response scale ranging from 1 (almost never) to 5 (almost always) [74].
The 12-Item General Health Questionnaire (GHQ-12): is the most extensively used screening instrument for common mental disorders, in addition to being a more general measure of mental well-being. It consists of 12 items, whose answers are given on a 4-point Likert scale [75].
Burnout Clinical Subtype Questionnaire (BCSQ-12): it aims to evaluate the most important clinical subtypes of burnout, comprising the dimensions of overload, lack of development and neglect. Consists of 12 items distributed in 3 dimensions, whose answers are given on a 7-point Likert scale ranging from “totally agree” to “totally disagree” [76].
WHOQOL-SRPB-BREF: this scale measures the domains of spirituality, religiosity and personal beliefs in the quality of life from a cross-cultural perspective. Combines one item extracted from each of the eight SRPB facets in the WHOQOL-SRPB, with the 26 WHOQOL-BREF items, extracted from the WHOQOL-100, to construct the 34 item WHOQOL-SRPB-BREF [77].
Duke University Religion Index (DUREL): scale of religiousness developed by Duke University, 5 items are used to evaluate religious involvement. It captures the three dimensions of religiosity that most correlate with health outcomes: organizational religiosity, non-organizational religiosity, and intrinsic religiosity (or subjective religiosity) [78].
To explore the feasibility and adherence of MBHP among police officers, the frequency of attendance to the sessions will be assessed. At the post-intervention and the six-month follow-up evaluations we will address mindfulness practice parameters such as type, frequency and length of personal meditative practice through a questionnaire created by our research group [79].
Statistical analysis
Intention-to-treat (ITT) and per protocol analyses (PPA) will be conducted following the CONSORT recommendations for reporting the results [41]. Baseline differences between groups on sociodemographic and clinical variables will be assessed using Chi-square tests for categorical variables and analysis of variance (ANOVA) for continuous data. A 2 (Group: MBI vs. WL) × 3 (Time: baseline, post, and 6-month follow-up) repeated measures ANOVA will be conducted to test the effects of the intervention for all primary and secondary outcomes. Effect sizes (Cohen’s d) and confidence intervals for within- and between-group comparisons will be performed for each study outcome. Missing data will be handled according to the most appropriate method depending on the reasons for missingness, following the authors’ recommendations and sensitivity analyses principles [80].
To study potential working mechanisms of mindfulness intervention, mediation analysis will be conducted using the Preacher and Hayes (2004) procedure [81]. The mediation effects of mindfulness, self-compassion, resilience, decentering and spirituality on burnout symptoms and quality of life will be evaluated.
Ethical considerations
The study is registered at ClinicalTrials.gov as NCT03114605 and we have adopted the SPIRIT Statement recommendations for Clinical Trials [40]. Declaration of Helsinki protocols are being followed and patients will give written informed consent. The study was approved by HCPA and UNIFESP Research Ethics Committees under number 60406416.9.1001.5327.
Trial status
At the time of this manuscript submission, recruitment for the POLICE study is ongoing.
Discussion
To our knowledge, the impact of an MBI on quality of life among police officers has yet to be scientifically investigated. The POLICE study will also empirically evaluate the influence of MBHP on burnout, anxiety, depression, self-compassion, spirituality, stress, mindfulness, and resilience post-intervention, and at six-month follow-up to assess if potential gains are maintained.
A previous study showed high levels of adherence to a MBI in Brazil [42]. It is relevant to address the feasibility and adherence of this intervention in Brazilian police officers, commonly exposed to dangerous environments and long shifts. We hope to demonstrate, assuming our a priori hypothesis is true, that the health promotion effects of MBIs already demonstrated for a diverse population, is also valid for these high-stress professionals. Great emphasis is placed on physical health cultivation in police training, however evidence-based mental health and quality of life enhancing programs are scarce [82].
One limitation of the study is the use of a waitlist control design, rather than an active control intervention. There is a growing discussion over the use of waitlist in psychological and behavioral research [83]. While there are ethical advantages to a waitlist design because it allows for the provision of care to research participants who are seeking help whilst permitting a non-intervention evaluation, specially in a non-clinical population as ours, it has been noted that such designs may overestimate intervention effects [84].
Despite this limitation, a better understanding of how MBIs may improve police officer mental health is essential to foster the development of future practices, procedures and policies for police institutions around the world. We believe the POLICE study will contribute to this understanding, by seeking to improve physical, emotional and mental fitness, and nourishing the conditions for more effective policing and contributing to society as a whole.
Acknowledgments
The authors would like to gratefully acknowledge the support by the Health and Social Departments of the Civil Police (Porto Alegre) and Civil Guard (São Paulo). Many thanks to Emerson Wendt, Leonel Fagundes Carivali, Fernanda Sobroza de Mello, Daniela da Silva Duarte Capoani, Najla Maria dos Santos, Lisiane Maria Paganotto, Francisco Salles, Henrique da Silva, Marianna Abreu Costa, Noé Zamel, Fernando Carlos Tozi, Maria Cândida Macedo de Barros and Ricardo da Silva. The authors extend their sincere appreciation to the Civil Police psychology team for their assistance.
Funding
The Police study is funded (financial support) by Hospital de Clínicas de Porto Alegre Research Incentive Fund (FIPE) and by Mente Aberta - Brazilian Center for Mindfulness and Health Promotion.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- DSM-IV
Diagnostic and Statistical Manual of Mental Disorders, 4th Edition
- HCPA
Hospital de Clínicas de Porto Alegre - Federal University of Rio Grande do Sul
- ICD-10
International Statistical Classification of Diseases and Related Health Problems, 10th Revision
- MBHP
Mindfulness-Based Health Promotion
- MBI
Mindfulness-Based Intervention
- MBIs
Mindfulness-Based Interventions
- RCT
Randomized Controlled Trial
- UNIFESP
Federal University of São Paulo
Authors’ contributions
MT, MMPD and NSR co-conceptualized and designed the study. MT wrote the first draft. DB planned the statistical analysis. MMPD, VS, KC and SBA are coordinating the study at São Paulo center. SBA is particularly involved in the implementation and conduction of the project at at this site. KC is responsible for the data collection. MT and NSR are coordinating the study implementation and conduction at Porto Alegre center. MSC, JGC, LR, VS and FC commented and critically reviewed the manuscript for important intellectual content. MMPD and NSR obtained funding and supervised all steps. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This study is approved by the HCPA and UNIFESP Research Ethics Committees. Reference number 60406416.9.1001.5327. Participants will be asked for informed consent in written form.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Marcelo Trombka, Email: marcelotrombka@gmail.com.
Marcelo Demarzo, Email: demarzo@unifesp.br.
Daniel Campos Bacas, Email: camposdcb@gmail.com.
Sonia Beira Antonio, Email: sonia@desenvolvesh.com.br.
Karen Cicuto, Email: karencicuto@hotmail.com.
Vera Salvo, Email: desalvo@terra.com.br.
Felipe Cesar Almeida Claudino, Email: lipec.almeida@gmail.com.
Letícia Ribeiro, Email: ribe6180@pacificu.edu.
Michael Christopher, Email: mchristopher@pacificu.edu.
Javier Garcia-Campayo, Email: jgarcamp@gmail.com.
Neusa Sica Rocha, Email: nrsica@gmail.com.
References
- 1.Anderson GS, Litzenberger R, Plecas D. Physical evidence of police officer stress. Policing: An International Journal of Police Strategies & Management. 2002;25(2):399–420. doi: 10.1108/13639510210429437. [DOI] [Google Scholar]
- 2.McCarty WP, Skogan WG. Job-related burnout among civilian and Sworn police personnel. Police Quarterly. 2013;16(1):66–84. doi: 10.1177/1098611112457357. [DOI] [Google Scholar]
- 3.Burke RJ. Burnout in police work. Stress in policing: sources, consequences and interventions. London: Routledge; 2016. p. 153. [Google Scholar]
- 4.Wang Z, Inslicht SS, Metzler TJ, Henn-Haase C, McCaslin SE, Tong H, Marmar CR. A prospective study of predictors of depression symptoms in police. Psychiatry Res. 2010;175(3):211–216. doi: 10.1016/j.psychres.2008.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCafferty FL, McCafferty E, McCafferty MA. Stress and suicide in police officers: paradigm of occupational stress. South Med J. 1992;85(3):233–243. doi: 10.1097/00007611-199203000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Clark DW, White EK, Violanti J. Law enforcement suicide: current knowledge and future directions. The Police Chief. 2012;79:48–51. [Google Scholar]
- 7.Violanti JM. Suicide or undetermined? A national assessment of police suicide death classification. Int J Emerg Ment Health. 2010;12(2):89–94. [PubMed] [Google Scholar]
- 8.Violanti J, et al. Associations of stress, anxiety, and resiliency in police work. Occup Environ Med. 2014;71(Suppl 1):A3. doi: 10.1136/oemed-2014-102362.8. [DOI] [Google Scholar]
- 9.Joseph PN, Violanti JM, Donahue R, Andrew ME, Trevisan M, Burchfiel CM, Dorn J. Police work and subclinical atherosclerosis. J Occup Environ Med. 2009;51(6):700–707. doi: 10.1097/JOM.0b013e3181a02252. [DOI] [PubMed] [Google Scholar]
- 10.McCraty R, Atkinson M. Resilience training program reduces physiological and psychological stress in police officers. Glob Adv Health Med. 2012;1(5):44–66. doi: 10.7453/gahmj.2012.1.5.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vena JE, Violanti JM, Marshall J, Fiedler RC. Mortality of a municipal worker cohort: III. Police officers. Am J Ind Med. 1986;10(4):383–397. doi: 10.1002/ajim.4700100406. [DOI] [PubMed] [Google Scholar]
- 12.Violanti JM, Vena JE, Petralia S. Mortality of a police cohort: 1950-1990. Am J Ind Med. 1998;33(4):366–373. doi: 10.1002/(SICI)1097-0274(199804)33:4<366::AID-AJIM6>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 13.Alexopoulos EC, et al. Exploring stress levels, job satisfaction, and quality of life in a sample of police officers in Greece. Safety and Health at Work. 2014;5(4):210–215. doi: 10.1016/j.shaw.2014.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Filho RTB, Júnior ADO. Metabolic syndrome and military Policemen’s quality of life. Am J Mens Health. 2014;8(6):503–509. doi: 10.1177/1557988314526750. [DOI] [PubMed] [Google Scholar]
- 15.Silva FC, et al. Health-related quality of life and related factors of military police officers. Health Qual Life Outcomes. 2014;12(1):60. doi: 10.1186/1477-7525-12-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barbosa WG, et al. Physical fitness, body composition and quality of life among Brazilian police recruits: 422 board #243 may 31 9: 30 AM - 11: 00 AM. Med Sci Sports Exerc. 2017;49(5S):112. doi: 10.1249/01.mss.0000517132.28918.17. [DOI] [Google Scholar]
- 17.Numbeo doo, 2017. Crime Index for Country 2017 Mid-Year. https://www.numbeo.com/crime/rankings_by_country.jsp . Accessed 15 June 2017.
- 18.Numbeo doo, 2017. Crime Index 2017. https://www.numbeo.com/crime/rankings.jsp?title=2017. Accessed 15 June 2017.
- 19.Rajaratnam SW, Brager LK, Lockley SW, Shea SA, Wang W, Landrigan CP, Czeisler CA. Sleep disorders, health and safety in police officers. J Am Med Assoc. 2011;306:2567–2578. doi: 10.1001/jama.2011.1851. [DOI] [PubMed] [Google Scholar]
- 20.Waggoner LB, et al. A combined field and laboratory design for assessing the impact of night shift work on police officer operational performance. Sleep. 2012;35(11):1575–1577. doi: 10.5665/sleep.2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martinussen M, Richardsen AM, Burke RJ. Job demands, job resources, and burnout among police officers. J Crim Just. 2007;35(3):239–249. doi: 10.1016/j.jcrimjus.2007.03.001. [DOI] [Google Scholar]
- 22.de la Fuente Solana EI, Aguayo R, Vargas Pecino C, Cañadas de la Fuente G. Prevalence and risk factors of burnout syndrome among Spanish police officers. Psicothema. 2013;25(4):488–493. doi: 10.7334/psicothema2013.81. [DOI] [PubMed] [Google Scholar]
- 23.Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York: Delta Trade Paperbacks; 2005. [Google Scholar]
- 24.Segal ZV, Williams JMG, Teasdale JD, Gemar MC. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. Clin Psychol Psychother. 2002;9(2):123–125. doi: 10.1002/cpp.320. [DOI] [Google Scholar]
- 25.Khoury B, et al. Mindfulness-based stress reduction for healthy individuals: a meta-analysis. J Psychosom Res. 2015;78(6):519–528. doi: 10.1016/j.jpsychores.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 26.Khoury B, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev. 2013;33(6):763–771. doi: 10.1016/j.cpr.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 27.Hofmann SG, et al. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. Consult Clin Psychol. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luken M, Sammons A. Systematic review of mindfulness practice for reducing job burnout. Am J Occup Ther. 2016;70(2):7002250020p1–7002250020p10. doi: 10.5014/ajot.2016.016956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Regehr C, et al. Interventions to reduce the consequences of stress in physicians: a review and meta-analysis. J Nerv Ment Dis. 2014;202(5):353–359. doi: 10.1097/NMD.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 30.Zenner C, Herrnleben-Kurz S, Walach H. Mindfulness-based interventions in schools—a systematic review and meta-analysis. Front Psychol. 2014;5(5):603. [DOI] [PMC free article] [PubMed]
- 31.Kallapiran K, et al. Review: effectiveness of mindfulness in improving mental health symptoms of children and adolescents: a meta-analysis. Child Adolesc Mental Health. 2015;20(4):182–194. doi: 10.1111/camh.12113. [DOI] [PubMed] [Google Scholar]
- 32.Johnson DC, Thom NJ, Stanley EA, Haase L, Simmons AN, Shih PAB, Paulus MP. Modifying resilience mechanisms in atrisk individuals: a controlled study of mindfulness training in marines preparing for deployment. Am J Psychiatr. 2014;171(8):844–853. doi: 10.1176/appi.ajp.2014.13040502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stanley EA, et al. Mindfulness-based mind fitness training: a case study of a high-stress predeployment military cohort. Cogn Behav Pract. 2011;18(4):566–576. doi: 10.1016/j.cbpra.2010.08.002. [DOI] [Google Scholar]
- 34.Epstein RM, Krasner MS. Physician resilience: what it means, why it matters, and how to promote it. Acad Med. 2013;88(3):301–303. doi: 10.1097/ACM.0b013e318280cff0. [DOI] [PubMed] [Google Scholar]
- 35.Schroeder DA, et al. A brief mindfulness-based intervention for primary care physicians: a pilot randomized controlled trial. Am J Lifestyle Med. 2016; 10.1177/1559827616629121. [DOI] [PMC free article] [PubMed]
- 36.Kaplan JB, et al. Role of resilience in mindfulness training for first responders. Mindfulness. 2017; 10.1007/s12671-017-0713-2. [DOI] [PMC free article] [PubMed]
- 37.Meiklejohn J, et al. Integrating mindfulness training into K-12 education: fostering the resilience of teachers and students. Mindfulness. 2012;3(4):291–307. doi: 10.1007/s12671-012-0094-5. [DOI] [Google Scholar]
- 38.Christopher MS, Goerling RJ, Rogers BS, Hunsinger M, Baron G, Bergman AL, Zava DT. A pilot study evaluating the effectiveness of a mindfulness-based intervention on cortisol awakening response and health outcomes among law enforcement officers. J Police Crim Psychol. 2016;31(1):15–28. doi: 10.1007/s11896-015-9161-x. [DOI] [Google Scholar]
- 39.Christopher MS, Hunsinger M, Goerling LRJ, Bowen S, Rogers BS, Gross CR, Dapolonia E, Pruessner JC. Mindfulness-based resilience training to reduce health risk, stress reactivity, and aggression among law enforcement officers: A feasibility and preliminary efficacy trial. Psychiatry Res. 2018;264:104-15. 10.1016/j.psychres.2018.03.059. [DOI] [PMC free article] [PubMed]
- 40.Chan AW, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200–207. doi: 10.7326/0003-4819-158-3-201302050-00583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schulz KF, Altman DG, Moher, D.CONSORT. Statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010; 10.1136/bmj.c332. [DOI] [PubMed]
- 42.Demarzo MM, Andreoni S, Sanches N, Perez S, Fortes S, Garcia-Campayo J. Mindfulness-based stress reduction (MBSR) in perceived stress and quality of life: an open, uncontrolled study in a Brazilian healthy sample. Explore: New York. 2014;10(2):118–20. [DOI] [PubMed]
- 43.Van Vliet IM, de Beurs E. The MINI-international neuropsychiatric interview. A brief structured diagnostic psychiatric interview for DSM-IV en ICD-10 psychiatric disorders. Tijdschr Psychiatr. 2007;49(6):393–397. [PubMed] [Google Scholar]
- 44.UK Network of Mindfulness Teacher Training Organizations. Good Practice Guidance for Teachers (2015). http://www.mindfulnessteachersuk.org.uk. Accessed 27 June 2017.
- 45.Brazilian Center for Mindfulness and Health Promotion. 2017. https://www.mindfulnessbrasil.com/formacao/formacao-modular/boas-praticas. Accessed 20 June 2017.
- 46.Demarzo M, Garcia-Campayo J. Manual Prático de mindfulness: curiosidade e aceitação. 1. São Paulo: Palas Athena; 2015. [Google Scholar]
- 47.Kabat-Zinn J. Mindfulness-based stress reduction (MBSR) Constr Hum Sci. 2003;8(2):73–107. [Google Scholar]
- 48.Brazilian Center for Mindfulness and Health Promotion. http://www.mindfulnessbrasil.com Accessed 7 July 2017.
- 49.Grupo de Investigación en Mindfulness y Compasión. Universidad de Zaragoza. http://www.webmindfulness.com (2017). Accessed 7 July 2017.
- 50.Dimeff L, Linehan M. M. (2001). Dialectical behavior therapy in a nutshell. Calif Psychol. 2001;34:10–13. [Google Scholar]
- 51.Luciano JV, Guallar JA, Aguado J, López-Del-Hoyo Y, et al. Effectiveness of group acceptance and commitment therapy for fibromyalgia: a 6-month randomized controlled trial (EFFIGACT study) Pain. 2014;155(4):693–702. doi: 10.1016/j.pain.2013.12.029. [DOI] [PubMed] [Google Scholar]
- 52.Ciarrochi J, Kashdan TB. Mindfulness, acceptance, and positive psychology\rThe seven foundations of WellBeing. California: New Harbinger; 2013. [Google Scholar]
- 53.SurveyMonkey. https://pt.surveymonkey.com/ (2017). Accessed 23 June 2017.
- 54.Fleck MP, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L, Pinzon V. (2000). Application of the Portuguese version of the abbreviated instrument of quality life WHOQOL-bref. Revista de Saude Publica. 2000;34(2):178–183. doi: 10.1590/S0034-89102000000200012. [DOI] [PubMed] [Google Scholar]
- 55.Tamayo MR. Universidade federal da Paraíba (org.). III Congresso Norte-Nordeste de Psicologia. Anais. João Pessoa: UFPB; 2003. Validação do Inventário de burnout de Maslach; pp. 392–393. [Google Scholar]
- 56.Cardoso, A.L.S. Validação de duas escalas de stresse ocupacional para a Polícia de Segurança Pública. Faculdade de Psicologia e de Ciências da Educação da Universidade de Coimbra, 2010. http://hdl.handle.net/10316/15597. Accessed 9 July 2017.
- 57.Pais-Ribeiro J, Silva I, Ferreira T, Martins A, Meneses R, Baltar M. Validation study of a Portuguese version of the hospital anxiety and depression scale. Psychol Health Med. 2007;12(2):225–237. doi: 10.1080/13548500500524088. [DOI] [PubMed] [Google Scholar]
- 58.Solano JPC, Bracher ESB, Faisal-Cury A, Ashmawi HA, Carmona MJC, Lotufo Neto F, Vieira JE. Factor structure and psychometric properties of the Connor-Davidson resilience scale among Brazilian adult patients. Sao Paulo Medical Journal. 2016;134(5):400–406. doi: 10.1590/1516-3180.2015.02290512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.de Barros VV, Kozasa EH, de Souza ICW, Ronzani TM. Validity evidence of the brazilian version of the mindful attention awareness scale (MAAS) Psicologia: Reflexão E Crítica. 2015;28(1):87–95. [Google Scholar]
- 60.Gregório S, Pinto-Gouveia J, Duarte C, Simões L. Expanding research on decentering as measured by the Portuguese version of the experiences questionnaire. Span J Psychol. 2015;18:1–14. doi: 10.1017/sjp.2015.18. [DOI] [PubMed] [Google Scholar]
- 61.Souza LK, Hutz CS. Adaptation of the self-compassion scale for use in Brazil: evidences of construct validity. Temas Em Psicologia. 2016;24(1):159–172. doi: 10.9788/TP2016.1-11. [DOI] [Google Scholar]
- 62.Gouveia VV, Barbosa GA, Andrade E de O, Carneiro MB. Factorial validity and reliability of the general health questionnaire (GHQ-12) in the Brazilian physician population. Cadernos de Saúde Pública. 2010;26(7):1439–1445. doi: 10.1590/S0102-311X2010000700023. [DOI] [PubMed] [Google Scholar]
- 63.Panzini RG, Maganha C, da Rocha NS, Bandeira DR, Fleck MP. Validação Brasileira do instrumento de qualidade de Vida/espiritualidade, religião e crenças pessoais. Revista de Saude Publica. 2011;45(1):153–165. doi: 10.1590/S0034-89102011000100018. [DOI] [PubMed] [Google Scholar]
- 64.Lucchetti G, Lucchetti ALG, Peres MF, Leão FC, Moreira-Almeida A, Koenig HG. Validation of the Duke religion index: DUREL (Portuguese version) J Relig Health. 2012;51(2):579–586. doi: 10.1007/s10943-010-9429-5. [DOI] [PubMed] [Google Scholar]
- 65.Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial a report from the WHOQOL group. Qual Life Res. 2004;13(2):299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 66.Lipp MEN. Stress and quality of life of senior Brazilian police officers. Span J Psychol. 2009;12(2):593–603. doi: 10.1017/S1138741600001967. [DOI] [PubMed] [Google Scholar]
- 67.MacMillan F, Karamacoska D, El Masri A, McBride KA, Steiner GZ, Cook A, Kolt GS, Klupp N, George ES. A systematic review of health promotion intervention studies in the police force: study characteristics, intervention design and impacts on health. Occup Environ Med. 2017;74(12):913-23. 10.1136/oemed-2017-104430. [DOI] [PubMed]
- 68.Bakker AB, Demerouti E, Schaufeli WB. Validation of the Maslach burnout inventory - general survey. Anxiety Stress Coping. 2002;15:245–260. doi: 10.1080/1061580021000020716. [DOI] [Google Scholar]
- 69.McCreary DR, Thompson MM. Development of two reliable and valid measures of stressors in policing: the operational and organizational police stress questionnaires. Int J Stress Manag. 2006;13(4):494–518. doi: 10.1037/1072-5245.13.4.494. [DOI] [Google Scholar]
- 70.Zigmond AS, Snaith RP. The hospital anxiety and depression scale (HADS) Acta Psychiatr Scand. 1983;67(361–370):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 71.Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 72.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being: mindfulness attention and awareness scale. J Pers Soc Psychol. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 73.Fresco DM, Moore MT, van Dulmen MHM, Segal ZV, Ma SH, Teasdale JD, Williams JMG. Initial psychometric properties of the experiences questionnaire: validation of a self-report measure of decentering. Behav Ther. 2007;38(3):234–246. doi: 10.1016/j.beth.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 74.Neff KD. Development and validation of a scale to measure self-compassion. Self Identity. 2003;2:223–250. doi: 10.1080/15298860309027. [DOI] [Google Scholar]
- 75.Hillier G. The 12-item general health questionnaire (GHQ-12) Soc Psychiatry Psychiatr Epidemiol. 1979;20(4):839–843. [Google Scholar]
- 76.Montero-Marín J, Skapinakis P, Araya R, Gili M, García-Campayo J. Towards a brief definition of burnout syndrome by subtypes: development of the “burnout clinical subtypes questionnaire” (BCSQ-12) Health Qual Life Outcomes. 2011;9(1):74. doi: 10.1186/1477-7525-9-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Skevington SM, Gunson KS, O’Connell KA. Introducing the WHOQOL-SRPB BREF: developing a short-form instrument for assessing spiritual, religious and personal beliefs within quality of life. Qual Life Res. 2013;22(5):1073–1083. doi: 10.1007/s11136-012-0237-0. [DOI] [PubMed] [Google Scholar]
- 78.Koenig H, GRJ P, Meador KG. Religion index for psychiatric research. Am J Psychiatry. 1997;154(6):885–886. doi: 10.1176/ajp.154.6.885b. [DOI] [PubMed] [Google Scholar]
- 79.Soler J, Cebolla A, Feliu-Soler A, Demarzo MM, Pascual JC, Baños R, García-Campayo J. Relationship between meditative practice and self-reported mindfulness: the MINDSENS composite index. PLoS One. 2014;9(1):e86622. 10.1371/journal.pone.0086622. [DOI] [PMC free article] [PubMed]
- 80.Thabane L, Mbuagbaw L, Zhang S, Samaan Z, Marcucci M, Ye C, Goldsmith CH. A tutorial on sensitivity analyses in clinical trials: the what, why, when and how. BMC Med Res Methodol. 2013;13(1):92. doi: 10.1186/1471-2288-13-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–731. doi: 10.3758/BF03206553. [DOI] [PubMed] [Google Scholar]
- 82.Patterson GT, Chung IW, Swan PW. Stress management interventions for police officers and recruits: a meta-analysis. J Exp Criminol. 2014;10(4):487–513. doi: 10.1007/s11292-014-9214-7. [DOI] [Google Scholar]
- 83.Hart T, Fann JR, Novack TA. The dilemma of the control condition in experience-based cognitive and behavioural treatment research. Neuropsychol Rehabil. 2008;18(1):1–21. doi: 10.1080/09602010601082359. [DOI] [PubMed] [Google Scholar]
- 84.Cunningham JA, Kypri K, McCambridge J. Exploratory randomized controlled trial evaluating the impact of a waiting list control design. BMC Med Res Methodol. 2013;13(1):150. doi: 10.1186/1471-2288-13-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


