Abstract
Context
The National Poison Data System (NPDS) is a database and surveillance system for US poison centers (PCs) call data. The Centers for Disease Control and Prevention (CDC) and American Association of Poison Control Centers (AAPCC) use NPDS to identify incidents of potential public health significance. State health departments are notified by CDC of incidents identified by NPDS to be of potential public health significance. Our objective was to describe the public health impact of CDC's notifications and the use of NPDS data for surveillance.
Methods
We described how NPDS data informed three public health responses: the Deepwater Horizon incident, national exposures to laundry detergent pods, and national exposures to e-cigarettes. Additionally, we extracted survey results of state epidemiologists regarding NPDS incident notification follow-up from 1 January 2015 to 31 December 2016 to assess current public health application of NPDS data using Epi Info 7.2 and analyzed data using SAS 9.3. We assessed whether state health departments were aware of incidents before notification, what actions were taken, and whether CDC notifications contributed to actions.
Discussion
NPDS data provided evidence for industry changes to improve laundry detergent pod containers safety and highlighted the need to regulate e-cigarette sale and manufacturing. NPDS data were used to improve situational awareness during the 2010 Deepwater Horizon oil spill. Of 59 health departments and PCs who responded to CDC notifications about anomalies (response rate = 49.2%), 27 (46%) reported no previous awareness of the incident, and 20 (34%) said that notifications contributed to public health action.
Conclusions
Monitoring NPDS data for anomalies can identify emerging public health threats and provide evidence-based science to support public health action and policy changes.
Keywords: National Poison Data System, Poison Control Center, public health, surveillance
Introduction
The National Poison Data System (NPDS) serves as the nationwide poison center (PC) data repository and near-real-time surveillance system [1]. To identify incidents related to chemical, radiological, or infectious agents, the National Center for Environmental Health of the Centers for Disease Control and Prevention (CDC) and the American Association of Poison Control Centers (AAPCC) have collaborated since 2002 to conduct surveillance on PC data using NPDS [2,3].
The US network of 55 PCs responds to questions from the public, health care professionals, and public health agencies. The PCs provide access to health care professionals who have specialized expertise in clinical and medical toxicology and who can provide treatment advice by telephone [1]. A toll-free number for 24-hour professional assistance is available, covering the 50 states, District of Columbia, American Samoa, Federated States of Micronesia, Guam, Puerto Rico, and the US Virgin Islands [1]. Physicians benefit from accessing the PC by receiving consultations in clinical and medical toxicology. These include the latest clinical recommendations and findings, information regarding emerging threats, and advice on case management. Callers to PCs play a crucial role in identifying public health threats (e.g., outbreaks, chemical spills) and informing PCs such that these public health threats can be tracked by NPDS.
Calls to PCs range from simple requests for information to concerns about a potential or confirmed hazardous exposure. An exposure is defined as an actual or suspected contact with any substance that has been ingested, inhaled, absorbed, applied to, or injected into the body [3]. The number of exposure and information calls to all US PCs averages 3 million annually [1]. In 2015, US PCs managed 5941 calls about human exposures per day, equivalent to about 2.2 million exposure cases per year [1]. Poison centers upload data to NPDS on average every 9.52 [IQR: 7.40, 13.60] minutes, creating a near real-time national exposure database and surveillance system [1].
NPDS surveillance and anomaly detection
After PC data are uploaded into NPDS, the system automatically aggregates and analyzes the data for anomalies [3]. Three different types of anomalies are identified by this system – increases in call volume, increases in reports of specific clinical effects, and reports of single cases of exposure to a pre-determined list of agents. Call volume surveillance identifies anomalies by comparing the hourly total call volume for each PC with 5 years of hourly data for the PC [2,3]. Clinical effect surveillance identifies anomalies for individual clinical effects by comparing the total call volume reporting that clinical effect nationally over a 24-hour period [2,3]. Case-based surveillance identifies anomalies meeting a specified definition. It is used to identify high priority exposures, including CDC category A (e.g., anthrax, botulism) and B (e.g., E. coli O157:H7, V. cholerae) biological agents [2,3]. Increased numbers trigger call volume and clinical effect volume surveillance, whereas case-based anomalies are identified by a single call matching a specified definition [2,3].
Anomalies identified by NPDS are reviewed by clinical and medical toxicologists and epidemiologists from AAPCC and CDC to determine public health significance [3]. An anomaly is determined to be a potential incident of public health significance if it meets any of the following criteria [4]:
Obvious geographic or spatial pattern;
High index of suspicion or credible threat;
Association with suspected terrorism event;
Obvious interest to appropriate state or national public health entity;
Part of a state or national public health investigation;
Unusual severity of magnitude;
Pattern not normally attributable to the implicated exposure.
Since May 2013, CDC has notified state health departments and PCs via email about incidents of potential public health significance that might warrant further public health involvement [2]. From May 2013 to December 2016, CDC sent a total of 177 email notifications regarding incidents that range from clustered cases of food poisoning to occupational exposures to gases or non-pharmaceutical chemicals. Previous reports have described the NPDS surveillance system and detected incidents of potential public health significance in detail and highlight the importance of this near real-time surveillance capability [2,3,5].
This paper adds to existing literature and describes the use of PC data for public health surveillance through historical successes and the future potential of NPDS surveillance. Three historical examples are provided to illustrate the public health impact of using NPDS surveillance data to prompt public health action and policy changes. To further understand the potential of NPDS surveillance, this paper is the first to describe the public health impact of CDC's notification to state epidemiologists of incidents of potential public health significance. This assessment is an essential step in conducting surveillance using NPDS for closing the loop between identification of an incident and resulting public health response, as well as an assessment of public health impact of surveillance using NPDS.
Methods
Three historical incidents of public health significance identified from surveillance activities demonstrate how further characterization of the incidents led to public health action or policy changes. Information for these examples was collected by reviewing the scientific literature and publically available official policy statements.
In May 2013, CDC began sending email notifications to state epidemiologists to alert them to incidents of potential public health significance identified through NPDS. Beginning in January 2015, CDC also sent an email with a link to a follow-up SurveyMonkey® (SurveyMonkey Inc., Palo Alto, CA) questionnaire to state epidemiologists three days after the email notification of an incident of potential public health significance. The survey captures whether public health action was taken, what the public health action was, whether the state was aware of the incident before the notification, and whether the notification contributed to any action (Appendix 1).
We used the following outcome variables to analyze survey responses from 1 January 2015 to 31 December 2016: number of notifications sent, number of surveys completed, and survey results. We extracted questionnaires from SurveyMonkey® into a Microsoft Access database using Epi Info 7.2 (CDC, Atlanta, GA) and performed descriptive analysis using SAS 9.3 (SAS Institute Inc., Cary, NC). We tracked the number of incidents of potential public health significance, email notifications sent, follow-up questionnaires sent, and follow-up questionnaires completed in a Microsoft Excel (2016) spreadsheet.
Results
Examples of notable public health impact by NPDS surveillance
Three historical examples of notable public health impact using NPDS for surveillance are described below.
2010 Deepwater horizon oil spill federal response
During the 2010 Deepwater Horizon oil spill response, CDC improved situational awareness of response leadership by conducting prospective surveillance with NPDS for incident-related exposures and illness [5,6]. Regional PCs served as a primary health information resource for clinicians and the public about the chemicals released and the ones used in recovery operations during April–September 2010 [7]. Between 30 April and 11 September 2010, NPDS identified 1766 incident-related calls, 1088 of which were identified as calls reporting a potential exposure. The PCs used a unique identifier to flag calls related to the oil spill. Many PCs had to initiate surge capacity protocols to handle the increase in calls resulting from the incident. Calls for information were also tracked to understand the concerns of the public.
CDC collected, analyzed, interpreted, and then disseminated NPDS data to the CDC Emergency Operations Center to enhance situational awareness of response leadership [8]. This information was disseminated via CDC director update briefs, situational reports, and to states for case follow up. Public health departments in the affected area used the data to track the number of exposures and types of concerns from the public [7]. These data were also used to create public health messaging regarding the spill. Information about potential occupational exposures was conveyed to the National Institute for Occupational Safety and Health (NIOSH) for follow-up. NPDS data were shared with the Food and Drug Administration (FDA) to help the agency identify food safety messaging concerns [7].
Laundry detergent pods
Laundry detergent pods are single-load, water-soluble capsules containing concentrated liquid detergent, softener, and other soap types [9]. AAPCC and CDC were notified by two PCs about several adverse health events resulting from ingestion of laundry detergent pod contents [10]. During 17 May to 17 June 2012, PCs reported 485 exposures involving laundry detergent pods to NPDS [10]. Ingestion accounted for 90% of exposures. The most frequently reported signs and symptoms included vomiting, drowsiness, and coughing or choking [10]. The mean age of exposure was 3 years and 96% of exposures occurred in children aged ≤5 years [10]. Children might be attracted by the colorful appearance and size of laundry detergent pods, thinking the pods are candy [9,10]. The evidence collated by NPDS and information disseminated by CDC and AAPCC contributed to the decision of the largest manufacturer of laundry detergent pods in the United States to add a double-latch lid safety feature to laundry detergent pod containers in 2012 [11]. In 2012, Consumer Reports called on manufacturers to make laundry detergent pods safer [12]. Suggestions included adding child-resistant latches to containers, adding labels and warnings, or changing from clear to opaque plastic containers [12]. In 2013, the US Consumer Products and Safety Commission issued a warning about the potential dangers of laundry detergent pods. The commission urged parents to take immediate action to ensure their family would not be exposed [12]. In 2015, based on continued reports of children harmed by exposure to laundry detergent pod contents, Consumer Reports removed laundry detergent pods from their list of recommended laundry detergents [13].
Electronic cigarettes
Electronic cigarettes (e-cigarettes) are battery-powered devices that typically deliver nicotine, flavorings (e.g., fruit, mint, and chocolate), and other chemicals to the user via an inhaled aerosol. During September 2010–February 2014, PCs reported 2405 calls related to e-cigarette exposures to NPDS. Calls involving e-cigarettes steadily increased from 1 call per month in September 2010 to 215 calls per month in February 2014 [14]. E-cigarette exposures were mostly reported as inhalations, eye exposures, and skin exposures. E-cigarette exposures were mostly among persons aged 0-5 years (51.1%) and >20 years (42.0%). The most common signs and symptoms reported were vomiting, nausea, and eye irritation [14]. In January 2016, the Child Nicotine Poisoning Prevention Act of 2015 was enacted with reference to the AAPCC report on liquid nicotine exposures reported to PCs [15]. This law requires any container of liquid nicotine that is sold, manufactured, distributed, or imported into the United States to be placed in packaging that is difficult to open by children aged < 5 years [16]. Additionally, in May 2016, United States FDA issued a rule – often referred to as the “deeming rule” – to extend its authority over all products meeting the definition of a tobacco product, except accessories of the newly deemed products [17]. This rule referenced the concerns about the growing number of calls to PCs due to accidental nicotine poisoning and extended FDA's tobacco product authorities to include e-cigarettes and their components and parts (e.g., nicotine cartridges) [17].
Survey of state epidemiologists
To better understand the public health impact of surveillance using NPDS at the local level, CDC surveyed state epidemiologists after CDC notification of an incident of public health significance. During the study period, CDC identified 136 anomalies of potential public health significance, emailed 126 notifications spanning 36 states, and sent 120 questionnaires (Figure 1). We did not administer multiple questionnaires or send duplicate notifications when NPDS identified anomalies related to the same incident. A total of 59 surveys were completed (49.2%). Among the incidents of potential public health significance discussed by survey respondents, 23 (39.0%) involve food poisoning/water contamination (e.g., ciguatera, botulinum toxin, listeria). Other incidents included 13 (22.0%) involving exposure to gas/vapor/fumes/smoke (e.g., carbon monoxide (CO), chlorine gas) and 10 (16.9%) involving exposure to non-pharmaceutical chemicals (e.g., herbicides, pesticides) (Table 1).
Figure 1.
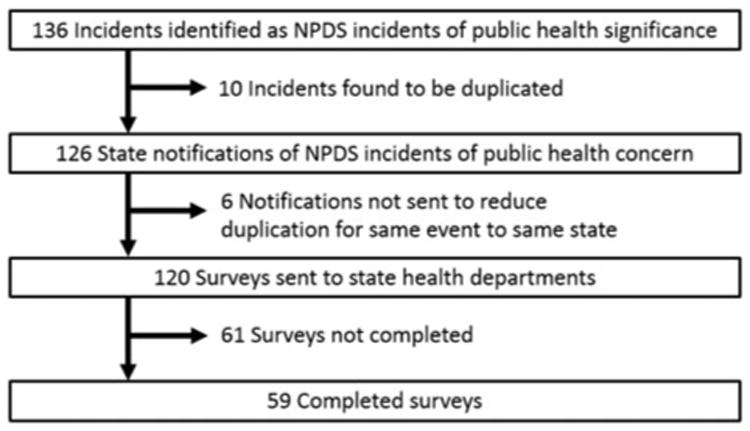
Breakdown of National Poison Data System (NPDS) anomalies identified to number of surveys completed by state epidemiologists, 1 January 2015–31 December 2016.
Table 1.
Types of incidents identified by the National Poison Data System from poison center reports by respondents aware of incident, respondents unaware of incident, all respondents, and non-responders, 1 January 2015–31 December 2016.
| Aware of incident (n = 32) n (%) | Unaware of incident (n = 27) n (%) | All respondents (N = 59) n (%) | Non-respondents (n = 61) n (%) | |
|---|---|---|---|---|
| Types of incidents surveyed | ||||
| Food poisoning/water contamination | 16 (50.0) | 7 (25.9) | 23 (39.0) | 8 (13.1) |
| Gas/vapor/fumes/smokea | 8 (25.0) | 5 (18.5) | 13 (22.0) | 23 (37.7) |
| Non-pharmaceutical chemicals | 2 (6.3) | 8 (29.6) | 10 (16.9) | 9 (14.8) |
| Environmental | 3 (9.4) | 4 (14.8) | 7 (11.9) | 14 (23.0) |
| Drug/product misuse | 2 (6.3) | 2 (7.4) | 4 (6.8) | 5 (8.2) |
| Unknown/other | 1 (3.1) | 1 (3.7) | 2 (3.4) | 2 (3.3) |
More than one substance type can be reported under a single call-volume incident.
Among all respondents, 49 (83.1%) took public health action in response to the incident. The top three types of public health action taken were requests for more information, public health investigation activities, and telephone consultations. While the majority of all respondents (n = 33, 55.9%) stated that public health actions taken in response to the incident would have occurred regardless of CDC notification, 20 (33.9%) respondents stated that CDC notification contributed to initiating public health action and six (10.2%) respondents stated that they did not know. Table 2 breaks down responses by respondents who knew about the incident before notification (n = 32, 54.2%) and respondents who did not know about the incident before notification (n = 27, 45.8%). Notably, 63.0% of respondents who did not know about the incident before notification (n = 17) stated that CDC notification contributed to initiating public health action.
Table 2.
National Poison Data System incident notification follow-up survey responses (1 January 2015–31 December 2016)a.
| All respondents (N = 59) n (%) | Respondents who knew about the incident before notification (n = 32) n (%) | Respondents who did not know about the incident before notification (n = 27) n (%) | |
|---|---|---|---|
| Public health action was taken in response to incident | |||
| Yes | 49 (83.1) | 28 (87.5) | 21 (77.8) |
| No | 9 (15.3) | 4 (12.5) | 5 (18.5) |
| Do not know | 1 (1.7) | 0 (0.0) | 1 (3.7) |
| Types of public health action takenb | |||
| Request more information | 36 (61.0) | 18 (56.3) | 18 (66.7) |
| Public health investigation activity | 27 (45.8) | 18 (56.3) | 9 (33.3) |
| Telephone consultation | 21 (35.6) | 14 (43.8) | 7 (25.9) |
| Coordination between partners | 10 (16.9) | 7 (21.9) | 3 (11.1) |
| Public health communication | 3 (5.1) | 2 (6.3) | 1 (3.7) |
| Do not know | 2 (3.4) | 0 (0.0) | 2 (7.4) |
| Notification contributed to initiate public health action | |||
| No, action would have occurred, regardless of notification | 33 (55.9) | 26 (81.3) | 7 (25.9) |
| Yes | 20 (33.9) | 3 (9.4) | 17 (63.0) |
| Do not know | 6 (10.2) | 3 (9.4) | 3 (11.1) |
Percentages might not add up to 100% because of rounding.
Multiple responses could be selected.
Table 3 illustrates the types of incidents that elicited public health investigation activities and where CDC notification contributed to public health action. Among respondents that conducted public health investigation activities, the majority (n = 16, 59.3%) were attributed to food poisoning/water contamination. Among respondents where CDC notification contributed to public health action, the top three types of incidents included food poisoning/water contamination, exposures involving non-pharmaceutical chemicals, and gas/vapor/fumes/smoke exposures.
Table 3.
Types of incidents identified by the National Poison Data System from poison center reports that elicited public health investigation activity and where CDC notification contributed to public health action, 1 January 2015–31 December 2016.
| Public health investigation activity conducted (n = 27) n (%) | CDC notification contributed to public health action (n = 20) n (%) | |
|---|---|---|
| Types of incidents surveyed | ||
| Food poisoning/water contamination | 16 (59.3) | 6 (30.0) |
| Gas/vapor/fumes/smokea | 4 (14.8) | 4 (20.0) |
| Non-pharmaceutical chemicals | 2 (7.4) | 6 (30.0) |
| Environmental | 4 (14.8) | 1 (5.0) |
| Drug/product misuse | 1 (3.7) | 1 (5.0) |
| Unknown/other | 0 (0.0) | 2 (10.0) |
More than one substance type can be reported under a single call-volume incident.
Discussion
This review demonstrates that PC data and NPDS surveillance can help inform state health departments about incidents that require follow up and public health action. Whether or not the NPDS surveillance system identifies anomalies as incidents of public health significance depends on the caller accurately reporting the exposure and the PC accurately capturing exposure information for novel exposures. Reporting hazardous exposures and illnesses related to chemicals, new consumer products, and regional events is important to optimizing NPDS system functionality. Therefore, reminding emergency medicine doctors and healthcare professionals that PCs are available for toxicological consultations would potentially improve treatment of novel hazards and facilitate public health surveillance in identifying new drugs or toxic hazards from novel consumer products. Increasing the utilization of PCs would increase the likelihood that a multi-state event would be identified and public health action initiated in a timely manner.
Although PCs and health departments collaborate at state and local levels, many state health departments are not aware of the incidents of potential public health significance that may be identified by the NPDS national surveillance system. Many of these incidents of potential public health significance are actionable. CDC notifications based on NPDS data made many state health departments aware of an incident of potential public health significance so that action could be taken. These notifications can be especially helpful for those who had not been aware of the incident. For example, hotel staff were exposed to chemicals from a clandestine drug laboratory in a hotel room. The health department was made aware of this exposure via CDC notification, leading to proper decontamination of the hotel room and proper treatment of hotel staff. Most respondents who did not know about an incident beforehand reported initiating public health action because of the CDC notification. These notifications provided a starting point for increased communication and collaboration between public health partners, including health departments, PCs, and first-line health care providers. Additionally, forums such as the Poison Center and Public Health Collaborations Community of Practice, spearheaded by the Council of State and Territorial Epidemiologists, AAPCC and CDC, also foster collaboration.
Along with initiating action and increasing communication and collaboration, NPDS monitoring has been instrumental in characterizing emerging public health threats and providing evidence for national emerging issues with consumer products. The examples concerning laundry detergent pods and e-cigarettes demonstrate that NPDS data can provide evidence to policymakers who are considering actions such as product warnings, product changes, and regulations to minimize and prevent harm. The resulting gain in public health investigation activities has been a benefit to public health.
NPDS surveillance can also be useful in larger-scale events, such as during public health disasters. This was seen in the use of NPDS during the 2010 Deepwater Horizon incident. NPDS data can be leveraged to supplement traditional surveillance data (i.e., emergency room visits) to understand chemical exposures and poisonings during a disaster. NPDS surveillance was utilized during disaster response and recovery to trackCO exposures in the 2009 Kentucky ice storms, calls related to the 2011 Fukushima Daiichi nuclear disaster, and CO exposures during the 2012 Hurricane Sandy [5]. Timely information from NPDS surveillance during a disaster can be used to create targeted public health messaging and mitigate future disaster-related morbidity and mortality.
This study is subject to limitations. First, there was a low response rate. The responses captured could be different from those who did not respond to the survey. Second, the number of incidents of public health significance may be under-reported because the number of exposures reported to PCs varies across the United States and territories geographically and among ethnic groups [18]. For unknown, emerging, or changing product exposures, it may take time for identification and development of permanent codes, thus NPDS surveillance may be less able to capture these exposures. Whether or not the NPDS surveillance system identifies anomalies as incidents of public health significance depends on the caller accurately reporting the exposure and the PC accurately capturing exposure information based on the level of information available and coding practices.
Conclusions
NPDS serves not only as a data repository for PCs, but also as a surveillance system for exposure information at the local, state, and national levels [2,3,5,19]. The exposure information captured by NPDS is important in tracking potential outbreaks and emerging public health concerns, spanning a wide range of events involving infectious, toxic, and environmental agents [3,20]. Our historical examples demonstrate that NPDS data can be used to increase communication and collaboration between PCs and public health departments during ongoing events, and provide evidence of potentially hazardous exposures to health departments, consumers, physicians, policymakers, and manufacturers. The survey of state epidemiologists receiving CDC notifications demonstrates that NPDS can identify emerging issues that public health departments may be unaware of, allowing them to initiate public health action, such as interviewing case patients, investigating consumer products, and coordinating confirmatory laboratory testing. Using NPDS data can improve public health practice by encouraging communication across sectors, improving the public health response, and ultimately minimizing morbidity and mortality from chemical, radiological, and biological exposures.
Appendix 1
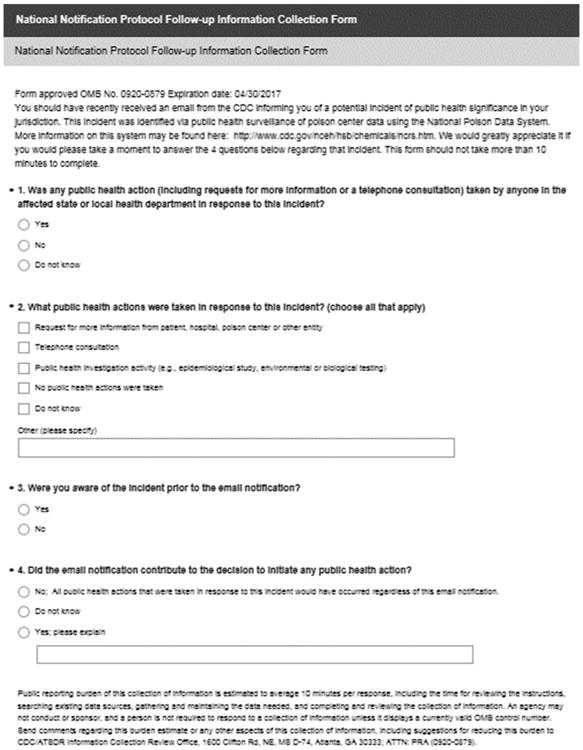
Survey collection form sent to state epidemiologists.
Footnotes
Disclosure statement: No potential conflict of interest was reported by the authors.
References
- 1.Mowry JB, Spyker DA, Brooks DE, et al. 2015 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 33rd Annual Report. Clin Toxicol. 2016;54:924–1109. doi: 10.1080/15563650.2016.1245421. [DOI] [PubMed] [Google Scholar]
- 2.Law R, Sheikh S, Bronstein A, et al. Incidents of potential public health significance identified using national surveillance of US poison center data (2008–2012) Clin Toxicol. 2014;52:958–963. doi: 10.3109/15563650.2014.953171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolkin A, Martin C, Law R, et al. Using poison center data for national public health surveillance for chemical and poison exposure and associated illness. Ann Emerg Med. 2012;59:56–61. doi: 10.1016/j.annemergmed.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 4.US Centers for Disease Control and Prevention; 2016. [cited 2016 Sep 13]. Health Studies Branch – Understanding Chemical Exposures Department of Health and Human Services. Available from: http://www.cdc.gov/nceh/hsb/chemicals/ncrs.htm. [Google Scholar]
- 5.Wolkin A, Schnall A, Law R, et al. Using poison center data for postdisaster surveillance. Prehosp Disaster Med. 2014;29:521–524. doi: 10.1017/S1049023X14000983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services; 2010. Evaluating the Health Impacts of the Gulf of Mexico Oil Spill. Available from: http://www.hhs.gov/asl/testify/2010/06/t20100615g.html. [Google Scholar]
- 7.The Weather Channel; 2012. [cited 2016 Oct 19]. CDC Response to the Gulf of Mexico Oil Spill. Available from: https://weather.com/health/airquality/news/cdc-response-gulf-oil-spill-20120328. [Google Scholar]
- 8.Centers for Disease Control and Prevention; 2010. Public Health Surveillance 2010 Deepwater Horizon Response. Available from: https://www.niehs.nih.gov/about/assets/docs/deitchman_deep-water_horizon_response_508.pdf. [Google Scholar]
- 9.Bonney AG, Mazor S, Goldman RD. Laundry detergent capsules and pediatric poisoning. Can Fam Phys. 2013;59:1295–1296. [PMC free article] [PubMed] [Google Scholar]
- 10.Beuhler M, Henretig FM, Gala P. Health hazards associated with laundry detergent pods – United States, May–June 2012. Morbid Mortal Week Rep. 2012;61:825–829. [PubMed] [Google Scholar]
- 11.Update 2-Tide to change pods lid over child safety concerns. [cited 2017 Mar 1];2012 May 25; Available from: http://www.reuters.com/article/2012/05/25/procter-tide-idusl1e8gp9pi20120525.
- 12.Laundry detergent pods remain a health hazard. [cited 2017 Jul 14];2013 Available from: http://www.consumerreports.org/cro/2013/03/laundry-detergent-pods-remain-a-health-hazard/index.htm.
- 13.The problem with laundry detergent pods. [cited 2017 Jul 14];2015 Available from: http://www.consumerreports.org/cro/magazine/2015/07/the-problem-with-laundry-detergent-pods/index.htm.
- 14.Chatham-Stephens K, Law R, Taylor E, et al. Notes from the field: calls to poison centers for exposures to electronic cigarettes – United States, September 2010–February 2014. Morbid Mortal Week Rep. 2014;63:292–293. [PMC free article] [PubMed] [Google Scholar]
- 15.Vol. 2015. US Government Publishing Office; 2017. S. Rept. 114-12 – CHILD NICOTINE POISONING PREVENTION ACT OF 2015. Available from: https://www.congress.gov/congressional-report/114th-con-gress/senate-report/12/1. [Google Scholar]
- 16.Child Nicotine Poisoning Prevention Act of 2015. Department of Health and Human Services; 2015. [Google Scholar]
- Department of Health and Human Services FaDA, editor. 21 CFR Parts 1100, 1140, 1143. Federal Register: National Archives and Records Administration; 2016. [Google Scholar]
- 18.Litovitz T, Benson BE, Youniss J, et al. Determinants of U.S. poison center utilization. Clin Toxicol. 2010;48:449–457. doi: 10.3109/15563651003757947. [DOI] [PubMed] [Google Scholar]
- 19.Wolkin AF, Patel M, Watson W, et al. Early detection of illness associated with poisonings of public health significance. Ann Emerg Med. 2006;47:176–470. doi: 10.1016/j.annemergmed.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 20.Dart RC. The secret life of America's Poison Centers. Ann Emerg Med. 2012;59:62–66. doi: 10.1016/j.annemergmed.2011.11.017. [DOI] [PubMed] [Google Scholar]


