Abstract
Background and Purpose
Rates of cerebral venous thrombosis (CVT) misdiagnosis in the Emergency Department (ED) and outcomes associated with misdiagnosis have been underexplored.
Methods
Using administrative data, we identified adults with CVT at New York, California, and Florida hospitals in 2005–2013. Our primary outcome was probable misdiagnosis of CVT, defined as a treat-and-release ED visit for headache or seizure within 14 days prior to CVT. In addition, logistic regression was used to compare rates of clinical outcomes in patients with and without probable CVT misdiagnosis. We performed a confirmatory study at two tertiary-care centers.
Results
We identified 5,966 CVT patients in whom 216 (3.6%; 95% CI, 1.1–4.1%) had a probable misdiagnosis of CVT. After adjusting for demographics, risk factors for CVT, and the Elixhauser comorbidity index, probable CVT misdiagnosis was not associated with in-hospital mortality (OR, 0.14; 95% CI, 0.02–1.05), intracerebral hemorrhage (OR, 0.97; 95% CI, 0.57–1.65), or unfavorable discharge disposition (OR, 0.90; 95% CI: 0.61–1.32); a longer length of hospital stay was seen among misdiagnosed CVT patients (OR, 1.62; 95% CI, 1.04–2.50). In our confirmatory cohort, probable CVT misdiagnosis occurred in 8 of 134 CVT patients (6.0%; 95% CI, 2.6–11.4%).
Conclusions
In a large, heterogeneous multi-state cohort, probable misdiagnosis of CVT occurred in 1 out of 30 patients but was not associated with the adverse clinical outcomes included in our study.
Keywords: cerebral venous thrombosis, diagnosis, emergency medicine, diagnostic error
Subject terms: Thrombosis, Quality and Outcomes
INTRODUCTION
Cerebral venous thrombosis (CVT) is a cerebrovascular disease that often affects young and middle aged patients resulting in substantial disability and death.1, 2 CVT patients present with nonspecific neurological complaints including headache and seizure.3, 4 The annual incidence of CVT may be as high as 15.7 cases per million persons,2 but many physicians encounter CVT infrequently. As a consequence, diagnosing CVT in the emergency setting can be challenging.5 We therefore sought to determine the rate of CVT misdiagnosis and explore whether misdiagnosis of CVT is associated with adverse clinical outcomes in a large heterogeneous cohort.
METHODS
The data and analytic methods of this study are available upon request from the corresponding author.
Design
We performed a retrospective cohort study of CVT patients using publically available data collected by the Agency for Healthcare Research and Quality, extracted from claims from New York, California, and Florida (Supplementary Methods). The institutional review board at Weill Cornell Medicine (WCM) approved this component of the study.
Patients
We included adults with a hospital admission with a first-recorded discharge diagnosis of CVT. CVT was defined using previously validated International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes (Supplementary Methods).
Measurements
The primary study outcome was probable misdiagnosis of CVT (Supplementary Methods), defined as an ED visit for headache or seizure in the 14 days prior to CVT hospitalization that did not result in an admission or transfer to another hospital (i.e., ED treat-and-release visit). The time frame of 14 days was chosen to ensure the ED visit was plausibly related to the subsequent hospitalization for CVT. ED visits for headache or seizure were used as these are common symptoms of CVT.4
To explore temporal trends of CVT hospitalization following ED discharge, we identified ED visits for back pain within 14 days prior to CVT hospitalization. Back pain is not a known early symptom of CVT and thus served as a negative control comparator.
We identified the following risk-factors for CVT at index hospitalization: traumatic brain injury, primary hypercoagulable state, polycethermia vera, any cancer, pregnancy and the puerperium, and CNS infections (Supplementary Methods).6 We used the Elixhauser comorbidity index to account for disease severity.7
To assess whether probable misdiagnosis of CVT was associated with adverse clinical outcomes, we evaluated rates of intracerebral hemorrhage (ICH), in-hospital death, and unfavorable discharge disposition. We defined unfavorable discharge disposition as discharge to a skilled nursing facility, subacute care center, chronic rehabilitation center, or hospice as opposed to discharge to home. Finally, in an exploratory analysis, we evaluated whether history of a primary headache disorder was associated with probable CVT misdiagnosis (Supplementary Methods).
Confirmatory Cohort Analysis
We performed a confirmatory cohort analysis via chart review of adult CVT patients hospitalized at WCM and Montefiore Medical Center (MMC) after obtaining approval from both institutional review boards. We included all available cases of CVT at WCM from 1/1/2007–1/1/2015 and at MMC from 9/1/2005–9/1/2015. Probable CVT misdiagnosis was defined as in our claims analysis. Modified Rankin Scale (mRS) at hospital discharge was abstracted for all patients; mRS >1 was defined as unfavorable.
Statistical Analysis
Descriptive statistics with exact CIs were used to calculate crude rates of probable CVT misdiagnosis. Comparisons between groups were performed using the t test for continuous variables and χ2 test for categorical variables. Variance weighted least squares regression was used to compare patterns of headache or seizure versus back pain ED treat-and-release visits. Multivariable logistic regression was used to evaluate whether probable CVT misdiagnosis was associated with ICH, death, increased length of stay, and unfavorable discharge disposition. Statistical significance was set at α=0.05.
RESULTS
We identified 5,966 patients with CVT, among whom the mean age was 44.2±18.4 years; 4,276 (71.7%) were female. A total of 216 (3.6%; 95% CI, 1.1–4.1%) cases had an ED treat-and-release visit 14 days prior to CVT hospitalization for headache or seizure (i.e., probable CVT misdiagnosis). Patients with a probable CVT misdiagnosis were younger (38.5 vs. 44.4 years) and more likely have a primary hypercoagulable state (Supplementary Table 1). Thirteen patients (0.2%; 95% CI, 0.1–0.4%) had an ED treat-and-release visit for back pain within 14 days prior to CVT hospitalization.
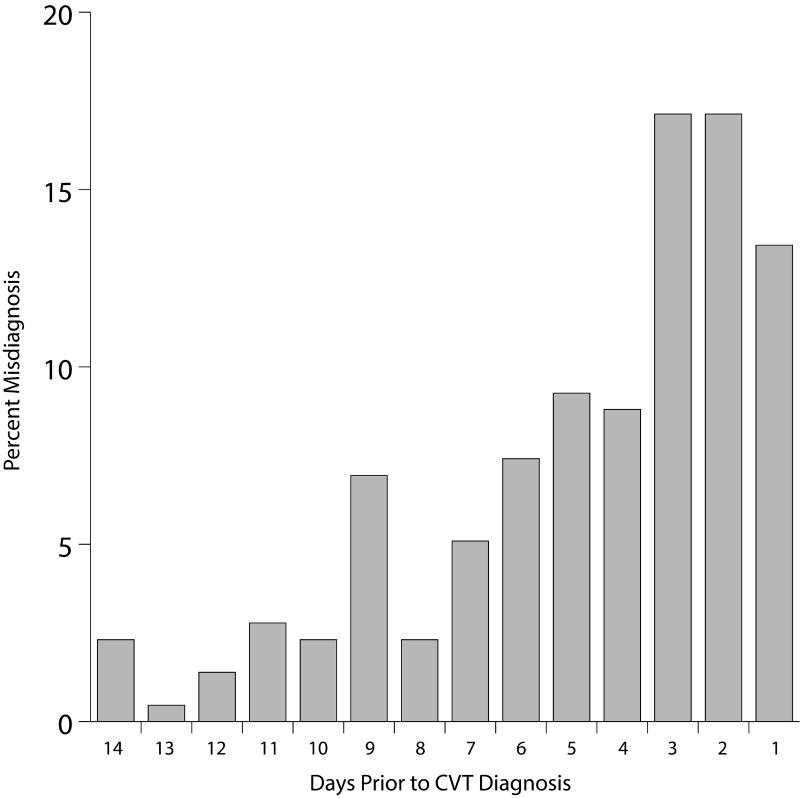
Among misdiagnosed CVT patients, headache was more common (96.8%) than seizure (3.2%, p<0.001). Rates of ED visits where headache or seizure were diagnosed steadily increased from 14 days before CVT to 1 day before CVT hospitalization (0.08% versus 0.49%, p=0.02; Figure 1). Rates of ED visits for back pain were unchanged from 14 days prior to CVT to 1 day before CVT hospitalization (0.01% versus 0.05%, p=0.2) (Figure). History of primary headache disorder was not associated with probable CVT misdiagnosis (19.0% misdiagnosed versus 14.9% non-misdiagnosed, p=0.1).
Figure 1.
Time from Emergency Department discharge diagnosis of seizure or headache to Cerebral Vein Thrombosis Hospitalization
When we adjusted for demographics, risk factors, and the Elixhauser comorbidity index, a probable misdiagnosis of CVT was neither associated with ICH (OR, 0.97; 95% CI, 0.57–1.65), in-hospital mortality (OR, 0.14; 95% CI, 0.02–1.05), or unfavorable discharge outcome (OR, 0.90; 95% CI: 0.61–1.32). A longer length of hospital stay was seen in misdiagnosed patients (OR, 1.62; 95% CI, 1.04–2.50) (Supplementary Table 2).
We identified a total of 134 CVT patients in the confirmatory cohort. Within the 14 days prior to CVT hospitalization, a total of 8 patients (6.0%; 95% CI, 2.6–11.4%) had an ED treat-and-release visit for headache; no patients had a visit for seizure. Probable misdiagnosis of CVT was not associated with an unfavorable discharge mRS (3/8 [37.5%] misdiagnosed vs. 51/126 [40.5%] non-misdiagnosed, p=0.9).
DISCUSSION
In a large, heterogeneous cohort, we found that approximately 1 in 30 patients with CVT were initially misdiagnosed. We did not find an association between probable misdiagnosis and any studied adverse outcomes aside from increased length of stay. In our smaller confirmatory cohort, approximately 1 in 18 patients were misdiagnosed and these patients had similar outcomes compared to patients without a CVT misdiagnosis.
Similar rates of CVT misdiagnosis in our study and confirmatory cohorts support our measurement technique. However, we acknowledge that we may have underestimated the rate of CVT misdiagnosis as we did not capture patients who did not return for medical evaluation after an ED visit, those who were not diagnosed with CVT when they did return, or those who died before an accurate diagnosis could be made. Alternatively, we may have overestimated rates of CVT misdiagnosis as some ED treat-and-release visits for seizure or headache may have been unrelated to subsequent CVT. However, this latter possibility seems less likely given the temporal relationship we found between ED treat-and-release visits for seizure or headache and subsequent CVT hospitalization.
Our finding of no differences in major clinical outcomes between patients with a CVT misdiagnosis versus those without a misdiagnosis is largely consistent with prior work. In the International Study on Cerebral Vein and Dural Sinus Thrombosis there were no significant differences in the delayed versus non-delayed diagnosis groups except among the CVT patients with isolated increased intracranial hypertension.8, 9 Given the increasingly recognized impact of CVT on long-term cognition and employment status,10 more granular outcome data than that used in our study, including visual field, visual acuity, and cognitive measurements, is needed to further quantify the clinical effects of misdiagnosis.
This study has several limitations. First, data on presenting headache semiology and physical examination findings are lacking. Additionally, since we relied exclusively on ED visits for seizure or headache to define probable CVT misdiagnosis, we failed to account for ED visits where misdiagnosis may have occurred due to alternative early manifestations of CVT such as isolated visual complaints. Second, misdiagnosis of CVT was limited to patients who were seen in the ED and not hospitalized. Third, we were unable to adjust for important CVT risk factors, such as use of hormonal therapy, which are unavailable in administrative claims data. Fourth, our outcomes were limited to in-hospital measurements and thus we were unable to evaluate long-term functional status. Finally, we lack hospital level (e.g. academic or community), provider level (e.g. ED physician practice experience), and detailed encounter level (e.g., was neurological consultation obtained, what imaging studies were performed) data as well as information about the extent of in-patient diagnostic evaluations in this study.
In summary, we identified CVT misdiagnosis in a small but non-trivial percentage of CVT patients using a large, heterogeneous multi-state cohort.
Supplementary Material
Acknowledgments
The authors are grateful to Monica Chen for copy editing.
SOURCES OF FUNDING:
HK is supported by NIH grants K23NS082367, R01NS097443, and U01NS095869 and the Michael Goldberg Research Fund. AEM is supported by NIH grant KL2TR0002385 and the Leon Levy Foundation in Neuroscience.
Footnotes
DISCLOSURES:
None
References
- 1.Dentali F, Gianni M, Crowther MA, Ageno W. Natural history of cerebral vein thrombosis: A systematic review. Blood. 2006;108:1129–1134. doi: 10.1182/blood-2005-12-4795. [DOI] [PubMed] [Google Scholar]
- 2.Devasagayam S, Wyatt B, Leyden J, Kleinig T. Cerebral venous sinus thrombosis incidence is higher than previously thought: A retrospective population-based study. Stroke. 2016;47:2180–2182. doi: 10.1161/STROKEAHA.116.013617. [DOI] [PubMed] [Google Scholar]
- 3.Tanislav C, Siekmann R, Sieweke N, Allendorfer J, Pabst W, Kaps M, et al. Cerebral vein thrombosis: Clinical manifestation and diagnosis. BMC Neurol. 2011;11:69. doi: 10.1186/1471-2377-11-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferro JM, Canhao P, Stam J, Bousser MG, Barinagarrementeria F Investigators I. Prognosis of cerebral vein and dural sinus thrombosis: Results of the international study on cerebral vein and dural sinus thrombosis (ISCVT) Stroke. 2004;35:664–670. doi: 10.1161/01.STR.0000117571.76197.26. [DOI] [PubMed] [Google Scholar]
- 5.Fischer C, Goldstein J, Edlow J. Cerebral venous sinus thrombosis in the emergency department: Retrospective analysis of 17 cases and review of the literature. J Emerg Med. 2010;38:140–147. doi: 10.1016/j.jemermed.2009.08.061. [DOI] [PubMed] [Google Scholar]
- 6.Silvis SM, Middeldorp S, Zuurbier SM, Cannegieter SC, Coutinho JM. Risk factors for cerebral venous thrombosis. Semin Thromb Hemost. 2016;42:622–631. doi: 10.1055/s-0036-1584132. [DOI] [PubMed] [Google Scholar]
- 7.Elixhauser A, Steiner C, Harris DR, Coffey RN. Comorbidity measures for use with administrative data. Med. Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Ferro JM, Canhao P, Stam J, Bousser MG, Barinagarrementeria F, Massaro A, et al. Delay in the diagnosis of cerebral vein and dural sinus thrombosis: Influence on outcome. Stroke. 2009;40:3133–3138. doi: 10.1161/STROKEAHA.109.553891. [DOI] [PubMed] [Google Scholar]
- 9.Gameiro J, Ferro JM, Canhao P, Stam J, Barinagarrementeria F, Lindgren A, et al. Prognosis of cerebral vein thrombosis presenting as isolated headache: Early vs. Late diagnosis. Cephalalgia. 2012;32:407–412. doi: 10.1177/0333102412439353. [DOI] [PubMed] [Google Scholar]
- 10.Hiltunen S, Putaala J, Haapaniemi E, Tatlisumak T. Long-term outcome after cerebral venous thrombosis: Analysis of functional and vocational outcome, residual symptoms, and adverse events in 161 patients. J. Neurol. 2016;263:477–484. doi: 10.1007/s00415-015-7996-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.