Abstract
Food shopping decisions are pathways between food environment, diet and health outcomes, including chronic diseases such as diabetes and obesity. The choices of where to shop and what to buy are interrelated, though a better understanding of this dynamic is needed. The U.S. Department of Agriculture’s nationally representative Food Acquisitions and Purchase Survey food-at-home dataset was joined with other databases of retailer characteristics and Healthy Eating Index-2010 (HEI) of purchases. We used linear regression models with general estimating equations to assess relationships between trip, store, and shopper characteristics with trip HEI scores. We examined HEI component scores for conventional supermarkets and discount/limited assortment retailers with descriptive statistics. Overall, 4,962 shoppers made 11,472 shopping trips over one-week periods, 2012-2013. Trips to conventional supermarkets were the most common (54.4%), followed by supercenters (19.3%). Compared to conventional supermarkets, purchases at natural/gourmet stores had significantly higher HEI scores (β=6.48, CI=[4.45, 8.51], while those from “other” retailers (including corner and convenience stores) were significantly lower (−3.89, [−5.87, −1.92]). Older participants (versus younger) and women (versus men) made significantly healthier purchases (1.19, [0.29, 2.10]). Shoppers with less than some college education made significantly less-healthy purchases, versus shoppers with more education, as did households participating in SNAP, versus those with incomes above 185% of the Federal Poverty Level. Individual, trip, and store characteristics influenced the healthfulness of foods purchased. Interventions to encourage healthy purchasing should reflect these dynamics in terms of how, where, and for whom they are implemented.
Keywords: diet, nutrition, food access, food environment, food shopping, store choice, food choice, SNAP, FoodAPS
INTRODUCTION
Food shopping decisions present a means of assessing possible pathways between food environment, diet and health outcomes, including highly prevalent chronic diseases such as diabetes and obesity (Drewnowski et al., 2016b). In obtaining foods to be eaten at home, individuals make a series of decisions; chief among these are 1) where to shop (store choice) and 2) what to buy (food choice). Previous mixed-methods studies have developed a better understanding of food shopping behavior among low-income urban residents and how they navigate community and consumer food environments (Glanz et al., 2005). Numerous studies at both local and national scales have found that most shoppers travel beyond their closest supermarket to do most of their food shopping (Hillier et al., 2011; Ver Ploeg et al., 2015), and that multiple stores are often used over the course of a month (Chrisinger et al., in review; DiSantis et al., 2016; Zenk et al., 2014).
Previous research also shows that while distance is an important part of choosing among possible food retailers, other factors are also significant for many households. For instance, food store choice was found to vary with individual and household characteristics, such as income, vehicle ownership, race/ethnicity, and gender, and activity space of food shoppers (Hillier et al., 2015, 2017). Store characteristics, such as proximity to transit, prices, size, and availability of healthful foods also appear to influence store choice, (Hillier et al., 2011; Jilcott et al., 2011; Kerr et al., 2012), and households appear to form different expectations and transportation needs for different types of food shopping trips (e.g., big trips versus small trips) (Cannuscio et al., 2014; Chrisinger, 2016; Hirsch and Hillier, 2013). Other studies have explored the influence of these factors among participants in the primary U.S. federal food assistance programs: the cash-like Supplemental Nutrition Assistance Program (SNAP, formerly known as the Food Stamp Program) in which over one in six households participated in 2017, and the item-specific, voucher-based Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) that reaches over seven million pregnant and postpartum women, their infants and young children (Gustafson, 2017; Hillier et al., 2017; Jilcott et al., 2011; Rose and Richards, 2004; U.S. Department of Agriculture, Food and Nutrition Service, Office of Policy Support, 2017; USDA Food and Nutrition Service, n.d.). Among studies of lower-income populations, the type of food store (e.g., full-service supermarket, limited assortment, convenience store) also appears to predict the healthfulness of foods purchased (Chrisinger et al., in review; Gustafson et al., 2013; Gustafson, 2017; Gustafson et al., 2012; Jilcott et al., 2011), perhaps, attributable to disparities in the consumer, or in-store, food environment, between types of retailers (Laska et al., 2010, 2015).
With the nationally representative National Household Food Acquisition and Purchase Survey (FoodAPS) dataset, we can broadly test nutritional differences between types of food retailers, and assess relationships between these differences and individual socioeconomic (SES) characteristics. Our analysis extends beyond lower-income populations, thus allowing us to compare how households that are eligible for food assistance programs shop compared to households with higher incomes. Our primary hypothesis was that purchases made at conventional supermarkets would be the healthiest compared to other retailer types, even after adjusting for individual, trip, and store-level characteristics thought to influence the items purchased. We also sought to explore possible variations in the healthfulness of purchases by participation in SNAP or WIC, and by use of these assistance programs during specific transactions.
METHODS
Dataset
Data collection for FoodAPS included 4,826 households across the United States in 2012 and 2013, and was specifically designed to enable nationally representative assessments. Respondents for each FoodAPS household reported all food acquisitions made over a one-week period, including food-at-home (FAH) and food-away-from-home (FAFH), using a variety of methods and instruments, described fully in USDA reports (USDA Economic Research Service, 2016). Information for each food shopping trip was extracted from participant data, including the number and type of foods purchased, amount spent, and the type and location of store. For our primary outcome variable, nutrient coding was applied to the primary FoodAPS dataset according to the Healthy Eating Index-2010 (HEI-2010), which is a density-based diet quality score (maximum score=100) designed to reflect adherence to the Dietary Guidelines for Americans (Guenther et al., 2013). The HEI-2010 is comprised of 12 component categories that account for both healthy and unhealthy foods: whole fruit, total fruit, whole grains, dairy, total protein foods, seafood and plant proteins, greens and beans, total vegetables, fatty acids, refined grains, sodium and empty calories (Guenther et al., 2013). We only included FAH transactions in this analysis.
We transformed and/or recoded several FoodAPS variables related to trip, store, and primary shopper characteristics for ease of interpretability. Our study variables included trip characteristics: date of purchase (week versus weekend), week of the month (first, second, third, fourth/fifth), total purchase amount (which may have included non-food items, recoded as a categorical variable: <$10.00, $10.00-$24.99, $25.00-$49.99, and $50.00+), payment type (SNAP, WIC, debit card, credit card, cash or check, or other), and distance from shopper’s home (defined in FoodAPS as Google Maps calculated driving distance in miles). We derived store type classifications from a linked Nielsen TDLinx dataset, which included conventional supermarkets, supercenters (e.g., SuperTarget, Walmart Supercenter), discount/limited assortment retailers (e.g., Aldi, Trader Joe’s, Sav-A-Lot), conventional clubs (warehouse-type stores that charge a membership fee, such as Costco and Sam’s Club), natural/gourmet stores, dollar stores (e.g., Dollar General, Dollar Tree, Family Dollar), and “other” retailers (including corner and convenience stores) (Rhone et al., 2017, p. 2). Primary shopper information in our analysis included gender, age (recoded as a categorical variable: 18-29, 30-39, 40-49, 50-59, 60+), SNAP status (based upon self-reported and USDA-estimated eligibility: SNAP-eligible non-participant, SNAP-ineligible with income 100-185% of the Federal Poverty Level (FPL), SNAP-ineligible with income 185%+ FPL, and SNAP participant) educational attainment, race/ethnicity, vehicle access (own/lease vehicle or not), and residence location.
Statistical Analyses
We generated descriptive statistics for all primary shopper and shopping trip variables (composite and component HEI scores for each trip, total number of items purchased, and amount spent), as well as the trip characteristics by store type. Linear regression models using general estimating equations were generated to assess the relationship between trip, store, and shopper characteristics with each trip’s composite HEI score. Here, household ID was treated as a repeated measure to account for varying numbers of trips between households. Based on our findings regarding discount/limited assortment retailers and conventional supermarkets, we also generated descriptive characteristics to compare the HEI composite and component scores between retailers and categories of household SNAP participation. Sampling weights were used for all statistical analyses.
RESULTS
Participant Characteristics
More than half of the participant sample was female (67.8%), non-Hispanic white (60.6%), was over the age of 40 (59.8%), had at least some college education (53.7%), and owned or leased a vehicle (86.2%). Approximately 45.0% of participants were not eligible for SNAP (6.8% with incomes 100-185% FPL, 38.2% with incomes above 185% FPL), while 32.5% were SNAP participants, and 22.5% were SNAP-eligible but not participating. See Table 1 for a summary of all participant characteristics and their weighted prevalence across the dataset.
Table 1.
Descriptive characteristics of participants, food expenditures and shopping trips included in the FoodAPS food-at-home dataset, 2012-2013.
| Individual Characteristics (unweighted n=4,962 having at least one trip) | Unweighted n (weighted %) |
|---|---|
| Age groups (years) | |
| 18–29 | 1,003 (14.2) |
| 30–39 | 990 (17.2) |
| 40–49 | 952 (18.5) |
| 50–59 | 940 (20.2) |
| 60+ | 1,077 (29.9) |
| Gender (Female) | 3,364 (63.7) |
| Race/ethnicity | |
| White (non-Hispanic) | 3,006 (70.0) |
| Black/Af Am (non-Hispanic) | 624 (10.2) |
| Hispanic (any) | 1,013 (13.7) |
| Other (non-Hispanic) | 319 (6.0) |
| SNAP/Income Status | |
| SNAP participant | 1,614 (13.1) |
| SNAP eligible, non-participant | 1,115 (19.3) |
| Non-SNAP eligible, 100–185% FPL | 339 (4.7) |
| Non-SNAP eligible, 185+% FPL | 1,894 (62.9) |
| Education | |
| <HS | 808 (8.9) |
| HS/GED | 1,476 (24.9) |
| Some college or more | 2,666 (66.1) |
| Missing | 12 (0.1) |
| Own/lease cara | 4,275 (90.7)b |
| Food Expenditures and Trip Characteristics (n=11,472) | n (%) |
| Weekend | 3,308 (30.0) |
| Week of month | |
| First (days 1–7) | 2,413 (21.8) |
| Second (days 8–14) | 2,827 (23.4) |
| Third (days 15–21) | 3,010 (24.8) |
| Fourth + Fifth (days 22–31) | 3,222 (29.9) |
| Amount spent ($) | |
| Median [IQR] | 22.74 [9.43–48.46] |
| < $10.00 | 3,380 (26.7) |
| $10.00 – $24.99 | 3,235 (26.3) |
| $25.00 – $49.99 | 2,370 (23.0) |
| $50.00+ | 2,487 (24.1) |
| Distance traveled from home (miles) Median [IQR] | 2.85 [1.36–6.82]c |
| Payment typed | |
| SNAP (any) | 1,791 (6.2) |
| WIC | 226 (0.8) |
| Cash or check | 4,730 (40.9) |
| Debit card | 3,000 (30.0) |
| Credit card | 1,534 (20.4) |
| Other (TANF or gift card) | 41 (0.2) |
| Missing | 145 (1.4) |
Reported at household level, but presented as individual level
Missing = 9
Missing = 552
Multiple payment types are possible
Abbreviations used: SNAP (Supplemental Nutrition Assistance Program), FPL (Federal Poverty Level), HS (high school degree), GED (General Equivalency Diploma), IQR (inter-quartile range), WIC (Special Supplemental Nutrition Program for Women, Infants and Children), TANF (Temporary Assistance for Needy Families Program).
Shopping Trip Characteristics
In total, 4,962 primary shoppers made a total of 11,472 FAH shopping trips (only trips with non-missing data were included, n=10,789). Shopping trips were made proportionately during weekdays compared to weekend days (71.2% on the five weekdays versus 28.8% of trips on the two weekend days, respectively). Participants spent a median of $19.79 per shopping trip, with 57.7% of trips involving expenditures of less than $25. Cash or check (41.2%) and debit (26.2%) were the most common form of payment, followed by SNAP (15.6%) and credit card (13.4%). Trips to conventional supermarkets were the most common (54.4% of all trips), followed by supercenters (19.3%) and “other” retailers (10.9%). Excepting dollar stores and retailers classified as “other,” all remaining retailers had mean purchase amounts over $30.00; notably, the mean conventional club transaction was approximately $100.00. Mean composite HEI scores ranged from 43.43 at dollar stores to 56.09 at natural/gourmet retailers. Other variations in trip characteristics between retailer types are described in Table 2.
Table 2.
Distribution of 11,472 food shopping trips made by 4,962 shoppers in the FoodAPS food-at-home dataset (2012-2013), grouped by HEI-2010 score
| Amount spent | Overall HEI score (max=100) | HEI Total fruits (max=5) |
HEI Total vegetables (max=5)a |
HEI greens and beans (max=5) |
HEI whole grains (max=10) |
||
|---|---|---|---|---|---|---|---|
| Store Type | # trips (%) | Mean ± standard error Median [IQR] | |||||
| Conventional supermarket | 6,238 (53.6) |
35.29±0.86 22.38 [9.88–45.01] |
48.12±0.35 48.19 [37.99–58.10] |
0.45±0.03 0 [0–0] |
2.27±0.04 1.80 [0–4.99] |
1.11±0.05 0 [0–0.34] |
1.75±0.09 0 [0–1.00] |
| Supercenter | 2,217 (18.5) |
49.80±2.68 33.20 [14.46–68.51] |
48.26±0.59 48.18 [38.68–57.48] |
0.41±0.03 0 [0–0] |
2.04±0.07 1.45 [0–4.63] |
1.02±0.07 0 [0–0.49] |
2.36±0.16 0 [0–4.17] |
| Discount/limited assortment | 569 (4.8) |
28.91±2.34 19.99 [9.94–34.86] |
47.13±0.99 46.91 [35.67–58.18] |
0.58±0.13 0 [0–0] |
2.75±0.11 3.14 [0–5] |
0.94±0.08 0 [0–0] |
1.18±0.09 0 [0–0] |
| Conventional club | 361 (4.1) |
109.51±9.21 76.07 [40.52–148.59] |
54.68±1.40 54.99 [42.76–67.23] |
0.49±0.08 0 [0–0] |
2.27±0.16 1.89 [0–4.91] |
1.29±0.21 0 [0–3.03] |
2.05±0.29 0 [0–2.58] |
| Natural/gourmet | 270 (4.1) |
40.48±2.42 30.68 [16.67–52.77] |
56.09±0.81 57.40 [47.27–65.98] |
0.67±0.18 0 [0–0] |
2.93±0.18 3.78 [0.07–4.99] |
1.79±0.13 0 [0–4.78] |
2.36±0.32 0 [0–5.11] |
| Dollar store | 570 (3.5) |
13.30±1.19 7.55 [3.55–19.16] |
43.43±0.74 43.63 [35.33–52.97] |
0.23±0.05 0 [0–0] |
1.25±0.09 0 [0–2.35] |
0.36±0.09 0 [0–0] |
1.51±0.18 0 [0–0] |
| Other | 1,247 (11.3) |
20.67±1.89 9.96 [4.24–24.63] |
43.91±0.64 44.88 [31.63–54.94] |
0.37±0.06 0 [0–0] |
1.52±0.09 0 [0–4.48] |
0.64±0.09 0 [0–0] |
0.97±0.13 0 [0–0] |
Includes vegetable-designated legumes
Abbreviations used: HEI (Healthy Eating Index), IQR (inter-quartile range)
Correlations with Composite HEI Scores for Individual Shopping Trips
Table 3 presents the results of the multivariate GEE model adjusting for all of the covariates included in the table. Compared to the HEI scores of purchases made at conventional supermarkets, those from purchases at natural gourmet stores were significantly higher (β=6.43, 95% CI=[4.46, 8.39]), while those from “other” retailers were significantly lower (β=−4.63, 95% CI=[−6.57, −2.70]). Older participants also made healthier purchases than younger participants (β=1.98, CI=[0.57,3.39]), as did women compared to men (β=1.19, CI=[0.29, 2.10]). Compared to non-Hispanic whites, Hispanic participants made significantly healthier purchases (β=2.24, CI=[1.18, 3.31]), as did non-Hispanic, non-Black/African American participants (β=2.59, CI=[0.64, 4.54]). In terms of education, participants with less than some college education made purchases with significantly lower HEI scores than those with more education, as did SNAP participants compared to households with income over 185% of the FPL.
Table 3.
Results of Weighted and Adjusted Multivariate Generalized Estimating Equation Modelsa assessing predictors of HEI-2010 scores among all food-at-home purchases in the FoodAPS dataset (2012–2013), displayed as effect (95% CI).
| Composite HEI | |
|---|---|
|
| |
| Store Type (ref: Conventional Supermarket) | |
| Supercenter | −0.54 (−1.93, 0.85) |
| Discount/limited assortment | 0.90 (−0.78, 2.57) |
| Conventional club | 2.18 (−0.63, 5.00) |
| Natural/gourmet | 6.48 (4.45, 8.51) |
| Dollar store | −1.37 (3.25, 0.50) |
| Other | −3.89 (−5.87, −1.92) |
|
| |
| Age groups (years) (ref: 18–29) | |
| 30–39 | −0.07 (−1.42, 1.28) |
| 40–49 | −0.76 (−1.99, 0.48) |
| 50–59 | 1.27 (−0.41, 2.96) |
| 60+ | 1.98 (0.57, 3.39) |
|
| |
| Sex (Female) | 1.19 (0.29, 2.10) |
|
| |
| Race/ethnicity (ref: White [non-Hispanic]) | |
| Black/Af Am (non-Hispanic) | 0.16 (−1.04, 1.37) |
| Hispanic (any) | 2.24 (1.18, 3.31) |
| Other (non-Hispanic) | 2.59 (0.64, 4.54) |
|
| |
| SNAP/Income Status (ref: Non-SNAP eligible, 185+% FPL) | |
| SNAP household | −1.96 (−2.76, −1.15) |
| SNAP eligible (non-household) | −0.92 (−1.64, −0.20) |
| Non-SNAP eligibile, 100–185% FPL | −0.76 (−2.18, 0.66) |
|
| |
| Education (ref: Some college +) | |
| <HS | −0.54 (−1.88, 0.80) |
| HS/GED | −1.49 (−2.34, −0.64) |
|
| |
| Own/lease car | 0.07 (−1.55, 1.68) |
|
| |
| Weekend | −0.37 (−1.30, 0.56) |
|
| |
| Week of month (ref: first [days 1–7]) | |
| Second (days 8–14) | −0.04 (−1.45, 1.38) |
| Third (days 15–21) | −0.84 (−1.67, −0.01) |
| Fourth + fifth (days 22–31) | −1.12 (−2.18, −0.06) |
|
| |
| Amount spent (ref: $50.00+) | |
| < $10.00 | −10.38 (−11.49, −9.28) |
| $10.00–$24.99 | −7.67 (−8.72, −6.61) |
| $25.00–$49.99 | −5.10 (−6.07, −4.14) |
|
| |
| Distance traveled from home (miles) | −0.02 (−0.05, 0.01) |
|
| |
| Payment type (ref: cash or check) | |
| SNAP (any) | 0.26 (−0.94, 1.46) |
| WIC | 8.29 (5.57, 11.00) |
| Debit card | 0.37 (−0.65, 1.39) |
| Credit card | 1.45 (0.22, 2.68) |
| Other (TANF or gift card) | 2.37 (−3.23, 7.82) |
Based on the complete case (non-missing) total of n=10,789
Abbreviations used: HEI (Healthy Eating Index), FPL (Federal Poverty Level), SNAP (Supplemental Nutrition Assistance Program), HS (high school degree), GED (General Equivalency Diploma), WIC (Special Supplemental Nutrition Program for Women, Infants and Children), TANF (Temporary Assistance for Needy Families Program)
Significant associations were also observed between the purchase amount and HEI score, with smaller purchases having significantly lower values. Compared to paying by cash or check, WIC purchases (made with food-specific WIC vouchers) had significantly higher HEI scores (β=8.29, CI=5.57, 11.00), as did those made with credit cards (β=1.45, CI=0.22, 2.68). Purchases made in the third or fourth weeks of the month were significantly less healthy than those made during the first seven days of the month. See Figure 1 and Table 3 for all variable coefficients and confidence intervals.
Figure 1.
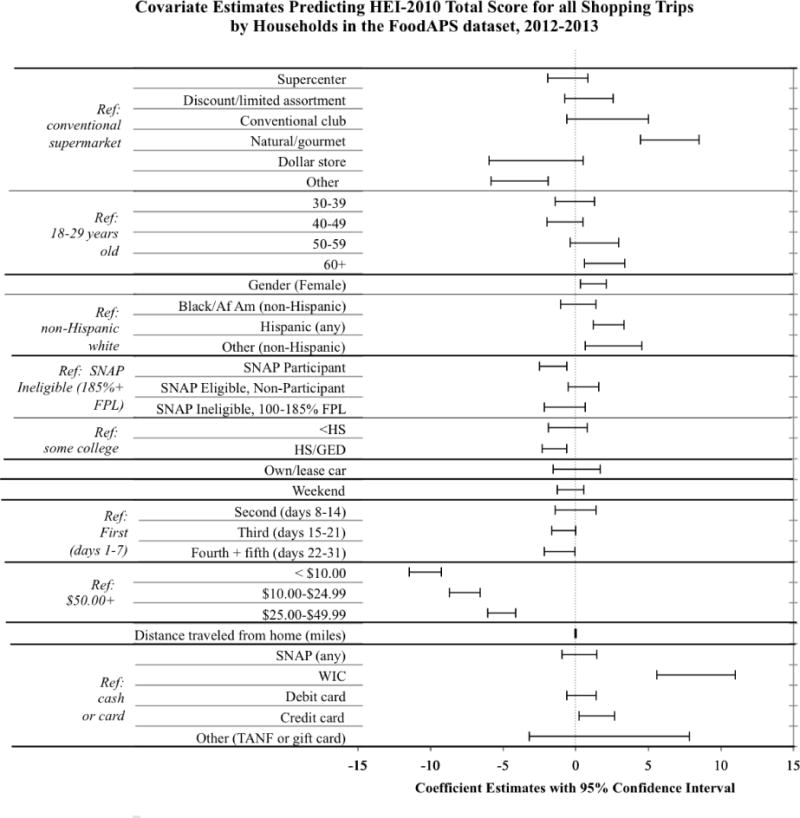
Covariate Estimates Predicting HEI-2010 Total Score for all Shopping Trips by Households in the FoodAPS dataset, 2012–2013
Differences in HEI Component Scores between Conventional Supermarkets and Discount/Limited Assortment Stores
Descriptive statistics of HEI scores from transactions at discount/limited assortment stores compared to supermarkets offer nuanced results (see Figure 2 and Supplemental Table A); only differences that represented more than five percent of a possible component score are reported below. For SNAP participants, purchases at discount/limited assortment stores were healthier, on average, for total vegetables (12% higher HEI component score), total protein foods (9% higher), seafood and plant proteins (7% higher) and sodium (16% higher). SNAP-eligible non-participants also had higher total vegetables and total protein foods at discount/limited assortment stores (8% higher for both), and had 9% lower HEI scores for dairy and sodium. SNAP-ineligible households with incomes over 185% FPL had, on average, higher HEI scores for total fruits, whole fruits, and total vegetables at discount/limited assortment stores (6%, 9%, and 11%, respectively), and lower scores for whole grains (9% lower). At discount/limited assortment stores, SNAP-ineligible households with lower incomes (100-185% FPL) had higher average HEI component scores for seafood and plant proteins (8% higher) and sodium (17% higher), and lower scores for total fruits (6% lower), whole fruits (16% lower), greens and beans (8% lower), whole grains (10% lower), and total protein foods (12% lower).
Figure 2.
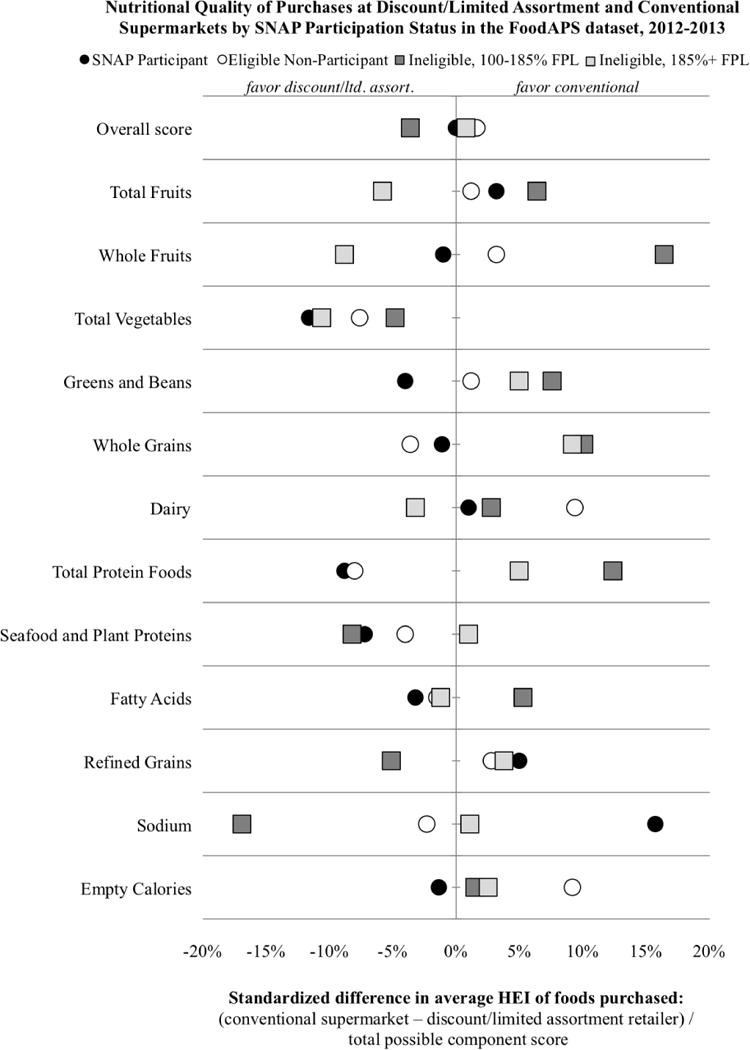
Nutritional Quality of Purchases at Discount/Limited Assortment and Conventional Supermarkets by SNAP Participation Status in the FoodAPS dataset, 2012–2013
For all SNAP participation categories (e.g., participant, eligible non-participant, not eligible), discount/limited assortment purchases had higher average HEI component scores for fatty acids, greens and beans, and total vegetables. On average, all SNAP participation categories had higher (healthier) refined grain scores at conventional supermarkets. Other HEI component scores varied between favoring discount/limited assortment and conventional supermarkets based on the SNAP participation status of the household (see Figure 2 and Table 2). Most purchases at conventional supermarkets were by non-SNAP eligible participants (44.1%), especially those with incomes over 185% FPL (37.4%), while most purchases at discount/limited assortment stores were made by SNAP participants (42.0%).
DISCUSSION
Our analysis of the nationally representative FoodAPS dataset is consistent with many smaller studies of food shopping in the United States in terms of where household buy healthy and unhealthy foods (Cannuscio et al., 2014; Vaughan et al., 2017; Ver Ploeg et al., 2015). We find that conventional supermarkets are the most common food shopping destination, representing over half of all shopping trips in this sample (54.4%). Compared to conventional supermarket transactions, average HEI scores were significantly higher at natural/gourmet stores, and lower at “other” retailers, namely corner and convenience stores. While neither of these findings are surprising given the context of these trips (e.g., choice of a natural/gourmet store, in-store environment with healthy options, etc.) and previous literature (e.g., healthy food availability and purchasing at corner stores), we were surprised to find that discount/limited assortment store trips did not differ significantly, but, on average, were comparable to those made at conventional supermarkets. Direct comparison of HEI component scores suggests that much of this difference is attributable to proportion of purchases comprised of vegetables at discount/limited assortment stores (total vegetable score mean=2.75, median=3.14) compared to conventional supermarkets (mean=2.27, median=1.80). Notably, total vegetable scores for trips to limited assortment stores were on average higher for participants across all income categories, and approximately higher by 12% (of the possible HEI score) than trips to conventional supermarkets for SNAP participants. Among SNAP participants, discount/limited assortment stores had higher average HEI component scores than conventional supermarket trips for 8/12 categories, while SNAP-eligible non-participants had higher components scores for 6/12 categories. While relatively small sample size may present another explanation for this finding (discount/limited assortment stores represent only 5.0% of trips), these retailers appear to be at least comparable with conventional supermarkets in terms of the healthfulness of purchases made.
Purchases made at “other” retailers (including corner and convenience stores) had significantly lower HEI scores compared to conventional supermarkets, consistent with other literature examining the nutritional quality of foods sold at these types of retailers (Caspi et al., 2017). From the descriptive statistics in Table 3, we see that these types of retailers had lower average values for all HEI component scores, compared to conventional supermarkets. Additionally, the average amount spent at these retailers was just over half of that spent at conventional supermarkets ($20.67 at “other” retailers versus $35.29 at conventional supermarkets).
Use of SNAP benefits was not significantly related to HEI outcomes. This runs contrary to one recent study of transactions involving specific food items within a Northeastern supermarket chain that found select unhealthy foods more likely to be purchased with SNAP benefits (Franckle et al., 2017), as well as to broader public policy discourse that often associates SNAP use with unhealthy purchasing (Barnhill, 2011; Chrisinger, 2017; Leung et al., 2013; Long et al., 2014). Still, this finding raises questions about why and how SNAP fell short of delivering on its namesake promise of “nutrition,” and possible avenues for improvement, such as the modest success of the Healthy Incentives Pilot, which offered participants additional SNAP bonuses when purchases were made on eligible healthy items (Bartlett et al., 2014; Klerman et al., 2014; Wilde et al., 2015). Conversely, we found that healthier transactions were predicted by WIC use. One straightforward explanation for the correlation of HEI with WIC use is the voucher-based nature of the program, which provides benefits that can be used only for designated healthy food items. Furthermore, the set of allowable food items within the WIC program was revised in 2009, with an emphasis on increasing participants’ purchasing of vegetables, fruits, whole grains, and low-fat diary, all items that would favorably increase the HEI score of a food shopping trip (Guenther et al., 2013; Schultz et al., 2015).
Households who were income-ineligible for SNAP purchased significantly healthier items on food shopping trips compared to participants with lower incomes. One possible interpretation of this pattern is the influence of SES on diet. Compared to higher-SES status, lower-SES has been correlated with lower dietary quality in both metropolitan- and national-level studies in a graded manner (e.g., additional income yields dietary improvements, even for individuals with adequate food security), with the gap between these groups widening between 2000 and 2010 (Darmon and Drewnowski, 2008; Drewnowski, 2014; Drewnowski et al., 2016a; Drewnowski and Eichelsdoerfer, 2010; Wang et al., 2014). Factors such as poor physical access to food retailers, higher prices for healthy foods, lower nutritional knowledge, limited time for shopping or cooking, or the high palatability and low satiety value of less-healthy foods have been identified as possible causal mechanisms explaining this relationship (Darmon and Drewnowski, 2008). In our study, the influence of SES on diet may also be illustrated by the positive and significant relationship with HEI among relevant indicators, including educational attainment, use of credit, and income above the SNAP eligibility threshold (Darmon and Drewnowski, 2008; Littwin, 2007).
Limitations
This study has several limitations. First, the FoodAPS dataset only represents one week of purchasing data per household. While making a rich dataset, it may still obscure important food purchasing habits of some households, especially those, like SNAP shoppers, who often make one or two large shopping trips per month (Hamrick and Andrews, 2016; Whiteman et al., in review). Second, while we analyzed the nutritional value of purchases made at different retailers with HEI, we do not actually know about household eating patterns. Thus, it is impossible to know how foods were prepared, or if they were shared equally between household members. Still, we believe it to be a reasonably robust and clinically relevant measure, as previous research has shown significant associations between diet and HEI, and between HEI and health outcomes (Guenther et al., 2013; Liese et al., 2015; McCullough et al., 2000, 2000; Rathod et al., 2012). Finally, we rely on a store classification system that allows us to analyze potentially meaningful differences between stores, though unobserved nuances are likely to exist within the largest category of conventional supermarket, such as store-specific merchandizing and promotions, presence of specific in-store departments (e.g., pharmacy, bakery, deli, etc.), and availability of culturally-relevant products. Further research should seek to incorporate additional store variables, such as in-store pricing or promotion strategies, to better capture difference between types of retailers.
Conclusion
A variety of individual and contextual factors influence how food shopping decisions are made, including where to shop and what to purchase. In this study, we used a nationally-representative dataset to analyze the relative healthfulness of purchases made at different types of retailers, adjusting for a variety of individual, store, and trip characteristics. We found that the majority of trips were to conventional supermarkets, and that these transactions were significantly healthier than those made at “other” retailers (e.g., corner and convenience stores), and significantly less healthy than those made at natural/gourmet stores. Households of lower socio-economic status also made significantly less healthy purchases compared to households with higher incomes. In sum, this study provides a picture of food shopping behaviors across the United States, and spotlights potential populations and locations for future interventions.
Supplementary Material
Highlights.
Trips to natural/gourmet stores were healthier overall (versus conventional supermarkets)
Trips to “other” smaller retailers were less healthy overall (versus conventional supermarkets)
Individual factors related to a trip’s HEI score included age, female gender, and race/ethnicity
Trip factors related to a trip’s HEI score included week of the month, amount spent, and payment type
Household SNAP participation was related to less-healthy trips, yet use of SNAP for payment was not
Acknowledgments
This research was supported by a grant through the University of Kentucky Center for Poverty Research FoodAPS Research Initiative, funded by the USDA Economic Research Service. The lead author was also supported by a National Science Foundation Graduate Research Fellowship and an NIH/NHLBI Institutional Training Grant (T32 HL007034) during the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts of interest to declare.
References
- Barnhill A. Impact and Ethics of Excluding Sweetened Beverages From the SNAP Program. Am J Public Health. 2011;101:2037–2043. doi: 10.2105/AJPH.2011.300225. https://doi.org/10.2105/AJPH.2011.300225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett S, Klerman J, Olsho L, et al. Evaluation of the Healthy Incentives Pilot (HIP) (Final Report) 2014. (Prepared by Abt Associates for the U.S. Department of Agriculture, Food and Nutrition Service). [Google Scholar]
- Cannuscio CC, Hillier A, Karpyn A, Glanz K. The social dynamics of healthy food shopping and store choice in an urban environment. Soc Sci Med. 2014;122:13–20. doi: 10.1016/j.socscimed.2014.10.005. https://doi.org/10.1016/j.socscimed.2014.10.005. [DOI] [PubMed] [Google Scholar]
- Caspi CE, Lenk K, Pelletier JE, Barnes TL, Harnack L, Erickson DJ, Laska MN. Food and beverage purchases in corner stores, gas-marts, pharmacies and dollar stores. Public Health Nutr. 2017;20:2587–2597. doi: 10.1017/S1368980016002524. https://doi.org/10.1017/S1368980016002524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrisinger B. A Mixed-Method Assessment of a New Supermarket in a Food Desert: Contributions to Everyday Life and Health. J Urban Health. 2016;93:425–37. doi: 10.1007/s11524-016-0055-8. https://doi.org/10.1007/s11524-016-0055-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrisinger BW. Ethical imperatives against item restriction in the Supplemental Nutrition Assistance Program. Prev Med. 2017;100:56–60. doi: 10.1016/j.ypmed.2017.04.009. https://doi.org/10.1016/j.ypmed.2017.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrisinger BW, DiSantis KI, Hillier A, Kumanyika SK. Purchases of High- and Low-Calorie Foods in Full-service Supermarkets and Other Food Retailers in an Urban Setting. doi: 10.1016/j.pmedr.2018.02.018. in review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87:1107–1117. doi: 10.1093/ajcn/87.5.1107. [DOI] [PubMed] [Google Scholar]
- DiSantis KI, Hillier A, Holaday R, Kumanyika S. Why do you shop there? A mixed methods study mapping household food shopping patterns onto weekly routines of black women. Int J Behav Nutr Phys Act. 2016;13:11. doi: 10.1186/s12966-016-0333-6. https://doi.org/10.1186/s12966-016-0333-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A. The Geography of Diabetes by Census Tract in a Large Sample of Insured Adults in King County, Washington, 2005-2006. Prev Chronic Dis. 2014;11 doi: 10.5888/pcd11.140135. https://doi.org/10.5888/pcd11.140135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A, Aggarwal A, Cook A, Stewart O, Moudon AV. Geographic disparities in Healthy Eating Index scores (HEI–2005 and 2010) by residential property values: Findings from Seattle Obesity Study (SOS) Prev Med. 2016a;83:46–55. doi: 10.1016/j.ypmed.2015.11.021. https://doi.org/10.1016/j.ypmed.2015.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A, Aggarwal A, Tang W, Hurvitz PM, Scully J, Stewart O, Moudon AV. Obesity, diet quality, physical activity, and the built environment: the need for behavioral pathways. BMC Public Health. 2016b;16:1153. doi: 10.1186/s12889-016-3798-y. https://doi.org/10.1186/s12889-016-3798-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A, Eichelsdoerfer P. Can Low-Income Americans Afford a Healthy Diet? Nutr Today. 2010;44:246–249. doi: 10.1097/NT.0b013e3181c29f79. https://doi.org/10.1097/NT.0b013e3181c29f79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franckle RL, Moran A, Hou T, Blue D, Greene J, Thorndike AN, Polacsek M, Rimm EB. Transactions at a Northeastern Supermarket Chain: Differences by Supplemental Nutrition Assistance Program Use. Am J Prev Med. 2017 doi: 10.1016/j.amepre.2017.06.019. https://doi.org/10.1016/j.amepre.2017.06.019. [DOI] [PMC free article] [PubMed]
- Glanz K, Sallis JF, Saelens BE, Frank LD. Healthy Nutrition Environments: Concepts and Measures. Am J Health Promot. 2005;19:330–333. doi: 10.4278/0890-1171-19.5.330. https://doi.org/10.4278/0890-1171-19.5.330. [DOI] [PubMed] [Google Scholar]
- Guenther PM, Casavale KO, Kirkpatrick SI, Reedy J, Hiza HAB, Kuczynski KJ, Kahle LL, Krebs-Smith SM. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013;113 doi: 10.1016/j.jand.2012.12.016. https://doi.org/10.1016/j.jand.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson A. Shopping pattern and food purchase differences among Supplemental Nutrition Assistance Program (SNAP) households and Non-supplemental Nutrition Assistance Program households in the United States. Prev Med Rep. 2017;7:152–157. doi: 10.1016/j.pmedr.2017.06.005. https://doi.org/10.1016/j.pmedr.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson A, Christian JW, Lewis S, Moore K, Jilcott S. Food venue choice, consumer food environment, but not food venue availability within daily travel patterns are associated with dietary intake among adults, Lexington Kentucky 2011. Nutr J. 2013;12:17. doi: 10.1186/1475-2891-12-17. https://doi.org/10.1186/1475-2891-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson AA, Sharkey J, Samuel-Hodge CD, Jones-Smith JC, Cai J, Ammerman AS. Food Store Environment Modifies Intervention Effect on Fruit and Vegetable Intake among Low-Income Women in North Carolina. J Nutr Metab. 2012;2012:932653. doi: 10.1155/2012/932653. https://doi.org/10.1155/2012/932653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamrick KS, Andrews M. SNAP Participants’ Eating Patterns over the Benefit Month: A Time Use Perspective. PLOS ONE. 2016;11:e0158422. doi: 10.1371/journal.pone.0158422. https://doi.org/10.1371/journal.pone.0158422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillier A, Cannuscio CC, Karpyn A, McLaughlin J, Chilton M, Glanz K. How Far Do Low-Income Parents Travel to Shop for Food? Empirical Evidence from Two Urban Neighborhoods. Urban Geogr. 2011;32:712–729. https://doi.org/10.2747/0272-3638.32.5.712. [Google Scholar]
- Hillier A, Smith T, Cannuscio CC, Karpyn A, Glanz K. A discrete choice approach to modeling food store access. Environ Plan B Plan Des. 2015;42:263–278. [Google Scholar]
- Hillier A, Smith TE, Whiteman ED, Chrisinger BW. Discrete Choice Model of Food Store Trips Using National Household Food Acquisition and Purchase Survey (FoodAPS) Int J Environ Res Public Health. 2017;14:1133. doi: 10.3390/ijerph14101133. https://doi.org/10.3390/ijerph14101133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch JA, Hillier A. Exploring the Role of the Food Environment on Food Shopping Patterns in Philadelphia, PA, USA: A Semiquantitative Comparison of Two Matched Neighborhood Groups. Int J Environ Res Public Health. 2013;10:295–313. doi: 10.3390/ijerph10010295. https://doi.org/10.3390/ijerph10010295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jilcott SB, Wall-Bassett ED, Moore JB, Sharkey JR. Use of Traditional and Nontraditional Food Venues Among Female Participants in the Supplemental Nutrition Assistance Program (SNAP) J Hunger Environ Nutr. 2011;6:64–74. https://doi.org/10.1080/19320248.2011.551028. [Google Scholar]
- Kerr J, Frank L, Sallis JF, Saelens B, Glanz K, Chapman J. Predictors of trips to food destinations. Int J Behav Nutr Phys Act. 2012;9:1–10. doi: 10.1186/1479-5868-9-58. https://doi.org/10.1186/1479-5868-9-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klerman JA, Bartlett S, Wilde P, Olsho L. The Short-Run Impact of the Healthy Incentives Pilot Program on Fruit and Vegetable Intake. Am J Agric Econ. 2014;96:1372–1382. https://doi.org/10.1093/ajae/aau023. [Google Scholar]
- Laska MN, Borradaile KE, Tester J, Foster GD, Gittelsohn J. Healthy food availability in small urban food stores: a comparison of four US cities. Public Health Nutr. 2010;13:1031–1035. doi: 10.1017/S1368980009992771. https://doi.org/10.1017/S1368980009992771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laska MN, Caspi CE, Pelletier JE, Friebur R, Harnack LJ. Lack of Healthy Food in Small-Size to Mid-Size Retailers Participating in the Supplemental Nutrition Assistance Program, Minneapolis–St. Paul, Minnesota, 2014. Prev Chronic Dis. 2015;12 doi: 10.5888/pcd12.150171. https://doi.org/10.5888/pcd12.150171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung CW, Hoffnagle EE, Lindsay AC, Lofink HE, Hoffman VA, Turrell S, Willett WC, Blumenthal SJ. A Qualitative Study of Diverse Experts’ Views about Barriers and Strategies to Improve the Diets and Health of Supplemental Nutrition Assistance Program (SNAP) Beneficiaries. J Acad Nutr Diet. 2013;113:70–76. doi: 10.1016/j.jand.2012.09.018. https://doi.org/10.1016/j.jand.2012.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liese AD, Krebs-Smith SM, Subar AF, George SM, Harmon BE, Neuhouser ML, Boushey CJ, Schap TE, Reedy J. The Dietary Patterns Methods Project: Synthesis of Findings across Cohorts and Relevance to Dietary Guidance. J Nutr. 2015;145:393–402. doi: 10.3945/jn.114.205336. https://doi.org/10.3945/jn.114.205336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littwin A. Beyond Usury: A Study of Credit-Card Use and Preference among Low-Income Consumers. Tex Law Rev. 2007;86:451–506. [Google Scholar]
- Long MW, Leung CW, Cheung LWY, Blumenthal SJ, Willett WC. Public support for policies to improve the nutritional impact of the Supplemental Nutrition Assistance Program (SNAP) Public Health Nutr. 2014;17:219–224. doi: 10.1017/S136898001200506X. https://doi.org/10.1017/S136898001200506X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough ML, Feskanich D, Rimm EB, Giovannucci EL, Ascherio A, Variyam JN, Spiegelman D, Stampfer MJ, Willett WC. Adherence to the Dietary Guidelines for Americans and risk of major chronic disease in men. Am J Clin Nutr. 2000;72:1223–1231. doi: 10.1093/ajcn/72.5.1223. [DOI] [PubMed] [Google Scholar]
- Rathod AD, Bharadwaj AS, Badheka AO, Kizilbash M, Afonso L. Healthy Eating Index and Mortality in a Nationally Representative Elderly Cohort. Arch Intern Med. 2012;172:275–277. doi: 10.1001/archinternmed.2011.1031. https://doi.org/10.1001/archinternmed.2011.1031. [DOI] [PubMed] [Google Scholar]
- Rhone A, Ver Ploeg M, Dicken C, Williams R, Breneman V. Low-Income and Low-Supermarket-Access Census Tracts, 2010-2015. U.S. Department of Agriculture, Economic Research Service; 2017. (Economic Information Bulletin No EIB-165). [Google Scholar]
- Rose D, Richards R. Food store access and household fruit and vegetable use among participants in the US Food Stamp Program. Public Health Nutr. 2004;7:1081–1088. doi: 10.1079/PHN2004648. https://doi.org/10.1079/PHN2004648. [DOI] [PubMed] [Google Scholar]
- Schultz DJ, Byker Shanks C, Houghtaling B. The Impact of the 2009 Special Supplemental Nutrition Program for Women, Infants, and Children Food Package Revisions on Participants: A Systematic Review. J Acad Nutr Diet. 2015;115:1832–1846. doi: 10.1016/j.jand.2015.06.381. https://doi.org/10.1016/j.jand.2015.06.381. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture, Food and Nutrition Service, Office of Policy Support. Characteristics of Supplemental Nutrition Assistance Program Households: Fiscal Year 2016. Alexandria, VA: 2017. (Food and Nutrition Service (No. SNAP-17-CHAR), Supplemental Nutrition Assistance Program Nutrition Assistance Program Report Series). [Google Scholar]
- USDA Economic Research Service. FoodAPS National Household Food Acquisition and Purchase Survey [WWW Document] 2016 URL http://www.ers.usda.gov/data-products/foodaps-national-household-food-acquisition-and-purchase-survey.aspx (accessed 5.13.16)
- USDA Food and Nutrition Service. Women, Infants, and Children (WIC) | Food and Nutrition Service [WWW Document] n.d. URL https://www.fns.usda.gov/wic/women-infants-and-children-wic (accessed 1.3.18)
- Vaughan CA, Cohen DA, Ghosh-Dastidar M, Hunter GP, Dubowitz T. Where do food desert residents buy most of their junk food? Supermarkets Public Health Nutr. 2017;20:2608–2616. doi: 10.1017/S136898001600269X. https://doi.org/10.1017/S136898001600269X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ver Ploeg M, Mancino L, Todd J, Clay DM, Scharadin B. Where Do Americans Usually Shop for Food and How Do They Travel To Get There? U.S. Department of Agriculture, Economic Research Service; Washington, DC: 2015. (Initial Findings From the National Household Food Acquisition and Purchase Survey (No. EIB-138)). [Google Scholar]
- Wang DD, Leung CW, Li Y, Ding EL, Chiuve SE, Hu FB, Willett WC. Trends in Dietary Quality Among Adults in the United States, 1999 Through 2010. JAMA Intern Med. 2014;174:1587–1595. doi: 10.1001/jamainternmed.2014.3422. https://doi.org/10.1001/jamainternmed.2014.3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteman E, Hillier A, Chrisinger BW. Eating at the End of the Month: Variation in Diet Quality During the Monthly SNAP-Cycle in review. [Google Scholar]
- Wilde P, Klerman JA, Olsho LEW, Bartlett S. Explaining the Impact of USDA’s Healthy Incentives Pilot on Different Spending Outcomes. Appl Econ Perspect. 2015 Policy ppv028. https://doi.org/10.1093/aepp/ppv028.
- Zenk SN, Schulz AJ, Israel BA, Mentz G, Miranda PY, Opperman A, Odoms-Young AM. Food shopping behaviours and exposure to discrimination. Public Health Nutr. 2014;17:1167–1176. doi: 10.1017/S136898001300075X. https://doi.org/10.1017/S136898001300075X. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


